30/07/2016-B.SC-MEDICAL SURGICAL-2-UPLOAD PAPER NO.4
PAPER SOLUTION NO.4
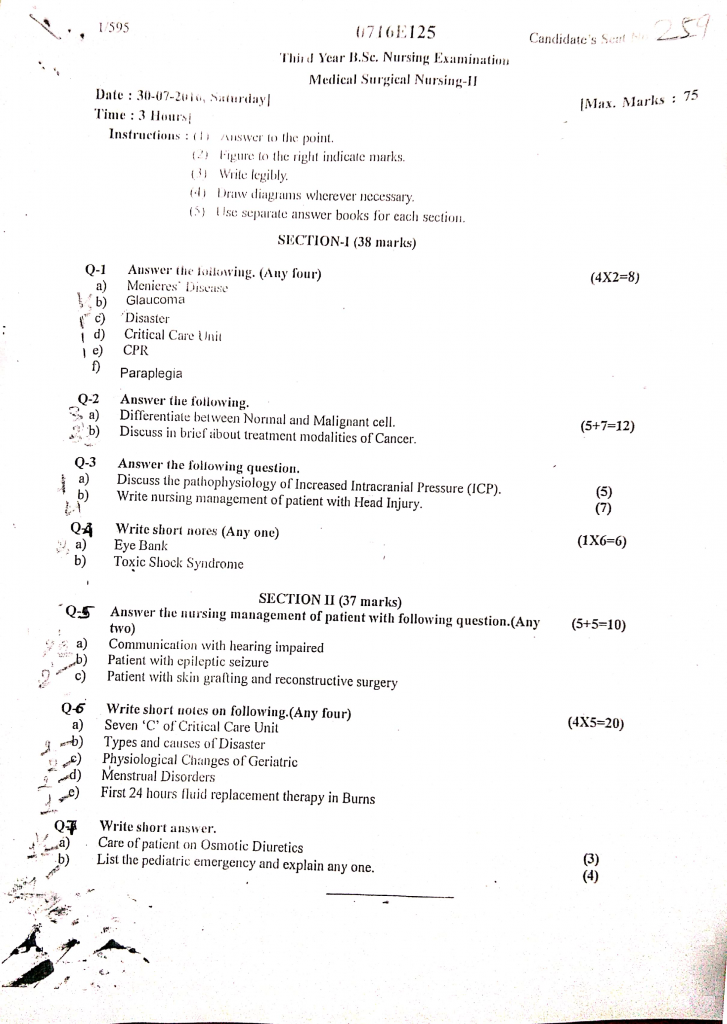
Section 1 (38 mark)
Q.1 Answer the following (any four) (8 mark)
1. Menieres disease
- It is a chronic disorder of the inner ear that affects balance and hearing, usually presenting with episodes of vertigo, tinnitus, hearing loss, and a feeling of fullness in the ear.
- Meniere’s disease is a progressive inner ear disorder that results in repeated episodes of dizziness and hearing problems, commonly affecting only one ear.
- It is believed to be caused by an abnormal accumulation of endolymphatic fluid in the inner ear (labyrinth), leading to sensory disturbances.
2. Glaucoma
- Glaucoma is a group of chronic eye conditions in which there is increased intraocular pressure (IOP) that causes damage to the optic nerve.
- This damage to the optic nerve can gradually lead to visual field defects and may result in permanent blindness if not treated on time.
- It is one of the leading causes of preventable blindness worldwide, especially among the elderly.
3. Disaster
- A disaster is a sudden, catastrophic event that causes significant disruption to life, property, environment, and normal functioning of a community or society.
- A disaster is an unexpected event causing widespread damage, loss of life, and disruption, which exceeds the ability of the affected community to cope using its own resources
- It may be caused by natural forces (such as earthquakes, floods, cyclones) or human activities (such as industrial accidents, war, or terrorism).
- Disasters usually overwhelm local resources and require immediate emergency response and aid.
4. Critical care unit
- A Critical Care Unit (CCU), also known as an Intensive Care Unit (ICU), is a specially equipped and staffed hospital unit designed to provide comprehensive and continuous care to patients with life-threatening conditions.
- It is used for patients who require intensive monitoring, advanced medical interventions, and life-support systems due to serious illness, trauma, or post-surgical complications.
- The unit is staffed by trained critical care nurses, intensivists, and other healthcare professionals skilled in managing critical and unstable patients.
5. CPR
- CPR (Cardiopulmonary Resuscitation) is a life-saving emergency procedure that combines chest compressions and rescue breaths to maintain circulation of oxygenated blood to the brain and vital organs when a person’s heart has stopped beating (cardiac arrest) or they have stopped breathing.
- It is intended to temporarily support circulation and breathing until advanced medical help becomes available.
- CPR helps in preserving brain function, preventing tissue death, and increasing survival chances in sudden cardiac arrest.
6. Paraplegia
- Paraplegia is defined as a type of paralysis that affects the lower half of the body, typically involving both legs and sometimes part of the lower abdomen, due to injury or disease of the spinal cord, especially in the thoracic or lumbar region.
- It results in loss of motor and/or sensory function below the level of injury and may be caused by spinal cord trauma, tumors, infections, or neurological disorders such as multiple sclerosis.
Q.2 Answer the following (5+7=12)
1. Difference between normal and malignant cell
| 🔸 Feature | 🔬 Normal Cell | 🧫 Malignant (Cancerous) Cell |
|---|---|---|
| 1. Growth Regulation | It is strictly controlled by internal and external signals. The cell divides only when necessary, and stops growing when neighboring cells are contacted (contact inhibition). | It shows uncontrolled and continuous division, disregarding regulatory mechanisms. It does not stop dividing even when overcrowded (loss of contact inhibition). |
| 2. Cell Shape and Size | It has uniform shape and size, specific to its tissue type, and maintains normal cell architecture. | It exhibits variation in shape and size (pleomorphism), irregular contours, and appears disorganized in tissue. |
| 3. Nucleus Characteristics | It has a small, round, and uniform nucleus with fine, evenly distributed chromatin and small nucleoli. | It often has a large, irregular, and hyperchromatic nucleus with coarse chromatin and prominent, multiple nucleoli. |
| 4. Function and Differentiation | It is highly differentiated, performing specialized functions specific to its location and tissue type (e.g., secretion, contraction). | It is poorly differentiated or undifferentiated (anaplasia), often losing the ability to perform normal tissue functions. |
| 5. Cell Division & Life Span | It has a limited number of divisions and undergoes apoptosis (programmed cell death) when damaged or aged. | It divides indefinitely, escapes apoptosis, and becomes immortal, continuing to proliferate even when abnormal. |
| 6. DNA Stability | It contains stable, unmutated DNA with correct chromosome number and structure. | It often contains mutated DNA, abnormal chromosomes (aneuploidy), and may have multiple gene alterations or translocations. |
| 7. Contact Inhibition | It respects cell boundaries and stops growing when touching adjacent cells. | It does not recognize boundaries and continues to grow, piling up and invading nearby cells and tissues. |
| 8. Invasion Ability | It remains confined within its tissue or organ and does not invade surrounding structures. | It has the ability to invade neighboring tissues, destroy basement membranes, and spread beyond its origin. |
| 9. Metastasis (Spread) | It does not metastasize, i.e., it stays localized where it developed. | It is capable of spreading through blood or lymphatics to distant organs like liver, lungs, or brain (metastasis). |
| 10. Blood Supply and Angiogenesis | It uses normal blood vessels of surrounding tissues and does not stimulate new vessel growth. | It stimulates angiogenesis, i.e., formation of new blood vessels to feed its high metabolic needs and growth. |
| 11. Immune Recognition | It is recognized as self by the immune system and usually does not trigger immune attack. | It may evade immune surveillance, alter surface proteins, and create an environment that suppresses immune response. |
| 12. Response to Signals | It responds normally to growth-inhibiting and death signals, such as contact with other cells or cytokines. | It ignores signals for growth inhibition, death, or repair, leading to uncontrolled proliferation. |
2. Discuss in brief about treatment modalities of cancer
1️⃣ Surgical Treatment
- It is used to physically remove cancerous tissues, either partially or completely, depending on the stage and type of tumor.
- It is most effective in early-stage, localized cancers such as breast, thyroid, colorectal, or skin cancers.
- It is categorized into curative surgery, diagnostic (biopsy), palliative surgery for symptom relief, preventive surgery, and reconstructive surgery.
- It helps in removal of tumor bulk, reducing symptoms like obstruction or bleeding in certain cancers.
- It may include lymph node dissection to prevent spread and for staging purposes.
- It is often combined with radiotherapy or chemotherapy to enhance cure rates (multimodal therapy).
- Postoperative care includes wound management, pain control, and early ambulation.
- Surgical risks include bleeding, infections, poor wound healing, and anesthesia-related complications.
2️⃣ Radiation Therapy (Radiotherapy)
- It involves the use of ionizing radiation to kill or control the growth of cancer cells by damaging their DNA.
- It is delivered through External Beam Radiation Therapy (EBRT), Brachytherapy (internal radiation), or Systemic radiotherapy using radioisotopes.
- It can be used for curative, adjuvant, neoadjuvant, or palliative purposes.
