03/07/2017-b.sc-Midwifery-paper-NO.1-juhi done-UPLOAD NO.1
PAPER SOLUTION AS PER REQUIRED ANSWER….
(KINDLY SEND YOUR UNIVERSITY PAPER IMAGE WATS APP ON – 8485976407 – WE PROVIDE ITS SOLUTION AS PER YOUR NEED)
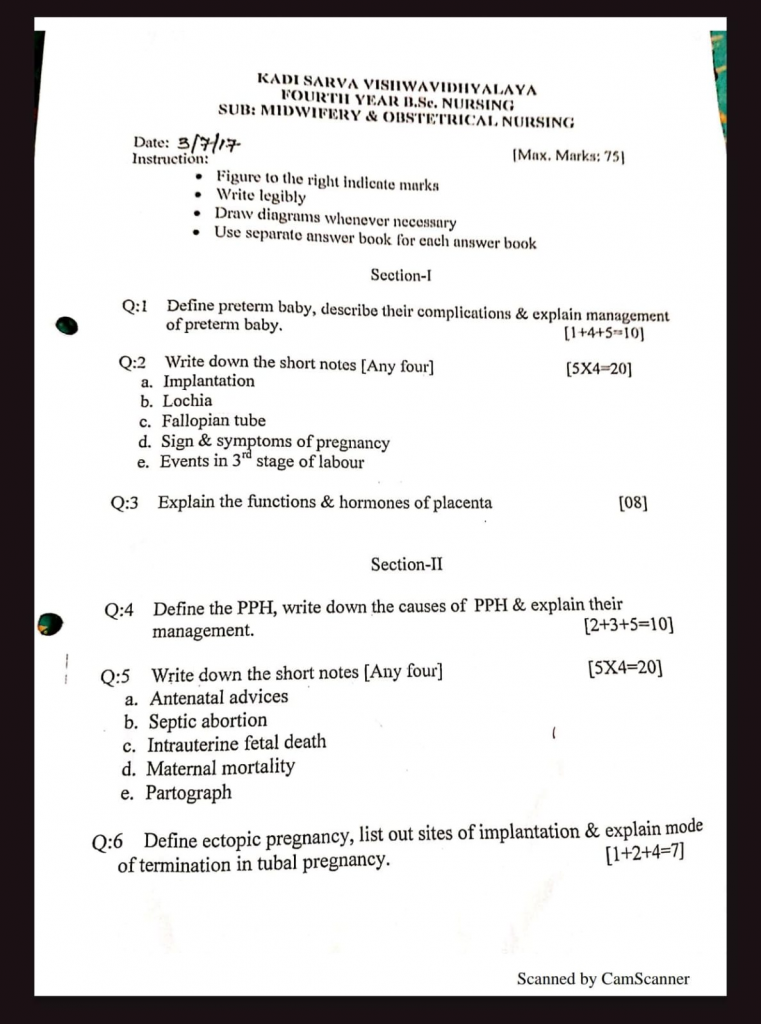
03/07/2017-b.sc-Midwifery-paper-UPLOAD NO.1
Section-1
Q:1 Define preterm baby, describe their complications & explain management of preterm baby. [1 + 4 + 5 = 10
Preterm baby
A preterm baby (also called premature infant) is defined as a baby born alive before 37 completed weeks of gestation (i.e., before 259 days from the first day of the last menstrual period), regardless of birth weight.
Complications of pre term baby
Preterm babies (born before 37 completed weeks of gestation) are at risk of multiple complications due to immature organ systems.
