B.SC-ADULT HEALTH NURSING-1-PAPER SOLUTION (AUGUST-2024)-PENDING
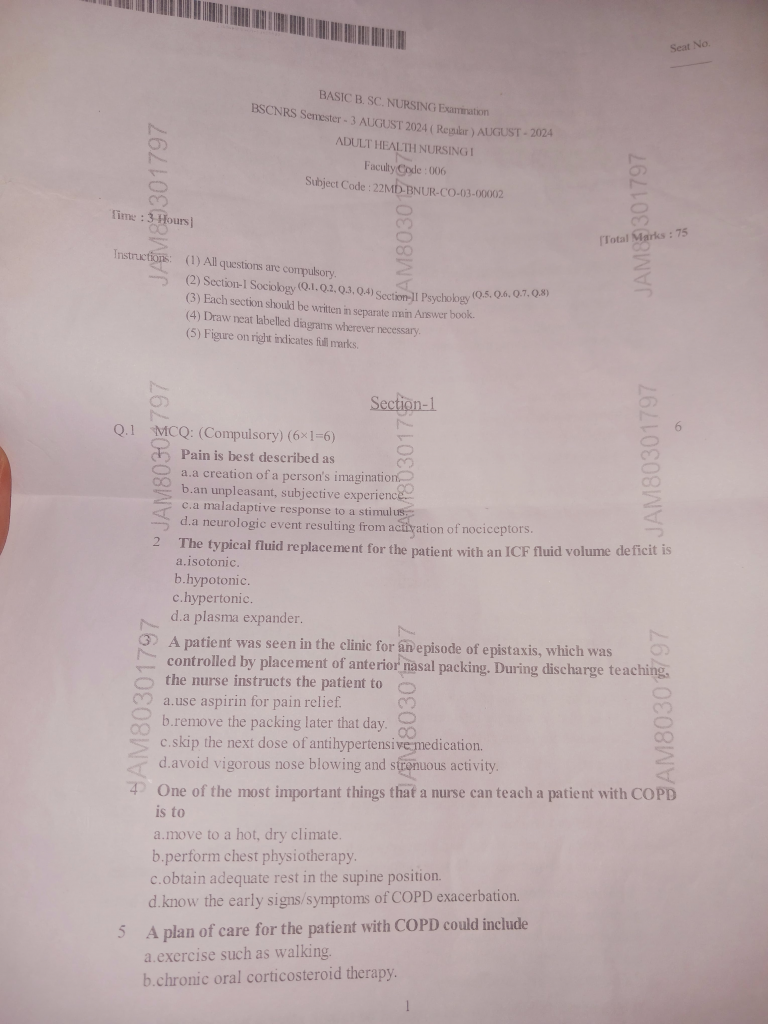
Section-1
Q.1 MCQ: (Compulsory) (6×1=6)
1. Pain is best described as
a. a creation of a person’s imagination
b.an unpleasant, subjective experience
c.a maladaptive response to a stimulu
d.a neurologic event resulting from achiyation of nociceptors.
2.The typical fluid replacement for the patient with an ICF fluid volume deficit is
a.Isotonic
b.Hypotonic
c.Hypertonic
d.A plasma expander
3.A patient was seen in the clinic for anvepisode of epistaxis, which was controlled by placement of anterior nasal packing. During discharge teaching the nurse instructs the patient to
a.Use aspirin for pain relief
b.Remove the packing later that day
c.Skip the next dose of antihypertensive medication.
d.Avoid vigorous nose blowing and strenuous activity
4.One of the most important things that a nurse can teach a patient with COPD is to
a.Move to a hot, dry climate.
b.Perform chest physiotherapy.
c. Obtain adequate rest in the supine position.
d Know the early signs/symptoms of COPD exacerbation.
