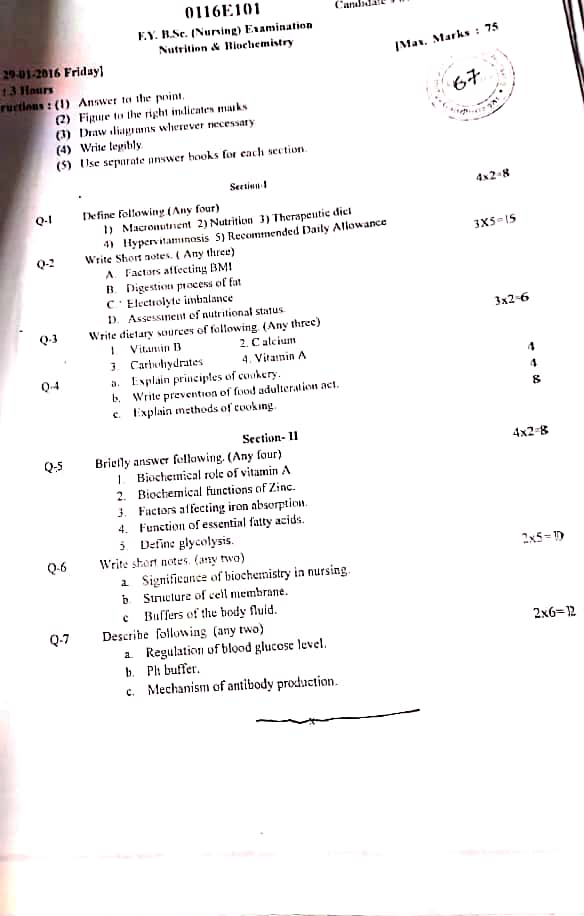
29/01/2016-NUTRI & BIOCHEM-PAPER NO.06
PAPER SOLUTION NO.06-29/01/2016
Section 1
Q.1 Define folowing (any four) (4×2=8)
1. Macronutrient
- Macronutrients are the essential nutrients required by the human body in large amounts to provide energy and support growth, maintenance, and overall physiological functions.
- They include carbohydrates, proteins, and fats, which supply the bulk of energy (measured in kilocalories) and are vital for body structure and metabolic processes.
2. Nutrition
- Nutrition is the science that studies the process by which the body takes in, absorbs, transports, utilizes, and excretes food substances to maintain health, support growth, repair tissues, and produce energy.
- It includes the intake of essential nutrients like carbohydrates, proteins, fats, vitamins, minerals, and water required for normal functioning of the body.
3. Therpeutic diet
- A therapeutic diet is a planned and medically prescribed modification of the regular diet, which is tailored to meet the specific nutritional needs of a patient to manage or treat a particular disease or medical condition.
- This type of diet may involve changes in nutrient content, texture, consistency, or meal frequency, and is used as part of the treatment regimen for conditions like diabetes, hypertension, renal disease, gastrointestinal disorders, or obesity.
4. Hypervitaminosis
- Hypervitaminosis is a condition resulting from the excessive intake or accumulation of one or more fat-soluble vitamins (mainly vitamins A, D, E, or K) in the body, leading to toxic effects and harmful clinical symptoms.
- This condition usually occurs due to over-supplementation rather than from food sources, and the symptoms vary depending on which vitamin is in excess.
- Common Examples:
Vitamin A toxicity may cause headache, liver damage, and dry skin
Vitamin D toxicity may result in hypercalcemia, nausea, and kidney damage
5. Recommended daily allowance
- Recommended Daily Allowance (RDA) refers to the average daily intake level of essential nutrients that is sufficient to meet the nutritional requirements of nearly all (97–98%) healthy individuals in a particular age group, gender, and physiological condition (such as pregnancy or lactation).
- RDA values are established by expert scientific bodies (like ICMR in India) and are used as guidelines for planning balanced diets and preventing nutritional deficiencies.
- Example:
RDA for Iron in adult women = 21 mg/day
RDA for Protein in adult men = 60 g/day
Q.2 Write short notes (any three) (3×5=15)
1. Factor affecting BMI
- Body Mass Index (BMI) is a numerical value derived by dividing a person’s weight in kilograms by the square of their height in meters (kg/m²), and it is used to assess the weight category of an individual as underweight, normal, overweight, or obese.
- BMI serves as an essential tool in clinical settings to identify risks associated with cardiovascular diseases, diabetes, and malnutrition, although it does not directly measure body fat percentage.
1️⃣ Age
- Age significantly influences BMI, as basal metabolic rate (BMR) tends to decrease with advancing age, leading to gradual fat accumulation even with constant dietary intake.
- In children and adolescents, BMI can vary due to growth spurts and developmental changes, making age-specific BMI percentiles more accurate for assessment.
- Elderly individuals often lose lean muscle mass (sarcopenia), which may result in a seemingly normal or low BMI despite unhealthy body composition.
2️⃣ Gender
- Gender differences in hormone levels influence fat distribution and body composition; males generally have more muscle mass while females have more subcutaneous fat, affecting BMI interpretation.
- During reproductive phases such as menstruation, pregnancy, and menopause, hormonal shifts in females can contribute to fluctuations in weight and BMI.
- In males, declining testosterone with age may contribute to increased abdominal fat and altered BMI.
3️⃣ Genetic Factors
- Genetic predisposition can affect appetite control, satiety mechanisms, resting energy expenditure, and tendency to store fat in specific body regions, thereby altering BMI.
- Mutations in genes such as FTO (fat mass and obesity-associated gene) are linked to increased risk of obesity and higher BMI.
- Family history of obesity or metabolic disorders raises susceptibility to abnormal BMI even under moderate lifestyle control.
4️⃣ Physical Activity Level
- Regular physical activity promotes calorie burning, improves muscle-to-fat ratio, and helps maintain optimal BMI.
- Lack of exercise or sedentary behavior leads to unused calorie storage as fat, gradually increasing BMI.
- Type, intensity, and duration of physical activity (e.g., aerobic vs resistance training) also influence muscle mass and BMI outcomes.
5️⃣ Dietary Habits
- Diets rich in fats, sugars, and processed foods lead to excessive calorie intake and fat accumulation, pushing BMI higher.
- Skipping meals or irregular eating patterns can disrupt metabolism and promote fat storage.
- Consuming a balanced diet with adequate protein, fiber, and hydration supports healthy metabolism and stable BMI.
6️⃣ Socioeconomic Status
- Low-income individuals may face barriers to accessing healthy food, resulting in reliance on inexpensive, calorie-dense foods that increase BMI.
- Limited access to safe recreational areas or gyms contributes to physical inactivity and weight gain.
- Education level influences awareness about nutrition, weight management, and health consequences related to BMI.
7️⃣ Psychological Factors
- Stress and depression often lead to emotional eating, binge-eating, or anorexia, which can result in either elevated or low BMI.
- Body image disturbances and eating disorders such as anorexia nervosa, bulimia nervosa, and binge-eating disorder directly alter body weight and BMI.
- Sleep disturbances, often associated with psychological stress, can influence hormonal regulation of hunger and contribute to weight changes.
8️⃣ Cultural and Environmental Influences
- Cultural norms and traditions influence food preferences, portion sizes, and attitudes towards physical activity, affecting BMI over time.
- Urban environments with high fast-food density and limited spaces for exercise contribute to a lifestyle that promotes higher BMI.
- Cultural perception of body image can influence motivation to maintain or change weight, affecting BMI behaviorally.
9️⃣ Medical Conditions
- Certain diseases such as hypothyroidism, Cushing’s syndrome, and polycystic ovarian syndrome (PCOS) slow down metabolism and promote fat accumulation, leading to higher BMI.
- Conditions like malabsorption syndromes, chronic infections, cancer, and anorexia may cause muscle wasting and reduce BMI drastically.
- Physical disability or chronic pain conditions may reduce physical activity, indirectly causing weight gain and BMI elevation.
🔟 Medications
- Medications such as corticosteroids, insulin, antidepressants, and antipsychotics can alter metabolism or appetite, resulting in significant weight gain and increased BMI.
- Long-term use of beta blockers and anticonvulsants may slow metabolic rate and promote fat deposition.
- Drug-induced weight changes are often overlooked but can complicate BMI interpretation in clinical practice.
🔢 Hormonal Imbalances
- Hormonal disturbances due to thyroid dysfunction, adrenal hyperfunction, or insulin resistance interfere with normal metabolism, affecting body fat levels and BMI.
- In women, hormonal shifts during menstrual cycle, pregnancy, or menopause can lead to temporary or permanent weight changes.
- Growth hormone deficiency in children or adults contributes to decreased lean mass and increased fat, influencing BMI.