Respiratory Complications
• Respiratory Distress Syndrome (RDS) due to lack of surfactant
• Apnea of prematurity (pauses in breathing)
Thermoregulation Issues
• Hypothermia due to poor subcutaneous fat and immature skin
• Inability to maintain body temperature
Feeding and Digestive Problems
• Poor sucking and swallowing reflexes
• Risk of Necrotizing Enterocolitis (NEC) – a serious intestinal infection
Neurological Complications
• Intraventricular hemorrhage (IVH) – bleeding into the brain
• Delayed milestones and developmental delays
Infections
• Immature immune system increases risk of sepsis, pneumonia, and meningitis
Management of preterm baby
Thermal Protection (Prevent Hypothermia)
• Keep the baby in a warm environment (radiant warmer or incubator)
• Use Kangaroo Mother Care (KMC) for skin-to-skin warmth
• Cover the head and extremities to reduce heat loss
Respiratory Support
• Monitor for Respiratory Distress Syndrome (RDS)
• Provide oxygen therapy or CPAP if needed
• Administer surfactant (in NICU setting) for lung immaturity
Nutritional Support
• Encourage breast milk feeding (expressed milk if unable to suck)
• Use nasogastric (NG) or orogastric feeding initially
• Gradually shift to direct breastfeeding as baby matures
Infection Prevention
• Maintain strict hand hygiene and aseptic techniques
• Monitor for signs of sepsis (fever, lethargy, poor feeding)
• Give antibiotics if infection is suspected
Monitoring and Supportive Care
• Monitor vital signs, weight, and urine/stool output regularly
• Observe for jaundice, apnea, or convulsions
• Provide developmental care in a calm, low-stimulation environment
Parental Education and Involvement
• Teach parents kangaroo care, feeding, hygiene, and danger signs
• Encourage emotional bonding and follow-up visits
Q:2 Write down the short notes [Any four] [5 x 4 = 20]
a. Implantation
Definition
Implantation is the process by which the fertilized ovum (blastocyst) attaches and embeds itself into the endometrial lining of the uterus to establish a nourishing connection with the maternal blood supply.
Timing of Implantation
• Occurs 6–7 days after fertilization
• Typically completed by 10th day post-fertilization
Process of Implantation
Apposition
The blastocyst comes in close contact with the endometrium (usually in the upper posterior wall of uterus).
Adhesion
The outer layer of the blastocyst (trophoblast) sticks to the endometrial cells.
Invasion
The trophoblast cells proliferate and form two layers :
• Cytotrophoblast (inner layer)
• Syncytiotrophoblast (outer layer which invades endometrium)
These layers erode the endometrium, allowing the embryo to embed itself.
Site of Implantation
Normally : Upper posterior wall of the uterus
Abnormal (ectopic) : Fallopian tube, ovary, cervix, or peritoneal cavity
Importance of Implantation
• Establishes the maternal-fetal interface for nutrition and gas exchange
• Initiates the formation of the placenta
• Critical step for continuation of pregnancy
b. Lochia
Definition
Lochia is the vaginal discharge that occurs after childbirth (normal vaginal delivery or cesarean section), consisting of blood, mucus, and placental tissue. It is a natural process that helps cleanse the uterus as it returns to its pre-pregnancy state (involution).
Duration
Lochia lasts for about 4 to 6 weeks postpartum, gradually changing in color and consistency.
Types of Lochia
1) Lochia Rubra
Color : Bright red
Duration : First 3–4 days postpartum
Content : Blood, fragments of decidua, fetal membranes, and cervical mucus
Characteristic : May contain small clots
2) Lochia Serosa
Color : Pinkish-brown or serous
Duration : From day 4 to day 10
Content : Serous fluid, leukocytes, old blood, and wound exudate
3) Lochia Alba
Color : Yellowish-white
Duration : From day 10 to around 4–6 weeks
Content : Leukocytes, epithelial cells, mucus, and minimal blood
Abnormal Lochia (Warning Signs) :
• Foul odor – may indicate infection
• Return to red lochia after it lightens
• Excessive bleeding or large clots
• Fever, pelvic pain, or uterine tenderness
Nursing Considerations
• Monitor the amount, color, and odor of lochia during postpartum assessments.
• Educate the mother on normal versus abnormal changes.
• Encourage proper perineal hygiene to prevent infection.