- It is highly effective in treating cancers such as brain tumors, cervical cancer, head and neck cancers, and prostate cancer.
- It is precisely targeted, but normal cells nearby may also be affected, leading to side effects.
- Common side effects include fatigue, localized skin burns, mucositis, nausea, or organ-specific toxicities.
- Patients may require multiple sessions over days or weeks, depending on tumor type and stage.
- Nurses must provide skin care, oral care, and educate patients to avoid sun exposure or harsh soaps on irradiated areas.
3️⃣ Chemotherapy
- It uses anti-cancer drugs that destroy or stop the growth of cancer cells, especially those rapidly dividing.
- It is used for curative, adjuvant (after surgery), neoadjuvant (before surgery), and palliative purposes.
- Drugs can be given via oral, intravenous, intramuscular, subcutaneous, or intrathecal routes depending on the type.
- Chemotherapy is administered in cycles (usually every 1–4 weeks) to allow the body to recover between doses.
- It is commonly used in leukemia, lymphoma, breast cancer, lung cancer, and ovarian cancer.
- Side effects include nausea, vomiting, alopecia, mucositis, neutropenia, anemia, thrombocytopenia, and fatigue.
- It may lead to immunosuppression, so patients are at higher risk of infections.
- Nurses must monitor blood counts, manage side effects, and provide emotional support during hair loss and body image changes.
4️⃣ Hormonal Therapy
- It is used in cancers that are hormone-dependent, such as breast, prostate, ovarian, and endometrial cancers.
- It works by blocking hormone receptors or reducing hormone production, thus slowing or stopping cancer growth.
- Drugs include tamoxifen, aromatase inhibitors, GnRH analogs, and anti-androgens.
- Hormonal therapy may be used alone or in combination with other treatments like surgery or radiotherapy.
- It is often a long-term therapy—sometimes continued for 5–10 years.
- Side effects include hot flashes, mood swings, weight gain, decreased libido, bone thinning, and fatigue.
- It may reduce recurrence risk in hormone receptor-positive cancers.
- Nurses should provide counseling about medication adherence, managing side effects, and performing DEXA scans for bone health.
5️⃣ Immunotherapy (Biological Therapy)
- It helps to stimulate the body’s own immune system to fight against cancer cells.
- It includes checkpoint inhibitors (e.g., nivolumab), monoclonal antibodies (e.g., rituximab), cytokines, vaccines, and CAR T-cell therapy.
- It is useful in cancers like melanoma, lung cancer, renal cell carcinoma, bladder cancer, and some blood cancers.
- It works by blocking immune evasion mechanisms used by tumor cells.
- Immunotherapy is usually well-tolerated, but can cause autoimmune reactions like colitis, hepatitis, dermatitis, or thyroid dysfunction.
- Nurses should monitor for fever, rash, diarrhea, and breathing difficulties, indicating immune-related adverse events.
- It is usually given intravenously in specialized centers due to potential side effects.
- Immunotherapy is often given in combination with chemotherapy or radiation for better outcomes.
6️⃣ Targeted Therapy
- It uses agents that specifically target cancer-related proteins, genes, or pathways, sparing most healthy cells.
- Common drugs include imatinib (for CML), trastuzumab (for HER2+ breast cancer), and erlotinib (for EGFR+ lung cancer).
- It is effective in tumors with specific genetic mutations and requires molecular profiling of the tumor.
- It is associated with fewer side effects compared to chemotherapy but may still cause rashes, diarrhea, hypertension, or liver toxicity.
- Resistance can develop over time; thus, therapy adjustments may be necessary.
- It is taken orally or intravenously, depending on the drug.
- Nurses must monitor for adverse reactions, teach compliance, and support regular follow-up testing.
- It offers personalized and precision-based cancer care for advanced or resistant tumors.
7️⃣ Stem Cell / Bone Marrow Transplantation
- It is used to replace damaged bone marrow after high-dose chemotherapy or radiotherapy.
- It is vital in treating leukemia, lymphoma, multiple myeloma, and some aplastic anemias.
- Types include autologous (own cells) and allogeneic (donor cells).
- The procedure involves harvesting stem cells, followed by conditioning therapy and then infusion of stem cells.
- It requires high-level isolation, strict asepsis, and immunosuppressive therapy post-transplant.
- Complications include graft-versus-host disease (GVHD), infections, mucositis, and organ damage.
- Recovery is slow, often requiring weeks of hospitalization and months of immune suppression.
- Nurses must provide supportive care, emotional support, and teach infection prevention practices.
8️⃣ Palliative Care
- It focuses on symptom management, pain relief, and improving quality of life, especially in advanced or terminal cancers.
- It is applicable at any stage of cancer but is essential when curative treatment is not possible.
- It includes pain management using opioids (e.g., morphine), antiemetics, appetite stimulants, and oxygen therapy.
- It also addresses psychological, social, and spiritual needs of both patient and family.
- It supports family involvement, advanced directives, and end-of-life planning.
- Palliative care may be provided in hospice settings, home care, or hospitals.
- Nurses must practice active listening, emotional reassurance, and respect for patient dignity and comfort.
- Holistic care is the goal — physical, emotional, and spiritual support go hand-in-hand.
Q.3 Answer the following
1. Discuss the pathophysiology of increased intra cranial pressure (5)
Increased intracranial pressure refers to a rise in pressure inside the skull that may result from swelling, bleeding, tumor, infection, or excess cerebrospinal fluid (CSF). The normal ICP is 5–15 mmHg, and values exceeding 20 mmHg require urgent intervention.
Pathophysiology of Increased Intracranial Pressure (ICP)
The pathophysiology of raised ICP follows a progressive sequence of events involving structural and vascular changes inside the cranial vault. Below is the step-wise detailed explanation:
1️⃣ Primary Cause or Triggering Event
- The process begins with trauma, tumor, hemorrhage, infection, or hydrocephalus, which leads to an increase in the volume of one or more intracranial components.
- Additional triggers may include status epilepticus, hepatic encephalopathy, or hypoxic injury causing cerebral edema.
2️⃣ Initial Compensation by the Body
- The body tries to maintain normal ICP by displacing CSF into the spinal canal and reducing venous blood volume.
- Cerebrovascular autoregulation adjusts vessel tone to maintain cerebral blood flow.
- CSF production slows down while absorption increases as an adaptive response.
3️⃣ Exhaustion of Compensatory Mechanisms
- Once the compensatory limits are exceeded, even minor increases in intracranial volume result in steep rises in ICP.
- Brain compliance is lost, and intracranial dynamics become unstable.
4️⃣ Reduction in Cerebral Perfusion Pressure (CPP)
- As ICP continues to rise, CPP (CPP = MAP – ICP) declines progressively, leading to cerebral ischemia.
- Brain tissues begin to suffer from oxygen and glucose deprivation, impairing neuronal function.
5️⃣ Cellular Hypoxia and Lactic Acidosis
- Hypoxia forces the cells to switch to anaerobic metabolism, producing lactic acid and free radicals.
- The acidic environment damages neurons, astrocytes, and endothelial cells, further compromising cerebral homeostasis.
6️⃣ Disruption of the Blood-Brain Barrier (BBB)
- The BBB becomes more permeable, allowing plasma proteins and water to leak into interstitial spaces, worsening vasogenic cerebral edema.
- Additional cytotoxic edema may result from cell swelling due to sodium and water retention inside neurons.
7️⃣ Compression of Brain Structures and Ventricles
- As swelling increases, brain tissue compresses ventricles, sulci, and gyri, distorting normal brain anatomy.
- Midline shift may occur, where the brain shifts to one side, visible on CT scan.
8️⃣ Obstruction of CSF Circulation and Absorption
- Enlarged brain structures impair CSF flow through the ventricles and subarachnoid space.
- This causes hydrocephalus, increasing pressure further.
9️⃣ Brain Herniation Syndromes
- Excessive ICP eventually causes herniation of brain tissue from high-pressure compartments to low-pressure areas.
- Herniation compresses the brainstem, affecting the respiratory and cardiovascular centers, and may lead to irreversible coma and death.
2. Write nursing management of patient with head injury (7)
Head injury refers to trauma to the scalp, skull, or brain that may be open (penetrating) or closed (non-penetrating), and can lead to serious complications including increased intracranial pressure (ICP), brain herniation, or death. It is classified as mild, moderate, or severe based on Glasgow Coma Scale (GCS) score.
✅ 1. Emergency Nursing Management (Pre-hospital or ER phase)
- The nurse must first ensure a clear and patent airway by using a head tilt-chin lift or jaw thrust maneuver (if no spinal injury is suspected).
- If spinal cord injury is suspected, the cervical spine must be stabilized using a rigid cervical collar or manual immobilization.
- The nurse should administer supplemental oxygen to maintain oxygen saturation above 95% and prevent hypoxia to brain tissue.
- It is critical to initiate cardiopulmonary resuscitation (CPR) if the patient is unresponsive with no pulse or respiration.
- Two large-bore IV lines should be secured, and isotonic fluids (like normal saline) started to manage shock.
- The nurse should assess and document Glasgow Coma Scale (GCS), pupil reaction, limb movement, bleeding, and any open wounds.
- A quick neurological assessment including verbal response, motor response, and eye-opening response is done to establish baseline.
