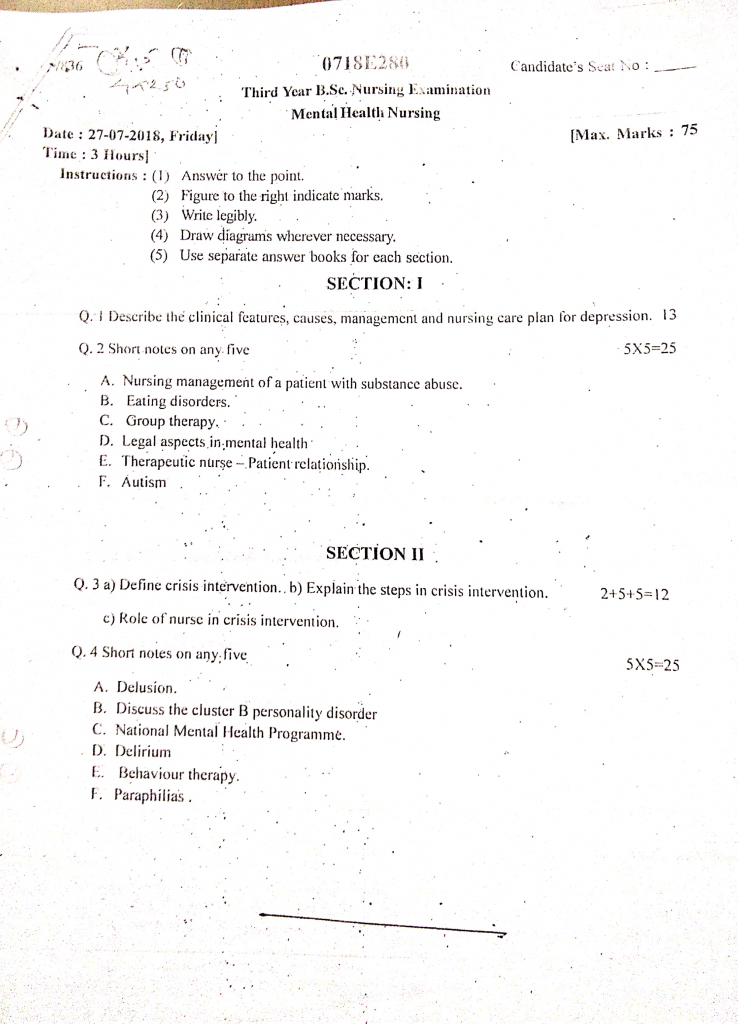
27/07/2018-B.SC-MENTAL HEALTH-PAPER DONE
Section 1
Q.1Described the clinical features, causes, management, nursing care plan for depression (13)
Clinical Features of Depression
These symptoms develop gradually and significantly interfere with the person’s social, occupational, and daily functioning.
1. Persistent Depressed Mood
It is observed that the patient experiences a continuous feeling of sadness, emptiness, or hopelessness, which persists for most of the day and nearly every day for at least two weeks.
2. Loss of Interest or Pleasure (Anhedonia)
The individual shows a marked reduction in interest or pleasure in almost all activities, even those that were previously enjoyable, such as hobbies, social interactions, or sexual activity.
3. Significant Weight Loss or Gain
There may be a noticeable decrease or increase in appetite, leading to unintentional weight loss or gain of more than 5% of body weight in a month without dieting.
4. Sleep Disturbances (Insomnia or Hypersomnia)
The patient may report difficulty falling asleep, early morning awakening, or excessive sleeping (hypersomnia) nearly every day.
5. Psychomotor Changes
There is either psychomotor retardation (slowing of speech and movements) or psychomotor agitation (restlessness, pacing), observed by others and not just reported by the patient.
6. Fatigue or Loss of Energy
It is often noted that the person feels tired and drained even without significant physical activity, making it difficult to perform daily tasks.
7. Feelings of Worthlessness or Guilt
The individual may have excessive or inappropriate guilt, or feelings of worthlessness, which are not based on reality and often lead to self-blame for events beyond their control.
8. Decreased Concentration and Indecisiveness
The person may experience difficulty concentrating, remembering, or making decisions, which can affect academic or work performance significantly.
9. Recurrent Thoughts of Death or Suicide
The patient may report recurrent thoughts of death, suicidal ideation without a plan, or even specific plans for suicide, which is a medical emergency.
10. Social Withdrawal and Isolation
The individual may avoid contact with family, friends, and colleagues, preferring to remain alone and detached from social activities.
11. Somatic Symptoms
The patient may complain of frequent headaches, body aches, or gastrointestinal issues like constipation, without any organic cause identifiable on physical examination.
12. Neglect of Personal Hygiene
It may be observed that the person stops grooming, bathing, or caring for their physical appearance, reflecting a decline in self-care and motivation.
13. Irritability or Restlessness (especially in adolescents or elderly)
Some individuals, particularly adolescents and older adults, may present with increased irritability, agitation, or frustration, instead of overt sadness.
Causes / Etiology of Depression
These causes are categorized under biological, psychological, and social models with detailed explanation.
1. Genetic Factors / Heredity
- Depression often runs in families, and individuals who have a first-degree relative (such as a parent or sibling) with depression are at a significantly higher risk of developing the disorder themselves.
- Twin and adoption studies have confirmed a genetic component, suggesting that multiple genes may be involved in the vulnerability to depression, especially in early-onset cases.
2. Neurobiological and Biochemical Causes
- Altered levels of neurotransmitters such as serotonin, norepinephrine, and dopamine in the brain are strongly linked to depressive symptoms, as they play a key role in mood regulation, sleep, appetite, and motivation.
- Imbalance of neurohormones like cortisol (stress hormone) is often found in patients with depression, indicating dysregulation of the hypothalamic-pituitary-adrenal (HPA) axis.
3. Psychological Causes
- Unresolved trauma or childhood abuse (emotional, physical, or sexual) can predispose individuals to develop depression later in life due to long-standing emotional dysregulation.
- Negative thinking patterns, poor coping mechanisms, and learned helplessness often contribute to the development of depression in response to stress.
4. Social and Environmental Causes
- Major life stressors such as the death of a loved one, divorce, unemployment, or financial crisis can trigger depressive episodes in vulnerable individuals.
- Loneliness, lack of emotional support, or strained relationships often serve as strong contributors to situational or reactive depression.
5. Medical and Physical Illnesses
- Chronic physical illnesses such as cancer, stroke, Parkinson’s disease, diabetes, or heart disease may lead to depression due to functional disability, lifestyle restrictions, or ongoing pain.
- Hormonal imbalances such as those occurring in thyroid dysfunction or postpartum period can also contribute to depressive symptoms.
6. Substance Abuse and Medications
- Excessive use of alcohol, sedatives, or illicit drugs can lead to depressive symptoms either due to direct brain effects or withdrawal states.
- Certain medications such as beta-blockers, corticosteroids, oral contraceptives, and chemotherapy agents may have side effects that include mood disturbances and depression.
7. Personality Traits and Temperament
- Individuals with low self-esteem, high levels of self-criticism, or perfectionist tendencies are more likely to develop depression under stressful situations.
- Introverted personality types with poor social skills may struggle to seek help or manage interpersonal stress, increasing the risk of depression.
8. Postpartum and Hormonal Factors
- Women are at increased risk of depression during major hormonal transitions, such as postpartum period, menopause, or during premenstrual dysphoric disorder.
- Postpartum depression is particularly concerning, as it affects the mother-child bonding and the overall well-being of the family unit.
9. Cultural and Societal Pressures
- Social stigma, cultural discrimination, and academic or occupational pressures, especially in developing countries, contribute to psychological distress and depression.
- Adolescents and young adults may face identity crises, social media comparison, and peer rejection, all of which are emerging contributors to modern depressive disorders.
Management of Depression
The management of depression is multidimensional and involves pharmacological, psychological, lifestyle, and supportive interventions.
1. Pharmacological Management (Medical Treatment)
- Antidepressant medications are the mainstay of treatment, especially in moderate to severe depression, and are prescribed under medical supervision after thorough psychiatric evaluation.
- Selective Serotonin Reuptake Inhibitors (SSRIs) such as Fluoxetine, Sertraline, and Escitalopram are most commonly used due to their relatively safe side effect profile and ease of use.
- Serotonin-Norepinephrine Reuptake Inhibitors (SNRIs) like Venlafaxine and Duloxetine are prescribed when SSRIs are ineffective or if pain symptoms are also present.
- Tricyclic Antidepressants (TCAs) such as Amitriptyline or Imipramine are older agents, effective but associated with more anticholinergic side effects and thus used cautiously.
- Monoamine Oxidase Inhibitors (MAOIs) such as Phenelzine are used in treatment-resistant cases but require dietary restrictions due to risk of hypertensive crisis.
- Atypical antidepressants like Bupropion or Mirtazapine are considered in patients with specific symptoms such as fatigue, sleep disturbances, or weight loss.
- Mood stabilizers (e.g., Lithium, Lamotrigine) or antipsychotics (e.g., Quetiapine, Aripiprazole) may be added in cases of bipolar depression or psychotic depression.
- Electroconvulsive Therapy (ECT) is recommended for patients with severe, treatment-resistant depression, suicidal ideation, or catatonia; it is safe and effective under anesthesia.
2. Psychotherapeutic Management (Non-Medical Therapies)
- Cognitive Behavioral Therapy (CBT) helps patients identify and modify negative thought patterns and behaviors contributing to their depression.
- Interpersonal Therapy (IPT) focuses on improving communication, resolving interpersonal conflicts, and managing grief or role transitions that contribute to mood disturbances.
- Behavioral Activation Therapy involves helping the patient gradually re-engage in meaningful activities to counteract inactivity and loss of interest.
- Supportive Psychotherapy offers emotional support, encouragement, and validation through a trusting therapeutic relationship.
- Group Therapy allows individuals to share experiences with others, reducing isolation and offering peer support and feedback.