5 A plan of care for the patient with COPD could include
a Exercise such as walking
b.chronic oral corticosteroid therapy.
c.bigh flow rate of 02 administration.
d breathing exercises that involve inhaling longer than exhaling
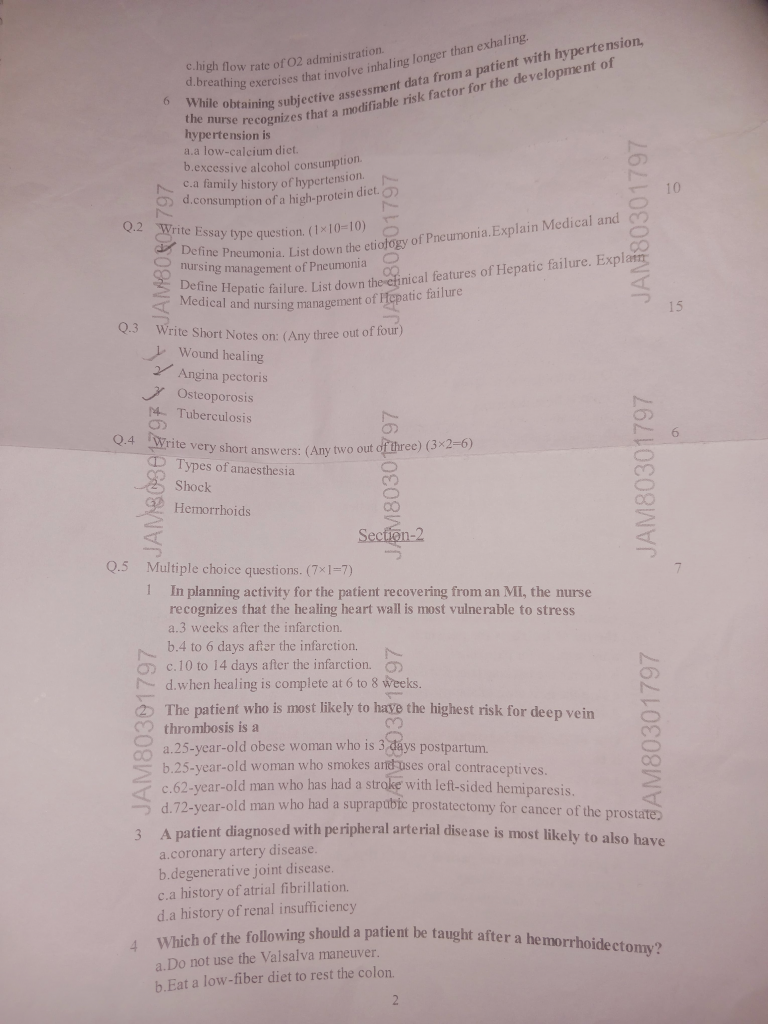
6 While obtaining subjective assessment data from a patient with hypertension, the nurse recognizes that a modifiable risk factor for the development of hypertension is
a. A low-calcium diet
b Excessive alcohol consumption
c Family history of hypertension
d. Consumption of a high-protein diet
Q.2 Write Essay type question (1X10=10)
Q-1. Define Pneumonia. List down the etiology of Pneumonia. Explain Medical and nursing management of Pneumonia
ANSWER:-
📘 Definition of Pneumonia
Pneumonia is an inflammatory condition of the lung parenchyma, primarily affecting the alveoli (air sacs), caused by infection with microorganisms such as bacteria, viruses, fungi, or parasites. It results in consolidation and impaired gas exchange, leading to respiratory symptoms such as cough, fever, chest pain, and dyspnea.
🦠 Etiology of Pneumonia (Causes)
Pneumonia can be classified based on causative agents and site of acquisition. Below is a breakdown:
✅ 1. Based on Causative Organism
🔹 Bacterial Pneumonia
- Streptococcus pneumoniae (most common)
- Haemophilus influenzae
- Staphylococcus aureus
- Klebsiella pneumoniae
- Pseudomonas aeruginosa
- Mycoplasma pneumoniae (atypical)
- Chlamydia pneumoniae
- Legionella pneumophila
🔹 Viral Pneumonia
- Influenza virus
- Respiratory Syncytial Virus (RSV)
- Adenovirus
- Coronavirus (e.g., SARS-CoV-2)
- Parainfluenza virus
- Herpes Simplex Virus (HSV) in immunocompromised patients
🔹 Fungal Pneumonia (often in immunocompromised patients)
- Aspergillus spp.