✅ 2. Acute Phase Nursing Management (In ICU or Neuro Ward)
A. Neurological Monitoring and Assessment
- The nurse must assess level of consciousness hourly using the GCS, noting any decline which could indicate brain swelling or hemorrhage.
- Regularly check pupil size, symmetry, and reaction to light to detect early signs of increased intracranial pressure (ICP) or brain herniation.
- Monitor for abnormal posturing such as decorticate or decerebrate postures which indicate severe brain injury.
- The nurse should watch for seizure activity and have emergency anticonvulsants like lorazepam or phenytoin readily available.
B. Respiratory Support and Airway Management
- The airway must be kept clear with suctioning and humidified oxygen administration as needed.
- If the patient has GCS ≤ 8, endotracheal intubation or mechanical ventilation may be required to prevent respiratory failure.
- Maintain the head of the bed elevated at 30 degrees unless contraindicated to facilitate venous drainage from the brain.
- Avoid neck flexion, tight tracheostomy ties, or anything that could increase ICP.
C. Hemodynamic and Fluid Balance Management
- Regularly monitor blood pressure, heart rate, central venous pressure (CVP), and urine output to detect hypovolemia or shock.
- Avoid hypotension, which can worsen cerebral perfusion, by administering IV fluids and vasopressors as prescribed.
- Monitor for diabetes insipidus (excessive urine output) or SIADH (low urine output), which are endocrine complications of head trauma.
- Administer osmotic diuretics (e.g., Mannitol) or hypertonic saline as ordered to reduce cerebral edema.
D. Nutritional Support and GI Care
- Initiate enteral nutrition via nasogastric tube within 48–72 hours to maintain nutritional status.
- Monitor for abdominal distension, bowel sounds, and constipation due to immobility or medications.
- Provide proton pump inhibitors (PPIs) or H2 blockers to prevent stress ulcers or gastric bleeding.
E. Pain and Sedation Management
- Pain must be assessed and managed with analgesics like paracetamol or opioids, being cautious not to mask neurological signs.
- Use sedatives cautiously (e.g., midazolam) to calm agitated patients but avoid over-sedation.
- Apply cold compresses or dark room conditions to relieve photophobia and headaches.
F. Skin Integrity and Pressure Ulcer Prevention
- Turn and reposition the patient every 2 hours using log-roll technique to prevent spinal misalignment.
- Use pressure-relieving mattresses, heel protectors, and clean, dry linens.
- Monitor skin for redness, blisters, or pressure injuries, especially on sacrum, elbows, and heels.
G. Bowel and Bladder Care
- Monitor for urinary retention or incontinence, and maintain a sterile technique during catheter care.
- Initiate bladder training or intermittent catheterization once the patient regains consciousness.
- Provide stool softeners to prevent straining, which increases ICP.
✅ 3. Psychological and Emotional Nursing Support
- Offer empathy, reassurance, and psychological comfort to the patient and family.
- Maintain effective communication with the family, updating them on the patient’s condition and prognosis.
- Provide referral to counseling services, especially if the patient develops depression, personality changes, or PTSD.
- Encourage family involvement in care, and provide education on behavior changes that may occur post-head injury.
✅ 4. Rehabilitation Phase Nursing Care
- Collaborate with physiotherapists for early mobilization, passive and active range-of-motion exercises.
- Support speech therapy, especially in patients with aphasia, dysarthria, or dysphagia.
- Help the patient with cognitive retraining including memory exercises, reality orientation, and attention tasks.
- Educate the family on home safety modifications, such as installing handrails, removing trip hazards, and using helmets.
- Assess for community resources like home nursing, occupational therapy, and vocational rehabilitation.
✅ 5. Discharge Planning and Education
- Educate the patient and family about medication adherence, warning signs of complications (e.g., vomiting, drowsiness, seizure).
- Encourage regular follow-up with neurology, psychiatry, and rehabilitation services.
- Counsel regarding avoidance of alcohol, driving, or strenuous activities until medically cleared.
- Provide written instructions on nutrition, hygiene, and wound care if surgery was performed.
✅ 6. Documentation and Legal Aspects
- Accurately document neurological assessments, nursing interventions, and patient’s response to treatment.
- Maintain chain of evidence if head injury is due to assault or accident (medico-legal case).
- Ensure all informed consent procedures are appropriately signed and witnessed, especially before surgery or CT scans.
Q.4 Write short notes (any one) (6 mark)
1. Eye bank
Definition of Eye Bank
- Eye banking is a systematic and regulated medical service that involves the collection, preservation, evaluation, and distribution of human eyes or corneal tissue donated after death for the purpose of restoring vision through corneal transplantation, and for research and education.
- Eye banks work under strict legal, medical, and ethical guidelines, and play a vital role in the treatment of corneal blindness, which is the second most common cause of blindness in India after cataract.
Objectives of Eye Bank
- It is the primary objective of eye banks to collect and preserve donated human eyes in a safe and sterile manner.
- It is aimed at evaluating and screening the collected corneas to ensure suitability for transplantation.
- It is essential to distribute the healthy corneas to hospitals and surgeons for corneal graft surgeries.
- It is also the objective to create public awareness about eye donation, to reduce the gap between demand and supply of donor tissue.
- It serves as a training center for ophthalmic staff, and provides materials for corneal research and academic purposes.
Functions of Eye Bank
1️⃣ Collection of Donated Eyes
- It is the responsibility of the eye bank to collect eyes from registered and voluntary donors after death.
- The donation must occur within 6 hours of death, and proper informed consent must be obtained from the next of kin.
- Eye banks often operate through Hospital Cornea Retrieval Programs (HCRP) and home collection services.
2️⃣ Evaluation and Screening of Donor Eyes
- After collection, it is essential to perform a medical evaluation to rule out any infectious diseases such as HIV, Hepatitis B, C, sepsis, or rabies.
- Eye banks use specular microscopy, slit-lamp examination, and serology tests to assess the quality of corneal tissue.
- It is important to classify corneas as suitable for therapeutic use, research, or educational purposes.
3️⃣ Preservation and Storage
- It is essential to preserve donor corneas in sterile preservation media such as McCarey-Kaufman (MK) medium, Optisol-GS, or Cornisol.
- These media help to store corneas for 7–14 days depending on the solution used.
- Preservation must be done under controlled temperature (4°C) and sterile conditions.
4️⃣ Distribution and Transplantation
- It is the duty of the eye bank to allocate corneas to certified ophthalmic surgeons based on urgency and priority.
- Documentation must be maintained for traceability, utilization, and surgical outcomes.
- Emergency cases like corneal perforation or ulceration are given priority for transplantation.
5️⃣ Education and Public Awareness
- Eye banks conduct regular awareness programs, rallies, seminars, and health talks to promote eye donation.
- They collaborate with NGOs, schools, hospitals, and religious leaders to encourage voluntary pledging.
- Campaigns like Eye Donation Fortnight (August 25 – September 8) are observed to boost community participation.
Eligibility for Eye Donation
- Any person, regardless of age, gender, or religion, can donate eyes after death.
- People with cataracts, spectacle use, hypertension, or diabetes can still donate their corneas.
- Individuals with communicable diseases like HIV/AIDS, hepatitis, septicemia, and active cancers are not eligible for donation.
Legal and Ethical Guidelines
- Eye donation is regulated in India by the Transplantation of Human Organs and Tissues Act, 1994 (THOTA).
- Consent must be obtained ethically and in writing by trained personnel.
- No financial or commercial transactions are allowed in the donation or allocation of eye tissues.
- Eye banks must ensure confidentiality, respect, and dignity of the donor.
Role of Nurse in Eye Banking
- It is the duty of the nurse to motivate and counsel grieving families about the importance of eye donation.
- It is necessary for the nurse to identify potential donors in hospital ICUs, wards, or emergency departments, especially when brain death or death is declared.
- The nurse should immediately inform the eye bank team upon patient death to ensure timely retrieval.
- It is important to assist with documentation, consent process, and ensure privacy and comfort for the donor family.
- Nurses also play a major role in community health campaigns, school visits, and health melas to educate the public about myths and facts related to eye donation.
- During preservation, the nurse may help in eye enucleation, applying dressing, and maintaining sterile protocol.
2. Toxic shock syndrome
Definition of Toxic Shock Syndrome (TSS)
Toxic Shock Syndrome is a rare but life-threatening condition caused by toxins produced by certain strains of bacteria, most commonly Staphylococcus aureus and sometimes Streptococcus pyogenes. These toxins cause a systemic inflammatory response, leading to multi-organ failure.
Etiology (Causes)
- Staphylococcus aureus (main cause)
- Streptococcus pyogenes (less common)
- Use of high-absorbency tampons during menstruation
- Infected wounds, burns, or surgical incisions
- Use of nasal packing, contraceptive sponges, or diaphragms
- Postpartum infections or foreign body retention
Pathophysiology of Toxic Shock Syndrome
Bacterial Colonization and Toxin Release
- S. aureus or S. pyogenes colonizes mucosal surfaces or wounds and produces exotoxins such as TSST-1 (toxic shock syndrome toxin-1).
Toxin Absorption into Bloodstream
- The exotoxins enter the systemic circulation and spread throughout the body.