- Family Therapy may be used when family conflicts or lack of support are contributing factors, helping to improve communication and understanding.
3. Lifestyle and Supportive Measures
- Regular physical exercise such as walking, yoga, or swimming helps in boosting endorphins and improving mood and energy levels.
- A structured daily routine is encouraged to bring back regular sleep, meal, and activity patterns, providing a sense of control and stability.
- Healthy nutrition with adequate intake of vitamins and minerals, especially folate, omega-3, and vitamin D, supports brain health and mood regulation.
- Sleep hygiene practices such as fixed sleep schedules, reduced screen time, and avoiding caffeine before bedtime are important in managing insomnia related to depression.
- Avoidance of alcohol, recreational drugs, and stimulants is strongly advised, as these substances can worsen depressive symptoms or interfere with medications.
4. Psychoeducation and Social Support
- Educating the patient and family about the nature, course, and treatment of depression helps reduce stigma and improves treatment adherence.
- Involving family and caregivers in the recovery process ensures better emotional support, understanding, and monitoring for relapse or side effects.
- Linking the patient with social services, community mental health resources, or support groups helps reduce isolation and promote community integration.
- Occupational rehabilitation and skill-building programs may be necessary if the depression has affected the patient’s work performance or independence.
5. Emergency Management
- In cases of acute suicidal ideation or suicide attempt, immediate hospitalization is needed for safety, observation, and intensive therapy.
- Crisis intervention services, including helplines, emergency psychiatry units, and mental health response teams, should be involved.
- If the patient is unable to care for themselves, short-term inpatient care may be provided until stabilization occurs.
Nursing Management for Depression
🟦 1. Nursing Diagnosis : Risk for Suicide related to hopelessness and feelings of worthlessness
- It is important to frequently assess the patient’s verbal and non-verbal cues for suicidal ideation, using tools like the Columbia Suicide Severity Rating Scale (C-SSRS).
- It is essential to implement suicide precautions, such as removing belts, shoelaces, glass items, and medications from the patient’s environment.
- The nurse should maintain close observation through one-on-one monitoring, especially during high-risk times like shift changes or nights.
- The nurse must document all suicidal threats or attempts immediately and communicate with the mental health team promptly.
- It is necessary to encourage the patient to verbalize feelings and explore reasons behind their suicidal thoughts in a non-judgmental setting.
- The nurse should involve family members in the treatment plan, educating them on warning signs and how to provide support.
- It is advised to establish a written or verbal safety contract with the patient, committing not to self-harm and to seek help when overwhelmed.
2. Nursing Diagnosis : Disturbed Sleep Pattern related to psychological distress
- The nurse should identify specific stressors interfering with sleep and assist in developing coping strategies.
- It is beneficial to create a calm and dark sleep environment, avoiding bright lights or noise during resting hours.
- Encourage consistent sleep-wake cycles, even on weekends, to regulate the circadian rhythm.
- The nurse should monitor for side effects of antidepressants, such as insomnia, and report them to the physician.
- Offer non-pharmacological interventions such as warm milk, guided imagery, or calming music before bedtime.
- Educate the patient on avoiding naps during the day, which can interfere with nighttime sleep.
- If necessary, coordinate with the physician for melatonin supplements or sedative-hypnotics, with clear monitoring.
3. Nursing Diagnosis : Imbalanced Nutrition less than body requirements related to decreased appetite
- It is essential to monitor serum electrolytes, albumin, and body weight regularly to assess nutritional risk.
- Provide nutritional education in small segments, especially if the patient has cognitive difficulty due to depression.
- Allow patient’s choice of food, especially favorite or comfort meals, to promote intake and autonomy.
- Offer nutritional supplements (e.g., protein shakes, multivitamins) if oral intake remains low despite encouragement.
- It is necessary to praise even small efforts made to eat, reinforcing positive behavior without scolding.
- The nurse should coordinate with a dietitian for a patient-specific nutritional care plan, especially in severe weight loss.
- Offer meals in a supportive environment, possibly with a companion, to reduce the sense of loneliness during eating.
4. Nursing Diagnosis : Low Self-Esteem related to guilt, shame, and self-blame
- The nurse should encourage patients to engage in journaling or other expressive activities that build self-awareness and confidence.
- It is necessary to set short-term, achievable goals to help the patient experience success and regain control.
- Promote self-care activities like grooming, dressing, and personal hygiene to improve self-image.
- Encourage participation in skill-building or recreational therapy sessions, such as art, dance, or writing therapy.
- Avoid criticism and comparisons, instead reinforcing strengths and highlighting past achievements.
- The nurse should reinforce the belief that setbacks are part of healing, and guide them to view mistakes as learning opportunities.
- Provide structured daily routines, as predictability can reduce feelings of inadequacy and boost confidence.
5. Nursing Diagnosis : Social Isolation related to withdrawal and fear of rejection
- It is important to validate the patient’s fears and discomforts about social situations, without forcing them into interactions.
- Begin with non-threatening, brief interactions, such as greeting staff, progressing slowly to group activities.
- Encourage family visits, video calls, or messages from loved ones to re-establish emotional bonds.
- Introduce pet therapy or animal-assisted therapy if available, which can improve emotional engagement.
- Provide positive reinforcement for every attempt at social interaction, even if minimal.
- The nurse should help identify specific barriers to social participation, such as shame or past trauma, and work with the therapist to address them.
- Plan and schedule community re-entry programs, if applicable, to help patient transition back into society gradually.
Q.2 Shorts notes any five (5×5=25)
A. Nursing management of a patient with substance abuse
1. Assessment Phase
- It is essential for the nurse to conduct a comprehensive assessment of the patient’s drug history, including the type of substance used, duration, frequency, route of intake, and any history of withdrawal or overdose.
- The nurse must assess physical health status, including signs of malnutrition, liver damage, infections (like hepatitis or HIV), or withdrawal symptoms such as tremors, agitation, and sweating.
- Psychological evaluation should be done to identify co-occurring mental health disorders like depression, anxiety, or psychosis.
- The nurse should also assess the patient’s level of motivation for change, insight into their addiction, and readiness for rehabilitation.
- It is important to gather social history, including family dynamics, employment status, peer influence, and legal problems related to substance use.
2. Detoxification and Withdrawal Care
- During detoxification, the nurse should provide 24-hour monitoring for withdrawal symptoms and administer prescribed medications such as benzodiazepines (e.g., diazepam) for alcohol withdrawal.
- The nurse should monitor vital signs frequently, especially blood pressure, pulse, temperature, and respiratory rate, to detect complications like delirium tremens.
- The patient should be kept in a low-stimulus, quiet environment to reduce anxiety and agitation during withdrawal.
- It is necessary to provide adequate hydration, electrolyte balance, and nutritional support, as many patients may present with dehydration or vitamin deficiencies.
- The nurse may administer vitamin supplements like thiamine (Vitamin B1) to prevent Wernicke’s encephalopathy, especially in alcohol-dependent individuals.
3. Therapeutic Communication and Emotional Support:
- The nurse must use non-judgmental, empathetic, and therapeutic communication techniques to build trust and encourage openness from the patient.
- It is important to acknowledge the patient’s denial and defense mechanisms and guide them gently toward acceptance and responsibility.
- The nurse should validate the patient’s feelings of guilt, shame, or fear, while offering hope and support for recovery.
- Motivational interviewing techniques may be used by the nurse to explore ambivalence and enhance the patient’s motivation for change.
4. Health Education and Behavior Modification
- The nurse plays a key role in educating the patient about the harmful effects of substance use on health, family life, and career.
- Teaching relapse prevention strategies is crucial, including coping mechanisms, trigger identification, and avoiding high-risk situations.
- Cognitive-behavioral approaches can be encouraged to help patients replace negative thought patterns with healthy behaviors.
- The nurse should help in developing a structured daily routine to promote discipline and reduce idle time that may lead to cravings.
5. Family Involvement and Psychosocial Support
- The nurse should involve family members in therapy sessions and psychoeducation programs to help them understand the nature of addiction and their role in recovery.
- It is important to assess family stress, co-dependency patterns, and enabler behaviors that may contribute to the addiction cycle.
- Nurses should provide referrals to support groups like Alcoholics Anonymous (AA) or Narcotics Anonymous (NA) for both patients and families.
- Social services or vocational guidance may be required to help the patient reintegrate into society and find employment or housing.
6. Rehabilitation and Follow-Up Care
- The nurse should collaborate with the healthcare team to formulate a long-term rehabilitation plan that includes inpatient or outpatient treatment programs.
- The patient should be encouraged to participate in group therapy, occupational therapy, and spiritual or recreational activities as part of rehabilitation.
- It is the nurse’s role to maintain contact through regular follow-up visits, telephone calls, or home visits to monitor progress and address any relapse signs.
- The nurse must also keep detailed records of behavior changes, treatment adherence, and progress toward goals.
7. Legal and Ethical Considerations
- The nurse must maintain confidentiality and uphold the rights of the patient, especially in cases involving criminal behavior or social stigma.
- In case of suicidal or violent behavior, the nurse may be required to act promptly by notifying authorities or initiating emergency psychiatric care.
B. Eating disorder
Definition
- Eating disorders are serious mental health conditions characterized by abnormal eating behaviors, disturbed body image, and unhealthy preoccupation with food, weight, and shape.
- These disorders can lead to severe physical and psychological consequences, including malnutrition, organ damage, and even death if untreated.
- Eating disorders are often associated with underlying emotional issues, such as low self-esteem, anxiety, perfectionism, or trauma.
Major Types of Eating Disorders (As per DSM-5)
1️⃣ Anorexia Nervosa
- It is a disorder in which the individual has an intense fear of gaining weight and a distorted body image, leading to severe restriction of food intake.
- Despite being underweight, the person perceives themselves as overweight and may engage in excessive exercise or starvation.
Subtypes include :
- Restricting type: weight loss is achieved through dieting, fasting, or excessive exercise.
- Binge-eating/purging type: includes episodes of binge eating or purging (vomiting, laxatives).