- Candida albicans
- Histoplasma capsulatum
- Pneumocystis jirovecii (formerly Pneumocystis carinii) – common in HIV/AIDS
🔹 Parasitic Pneumonia (rare)
- Toxoplasma gondii
- Strongyloides stercoralis
- Echinococcus granulosus
✅ 2. Based on Mode of Acquisition
🔸 Community-Acquired Pneumonia (CAP)
- Occurs outside hospital
- Caused mainly by Streptococcus pneumoniae, Mycoplasma, Influenza
🔸 Hospital-Acquired Pneumonia (HAP)
- Occurs 48+ hours after hospitalization
- Commonly caused by Pseudomonas, MRSA, Klebsiella
🔸 Ventilator-Associated Pneumonia (VAP)
- Occurs in patients on mechanical ventilation
- Common organisms: Acinetobacter, Pseudomonas
🔸 Aspiration Pneumonia
- Caused by inhalation of gastric contents, saliva, or food
- Organisms include anaerobes like Bacteroides, Fusobacterium
🔸 Immunocompromised Host Pneumonia
- Seen in HIV/AIDS, cancer, transplant patients
- Opportunistic infections like Pneumocystis, Aspergillus, CMV
🩺 I. Medical Management of Pneumonia
🎯 Goals:
- Eradicate infection
- Relieve symptoms
- Maintain oxygenation
- Prevent complications
🔹 1. Pharmacological Management
💊 A. Antibiotics (For bacterial pneumonia)
- Start empirical antibiotics immediately; modify after culture sensitivity reports
- Community-Acquired Pneumonia (CAP):
- Mild (Oral): Amoxicillin, Doxycycline, Azithromycin
- Moderate-Severe (IV): Ceftriaxone + Azithromycin or Levofloxacin
- Hospital-Acquired Pneumonia (HAP):
- Piperacillin-Tazobactam, Meropenem, Vancomycin, Linezolid (if MRSA suspected)
💊 B. Antivirals
- Oseltamivir (Tamiflu) – for influenza
- Remdesivir – for COVID-related pneumonia
- Acyclovir – if Herpes viruses are involved
💊 C. Antifungals
- Amphotericin B, Voriconazole, Fluconazole – for fungal pneumonia (esp. in immunocompromised)
💊 D. Supportive Medications
- Antipyretics: Paracetamol, Ibuprofen
- Expectorants: Ambroxol, Guaifenesin
- Bronchodilators: Salbutamol, Ipratropium – if wheezing present
- Corticosteroids: Methylprednisolone, Dexamethasone – in severe or inflammatory cases
- Mucolytics: N-acetylcysteine (NAC) – helps liquify sputum
🔹 2. Respiratory Support
💨 Oxygen Therapy
- Maintain SpO₂ ≥ 92% (unless COPD – target 88–92%)
- Nasal cannula → Face mask → Non-rebreather → NIV → Mechanical ventilation
🧴 Nebulization
- Nebulize with Bronchodilators (e.g., Salbutamol + Ipratropium) every 4–6 hours
🩻 Mechanical Ventilation
- Indicated if respiratory failure, ARDS, or altered mental status
🔹 3. Hydration & Electrolyte Balance
- IV fluids for dehydration or shock
- Monitor for electrolyte imbalance (esp. sodium, potassium) due to fever and vomiting
🔹 4. Investigations & Monitoring
- 🔬 CBC – look for leukocytosis
- 💉 CRP, ESR, Procalcitonin – inflammatory markers
- 🧪 Blood/sputum cultures – before starting antibiotics
- 🩻 Chest X-ray – consolidation or infiltrates
- 🩸 Arterial Blood Gas (ABG) – if oxygen saturation is low
- 🔍 Pulse oximetry and temperature charting
🧑⚕️ II. Nursing Management of Pneumonia
🎯 Nursing Objectives:
- Promote airway clearance
- Maintain oxygenation
- Relieve symptoms
- Educate and support patient
- Prevent complications
