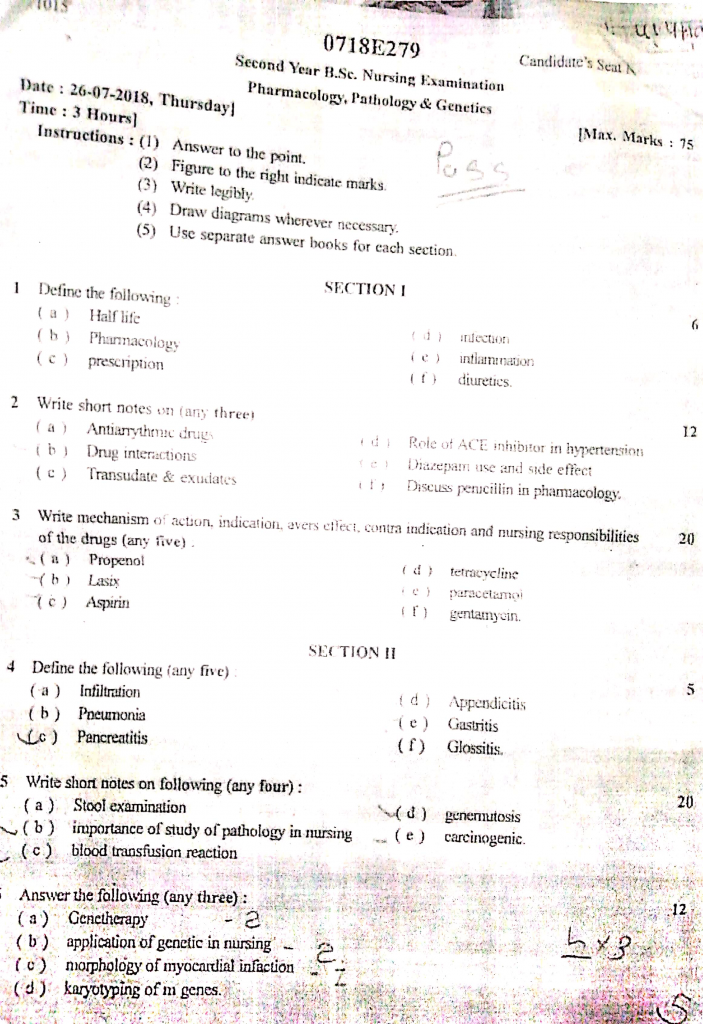
26/07/2018-PHARMA,PATHO,GENETICS-JUHI DONE-PAPER NO.7
PHARMA,PATHO,GENETICS-PAPER SOLUTION NO.7
Section 1
Q.1 Define the following (6)
a) Half life
- Half-life is the amount of time required for the concentration of a drug in the bloodstream to decrease by 50% after administration.
- It is an important pharmacokinetic property that helps determine dosing frequency, duration of drug action, and the time required to reach steady-state levels or eliminate the drug from the body. A drug with a short half-life requires frequent dosing, while one with a long half-life stays in the body for an extended period.
b) Pharmacology
- Pharmacology is the branch of medical science that deals with the study of drugs, including their origin, chemical composition, biological effects, mechanisms of action, therapeutic uses, side effects, interactions, and toxicology.
c) Prescription
- A prescription is a written, electronic, or verbal order by a licensed medical practitioner, such as a doctor or nurse practitioner, directing the dispensing and administration of specific medications or treatments to a patient.
- It includes essential details such as the patient’s name, date, drug name, dosage, route, frequency, duration, and special instructions, and must be signed and authorized by the prescribing professional to ensure legal and safe medication administration.
d) Infection
- Infection is the invasion and multiplication of pathogenic microorganisms such as bacteria, viruses, fungi, or parasites within the body tissues, which may lead to tissue damage, immune response, and clinical illness.
- It can be localized (confined to one area) or systemic (spread throughout the body), and commonly presents with signs such as fever, redness, swelling, pain, warmth, and pus formation, depending on the site and severity of the infection.
e) Inflammation
- Inflammation is the body’s natural protective response to injury, infection, or harmful stimuli, characterized by redness, heat, swelling, pain, and loss of function at the affected site.
- It occurs due to the activation of immune cells, blood vessels, and molecular mediators, and its purpose is to eliminate the cause of injury, clear out damaged tissues, and initiate tissue repair. Inflammation can be acute (short-term) or chronic (long-term) depending on the nature and duration of the stimulus.
f) Diuretics
- Diuretics are a class of drugs that promote the removal of excess water and electrolytes from the body by increasing urine production through the kidneys.
- They are commonly used in the treatment of hypertension, heart failure, edema, renal disorders, and certain liver conditions, and are classified into types such as loop diuretics (e.g., furosemide), thiazide diuretics (e.g., hydrochlorothiazide), and potassium-sparing diuretics (e.g., spironolactone).
Q.2 Write short notes (any three) (12)
a) Antiarrhythmic drugs
Definition
- It is a group of drugs that is used to correct or control abnormal electrical activity in the heart, which may cause irregular heart rhythms (arrhythmias).
- It is used specifically to treat conditions like atrial fibrillation, ventricular tachycardia, and supraventricular tachycardia, among others.
- It acts by altering the ionic flow across cardiac cell membranes, affecting depolarization and repolarization processes of myocardial cells.
Classification – Vaughan Williams Classification
Antiarrhythmic drugs are divided into five classes (I–V) :
Class I – Sodium Channel Blockers
- These drugs block sodium (Na⁺) channels during the depolarization phase (Phase 0) of the cardiac action potential, altering impulse conduction.
Class IA (Moderate Na⁺ block, prolong APD)
- These drugs slow conduction and prolong repolarization, increasing QT interval.
- They are used in atrial fibrillation, flutter, and ventricular tachycardia.
- Examples : Quinidine, Procainamide, Disopyramide
Class IB (Weak Na⁺ block, shorten APD)
- These drugs preferentially affect ischemic or depolarized Purkinje and ventricular tissue.
- They are used in ventricular arrhythmias, especially post-MI.
- Examples : Lidocaine (IV), Mexiletine (oral)
Class IC (Strong Na⁺ block, no change in APD)
- These drugs markedly slow conduction velocity but have minimal effect on repolarization.
- They are used in life-threatening ventricular arrhythmias.
- Examples : Flecainide, Propafenone
Class II – Beta-Adrenergic Blockers
- These drugs inhibit sympathetic stimulation of the heart by blocking β1-adrenergic receptors.
- They reduce heart rate, AV node conduction, and automaticity, especially useful in stress-induced arrhythmias.
- Commonly used in atrial fibrillation, atrial flutter, and post-MI arrhythmias.
- Examples: Propranolol, Atenolol, Metoprolol, Esmolol
Class III – Potassium Channel Blockers
- These drugs prolong repolarization (Phase 3) by blocking potassium channels.
- They increase the duration of action potential and effective refractory period, preventing re-entry arrhythmias.
- Used in both atrial and ventricular arrhythmias, especially ventricular tachycardia and fibrillation.
- Examples: Amiodarone, Sotalol, Dofetilide, Ibutilide
Class IV – Calcium Channel Blockers (Non-DHP)
- These drugs block L-type calcium channels, particularly affecting the SA and AV nodes.
- They slow conduction, decrease heart rate, and prolong the refractory period in nodal tissue.
- Indicated for SVT (supraventricular tachycardia), atrial fibrillation, and atrial flutter.
- Examples: Verapamil, Diltiazem
Class V – Miscellaneous Agents
- These drugs do not fall under the first four classes but are widely used to treat arrhythmias.
a) Adenosine
- It activates A1 adenosine receptors in the AV node → hyperpolarization → slows conduction.
- Used in paroxysmal supraventricular tachycardia (PSVT).
- Has an ultra-short half-life (~10 seconds).
b) Digoxin
- Increases vagal tone, slows AV node conduction.
- Used in atrial fibrillation with heart failure.
c) Magnesium sulfate
- Stabilizes myocardial cell membranes and is used in torsades de pointes and digoxin toxicity.
Mechanism of Action
Class I
- It blocks sodium channels, which are responsible for phase 0 depolarization → slows conduction velocity in myocardial tissue.
- Subtypes IA, IB, IC differ in the strength of sodium channel blockade and effect on repolarization.
Class II
- It blocks beta-adrenergic receptors, reducing catecholamine effects → slows SA and AV node conduction and decreases heart rate.
Class III
- It blocks potassium channels, prolonging repolarization and increasing action potential duration → prevents premature impulses.
Class IV
- It inhibits L-type calcium channels, especially in AV node → slows conduction and prolongs refractory period in nodal tissue.
Class V
- Adenosine opens K⁺ channels and blocks AV nodal conduction transiently.
- Digoxin enhances vagal activity.
- Magnesium affects Ca²⁺ and Na⁺ movement across membranes.
Indications of Antiarrhythmic Drugs
- It is used to control rate and rhythm in atrial fibrillation and atrial flutter.
- It is indicated for ventricular tachycardia, especially post-MI.
- It is used in supraventricular tachycardia (SVT) and AV nodal reentrant tachycardia (AVNRT).
- It is used in emergency management of ventricular fibrillation and torsades de pointes.
- It is given in digitalis-induced arrhythmias or arrhythmias secondary to electrolyte imbalance.
Adverse Effects
- It may lead to new or worsened arrhythmias (proarrhythmia) due to altered conduction pathways.
- It can cause sinus bradycardia and heart block, particularly with beta-blockers and calcium channel blockers.
- Hypotension, dizziness, and syncope are common due to decreased cardiac output.
- Amiodarone can cause pulmonary fibrosis, hepatotoxicity, thyroid dysfunction (both hypo- and hyperthyroidism), corneal deposits, and skin pigmentation.
- Beta-blockers may cause bronchospasm, fatigue, depression, and erectile dysfunction.
- Quinidine may lead to cinchonism (tinnitus, headache, nausea, visual disturbance).