2️⃣ Bulimia Nervosa
- This disorder involves repeated episodes of binge eating, followed by inappropriate compensatory behaviors such as self-induced vomiting, use of laxatives, fasting, or over-exercising.
- Unlike anorexia, individuals with bulimia usually maintain a normal body weight or are slightly overweight.
- They experience feelings of guilt, shame, and secrecy about their eating habits.
3️⃣ Binge-Eating Disorder
- It is marked by recurrent episodes of eating large amounts of food in a short period, often quickly and to the point of discomfort.
- The person experiences a lack of control during the binge, but unlike bulimia, there are no purging behaviors.
- It often leads to obesity, guilt, and low self-esteem.
4️⃣ Other Specified Feeding or Eating Disorders (OSFED)
- Includes atypical eating behaviors that do not meet full criteria of anorexia, bulimia, or binge-eating disorder but are still clinically significant.
- Examples include night eating syndrome or purging disorder without bingeing.
Causes and Risk Factors
- Biological factors, such as genetics, hormonal imbalance, and neurotransmitter abnormalities (e.g., serotonin dysfunction), contribute to vulnerability.
- Psychological factors include low self-worth, perfectionism, trauma, body dissatisfaction, and poor emotional regulation.
- Sociocultural influences like media, fashion standards, peer pressure, and social media can idealize thinness and promote unhealthy body ideals.
- Family dynamics, such as overly controlling or critical parenting, or exposure to dieting and body-shaming at home, also play a role.
Signs and Symptoms
Anorexia Nervosa
- Severe weight loss, fear of weight gain, refusal to eat
- Amenorrhea (absence of menstruation) in females
- Dry skin, hair thinning, brittle nails
- Cold intolerance, bradycardia (slow pulse), and fatigue
Bulimia Nervosa
- Normal weight or slight overweight
- Evidence of vomiting (tooth decay, swollen cheeks, calluses on knuckles)
- Secretive eating, excessive concern with weight
- Dehydration and electrolyte imbalance
Binge-Eating Disorder
- Frequent overeating episodes, often at night or in solitude
- Feelings of guilt, distress, and depression after eating
- Rapid weight gain and associated health problems
Complications
- Electrolyte imbalances (especially low potassium) leading to cardiac arrhythmias.
- Malnutrition and organ failure, especially in prolonged anorexia.
- Esophageal tears and gastric rupture due to repeated vomiting in bulimia.
- Depression, anxiety, and suicidal tendencies are common psychological complications.
- Infertility, osteoporosis, and growth retardation in adolescents with anorexia.
Medical Management of Eating Disorders
Hospitalization (When Required)
- Hospitalization is necessary when the patient shows life-threatening complications such as severe malnutrition, dehydration, bradycardia, hypotension, or electrolyte imbalance.
- It is also considered in cases of suicidal risk, cardiac arrhythmias, or refusal to eat or cooperate with outpatient care.
Nutritional Rehabilitation
- The primary goal is to restore the patient’s nutritional status, correct deficiencies, and reach a safe body weight.
- A gradual refeeding plan is developed, starting with calorie-controlled diets and increasing gradually to avoid refeeding syndrome.
- Multivitamin supplements are given, especially Vitamin B complex, calcium, magnesium, and iron to address malnutrition-related complications.
Pharmacotherapy (Medication)
For Anorexia Nervosa :
- Medications are generally less effective in underweight anorexia patients, but may be used after weight restoration.
- Selective Serotonin Reuptake Inhibitors (SSRIs) like fluoxetine may help in reducing obsessive thoughts and preventing relapse.
- Atypical antipsychotics such as olanzapine may be used in low doses to help with weight gain and reduce anxiety around eating.
For Bulimia Nervosa :
- SSRIs (especially fluoxetine 60 mg/day) are FDA-approved and effective in reducing binge-purge episodes and improving mood.
- Antidepressants like sertraline or citalopram may also be helpful in improving control over eating behaviors and managing depression.
- Avoid bupropion in bulimia due to increased risk of seizures.
For Binge-Eating Disorder :
- Lisdexamfetamine (Vyvanse) is FDA-approved and effective in reducing binge frequency.
- SSRIs, topiramate, and naltrexone-bupropion combinations may also reduce cravings and binge episodes.
Psychotherapy (Essential Adjunct to Medical Treatment)
- Cognitive Behavioral Therapy (CBT) is the most effective psychological intervention, helping patients recognize and modify distorted body image and eating behaviors.
- Family-Based Therapy (FBT), also called the Maudsley method, is especially effective in adolescents with anorexia.
- Dialectical Behavior Therapy (DBT) may help manage impulsivity and emotional dysregulation, especially in bulimia and binge-eating disorder.
Nursing Management of Eating Disorders
- The nurse must perform a comprehensive assessment of dietary habits, weight history, physical signs, and psychological status.
- It is important to monitor vital signs, weight, fluid and electrolyte balance, and intake-output charts daily.
- The nurse should provide nutritional education and meal supervision, ensuring gradual weight restoration if needed.
- Cognitive-behavioral therapy (CBT) can be supported by the nurse through reinforcement of positive body image and thought restructuring.
- The nurse must establish a therapeutic, non-judgmental, and trusting relationship, encouraging honest communication about body image and eating behavior.
- Health education should be given to the patient and family regarding the dangers of dieting, purging, and unhealthy body comparisons.
- Nurses must monitor for self-harm or suicidal ideation, especially in severe or treatment-resistant cases.
- Collaboration with a multidisciplinary team including dietitians, psychologists, psychiatrists, and social workers is essential for holistic care.
- Support group participation and ongoing counseling may be recommended after discharge for relapse prevention.
- Nurses should reinforce the importance of follow-up care, medication adherence (if prescribed), and healthy lifestyle practices.
C. Group therapy
Definition
- Group therapy is a form of psychotherapy in which a small number of individuals with similar emotional or psychological problems meet together under the guidance of a trained therapist.
- It is a structured therapeutic environment where patients share their experiences, learn coping skills, and gain support from both the therapist and fellow group members.
Goals of Group Therapy
- The primary goal is to help individuals explore their thoughts, emotions, and behaviors in a safe, supportive setting.
- Group therapy aims to enhance self-awareness, self-esteem, and social skills through peer feedback and therapist guidance.
- It provides emotional support, shared learning, and encouragement from others who have similar issues.
- The goal is also to help patients learn new behaviors and adaptive coping mechanisms through role-playing, discussion, and reflection.
- It is meant to facilitate change in attitudes, behaviors, and beliefs through interpersonal interaction.
Types of Group Therapy
1️⃣ Psychoeducational Group Therapy
- Psychoeducational groups are designed to educate clients about specific psychological or medical conditions, such as depression, anxiety, schizophrenia, substance use, or chronic illnesses.
- It is used to provide structured information, teach coping strategies, improve medication compliance, and enhance self-management skills.
2️⃣ Supportive Group Therapy
- Support groups are meant to offer emotional support, reassurance, and shared experience among members facing similar challenges.
- It helps patients feel less alone in their struggles, reduces stress, and promotes hope and motivation for recovery.
- Common examples include bereavement groups, cancer survivor groups, HIV support groups, and mental health peer groups.
3️⃣ Cognitive-Behavioral Therapy (CBT) Group
- CBT group therapy focuses on helping individuals recognize and change negative thought patterns, beliefs, and behaviors that contribute to emotional problems.
- This type of group therapy is goal-oriented and structured, often using homework assignments, role-play, and worksheets.
- It is especially effective in anxiety disorders, phobias, OCD, depression, and substance abuse.
4️⃣ Interpersonal Therapy (IPT) Group
- IPT group therapy focuses on improving interpersonal functioning and relationships, helping clients explore how past and current relationships affect their emotions and mental health.
- It encourages participants to develop better communication, conflict resolution, and social interaction skills.
- It is especially useful in depression, social anxiety, and personality disorders.
5️⃣ Skills Training Group Therapy
- These groups are formed to teach practical life skills, vocational abilities, and social interaction skills in a therapeutic setting.
- Common skills taught include assertiveness, stress management, time management, communication, and anger control.
- It is highly beneficial for patients with schizophrenia, developmental delays, or chronic mental illness.
6️⃣ Self-Help or Peer-Led Groups
- These groups are voluntary and typically led by members, rather than professionals, who have experience with the same condition or challenge.
- Members provide mutual support, share experiences, and promote recovery through empathy and solidarity.
- Examples include Alcoholics Anonymous (AA), Narcotics Anonymous (NA), and Depression Support Groups.
7️⃣ Expressive Therapy Groups
- These groups use creative arts such as music, dance, art, or drama as a medium for self-expression and emotional healing.
- It allows clients to express feelings non-verbally, especially when they struggle to articulate emotions.
Indications for Group Therapy
- Depression, anxiety, and stress-related disorders where patients benefit from shared experiences.
- Substance use disorders, where group settings provide peer accountability and support.
- Grief and loss, where individuals find comfort in connecting with others facing similar pain.
- Chronic medical conditions, such as cancer, diabetes, or HIV, for emotional and informational support.
- Adolescent and family issues, like school problems or parent-child conflict, are often addressed in group formats.
- Social skill deficits, especially in autism spectrum disorder or schizophrenia.
Contraindications of Group Therapy
- Patients with acute psychosis or suicidal risk who may be disruptive or unsafe for group participation.
- Individuals with severe cognitive impairment, who may not understand or benefit from discussion.
- Those with extreme social anxiety or hostility, who may struggle to engage or may harm group dynamics.
Advantages of Group Therapy
- It provides a sense of belonging and acceptance, reducing feelings of isolation.
- Group therapy offers multiple perspectives and feedback from peers.
- It is cost-effective, as one therapist can help multiple patients at once.
- It helps improve interpersonal communication and relationship-building skills.
- Patients learn by observing others and can model positive behaviors.
- It can motivate change through peer influence and role models within the group.
Disadvantages / Limitations
- Some individuals may feel shy or anxious to speak in a group setting.