👩⚕️ 1. Comprehensive Nursing Assessment
- Airway: Look for sputum color, consistency, hemoptysis
- Breathing: Observe RR, chest expansion, wheezes, crackles
- Circulation: Check BP, HR, perfusion
- Temperature: Fever profile – record every 4 hours
- Mental Status: Confusion in elderly = red flag
- Intake-Output Monitoring: Detect dehydration or renal compromise
👩⚕️ 2. Airway Clearance
- Encourage:
- 💨 Deep breathing & coughing exercises
- 💨 Incentive spirometry
- 💨 Chest physiotherapy (percussion and postural drainage)
- Suctioning – if patient is unable to expectorate
- Provide humidified air to prevent mucosal dryness
👩⚕️ 3. Oxygen Therapy & Respiratory Support
- Administer oxygen per prescription
- Monitor SpO₂ continuously
- Watch for signs of hypoxia: restlessness, cyanosis, confusion
- Position in semi-Fowler’s or high-Fowler’s for easy breathing
👩⚕️ 4. Nutrition & Hydration
- High-protein, high-calorie diet to support immune function
- Encourage fluids: 2000–3000 mL/day (unless contraindicated – e.g., CHF, renal failure)
- Oral hygiene after meals and coughing
👩⚕️ 5. Medication Administration & Monitoring
- Strict timing of antibiotics
- Observe for drug allergies, side effects
- Evaluate response to bronchodilators or nebulization
- Document pain, fever relief, and respiratory status post-medication
👩⚕️ 6. Infection Control
- Practice strict hand hygiene
- Isolate patient if infection is contagious (e.g., Influenza, COVID)
- Use PPE – gloves, masks, gowns as needed
- Educate family on hygiene precautions
👩⚕️ 7. Patient & Family Education
- Complete full antibiotic course
- Importance of cough etiquette, handwashing
- Encourage vaccinations:
- Pneumococcal vaccine (once every 5 years for high-risk groups)
- Annual influenza vaccine
- Avoid smoking, pollutants, and allergens
👩⚕️ 8. Prevention of Complications
- Monitor for:
- 🩸 Sepsis (↓BP, ↑HR, altered LOC)
- 🫁 Pleural effusion (decreased breath sounds, dull percussion)
- 😷 Respiratory failure
- 🦠 Multiorgan involvement
Q.3 Write Short Notes on: (Any three out of four)
1.Wound healing
2.Angina pectoris
3.Osteoporosis
4.Tuberculosis
Q.4 Write very short answers: (Any two out of three) (3X2=6)
1.Types of ataesthesia
2.Shock
3.Hemorrhoids
Section-2
Q.5 Multiple choice questions. (7X1=7)
1 In planning activity for the patient recovering from an MI. the nurse recognizes that the healing heart wall is most vulnerable to stress
a.3 weeks after the infarction.
b.4 to 6 days after the infarction.
c.10 to 14 days after the infarction.
d. when healing is complete at 6 to 8 weeks. 1
2.The patient who is most likely to have the highest risk for deep vein thrombosis is a
a.25-year-old obese woman who is 3 days postpartum.
h.25-year-old woman who smokes antipses oral contraceptives.
c.62-year-old man who has had a stroke with left-sided hemiparesis.
d.72-year-old man who had a suprapubic prostatectomy for cancer of the prostate
3 A patient diagnosed with peripheral arterial disease is most likely to also have
a.coronary artery disease.
b. degenerative joint disease.
ca history of atrial fibrillation.