Superantigen Activity
- The toxins act as superantigens, triggering massive T-cell activation and excessive cytokine release.
Cytokine Storm and Inflammatory Response
- The large-scale release of interleukins and tumor necrosis factor (TNF) causes vasodilation, capillary leak, and hypotension.
Multisystem Involvement
- Inflammatory mediators lead to organ dysfunction, including renal failure, liver injury, and cardiac involvement.
Progression to Shock
- The rapid drop in blood pressure results in circulatory collapse and hypoperfusion of tissues, resembling septic shock.
Possible Disseminated Intravascular Coagulation (DIC)
- In severe cases, coagulation abnormalities may occur, leading to bleeding and clotting complications.
Clinical Manifestations
- Sudden high fever (>102°F or 39°C)
- Hypotension (low blood pressure)
- Sunburn-like rash (especially on palms and soles)
- Vomiting, diarrhea, and abdominal pain
- Confusion, dizziness, or altered mental state
- Muscle aches and chills
- Redness of eyes, mouth, and throat
- Desquamation (peeling of skin) after a few days
- Multiorgan dysfunction in severe cases
Diagnostic evaluation
- History and physical examination
- CBC: may show leukocytosis
- Liver and kidney function tests
- Blood culture: to identify causative organism
- Vaginal/cervical swab (if tampon-related)
- Coagulation profile for DIC evaluation
Medical Management
Hospitalization and Supportive Care
- Immediate admission to ICU for fluid resuscitation and organ support.
- Intravenous fluids are given to treat hypotension and prevent shock.
Antibiotic Therapy
- Clindamycin + Vancomycin or Linezolid are used to stop toxin production and cover resistant strains.
- Penicillin may be added for Group A Streptococcal infections.
Removal of Source
- Tampon, nasal packing, or any foreign body must be removed immediately.
- Surgical drainage of abscesses or debridement of infected tissue may be necessary.
Vasopressors
- Norepinephrine or dopamine is used to maintain blood pressure if fluids fail.
IV Immunoglobulin (IVIG)
- Used in severe streptococcal cases to neutralize circulating toxins.
Monitoring of Organs
- Continuous monitoring of renal, hepatic, respiratory, and cardiac functions is essential.
Nursing Management of Toxic Shock Syndrome
1️⃣ Assessment and Monitoring
- Monitor vital signs (temperature, BP, pulse, RR) frequently, especially for signs of shock.
- Check for rash, desquamation, and progression of infection.
- Assess for mental status changes, confusion, or drowsiness.
- Observe for urine output, noting signs of acute renal failure.
- Monitor for organ dysfunction by evaluating liver and kidney function tests.
2️⃣ Medication Administration
- Administer IV antibiotics as per prescription and observe for allergic reactions.
- Provide antipyretics (like paracetamol) for fever management.
- Ensure strict aseptic technique during all IV infusions.
- Administer vasopressors (like norepinephrine) if hypotension persists after fluids.
- Prepare and assist with IV immunoglobulin (IVIG) administration if ordered.
3️⃣ Fluid and Electrolyte Management
- Maintain accurate intake and output (I/O) charting to monitor fluid balance.
- Replace fluids as per physician’s orders to prevent hypovolemia and circulatory collapse.
- Monitor for electrolyte imbalances (Na+, K+, Ca++) and report abnormalities.
4️⃣ Infection Control
- Use personal protective equipment (PPE) while handling patient.
- Follow strict hand hygiene and isolation precautions if indicated.
- Assist in removal of tampon, contraceptive device, or other sources of infection.
- Educate patient/family about infection prevention practices.
5️⃣ Wound and Skin Care
- Inspect and clean wounds or surgical sites regularly using sterile technique.
- Apply prescribed topical antiseptics to affected areas if needed.
- Monitor for signs of wound infection or abscess formation.
6️⃣ Supportive and Comfort Measures
- Provide tepid sponging or cold compress for high-grade fever.
- Maintain adequate oxygenation using nasal cannula or face mask if needed.
- Encourage bed rest in early stages to reduce metabolic demand.
- Provide psychological support to patient and family during ICU stay.
7️⃣ Health Education and Counseling
- Instruct females on safe tampon usage: frequent changing, avoid overnight use.
- Educate about early warning signs: high fever, rash, dizziness, hypotension.
- Promote awareness about the importance of hygiene during menstruation and post-surgery.
- Explain the need for follow-up appointments to monitor organ recovery and recurrence prevention.
Section 2 (37 marks)
Q.5 Answer the nursing management of patient with following question (any two) (10 mark)
1. Communication with hearing impaired
1️⃣ Assessment of Hearing Ability
- The nurse should begin by assessing the degree and type of hearing loss, such as conductive, sensorineural, or mixed.
- Observation should include whether the hearing loss affects one or both ears, and whether the patient uses lip reading, sign language, or hearing devices.
- The nurse should review the medical and audiological history to determine the onset, cause, and progression of the hearing loss.
- It is also necessary to assess the patient’s comfort level and emotional response regarding their communication barriers.
2️⃣ Creating a Conducive Environment
- The communication environment should be quiet, well-ventilated, and well-lit, as good lighting enhances lip reading and visibility of facial expressions.
- Background noise should be minimized by closing doors, silencing mobile phones, and avoiding noisy machines.
- The nurse must position themselves in front of the patient, maintain eye-level contact, and avoid speaking while turning away or walking.
- A private, interruption-free setting can reduce anxiety and encourage open communication, especially during teaching or consent discussions.
3️⃣ Use of Visual and Non-Verbal Cues
- The nurse should use simple gestures, facial expressions, and demonstration techniques to enhance message clarity.
- Visual aids such as pictures, cue cards, whiteboards, or printed materials are helpful in explaining procedures or instructions.
- Flashcards with daily activities or medical terms can be used for repetitive communication tasks.
- Nurses can also use videos with subtitles or digital tools to support patient understanding in educational sessions.
4️⃣ Speaking Techniques
- The nurse must speak at a moderate pace, using clear articulation without exaggeration or shouting, which can distort sounds.
- Short, simple sentences with pauses between key phrases help in better understanding.
- The nurse should maintain eye contact, avoid chewing gum or covering the mouth, and make sure the patient can see their lips.
- It is helpful to repeat or rephrase if the patient does not understand, and confirm understanding by asking them to repeat back important points.
5️⃣ Use of Assistive Devices
- The nurse should ensure the patient’s hearing aids or cochlear implants are functioning, clean, and worn correctly.
- Batteries should be checked and replaced regularly, and the patient should be trained in basic troubleshooting.
- Assistive listening devices such as pocket talkers, speech-to-text software, or captioned phones can be introduced.
- The nurse should be familiar with hospital-based alert systems compatible with hearing impairment, such as flashing call bells or vibrating pagers.
6️⃣ Patient and Family Education
- Nurses must teach both the patient and family how to maintain hearing devices, such as cleaning, drying, and storing them safely.
- Simple sign language techniques or basic hand signs can be taught to caregivers and family for everyday use.
- Education should also include what not to do, like shouting or speaking too quickly, and respecting the patient’s independence.
- Provide access to local or national resources, such as the Indian Association of the Deaf or audiology centers.
7️⃣ Documentation and Interdisciplinary Collaboration
- Nursing records should document the preferred communication method, type of hearing loss, and assistive devices used.
- The nurse should alert all healthcare providers involved to ensure consistent communication strategies across departments.
- Collaboration with audiologists, speech therapists, ENT specialists, and social workers should be initiated for comprehensive care.
- Updates should be communicated at shift changes and during rounds to maintain continuity and patient-centered care.
8️⃣ Promoting Psychosocial Well-being
- The nurse should assess for signs of social withdrawal, frustration, depression, or anxiety due to communication challenges.
- Encouraging participation in group therapy, social support programs, or patient forums for hearing-impaired individuals can promote inclusion.
- The nurse should reinforce positive self-esteem, respect patient autonomy, and create opportunities for the patient to make choices in care.
- Family counseling may be provided to address emotional impact and caregiver burden.
9️⃣ Emergency Preparedness
- The nurse must ensure visual alert systems (e.g., flashing lights for alarms, vibrating alerts) are in place in case of emergencies.
- Emergency plans should include written instructions and clear signage for evacuation or medical alert purposes.
- Staff should be trained to tap gently or wave to get the patient’s attention in urgent situations instead of calling aloud.
- In high-risk areas like ICUs, non-verbal code systems can be implemented for safety alerts.
🔟 Legal and Ethical Considerations
- Nurses must ensure all informed consents and health education are communicated in a manner the patient understands.
- All interactions should respect confidentiality, dignity, and the right to equal healthcare access.
- Ethical communication includes providing interpreters or assistive support as needed to avoid discrimination.
- The nurse should be aware of and follow policies aligned with the Rights of Persons with Disabilities Act (RPWD Act, India)
2. Patient with epileptic seizure
1. Pre-Ictal Phase Nursing Responsibilities (Before Seizure Begins)
- The nurse identifies and records the patient’s aura or pre-seizure symptoms such as dizziness, visual changes, tingling sensations, or anxiety.
- She ensures the environment is safe and clutter-free, removing sharp objects, loose wires, or anything that may cause injury.