- There may be conflicts or domination by certain group members, disrupting harmony.
- Confidentiality is harder to maintain, as group members must voluntarily respect others’ privacy.
Role of the Nurse in Group Therapy
- The nurse may act as a co-therapist or facilitator in psychoeducational and support groups.
- It is the nurse’s role to observe group dynamics and ensure a safe, respectful environment.
- The nurse helps in screening suitable patients for group therapy, based on psychological readiness and diagnosis.
- She must encourage participation and manage disruptive behaviors during group sessions.
- The nurse is responsible for documenting patient progress, participation, and any significant observations.
- She also provides emotional support before and after sessions, especially for patients who feel overwhelmed.
- The nurse can use group feedback to reinforce individual care plans and collaborate with other mental health professionals.
D. Legal aspects in mental health
1. Legal Recognition under Disability Laws
- It is important to understand that Autism Spectrum Disorder (ASD) is officially recognized as a form of disability under the Rights of Persons with Disabilities (RPwD) Act, 2016, ensuring legal protection and entitlement to services.
- It is legally acknowledged that autism is a lifelong developmental condition, and individuals with autism must be granted the same rights and dignity as other citizens.
- It is mandated that certification of disability must be provided based on standard tools like INCLEN or Indian Scale for Assessment of Autism (ISAA), allowing access to benefits.
2. Right to Education and Inclusive Learning
- It is guaranteed under the Right to Education Act (2009) that children with autism are entitled to free and compulsory education up to the age of 18 years, in a manner inclusive of their needs.
- It is required that schools provide Individualized Education Plans (IEPs) tailored to the specific strengths and challenges of each autistic learner.
- It is directed that no child with autism shall be denied admission in any school on the grounds of disability, and barriers to learning must be removed through curriculum adaptation.
3. Guardianship and Legal Capacity
- It is facilitated under the National Trust Act, 1999, that legal guardians can be appointed for individuals with severe autism to handle personal, medical, or financial decisions in their best interest.
- It is also emphasized in the Mental Healthcare Act, 2017, that individuals with autism must be supported through advance directives and nominated representatives, ensuring participation in decision-making.
- It is recognized that individuals with mild to moderate autism can exercise partial legal capacity and should be empowered to make decisions wherever possible with suitable support.
4. Mental Health Care Rights and Protection
- It is clearly stated under the Mental Healthcare Act, 2017, that persons with autism have the right to access mental health care in a safe, non-discriminatory, and community-based environment.
- It is essential that consent for psychiatric care is obtained from the individual or guardian, and coercive treatments like isolation or physical restraint must be avoided unless absolutely necessary and reported.
- It is provided that mental health services must be affordable, accessible, and acceptable, and every autistic person has the right to confidentiality and respectful communication.
5. Prevention of Abuse and Exploitation
- It is a legal obligation under the Protection of Children from Sexual Offences (POCSO) Act, 2012) to ensure that children with autism are safeguarded from abuse, neglect, or exploitation in institutional or home settings.
- It is essential for healthcare workers, teachers, and caregivers to report any suspicion of abuse or neglect immediately to child protection authorities or police as mandatory reporters.
- It is important that counseling and trauma-informed support are provided to the child and family, and that abuse-related investigations are conducted sensitively, respecting communication limitations.
6. Access to Health and Rehabilitation Services\
- It is the responsibility of the government under RPwD Act, 2016, to ensure that persons with autism receive early identification, therapeutic services, and assistive technology devices without discrimination.
- It is mandated that public hospitals and community health centers maintain dedicated disability desks, and provide free medicines, therapies, and diagnostic services for persons with autism.
- It is legally required that annual review and reassessment of disability is conducted to monitor progress and update intervention plans.
7. Reservation and Employment Rights
- It is stated that persons with autism and 40% or more benchmark disability are eligible for 4% reservation in government jobs and 5% in higher education, as per the RPwD Act.
- It is necessary that workplace environments provide assistive technologies, flexible schedules, and sensitization training to promote inclusion.
- It is also mentioned that autistic adults should be offered vocational guidance, skill-building, and on-the-job training programs, especially in protected or supported employment settings.
8. Role of Nurse in Legal Compliance
- It is the professional and legal responsibility of nurses to ensure that informed consent is always obtained from either the autistic individual or their guardian before initiating therapy or interventions.
- It is necessary that nurses maintain confidential, unbiased, and respectful interactions, avoiding any form of stigma or labeling in their care delivery.
- It is also the nurse’s duty to be aware of the patient’s rights under RPwD and Mental Health Acts, and to act as an advocate, ensuring that legal protections are implemented in the clinical setting.
E. Therapeutic nurse – patient relationship
Definition
- It is a professional, goal-directed, and time-limited interaction between a nurse and a patient, which is established to promote the patient’s well-being and recovery.
- It is based on trust, empathy, respect, confidentiality, and effective communication, and it is essential in psychiatric as well as general nursing care.
Objectives of Therapeutic Nurse-Patient Relationship
- To develop trust and build rapport between nurse and patient.
- To encourage open and honest communication.
- To support emotional, psychological, and physical healing.
- To promote patient’s independence and self-esteem.
- To help the patient express feelings and concerns freely.
- To provide a safe, empathetic, and non-judgmental environment.
- To guide the patient in identifying problems and setting goals.
- To enhance treatment compliance and coping skills.
- To maintain professional, ethical, and therapeutic boundaries.
- To educate the patient about illness and promote health awareness.
Characteristics of a Therapeutic Relationship
- It is goal-oriented, where the main focus is on the patient’s mental, emotional, physical, or social recovery.
- It is patient-centered, meaning the patient’s needs and problems guide the entire process.
- It involves clear boundaries, ensuring professional distance and emotional safety.
- It is built on trust, where the patient feels safe, understood, and accepted.
- It requires active listening and empathy, where the nurse attentively responds to the patient’s concerns and emotions.
- It promotes mutual respect and dignity, encouraging patient autonomy and participation in care.
- It involves the use of professional communication skills, including verbal and non-verbal methods.
- It is time-bound and purposeful, unlike social or personal relationships.
Phases of Therapeutic Relationship (by Hildegard Peplau)
1️⃣ Pre-Interaction Phase
- It is the phase before meeting the patient, where the nurse prepares mentally and gathers background information.
- It is the phase of self-reflection, where the nurse evaluates personal attitudes, fears, or biases.
- It involves planning for the first interaction, such as reviewing the patient’s case history or environment.
2️⃣ Orientation Phase
- It is the introductory phase, where the nurse and patient meet and start building trust.
- It involves introducing oneself, explaining the purpose of the relationship, and discussing boundaries and confidentiality.
- The nurse begins assessing the patient’s needs, problems, and goals in this phase.
- It is the phase where rapport is established, which forms the foundation of the therapeutic process.
3️⃣ Working Phase (or Exploitation Phase)
- It is the active phase of the relationship, where most therapeutic work is carried out.
- The nurse encourages the patient to express feelings, explore problems, and work towards set goals.
- It is the phase where the nurse provides support, guidance, and therapeutic interventions.
- Transference and counter-transference may occur, and must be managed appropriately by the nurse.
- It is also the phase where trust deepens, and patients start becoming more independent and cooperative.
4️⃣ Termination Phase
- It is the final phase, where the therapeutic relationship is ended in a planned and healthy manner.
- The nurse and patient review the progress made, and evaluate whether the goals were achieved.
- It involves expressing feelings about ending the relationship, both by the nurse and the patient.
- The nurse provides guidance for the future and refers the patient if needed.
- It is important for the nurse to ensure closure, avoid abrupt endings, and handle emotional responses with care.
Nursing Responsibilities in the Therapeutic Relationship
- It is the nurse’s responsibility to develop trust and maintain professional boundaries throughout the interaction.
- The nurse must respect the patient’s privacy, confidentiality, and cultural background during care.
- It is essential for the nurse to use therapeutic communication skills, such as empathy, active listening, reflection, and clarification.
- The nurse should observe non-verbal cues and respond appropriately to the patient’s verbal and emotional expressions.
- The nurse must be emotionally stable and self-aware, avoiding counter-transference or emotional dependency.
- The nurse is expected to document the progress and maintain accurate records of patient interactions.
- It is important for the nurse to encourage patient participation and support patient autonomy and decision-making.
- The nurse must be consistent and reliable, following through on promises and scheduled interactions.
- The nurse should intervene therapeutically in times of crisis, helping the patient manage anxiety, fear, or aggression.
- The nurse needs to evaluate the effectiveness of the relationship and make necessary adjustments as needed.
F. Autism
Definition
Autism Spectrum Disorder (ASD) is a neurodevelopmental disorder characterized by persistent deficits in social communication and interaction, along with restricted, repetitive patterns of behavior, interests, or activities, typically manifesting in early childhood.
Etiology (Causes)
- Genetic mutations (e.g., chromosomal abnormalities, single-gene syndromes)
- Family history of autism
- Prenatal factors (e.g., maternal infections, exposure to toxins)
- Advanced parental age at conception
- Low birth weight or prematurity
Pathophysiology
- Neurobiological basis: Altered brain development and connectivity, especially in areas like the amygdala, frontal cortex, and cerebellum.
- Synaptic dysfunction: Abnormalities in neuronal signaling and neurotransmitters (e.g., serotonin, dopamine).
- Genetic alterations: Involvement of genes such as MECP2, SHANK3, and FMR1 that regulate brain growth and synaptic development.
- Immune dysregulation: Inflammatory cytokines may affect neurodevelopment during the fetal period.
- Mirror neuron dysfunction: Impaired empathy and imitation abilities due to mirror neuron system abnormalities.