d.a history of renal insufficiency
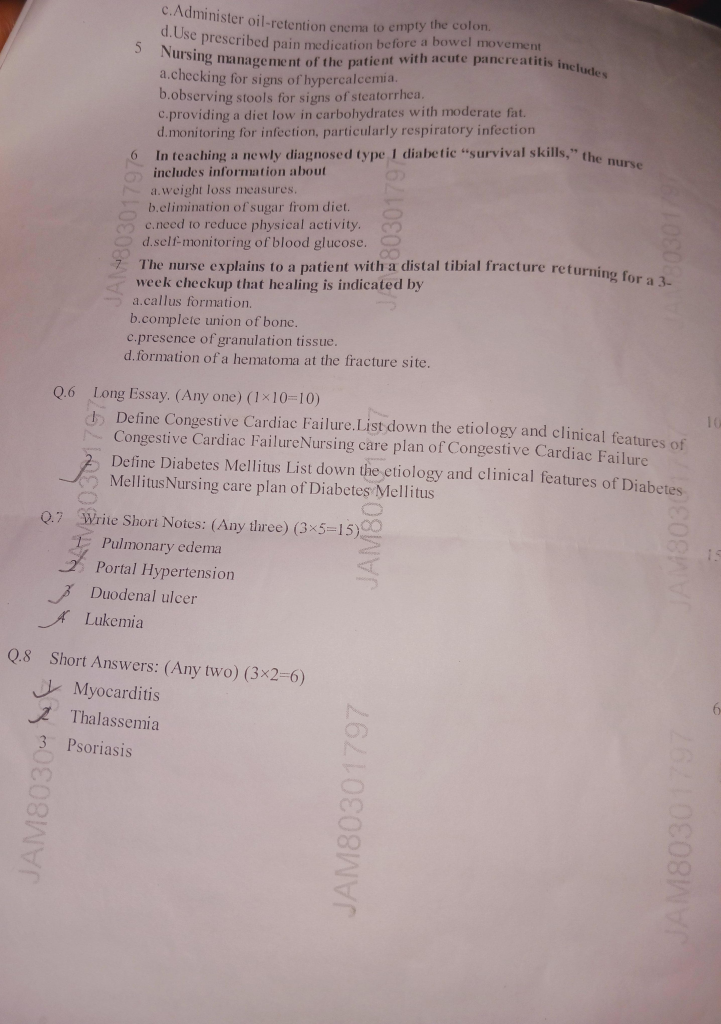
4 Which of the following should a patient be taught after a hemorrhoidectomy?
a.Do not use the Valsalva maneuver.
b. Eat a low-fiber diet to rest the colon
c. Administer oil-retention enema to empty the colon
d. Use prescribed pain medication before a bowel movement
5 Nursing management of the patient with acute pancreatitis includes
a.checking for signs of hypercalcema.
b.observing stools for signs of steatorrhea.
c.providing a diet low in carbohydrates with moderate fat.
d.monitoring for infection, particularly respiratory infection
6.In teaching a newly diagnosed type. I diabetic “survival skills,” the nurse includes information about
a. Weight loss measures.
b.Elimination of sugar from diet.
c.Need to reduce physical activity.
d.Self-monitoring of blood glucose.
7.The nurse explains to a patient with a distal tibial fracture returning for a 3-week checkup that healing is indicated by
a.callus formation.
b.complete union of bone.
c.presence of granulation tissue.
d. formation of a hematoma at the fracture site.
Q.6 Long Essay. (Any one) (1×10=10)
1.Define Congestive Cardiac Failure List down the etiology and clinical features of Congestive Cardiac FailureNursing care plan of Congestive Cardiac Failure
2.Define Diabetes Mellitus List down the etiology and clinical features of Diabetes Mellitus Nursing care plan of Diabetes Mellitus
Q.7 Write Short Notes: (Any three) (3×5=15)
1.Pulmonary edema
2.Portal Hypertension
3.Duodenal ulcer
4.Lukemia
Q.8 Short Answers: (Any two) (3×2=6)
1.Myocarditis
2.Thalassemia
3.Psoriasis