Contraindications
- It is contraindicated in severe bradycardia or complete heart block without a pacemaker.
- Class IC drugs are not used post-myocardial infarction due to the risk of sudden cardiac death.
- Beta-blockers are avoided in bronchial asthma or severe chronic obstructive pulmonary disease (COPD).
- Calcium channel blockers like verapamil are avoided in heart failure with reduced ejection fraction.
- It should not be used without correction of electrolyte disturbances like hypokalemia or hypomagnesemia, as they increase toxicity risk.
Nursing Responsibilities
✅ 1. Monitoring and Assessment
- It is essential for the nurse to monitor the patient’s ECG before, during, and after administering antiarrhythmic drugs, to detect any changes in rhythm or new onset of arrhythmia.
- The nurse should assess the baseline heart rate, blood pressure, and electrolyte levels, especially potassium and magnesium levels.
- It is necessary for the nurse to observe the patient closely for signs of bradycardia, hypotension, syncope, or QT prolongation, especially during IV infusion.
- The nurse must monitor for side effects like vision changes, skin discoloration, or respiratory symptoms, particularly in patients on Amiodarone.
✅ 2. Drug Administration Care
- It is the nurse’s responsibility to follow the correct dose and rate of administration, especially for IV medications like Lidocaine or Adenosine, which act very quickly.
- The nurse must ensure that emergency resuscitation equipment is available at bedside while administering IV antiarrhythmic drugs.
- It is important for the nurse to dilute and flush IV medications properly, especially Adenosine which is given as a rapid IV push followed by a saline flush.
- The nurse should double-check the drug-drug interactions, such as avoiding combining beta-blockers with calcium channel blockers.
✅ 3. Patient Education
- It is important to educate the patient about reporting signs of dizziness, chest pain, or palpitations, which may indicate arrhythmia recurrence.
- The nurse should counsel the patient on adherence to prescribed dosing schedule, especially with drugs like Amiodarone, which require long-term therapy.
- The nurse must inform the patient about periodic thyroid, liver, and eye testing, particularly for those on Amiodarone.
- It is essential to advise the patient to avoid over-the-counter drugs that can affect heart rhythm, like decongestants.
b) Durg interaction
Definition of Drug Interaction
- Drug interaction is defined as a condition in which the effect of a drug is altered—either increased, decreased, or modified—due to the presence of another drug, food, drink, or medical condition in the patient’s body.
- It is considered clinically important because it can either enhance the therapeutic effect, reduce drug efficacy, or even cause dangerous toxic reactions.
- These interactions are critical to nursing care, especially in elderly patients, ICU setups, or chronic illnesses, where polypharmacy is common.
Classification of Drug Interactions
1️⃣ Drug–Drug Interactions (DDI)
- This occurs when two or more drugs react with each other inside the body, causing modification in the absorption, metabolism, action, or elimination of one or both drugs.
- For example, aspirin and warfarin together can cause increased risk of bleeding due to additive anticoagulant effect.
- Another example is rifampicin decreasing the effectiveness of oral contraceptives by increasing their metabolism in the liver.
- Nurses must be cautious when administering multiple cardiac, antiepileptic, or psychiatric medications, as these often have known DDIs.
2️⃣ Drug–Food Interactions
- These occur when food components affect the pharmacological action or absorption of drugs in the body.
- For example, grapefruit juice inhibits the CYP3A4 enzyme in the liver, leading to increased plasma levels of drugs like nifedipine or simvastatin, which may result in toxicity.
- Calcium-containing foods or milk interfere with the absorption of tetracycline or ciprofloxacin by forming insoluble complexes.
- Nurses should instruct patients on when to take medications with food or on an empty stomach to avoid such interactions.
3️⃣ Drug–Alcohol Interactions
- When alcohol is consumed with certain drugs, it may enhance or oppose the drug’s pharmacological effects, sometimes causing CNS depression or hepatotoxicity.
- For instance, alcohol taken with benzodiazepines (like diazepam or lorazepam) can lead to respiratory depression, excessive sedation, and confusion.
- Chronic alcohol consumption may induce liver enzymes, leading to faster metabolism of drugs like warfarin or phenytoin, reducing their effect.
- Nurses should advise patients to avoid alcohol entirely when on CNS depressants or hepatotoxic drugs.
4️⃣ Drug–Disease Interactions
- These interactions occur when a drug adversely affects a pre-existing medical condition, making the disease worse.
- For example, non-selective beta-blockers like propranolol can worsen asthma symptoms by causing bronchoconstriction.
- NSAIDs like ibuprofen may worsen kidney function in patients with chronic renal disease.
- Nurses must assess the patient’s comorbidities before administering medications and monitor for any disease-specific complications.
5️⃣ Drug–Lab Test Interactions
- Some drugs can interfere with laboratory test results, causing false positives or false negatives.
- For example, high doses of vitamin C may give a false-negative result in glucose urine tests, and levodopa can interfere with glucose monitoring kits.
- This can lead to misdiagnosis or unnecessary treatment, hence nurses should always document the drugs taken before testing and notify the lab team.
Mechanisms of Drug Interaction
1️⃣ Pharmacokinetic Interactions – Involves changes in absorption, distribution, metabolism, or excretion of drugs.
2️⃣ Pharmacodynamic Interactions – Occur when two drugs act at the same or related receptor sites, producing additive, synergistic, or antagonistic effects.
3️⃣ Enzyme Induction/Inhibition – Some drugs induce or inhibit cytochrome P450 enzymes, leading to altered drug levels (e.g., rifampicin induces, ketoconazole inhibits).
Clinical Consequences of Drug Interactions
- It may lead to increased toxicity or adverse effects, such as nephrotoxicity when aminoglycosides are combined with diuretics.
- It can cause treatment failure, such as antacids reducing the effectiveness of iron supplements.
- It can result in unexpected therapeutic effects, such as enhanced sedation with combination of CNS depressants.
- In some cases, it may require dose adjustment, substitution, or careful monitoring.
Nursing Responsibilities in Preventing Drug Interactions
1️⃣ The nurse should always review the patient’s complete medication history, including prescribed, over-the-counter, herbal, and dietary supplements.
2️⃣ The nurse must use drug interaction checkers or consult with pharmacists or drug manuals before administering new medications.
3️⃣ It is important for the nurse to educate patients about avoiding certain food items (like grapefruit, dairy, caffeine) while taking specific medications.
4️⃣ The nurse must observe the patient closely for any signs of increased side effects or reduced drug effectiveness and report immediately.
5️⃣ The nurse should ensure that medications are given at appropriate time intervals, especially when drug absorption is affected by food or other drugs.
6️⃣ The nurse should document and report any suspected drug interaction in the patient’s record for clinical safety and future reference.
7️⃣ The nurse must monitor vital signs, lab values, and therapeutic drug levels when high-risk combinations are being used (e.g., digoxin + diuretics).
8️⃣ The nurse should counsel patients to avoid self-medication, as over-the-counter drugs can interact dangerously with prescribed drugs.
c) Transduate and exudates
- It is important to differentiate between transudate and exudate when examining abnormal fluid collections in body cavities such as pleura, peritoneum, or pericardium, as they help in diagnosing underlying disease conditions.
- These fluids are collected and analyzed during procedures such as paracentesis (for ascitic fluid), thoracentesis (for pleural fluid), and pericardiocentesis (for pericardial fluid).
TRANSUDATE
Definition
It is a type of fluid that accumulates in a body cavity due to disturbances in the balance of hydrostatic pressure and oncotic pressure across the capillary wall without any damage to the vascular membrane.
Cause (Etiology)
- It is commonly caused by systemic, non-inflammatory conditions.
- It results from increased hydrostatic pressure (as seen in congestive heart failure) or decreased oncotic pressure (as in nephrotic syndrome or liver cirrhosis).
Characteristics
- It is usually clear, pale yellow, and watery in appearance.
- It has very low protein content (usually < 3.0 g/dL).
- It contains very few or no white blood cells or red blood cells.
- It has low specific gravity (less than 1.012).
- It has low levels of lactate dehydrogenase (LDH).
- It does not clot because it contains no or very little fibrinogen.
- It has low cholesterol and low albumin levels.
Pathophysiology
- It forms when there is an imbalance in Starling forces—either increased hydrostatic pressure pushes more fluid out, or decreased plasma oncotic pressure reduces the pull of fluid back into capillaries.
- The capillary walls remain intact, so large proteins and cells do not pass into the interstitial or body cavity spaces.
Common Conditions Associated
- Congestive heart failure – due to increased venous pressure.
- Cirrhosis of liver – due to decreased albumin and portal hypertension.
- Nephrotic syndrome – due to massive protein loss in urine.
- Hypoalbuminemia – due to protein malnutrition.
- Peritoneal dialysis – due to osmotic changes.
EXUDATE
Definition
It is a type of fluid that escapes into tissues or cavities due to inflammation, infection, malignancy, or injury causing increased capillary permeability and damage to the vascular membrane.
Cause (Etiology)
- It occurs in response to local tissue injury or inflammation.
- The inflammatory process leads to dilation of blood vessels and increased permeability of the endothelial lining, allowing plasma proteins, leukocytes, and even red blood cells to leak out.
Characteristics
- It appears cloudy, turbid, or opaque depending on the type of infection or inflammation.
- It contains high levels of protein (usually > 3.0 g/dL).
- It is rich in inflammatory cells, including neutrophils, lymphocytes, or macrophages.
- It has high specific gravity (greater than 1.020).
- It has elevated lactate dehydrogenase (LDH) due to cellular damage.
- It may clot on standing due to high fibrinogen content.
- It often contains bacteria, cancer cells, or other pathological agents on cytology or culture.
Pathophysiology
- During inflammation or infection, cytokines and inflammatory mediators such as histamine and interleukins cause damage to vascular endothelium.
- This allows escape of plasma proteins, immunoglobulins, WBCs, and other large molecules into the extravascular space, resulting in exudate.