• Report signs of infection or hemorrhage to the physician promptly.
c. Fallopian tube
Definition
The fallopian tubes (also known as uterine tubes or oviducts) are paired muscular tubes in the female reproductive system that connect the ovaries to the uterus. They serve as the site of fertilization and help transport the ovum (egg) from the ovary to the uterus.
Anatomical Structure
Each fallopian tube is approximately 10–12 cm long and has four parts:
Infundibulum
• Funnel-shaped, open end near the ovary
• Contains fimbriae (finger-like projections) that catch the ovum during ovulation
Ampulla
• Longest and widest portion
• Site of fertilization in most cases
Isthmus
• Narrow, muscular part
• Connects ampulla to the uterine wall
Interstitial (Intramural) Part
Passes through the uterine wall and opens into the uterine cavity
Functions of Fallopian Tube
• Capture of ovum after ovulation using fimbriae
• Transport of ovum toward the uterus using cilia and peristaltic movements
• Site of fertilization (usually in the ampulla)
• Supports early embryonic transport to the uterine cavity for implantation
Clinical Significance
• Ectopic pregnancy often occurs in the fallopian tube (especially the ampulla)
• Tubal block can cause infertility
• Tubectomy (surgical ligation of fallopian tubes) is a method of female sterilization
d. Sign & symptoms of pregnancy
The signs and symptoms of pregnancy are the physical and physiological changes that occur in a woman’s body due to conception and implantation of a fertilized ovum. These signs are categorized into presumptive, probable, and positive signs based on their diagnostic value.
Presumptive Signs (Subjective – Felt by the Woman)
These are not conclusive as they may be caused by other conditions too.
• Amenorrhea (absence of menstruation)
• Nausea and vomiting (especially in the morning)
• Breast changes (tenderness, enlargement, darkened areola)
• Fatigue and drowsiness
• Increased urination
• Quickening (feeling of fetal movement around 18–20 weeks)
Probable Signs (Objective – Observed by the Examiner
These are more suggestive but not definitive of pregnancy.
• Positive pregnancy test (urine hCG test)
• Abdominal enlargement
• Chadwick’s sign : bluish discoloration of cervix and vagina
• Hegar’s sign : softening of the uterine isthmus
• Goodell’s sign : softening of the cervix
• Braxton Hicks contractions (painless, irregular uterine contractions)
Positive Signs (Diagnostic – Confirm Pregnancy)
These signs confirm pregnancy with certainty.
• Fetal heart sounds (by Doppler at ~10–12 weeks or stethoscope at ~18–20 weeks)
• Visualization of fetus on ultrasound
• Palpation of fetal movements by the examiner
e. Events in 3 (rd) stage of labour
Definition
The third stage of labour is the period between the delivery of the baby and the expulsion of the placenta and membranes. It usually lasts about 5–30 minutes.
Major Events in the Third Stage
Uterine Contraction and Retraction
• After the birth of the baby, the uterus continues to contract.
• These contractions cause the placenta to separate from the uterine wall.
Placental Separation
• The decidua basalis layer separates from the placenta.
Signs of placental separation include :
• Sudden gush of blood
• Lengthening of the umbilical cord
• Rising and firm uterus
Descent and Expulsion of the Placenta
• The separated placenta descends into the lower uterine segment and vagina.
• It is expelled either spontaneously or with controlled cord traction (e.g., Modified Brandt–Andrews technique).
Expulsion of Membranes
• Follows the placenta or may be gently removed.
• Should be inspected for completeness to avoid retained fragments.
Uterine Contraction and Hemostasis
• The uterus contracts firmly to close maternal blood vessels.
• Uterine massage and uterotonics (e.g., oxytocin) are administered to promote contraction and prevent postpartum hemorrhage (PPH).
Q:3 Explain the functions & hormones of placenta [08]
The placenta is a temporary yet vital organ formed during pregnancy that connects the developing fetus to the uterine wall. It plays a crucial role in nutrition, respiration, excretion, protection, hormone production, and immune support.