Clinical Manifestations
- Impaired eye contact and difficulty in social interactions
- Delayed or absent speech and language development
- Repetitive behaviors (e.g., hand-flapping, rocking)
- Insistence on sameness or routines
- Hyper- or hypo-reactivity to sensory input
- Lack of interest in peers or group play
Diagnostic Evaluation
- Developmental screening (e.g., M-CHAT)
- Diagnostic tools: Autism Diagnostic Observation Schedule (ADOS), Autism Diagnostic Interview-Revised (ADI-R)
- Neurological examination
- Genetic testing (if syndromic features present)
- Audiological assessment (to rule out hearing loss)
Medical Management
There is no definitive cure for autism; hence, management is mainly supportive and focused on symptom control.
Pharmacological therapy includes:
- Risperidone or Aripiprazole for irritability and aggression.
- SSRIs for managing anxiety or obsessive behaviors.
- Stimulants like methylphenidate for controlling hyperactivity.
Therapeutic interventions include:
- Applied Behavior Analysis (ABA) to improve learning and behavior.
- Speech and language therapy to enhance communication.
- Occupational therapy for improving daily living skills.
- Sensory integration therapy to help manage sensory sensitivities.
- Parental training and family counseling for effective home care.
Nursing Management
1. Behavioral Support
- Encourage consistent routines to reduce anxiety and behavioral outbursts in the child, using structured schedules and visual cues.
- Employ positive reinforcement techniques for desirable behaviors and avoid punishment-based strategies.
- Help caregivers implement basic behavioral interventions and redirect repetitive behaviors appropriately.
2. Communication Enhancement
- Facilitate the use of augmentative and alternative communication methods (e.g., picture exchange systems, gestures).
- Collaborate with speech-language therapists to support development of functional communication.
- Speak slowly, using short, clear phrases with visual support to enhance understanding.
3. Sensory Integration Support
- Identify sensory triggers (e.g., noise, light, textures) and modify the environment to reduce sensory overload.
- Provide sensory toys, weighted blankets, or deep-pressure activities for calming sensory input.
- Ensure a calm, quiet, and safe environment, especially during transitions or new activities.
4. Family Education and Counseling
- Educate parents about the nature of autism, expected behaviors, and prognosis.
- Provide emotional support and connect families with local resources, support groups, and special education services.
- Encourage active family involvement in therapy planning and implementation.
5. Health Monitoring and Safety
- Monitor for associated conditions like epilepsy, sleep disorders, or gastrointestinal issues.
- Assess for risks such as self-harming behaviors and implement safety precautions accordingly.
- Ensure routine immunizations, nutrition, and sleep hygiene are maintained.
Section 2
Q.3
a) Define crisis intervention (2)
- Crisis intervention is an immediate, short-term, and goal-directed therapeutic technique used to support an individual facing an overwhelming psychological emergency, with the aim of restoring emotional stability, reducing distress, and preventing long-term psychological trauma.
- It focuses on resolving the immediate problem, enhancing coping mechanisms, and helping the individual return to pre-crisis level of functioning or better through active support and structured steps.
b) Explain the steps in crisis intervention (5)
Crisis intervention is a short-term, focused, and goal-directed process aimed at stabilizing an individual’s psychological condition, restoring their functioning, and preventing long-term trauma. It typically follows six structured steps as part of a therapeutic process.
Step 1: Assessment of the Crisis Situation
- The nurse begins by conducting a thorough, immediate assessment of the crisis, identifying the triggering event, emotional reactions, and severity of the distress.
- It is essential to evaluate whether the crisis is situational (e.g., job loss), maturational (e.g., adolescence), or traumatic (e.g., abuse, disaster, or sudden death).
- The nurse must assess for suicidal thoughts, violent behavior, or substance use, which may increase the urgency of intervention.
- Gathering information about the patient’s support system, coping history, recent stressors, and mental health background gives a holistic understanding of the crisis.
- Physical health must also be evaluated, as fatigue, malnutrition, or chronic illness can intensify psychological breakdown during crisis.
Step 2: Establishing Rapport and Therapeutic Relationship
- Building trust is essential, so the nurse uses active listening, empathy, open body language, and a calm, supportive tone.
- Creating a safe and non-threatening environment helps the patient feel emotionally secure and able to express thoughts without judgment.
- The nurse must show respect for the patient’s emotions, culture, beliefs, and pace, avoiding criticism or forced conversation.
- Rapport is also built by validating the patient’s feelings, using statements like “It’s okay to feel overwhelmed.”
- Trust is strengthened by being honest, consistent, and present, even during silence or moments of resistance.
Step 3: Identifying the Major Problems
- After rapport is built, the nurse helps the patient clarify the core issue that triggered the crisis, rather than focusing only on surface complaints.
- It is important to identify any secondary stressors that may be adding to the emotional overload, such as financial problems or family conflicts.
- The nurse encourages the patient to describe their thoughts and feelings openly, which may reveal underlying guilt, fear, shame, or helplessness.
- Understanding how the patient perceives the crisis is key, because the same event can be traumatic for one and manageable for another.
- At this stage, the nurse identifies maladaptive coping behaviors such as avoidance, isolation, or aggression, that may need to be redirected.
Step 4: Exploring Feelings and Developing Coping Strategies
- The nurse helps the patient identify healthy coping resources they have used in the past, including personal strengths, spiritual beliefs, or hobbies.
- Patients are guided to recognize which of their current responses are helpful, harmful, or avoidant, and how to shift toward more adaptive strategies.
- Teaching relaxation techniques, breathing exercises, and problem-solving skills helps reduce immediate anxiety and restore emotional balance.
- The nurse may encourage the patient to write down their thoughts or maintain a crisis journal to gain clarity and emotional release.
- In some cases, role-playing or rehearsing positive responses can build confidence and reduce fear of future triggers.
Step 5: Formulating an Action Plan
- The nurse collaborates with the patient to create a simple, realistic, and specific plan, which may include making calls, reconnecting with family, or setting short-term goals.
- This plan should include daily structure, activity scheduling, and setting boundaries with stressors, to rebuild stability.
- The nurse ensures that the plan includes available support systems, such as community resources, therapists, or crisis hotlines.
- Empowering the patient by involving them in the planning builds self-efficacy and confidence, which is often diminished during crisis.
- The action plan must also include safety planning, especially for patients with suicidal or violent ideation, detailing steps to seek help immediately.
Step 6: Follow-Up and Evaluation
- Follow-up care involves checking in on the patient’s progress, evaluating the effectiveness of the action plan, and making necessary adjustments.
- The nurse observes whether the patient is applying new coping strategies, showing improvement in mood, communication, and behavior.
- Continued monitoring helps detect early signs of relapse, avoidance, or recurring distress, allowing for timely intervention.
- The nurse also facilitates referrals to long-term counseling, mental health services, support groups, or rehabilitation programs for ongoing care.
- Follow-up helps in reinforcing positive behaviors, acknowledging small successes, and maintaining therapeutic contact for recovery continuity.
c) Role of nurse in crisis intervention (5)
1. Ensuring Immediate Safety and Stabilization
- The nurse plays a vital role in creating a physically and emotionally safe environment, especially when the patient is suicidal, aggressive, or experiencing extreme panic.
- It is the nurse’s responsibility to assess the patient’s risk for harm to self or others, and take preventive actions like removing sharp objects, securing the area, and implementing suicide precautions.
- The nurse may need to provide immediate first aid or medical attention, such as in cases of drug overdose, trauma, or fainting due to emotional shock.
- Nurses also ensure basic needs such as hydration, rest, and warmth are addressed, as these are often neglected during crises.
2. Rapid and Focused Crisis Assessment
- The nurse performs a quick and focused psychological assessment, identifying the type of crisis (e.g., situational, maturational, or traumatic).
- She explores the patient’s perception of the crisis, immediate concerns, current coping abilities, and social supports available.
- The nurse should also observe non-verbal signs such as withdrawal, tearfulness, pacing, or mutism, which may signal emotional distress.
- It is also important to assess for past mental health history, previous crises, and history of substance use or psychiatric illness.
3. Emotional Support and Therapeutic Communication
- The nurse must establish a therapeutic relationship by offering empathy, reassurance, and non-judgmental presence during times of distress.
- Active listening, open-ended questioning, and validating the patient’s emotions are essential to help the individual feel understood and supported.
- The nurse must provide psychological first aid, reminding the patient that strong emotional responses in crisis are normal and temporary.
- She can use calming techniques, such as speaking slowly, using the patient’s name, and maintaining appropriate physical proximity to de-escalate anxiety.
4. Helping in Problem-Solving and Goal Setting
- After initial stabilization, the nurse guides the patient in breaking down the crisis into manageable problems and prioritizing what can be controlled.
- The nurse helps the patient set short-term, achievable goals, which improves confidence and reduces helplessness.
- She facilitates the development of alternate solutions, teaching how to weigh consequences, seek help, and make healthy decisions.
- The nurse also reinforces the patient’s own past coping strengths, reminding them of earlier challenges they’ve overcome.
5. Mobilizing Social and Community Support
- The nurse identifies support persons such as family, friends, or neighbors and encourages their involvement in the recovery process.
- In case of homelessness, abuse, or abandonment, the nurse arranges emergency shelters, social services, or crisis centers.
- She collaborates with psychiatrists, social workers, and counselors to build a multidisciplinary plan for long-term support.
- Nurses also help link patients to tele-mental health services, legal aid, NGOs, and government mental health schemes.
6. Crisis Stabilization and Emotional Recovery
- The nurse helps the patient regain control over daily functioning, including self-care, nutrition, and sleep regulation.
- She reinforces constructive behaviors such as journaling, creative expression, or talking to trusted individuals, which promote healing.
- Nurses monitor for relapse signs or unresolved grief, referring patients to continued care when needed.
- She also promotes self-efficacy and positive affirmations, helping the individual believe in their strength to recover.
7. Documentation and Legal Responsibilities
- It is the nurse’s duty to document all assessments, actions taken, and the patient’s responses clearly and accurately.
- She must follow legal and ethical guidelines, especially in cases of mandatory reporting (e.g., child abuse, domestic violence).
- In case of suicide risk, the nurse initiates emergency psychiatric admission or notifies mental health authorities, while maintaining patient confidentiality as far as safety allows.
- Documentation must also include informed consent, emergency decisions, and referrals made during the intervention.