Common Conditions Associated
- Bacterial pneumonia – exudative pleural effusion.
- Tuberculosis – caseating exudate in lungs or pleura.
- Rheumatoid arthritis – joint exudate in synovium.
- Cancer – malignant pleural or peritoneal effusion.
- Peritonitis – exudate in abdominal cavity.
- Pancreatitis – enzyme-rich inflammatory exudate.
d) Role of ACE inhibitors in hypertension
✅ 1. Reduction of Systemic Vascular Resistance
- It is one of the primary roles of ACE inhibitors to reduce systemic vascular resistance by blocking the conversion of angiotensin I to angiotensin II, a potent vasoconstrictor.
- It is this vasodilatory effect that reduces peripheral vascular tone, helping to lower both systolic and diastolic blood pressure.
- It is also significant that by decreasing vascular resistance, the afterload on the heart is reduced, which facilitates easier blood ejection and decreases myocardial oxygen demand.
✅ 2. Decrease in Aldosterone Secretion and Volume Overload
- It is observed that ACE inhibitors decrease the secretion of aldosterone, which limits sodium and water retention in the renal tubules.
- It is through this action that they help reduce blood volume and control fluid overload, which is common in hypertensive and heart failure patients.
- It is also true that by preventing potassium loss, ACE inhibitors reduce the risk of hypokalemia, unlike many other diuretics used in hypertension.
✅ 3. Prevention of Vascular and Cardiac Remodeling
- It is known that chronic hypertension leads to hypertrophy and remodeling of blood vessels and cardiac muscle, which worsens cardiovascular function over time.
- It is by reducing angiotensin II levels that ACE inhibitors prevent these pathological structural changes, especially in the myocardium and arteries.
- It is crucial to note that this role improves long-term cardiovascular outcomes, including reducing the risk of left ventricular hypertrophy and heart failure.
✅ 4. Renal Protection in Hypertensive Diabetic Patients
- It is evident that ACE inhibitors dilate the efferent arterioles of the glomeruli, thus reducing glomerular hypertension and protecting kidney filtration mechanisms.
- It is essential to understand that in diabetic patients with microalbuminuria or proteinuria, ACE inhibitors slow the progression of nephropathy.
- It is further beneficial that this nephroprotective effect helps delay the onset of end-stage renal disease (ESRD) in both diabetic and hypertensive individuals.
✅ 5. Improvement of Cardiac Function in Hypertensive Heart Failure
- It is well-documented that ACE inhibitors improve cardiac output by reducing both preload (venous return) and afterload (resistance to ejection).
- It is this dual benefit that makes them cornerstone therapy in hypertensive patients with congestive heart failure, especially those with reduced ejection fraction.
- It is also vital to note that ACE inhibitors reduce hospitalization and mortality in chronic heart failure associated with hypertension.
✅ 6. Enhancement of Bradykinin-Mediated Vasodilation
- It is known that ACE inhibitors prevent the breakdown of bradykinin, a natural vasodilator, thereby enhancing its effects on blood vessels.
- It is this mechanism that contributes to additional vasodilation, further reducing blood pressure beyond the renin-angiotensin system blockade.
- It is also the reason for one of the major side effects — dry cough — due to bradykinin accumulation in the lungs.
✅ 7. Prevention of Cardiovascular Complications
- It is clearly established that ACE inhibitors significantly reduce the risk of stroke, myocardial infarction, and cardiovascular death in hypertensive patients.
- It is their ability to protect end organs such as the brain, heart, and kidneys that makes them superior to some other antihypertensive drugs.
- It is particularly important in high-risk populations (e.g., diabetics, elderly) where vascular events are more common.
✅ 8. Compatibility with Combination Therapy
- It is often necessary to combine ACE inhibitors with other drugs, such as diuretics, calcium channel blockers, or beta-blockers when monotherapy does not control BP effectively.
- It is observed that they work synergistically with thiazide diuretics, reducing side effects and improving blood pressure control.
- It is essential to understand that this flexibility allows physicians to tailor treatment according to patient comorbidities and response.
✅ 9. Use in Post-Myocardial Infarction Hypertension
- It is strongly recommended to use ACE inhibitors after myocardial infarction, especially in hypertensive patients with reduced left ventricular function.
- It is through their anti-remodeling and hemodynamic effects that they improve long-term cardiac survival, preventing the development of heart failure.
- It is also shown in clinical trials that early initiation of ACE inhibitors post-MI reduces infarct size, improves recovery, and enhances prognosis.
✅ 10. Favorable Metabolic Profile
- It is a key advantage of ACE inhibitors that they have neutral or beneficial effects on insulin sensitivity and lipid profile, unlike beta-blockers or diuretics.
- It is this property that makes ACE inhibitors suitable for patients with hypertension associated with type 2 diabetes or metabolic syndrome.
- It is also relevant that they do not increase uric acid levels, which is useful in hypertensive patients with gout.
e) Dizepam use and side effects
USES OF DIAZEPAM
1️⃣ Use in Anxiety Disorders
- It is widely used in the treatment of generalized anxiety disorder (GAD), panic disorder, and acute anxiety episodes.
- It is effective due to its anxiolytic (anti-anxiety) action which calms excessive brain activity.
2️⃣ Use in Acute Alcohol Withdrawal
- It is given to manage symptoms such as tremors, agitation, hallucinations, and risk of seizures during alcohol withdrawal.
- It helps prevent delirium tremens by stabilizing the CNS.
3️⃣ Use in Preoperative Sedation
- It is administered before surgery or diagnostic procedures to produce sedation, reduce anxiety, and cause amnesia.
- It helps the patient feel calm and relaxed before medical interventions.
4️⃣ Use in Status Epilepticus and Seizures
- It is an emergency drug used intravenously or rectally to control status epilepticus (continuous seizures).
- It enhances GABA activity, helping to stop seizure activity rapidly.
5️⃣ Use as a Muscle Relaxant
- It is used in treating muscle spasms, spasticity, and tetanus due to its central muscle-relaxing effects.
- It is effective in conditions like multiple sclerosis, cerebral palsy, and back injuries.
6️⃣ Use in Insomnia (Short-Term)
- t is prescribed for short-term relief of insomnia, especially when related to anxiety or stress.
- It induces sleep and reduces night-time awakenings, but long-term use is avoided.
7️⃣ Use in Febrile Seizures in Children
- Rectal diazepam is used in children during high fever-induced seizures.
- It helps quickly terminate convulsions and prevent brain damage.
8️⃣ Use in Palliative and Terminal Care
- It is administered to reduce terminal agitation, severe anxiety, or dyspnea in end-of-life care.
- It promotes patient comfort and dignity in the final stage of life.
SIDE EFFECTS OF DIAZEPAM
1️⃣ Drowsiness and Sedation
- It is one of the most common side effects, especially in the initial phase of therapy or after high doses.
- It causes sleepiness, mental dullness, and reduced alertness, which can interfere with daily activities or driving.
2️⃣ Dizziness and Lightheadedness
- It is caused due to the CNS depressant effect of diazepam.
- Patients may feel faint, weak, or unsteady, particularly when standing suddenly, leading to risk of falls.
3️⃣ Cognitive Impairment and Confusion
- It may result in slowed thinking, poor concentration, and memory issues, especially in the elderly.
- Confusion and disorientation may occur even after short-term use in sensitive individuals.
4️⃣ Muscle Weakness
- As a muscle relaxant, diazepam may cause weakness and fatigue in skeletal muscles, especially in bedridden patients.
- It may impair mobility and daily functioning in some cases.
5️⃣ Respiratory Depression
- High doses or IV administration can cause slowed or shallow breathing, particularly when combined with other CNS depressants (like opioids or alcohol).
- This can be life-threatening in overdose situations.
6️⃣ Dependence and Withdrawal Symptoms
- Long-term use can lead to physical and psychological dependence.
- Abrupt discontinuation may cause rebound anxiety, insomnia, agitation, or seizures.
7️⃣ Paradoxical Reactions
- Rarely, some individuals (especially children or elderly) may experience increased anxiety, aggression, agitation, or hallucinations.
- These are called paradoxical effects because they are opposite to the expected calming effect.
8️⃣ Ataxia and Unsteady Gait
- It can impair motor coordination leading to balance problems and clumsiness.
- It increases the risk of falls or injury, especially in older adults.
9️⃣ Gastrointestinal Disturbances
- It may cause nausea, dry mouth, constipation, or abdominal discomfort in some patients.
- These effects are generally mild but may affect compliance with medication.
🔟 Cardiovascular Effects
- IV diazepam may cause hypotension (low BP), bradycardia (slow heart rate), or palpitations.
- Monitoring is essential during IV use in critically ill or elderly patients.
f) Discuss penicillin in pharmacology
Introduction to Penicillin
- Penicillin is a group of β-lactam antibiotics that are primarily used to treat bacterial infections caused by Gram-positive organisms, and some Gram-negative bacteria.
- It was the first antibiotic discovered by Alexander Fleming in 1928, derived from the fungus Penicillium notatum.
- It acts by inhibiting bacterial cell wall synthesis, making it bactericidal in action.
Classification of Penicillin
1️⃣ Natural penicillins
Natural penicillin such as Penicillin G and Penicillin V, are the earliest discovered antibiotics mainly effective against Gram-positive bacteria but are not resistant to penicillinase enzymes.
2️⃣ Penicillinase-resistant penicillins
Penicillinase resistant penicillins, including Methicillin, Oxacillin, and Cloxacillin, are modified to resist degradation by penicillinase and are specifically used for staphylococcal infections.
3️⃣ Aminopenicillins
Aminopenicillins like Ampicillin and Amoxicillin, are broad-spectrum penicillins that are active against both Gram-positive and certain Gram-negative organisms but are still penicillinase-sensitive.