Functions of the Placenta
Respiratory Function (Gas Exchange)
• Facilitates exchange of oxygen and carbon dioxide between mother and fetus via diffusion.
Nutritional Function
• Transfers essential nutrients like glucose, amino acids, fatty acids, vitamins, and minerals from maternal to fetal blood.
Excretory Function
• Removes fetal waste products such as urea, uric acid, bilirubin, and carbon dioxide to maternal circulation for excretion.
Protective Function
• Acts as a partial barrier against harmful substances (though not completely), and provides immunoglobulin G (IgG) to the fetus for passive immunity.
Endocrine (Hormonal) Function
• Produces important hormones required for the maintenance of pregnancy and fetal development (explained below).
Hormones Produced by the Placenta (4 Key Hormones)
Human Chorionic Gonadotropin (hCG)
• Detected in early pregnancy tests
• Maintains the corpus luteum → continuous production of progesterone and estrogen in early pregnancy
Human Placental Lactogen (hPL)
• Also called hCS – human chorionic somatomammotropin)
• Modifies maternal metabolism to favor fetal nutrition
• Increases maternal insulin resistance, promotes lipolysis, and helps in breast development
Estrogen (mainly Estriol)
• Helps in uterine growth, mammary gland development, and increased uteroplacental blood flow
Progesterone
• Maintains endometrial lining
• Suppresses uterine contractions
• Prepares breasts for lactation
Additional Hormones (Minor)
Relaxin – Relaxes pelvic ligaments and cervix
Prostaglandins – Help in cervical ripening and uterine contractions at term
Section-II
Q:4 Define the PPH, write down the causes of PPH & explain their management. [2 + 3 + 5 = 10]
Postpartum Hemorrhage (PPH)
Postpartum Hemorrhage (PPH) is defined as Blood loss of 500 ml or more after vaginal delivery or 1000 ml or more after cesarean section within 24 hours of childbirth (primary PPH) or after 24 hours to 6 weeks postpartum (secondary PPH).
Causes of Postpartum Hemorrhage (PPH)
PPH is classified based on causative factors, often summarized using the mnemonic “4 T’s”:
1) Tone (Uterine Atony) : ~70–80%
• Most common cause of PPH
• Uterus fails to contract after delivery
Seen in :
• Overdistended uterus (twins, polyhydramnios)
• Prolonged or rapid labor
• Use of uterine relaxants (e.g., magnesium sulfate)
• Grand multiparity
2) Trauma : ~10–15%
• Injury to birth canal during delivery
Includes :
• Vaginal or cervical lacerations
• Uterine rupture
• Uterine inversion
• Episiotomy complications
• Forceps or vacuum-assisted delivery
3) Tissue : ~5–10%
• Retained placental tissue or membranes
Placental abnormalities :
• Retained cotyledons
• Placenta accreta, increta, or percreta
• Prevents uterine contraction → continued bleeding
4) Thrombin (Coagulopathy) – <1%
• Clotting disorders or inability to form clots
Examples :
• DIC (Disseminated Intravascular Coagulation)
• HELLP syndrome
• Pre-existing conditions : hemophilia, ITP
• Abruptio placentae or fetal death in uteros
Management of post partum hemorrhage (PPH)
Immediate Assessment and Stabilization
• Assess vital signs : BP, pulse, respiration, oxygen saturation.
• Start high-flow oxygen (via face mask or nasal cannula).
• Establish two large-bore IV lines (16G/18G)
• Begin IV fluid resuscitation with crystalloids (e.g., Ringer lactate or NS).
• Send blood for cross-matching, CBC, coagulation profile.
Uterotonic Drug Administration
• Give Injection Oxytocin 10 units IM/IV slowly.