2. Digestion process of fat
- Fat digestion refers to the physiological process through which complex lipids consumed in the diet are broken down into simpler absorbable molecules such as monoglycerides and free fatty acids.
- The process involves a series of mechanical actions, emulsification by bile, and enzymatic breakdown primarily in the small intestine.
- Since fats are hydrophobic and insoluble in water, their digestion is more complex than that of carbohydrates or proteins and requires specialized enzymes and transport mechanisms.
1️⃣ Ingestion of Fat
- Dietary fats such as triglycerides, phospholipids, and cholesterol esters are consumed through foods like oils, butter, dairy products, meat, and nuts.
- Triglycerides make up the bulk of dietary fats, consisting of a glycerol molecule bound to three fatty acid chains.
- Fat-soluble vitamins (A, D, E, K) are also consumed along with lipids and depend on fat digestion and absorption for their own uptake into the body.
- In this initial stage, fat is not chemically altered but is chewed and mixed with saliva for transport to the stomach.
2️⃣ Minimal Digestion in the Mouth
- In the oral cavity, lingual lipase is secreted by the Ebner’s glands located on the tongue and becomes more active in acidic pH later in the stomach.
- Though lingual lipase initiates fat digestion, its activity in the mouth is very limited due to neutral pH and short retention time.
- Chewing mixes fat with other food particles and prepares it for further processing in the gastrointestinal tract.
- Lipids remain in large globules, which are poorly dispersed without bile.
3️⃣ Partial Digestion in the Stomach
- In the stomach, gastric lipase, secreted by chief cells, begins hydrolysis of short- and medium-chain triglycerides, mainly effective in infants.
- The churning and muscular contractions of the stomach help in mechanically breaking fat globules into smaller droplets, increasing their surface area.
- The acidic pH of the stomach enhances the activity of lingual and gastric lipases, although digestion remains incomplete at this stage.
- Fats delay gastric emptying, allowing prolonged contact time with gastric enzymes.
4️⃣ Emulsification in the Duodenum
- Arrival of partially digested fat in the duodenum triggers the secretion of cholecystokinin (CCK) from enteroendocrine cells.
- CCK stimulates the gallbladder to contract and release bile, which contains bile salts, bile pigments, cholesterol, and phospholipids essential for emulsification.
- Bile salts act like detergents and break large fat globules into tiny droplets, forming a stable emulsion that increases the surface area for enzyme action.
- Bile also activates pancreatic enzymes and aids in the solubilization of cholesterol and fat-soluble vitamins for absorption.
5️⃣ Enzymatic Digestion by Pancreatic Lipase
- Pancreatic lipase, secreted by the exocrine pancreas, is the most potent enzyme responsible for hydrolyzing triglycerides into 2-monoglycerides and free fatty acids.
- The action of pancreatic lipase is enhanced by colipase, which anchors the enzyme to the emulsified fat droplet and prevents inactivation by bile salts.
- In addition to lipase, cholesterol esterase and phospholipase A2 break down cholesterol esters and phospholipids, respectively.
- Enzyme action in the small intestine is most effective in the neutral to slightly alkaline pH, maintained by bicarbonate secreted from the pancreas.
6️⃣ Micelle Formation
- After enzymatic digestion, free fatty acids, monoglycerides, cholesterol, and fat-soluble vitamins combine with bile salts to form micelles, which are tiny spherical complexes.
- Micelles are water-soluble on the outside and hydrophobic on the inside, allowing them to transport lipids across the watery intestinal lumen to the brush border.
- Without micelle formation, the absorption of fat components would be severely impaired due to their poor solubility in water.
- Micelles constantly release and reabsorb lipids at the surface of enterocytes, facilitating steady absorption.
7️⃣ Absorption in the Small Intestine
- At the brush border of the jejunum and ileum, micelles disintegrate and release their contents, which then passively diffuse into the intestinal epithelial cells (enterocytes).
- Inside the enterocyte, fatty acids and monoglycerides are transported to the smooth endoplasmic reticulum, where they are re-esterified into triglycerides.
- These triglycerides, along with phospholipids, cholesterol, and apolipoproteins, are packed into chylomicrons—lipoprotein complexes ready for transport.
- Short- and medium-chain fatty acids may bypass chylomicron packaging and enter the portal circulation directly.
8️⃣ Transport of Chylomicrons via Lymphatic System
- Chylomicrons are too large to enter blood capillaries and are instead absorbed into lacteals, the lymphatic vessels in the intestinal villi.
- These chylomicrons enter the lymphatic circulation, then drain into the thoracic duct, which empties into the left subclavian vein, entering systemic circulation.
- In the bloodstream, lipoprotein lipase on capillary walls breaks down triglycerides in chylomicrons, allowing uptake by tissues like muscle and adipose tissue.
- Remnants of chylomicrons are taken up by the liver, where further processing of lipids occurs.
Utilization and Storage of Fat
- Once inside body cells, fatty acids are either oxidized via β-oxidation to produce energy (ATP) or stored in adipose tissue as triglycerides.
- Liver plays a central role in regulating lipid metabolism, converting excess carbohydrates and proteins into fatty acids through lipogenesis.
- During fasting or starvation, stored fat is broken down into free fatty acids and ketone bodies to supply energy to the brain and body tissues.
- Any excess fat not used is stored long-term, contributing to body fat reserves and obesity risk.
3. Electrolyte imbalance
Definition of Electrolyte Imbalance
- Electrolyte imbalance is defined as a condition in which the concentration of one or more electrolytes in the body becomes too high or too low, affecting the body’s ability to maintain homeostasis, fluid balance, nerve conduction, muscle contraction, and acid-base equilibrium.
- Electrolytes are charged minerals present in blood and body fluids including sodium (Na⁺), potassium (K⁺), calcium (Ca²⁺), magnesium (Mg²⁺), chloride (Cl⁻), bicarbonate (HCO₃⁻), and phosphate (PO₄³⁻).
Common Electrolytes and Their Normal Values
| Electrolyte | Normal Value |
|---|---|
| Sodium (Na⁺) | 135–145 mEq/L |
| Potassium (K⁺) | 3.5–5.0 mEq/L |
| Calcium (Ca²⁺) | 8.5–10.5 mg/dL |
| Magnesium (Mg²⁺) | 1.5–2.5 mEq/L |
| Chloride (Cl⁻) | 96–106 mEq/L |
| Phosphate (PO₄³⁻) | 2.5–4.5 mg/dL |
| Bicarbonate (HCO₃⁻) | 22–28 mEq/L |
Types of Electrolyte Imbalance and Their Symptoms
1. Hyponatremia (Serum Sodium < 135 mEq/L)
- Hyponatremia is a condition in which sodium levels in the blood fall below 135 mEq/L, often due to fluid overload, kidney disorders, SIADH, or prolonged vomiting and diarrhea.
- Symptoms include nausea, vomiting, muscle cramps, fatigue, headache, and mental confusion.
- In severe cases, the patient may experience seizures, altered sensorium, cerebral edema, and even coma, due to swelling of brain cells from excess water.
2. Hypernatremia (Serum Sodium > 145 mEq/L)
- Hypernatremia is characterized by elevated blood sodium levels, usually caused by dehydration, excessive salt intake, diabetes insipidus, or osmotic diuresis.
- The patient may complain of extreme thirst, dry tongue, dry mucous membranes, restlessness, irritability, and weakness.
- Severe cases may progress to neuromuscular excitability, seizures, and intracranial hemorrhage due to brain cell dehydration.
3. Hypokalemia (Serum Potassium < 3.5 mEq/L)
- Hypokalemia is defined as low potassium levels in the blood, often seen in patients using loop diuretics, corticosteroids, insulin therapy, or in chronic vomiting/diarrhea.
- Common symptoms include muscle weakness, leg cramps, fatigue, constipation, and flattened T waves or ST depression on ECG.
- If untreated, it can lead to life-threatening arrhythmias, hypotonia, respiratory weakness, and paralysis.
4. Hyperkalemia (Serum Potassium > 5.0 mEq/L)
- Hyperkalemia occurs when there is an excess of potassium in the blood, most commonly due to renal failure, burns, hemolysis, potassium-sparing diuretics, or tissue damage.
- Symptoms include muscle twitching, numbness, weakness, bradycardia, and gastrointestinal upset.
- ECG may show peaked T waves, widened QRS complexes, and in severe cases, ventricular fibrillation or cardiac arrest.
5. Hypocalcemia (Serum Calcium < 8.5 mg/dL)
- Hypocalcemia is a condition where calcium levels are low, often associated with vitamin D deficiency, hypoparathyroidism, pancreatitis, or renal failure.
- Clinical signs include numbness or tingling in the hands and feet, muscle spasms, laryngospasm, and positive Chvostek’s and Trousseau’s signs (indicators of neuromuscular excitability).