4️⃣ Extended-spectrum penicillins
Such as Piperacillin and Ticarcillin, are effective against a wider range of Gram-negative bacteria including Pseudomonas aeruginosa and are used in serious hospital-acquired infections.
5️⃣ β-lactamase inhibitor combinations
Like Amoxicillin with Clavulanic acid or Piperacillin with Tazobactam, are formulated to overcome bacterial resistance by inhibiting the β-lactamase enzyme.
Mechanism of Action
1️⃣ Penicillin acts by binding to Penicillin Binding Proteins (PBPs) located inside the bacterial cell wall.
2️⃣ These PBPs are essential enzymes that help in cross-linking peptidoglycan chains, which provide rigidity and structure to bacterial cell walls.
3️⃣ When penicillin binds to PBPs, it inhibits the final transpeptidation step, preventing cell wall synthesis.
4️⃣ The bacterial cell wall becomes weak and unstable, leading to cell lysis and death, especially in actively growing bacteria.
5️⃣ Thus, penicillin is considered a time-dependent bactericidal agent.
4. Indications / Therapeutic Uses
- Treatment of streptococcal infections (e.g., pharyngitis, cellulitis)
- Treatment of pneumonia, otitis media, sinusitis
- Management of gonorrhea and syphilis
- Used in bacterial endocarditis prophylaxis
- Effective against diphtheria, anthrax, and tetanus (with supportive care)
- Used in combination therapy for H. pylori infections (e.g., Amoxicillin)
Adverse Effects
- Allergic reactions (rash, urticaria, anaphylaxis)
- Gastrointestinal upset (nausea, vomiting, diarrhea)
- Superinfection (e.g., Candidiasis)
- Hemolytic anemia (rare)
- Seizures at high doses (especially in renal failure patients)
Contraindications
- Known hypersensitivity to penicillin or other β-lactam antibiotics
- History of anaphylaxis due to penicillin use
- Use cautiously in patients with renal impairment or epilepsy
Nursing Responsibilities
1️⃣ The nurse must carefully check for any history of allergy to penicillin or other β-lactam antibiotics before administering the drug, as allergic reactions can be life-threatening.
2️⃣ The nurse should observe the patient for at least 30 minutes after parenteral administration to monitor for any signs of immediate hypersensitivity or anaphylactic shock.
3️⃣ The nurse must ensure that the complete prescribed course is taken by the patient, even if symptoms subside early, to avoid antibiotic resistance or relapse of infection.
4️⃣ The nurse should monitor the patient for signs of superinfection, such as oral thrush, vaginal candidiasis, or diarrhea, especially with prolonged use.
5️⃣ It is important for the nurse to educate the patient to report any signs of rash, itching, or breathing difficulty immediately to the healthcare provider.
6️⃣ The nurse should adjust dosage carefully in patients with renal impairment, and monitor renal function tests as penicillin is primarily excreted by the kidneys.
7️⃣ The nurse must administer penicillin on an empty stomach, especially Penicillin V, unless otherwise prescribed, to enhance absorption.
8️⃣ The nurse must check for possible drug interactions, such as with oral contraceptives (may reduce effectiveness) or methotrexate (increased toxicity).
9️⃣ The nurse should be aware of specific storage conditions—some penicillin injections require refrigeration or reconstitution before use.
🔟 The nurse should document the route, dose, time of administration, and any patient reactions clearly in the medical record.
Q.3 Write the mechanism of action, indication, adverse effects, contraindications and nursing responsibilies (any five) (20)
a) Propenol
Mechanism of Action of Propranolol
- It is a non-selective beta-adrenergic receptor antagonist, which means it blocks both β1 and β2 receptors located in the heart, lungs, and blood vessels.
- By blocking β1 receptors, it decreases the heart rate, myocardial contractility, and cardiac output, which results in a reduction in blood pressure.
- It also reduces renin release from the kidneys, which leads to a decrease in angiotensin II and aldosterone production, thereby lowering blood pressure and fluid retention.
- By blocking β2 receptors in bronchial smooth muscle, it can cause bronchoconstriction, which is why it must be used cautiously in asthma patients.
- It has membrane-stabilizing activity similar to anti-arrhythmic drugs, making it effective in treating arrhythmias.
- It crosses the blood-brain barrier and affects the central nervous system, leading to reduced tremors and prevention of migraine headaches.
Indications of Propranolol
- Hypertension (High Blood Pressure)
- Angina pectoris (Chest Pain)
- Cardiac arrhythmias (e.g., atrial fibrillation)
- Myocardial infarction (Post-MI management)
- Migraine prophylaxis
- Essential tremors
- Hyperthyroidism symptoms (e.g., tachycardia)
- Anxiety (off-label use)
Adverse Effects of Propranolol
- Bradycardia (slow heart rate)
- Hypotension (low blood pressure)
- Bronchospasm or breathing difficulty (especially in asthma patients)
- Fatigue and dizziness
- Depression or mood changes
- Cold extremities (due to vasoconstriction)
- Impotence or sexual dysfunction
- Sleep disturbances or vivid dreams
Contraindications of Propranolol
- Bronchial asthma or COPD (due to risk of bronchospasm)
- Severe bradycardia or heart block
- Hypotension or cardiogenic shock
- Uncompensated heart failure
- Hypersensitivity to propranolol
- Peripheral arterial disease (with caution)
Nursing Responsibilities While Administering Propranolol
1️⃣ Assessment & Monitoring
- It is important for the nurse to assess baseline vital signs, especially heart rate and blood pressure before administering the drug.
- The nurse must hold the dose and notify the physician if pulse is below 60 bpm or if systolic BP is less than 90 mmHg.
- The nurse should closely monitor for signs of heart failure, such as edema, dyspnea, weight gain, or crackles on auscultation.
2️⃣ Patient Safety
- It is necessary for the nurse to advise the patient to rise slowly from sitting or lying position to prevent orthostatic hypotension.
- The nurse must ensure that fall precautions are in place for elderly or weak patients receiving propranolol.
3️⃣ Respiratory Care
- It is essential to monitor for any signs of bronchospasm, wheezing, or breathing difficulty, especially in patients with a history of asthma or lung disease.
4️⃣ Patient Education
- The nurse should educate the patient not to abruptly stop the medication, as it may lead to rebound hypertension or angina.
- It is important to teach the patient about potential side effects like dizziness, fatigue, and cold extremities.
- The nurse must advise the patient to check pulse daily and report any unusual slowing.
5️⃣ Drug Interaction Monitoring
- The nurse should check for drug interactions with calcium channel blockers, digoxin, or insulin (as propranolol may mask hypoglycemia symptoms).
6️⃣ Lab and Follow-up
- The nurse should monitor blood glucose levels in diabetic patients as propranolol may mask signs of hypoglycemia.
- Liver function tests may be required in long-term use to evaluate hepatotoxicity.
b) Lasix
Mechanism of Action of Lasix (Furosemide)
- It is a potent loop diuretic that works primarily in the ascending limb of the loop of Henle in the nephron of the kidney.
- It inhibits the sodium-potassium-chloride (Na⁺/K⁺/2Cl⁻) co-transporter, which blocks the reabsorption of sodium and chloride ions.
- This action leads to increased excretion of sodium, chloride, potassium, calcium, and water, causing a powerful diuretic (urine-producing) effect.
- It results in a rapid decrease in blood volume and preload, which helps in reducing blood pressure and relieving pulmonary congestion or edema.
- It causes vasodilation of the blood vessels in the kidneys even before diuresis begins, helping to improve renal blood flow.
Indications of Lasix (Furosemide)
- Congestive Heart Failure (CHF) with pulmonary edema
- Acute and chronic renal failure
- Liver cirrhosis with ascites
- Hypertension (especially in patients with fluid overload)
- Hypercalcemia
- Pulmonary edema (emergency use)
- Nephrotic syndrome
- Cerebral edema (with other supportive care)
Adverse Effects of Lasix (Furosemide)
- Hypokalemia (low potassium levels)
- Hyponatremia (low sodium levels)
- Dehydration and hypotension
- Dizziness, headache
- Muscle cramps and weakness
- Ototoxicity (hearing loss at high doses or rapid IV push)
- Hyperuricemia and gout attacks
- Metabolic alkalosis
Contraindications of Lasix (Furosemide)
- Hypersensitivity to furosemide or sulfa drugs
- Anuria (absence of urine production)
- Severe electrolyte imbalance (especially low potassium/sodium)
- Hepatic coma or severe liver disease (relative contraindication)
- Pregnancy and lactation (use with caution)
- Dehydrated or hypotensive patients
Nursing Responsibilities While Administering Lasix (Furosemide)
1️⃣ Pre-administration Assessment
- The nurse must assess baseline blood pressure, pulse rate, respiratory status, and oxygen saturation before giving the drug.
- It is necessary to review serum electrolytes (Na⁺, K⁺, Cl⁻, Ca²⁺) and renal function tests (BUN, creatinine).
2️⃣ During Administration
- The nurse must administer IV doses slowly (e.g., 20 mg/min) to avoid ototoxicity.
- Oral Lasix should be given in the morning to prevent nocturia (urination at night).
- The nurse should ensure that the patient has easy access to a bathroom due to increased urine output.
3️⃣ Monitoring
- It is important to monitor daily weight, intake/output, and signs of fluid volume deficit.
- The nurse should watch for symptoms of hypokalemia such as muscle weakness, fatigue, or ECG changes.
- Vital signs must be monitored for signs of orthostatic hypotension or sudden drop in BP.
4️⃣ Patient Education
- The nurse must teach the patient to take the drug in the morning and avoid taking it late in the day.
- The nurse should advise the patient to report signs of dizziness, irregular heartbeat, muscle cramps, or tinnitus.
- It is important to advise potassium-rich diet or supplements (e.g., banana, orange juice), unless contraindicated.
5️⃣ Lab Follow-up
- The nurse must follow-up with regular blood tests to monitor electrolytes and kidney function.