- The nurse keeps bed in a low position, raises padded side rails, and ensures oxygen and suction are available at the bedside.
- She administers prescribed antiepileptic medications (e.g., phenytoin, carbamazepine, valproate) on time and watches for therapeutic levels.
- The nurse educates the patient to alert staff if an aura begins, and avoid standing or walking alone during this time.
- She ensures IV access is maintained, especially in ICU, for rapid medication administration during prolonged seizures.
2. Ictal Phase Nursing Responsibilities (During Seizure Activity)
- The nurse must remain calm and stay with the patient, ensuring immediate safety and avoiding unnecessary panic.
- She positions the patient in a side-lying position to prevent aspiration and support drainage of saliva or vomitus.
- The nurse supports the head with a pillow or folded blanket to prevent head trauma from banging against hard surfaces.
- She does not insert anything into the patient’s mouth (like fingers, spoon, or gauze), as it may cause choking or dental injury.
- The nurse loosens tight clothing around the neck or waist to promote airway comfort.
- She observes and records the onset, duration, body part involved first, type of movements, eye deviation, cyanosis, and whether the patient lost bladder/bowel control.
- The nurse calls for emergency assistance if seizure lasts more than 5 minutes (status epilepticus) or if another seizure begins before recovery.
- She administers emergency anticonvulsants (e.g., lorazepam, diazepam, midazolam IV or IM) if prescribed.
3. Post-Ictal Phase Nursing Responsibilities (After Seizure Ends)
- The nurse ensures airway patency by continuing the patient in a side-lying position and suctioning if needed.
- She monitors vital signs, consciousness level, pupil reactions, and respiratory status every 15–30 minutes until stable.
- She performs a quick neurological assessment to evaluate post-seizure deficits such as limb weakness, disorientation, or speech difficulty.
- The nurse documents the entire seizure episode, including triggers, type, duration, postictal confusion, and response to treatment.
- She allows the patient to rest in a quiet, low-stimulation environment, turning off bright lights or noise to promote calm.
- The nurse offers emotional support and reassurance, as patients may feel anxious, embarrassed, or fearful.
- She checks for injuries sustained during the seizure—tongue bite, bruises, head trauma, or dislocated limbs.
- The nurse assesses bladder/bowel incontinence, provides hygiene care, and ensures privacy and dignity.
4. Long-Term & General Nursing Management
- The nurse ensures strict compliance with long-term antiepileptic medication regimens, and observes for side effects like drowsiness or gum overgrowth (e.g., with phenytoin).
- She provides lifestyle counseling to help avoid triggers: sleep deprivation, flashing lights, skipping meals, and emotional stress.
- The nurse encourages regular neurological follow-up, EEG tests, and medication level monitoring.
- She educates the patient and family on how to respond to seizures at home: keeping calm, protecting the head, and timing the episode.
- The nurse promotes dietary support such as a ketogenic diet (in children or refractory epilepsy), as advised.
- She advises against driving, swimming alone, or using heavy machinery unless seizure-free for a medically approved period.
- The nurse encourages wearing medical identification bracelets with diagnosis and emergency instructions.
5. Hospital/ICU-Specific Seizure Precaution Measures
- The nurse ensures a seizure warning sign is placed at the patient’s bedside.
- She places padded side rails, removes restraints or restraints are padded to avoid injury.
- The nurse ensures oxygen cylinder, Ambu bag, suction machine, oral airways, and emergency drugs are within reach.
- She keeps airway adjuncts and IV diazepam or lorazepam ready, especially for patients with frequent seizures.
- The nurse includes seizure activity as part of the nursing care plan, shift reports, and ICU handovers.
- She coordinates with the team for neurology referrals, imaging (CT/MRI), and EEG scheduling.
3. Patient with skin grafting and reconstructive surgery
1️⃣ Preoperative Nursing Care
- Assess the extent, depth, and location of skin damage to determine the type of graft required.
- Educate the patient about the procedure, expectations, and recovery period.
- Obtain informed consent after explaining risks such as graft failure or infection.
- Provide psychological support to reduce anxiety related to appearance changes or pain.
- Ensure the patient is nutritionally optimized, as protein and vitamins are essential for wound healing.
- Prepare the donor and recipient sites with proper cleansing and antiseptic application.
2️⃣ Immediate Postoperative Care
- Maintain strict aseptic technique while handling dressings at graft and donor sites.
- Ensure immobilization of grafted area using splints or bandages to allow graft adherence.
- Monitor vital signs frequently, especially for signs of hypovolemia, infection, or graft rejection.
- Administer IV fluids and prescribed antibiotics to prevent dehydration and sepsis.
- Keep the patient in a position that reduces pressure on the graft site (e.g., limb elevation).
- Assess the graft site for color, warmth, bleeding, or fluid collection, which may indicate complications.
3️⃣ Pain Management
- Administer analgesics regularly as prescribed to manage pain from both donor and graft sites.
- Use cold compresses if advised for localized swelling (avoid direct application on graft).
- Encourage deep breathing and relaxation techniques to reduce anxiety-induced pain.
- Monitor the effectiveness of pain relief interventions and adjust accordingly.
4️⃣ Monitoring for Complications
- Observe for graft failure, which may present as discoloration, necrosis, or foul odor.
- Check for signs of wound infection, including pus, fever, or increased pain at the site.
- Monitor for hematoma formation under the graft, which may require evacuation.
- Assess the donor site for delayed healing, bleeding, or hypertrophic scarring.
- Record any signs of allergic reaction or systemic complications.
5️⃣ Wound Care and Dressing
- Change dressings as per schedule and surgeon’s instruction, usually after 3–5 days.
- Use non-adherent sterile dressings to protect graft and avoid trauma during removal.
- Clean wounds with normal saline or antiseptic solutions as prescribed.
- Monitor for exudate quantity, color, and odor during each dressing change.
6️⃣ Nutritional Support
- Provide a high-protein, high-calorie diet to promote tissue regeneration.
- Encourage oral intake of fluids, vitamin C, and zinc-rich foods for skin healing.
- Monitor intake-output and daily weight to assess nutritional progress.
- Consult a dietitian if special supplements are needed.
7️⃣ Mobility and Physiotherapy
- Initiate early passive or active range-of-motion (ROM) exercises after surgeon approval.
- Avoid shearing forces on the graft area during movement.
- Educate the patient on gradual ambulation and joint movement to prevent contractures.
- Collaborate with the physiotherapist for long-term rehabilitation planning.
8️⃣ Psychological and Emotional Support
- Address concerns related to body image, visible scars, and self-esteem.
- Provide opportunities for emotional expression and grief over appearance loss.
- Refer to counseling services or support groups when needed.
- Encourage family participation and emotional support throughout recovery.
9️⃣ Patient and Family Education
- Instruct the patient to avoid scratching or rubbing the grafted area.
- Teach the importance of protecting the graft from sun exposure or trauma.
- Educate about signs of infection or rejection and when to seek medical help.
- Instruct on proper home care, dressing changes, and scheduled follow-ups.
- Promote hygiene practices and adherence to medications post-discharge.
🔟 Discharge and Long-term Care
- Reinforce the need for regular follow-up appointments to monitor graft take and healing.
- Encourage use of compression garments or silicone sheets if prescribed to reduce scarring.
- Instruct patient to avoid heavy physical activities or contact sports until fully healed.
- Educate about scar massage, skin moisturization, and cosmetic rehabilitation.
Q.6 Write short notes on following (any four) (20 mark)
1. Seven ‘C’ of critical care unit
The Seven ‘C’s represent core principles or pillars that guide the operations, ethics, and functioning of an Intensive Care Unit (ICU) or Critical Care Unit. These are essential for maintaining high-quality care for critically ill patients.
1️⃣ Care
- It is the foundation of ICU functioning that involves continuous, intensive, and patient-specific medical support for life-threatening conditions.
- It includes advanced monitoring of vitals, neurological status, oxygen saturation, and hemodynamic parameters around the clock.
- It is provided using specialized equipment like cardiac monitors, infusion pumps, mechanical ventilators, and dialysis machines.
- It also includes prevention of complications like pressure ulcers, infections, DVT, and nutritional deficiencies.
- It is inclusive of both curative and palliative approaches, depending on the patient’s prognosis and medical condition.
- It demands that the care be multi-dimensional, including physical, emotional, psychological, and spiritual support.
2️⃣ Compassion
- It is the act of understanding and addressing the emotional suffering of critically ill patients and their families with empathy.
- It is especially needed in ICUs, where many patients are unconscious, ventilated, or in terminal stages and cannot express their needs.
- It includes respecting patient dignity, involving family in care decisions, and listening with empathy during emotional breakdowns.
- It is shown through gentle touch, eye contact, soft voice tone, and being emotionally present.
- It is vital in breaking bad news, where compassion balances truth with kindness.
- It helps relieve fear and anxiety, enhancing patient satisfaction and family trust in ICU services.
3️⃣ Communication
- It is a critical function in ICU that ensures smooth coordination between multidisciplinary team members (doctors, nurses, physiotherapists, etc.).
- It involves accurate shift handover reports, documentation of patient changes, and emergency alerts.
- It includes clear and honest discussions with patient families regarding treatment plans, progress, or prognosis.