- If not corrected, it can lead to seizures, tetany, and cardiac arrhythmias.
6. Hypercalcemia (Serum Calcium > 10.5 mg/dL)
- Hypercalcemia is an excess of calcium in the blood, which may occur due to hyperparathyroidism, malignancies, prolonged immobilization, or excessive vitamin D intake.
- Symptoms include bone pain, abdominal pain, constipation, polyuria, nausea, vomiting, and confusion.
- Severe hypercalcemia can cause renal stones, muscle weakness, and cardiac rhythm disturbances.
7. Hypomagnesemia (Serum Magnesium < 1.5 mEq/L)
- Hypomagnesemia results from alcoholism, chronic diarrhea, poor nutrition, or diuretic therapy.
- Symptoms include muscle tremors, hyperreflexia, irritability, confusion, and in severe cases, seizures and cardiac arrhythmias.
- ECG may show prolonged QT interval or Torsades de Pointes.
8. Hypermagnesemia (Serum Magnesium > 2.5 mEq/L)
- Hypermagnesemia typically occurs in renal failure patients or due to excessive use of magnesium-containing medications like antacids and laxatives.
- Symptoms include flushing, hypotension, lethargy, bradycardia, diminished deep tendon reflexes, and respiratory depression.
- Very high levels can result in coma and cardiac arrest.
Causes of Electrolyte Imbalance
- Excessive fluid loss (vomiting, diarrhea, sweating)
- Renal failure or dialysis
- Hormonal disorders (ADH, aldosterone dysfunction)
- Inappropriate IV fluid therapy
- Medications (diuretics, corticosteroids, chemotherapy)
- Inadequate dietary intake or malabsorption
- Burns and trauma
Diagnostic Evaluation
- History collection
- Physical examination
- Serum electrolyte levels (Na⁺, K⁺, Ca²⁺, etc.)
- ECG (to detect arrhythmias)
- Renal function tests (creatinine, BUN)
- Arterial blood gas (ABG) for acid-base balance
- Urine electrolytes and osmolality
Medical Management
- Replace or restrict specific electrolytes (oral or IV) based on lab reports.
- Treat underlying cause (renal failure, vomiting, endocrine disorder).
- Monitor cardiac activity closely, especially in potassium and calcium disturbances.
- Use electrolyte binders or diuretics if needed (e.g., Kayexalate for hyperkalemia).
- Fluid management and monitoring to avoid overload or dehydration.
Nursing Management of Electrolyte Imbalance
- The nurse should assess the patient’s level of consciousness, muscle strength, cardiac rhythm, and fluid status frequently.
- Nurses must monitor serum electrolyte values and ECG in patients at risk, especially those on diuretics or IV fluids.
- Administer electrolyte replacements (oral or IV) as prescribed, such as potassium chloride, calcium gluconate, or magnesium sulfate.
- Educate the patient on dietary sources of deficient electrolytes, e.g., banana for potassium, milk for calcium.
- Maintain accurate intake/output charting, daily weight, and monitor for fluid retention or dehydration.
- Avoid rapid correction, particularly in sodium imbalances, to prevent complications like central pontine myelinolysis.
- Collaborate with the health team to adjust fluid therapy, medication, and diet based on lab values.
- Prepare for emergency interventions such as insulin-glucose infusion for hyperkalemia or dialysis in renal failure cases.
4. Assessment of nutritional status
- Assessment of nutritional status refers to the systematic evaluation of an individual’s dietary intake, physical measurements, clinical signs, and biochemical data to determine whether their nutritional needs are being adequately met.
- This process helps in identifying malnutrition, obesity, micronutrient deficiencies, or specific nutritional risks, and is crucial for planning appropriate dietary, medical, and nursing interventions.
1️⃣ Anthropometric Measurements
- Anthropometry involves measuring the physical dimensions and composition of the human body to evaluate nutritional status.
- Common parameters include weight, height, Body Mass Index (BMI), mid-upper arm circumference (MUAC), skinfold thickness, and waist-hip ratio.
- BMI is calculated by dividing weight in kilograms by the square of height in meters (kg/m²) and used to classify individuals as underweight, normal weight, overweight, or obese.
- MUAC is especially useful in children and pregnant women to detect undernutrition or fat and muscle wasting.
- Regular tracking of these measurements helps in monitoring growth trends, obesity risk, and wasting conditions.
2️⃣ Dietary Assessment
- Dietary assessment refers to evaluating an individual’s food intake pattern, frequency, quantity, and quality of consumed nutrients.
- Methods include 24-hour dietary recall, food frequency questionnaire (FFQ), food diary, and direct observation.
- This helps to detect inadequate, excessive, or imbalanced consumption of calories, protein, vitamins, and minerals.
- Dietary history should consider meal patterns, food allergies, economic condition, cultural preferences, and feeding difficulties.
- In hospital settings, nutritional charting can help monitor patient intake compared to daily requirements.
3️⃣ Biochemical Assessment
- Biochemical analysis involves laboratory tests that measure nutrient levels and markers in blood, urine, or other body fluids.
- Common indicators include hemoglobin (for anemia), serum albumin (for protein status), blood glucose (for carbohydrate metabolism), lipid profile, vitamin D, calcium, and iron levels.
- These values help in detecting hidden deficiencies (like subclinical anemia), metabolic imbalances, or organ dysfunctions related to nutrition.
- Repeated testing is essential in critically ill, elderly, or chronically malnourished patients to monitor response to nutritional therapy.
4️⃣ Clinical Examination
- Clinical assessment focuses on physical signs and symptoms that may indicate nutritional deficiencies or imbalances.
- Nurses and clinicians look for pallor (anemia), dry skin (vitamin A or E deficiency), glossitis (B-complex deficiency), edema (protein deficiency), hair thinning, and poor wound healing.
- Examination of skin, eyes, mouth, nails, muscle mass, and general appearance offers important clues about overall nutritional health.
- This step is especially vital in patients with chronic diseases, infections, post-surgery conditions, or eating disorders.
5️⃣ Functional Assessment
- Functional assessment evaluates how nutrition impacts physical performance and activity level.
- Handgrip strength, walking speed, and ability to perform daily activities are used to assess muscle strength and functional decline due to malnutrition.
- In older adults, frailty tests and fall risk assessments are linked to nutritional depletion, especially in cases of protein-energy malnutrition.
6️⃣ Socioeconomic and Lifestyle Assessment
- This includes evaluating economic condition, education level, food access, occupation, living conditions, and cultural practices that influence nutrition.
- Emotional and mental health status also plays a role, as depression, stress, or isolation can affect appetite and food choices.
- Assessment of alcohol intake, smoking habits, physical activity, and medication use is also relevant in determining nutritional health.
7️⃣ Special Group Considerations
- Nutritional assessment varies by age group, gender, physiological state, and medical condition.
- Infants, children, pregnant and lactating women, elderly individuals, and patients with chronic diseases need age- and condition-specific tools.
- Growth charts, WHO Z-scores, and BMI-for-age are used for pediatric evaluation, while nutritional risk screening tools are used for hospitalized or geriatric patients.
Nursing Responsibilities in Nutritional Assessment
- Record accurate anthropometric data and monitor for changes over time.
- Observe and document clinical signs of nutritional deficiencies.
- Assist in collecting blood samples for biochemical analysis and interpreting lab reports.
- Conduct dietary recall or food frequency questionnaires during patient interviews.
- Educate patients and families about balanced diet, food safety, and meal planning.
- Collaborate with dietitians to develop individualized nutrition care plans.
- Identify high-risk patients early and initiate timely interventions to prevent complications.
Q.3 Write dietary sources of following (any three) (3×2=6)
1. Vitamin B
1️⃣ Whole grains (wheat, rice, oats)
2️⃣ Meat, liver, eggs, fish, and poultry
3️⃣ Milk and dairy products
4️⃣ Green leafy vegetables (spinach, broccoli)
5️⃣ Legumes (peas, beans, lentils)
6️⃣ Nuts and seeds
2. Calcium
1️⃣ Milk and dairy products – such as milk, cheese, paneer, and curd
2️⃣ Green leafy vegetables – like spinach, kale, fenugreek, and broccoli
3️⃣ Ragi (finger millet) – one of the richest plant sources of calcium
4️⃣ Soy products – including tofu and soy milk
5️⃣ Nuts and seeds – especially almonds and sesame seeds
6️⃣ Fish with bones – such as sardines and salmon
7️⃣ Fortified foods – like calcium-fortified cereals, juices, and breads
3. Carbohydrates
1️⃣ Cereals and grains – such as rice, wheat, maize, and cornflakes
2️⃣ Starchy vegetables – like potatoes, sweet potatoes, and yam
3️⃣ Fruits – such as bananas, mangoes, apples, and grapes
4️⃣ Legumes and pulses – including lentils, chickpeas, and beans
5️⃣ Milk and milk products – which contain lactose (a natural sugar)
6️⃣ Sugary foods – like jaggery, honey, sugar, and sweets
7️⃣ Bakery products – including bread, biscuits, and cakes
4. Vitamin A
1️⃣ Liver and fish liver oils – like cod liver oil (richest source)
2️⃣ Milk and dairy products – such as milk, butter, ghee, and cheese
3️⃣ Egg yolk – provides preformed vitamin A (retinol)
4️⃣ Green leafy vegetables – spinach, amaranth, coriander leaves
5️⃣ Yellow-orange fruits and vegetables – like carrots, mangoes, papaya, pumpkin, and sweet potato (contain beta-carotene)
6️⃣ Fortified foods – like vitamin A-fortified milk and margarine
Q.4
a. Explain principles of cookery (4)
- Cookery refers to the science and art of preparing food using various methods such as boiling, roasting, baking, steaming, and frying to make it palatable, safe, and digestible.