- Urinalysis and blood pressure readings should be documented and evaluated regularly.
c) Aspirin
Mechanism of Action of Aspirin
- Aspirin irreversibly inhibits cyclooxygenase enzymes (COX-1 and COX-2), which are essential for the conversion of arachidonic acid into prostaglandins and thromboxane A2.
- By blocking COX-1, it reduces thromboxane A2 production, leading to inhibition of platelet aggregation, which helps in preventing clot formation.
- By blocking COX-2, it decreases prostaglandin synthesis, resulting in anti-inflammatory, analgesic (pain relief), and antipyretic (fever-reducing) effects.
- This effect on platelets is irreversible and lasts for the entire life of the platelet (7–10 days), making it effective as a long-acting antiplatelet agent.
- Aspirin is rapidly absorbed in the stomach and small intestine, metabolized in the liver, and excreted via the kidneys.
Indications of Aspirin
- Pain (mild to moderate), especially headache, toothache, and muscle pain
- Fever (antipyretic)
- Inflammation (e.g., arthritis, rheumatic fever)
- Acute coronary syndrome (e.g., myocardial infarction)
- Stroke and transient ischemic attack (TIA) prevention
- Deep vein thrombosis (DVT) and pulmonary embolism (PE) prevention
- Prophylaxis in patients with a history of ischemic heart disease
- Post-stent placement in combination with other antiplatelets
Adverse Effects of Aspirin
- Gastric irritation and peptic ulcer
- Heartburn, nausea, or vomiting
- Tinnitus (ringing in ears) at high doses
- Bleeding (GI bleeding, easy bruising)
- Allergic reactions (especially in asthmatics)
- Reye’s syndrome in children (especially with viral fever)
- Hepatotoxicity with prolonged use
- Renal impairment
Contraindications of Aspirin
- Hypersensitivity to aspirin or other NSAIDs
- History of peptic ulcer or GI bleeding
- Bleeding disorders (e.g., hemophilia)
- Children with viral infections (due to risk of Reye’s syndrome)
- Severe hepatic or renal impairment
- Asthma induced by NSAIDs
- Third trimester of pregnancy (risk of fetal complications)
Nursing responsibilities while Administering aspirin
1️⃣ Assessment & Monitoring
- The nurse must assess for history of GI disorders, bleeding tendencies, and allergies before administration.
- It is essential to monitor for signs of bleeding, such as petechiae, bruises, black tarry stools, or hematemesis.
- The nurse should check liver and kidney function tests during long-term use.
2️⃣ Patient Education
- The nurse must teach the patient to take aspirin with food or milk to reduce gastric irritation.
- It is necessary to instruct the patient to avoid alcohol while taking aspirin to reduce the risk of GI bleeding.
- The nurse must teach patients to report any signs of ringing in the ears, persistent stomach pain, or unusual bleeding.
3️⃣ Drug Interaction Precautions
- The nurse should monitor if the patient is taking other anticoagulants or antiplatelets (e.g., warfarin, clopidogrel), which can increase bleeding risk.
- NSAIDs like ibuprofen may interfere with the antiplatelet effect of aspirin if taken concurrently.
4️⃣ Dosage and Route
- The nurse should follow physician orders carefully, especially in cardiac cases where low-dose aspirin (75–150 mg/day) is used for antiplatelet action.
- Higher doses (300–600 mg) are used for pain and fever and must be given with caution.
5️⃣ Lab Monitoring and Follow-up
- Regular monitoring of CBC, PT/INR, and liver function tests may be necessary for long-term users.
- The nurse should ensure the patient attends follow-up appointments to review therapy efficacy and complications.
6️⃣ Prevention of Complications
- The nurse should monitor for signs of aspirin toxicity (salicylism), such as confusion, rapid breathing, sweating, or drowsiness, especially in elderly patients or those on high doses.
- It is important for the nurse to ensure the patient is well-hydrated, as dehydration can increase the risk of renal damage and salicylate accumulation.
7️⃣ Preoperative and Dental Procedure Caution
- The nurse must inform patients to notify healthcare providers before surgery or dental work, as aspirin may increase the risk of bleeding.
- Aspirin should be stopped 5–7 days before planned surgery under physician guidance, and the nurse must document and communicate accordingly.
d) Tetracycline
Mechanism of Action of Tetracycline
- It is a bacteriostatic antibiotic that works by inhibiting protein synthesis in bacteria, thereby stopping their growth and reproduction.
- Tetracycline binds reversibly to the 30S ribosomal subunit of susceptible microorganisms, blocking the attachment of aminoacyl-tRNA to the RNA-ribosome complex.
- This binding prevents the addition of amino acids to the growing peptide chain, which effectively inhibits bacterial protein synthesis.
- It is effective against gram-positive and gram-negative organisms, including Rickettsia, Chlamydia, Mycoplasma, and some protozoa.
- Tetracycline also exhibits anti-inflammatory effects in conditions like acne vulgaris and rosacea, due to inhibition of neutrophil chemotaxis and metalloproteinases.
Indications of Tetracycline
- Respiratory tract infections
- Acne vulgaris and rosacea
- Urinary tract infections (UTIs)
- Sexually transmitted infections (e.g., chlamydia, syphilis)
- Rickettsial infections (e.g., Rocky Mountain spotted fever, typhus)
- Cholera and plague
- Malaria prophylaxis (in combination therapy)
Adverse Effects of Tetracycline
- Nausea, vomiting, and abdominal cramps
- Diarrhea or pseudomembranous colitis
- Photosensitivity reactions (sunburn-like skin reaction)
- Staining of teeth (in children under 8 years)
- Hepatotoxicity (especially in pregnancy or renal disease)
- Superinfection with Candida or resistant bacteria
- Dizziness and headache
Contraindications of Tetracycline
- Hypersensitivity to tetracyclines
- Pregnancy (Category D – risk of fetal harm and teeth discoloration)
- Lactation (passes into breast milk)
- Children under 8 years (due to permanent tooth discoloration and bone growth inhibition)
- Severe liver or kidney impairment
Nursing Responsibilities While Administering Tetracycline
1️⃣ Pre-Administration Check
- It is essential for the nurse to assess the patient’s history of drug allergy, pregnancy, age, and renal/hepatic status before initiating tetracycline therapy.
2️⃣ Administration Guidelines
- The nurse must instruct the patient to take tetracycline on an empty stomach, at least 1 hour before or 2 hours after meals, to enhance absorption.
- It is important to advise the patient to avoid taking tetracycline with milk, dairy products, antacids, or iron supplements, as these interfere with drug absorption.
3️⃣ Monitoring and Observation
- The nurse should monitor the patient for gastrointestinal side effects, such as nausea, vomiting, and diarrhea, and ensure hydration is maintained.
- It is necessary to observe for signs of superinfection, such as oral thrush, vaginal yeast infection, or persistent diarrhea.
4️⃣ Photosensitivity Precaution
- The nurse must educate the patient to avoid direct sunlight or use sun protection, as tetracycline can cause severe sunburn or phototoxic reactions.
5️⃣ Pediatric and Pregnancy Concerns
- It is crucial for the nurse to withhold tetracycline in pregnant women and children below 8 years, unless life-saving, due to risks of tooth discoloration and skeletal effects.
6️⃣ Patient Compliance and Education
- The nurse should instruct the patient to complete the full course of antibiotics, even if symptoms improve, to prevent resistance.
- It is important to advise the patient to report any symptoms of allergic reaction, such as rash, itching, or breathing difficulty, immediately.
7️⃣ Follow-up and Evaluation
- The nurse must ensure that the patient returns for follow-up blood tests, liver/kidney function monitoring, and infection response evaluation.
e) Paracetamol
Mechanism of Action of Paracetamol
- Paracetamol acts mainly by inhibiting the enzyme cyclooxygenase (COX), especially COX-2, in the central nervous system (CNS) rather than in peripheral tissues.
- This central inhibition of COX leads to decreased synthesis of prostaglandins that are involved in pain and fever, thereby reducing both.
- Paracetamol raises the pain threshold by inhibiting prostaglandin action in the brain, which results in analgesic (pain-relieving) effects.
- It also affects the hypothalamic heat-regulating center, promoting peripheral vasodilation and sweating, which leads to antipyretic (fever-reducing) action.
- Unlike NSAIDs, it lacks significant anti-inflammatory activity because it does not inhibit COX in peripheral tissues.
Indications of Paracetamol
- Fever (antipyretic use)
- Mild to moderate pain (e.g., headache, dental pain, muscle ache)
- Osteoarthritis and back pain
- Pain relief in patients allergic to NSAIDs
- Used in combination with opioids for severe pain (e.g., post-operative pain)
Adverse Effects of Paracetamol
- Hepatotoxicity (especially with overdose)
- Nausea or vomiting
- Skin rash or allergic reaction
- Rare: thrombocytopenia, neutropenia
- Dizziness or hypotension (in IV form)
- Renal impairment (in chronic high doses)
Contraindications of Paracetamol
- Hypersensitivity to paracetamol
- Severe liver disease or hepatic impairment
- Chronic alcoholism
- Caution in renal disease
- Avoid with other hepatotoxic drugs
Nursing Responsibilities While Administering Paracetamol
1️⃣ Assessment Before Administration
- The nurse must assess the patient’s pain level and body temperature before administering paracetamol to ensure the correct indication for use.
- It is important for the nurse to review the patient’s liver function tests (ALT, AST) and history of liver disease or alcohol use before giving paracetamol.
2️⃣ Safe Dosing and Administration
- The nurse must ensure that the total daily dose does not exceed 4 grams (4000 mg/day) in adults to prevent liver damage.
- In children, the nurse should calculate and administer the dose strictly based on weight, following pediatric guidelines.
3️⃣ Monitoring and Observations
- The nurse must monitor for signs of hepatotoxicity, such as jaundice, dark urine, or abdominal pain, especially with long-term or high-dose use.
- It is important to observe for any allergic reactions, such as skin rashes, itching, or facial swelling.