8. Health Education and Psychoeducation
- The nurse educates the patient and family about normal stress reactions, coping strategies, and the recovery process.
- She teaches the use of deep breathing, progressive muscle relaxation, and distraction techniques for anxiety relief.
- Education also includes information about medication adherence, side effects, and importance of follow-up visits.
- The nurse emphasizes early warning signs of future crisis episodes and how to respond constructively.
9. Advocacy, Counseling, and Follow-Up
- Nurses act as advocates by representing the patient’s needs and ensuring access to crisis care, medication, and psychosocial rehabilitation.
- In the role of counselor, the nurse helps patients explore their emotional reactions, regain confidence, and plan for the future.
- The nurse arranges timely follow-up appointments, phone check-ins, or home visits to monitor ongoing well-being.
- She encourages involvement in peer support groups, therapy sessions, or vocational programs as needed.
Q.4 Short notes on any five (5×5=25)
A. Delusion
Definition of Delusion
- A delusion is a fixed, false belief that is firmly held by a person, even when there is strong and undeniable evidence that contradicts the belief.
- It is considered a disturbance of thought content, where the individual has lost the ability to judge reality appropriately.
- A person with delusion cannot be convinced through reasoning, evidence, or logic that their belief is untrue, regardless of how irrational it may be.
- Delusions are commonly seen in psychotic disorders such as schizophrenia, schizoaffective disorder, and delusional disorder, and also in severe mood disorders like bipolar disorder with psychotic features.
Types of Delusion (Based on DSM-5)
1️⃣ Delusion of Persecution
- The person strongly believes that someone is trying to harm, spy, cheat, or conspire against them.
- For example, the patient may say, “The government is monitoring me through hidden cameras.”
2️⃣ Delusion of Grandeur (Grandiose Delusion)
- The person believes that they have extraordinary powers, wealth, knowledge, or identity, beyond what is real.
- For example, “I am a prophet sent to save the world,” or “I am richer than the president.”
3️⃣ Delusion of Reference
- The person believes that common events, objects, or people have a special and personal message just for them.
- For example, “The news anchor is speaking only to me,” or “That billboard is signaling something about my life.”
4️⃣ Delusion of Control (Passivity Delusion)
- The belief that the person’s thoughts, feelings, or actions are being controlled by external forces like machines or spirits.
- Example: “Aliens are controlling my arms” or “My thoughts are being inserted into my brain.”
5️⃣ Nihilistic Delusion
- The person believes that they do not exist, or that parts of their body are missing, or that the world has ended or no longer exists.
- Example: “My heart has stopped beating” or “I am already dead.”
6️⃣ Somatic Delusion
- A false belief that one’s body is diseased, deformed, infested, or malfunctioning, even when medically proven otherwise.
- Example: “There are worms inside my stomach,” or “My brain is melting.”
7️⃣ Erotomanic Delusion
- The person believes that another individual, often someone of higher status or a stranger, is in love with them.
- For example, “The film actress loves me and is sending me signals through her movies.”
Causes and Risk Factors
- Genetic factors and family history of psychotic disorders increase the risk of developing delusions.
- Neurochemical imbalances, particularly involving dopamine and serotonin, are associated with the formation of delusional thinking.
- Structural brain abnormalities, such as in the frontal lobe and limbic system, may impair judgment and increase susceptibility to psychosis.
- Psychosocial factors, such as childhood trauma, social isolation, or chronic stress, can trigger delusional episodes in vulnerable individuals.
- Substance abuse, including stimulants like cocaine or hallucinogens like LSD, can cause temporary or long-term delusions.
- Medical conditions such as dementia, brain tumors, epilepsy, or infections (like encephalitis) can produce organic delusions.
Diagnosis
- Diagnosis is based on detailed psychiatric evaluation, clinical history, and mental status examination (MSE).
- The DSM-5 (Diagnostic and Statistical Manual of Mental Disorders, 5th Edition) provides criteria for identifying delusional disorders.
- Neuroimaging and laboratory tests are used to rule out organic causes such as brain lesions, tumors, or metabolic disturbances.
- Assessment tools like Brief Psychiatric Rating Scale (BPRS) and PANSS (Positive and Negative Syndrome Scale) help quantify symptoms.
Medical Management
- Antipsychotic drugs such as haloperidol, olanzapine, risperidone, and clozapine are commonly prescribed.
- Mood stabilizers or antidepressants may be used if delusions are part of mood disorders.
- Psychotherapy and cognitive-behavioral therapy (CBT) may help reduce delusional intensity over time.
Nursing Management of Delusions
- The nurse must maintain a calm, supportive, and non-threatening environment, as patients with delusions are often anxious or fearful.
- It is essential not to argue or directly challenge the delusion, as this can provoke agitation or mistrust.
- The nurse should use therapeutic communication techniques such as reflecting the patient’s feelings and redirecting conversation to reality-based topics.
- Building trust and a therapeutic relationship is critical to help the patient feel safe and gradually accept care.
- The nurse must observe for signs of self-harm, suicidal thoughts, or violence, especially in persecutory or nihilistic delusions.
- Reality orientation should be done gently, focusing on current events, routine tasks, and grounded experiences without forceful confrontation.
- It is important to encourage medication compliance, as antipsychotics help reduce delusional intensity and associated symptoms.
- The nurse should engage the patient in structured activities, group therapy, and routines to promote social interaction and reduce fixation on delusions.
- Family education is crucial—nurses must teach family members how to respond appropriately without reinforcing or ridiculing the delusions.
- Documentation of patient behavior, verbal content, and response to treatment is vital for continued care and evaluation.
B. Discuss the cluster B personality disorder
Introduction
- Personality disorders are enduring patterns of inner experience and behavior that deviate markedly from the expectations of the individual’s culture.
- According to the DSM-5 (Diagnostic and Statistical Manual of Mental Disorders – 5th Edition), personality disorders are grouped into three clusters: A, B, and C.
- Cluster B personality disorders are characterized by dramatic, overly emotional, unpredictable, and erratic behavior, and they often cause significant interpersonal problems.
Types of Cluster B Personality Disorders
1️⃣ Antisocial Personality Disorder (ASPD)
- It is a disorder in which the individual consistently violates the rights of others, shows disregard for social rules, and lacks remorse.
- It is often associated with deceitfulness, impulsivity, irritability, aggression, and criminal behavior.
- Individuals with ASPD may appear charming and manipulative, but they are unable to sustain relationships.
- It is more common in males, especially those with a history of childhood conduct disorder.
2️⃣ Borderline Personality Disorder (BPD)
- It is characterized by intense emotional instability, distorted self-image, and fear of abandonment.
- Individuals often show impulsive behavior, self-harming tendencies, suicidal threats, and unstable relationships.
- Their mood can change rapidly, and they may experience feelings of emptiness and identity confusion.
- BPD is more frequently diagnosed in females, and is often linked to early trauma or abuse.
3️⃣ Histrionic Personality Disorder (HPD)
- Individuals with HPD display excessive emotionality and attention-seeking behavior in social settings.
- They often use physical appearance, flirtation, or dramatic expressions to gain approval and validation.
- Their emotional expressions may appear shallow or exaggerated, and they may be easily influenced by others.
- They often feel uncomfortable when they are not the center of attention.
4️⃣ Narcissistic Personality Disorder (NPD)
- It is characterized by a grandiose sense of self-importance, a constant need for admiration, and a lack of empathy for others.
- Individuals may overestimate their achievements, expect special treatment, and exploit others for personal gain.
- Criticism is poorly tolerated and may result in rage, shame, or humiliation.
- Although they appear confident, their self-esteem is often fragile and dependent on external validation.
General Features of Cluster B Personality Disorders
- Individuals often have intense and unstable emotions, which make their relationships chaotic and short-lived.
- There is a tendency toward impulsivity, manipulation, or dramatic behavior, which can create distress for others.
- Empathy is often lacking, and there may be little regard for the consequences of their actions.
- They are highly sensitive to rejection or abandonment, especially in borderline and histrionic types.
- Substance abuse, self-harm, or suicidal threats may also be present, particularly in BPD.
Causes and Risk Factors
- Genetic predisposition plays a significant role, especially in Antisocial and Borderline types.
- A history of childhood trauma, neglect, or abuse is strongly associated with Cluster B disorders.
- Dysfunctional family environment, parental rejection, or inconsistent discipline during childhood can be contributing factors.
- Neurobiological abnormalities, such as serotonin and dopamine imbalance, may influence impulsivity and aggression.
- Environmental stressors like loss of parents, chronic illness, or abandonment during early life may also trigger symptoms.
Diagnosis
- Diagnosis is made based on DSM-5 criteria using structured interviews and observation.
- Tools like Personality Diagnostic Questionnaire (PDQ-4+), Minnesota Multiphasic Personality Inventory (MMPI), and clinical history are used.
- Assessment includes evaluation of past behavior, emotional regulation, interpersonal functioning, and thought patterns.
Nursing Management of Cluster B Personality Disorders
- It is important for the nurse to build trust and therapeutic rapport while maintaining clear professional boundaries.
- The nurse should use consistent, structured, and predictable routines to reduce anxiety and manipulative behaviors.
- It is essential to practice limit-setting and behavior contracts, especially with manipulative or aggressive patients.
- The nurse should use therapeutic communication techniques such as active listening, reflection, and validation of feelings.
- Suicide risk assessment and observation are crucial, particularly in Borderline Personality Disorder with self-harming behavior.
- The nurse must provide emotional support and teach coping strategies to help manage impulsivity and stress.
- Nurses should educate the family about the disorder, its nature, prognosis, and importance of consistent support.
- Collaboration with a multidisciplinary mental health team, including psychologists, social workers, and psychiatrists, is vital.
- Nurses should monitor compliance with pharmacotherapy, such as mood stabilizers or antipsychotics, when prescribed.
- The nurse must be alert to transference or counter-transference issues and seek supervision or support when needed.