- The principles of cookery involve understanding how heat affects the physical and chemical properties of food, in order to enhance taste, texture, nutrition, and safety.
- Proper cooking techniques are essential in hospitals, homes, and community nutrition settings to ensure nutritional adequacy and patient recovery.
1️⃣ Principle of Applying Heat
- Cooking involves the application of heat to food, which changes its structure, texture, and flavor, making it more enjoyable and safer to eat.
- Heat can be transferred by three main methods: conduction (direct heat transfer), convection (through air or liquid), and radiation (infrared or microwave rays).
- Cooking also kills pathogenic microorganisms and deactivates natural toxins or anti-nutrients in certain raw foods.
2️⃣ Principle of Temperature Control
- Different foods require different temperatures for optimal cooking, as overheating can lead to nutrient loss, burning, or undesirable texture.
- Gentle heat is used for simmering, poaching, and steaming, while high heat is applied for roasting, frying, or grilling to create a crisp texture and rich flavor.
- Sudden or uneven temperature changes can toughen proteins, curdle milk, or cause uneven cooking.
3️⃣ Principle of Protein Coagulation
- Proteins in foods such as meat, eggs, milk, and legumes undergo coagulation when heated, which results in a change from a soft to firm texture.
- Overheating may make proteins tough and rubbery, while undercooking may leave them unsafe or indigestible.
- Understanding this principle is essential in preparing dishes like boiled eggs, curdled sauces, or custards.
4️⃣ Principle of Gelatinization of Starch
- Starch-rich foods like rice, wheat, and potatoes absorb water when heated and swell, leading to gelatinization, which softens the food and improves digestion.
- Inadequate heat or insufficient water can result in under-gelatinized, hard, or lumpy food textures.
- This principle is important in cooking cereals, making puddings, thickening sauces, or baking bread.
5️⃣ Principle of Maillard Reaction and Caramelization
- The Maillard reaction occurs when amino acids and sugars react under high heat, producing brown color and complex flavors, especially in roasted or grilled meat and baked items.
- Caramelization refers to the browning of sugars when heated, creating a sweet, nutty aroma, common in desserts, caramel sauces, and roasted vegetables.
- These reactions enhance flavor and appearance but should be controlled to avoid burning or acrid taste.
6️⃣ Principle of Flavor and Seasoning
- Cooking brings out the natural flavor of ingredients, and seasonings such as salt, herbs, and spices enhance the taste and aroma of dishes.
- Proper seasoning balances the overall dish and improves appetite and satisfaction, especially in therapeutic diets.
- Over-seasoning or under-seasoning can make food unpalatable or inappropriate for clinical diets.
7️⃣ Principle of Retaining Nutrients
- Cooking should aim to preserve the maximum nutritional value of food, especially vitamins and minerals that are heat-sensitive.
- Methods such as steaming, sautéing, or pressure cooking are better at retaining nutrients compared to boiling or deep frying.
- Avoiding overcooking, excessive washing, or prolonged soaking helps prevent nutrient loss, particularly vitamin C and B-complex vitamins.
8️⃣ Principle of Proper Cooking Methods
- Choosing the correct cooking method is essential based on the type of food, desired texture, and health considerations.
- Methods such as boiling, steaming, grilling, roasting, baking, frying, and pressure cooking serve different purposes in achieving safety, palatability, and nutrient retention.
- In therapeutic or hospital diets, steaming and boiling are preferred, while frying is avoided due to its high fat content.
b. Write prevention of food adulteration act (4)
Introduction and Purpose of the Act
- The Prevention of Food Adulteration Act (PFA) was passed by the Parliament of India in 1954, with the main objective to protect consumers from health hazards caused by adulterated, contaminated, or misbranded food products.
- This act was a landmark legislation to ensure that the food consumed by the public is pure, safe, and wholesome, and to safeguard the population against foodborne diseases and toxic ingredients.
Scope and Application of the PFA Act
- The PFA Act applied to all food products manufactured, distributed, sold, or stored for sale in India, including those in markets, retail stores, restaurants, and public distribution systems.
- It covered every individual or company involved in food processing, transport, storage, marketing, and vending, thereby ensuring accountability across the entire food supply chain.
Definition of Adulterated Food Under the Act
- According to the Act, a food article is considered adulterated if it contains harmful substances, is substituted with inferior materials, is prepared in unhygienic conditions, or fails to meet the prescribed standards of quality, purity, and safety.
- The Act also classifies food as adulterated if it is misbranded, damaged, spoiled, or rendered injurious to health due to intentional or accidental contamination.
Key Provisions of the PFA Act
- The Act authorized the appointment of Food Inspectors and Public Analysts who are empowered to inspect food premises, collect food samples, and send them to certified laboratories for testing.
- The Act made it mandatory for food products to be properly labeled, packed, and stored, and prohibited the sale of food that is contaminated or does not meet the required standards.
- Any person found guilty of manufacturing, selling, or distributing adulterated food could be subjected to penalty, imprisonment, or both, depending on the severity of the violation.
Penalties and Punishments
- The Act prescribed strict penalties ranging from monetary fines to imprisonment up to 6 years, especially if the adulterated food caused injury or death.
- In cases of repeat offences or where adulteration results in serious health consequences, the punishment could include cancellation of business licenses, product seizure, and legal prosecution.
Repeal and Transition to FSSA, 2006
- Over time, with advancements in food safety technology and increasing complexity of food trade, the PFA Act was found to be outdated and fragmented.
- Hence, the Act was repealed in 2006, and replaced by the more comprehensive Food Safety and Standards Act (FSSA), 2006, which merged all previous food-related laws under a single regulatory authority known as the Food Safety and Standards Authority of India (FSSAI).
Importance of PFA Act in Nursing and Public Health
- The PFA Act played a major role in reducing the incidence of food adulteration-related diseases, improving public awareness about food safety, and promoting sanitation in food handling practices.
- For nurses and community health professionals, knowledge of food safety laws helps them to educate families, identify food-related illness outbreaks, and work with health authorities in enforcing food hygiene practices.
c. Explain method of cooking (8)
Introduction
- Cooking is defined as the process by which raw food is transformed into edible, palatable, digestible, and safe forms through the application of heat, moisture, or mechanical techniques.
- The primary aim of cooking is not only to make food appealing and improve taste but also to destroy harmful microorganisms, toxins, and anti-nutrients that may cause illness.
- Each method of cooking has a unique effect on the nutrient content, texture, flavor, appearance, and digestibility of food.
- Nurses must have knowledge of these methods to assist in therapeutic diet planning, especially for patients with specific dietary needs.
1️⃣ Moist Heat Methods
(These methods involve the use of water, steam, or other liquids to cook food)
✅ A. Boiling
- Boiling is a method in which food is completely submerged in water heated to 100°C and cooked until soft or tender.
- It is widely used for cooking vegetables, cereals (like rice), pulses, pasta, and eggs in both household and hospital kitchens.
- Boiling helps in destroying pathogens and making food safe, especially in the case of contaminated water or raw vegetables.
- However, excessive boiling can result in leaching of water-soluble nutrients, especially vitamin C, B1, B2, and some minerals.
- In hospitals, boiled rice, dal, and vegetables are common in light or bland diets, especially in fever or gastrointestinal disorders.
- Reuse of the leftover water as broth or soup can help recover lost nutrients.
✅ B. Simmering
- Simmering involves cooking food in water kept just below boiling point (around 85–95°C), which produces small bubbles rather than vigorous boiling.
- This gentle method is ideal for preparing soups, dals, porridge, milk dishes, and stews, where over-agitation could spoil the texture.
- Simmering helps in flavor blending, especially when ingredients like spices, herbs, and slow-cooking meats are added.
- It reduces nutrient destruction and is preferred when delicate proteins or dairy products are part of the dish.