- It must be timely, respectful, and non-judgmental, especially during critical situations.
- It helps in reducing medical errors, ethical dilemmas, and team conflicts in high-stakes ICU settings.
- It also includes use of non-verbal cues, communication aids, and writing tools for intubated or non-verbal patients.
4️⃣ Competence
- It is the ability of ICU staff to apply advanced clinical knowledge and technical skills confidently in emergency situations.
- It involves mastering ventilator settings, IV drug administration, CPR, and intubation protocols.
- It includes proficiency in interpreting ECG, ABG, X-ray, electrolyte values, and adjusting treatment accordingly.
- It also demands quick decision-making, problem-solving, and prioritizing care under pressure.
- It is maintained through regular skill drills, advanced life support training (BLS/ALS), and hands-on workshops.
- It involves staying updated with latest ICU protocols, research evidence, and new technologies in critical care.
5️⃣ Commitment
- It is the nurse’s or clinician’s dedication to preserving patient life and dignity, even under intense stress.
- It involves working extra hours, handling critical emergencies, and putting patient needs above personal comfort.
- It includes being present during end-of-life care, offering full support to both patient and family.
- It reflects in reporting errors honestly, following protocols strictly, and being available during code blue situations.
- It also involves voluntary participation in ICU audits, infection control programs, and team quality improvements.
- It creates a culture of reliability, professionalism, and patient-centeredness in the ICU.
6️⃣ Consistency
- It ensures that every patient receives uniform, high-quality care at all times, regardless of time, staff, or workload.
- It involves following evidence-based guidelines and ICU protocols without deviation.
- It is maintained by using checklists, standard drug charts, and time-bound interventions (e.g., VAP bundles, feeding protocols).
- It ensures patient safety by avoiding missed doses, documentation errors, or delayed interventions.
- It is the result of effective teamwork, role clarity, and disciplined nursing practice.
- It builds trust among staff and families, knowing that the care remains consistent across shifts.
7️⃣ Continuous Improvement
- It is the ongoing effort to upgrade ICU services, clinical skills, and patient outcomes using audit, feedback, and innovation.
- It includes morbidity/mortality reviews, root cause analysis, and risk assessments for critical events.
- It involves participation in quality improvement programs, NABH/NABL accreditation, and ICU benchmarking.
- It encourages reporting of near-misses, adverse events, and taking steps for prevention.
- It is supported by regular in-service education, hands-on training, and certification courses for ICU nurses.
- It promotes a culture of safety, accountability, and lifelong learning in ICU teams.
2. Types and causes of disaster
Types of Disasters
Disasters are broadly classified into three major types:
✅ Natural Disasters
Natural disasters are caused by natural forces and phenomena that occur without human intervention. These disasters can cause large-scale destruction and are often unpredictable.
Earthquakes
An earthquake is caused by the sudden movement of tectonic plates beneath the Earth’s surface. It results in violent shaking of the ground, collapsing buildings, bridges, and causing widespread injury and death.
Floods
Floods occur when water overflows its normal boundaries, due to heavy rainfall, river overflow, dam breakage, or glacier melting. Flooding can cause property damage, displacement of people, and waterborne diseases.
Cyclones, Hurricanes, and Typhoons
These are severe windstorms accompanied by heavy rain, formed over warm ocean waters. They cause destruction of houses, flooding, power outages, and loss of life, especially in coastal areas.
Droughts
A drought is a prolonged period of inadequate rainfall, leading to water shortages, crop failure, famine, and socio-economic crises. It can last for months or even years.
Tsunamis
A tsunami is a series of massive sea waves caused by underwater earthquakes or volcanic eruptions. Tsunamis can travel thousands of kilometers and flood coastal towns within minutes.
Volcanic Eruptions
This type of disaster involves the eruption of lava, ash, and gases from beneath the Earth’s surface. The lava flow can destroy vegetation, settlements, and affect air quality over large areas.
Landslides
Landslides occur when soil, rocks, or debris move down a slope due to gravity, often triggered by earthquakes, deforestation, or heavy rain. Landslides block roads and rivers and may bury homes.
Extreme Weather Events
These include hailstorms, heatwaves, snowstorms, and cold waves. Climate change has increased the frequency and severity of such weather disasters in recent years.
✅ Man-made or Anthropogenic Disasters
Man-made disasters occur as a result of human negligence, unsafe practices, conflict, or poor planning. These are preventable but often have severe consequences when they occur.
Industrial Accidents
These include chemical spills, gas leaks, or factory explosions. For example, the Bhopal gas tragedy in 1984 killed thousands due to a methyl isocyanate leak.
Nuclear Accidents
Nuclear disasters occur from malfunctions in nuclear reactors or poor handling of radioactive substances. The Chernobyl (1986) and Fukushima (2011) accidents are examples.
Transport Accidents
Disasters such as plane crashes, train derailments, or shipwrecks cause multiple fatalities and disrupt transportation systems.
Fires and Explosions
Fires in residential areas, hospitals, industries, or forests can result from short circuits, gas leaks, or carelessness. They cause injuries, loss of shelter, and even death.
Wars and Terrorism
Armed conflicts and terrorist attacks result in mass destruction of property, psychological trauma, displacement of people, and health crises.
Urbanization and Construction Failures
Unplanned urban growth and poorly constructed buildings lead to disasters like building collapse, fire outbreaks, and overburdened infrastructure.
Environmental Degradation
Overexploitation of natural resources, deforestation, and pollution contribute to soil erosion, flooding, and increased vulnerability to natural hazards.
✅ Biological Disasters
Biological disasters are caused by living organisms such as bacteria, viruses, parasites, and may spread rapidly among populations.
Epidemics and Pandemics
These are outbreaks of infectious diseases like cholera, dengue, COVID-19, and swine flu. They spread through contact, air, water, or vectors and affect public health systems.
Zoonotic Diseases
Diseases like avian influenza, Ebola, and rabies spread from animals to humans. Poor hygiene, close animal contact, and urbanization increase the risk.
Bioterrorism
This is the deliberate use of biological agents such as viruses or toxins to cause illness or death. Anthrax attacks are examples of bioterrorism.
Insect or Pest Infestation
These disasters destroy crops, leading to famine, food insecurity, and economic loss, especially in agrarian regions.
Causes of Disasters
Disasters may arise from one or a combination of multiple factors:
Natural Causes
- Movement of tectonic plates (earthquakes, tsunamis)
- Weather patterns and oceanic disturbances (cyclones, floods)
- Climatic changes (droughts, heatwaves)
- Geological changes (landslides, volcanic eruptions)
Human-induced Causes
- Industrial pollution and unsafe factory conditions
- Deforestation and urban sprawl without planning
- Wars, terrorism, and political conflicts
- Negligence in nuclear or chemical safety
- Poor waste management and sanitation
Biological Causes
- Emergence of new or drug-resistant pathogens
- Breakdown in public health infrastructure
- Animal-human interaction and poor veterinary care
- Global travel and urban overcrowding, aiding rapid spread
3. Physiological changes of geriatic
Physiological changes in the geriatric population refer to the gradual, progressive decline in the structure and function of body systems that naturally occurs with aging, typically after the age of 60. These changes increase susceptibility to disease, prolong recovery times, and reduce physical reserves, even in otherwise healthy individuals.
1️⃣ Cardiovascular System
- Arterial walls stiffen with age, increasing systolic blood pressure and cardiac workload.
- Left ventricular wall thickens, reducing the heart’s ability to increase output under stress.
- Heart valves may calcify, affecting blood flow and increasing the risk of murmurs and valvular disease.
- Peripheral circulation diminishes, often causing cold extremities and slower healing.
- Baroreceptor sensitivity declines, making elderly prone to orthostatic hypotension and falls.
2️⃣ Respiratory System
- Lung compliance decreases, reducing gas exchange and respiratory efficiency.
- Respiratory muscles weaken, leading to shallow breathing and reduced cough strength.
- Alveolar surface area shrinks, which decreases oxygen absorption into the bloodstream.
- Mucociliary clearance slows down, increasing the risk of respiratory infections.
- Pulmonary reserves diminish, limiting tolerance for physical exertion or stress.
3️⃣ Musculoskeletal System
- Bone resorption exceeds bone formation, leading to osteoporosis and fracture risk.
- Cartilage becomes thinner and more brittle, promoting stiffness and degenerative joint disease.
- Muscle mass and strength decline, impairing balance and mobility.
- Joint ligaments and tendons lose elasticity, causing decreased flexibility.
- Posture may change due to vertebral compression, leading to kyphosis or stooped appearance.
4️⃣ Nervous System
- Brain mass gradually decreases, affecting processing speed and complex learning.
- Reaction times slow, reducing ability to respond to sudden stimuli.
- Sleep quality declines with reduced deep and REM sleep stages.
- Sensory perception may dull, impairing detection of pain, temperature, or touch.
- Reflexes become less brisk, especially in the lower limbs, leading to coordination issues.
5️⃣ Gastrointestinal System
- Saliva production decreases, leading to dry mouth and difficulty swallowing.
- Gastric acid secretion reduces, impairing protein digestion and B12 absorption.
- Slower intestinal motility results in constipation and gas buildup.
- Liver metabolism declines, affecting drug processing and detoxification.