Common Treatments
- Psychotherapy (especially dialectical behavior therapy and cognitive behavior therapy) is the treatment of choice.
- Medications like SSRIs, antipsychotics, or mood stabilizers may be used to treat symptoms like depression, impulsivity, or aggression.
C. National mental health program
Introduction
- The National Mental Health Programme (NMHP) was launched by the Government of India in 1982, making it the first major public health initiative in a developing country focused entirely on mental health.
- This program was introduced due to the increasing burden of mental disorders, lack of mental health services in rural areas, and shortage of trained professionals.
- It is based on the principle of integration of mental health services with general health care services, so that even Primary Health Centers (PHCs) and Community Health Centers (CHCs) can provide basic mental health care.
- The program was formulated with the technical assistance of the World Health Organization (WHO) and the Indian Council of Medical Research (ICMR), with a long-term vision to make mental health services accessible, equitable, and affordable.
Objectives of NMHP
- The primary objective of NMHP is to ensure the availability and accessibility of minimum mental healthcare for all—especially to the most vulnerable and underprivileged sections of the population.
- It aims to integrate mental health knowledge and treatment into general healthcare systems, particularly at the grassroots level through PHCs and CHCs.
- It is designed to promote community participation and awareness, thereby reducing stigma, myths, and misconceptions about mental illness.
- Another goal is to improve the quality of life of people suffering from mental disorders through rehabilitation and follow-up care at the community level.
- It also seeks to encourage and support research in mental health, including indigenous and cost-effective models of treatment.
Key Components of NMHP
Treatment of Mental Illness – Ensuring diagnosis and management of common and severe mental disorders through public health systems.
Prevention and Promotion – Promoting mental well-being, early detection of mental health issues, and preventing complications through community involvement.
Rehabilitation of Mentally Ill Patients – Providing psychosocial and vocational rehabilitation services to help reintegrate patients into society.
Sub-Programs and Strategic Additions
1. District Mental Health Programme (DMHP)
- DMHP was introduced in 1996 as an extension of NMHP to take mental health care to the district level.
- Under DMHP, each district has a mental health team including a psychiatrist, psychologist, social worker, nurse, and health educators.
- The DMHP provides outpatient and inpatient services, school mental health programs, suicide prevention efforts, substance abuse treatment, and Information-Education-Communication (IEC) activities.
2. National Mental Health Policy (2014)
- This policy was formulated to provide a rights-based, inclusive, and community-oriented approach to mental health.
- It focuses on reducing stigma, ensuring treatment for vulnerable populations, and training health workers and caregivers.
3. Mental Healthcare Act (2017)
- Replacing the earlier Mental Health Act of 1987, this Act gives legal rights to every citizen to access mental health services and ensures that treatment is provided in a dignified and non-discriminatory manner.
Activities and Services Under NMHP/DMHP
- Provision of mental health services at the district, taluka, and village levels using existing health infrastructure.
- Training of medical officers, nurses, health workers, and ASHA workers in early identification and basic management of mental illnesses.
- Community awareness and IEC (Information, Education, Communication) campaigns to educate people about mental illness and reduce stigma.
- School mental health programs to identify behavioral problems and provide emotional support to children and adolescents.
- Suicide prevention helplines and interventions, especially targeting youth, farmers, and at-risk populations.
- De-addiction services, particularly for alcohol and substance abuse, integrated with general mental health services.
Role of Nurse in Implementation of NMHP
- The nurse plays a crucial role in assisting the psychiatrist in outpatient clinics, screening and identifying patients with mental health problems.
- It is the responsibility of the nurse to provide health education in schools, Anganwadi centers, and rural communities about stress management, suicide prevention, and emotional well-being.
- The nurse must also conduct home visits for follow-up and medication compliance, especially in chronic psychiatric patients.
- Nurses help in organizing mental health awareness camps, IEC activities, and family counseling sessions at the PHC and sub-center levels.
- Nurses are involved in record keeping, documentation, and reporting of mental health services to the district authority.
- They are also expected to train ASHAs, community health workers, and local volunteers in mental health awareness and referral systems.
- In school health programs, nurses assess emotional, behavioral, and social problems among students and refer them for counseling or treatment as needed.
Achievements of NMHP So Far
- NMHP has helped in increasing awareness and reducing stigma about mental illness in both urban and rural areas.
- It has led to the integration of mental health into the general health care system, making basic services more widely available.
- Several districts now have functional mental health teams, and many medical colleges offer psychiatric training as part of MBBS and nursing education.
- The Mental Healthcare Act 2017 has strengthened the legal rights of persons with mental illness and brought accountability in mental health care.
Challenges Faced by NMHP
- There is still a shortage of trained psychiatrists, psychologists, and psychiatric nurses, especially in rural areas.
- Stigma and misconceptions continue to prevent many people from seeking mental health care.
- Many districts still lack proper infrastructure and medication supply for psychiatric care.
- Poor inter-sectoral coordination between health, education, and social welfare departments weakens the program’s full potential.
D. Delirium
Definition
Delirium is an acute and reversible disturbance in attention, awareness, and cognition that develops over a short period of time and tends to fluctuate during the course of the day, commonly caused by medical illness, substance intoxication, withdrawal, or medication side effects.
Types of Delirium
1️⃣ Hyperactive Delirium
- This type is characterized by restlessness, agitation, mood lability, hallucinations, and delusions.
- The patient may become aggressive, combative, or extremely anxious.
2️⃣ Hypoactive Delirium
- In this type, the patient appears quiet, drowsy, lethargic, or withdrawn.
- It is more easily missed and often confused with depression or dementia.
3️⃣ Mixed Delirium
- This form includes both hyperactive and hypoactive features, alternating over a short period.
- It is the most common type observed in hospitalized elderly patients.
Etiology (Causes)
- Acute infections (e.g., UTI, pneumonia)
- Metabolic imbalances (e.g., electrolyte disturbances, hypoxia)
- Medications (e.g., anticholinergics, benzodiazepines)
- Drug or alcohol intoxication or withdrawal
- Neurological conditions (e.g., stroke, head injury)
- Sleep deprivation, pain, or environmental changes in ICU
Pathophysiology
- Delirium results from disruption in neurotransmission, especially involving acetylcholine, dopamine, and GABA.
- There is global cerebral dysfunction caused by inflammation, oxidative stress, or hypoxia.
- Reduced cerebral metabolism and cortical disconnection lead to disordered consciousness and cognition.
Clinical Manifestations
- Sudden onset of confusion
- Fluctuating attention and alertness
- Disorganized thinking
- Hallucinations or illusions
- Restlessness or lethargy
- Inappropriate or incoherent speech
- Sleep-wake cycle disturbances
Diagnostic Evaluation
- Detailed history and physical examination
- Use of screening tools (e.g., CAM – Confusion Assessment Method)
- Laboratory tests (CBC, electrolytes, liver and renal function tests)
- CT scan or MRI if neurological causes are suspected
- Urinalysis and chest X-ray to identify infections
Medical Management
1️⃣ Identify and Treat Underlying Cause
- Immediate correction of causes such as infection, hypoxia, hypoglycemia, or drug toxicity.
- Stop or replace deliriogenic medications.
2️⃣ Pharmacological Therapy
- Low-dose Haloperidol or Risperidone may be used to control agitation or hallucinations.
- Benzodiazepines (e.g., lorazepam) are reserved for alcohol withdrawal-related delirium.
- Adequate pain management with non-deliriogenic analgesics.
3️⃣ Supportive Therapy
- Ensure oxygenation, hydration, electrolyte balance, and nutritional support.
- Avoid unnecessary catheterizations and restraints.
Nursing Management
1️⃣ Assessment and Monitoring
- The nurse should regularly assess level of consciousness, attention, and orientation, using validated tools like CAM.
- Monitor vital signs, intake-output, and signs of underlying infection or distress.
2️⃣ Maintain Safety
- The nurse must ensure a safe environment, free of hazards, to prevent falls and injury.
- Side rails should be raised, and bed alarms may be used in confused patients.
3️⃣ Provide Orientation and Comfort
- It is essential to reorient the patient frequently using clocks, calendars, and familiar objects.
- Nurses should speak slowly and clearly, maintaining eye contact and reducing environmental noise.
4️⃣ Promote Rest and Sleep
- The nurse should minimize nighttime disturbances, dim the lights, and follow a routine sleep schedule.
- Provide relaxation techniques like soft music or back rubs if appropriate.
5️⃣ Support Family and Caregivers
- The nurse should educate the family about the temporary nature of delirium and encourage their presence to reduce anxiety in the patient.
- Emotional support and reassurance are important for caregivers.
6️⃣ Prevent Complications
- Nurses must ensure hydration, nutrition, mobility, and skin integrity to avoid complications like bedsores, constipation, or pneumonia.
- Early mobilization and physiotherapy may aid recovery.
E. Behaviour therapy
Definition
- Behavior therapy is a form of psychotherapy that focuses on changing maladaptive behaviors through learning principles, such as conditioning, reinforcement, and modeling.
- It is based on the idea that all behaviors are learned and therefore can be unlearned or modified through specific techniques.
Aims / Objectives of Behavior Therapy
- To identify problematic or deviant behaviors that interfere with daily life, functioning, or social relationships.
- To replace negative behaviors with more positive, adaptive responses using structured methods.
- To increase self-control, coping mechanisms, and decision-making skills in the client.
- To prevent relapse of inappropriate behaviors through reinforcement and skill-building.
Techniques of Behavior Therapy
(Also called Behavioral Techniques or Behavior Modification Strategies)
1️⃣ Positive Reinforcement
- It is a technique in which desirable behavior is followed by a rewarding stimulus, such as praise, tokens, or privileges, to increase the likelihood of the behavior being repeated.
- It is commonly used in schools, hospitals, and rehabilitation centers to promote cooperation, hygiene, social interaction, or skill development.
2️⃣ Negative Reinforcement
- It involves the removal of an unpleasant stimulus after the desired behavior occurs, thereby increasing the chances of the behavior being repeated.