- Steady simmering is also used for convalescent patients who require soft, easy-to-digest, and warm meals.
✅ C. Steaming
- Steaming is a cooking method where food is exposed to steam from boiling water, without coming into direct contact with it.
- This method is commonly used for idli, dhokla, fish, vegetables, and momos, and it is considered one of the healthiest methods.
- Steaming preserves vitamins (especially B-complex and C), minerals, color, texture, and flavor of food better than boiling or frying.
- It also requires no oil, making it ideal for cardiac, diabetic, hypertensive, and obese patients.
- Steam-cooked food is easier to digest and soft in texture, making it suitable for infants, elderly, or post-surgical patients.
- Equipment like idli steamers, pressure steamers, and bamboo baskets are used depending on the food item.
✅ D. Poaching
- Poaching involves cooking food in hot liquid (60–80°C), keeping the temperature low to avoid damage to fragile foods.
- This method is ideal for eggs, fish, fruits, or chicken breasts, where maintaining the original structure and delicacy of the food is important.
- The liquid used can be water, milk, broth, or stock, depending on nutritional needs and flavor profile.
- Poached food retains moisture, softness, and light flavor, making it perfect for ulcer, liver disease, or gastritis diets.
- Since no browning occurs, it is preferred in dishes where color preservation is important.
✅ E. Pressure Cooking
- Pressure cooking uses a sealed container (pressure cooker) where steam builds up pressure, raising the boiling point of water above 100°C, leading to faster cooking.
- Used widely for pulses, meats, rice, potatoes, and lentils, pressure cooking saves time, fuel, and preserves nutrients due to reduced cooking time.
- Overcooking can occur if pressure is not released properly, affecting taste and nutrient value.
- It is extensively used in hospital kitchens for preparing soft food in bulk, ensuring hygiene and ease of digestion.
- Protein and carbohydrate digestibility improves due to high temperature and moisture, making it suitable for therapeutic diets.
2️⃣ Dry Heat Methods
(These methods involve cooking food without any added water or liquid)
✅ A. Roasting
- Roasting refers to cooking food using dry heat, either in an oven or over an open flame or heated pan.
- Used for nuts, potatoes, brinjal, papad, and meat, roasting enhances flavor through browning reactions like the Maillard reaction.
- It helps reduce moisture content, making food crispy, light, and easier to store.
- Roasting is often used as a preliminary step before grinding spices or grains, increasing shelf life and aroma.
- Minimal oil is used, making it suitable for low-fat diets.
✅ B. Baking
- Baking is a method of cooking food using dry heat in a closed oven, where heat circulates evenly from all directions.
- Commonly used for bread, cakes, biscuits, pies, pastries, and lasagna, it is ideal for producing uniform texture and golden crusts.
- Baking helps avoid nutrient loss that occurs in boiling or frying, making it better for protein-based and starchy foods.
- Correct control of temperature and time is essential to avoid undercooked or burnt products.
- In therapeutic diets, baked items like vegetable casserole or protein-rich muffins can be customized for patient needs.
✅ C. Grilling / Broiling
- Grilling (heat from below) and broiling (heat from above) involve exposing food to direct heat or flame, allowing fats to drip away.
- Commonly used for meat, paneer, vegetables, and burgers, grilling provides a charred texture and smoky aroma.
- It enhances protein flavor without using oil, making it suitable for low-fat or high-protein diets.
- However, improper grilling can lead to burnt food, which may contain carcinogenic substances (e.g., benzopyrene).
- Grilled food is popular in hospital and community diets where crispy texture with minimal oil is desired.
✅ D. Toasting
- Toasting involves browning and crisping food by direct exposure to dry heat using a toaster, pan, or oven.
- Commonly used for bread slices, rava (semolina), nuts, or seeds, toasting enhances flavor, reduces moisture, and makes food crunchy.
- Toasted food is light, low-fat, and easy to digest, often included in fever diets, post-operative diets, or soft-solid diets.
- Over-toasting can lead to hardness or burning, especially in carbohydrate-rich items.
3️⃣ Frying Methods
(Food is cooked in heated oil or fat)
✅ A. Shallow Frying
- Shallow frying uses a small amount of oil in a pan, and food is flipped to cook on both sides until golden brown.
- Used for cutlets, omelets, tikkis, dosas, and vegetable patties, it enhances flavor and mouthfeel.
- Compared to deep frying, it uses less oil, making it marginally healthier.
- Food must be drained on absorbent paper to remove excess oil.
- Excessive reuse of oil or prolonged frying at high temperature can lead to trans fat formation.
✅ B. Deep Frying
- Deep frying submerges food completely in hot oil (around 180°C), resulting in crispy exterior and soft interior.
- Used for samosas, puris, pakoras, chips, and festive items.
- Greatly increases caloric and fat content, hence not suitable for patients with obesity, heart disease, or diabetes.
- Repeated oil use may form free radicals and oxidized fats, which are harmful.
- Deep-fried food is more palatable, but should be limited in therapeutic and general diets.
✅ C. Stir Frying
- Stir frying uses minimal oil and high heat, with constant movement of food in a wok or shallow pan.
- Common in Chinese-style cooking, ideal for vegetables, lean meats, tofu, or noodles.
- Retains color, crunchiness, and nutrients due to short cooking time.
- Requires quick preparation and cutting of food into uniform sizes.
- A preferred method for making low-calorie, high-nutrient meals for weight-conscious or diabetic individuals.
4️⃣ Combination Methods
(Involve both dry and moist heat techniques)
✅ A. Braising
- Braising starts with searing food in oil, followed by slow cooking in a covered pot with minimal liquid.
- Common for tough cuts of meat, chicken, and root vegetables, making them tender and flavorful.
- This method allows complex flavor development and nutrient retention.
- Cooking time is longer, but suitable for high-protein diets where digestibility is important.
✅ B. Stewing
- Stewing involves cooking small food pieces fully submerged in liquid at low heat over a long time.
- Used for meat, lentils, mixed vegetable dishes, and soups, it is gentle and nutritious.
- The liquid is not discarded, preserving vitamins and minerals.
- Ideal for complete one-pot meals where ingredients blend well and provide easy digestion and maximum nutrition.
Section 2
Q.5 Briefly answer following (any four) (4×2=8)
1. Biochemical role of vitamin A
1️⃣ Vitamin A plays a vital role in the synthesis of rhodopsin, which is a visual pigment essential for vision in dim light, especially helping in night vision.
2️⃣ Vitamin A is actively involved in the maintenance of healthy epithelial tissues, such as those in the skin, respiratory tract, gastrointestinal lining, and urinary tract, by supporting cell growth and differentiation.
3️⃣ It functions as an antioxidant, thereby protecting cells from oxidative damage caused by free radicals, contributing to immune defense and skin health.
4️⃣ Vitamin A regulates gene expression and immune responses, as retinoic acid (its active form) acts like a hormone influencing DNA transcription related to cell growth and immune function.
5️⃣ It is essential in embryonic development and reproduction, as it plays a role in morphogenesis, organ development, and fetal growth.
2. Biochemical function of zinc
1️⃣ Zinc acts as a crucial cofactor for over 300 enzymes, which are involved in important biochemical processes such as protein synthesis, DNA synthesis, and cell division, thereby maintaining cellular and metabolic functions.
2️⃣ Zinc plays an essential role in immune system regulation, by supporting the activity of immune cells like T-lymphocytes and neutrophils, enhancing wound healing and defense against infections.
3️⃣ Zinc is involved in antioxidant defense, by stabilizing cell membranes and contributing to the function of antioxidant enzymes such as superoxide dismutase, which protect cells from oxidative stress.
4️⃣ Zinc is vital for the synthesis and action of insulin, and it helps in maintaining normal glucose metabolism and pancreatic function.
3. Factor affecting iron absorption
1️⃣ Iron absorption is enhanced by the presence of vitamin C (ascorbic acid), because it helps in reducing ferric (Fe³⁺) iron to the more absorbable ferrous (Fe²⁺) form and promotes its solubility in the intestinal lumen.
2️⃣ Iron absorption is better when iron is consumed in the heme form (from animal sources like meat, liver, fish), as heme iron is more efficiently absorbed compared to non-heme iron found in plant-based sources.
3️⃣ Phytates (found in cereals and legumes), oxalates (in spinach and tea), and calcium inhibit iron absorption, because they bind to iron in the gastrointestinal tract and form insoluble complexes that reduce its bioavailability.
4️⃣ Gastric acid plays an important role in enhancing iron absorption, as it maintains the solubility of iron and aids its conversion to the absorbable ferrous form in the stomach.
4. Function of essential fatty acid
1️⃣ Essential fatty acids play a vital role in the formation and maintenance of cell membranes, especially phospholipid bilayers, thereby ensuring cellular integrity, fluidity, and proper functioning of tissues and organs.