• If bleeding continues, administer :
• Methylergometrine 0.2 mg IM
• Carboprost 250 mcg IM (repeat every 15 min up to max 2 mg)
• Misoprostol 800–1000 mcg per rectum
Identify and Treat Underlying Cause (4 Ts)
• Tone : Massage the uterus if atonic.
• Tissue : Check and remove retained placenta or membranes.
• Trauma : Inspect birth canal for tears or lacerations; repair surgically.
• Thrombin : Manage clotting abnormalities with blood products (FFP, platelets).
Advanced Interventions (If Needed) :
• Bakri balloon or uterine tamponade.
• Uterine artery ligation or B-Lynch sutures in refractory cases.
• Hysterectomy as a last resort if life-threatening bleeding persists
Nursing Management of Postpartum
• Hemorrhage Quickly assess vital signs : pulse, BP, respiration, temperature, oxygen saturation.
• Monitor uterine tone, fundal height, and vaginal bleeding.
• Record the amount and color of blood loss.
• Watch for signs of shock: cold clammy skin, pallor, restlessness Insert two large-bore IV cannulas (16G/18G).
• Administer crystalloids (e.g., normal saline or Ringer lactate) rapidly.
• Prepare for blood transfusion if necessary; send blood for grouping and cross-matching.
• Give prescribed uterotonics to contract the uterus :
• Oxytocin IV/IM
• Methylergometrine
• Carboprost or Misoprostol
• Record drug name, dose, route, and time accurately.
• Place the mother in flat or Trendelenburg position to improve circulation.
• Provide reassurance and emotional support to the mother and family.
• Educate on signs of recurrent bleeding and importance of postpartum follow-up.
Q:5 Write down the short notes [Any four] [5 X 4 = 20]
a. Antenatal advices
Definition
Antenatal advice refers to the information, guidance, and education given to a pregnant woman during the antenatal period (before childbirth) to ensure the health and well-being of both the mother and fetus.
Key Areas of Antenatal Advice
Nutrition & Diet
• Eat a balanced diet rich in protein, iron, calcium, and folic acid.
• Take Iron and Folic Acid (IFA) tablets regularly.
• Drink plenty of water and avoid junk food.
Personal Hygiene
• Maintain good perineal and breast hygiene.
• Wear loose-fitting and cotton clothes.
• Avoid harsh soaps and keep the skin moisturized.
Rest and Exercise
• Take adequate rest and sleep (at least 8 hours at night and 1–2 hours during the day).
• Practice light exercises or antenatal yoga as advised.
• Avoid lifting heavy weights or strenuous work.
Antenatal Visits
• Minimum 4 ANC visits: 1st trimester (1 visit), 2nd trimester (1 visit), 3rd trimester (2 visits).
• Regular BP, weight, hemoglobin, urine, and fetal growth monitoring.
• Take TT immunization as scheduled.
Warning Signs to Report Immediately
• Bleeding or watery discharge per vagina
• Severe headache or visual disturbances
• Swelling in hands/face
• Decreased fetal movements
• High fever or convulsions
Avoid Harmful Habits
• Do not smoke, consume alcohol, or take unprescribed medications.
• Avoid stress and domestic violence situations.
b. Septic abortion
Definition
Septic abortion refers to an abortion (spontaneous or induced) that is complicated by infection of the uterus and surrounding tissues, leading to sepsis, which can be life-threatening if untreated.