- For example, a nurse might stop constant verbal prompting once the patient completes a task independently.
3️⃣ Systematic Desensitization
- It is a method used to treat phobias and anxiety by gradual exposure to the feared object or situation, combined with relaxation training.
- It starts with the least feared scenario and progresses to the most feared, while the patient is guided to remain calm.
4️⃣ Flooding (Implosion Therapy)
- It is an anxiety-reduction technique in which the patient is suddenly and intensively exposed to the feared stimulus without any gradual buildup.
- The purpose is to extinguish the fear response by realizing that the feared consequences do not occur.
5️⃣ Aversion Therapy
- It involves pairing an undesirable behavior with an unpleasant stimulus, such as an electric shock, bitter taste, or nausea-inducing drug.
- It is often used in treating addictions (e.g., alcohol, smoking) and certain paraphilic disorders.
6️⃣ Modeling (Observational Learning)
- In this technique, the client learns a new behavior by watching a role model or therapist demonstrate the desired behavior.
- It is widely used in children, social skills training, and developmental disorders.
7️⃣ Token Economy System
- This technique uses tokens (points, stars, chips) as rewards for specific behaviors, which can later be exchanged for tangible rewards like toys, snacks, or extra privileges.
- It is especially effective in institutional settings like psychiatric hospitals, classrooms, or correctional facilities.
8️⃣ Shaping (Successive Approximation)
- It is the process of reinforcing small steps that lead toward the desired behavior, especially when the final behavior is too complex to occur naturally.
- Each step is rewarded until the full behavior is achieved (e.g., teaching speech or self-care to developmentally delayed children).
9️⃣ Chaining
- Chaining involves breaking a task into smaller components and teaching each step in sequence, either from start to finish (forward chaining) or from end to beginning (backward chaining).
- It is used in teaching complex behaviors such as dressing, cooking, or academic tasks.
🔟 Time-Out Technique
- This technique involves removing the individual from a reinforcing environment for a brief period to reduce undesirable behavior.
- It is effective in managing tantrums or aggression in children, especially when done consistently.
1️⃣1️⃣ Extinction
- In extinction, the reinforcement that maintains a behavior is withdrawn, causing the behavior to gradually decrease and eventually stop.
- For example, ignoring attention-seeking behavior like whining can help reduce it over time.
Indications (Uses) of Behavior Therapy
- Phobias and anxiety disorders
- Obsessive-Compulsive Disorder (OCD)
- Post-Traumatic Stress Disorder (PTSD)
- ADHD and childhood behavior problems
- Substance abuse
- Sexual disorders including paraphilias
- Eating disorders like bulimia or anorexia
- Autism and developmental delays
- Anger management and conduct disorders
Nursing Responsibilities in Behavior Therapy
1️⃣ It is the nurse’s responsibility to build a strong therapeutic rapport with the patient, which encourages openness and trust, helping the client engage actively in behavioral interventions without fear or resistance.
2️⃣ It is essential for the nurse to assist in identifying specific target behaviors, their triggers, frequency, and consequences, using behavior charts or functional behavior assessments as part of the care plan.
3️⃣ It is necessary for the nurse to educate the patient and caregivers about the goals, expectations, and structure of behavior therapy, so they can understand the rationale behind the techniques and support the process outside therapy sessions.
4️⃣ It is the nurse’s duty to provide consistent positive reinforcement immediately after desired behaviors occur, as timely feedback enhances learning and strengthens behavior change.
5️⃣ It is important for the nurse to assist the patient during exposure-based therapies (such as systematic desensitization), by teaching and reinforcing relaxation techniques like deep breathing, progressive muscle relaxation, or guided imagery.
6️⃣ It is crucial for the nurse to help the patient transfer newly learned behaviors into daily life, by encouraging practice in real-world environments such as family settings, community, school, or workplace.
7️⃣ It is the nurse’s role to monitor for signs of distress, frustration, or emotional resistance during behavior therapy, and to report any setbacks to the therapist or multidisciplinary team for timely modifications in the treatment plan.
8️⃣ It is the nurse’s responsibility to ensure that reinforcement strategies are applied consistently across caregivers, staff, or shifts, as inconsistent application may lead to confusion and ineffective outcomes.
9️⃣ It is also necessary to provide psychoeducation about relapse prevention, helping the patient recognize early warning signs of reverting to old behaviors and encouraging the use of adaptive coping skills.
🔟 It is the nurse’s ethical responsibility to maintain confidentiality and dignity, especially when dealing with sensitive behaviors such as sexual deviations, self-harm, or substance-related issues.
F. Paraphilias
Definition
- Paraphilias are defined as mental disorders characterized by intense, persistent sexual interest or urges toward atypical objects, activities, or situations that are considered socially or legally unacceptable.
- It is a type of sexual deviation in which gratification is linked to unusual behaviors or targets that are not typically considered sexual by cultural standards.
- According to DSM-5 (Diagnostic and Statistical Manual of Mental Disorders – 5th Edition), paraphilias become paraphilic disorders when they cause distress, harm, or impairment to the individual or others.
Types of Paraphilias
1️⃣ Fetishism
- It is a paraphilic disorder in which an individual becomes sexually aroused by non-living objects (e.g., shoes, undergarments, leather items).
- It is often focused on specific parts or textures of the object, such as smoothness, softness, or shine.
2️⃣ Exhibitionism
- It is the act of gaining sexual pleasure by exposing one’s genitals to unsuspecting strangers, often in public places.
- The arousal comes not from physical contact but from the shock, surprise, or reaction of the observer.
3️⃣ Voyeurism
- This disorder involves watching others (usually strangers) who are naked, undressing, or engaging in sexual acts, without their consent.
- It is sometimes referred to as “peeping Tom behavior.”
4️⃣ Frotteurism
- It involves sexual gratification from rubbing one’s body or genitals against a non-consenting person, often in crowded places like buses or trains.
- The individual may fantasize about a relationship with the victim, although no verbal interaction typically occurs
5️⃣ Pedophilia
- It is defined by sexual attraction or activity toward prepubescent children, typically under the age of 13.
- It is considered a severe psychiatric disorder and a criminal offense in all legal systems.
6️⃣ Sexual Sadism
- It involves sexual arousal through inflicting pain, suffering, humiliation, or fear on another person.
- This can include verbal abuse, restraints, or physical punishment.
7️⃣ Sexual Masochism
- It refers to experiencing sexual arousal through receiving pain, humiliation, or punishment.
- The behavior may involve tying, beating, or verbal degradation by a partner.
8️⃣ Transvestic Disorder
- It is characterized by sexual arousal obtained by cross-dressing in clothes of the opposite gender, typically in heterosexual males.
- The behavior is associated with intense sexual excitement and not necessarily linked with gender identity disorders.
9️⃣ Bestiality (Zoophilia)
- It involves sexual activity or attraction toward animals, which is both illegal and considered highly unethical.
- It can result in serious physical injuries to the person and is also a form of animal abuse.
🔟 Necrophilia
- It is a rare and extreme paraphilia where the person has sexual fantasies or actions involving dead bodies.
- It is both a criminal act and a sign of profound psychological disturbance.
Causes of Paraphilias
- Childhood sexual abuse
- Social or emotional neglect
- Hormonal imbalance
- Brain dysfunction
- Learned deviant behavior
- Personality disorders
Signs & Symptoms of Paraphilias
- Unusual sexual urges
- Fixation on non-normal objects/acts
- Repetitive abnormal behavior
- Guilt or shame after act
- Trouble in relationships
- Risk of legal/social issues
Treatment and Management
1. Psychotherapy
- It is primarily based on cognitive-behavioral therapy (CBT), which helps individuals identify and modify harmful sexual thoughts and behaviors.
- It is useful to include aversion therapy or covert sensitization, where negative consequences are imagined to reduce arousal.
- Group therapy or supportive psychotherapy may also assist in emotional regulation and improving social skills.
2. Pharmacological Treatment
- Anti-androgen medications like medroxyprogesterone acetate (MPA) may be used to reduce libido.
- SSRIs (Selective Serotonin Reuptake Inhibitors) like fluoxetine are often used to treat compulsive sexual behavior and associated anxiety or depression.
3. Legal and Ethical Counseling
- It is necessary to provide legal counseling in cases involving pedophilia, bestiality, or other criminal offenses.
- Ethical education and behavior monitoring are essential components of long-term care.
Nursing Management
1️⃣ It is the responsibility of the nurse to establish a therapeutic and non-judgmental relationship, which helps the patient feel safe, accepted, and willing to discuss sensitive sexual thoughts or behaviors without fear of stigma.
2️⃣ It is important to assess the patient’s sexual history, behavioral patterns, and any underlying psychiatric comorbidities, such as depression, anxiety, obsessive traits, or substance abuse.
3️⃣ It is necessary to monitor the risk of harm to self or others, especially in cases like pedophilia, sadism, or voyeurism, where safety and legal issues are involved.
4️⃣ It is essential for the nurse to educate the patient and family about the nature of paraphilic disorders, including the difference between fantasies and illegal actions, and the need for long-term treatment.
5️⃣ It is the nurse’s role to encourage participation in therapy, such as Cognitive Behavioral Therapy (CBT), behavior modification, group therapy, and psychosexual education.
6️⃣ It is necessary to administer prescribed medications such as SSRIs or anti-androgens, and monitor the patient for side effects, adherence, and changes in sexual behavior.
7️⃣ It is essential to maintain strict confidentiality, as patients may fear shame or legal exposure, and confidentiality promotes trust and compliance with treatment.
8️⃣ It is important to involve the mental health team, including the psychiatrist, clinical psychologist, and social worker, for coordinated and multidisciplinary care.
9️⃣ It is the nurse’s duty to observe for signs of emotional distress or suicidal ideation, especially if the patient feels guilt or hopelessness related to their condition.
🔟 It is beneficial to help the patient develop healthy social and interpersonal skills, replacing deviant sexual behavior with appropriate outlets for emotional expression and intimacy.