2️⃣ They are crucial precursors for the synthesis of eicosanoids such as prostaglandins, thromboxanes, and leukotrienes, which regulate physiological processes like inflammation, blood pressure, immune response, and blood clotting.
3️⃣ Essential fatty acids help in brain development and function, especially omega-3 fatty acids like DHA (docosahexaenoic acid), which are important for neural growth and visual development in infants.
4️⃣ They assist in the transport and metabolism of cholesterol and fat-soluble vitamins (A, D, E, K), thereby supporting cardiovascular health and nutrient absorption.
5. Define glycoysis
- Glycolysis is a metabolic pathway in which one molecule of glucose (a six-carbon sugar) is broken down enzymatically in the cytoplasm of the cell into two molecules of pyruvic acid (a three-carbon compound), along with the production of a small amount of energy in the form of ATP (Adenosine Triphosphate) and NADH (Nicotinamide Adenine Dinucleotide – reduced form).
- It is an anaerobic process (does not require oxygen) and serves as the first step in both aerobic and anaerobic respiration.
Q.6 Write short notes any two (2×5=10)
1. Significance of biochemistry in nursing
- Biochemistry is the branch of science that studies the chemical composition, molecular structure, and biochemical processes occurring in living organisms.
- In nursing, biochemistry plays a foundational role in understanding how the human body functions at the cellular and molecular levels, especially in relation to health, disease, nutrition, and drug metabolism.
- A sound knowledge of biochemistry allows nurses to interpret diagnostic reports, monitor clinical conditions, and participate effectively in patient care and health education.
1️⃣ Understanding Normal Body Function
- Biochemistry helps nurses understand how carbohydrates, proteins, lipids, nucleic acids, and enzymes function in maintaining normal body physiology.
- Nurses learn how metabolic pathways like glycolysis, Krebs cycle, and protein synthesis operate under normal and abnormal conditions.
- This understanding enables nurses to correlate clinical signs and symptoms with biochemical imbalances, such as in fever, fatigue, or poor wound healing.
2️⃣ Interpreting Laboratory Reports
- Nurses frequently encounter biochemical test reports such as blood glucose, serum electrolytes, liver function tests, renal function tests, lipid profile, and ABG (arterial blood gas) values.
- Knowledge of biochemistry helps in understanding these reports and identifying abnormal values indicating disease progression or organ dysfunction.
3️⃣ Role in Nutrition and Diet Therapy
- Biochemistry explains how macronutrients (carbohydrates, proteins, fats) and micronutrients (vitamins and minerals) are digested, absorbed, and utilized by the body.
- Nurses use this knowledge to plan therapeutic diets for patients with diabetes, hypertension, kidney disease, or malnutrition.
- Biochemical principles also guide nurses in nutritional assessment, fluid and electrolyte balance, and vitamin supplementation.
4️⃣ Understanding Disease Mechanisms
- Biochemistry is essential for understanding the pathophysiology of diseases like diabetes mellitus, liver cirrhosis, renal failure, metabolic acidosis, and electrolyte imbalances.
- Nurses apply biochemical knowledge to identify early warning signs of deterioration, such as ketone bodies in DKA or elevated creatinine in renal disease.
- Biochemical concepts are used to understand tumor markers, hormone assays, and enzyme deficiencies in various conditions.
5️⃣ Drug Action and Detoxification
- Biochemistry explains how drugs are metabolized by the liver, distributed in the body, and excreted through the kidneys.
- Nurses monitor drug interactions, adverse reactions, and the biochemical basis of pharmacokinetics and pharmacodynamics.
- Understanding detoxification pathways helps nurses in managing poisoning cases, antidote administration, and safe drug use in hepatic or renal impairment.
6️⃣ Fluid and Electrolyte Balance
- Biochemical knowledge is vital in maintaining acid–base balance, and sodium, potassium, calcium, chloride, and bicarbonate levels in patients.
- Nurses assess signs of dehydration, edema, or fluid overload, and intervene using IV fluids or electrolyte replacements.
- Biochemistry helps in interpreting ABG analysis, guiding the management of respiratory or metabolic acidosis and alkalosis.
7️⃣ Role in Clinical Procedures and Diagnosis
- Biochemistry underpins procedures like blood transfusion (ABO grouping), urinalysis, glucometer use, and rapid diagnostic kits.
- Nurses collect samples properly, prevent contamination, and understand the significance of biochemical markers in detecting infections, inflammation, or organ failure.
- Biochemistry also aids in understanding hormone levels (like insulin, T3, T4, cortisol) and how they affect patient health.
8️⃣ Education and Health Promotion
- Nurses use biochemical principles to educate patients and families about healthy diets, diabetes care, hydration, and avoiding toxin exposure.
- Biochemistry supports public health nursing in explaining conditions like iron-deficiency anemia, iodine deficiency, or vitamin D deficiency.
- Nurses also use biochemical reasoning in counseling on breastfeeding, complementary feeding, and dietary changes in chronic diseases.
2. Structure of cell membrane
Definition of Cell Membrane
- The cell membrane, also called the plasma membrane, is a thin, flexible, semi-permeable boundary that surrounds the cytoplasm of all living cells, providing both structural support and regulation of substance exchange between the internal cell environment and the external surroundings.
- It plays a critical role in protecting cellular contents, facilitating communication, and controlling the movement of ions, nutrients, and waste products.
Basic Composition of the Cell Membrane
- The cell membrane is mainly composed of lipids, proteins, and carbohydrates, with water also forming part of its environment.
- The average membrane consists of approximately 40% lipids, 50% proteins, and 10% carbohydrates by mass.
Fluid Mosaic Model (Proposed by Singer and Nicolson, 1972)
- According to the Fluid Mosaic Model, the cell membrane is structured like a “mosaic” of various molecules that float in a fluid lipid bilayer.
- The lipid molecules provide a flexible, dynamic foundation, and the proteins are embedded like tiles or float like icebergs within the lipid sea.
- This model emphasizes that the membrane is not rigid but fluid, flexible, and constantly changing.
Phospholipid Bilayer
- The foundation of the membrane is formed by a bilayer of phospholipids, which are amphipathic molecules containing hydrophilic (water-attracting) heads and hydrophobic (water-repelling) tails.
- In aqueous environments, these phospholipids arrange themselves into two layers, where the hydrophobic tails face inward, away from water, and the hydrophilic heads face outward toward the water inside and outside the cell.
- This bilayer forms a semi-permeable barrier that allows selective transport of substances.
Membrane Proteins
Proteins are embedded within or attached to the lipid bilayer and serve various functional roles.
✅ A. Integral Proteins (Intrinsic)
- These proteins are embedded within the phospholipid bilayer and may span the membrane completely.
- They function as channels, transporters, or receptors to move substances across the membrane or transmit signals.
✅ B. Peripheral Proteins (Extrinsic)
- These proteins are loosely attached to the surface of the membrane or to integral proteins.
- They are involved in cell signaling, structural support, and interactions with the cytoskeleton.
Carbohydrates
- Carbohydrate molecules are present on the external surface of the membrane, often attached to proteins (forming glycoproteins) or lipids (forming glycolipids).
- These carbohydrates form a coating called the glycocalyx, which functions in cell recognition, immune response, and protection against mechanical and chemical injury.
Cholesterol
- Cholesterol molecules are interspersed between the phospholipids in animal cells and help to regulate membrane fluidity and stability.
- At high temperatures, cholesterol reduces membrane fluidity, and at low temperatures, it prevents the membrane from becoming too rigid.
Functions of the Cell Membrane (Structural and Functional)
- It serves as a selective barrier, regulating the entry and exit of ions, nutrients, and waste materials.
- It maintains cell shape and internal environment (homeostasis).
- It facilitates cell communication and signaling through receptor proteins.
- It is involved in endocytosis (entry) and exocytosis (exit) of macromolecules.
- It anchors the cytoskeleton and connects with the extracellular matrix for support and cell interaction.
- It plays a role in immune recognition and tissue differentiation via surface antigens.
3. Buffer of the body fluid
- Buffers are chemical systems present in the body fluids that resist sudden changes in pH by neutralizing excess hydrogen ions (H⁺) or hydroxyl ions (OH⁻).
- These buffer systems are vital in maintaining the acid–base balance of blood and other fluids within a narrow pH range of 7.35 to 7.45, which is essential for the normal functioning of enzymes, cells, and organs.
- In nursing, understanding buffers helps in managing patients with acidosis, alkalosis, renal failure, and respiratory disorders where pH regulation is impaired.
Types of Buffer Systems in the Human Body
1️⃣ Bicarbonate Buffer System (HCO₃⁻ / H₂CO₃)
- This is the most important and abundant buffer system in the extracellular fluid (especially in blood plasma).