4️⃣ Patient Education
- The nurse should educate the patient not to take multiple OTC products containing paracetamol, as this increases the risk of unintentional overdose.
- It is necessary to advise the patient not to consume alcohol while taking paracetamol, as it increases the risk of liver toxicity.
5️⃣ Documentation and Evaluation
- The nurse must record the time, dose, route, and reason for administration, and evaluate the patient’s response after 30 to 60 minutes.
- The nurse should ensure adequate fluid intake with oral paracetamol to aid absorption and reduce gastrointestinal discomfort.
f) Gentamycin
Mechanism of Action of Gentamycin
- Gentamycin is a bactericidal antibiotic that acts by inhibiting bacterial protein synthesis in gram-negative and some gram-positive bacteria.
- It binds irreversibly to the 30S subunit of the bacterial ribosome, interfering with the initiation complex formation during translation of mRNA.
- It causes misreading of mRNA, leading to the production of non-functional or toxic proteins, which ultimately results in bacterial cell death.
- Gentamycin is concentration-dependent, meaning its killing ability increases with higher drug levels in plasma.
- It is effective mainly against aerobic gram-negative bacilli (e.g., E. coli, Klebsiella, Pseudomonas) and used synergistically with beta-lactams for some gram-positive infections.
Indications of Gentamycin
- Severe gram-negative infections (e.g., Pseudomonas, E. coli)
- Septicemia and bacteremia
- Urinary tract infections (UTIs)
- Respiratory tract infections
- Abdominal infections (e.g., peritonitis)
- Endocarditis (in combination with penicillin)
- Meningitis (in neonates)
- Wound and burn infections
Adverse Effects of Gentamycin
- Nephrotoxicity (kidney damage)
- Ototoxicity (hearing loss, vertigo, tinnitus)
- Neurotoxicity (rare, includes confusion, tremors)
- Allergic skin reactions or rash
- Nausea or vomiting
- Local irritation at injection site
- Muscle weakness (especially in myasthenia gravis)
Contraindications of Gentamycin
- Hypersensitivity to gentamycin or other aminoglycosides
- Pre-existing renal impairment
- Pre-existing hearing impairment
- Myasthenia gravis or neuromuscular disorders
- Pregnancy (Category D – fetal harm possible)
- Concurrent use of other nephrotoxic drugs (e.g., vancomycin, amphotericin B)
Nursing Responsibilities While Administering Gentamycin
1️⃣ Pre-administration Assessment
- The nurse should assess baseline renal function tests (BUN, serum creatinine) and hearing status before starting gentamycin, as the drug can affect both kidneys and ears.
- It is essential to review the patient’s medication history for any other nephrotoxic or ototoxic drugs being taken concurrently.
2️⃣ Dosing and Timing
- The nurse must ensure that gentamycin is administered strictly as per prescribed dose and timing, often once-daily or in divided doses based on renal function and weight.
- It is important for the nurse to confirm the correct route (IM or IV) and use proper dilution and infusion rate for IV administration to prevent local irritation or systemic toxicity.
3️⃣ Monitoring and Lab Follow-up
- The nurse should monitor peak and trough levels if ordered, especially in long-term or high-dose therapy, to avoid accumulation and toxicity.
- The nurse must assess for signs of nephrotoxicity (e.g., reduced urine output, elevated BUN/creatinine) and ototoxicity (e.g., hearing loss, ringing in the ears, or balance issues).
4️⃣ Patient Education
- The nurse should instruct the patient to report any hearing changes, dizziness, or difficulty balancing immediately, as these could indicate early ototoxicity.
- It is essential to advise patients to drink adequate fluids to maintain renal function and avoid dehydration during treatment.
5️⃣ Infection Control and Evaluation
- The nurse must evaluate the effectiveness of treatment by monitoring for decrease in fever, improvement in infection symptoms, and normalizing WBC count.
- The nurse should also maintain strict aseptic technique during administration, especially in IV or IM use, to prevent further infection.
6️⃣ Drug Interaction Monitoring
- The nurse must carefully monitor and report any concurrent use of drugs like loop diuretics (e.g., furosemide) or vancomycin, as these combinations can significantly increase the risk of ototoxicity and nephrotoxicity when used with gentamycin.
7️⃣ Documentation and Safety Measures
- It is important for the nurse to document the exact time, dose, route, and site of gentamycin administration, and to rotate IM injection sites if used frequently to avoid tissue irritation and localized muscle damage.
Section 2
Q.4 Define the following (any five) (5)
a) Infiltration
- Infiltration is the process by which intravenous (IV) fluids or medications accidentally leak into the surrounding subcutaneous tissues instead of entering the vein due to improper placement or displacement of the IV cannula.
- It is commonly caused by IV catheter dislodgement, vein rupture, or blockage, and is characterized by swelling, coolness, pain, and pallor at the IV site.
b) Pneumonia
- Pneumonia is a lung infection that causes inflammation of the alveoli (air sacs) in one or both lungs, which may fill with fluid, pus, or cellular debris, resulting in cough with sputum, fever, chills, chest pain, and difficulty in breathing.
- It is usually caused by bacteria, viruses, fungi, or inhaled irritants, and can range from mild to life-threatening, especially in the elderly, infants, and immunocompromised individuals.
c) Pancreatitis
- Pancreatitis is a sudden or chronic inflammation of the pancreas, in which the pancreatic enzymes become active within the pancreas itself, leading to self-digestion of pancreatic tissue and surrounding organs.
- It is usually caused by gallstones, chronic alcohol intake, infections, trauma, or certain medications, and is characterized by severe abdominal pain, nausea, vomiting, and elevated pancreatic enzyme levels (amylase and lipase).
d) Appendicitis
- Appendicitis is a sudden inflammation of the vermiform appendix, a small finger-like pouch attached to the cecum in the lower right side of the abdomen.
- It is usually caused by obstruction due to fecal matter, infection, or foreign body, and leads to severe right lower abdominal pain, nausea, vomiting, loss of appetite, and fever. If untreated, it may result in perforation or rupture of the appendix, causing peritonitis.
e) Gastritis
- Gastritis is a condition characterized by inflammation, irritation, or erosion of the gastric (stomach) mucosal lining, which can occur suddenly (acute) or gradually over time (chronic).
- It is commonly caused by Helicobacter pylori infection, excessive alcohol use, prolonged NSAID use, stress, or spicy food, and presents with symptoms like epigastric pain, nausea, vomiting, bloating, indigestion, and loss of appetite.
f) Glossitis
- Glossitis is a condition that involves inflammation of the tongue, leading to swelling, redness, smooth appearance, and pain or burning sensation, especially while eating or speaking.
- It is usually caused by nutritional deficiencies (especially vitamin B12, folic acid, or iron), infections, allergic reactions, irritants (like tobacco or spicy foods), or systemic diseases, and may result in a shiny or smooth tongue surface due to atrophy of papillae.
Q.5 Write short notes on following (any four) (20)
a) Stool examination
Definition
Stool examination is a diagnostic procedure that involves the collection, observation, and laboratory testing of a patient’s feces to detect the presence of gastrointestinal infections, malabsorption, inflammation, parasites, bleeding, or other digestive system disorders.
Purpose of Stool Examination
- It is done to detect and identify parasitic infections like Giardia, Entamoeba histolytica, or Ascaris lumbricoides.
- It is used to evaluate gastrointestinal bleeding by detecting occult (hidden) blood in the stool.
- It is carried out to assess malabsorption syndromes by identifying undigested fat, food particles, or abnormal color.
- It helps in detecting bacterial infections (e.g., Salmonella, Shigella, Clostridium difficile) by culture and sensitivity testing.
- It is useful to evaluate inflammatory bowel diseases like ulcerative colitis or Crohn’s disease by observing pus, mucus, or blood in stool.
Types of Stool Examination
1️⃣ Macroscopic Examination
- It involves visual observation of stool to assess color, consistency, amount, and odor.
- It helps identify blood, mucus, pus, parasites, or undigested food.
- Tarry black stool may suggest upper GI bleeding, while fresh red blood suggests lower GI bleeding or hemorrhoids.
- Presence of fatty, bulky, foul-smelling stool suggests malabsorption.
- It is the first and fastest method in emergency GI assessments.
2️⃣ Microscopic Examination
- It is done using wet mount and stained smear to detect parasites (ova, cysts, trophozoites).
- It also helps detect WBCs, RBCs, fat globules, and starch granules.
- It is most effective when the sample is examined within 30 minutes after collection.
- Lugol’s iodine is used to enhance visibility of protozoal cysts.
- It helps differentiate infective diarrhea (WBC present) from non-infective types.
3️⃣ Chemical Examination
- It detects occult (hidden) blood using Guaiac or Benzidine test.
- It includes tests for reducing substances (e.g., glucose in stool), indicating carbohydrate malabsorption.
- Stool pH is measured to detect acidic stool due to fermentation (e.g., rotavirus).
- Sudan III stain may be used to detect fat droplets in cases of steatorrhea.
- Helps in screening for colon cancer, ulcers, or celiac disease.
4️⃣ Microbiological (Culture) Examination
- It involves culturing stool on specific media to detect pathogens like Salmonella, Shigella, E. coli.
- It is useful in diagnosing infectious diarrhea and food poisoning outbreaks.
- Clostridium difficile toxin assay is performed in suspected antibiotic-associated diarrhea.
- Antibiotic sensitivity testing is done on cultured organisms.
- Sample must be collected in sterile conditions and sent immediately to lab.
5️⃣ Immunological / Molecular Examination
- It includes ELISA for detecting microbial antigens/toxins like Giardia, Cryptosporidium, or C. difficile.
- PCR (Polymerase Chain Reaction) is used to detect microbial DNA/RNA with high sensitivity.
- Helps identify infections in immunocompromised patients and infants.
- It is highly specific and used in viral gastroenteritis detection (e.g., Rotavirus).
- Results are fast and helpful in epidemic or outbreak control.