Causes
• Unsafe or unsterile abortion procedures
• Use of non-sterile instruments or materials
• Retained products of conception (e.g., placental tissue)
• Poor hygiene after abortion
• Illegal or self-induced abortion without medical supervision
Signs and Symptoms
• Fever and chills
• Foul-smelling vaginal discharge
• Lower abdominal pain or tenderness
• Heavy or prolonged vaginal bleeding
• Rapid pulse, low BP (signs of septic shock)
• Enlarged, tender uterus
• Nausea, vomiting, or diarrhea
Diagnostic evaluation
• History collection
• Physical examination
• Complete blood count (CBC) : Elevated WBC count
• Ultrasound : Retained products in uterus
• Blood culture and high vaginal swab
• Serum lactate or other sepsis markers
Medical Management
• Hospitalization is required
• Broad-spectrum IV antibiotics :
e.g., Ampicillin + Gentamicin + Metronidazole
• IV fluids to manage shock
• Antipyretics and pain management
• Blood transfusion if anemic or in hemorrhagic shock
Surgical Management
• Evacuation of the uterus via suction curettage or D&E
• Hysterectomy in severe cases with uterine perforation or gangrene
Nursing Management
• Monitor vital signs and sepsis markers
• Strict aseptic precautions maintain
• IV therapy and antibiotic administration
• Emotional support and counseling
• Monitor for signs of shock or organ failure
• Educate on safe abortion practices and contraceptive use
Complications
• Septicemia (blood infection)
• Pelvic abscess
• Peritonitis
• Infertility
• Multi-organ failure
• Death (if not treated promptly)
c. Intrauterine fetal death
Definition
Intrauterine fetal death (IUFD) refers to the death of a fetus in the uterus after the age of 20 weeks of gestation or when the fetus weighs more than 500 grams, but before the onset of labor.
Causes of IUFD
Maternal Causes
• Preeclampsia / Eclampsia
• Diabetes mellitus
• Infections (e.g., syphilis, TORCH infections)
• Trauma or injury
• Rh incompatibility
Fetal Causes
• Congenital anomalies
• Chromosomal disorders
• Multiple umbilical cord knots or accidents
Placental Causes
• Abruptio placentae (premature separation of the placenta)
• Placental insufficiency
• Cord prolapse or true knots
Signs and Symptoms
• Absence of fetal movements
• No fetal heart sounds on auscultation
• Uterus smaller than gestational age
• Brownish vaginal discharge
• Regression of pregnancy symptoms
Diagnostic evaluation
• Ultrasound
• Non-stress test (NST)
• Laboratory tests : CBC, clotting profile, LFT, KFT
Medical Management
• Induction of labor using misoprostol or oxytocin
• Prostaglandin E2 for cervical ripening
• Monitor for retained placenta and coagulation abnormalities
Surgical Management (if indicated)
• Dilatation & Evacuation (D&E) in early gestation
• Cesarean Section if vaginal delivery is not safe
Nursing Care
• Provide emotional and psychological support
• Prepare the mother for induction or surgical procedure
• Monitor for vital signs, bleeding, and infection
• Post-delivery care : uterine tone, lochia, Rh status
• Arrange for grief counseling and support groups
d. Maternal mortality
Definition
Maternal mortality refers to the death of a woman while pregnant or within 42 days of termination of pregnancy, irrespective of the duration and site of pregnancy, from any cause related to or aggravated by the pregnancy or its management, but not from accidental or incidental causes.
Maternal Mortality Ratio (MMR) :
MMR = Number of maternal deathsNumber of live births × 1,00,000 \ Number of live births
It reflects the quality of maternal health care in a region.
Causes of Maternal Mortality
Direct Obstetric Causes
• Hemorrhage (e.g., postpartum hemorrhage)
• Sepsis
• Eclampsia/Preeclampsia
• Obstructed labor
• Unsafe abortion
Indirect Causes
• Anemia
• Malaria, HIV/AIDS, heart disease
• Delayed access to care
Prevention
• Early registration and regular antenatal check-ups
• Skilled birth attendants at delivery
• Availability of emergency obstetric care (EmOC)
• Timely referral to higher centers
• Iron & folic acid supplementation, TT immunization
• Promotion of institutional deliveries
e. Partograph
Definition
A Partograph is a graphical tool used to monitor the progress of labor and record key information about the mother and fetus during childbirth. It is recommended by the World Health Organization (WHO) for use in active labor to ensure safe delivery.
Purposes
• To monitor the progress of labor and detect deviations early.
• To identify complications such as prolonged or obstructed labor.