- Appetite may be reduced due to changes in taste, smell, and hormone levels.
6️⃣ Genitourinary System
- Renal mass and nephron number decline, reducing glomerular filtration and urine concentration.
- Bladder elasticity and capacity decrease, causing urgency and incomplete emptying.
- Post-void residual urine increases, raising the risk of urinary tract infections.
- Prostate gland enlarges in males, leading to urinary hesitancy or retention.
- Estrogen loss in females leads to vaginal dryness, irritation, and stress incontinence.
7️⃣ Integumentary System (Skin, Hair, Nails)
- Epidermis thins, making the skin fragile and more prone to tearing or bruising.
- Sebaceous and sweat gland activity diminishes, causing dryness and poor thermoregulation.
- Wound healing is delayed due to reduced blood flow and cellular repair.
- Pigmentation changes may occur, such as age spots or uneven tone.
- Nails grow more slowly and may become thickened, discolored, or ridged.
8️⃣ Endocrine System
- Insulin sensitivity declines, increasing the risk of glucose intolerance and diabetes.
- Thyroid hormone levels may decrease slightly, contributing to fatigue and cold sensitivity.
- Cortisol regulation becomes less responsive to stress, affecting immune and metabolic response.
- Growth hormone levels fall, reducing muscle mass and increasing body fat.
- Declines in sex hormones affect libido, bone density, and energy levels.
9️⃣ Immune System
- T-cell and B-cell function declines, weakening adaptive immunity.
- Autoimmune activity may increase, leading to chronic inflammatory conditions.
- Elderly individuals respond poorly to vaccinations and are more prone to infections.
- Inflammatory responses become exaggerated or prolonged, delaying recovery.
- Fever response may be absent or blunted during infection, delaying diagnosis.
🔟 Sensory System (Vision, Hearing, Taste, Smell)
- Lens stiffens and becomes opaque, causing presbyopia and risk of cataracts.
- Pupillary response slows, impairing adaptation to changes in light.
- Auditory nerve degeneration results in difficulty hearing high-frequency sounds.
- Taste bud count decreases, reducing the perception of salty and sweet flavors.
- Smell receptor function declines, affecting enjoyment of food and detection of hazards like smoke.
4. Menstrual disorder
Definition of Menstrual Disorders
- It is a broad term used to describe abnormalities in menstrual cycle frequency, duration, regularity, or volume of flow in females during reproductive age.
- It includes absence of menstruation, heavy bleeding, painful periods, irregular cycles, or pre-menstrual issues, which may indicate hormonal imbalance, structural pathology, or systemic diseases.
Types of Menstrual Disorders
1️⃣ Amenorrhea
- It is the absence of menstruation.
- Primary amenorrhea is when menstruation has not started by age 15.
- Secondary amenorrhea is the cessation of menses for more than 3 months in a previously menstruating female.
2️⃣ Dysmenorrhea
- It is the condition in which the female experiences painful menstruation, typically in the lower abdomen or pelvis.
- Primary dysmenorrhea occurs without pelvic pathology, while secondary dysmenorrhea is associated with diseases like endometriosis or fibroids.
3️⃣ Menorrhagia
- It is defined as excessive menstrual bleeding (>80 mL per cycle or lasting more than 7 days).
- It is commonly associated with fibroids, adenomyosis, coagulation disorders, or hormonal imbalances.
4️⃣ Metrorrhagia
- It is the occurrence of bleeding between menstrual periods.
- It is commonly caused by hormonal imbalance, endometrial polyps, infections, or contraceptive use.
5️⃣ Oligomenorrhea
- It refers to infrequent menstrual periods, with cycles exceeding 35 days.
- It is often linked with PCOS, thyroid dysfunction, or excessive exercise.
6️⃣ Polymenorrhea
- It is the condition in which menstrual cycles occur more frequently than every 21 days.
- It may result in reduced fertility due to shortened follicular phase.
7️⃣ Hypomenorrhea
- It is defined as scanty menstrual flow or bleeding lasting less than 2 days.
- It is often seen in women using oral contraceptives or having uterine adhesions (Asherman’s syndrome).
8️⃣ Premenstrual Syndrome (PMS)
- It is a combination of emotional, physical, and behavioral symptoms that occur 1–2 weeks before menstruation and resolve with onset.
- Common symptoms include mood swings, irritability, bloating, breast tenderness, and fatigue.
9️⃣ Premenstrual Dysphoric Disorder (PMDD)
- It is a severe form of PMS, in which psychological symptoms like depression, anger, or anxiety significantly interfere with daily functioning.
- It may require antidepressants or hormonal therapy for control.
Etiology
- Hormonal imbalance (estrogen/progesterone)
- Polycystic Ovary Syndrome (PCOS)
- Thyroid disorders
- Uterine fibroids or endometriosis
- Emotional stress or eating disorders
- Weight loss/gain or excessive exercise
- Coagulation disorders
- Use of certain drugs (antipsychotics, chemo)
Clinical Manifestations
- Missed or delayed periods
- Excessive or scanty bleeding
- Severe abdominal cramps
- Breast tenderness, mood changes
- Bloating, headache, fatigue
- Intermenstrual spotting or bleeding
Diagnostic Evaluation
- Menstrual history and physical exam
- Pregnancy test (to rule out pregnancy)
- Pelvic ultrasound
- Hormonal profile (TSH, FSH, LH, Prolactin)
- Pap smear
- Endometrial biopsy (if needed)
Management
1️⃣ Hormonal Therapy
- It is common to prescribe oral contraceptive pills (OCPs) to regulate cycles and reduce heavy bleeding.
- It is advised to give progesterone therapy in cases of luteal phase defects or amenorrhea.
- It is necessary to treat underlying endocrine disorders, like using levothyroxine for hypothyroidism or metformin for PCOS.
2️⃣ Non-Hormonal Medications
- It is helpful to use NSAIDs (e.g., ibuprofen) for pain relief in dysmenorrhea and to reduce bleeding.
- It is recommended to give tranexamic acid in cases of heavy menstrual bleeding (menorrhagia).
3️⃣ Surgical Management
- It may include dilation and curettage (D&C), myomectomy, endometrial ablation, or hysterectomy in severe cases.
- It is required when medical treatment fails or structural abnormality exists.
Nursing Management
1️⃣ Assessment and History Taking
- It is important to obtain a detailed menstrual history including age of menarche, cycle duration, amount of bleeding, and associated symptoms.
- It is necessary to assess for emotional stress, weight changes, and use of contraceptives or medications.
2️⃣ Monitoring and Observation
- It is essential to monitor vital signs, especially if heavy bleeding is present (watch for signs of anemia).
- It is the nurse’s responsibility to record menstrual flow patterns, clots, and duration during hospitalization or follow-up.
3️⃣ Medication Administration and Support
- It is necessary to administer prescribed hormonal or pain medications and observe for side effects.
- It is the nurse’s role to ensure patient adherence to medication schedules and follow-up.
4️⃣ Psychological and Emotional Support
- It is important to address anxiety and embarrassment related to abnormal menstruation.
- It is helpful to provide a supportive, non-judgmental environment, especially for adolescents or unmarried females.
5️⃣ Nutritional and Lifestyle Counseling
- It is advised to promote a balanced diet rich in iron, calcium, and vitamins to correct nutritional deficiencies.
- It is necessary to educate about weight maintenance, exercise, and stress reduction techniques.
6️⃣ Health Education and Follow-up
- It is essential to explain the nature of the disorder, treatment options, and importance of compliance.
- It is important to teach how to track menstrual cycles and recognize abnormal patterns.
- It is the nurse’s duty to arrange regular gynecological follow-ups and referral if required.
5. First 24 hours fluid replacement therapy in burns
Definition
- It is the emergency administration of intravenous fluids to a burn patient during the first 24 hours post-injury, in order to restore circulating volume, maintain organ perfusion, and prevent burn shock.
- It is especially critical in patients with burns >15% of Total Body Surface Area (TBSA) in adults or >10% TBSA in children.
Purpose of Fluid Replacement Therapy
- It is to prevent hypovolemic shock due to massive fluid loss from burned tissues.
- It is done to maintain urine output, tissue perfusion, and acid-base balance.
- It is necessary to support cardiovascular and renal function during the acute phase.
Common Formula Used – Parkland Formula
- It is the most widely used formula for fluid resuscitation during the first 24 hours.
- It is calculated as :
- Parkland Formula = 4 mL × body weight (kg) × % TBSA burned
- It is used to determine the total volume of Ringer’s Lactate solution to be given in the first 24 hours.
Fluid Distribution Schedule
1️⃣ First 8 Hours (from time of burn, not admission):
- It is mandatory to give 50% of total calculated fluid volume during this period.
- It is essential to adjust timing if there’s a delay in admission — fluids must be given based on the time of burn.
2️⃣ Next 16 Hours :
- It is advised to give the remaining 50% of the total fluid slowly over the next 16 hours.
- It is necessary to monitor urine output and vital signs during this phase to adjust rate.
Example Calculation
Adult patient : 70 kg weight, 40% TBSA burn
4 mL × 70 kg × 40 = 11,200 mL in 24 hours
First 8 hours : 5,600 mL
Next 16 hours : 5,600 mL
Type of Fluid Used
- It is recommended to use Ringer’s Lactate (RL) solution, as it closely resembles extracellular fluid and contains electrolytes.