Procedure for Collection of Stool Sample
- It is essential to use a clean, wide-mouth, dry, sterile, and leak-proof stool collection container to prevent contamination and sample degradation.
- The patient must be instructed to defecate into a clean dry pan or disposable paper and then transfer the stool into the container using a sterile spatula.
- It is critical to avoid contamination of the stool sample with urine, water, or disinfectants, as these can interfere with test accuracy.
- The container must be properly labeled with patient details including name, hospital ID, date, and time of collection to ensure accurate identification.
- The specimen should be transported to the laboratory as soon as possible, ideally within 30–60 minutes, to maintain viability of parasites and bacteria.
- If the sample is to be delayed, it must be preserved in appropriate media, such as formalin or polyvinyl alcohol (PVA) for parasite testing, or transport media like Cary-Blair for bacterial cultures.
Nursing Responsibilities in Stool Examination
Before the Procedure
- It is the nurse’s responsibility to explain the purpose and procedure of stool collection to the patient in a clear and respectful manner.
- It is important for the nurse to ensure the patient understands the correct technique of stool sample collection, including hygiene and avoiding contamination.
- It is essential to provide all necessary equipment like gloves, spatula, labeled container, and disposable collection sheet or pan.
- The nurse must ensure the patient has not taken interfering medications, such as antibiotics, iron, barium, or laxatives, prior to the test (especially for occult blood or culture).
During the Procedure
- The nurse should use personal protective equipment (PPE) including gloves and follow standard precautions to prevent infection.
- The nurse must observe and assist elderly, pediatric, or critically ill patients who are unable to collect the sample themselves.
- It is essential to inspect the sample visually for any abnormalities (e.g., blood, worms) before sending it to the lab.
After the Procedure
- It is the nurse’s role to dispose of contaminated materials safely and perform hand hygiene thoroughly after sample collection.
- It is important to document the procedure, time of collection, and any significant findings observed in the sample.
- The nurse should ensure the sample reaches the laboratory without delay, maintaining the cold chain or preservation techniques as needed.
- The nurse should follow up on laboratory results and inform the medical team of any critical findings (e.g., positive for occult blood or pathogens).
Common Abnormal Findings and Their Clinical Significance
| 💩 Stool Finding | 🔍 Clinical Indication |
|---|---|
| Ova and cysts | Parasitic infections like Amoebiasis, Giardiasis |
| Blood (fresh or occult) | Colorectal cancer, peptic ulcer, bleeding hemorrhoids |
| Fat globules (steatorrhea) | Malabsorption syndromes, chronic pancreatitis |
| Pus and mucus | Inflammatory bowel disease, bacterial infections |
| Undigested food | Incomplete digestion, rapid intestinal transit |
| High WBCs/RBCs | Ulcerative colitis, dysentery |
b) Importance of study of pathology in nursing
1️⃣ Understanding Disease Mechanisms
- It is important for nurses to study pathology because it provides a scientific basis for understanding how diseases affect cells, tissues, and organ systems.
- It enables the nurse to understand the progression from normal to abnormal physiology, which helps in assessing the severity and stage of disease.
- It enhances the ability of the nurse to understand terms like necrosis, inflammation, ischemia, or fibrosis, which are common in medical reports and diagnoses.
2️⃣ Enhances Clinical Decision-Making
- Studying pathology is important because it empowers nurses to make informed clinical judgments based on objective findings and the biological behavior of diseases
- It supports nurses in prioritizing care, recognizing warning signs, and choosing the best nursing intervention.
- It also helps in identifying patient deterioration early, especially in critical care settings, thus preventing complications.
3️⃣ Improves Quality of Patient Care
- Understanding disease pathology allows the nurse to develop a holistic care plan tailored to the patient’s condition.
- It contributes to reducing errors and improving patient outcomes through scientific knowledge and evidence-based interventions.
- It enables the nurse to deliver anticipatory guidance, especially in chronic or progressive diseases like diabetes, cancer, or COPD.
4️⃣ Assists in Interpretation of Laboratory Results
- Nurses with pathology knowledge can interpret lab results more effectively, linking them with disease progression and treatment response.
- It enables the nurse to monitor changes in patient condition by evaluating blood reports, urine analysis, biopsy findings, etc.
- It improves communication with the medical team by allowing the nurse to use correct terminology while reporting abnormalities.
5️⃣ Facilitates Patient and Family Education
- Pathology knowledge enables nurses to explain disease processes, expected outcomes, and possible complications in patient-friendly language.
- It helps the nurse answer questions like “Why is this happening to me?” with confidence and empathy.
- It also allows nurses to guide family members about genetic risks, prognosis, and home care measures based on the pathological basis of disease.
6️⃣ Supports in Early Detection and Prevention
- A strong foundation in pathology helps nurses identify early warning signs and pre-disease conditions, especially in community screening programs.
- It enables the nurse to educate the public about risk factors, triggers, and lifestyle modifications for disease prevention.
- It enhances participation in screening camps, vaccination drives, and health promotion campaigns, thus reducing disease prevalence.
7️⃣ Enhances Skills in Specialized Nursing Areas
- Nurses in oncology, cardiology, nephrology, and ICU settings require in-depth knowledge of pathology to understand disease behavior and complications.
- It assists in managing patients undergoing chemotherapy, dialysis, or complex surgeries, by understanding cellular and tissue-level damage.
- It is also useful in palliative care settings where nurses must interpret pathology reports to adjust comfort-focused care.
8️⃣ Promotes Interdisciplinary Collaboration
- Pathology knowledge equips nurses to actively participate in case discussions, rounds, and clinical decision-making alongside doctors and specialists.
- It helps the nurse advocate for patients when abnormalities are detected, ensuring prompt medical review and action.
- It also fosters teamwork with diagnostic labs and radiology departments, improving the efficiency and accuracy of care delivery.
9️⃣ Strengthens Academic and Professional Knowledge
- A sound understanding of pathology prepares nursing students for better performance in case presentations, clinical exams, and viva.
- It helps in writing evidence-based care plans, nursing diagnoses, and research projects with scientific backing.
- It is essential for continuing education, higher studies, and specialization, as pathology forms the basis for all advanced nursing practice.
c) Blood transfusion reaction
1️⃣ Acute Hemolytic Transfusion Reaction (AHTR)
- It is a life-threatening reaction caused by ABO blood group incompatibility, where the recipient’s antibodies attack the donor red blood cells, leading to their destruction.
- It occurs within minutes of starting the transfusion and leads to the release of free hemoglobin into circulation, which can cause acute kidney injury.
- It is also associated with activation of the complement system and coagulation pathway, which can result in disseminated intravascular coagulation (DIC).
2️⃣ Febrile Non-Hemolytic Transfusion Reaction (FNHTR)
- It is the most common immune-mediated transfusion reaction, caused by the recipient’s antibodies reacting with donor leukocytes or cytokines.
- It typically occurs 1–6 hours after transfusion begins and presents with chills, rise in temperature by ≥1°C, headache, and malaise.
- It is more frequent in patients who have had multiple previous transfusions or pregnancies due to leukocyte sensitization.
- It can be minimized by using leukocyte-reduced or pre-storage leukodepleted blood products.
3️⃣ Allergic Transfusion Reaction (Mild to Moderate)
- It is a hypersensitivity reaction to plasma proteins in the donor’s blood, commonly occurring within minutes of transfusion.
- It is characterized by itching, urticaria (hives), localized or generalized rash, and flushing.
- It is usually self-limiting but may require antihistamines; transfusion can often be resumed after symptom resolution.
- It is more common in patients with atopy or history of allergic disorders.
4️⃣ Anaphylactic Transfusion Reaction
- It is a rare but severe reaction that occurs suddenly and requires immediate medical intervention.
- It is most often seen in IgA-deficient patients with anti-IgA antibodies reacting to IgA in transfused plasma.
- Symptoms include bronchospasm, laryngeal edema, hypotension, shock, and loss of consciousness.
- It requires prompt administration of epinephrine, corticosteroids, and discontinuation of the transfusion.
5️⃣ Delayed Hemolytic Transfusion Reaction (DHTR)
- It occurs several days to weeks after transfusion due to the recipient’s anamnestic response to red cell antigens previously encountered.
- The antibodies formed destroy transfused red cells slowly, leading to mild jaundice, low-grade fever, and anemia.
- This reaction is often missed or misdiagnosed as inadequate response to transfusion unless direct antiglobulin test (Coombs) is performed.
- It is commonly associated with Kidd, Duffy, Kell, or Rh antigens.
6️⃣ Graft-versus-Host Disease (GVHD)
- It is a fatal complication seen in immunocompromised patients (e.g., neonates, transplant recipients), where donor lymphocytes attack host tissues.
- Symptoms include fever, rash, watery diarrhea, liver dysfunction, and pancytopenia.
- It usually occurs within 1–2 weeks after transfusion and has a very poor prognosis.
- Prevention includes gamma irradiation of blood products to inactivate donor T lymphocytes.
7️⃣ Septic Transfusion Reaction
- It occurs due to bacterial contamination of blood components, especially platelets which are stored at room temperature.
- Common organisms include Yersinia enterocolitica, E. coli, and Staphylococcus aureus.
- It presents with sudden high fever, chills, hypotension, vomiting, and signs of septic shock.
- It requires immediate cessation of transfusion, blood cultures, broad-spectrum antibiotics, and supportive care.
8️⃣ Iron Overload (Transfusion-Related Hemosiderosis)
- It is a chronic complication seen in patients requiring repeated blood transfusions such as thalassemia, aplastic anemia, or sickle cell disease.
- It occurs because each unit of packed red cells contains about 250 mg of iron, and the body has no mechanism for excreting excess iron.
- Iron accumulates in vital organs such as liver, heart, pancreas, and endocrine glands, leading to cirrhosis, cardiomyopathy, and diabetes.