• To evaluate the fetal condition throughout labor.
• To assess maternal well-being (vital signs, urine output, etc.).
• To assist in making timely clinical decisions, including the need for referral or interventions.
Main Components of Partograph
Fetal Condition
Fetal Heart Rate (FHR) : Monitored every 30 minutes.
Amniotic Fluid : Color and presence (intact, clear, meconium-stained).
Moulding : Overlapping of fetal skull bones.
Labor Progress
Cervical Dilatation : Plotted over time (expectation = 1 cm/hr).
Descent of Fetal Head : Assessed by abdominal palpation.
Uterine Contractions : Duration and frequency (every 30 minutes).
Maternal Condition
Vital Signs : Pulse, BP, temperature (regularly recorded).
Urine Output : Assessed for volume, protein, and ketones.
Medications & Fluids : Noted in the appropriate column.
Key Lines in the Graph
Alert Line : Begins at 4 cm dilation and proceeds at 1 cm/hour. Crossing this line suggests delayed labor progress.
Action Line : Located 4 hours to the right of the alert line. Crossing this line requires medical intervention or referral.
Clinical Importance
• Reduces risk of prolonged labor, obstructed labor, and maternal exhaustion.
• Enhances maternal and neonatal outcomes.
• Promotes evidence-based and timely interventions.
Q:6 Define ectopic pregnancy, list out sites of implantation & explain mode of termination in tubal pregnancy. [1 + 2 + 4 = 7]
Ectopic pregnancy
Ectopic pregnancy is defined as the implantation of a fertilized ovum outside the uterine cavity, most commonly in the fallopian tube (especially the ampullary region), but it may also occur in the ovary, cervix, or abdominal cavity
Sites of implantation in ectopic pregnancy
Ectopic pregnancy refers to implantation outside the uterine cavity. The possible sites include:
1) Tubal Pregnancy (Most Common – ~95%)
• Ampullary region – most common site (70%)
• Isthmic region
• Fimbrial end
• Interstitial (cornual) region
2) Ovarian Pregnancy
3) Cervical Pregnancy
4) Abdominal Pregnancy
Peritoneal surfaces such as bowel, omentum, or pouch of Douglas
5) Cesarean Scar Pregnancy
Implantation at the site of previous cesarean section scar
Modes of Termination
Fallopian tube is not designed to support the growing embryo, the pregnancy cannot continue and eventually terminates in one of the following ways :
Tubal Abortion
• Seen mainly in ampullary and fimbrial pregnancies
• The growing conceptus is expelled through the fimbrial end of the tube into the peritoneal cavity
Types :
Complete : All products of conception expelled
Incomplete : Partial expulsion; remnants may cause internal bleeding
Clinical Signs :
• Abdominal pain
• Vaginal bleeding
Tenderness in the lower abdomen
Signs of internal bleeding (if peritoneal irritation)
Tubal Rupture
Most common in isthmic or interstitial pregnancies
The thin tubal wall ruptures due to pressure from the growing embryo
Occurs typically between 6–10 weeks of gestation
Leads to severe internal hemorrhage – a surgical emergency
Clinical Signs:
Sudden, severe abdominal pain
Signs of hypovolemic shock: pallor, fainting, weak pulse, hypotension
Referred shoulder-tip pain (due to diaphragmatic irritation)
Positive pregnancy test and empty uterus on ultrasound
Chronic Rupture (Chronic Ectopic Pregnancy)
A slow and incomplete rupture
Blood leaks gradually, forming a pelvic hematoma or organized mass
May present weeks later with :
• Chronic pelvic pain
• Irregular bleeding
• Palpable adnexal mass
• Often diagnosed incidentally or during infertility workup
Complications
Following Termination:
• Massive internal bleeding
• Peritonitis
• Shock
• Infertility (due to tubal damage)
• Death, if rupture is unrecognized or untreated
👍👍👍👍ALL THE BEST👍👍👍👍