- It consists of sodium bicarbonate (NaHCO₃) as the base and carbonic acid (H₂CO₃) as the weak acid.
- When there is excess acid (H⁺) in the body, bicarbonate neutralizes it to form carbonic acid, which is then broken down into water and carbon dioxide, and the CO₂ is exhaled through the lungs.
- When there is excess base (OH⁻), carbonic acid donates hydrogen ions to neutralize it, forming water and bicarbonate.
- This system works closely with the respiratory system (lungs) and renal system (kidneys) to regulate blood pH.
- It plays a key role in managing respiratory acidosis, alkalosis, and metabolic disturbances.
2️⃣ Phosphate Buffer System (HPO₄²⁻ / H₂PO₄⁻)
- This buffer system operates primarily in the intracellular fluid and also in renal tubular fluid (especially in the kidneys).
- It includes monohydrogen phosphate (HPO₄²⁻) which acts as a weak base and dihydrogen phosphate (H₂PO₄⁻) which acts as a weak acid.
- In conditions of acidosis, HPO₄²⁻ neutralizes excess H⁺ ions, and in alkalosis, H₂PO₄⁻ neutralizes OH⁻ ions, helping to stabilize intracellular pH.
- The phosphate buffer is especially important in urine pH regulation and plays a vital role in excreting hydrogen ions by the kidney.
- It also contributes to bone buffering by exchanging phosphate ions with the blood in chronic acid-base disorders.
3️⃣ Protein Buffer System (e.g., Hemoglobin, Albumin)
- This is the most powerful buffer system in the body, mainly found in intracellular fluid and also contributes in plasma.
- Proteins contain amino acid side chains that can accept or donate hydrogen ions, depending on the pH of the surrounding fluid.
- Hemoglobin (Hb), found inside red blood cells, acts as an effective buffer by binding to hydrogen ions and releasing oxygen, especially under acidic conditions.
- Plasma proteins like albumin help buffer the blood by attracting hydrogen ions, especially during metabolic acidosis or alkalosis.
- This system helps maintain intracellular pH stability and also supports oxygen transport and pH buffering in tissues.
4️⃣ Respiratory Buffer System
- Although not a chemical buffer, the respiratory system acts as a physiological buffer by regulating carbon dioxide (CO₂) levels in the blood.
- CO₂ combines with water in the blood to form carbonic acid (H₂CO₃); when CO₂ is exhaled, it reduces acid load, thereby increasing blood pH.
- In conditions like metabolic acidosis, the respiratory rate increases (Kussmaul respiration) to eliminate more CO₂, thus compensating for acidosis.
- This system acts within minutes, making it a quick-response buffer during acute acid-base imbalances.
5️⃣ Renal (Kidney) Buffer System
- The renal system plays a long-term role in acid–base balance by excreting hydrogen ions (H⁺) and reabsorbing bicarbonate ions (HCO₃⁻).
- The kidneys produce new bicarbonate, reabsorb filtered bicarbonate, and eliminate non-volatile acids like lactic acid, ketone bodies, and sulfuric acid.
- In chronic acidosis, kidneys increase H⁺ secretion and HCO₃⁻ retention, helping maintain blood pH over days.
- The renal buffer system is slow-acting but powerful, and crucial in managing chronic metabolic conditions such as renal failure and diabetic ketoacidosis.
Q.7 Describe following (any two) (2×6=12)
1. Regulation of blood glucose level
- The regulation of blood glucose level is a critical physiological process that ensures the availability of glucose—the body’s primary energy source—especially for vital organs like the brain, heart, and red blood cells, which rely almost exclusively on glucose for fuel.
- This regulation keeps the blood glucose level stable, typically within the normal fasting range of 70–110 mg/dL, despite continuous changes due to food intake, fasting, exercise, stress, or illness.
- The process involves endocrine feedback loops, primarily through hormones released by the pancreas, as well as contributions from the liver, muscle tissues, adrenal glands, and other hormonal systems.
1️⃣ Role of Pancreas in Glucose Regulation
- The pancreas, particularly the islets of Langerhans, contains specialized endocrine cells: β (beta) cells that secrete insulin, and α (alpha) cells that secrete glucagon, both of which work antagonistically to maintain glucose balance.
- Insulin is released in response to elevated blood glucose levels, such as after food intake, and promotes glucose uptake into cells, while glucagon is released during low blood glucose, such as during fasting, and acts to increase blood glucose levels.
- The coordinated actions of insulin and glucagon are crucial in maintaining homeostasis and preventing metabolic disturbances like hypoglycemia or hyperglycemia.
2️⃣ Mechanism of Insulin Action (Glucose-Lowering Hormone)
- Insulin, a peptide hormone, binds to insulin receptors on muscle and adipose tissues, stimulating the insertion of GLUT-4 transporters into the cell membrane, which facilitates active uptake of glucose from the blood into the cells.
- Inside the cells, insulin promotes glycogenesis, which is the conversion of excess glucose into glycogen, primarily in the liver and skeletal muscles, for energy storage.
- Insulin also promotes lipogenesis (conversion of glucose into fatty acids), enhances protein synthesis, and inhibits lipolysis (fat breakdown) and proteolysis (protein breakdown), helping in anabolic body processes.
- Insulin suppresses hepatic glucose production (gluconeogenesis), thereby preventing further release of glucose into circulation.
- This hormone is crucial for maintaining postprandial glucose control, preventing dangerous spikes in blood sugar levels.
3️⃣ Mechanism of Glucagon Action (Glucose-Raising Hormone)
- Glucagon is released when blood glucose drops, typically during prolonged fasting, intense exercise, or insulin overdose.
- It acts mainly on hepatocytes (liver cells) to promote glycogenolysis—the breakdown of stored glycogen into glucose—and gluconeogenesis—the production of glucose from non-carbohydrate sources like amino acids and lactate.
- Glucagon also reduces glycogenesis and promotes the release of free glucose into the bloodstream, thus counteracting insulin.
- This hormone ensures that glucose-dependent organs like the brain and heart receive a continuous energy supply even when no food is consumed.
4️⃣ Role of Other Hormones in Glucose Regulation
🔷 Epinephrine (Adrenaline)
- Released during stress or emergency (“fight or flight” situations) from the adrenal medulla, it increases blood glucose by stimulating glycogenolysis in the liver and muscles.
- It inhibits insulin release and promotes lipolysis, ensuring energy availability during emergencies or trauma.
- Epinephrine is especially important during hypoglycemia or physical stress.
🔷 Cortisol (Glucocorticoid Hormone)
- Released from the adrenal cortex in response to chronic stress or low blood glucose, cortisol enhances gluconeogenesis in the liver.
- It also reduces peripheral glucose uptake and increases protein breakdown, providing substrates for glucose synthesis.
- Cortisol plays a role in sustained glucose elevation during starvation, illness, or psychological stress.
🔷 Growth Hormone (GH)
- Secreted by the anterior pituitary gland, GH increases blood glucose by reducing insulin sensitivity in muscles and adipose tissues.
- It increases lipolysis and protein retention, conserving glucose for vital organs.
- GH is particularly important during childhood growth and recovery from illness.
🔷 Thyroid Hormones (T₃ and T₄)
- Thyroxine increases the basal metabolic rate (BMR) and promotes glucose absorption and utilization.
- It also enhances gluconeogenesis and glycogenolysis, indirectly affecting glucose homeostasis.
5️⃣ Glucose Regulation After Meals (Postprandial Phase)
- After a carbohydrate-rich meal, glucose levels rise in the bloodstream, stimulating the pancreatic beta cells to release insulin.
- Insulin promotes glucose uptake into muscle, fat, and liver cells, encourages glycogen and fat synthesis, and inhibits gluconeogenesis.
- As glucose levels normalize, insulin secretion gradually decreases, maintaining balance without causing hypoglycemia.
- This feedback ensures that the extra glucose is stored and not left circulating in the blood, which would otherwise damage tissues.
6️⃣ Glucose Regulation During Fasting or Starvation (Post-absorptive Phase)
- In the absence of food, blood glucose begins to fall, triggering glucagon release from alpha cells.
- The liver responds by breaking down glycogen stores and producing new glucose, ensuring that blood glucose remains within normal limits.
- If fasting continues, the body starts mobilizing fat stores for energy, and ketone bodies are produced for brain use (especially in prolonged fasting or starvation).
- Muscle proteins may also be broken down to provide amino acids for gluconeogenesis, ensuring survival in nutrient-deficient states.
2. PH buffer
Meaning and Definition of pH Buffer
- A pH buffer is a specially formulated aqueous solution that resists any significant change in its hydrogen ion concentration (pH) when a small amount of acid or base is added to it.
- In simpler terms, a buffer acts like a chemical shock absorber that helps maintain a stable pH level in both chemical solutions and biological systems, such as blood, cells, and tissues.