- It is preferred over Normal Saline, as NS can cause hyperchloremic acidosis in large volumes.
Nursing Responsibilities in First 24 Hours
1️⃣ Calculation and Preparation
- It is the nurse’s responsibility to accurately calculate fluid needs using Parkland formula based on TBSA, body weight, and time of injury.
- It is necessary to prepare and label IV fluids with the exact hourly rate.
2️⃣ Monitoring Parameters
- It is important to monitor urine output, which should be 0.5–1 mL/kg/hour in adults and 1–2 mL/kg/hour in children.
- It is necessary to assess vital signs hourly, including blood pressure, pulse, respiratory rate, and temperature.
- It is essential to observe for signs of fluid overload (pulmonary edema) or inadequate perfusion (hypotension, cold extremities).
3️⃣ IV Access and Line Maintenance
- It is vital to establish large-bore peripheral IV access (or central line in severe burns).
- It is the nurse’s duty to ensure patency and secure fixation of the IV line.
4️⃣ Documentation
- It is necessary to document input/output hourly, fluid volumes given, and urine characteristics.
- It is essential to record fluid adjustments made based on clinical parameters.
5️⃣ Patient and Family Education
- It is important to explain the purpose and process of fluid therapy to the patient (if conscious) and relatives.
- It is the nurse’s role to reduce anxiety and ensure emotional support during the acute phase.
Q.7 Write short answer
1. Care of patient on osmotic diuretics (3)
1️⃣ Pre-Administration Assessment
- It is essential to check for history of cardiovascular disorders such as CHF, as mannitol may worsen the condition.
- It is important to monitor fluid volume status, including edema, skin turgor, mucous membrane hydration, and weight.
- It is mandatory to assess serum glucose levels, especially in diabetic patients, as mannitol may cause hyperglycemia.
- It is advised to check for signs of increased ICP, such as headache, nausea, vomiting, or altered LOC.
- It is also important to ensure renal function tests are within acceptable limits (creatinine <1.5 mg/dL, adequate urine output).
2️⃣ Drug Administration Care
- It is required to administer mannitol slowly via IV infusion, typically over 30–60 minutes to prevent hypotension.
- It is necessary to use a micron filter (0.22 µm) while infusing mannitol to prevent crystallized particles entering circulation.
- It is important to label the line “MANNITOL” clearly and never mix with other IV drugs to prevent incompatibility.
- It is crucial to document time, dose, rate of administration, and patient response in the nursing record.
- It is also important to have emergency equipment ready, especially in high-risk patients for anaphylaxis or fluid overload.
3️⃣ Monitoring During Therapy
- It is essential to monitor neurological parameters, including Glasgow Coma Scale (GCS), pupillary reaction, and orientation.
- It is important to evaluate lung sounds every 4 hours to detect early signs of pulmonary edema.
- It is necessary to track serum sodium, potassium, and osmolality every 4–6 hours during aggressive therapy.
- It is advised to monitor for hypotension or tachycardia, which may indicate volume depletion or circulatory collapse.
- It is helpful to maintain an input-output chart, measure urine specific gravity, and report any significant changes.
4️⃣ Patient Education
- It is important to educate the patient about frequent urination and advise not to limit fluid intake unless restricted.
- It is essential to inform them about possible side effects like dry mouth, light-headedness, and fatigue.
- It is advised to educate the patient or family to report any confusion, blurred vision, chest pain, or breathing difficulty immediately.
- It is also necessary to provide psychological support, especially for patients with neurological disorders.
- It is helpful to explain the duration and purpose of therapy clearly to gain cooperation and reduce anxiety.
5️⃣ Post-Administration Care
- It is necessary to repeat serum creatinine, electrolytes, and osmolality to assess renal function and systemic response.
- It is essential to check daily body weight to monitor for fluid retention or excessive fluid loss.
- It is important to observe for signs of rebound increase in ICP, especially after stopping mannitol abruptly.
- It is also necessary to observe for signs of allergic reactions or phlebitis at IV site.
- It is critical to reassess the indication for continuation of therapy with the medical team daily.
2. List the pediatric emergency and explain any one (4)
Pediatric emergencies are life-threatening conditions that require immediate recognition and intervention in infants, children, and adolescents. These may be medical, surgical, traumatic, or related to congenital conditions.
Common Pediatric Emergencies Include
- Respiratory distress/failure
- Status asthmaticus (severe asthma attack)
- Seizures (including febrile seizures or status epilepticus)
- Severe dehydration
- Anaphylaxis (severe allergic reaction)
- Acute poisoning
- Foreign body aspiration
- Drowning or near-drowning
- Cardiac arrest
- Traumatic injuries (head injury, burns, fractures)
- Meningitis or encephalitis
- Shock (hypovolemic, septic, cardiogenic)
- Acute appendicitis or abdominal pain
- High-grade fever with altered sensorium
- Diabetic ketoacidosis (DKA)
Respiratory distress
Definition of Respiratory Distress
- It is a clinical condition seen in neonates and children in which the respiratory system is unable to maintain adequate gas exchange, leading to impaired oxygenation and/or carbon dioxide removal.
- It is most commonly due to airway obstruction, lung pathology, or neuromuscular weakness, and can rapidly progress to respiratory failure if not identified and managed promptly.
Etiology
- Congenital anomalies (e.g., choanal atresia, diaphragmatic hernia)
- Infections (e.g., pneumonia, bronchiolitis, sepsis)
- Prematurity (surfactant deficiency)
- Airway obstruction (foreign body, croup, epiglottitis)
- Asthma or allergic reactions
- Neuromuscular disorders (e.g., spinal muscular atrophy)
- Cardiac anomalies (e.g., congenital heart disease)
Clinical Manifestations
- Tachypnea (increased respiratory rate)
- Nasal flaring
- Grunting or stridor
- Subcostal/intercostal retractions
- Cyanosis (especially lips and fingertips)
- Head bobbing (in infants)
- Restlessness or irritability
- Poor feeding or lethargy
- Decreased oxygen saturation (SpO₂)
Diagnostic Evaluation
- Pulse oximetry (SpO₂ monitoring)
- Arterial blood gas (ABG)
- Chest X-ray
- CBC and blood cultures (if infection suspected)
- Nasopharyngeal swab (viral PCR)
- Echocardiography (if congenital heart disease suspected)
- Lung ultrasound (in neonates)
Medical Management
1️⃣ Oxygen Therapy
- It is the first step in treating hypoxia and is delivered using hood, nasal cannula, face mask, or high-flow nasal oxygen.
- It is adjusted according to age and SpO₂ levels, maintaining target SpO₂ > 94%.
2️⃣ Surfactant Therapy (Neonatal RDS)
- It is given through an endotracheal tube in premature babies to reduce surface tension and improve alveolar expansion.
- It helps decrease the need for mechanical ventilation.
3️⃣ Antibiotic or Antiviral Therapy
- It is initiated if bacterial or viral infection is suspected (e.g., pneumonia, RSV).
- It should be culture-guided and age-appropriate.
4️⃣ Bronchodilators and Steroids
- It is used in asthma or bronchiolitis to relieve bronchospasm.
- Inhaled salbutamol, nebulized adrenaline, or oral dexamethasone may be given depending on the diagnosis.
5️⃣ Ventilatory Support
- It includes CPAP (Continuous Positive Airway Pressure) or mechanical ventilation in cases of moderate to severe respiratory failure.
- Endotracheal intubation is done in case of apnea, bradycardia, or refractory hypoxia.
6️⃣ Hydration and Electrolyte Management
- It is important to maintain fluid balance, especially in cases of increased insensible losses due to tachypnea.
- IV fluids may be needed when oral feeding is difficult.
Nursing Management
1️⃣ Assessment and Monitoring
- It is important to monitor respiratory rate, pattern, effort, and SpO₂ continuously.
- It is necessary to observe for retractions, grunting, nasal flaring, and changes in mental status.
- It is essential to assess for cyanosis and perfusion (capillary refill time).
2️⃣ Oxygen and Airway Management
- It is the nurse’s duty to administer humidified oxygen, ensure patency of airway, and position the child in semi-Fowler’s or sniffing position.
- It is necessary to provide suctioning, if secretions obstruct the airway.
- It is essential to prepare for intubation equipment if signs of respiratory failure develop.
3️⃣ Medication Administration
- It is the nurse’s role to administer bronchodilators, antibiotics, steroids, and antipyretics as prescribed.
- It is necessary to observe for adverse drug reactions, especially with nebulized agents or steroids.
- It is vital to record medication timings and respiratory response post-administration.
4️⃣ Nutrition and Fluid Management
- It is important to monitor fluid intake and output and prevent dehydration, especially in infants.
- It is advisable to withhold oral feeding during severe distress to prevent aspiration.
- IV fluids or NG feeds may be used to maintain nutrition.
5️⃣ Family Support and Education
- It is necessary to keep parents informed and involved in the treatment plan and care process.
- It is helpful to provide psychological reassurance, especially when the child is in NICU or on a ventilator.
- It is the nurse’s responsibility to educate parents about home care, warning signs, and follow-up visits.