- This property of resisting pH change is essential for normal cellular function, enzymatic activity, and homeostasis in living organisms.
Composition of a Buffer Solution
- A buffer solution usually contains a weak acid and its conjugate base or a weak base and its conjugate acid, which work together to neutralize any incoming acid or base.
- This composition allows the buffer to “absorb” added hydrogen ions (H⁺) from acids or hydroxide ions (OH⁻) from bases without altering the overall pH significantly.
- Example of acidic buffer: Acetic acid (CH₃COOH) and sodium acetate (CH₃COONa)
- Example of basic buffer: Ammonium hydroxide (NH₄OH) and ammonium chloride (NH₄Cl)
Types of Buffers Based on pH Range
✅ A. Acidic Buffer (pH < 7)
- It is a buffer that maintains an acidic pH, usually in the range of 4–6.
- It contains a weak acid and its salt with a strong base.
- Example: Acetic acid + Sodium acetate
- This buffer can neutralize added bases and maintain acidic conditions, useful in biochemical labs and stomach pH maintenance.
✅ B. Basic or Alkaline Buffer (pH > 7)
- It is a buffer that maintains a basic pH, typically between 8–10.
- It is composed of a weak base and its salt with a strong acid.
- Example: Ammonium hydroxide + Ammonium chloride
- This buffer resists changes caused by added acids and is important in urinary pH regulation and industrial processes.
Mechanism of Buffer Action (How It Works)
- When a small amount of strong acid (HCl or H⁺) is added to the buffer, the conjugate base component of the buffer reacts with the extra H⁺ ions and neutralizes them, thus preventing a drop in pH.
- When a small amount of strong base (NaOH or OH⁻) is added to the buffer, the weak acid part of the buffer neutralizes the OH⁻ ions by donating H⁺, preventing a sharp rise in pH.
- This dynamic equilibrium keeps the pH of the solution stable under physiological or laboratory conditions.
Important Physiological Buffers in the Human Body
✅ A. Bicarbonate Buffer System (H₂CO₃ ↔ H⁺ + HCO₃⁻)
- It is the most important buffer in extracellular fluid and blood plasma.
- Carbonic acid (H₂CO₃) acts as the weak acid, and bicarbonate (HCO₃⁻) acts as the conjugate base.
- It helps maintain blood pH in the range of 7.35 to 7.45.
- When blood becomes acidic, bicarbonate ions neutralize excess H⁺; when blood becomes basic, carbonic acid releases H⁺.
✅ B. Phosphate Buffer System (H₂PO₄⁻/HPO₄²⁻)
- This buffer is important in intracellular fluid and renal tubules.
- It maintains pH in the range of 6.8 to 7.4 and helps in urine pH control.
- Works similarly by converting between dihydrogen phosphate and monohydrogen phosphate.
✅ C. Protein Buffer System (e.g., Hemoglobin)
- Proteins, especially hemoglobin, act as buffers by accepting or donating H⁺ ions through their amino acid side chains.
- Hemoglobin buffer system plays a vital role in transporting CO₂ and buffering blood pH in red blood cells.
Importance of Buffers in Nursing and Clinical Practice
- Buffers are crucial in maintaining acid-base balance in patients, especially those in critical care, ICU, and post-operative settings.
- Nurses must understand buffer systems when interpreting Arterial Blood Gas (ABG) reports for patients with acidosis or alkalosis.
- Buffer systems are present in IV fluids, parenteral nutrition, and dialysis solutions to ensure proper body pH.
- In emergency cases like diabetic ketoacidosis, sepsis, or respiratory failure, buffer balance helps guide therapeutic interventions.
Clinical Conditions Involving Buffer Disturbance
- Metabolic Acidosis: Due to kidney failure or diabetic ketoacidosis; requires bicarbonate administration.
- Metabolic Alkalosis: Caused by vomiting or diuretics; treated by correcting electrolyte imbalances.
- Respiratory Acidosis: Caused by hypoventilation or COPD; carbonic acid accumulates, treated with ventilation support.
- Respiratory Alkalosis: Due to hyperventilation (e.g., anxiety); managed by re-breathing techniques or sedation.
3. Mechanism of antibody production
- Antibody production refers to the complex immune process through which B lymphocytes identify, bind, and respond to specific antigens by producing antigen-specific immunoglobulins.
- The entire process is a coordinated effort between B cells, T-helper cells, antigen-presenting cells, and cytokines to ensure precision and immune memory.
1️⃣ Antigen Recognition and Entry
- A pathogen or foreign substance such as a virus, bacterium, or allergen enters the body through breaches in natural barriers like skin or mucosa.
- Pathogen-associated molecular patterns (PAMPs) on the antigen surface trigger immune detection by innate immune receptors like toll-like receptors (TLRs).
- Early activation of innate immunity helps recruit antigen-presenting cells to the site of antigen entry for further processing.
2️⃣ Antigen Processing by APCs
- Dendritic cells, macrophages, and B cells engulf the invading antigen, enzymatically degrade it into peptides, and load these onto MHC class II molecules.
- Processed antigen-MHC-II complexes migrate to the surface of the APC for presentation to naïve CD4+ T-helper lymphocytes in regional lymphoid tissues.
- Costimulatory molecules such as B7 (on APC) and CD28 (on T cell) are essential to confirm antigenic danger and ensure full T-cell activation.
3️⃣ Antigen Presentation to T-helper Cells
- CD4+ T-helper cells interact with antigen-MHC-II complexes on the surface of APCs using their T-cell receptor (TCR) and associated CD4 coreceptor.
- Cytokines such as IL-12, secreted by APCs, guide the differentiation of naïve T-helper cells into specific subsets like Th1 or Th2 based on the immune need.
- Repeated exposure to antigen enhances the memory phenotype in T-helper cells, strengthening future B cell responses.
4️⃣ Activation of T-helper Cells
- Activated T-helper cells release a cytokine profile including IL-2, IL-4, IL-5, and IL-21, which facilitates B-cell proliferation and immunoglobulin class switching.
- Cross-talk between T cells and B cells occurs at immunological synapses within germinal centers of lymph nodes and spleen.
- Follicular helper T cells (Tfh) play a specialized role in assisting B cells during germinal center reactions, ensuring high-affinity antibody production.
5️⃣ Antigen Binding to B Cell Receptor (BCR)
- Naïve B lymphocytes express membrane-bound IgM and IgD that act as B cell receptors to detect and bind specific antigenic epitopes.
- BCR–antigen interaction induces intracellular signaling cascades that prime the B cell for activation.
- Additional stimulation from cytokines and direct contact with T-helper cells leads to B cell differentiation and immunoglobulin class switching.
6️⃣ Clonal Expansion of Activated B Cells
- Once fully activated, the B cell undergoes clonal proliferation, resulting in the formation of multiple identical daughter B cells with the same antigen specificity.
- Somatic hypermutation in the variable region of antibody genes occurs to enhance affinity for the antigen (affinity maturation).
- Class switching enables B cells to produce IgG, IgA, or IgE instead of only IgM, adapting the response to the type and location of infection.
7️⃣ Differentiation into Plasma and Memory B Cells
- A portion of the activated B cell clones differentiate into plasma cells that secrete large volumes of antibodies, while others become memory B cells.
- Plasma cells can reside in bone marrow and continue to secrete antibodies for weeks to months post-infection.
- Memory B cells retain antigen specificity and can rapidly mount a response upon re-exposure, forming the basis of long-term immunity and vaccination.
8️⃣ Antibody Secretion
- Plasma cells secrete antibodies that enter the circulation and tissues to neutralize pathogens, activate the complement system, and promote opsonization.
- IgG antibodies neutralize bacterial toxins and viruses, while IgA works on mucosal surfaces, and IgE helps in parasitic defense and allergy.
- Antibodies also induce antibody-dependent cell-mediated cytotoxicity (ADCC), where NK cells destroy antibody-coated target cells.
9️⃣ Formation of Immunological Memory
- Memory B cells generated during the primary immune response persist long after the antigen is cleared and provide enhanced protection upon future exposure.
- Re-exposure triggers a faster, stronger, and more specific secondary response with quicker antibody production and higher affinity antibodies.
- Longevity of memory B cells ensures lasting protection, making vaccines effective for months to years depending on the antigen.
Types of Immunoglobulins Produced
| Immunoglobulin | Function |
|---|---|
| IgM | It is the first antibody produced; highly effective at activating complement. |
| IgG | It is the most abundant antibody in circulation; crosses the placenta to protect the fetus. |
| IgA | It is found in mucosal secretions (tears, saliva, breast milk); protects mucosal surfaces. |
| IgE | It is involved in allergic reactions and protection against parasitic worms. |
| IgD | It is involved in B cell activation; mainly found on immature B cells. |