- Iron chelation therapy (e.g., with desferrioxamine or deferasirox) is used to manage this condition.
d) genemutosis
Definition
- It is defined as a permanent alteration or change in the nucleotide sequence of a gene within the DNA of a cell.
- It may occur spontaneously or due to exposure to mutagenic agents such as radiation, chemicals, or viruses.
- Gene mutations can affect gene function, protein synthesis, or lead to various genetic disorders and cancers.
Etiology (Causes)
- Spontaneous errors in DNA replication
- Exposure to ionizing radiation (e.g., X-rays, UV rays)
- Chemical mutagens (e.g., benzene, alkylating agents)
- Viral infections (e.g., HPV, HIV)
- Errors during meiosis or mitosis
- Inherited mutations from parents
Types of Gene Mutation
1. Point Mutation
- It involves a change in a single nucleotide base pair in the DNA sequence.
- It can result in various outcomes depending on the codon and amino acid produced.
a) Silent Mutation
- It is when the nucleotide change does not affect the amino acid due to codon redundancy.
- It is often harmless but may affect gene regulation.
b) Missense Mutation
- It is when the base change results in a different amino acid being incorporated into the protein, which may alter its function.
- Example: Sickle Cell Anemia (Glu → Val substitution).
c) Nonsense Mutation
- It is when the base change introduces a premature stop codon, leading to a truncated and usually nonfunctional protein.
- Often leads to severe disorders like Thalassemia.
2. Insertion Mutation
- It is when one or more nucleotides are added into the DNA sequence.
- It can cause a frameshift mutation if the number of inserted bases is not a multiple of 3, altering downstream amino acids.
3. Deletion Mutation
- It involves the loss of one or more nucleotides from the DNA sequence.
- It also causes a frameshift, leading to defective or nonfunctional proteins.
4. Duplication Mutation
- It occurs when a segment of the DNA is copied and inserted repeatedly into the gene.
- It can lead to abnormal protein function or overexpression of certain genes.
5. Frameshift Mutation
- It is caused by insertion or deletion that shifts the reading frame of the mRNA during translation.
- It changes all the downstream amino acids, usually leading to nonfunctional or harmful proteins.
6. Repeat Expansion Mutation
- It involves repeated sequences of DNA (e.g., trinucleotides) that expand abnormally.
- It is the cause of several neurological disorders like Huntington’s disease and Fragile X syndrome.
Effects of Gene Mutation
- It can lead to loss of function or gain of function of a gene.
- It may result in hereditary diseases (e.g., Cystic fibrosis, Sickle cell anemia).
- It can be neutral or silent, causing no visible effect.
- Some mutations may cause cellular transformation and cancer (e.g., p53 gene mutation in tumors).
- In reproductive cells, it may result in inherited genetic disorders.
- In somatic cells, it may lead to acquired diseases like cancer or resistance to drugs.
Clinical Significance
- Gene mutations are a major cause of inherited diseases like thalassemia, muscular dystrophy, and phenylketonuria.
- Some mutations can make individuals resistant or sensitive to specific drugs (pharmacogenomics).
- Prenatal genetic testing and counseling help detect harmful mutations in early stages.
- Mutation analysis is important in cancer diagnosis, prognosis, and treatment, especially in targeted therapies.
- It forms the basis of genetic engineering and gene therapy for correcting defective genes.
Examples of Disorders Caused by Gene Mutation
- Sickle Cell Anemia – Missense mutation (Glu→Val)
- Thalassemia – Nonsense or frameshift mutation
- Cystic Fibrosis – Deletion mutation (∆F508)
- Huntington’s Disease – Trinucleotide repeat expansion
- Tay-Sachs Disease – Point mutation in HEXA gene
- BRCA1/2 Mutation – Breast and ovarian cancer susceptibility
Prevention & Control
- Avoiding radiation exposure and carcinogenic chemicals.
- Genetic counseling and screening in high-risk families.
- Use of prenatal diagnostic tools (like amniocentesis, chorionic villus sampling).
- CRISPR-Cas9 gene editing technology is under research for correcting mutations.
- Public awareness and carrier screening in communities with prevalent genetic diseases.
e) Carcinogenic
Definition
- It is defined as any substance, agent, or exposure that is capable of causing cancer in living tissues by altering cellular DNA and disrupting normal cell growth and division.
- It is the property of a substance or exposure to induce or promote the formation of malignant tumors (neoplasms) in humans or animals.
Types of Carcinogens
1️⃣ Chemical Carcinogens
- It includes substances such as benzene, formaldehyde, tobacco smoke, asbestos, aflatoxins, and certain dyes that can damage cellular DNA leading to cancer.
- It is mainly present in industrial waste, processed foods, pesticides, cigarette smoke, etc.
2️⃣ Physical Carcinogens
- It includes ionizing radiation such as X-rays, gamma rays, and ultraviolet (UV) radiation that directly damage the DNA and increase the risk of cancer.
- It is also seen in exposure to radioactive materials like radon gas.
3️⃣ Biological Carcinogens
- It includes certain viruses, bacteria, and parasites that have the ability to cause mutations or chronic inflammation leading to cancer.
- Examples include Human papillomavirus (HPV) causing cervical cancer, Hepatitis B and C causing liver cancer, and Helicobacter pylori causing gastric cancer.
Mechanism of Carcinogenesis
- It is initiated when a carcinogen causes a mutation or alteration in the DNA of a normal cell.
- It is followed by promotion where the mutated cell starts uncontrolled proliferation without normal apoptosis.
- It leads to progression where further mutations accumulate, resulting in invasive cancer.
Examples of Common Carcinogens
It includes cigarette smoke (lung cancer), alcohol (liver and esophageal cancer), arsenic (skin cancer), asbestos (mesothelioma), and UV radiation (skin cancer).
Health Hazards of Carcinogens
- It may cause gene mutations and chromosomal abnormalities leading to uncontrolled cell growth.
- It can result in multiple organ system cancers depending on the exposure route (e.g., inhalation, ingestion, skin contact).
- It is linked to reproductive and developmental toxicity in some agents.
Prevention and Control
Avoidance of Exposure:
It includes stopping smoking, reducing alcohol consumption, avoiding processed meat and charred foods.
Use of Protective Equipment:
It is advised for workers in industries using chemicals like asbestos, benzene, etc., to use PPE (Personal Protective Equipment).
Regular Screening:
It is important to screen for early detection of cancers in high-risk populations (e.g., Pap smear, mammography).
Vaccination:
It includes vaccination against cancer-causing viruses like HPV and Hepatitis B.
Nursing Management & Role of Nurse in Carcinogen Exposure
✅ A. Health Education
- It is the nurse’s duty to educate the public regarding the risks of tobacco, alcohol, and exposure to industrial chemicals.
- It is important to create awareness about protective clothing, proper handling of chemicals, and sun protection.
✅ B. Early Detection and Screening
- It is the nurse’s role to encourage screening tests such as Pap smear, mammography, and colonoscopy.
- Nurses can identify early warning signs of cancer such as lumps, persistent cough, changes in skin/moles.
✅ C. Occupational Health Safety
- Nurses must enforce the use of Personal Protective Equipment (PPE) in workplaces dealing with carcinogens.
- They must educate workers about Material Safety Data Sheets (MSDS) and safe chemical storage.
✅ D. Patient Counseling and Support
- It is essential for nurses to provide emotional support to patients exposed to or diagnosed with carcinogen-related cancers.
- They can refer patients to oncology specialists and assist in psychological rehabilitation.
Q.6 Answer the following (any three) (12)
a) Genetherapy
Definition of Gene Therapy
- It is defined as a medical technique that involves the modification, replacement, or correction of defective genes in order to treat or prevent disease.
- It is the process in which functional or therapeutic genes are inserted into a patient’s cells to replace mutated genes or to enhance disease-fighting functions.
- It is used as an experimental treatment approach in genetic disorders, cancers, and some viral infections.
Goals of Gene Therapy
- It is used to correct inherited genetic defects such as cystic fibrosis or hemophilia.
- It is aimed to introduce new or modified genes into the body to help treat diseases like cancer or HIV.
- It is designed to inactivate or “knock out” malfunctioning genes that are functioning improperly.
- It is intended to enhance the body’s ability to fight diseases by stimulating immune responses using genetically engineered cells.
Types of Gene Therapy
✅ 1. Somatic Gene Therapy
- It is a type of gene therapy in which therapeutic genes are transferred into somatic (body) cells, not passed on to offspring.
- It is mostly used in adults and children with acquired diseases or non-inheritable genetic conditions.
✅ 2. Germline Gene Therapy
- It is a type of gene therapy in which genes are introduced into germ cells (sperm or egg), so the changes are heritable.
- It is ethically controversial and not permitted in humans in many countries.
✅ 3. Ex vivo Gene Therapy
- It involves removal of cells from the body, genetic modification in the lab, and reinfusion into the patient.
- Example: Modified T-cells for CAR-T therapy in leukemia.
✅ 4. In vivo Gene Therapy
- It involves direct delivery of therapeutic genes into the patient’s body using vectors like viruses or nanoparticles.
Methods of Gene Delivery
✅ 1. Viral Vectors
- Adenovirus, Retrovirus, Lentivirus are used to deliver therapeutic DNA into cells.
- These viruses are modified to be non-pathogenic but effective in gene transfer.
✅ 2. Non-Viral Methods
- Includes liposomes, nanoparticles, electroporation, or gene guns.
- These methods are safer but less efficient than viral vectors.
Indications of Gene Therapy
- It is used in genetic disorders like cystic fibrosis, sickle cell anemia, SCID (severe combined immunodeficiency).
- It is applied in cancer treatment, especially leukemia, lymphoma, and brain tumors.
- It is being studied in neurological disorders like Parkinson’s disease and Huntington’s disease.
- It is also tested in infectious diseases such as HIV and hepatitis B.
Advantages of Gene Therapy
- It offers a potential permanent cure by targeting the root genetic cause of the disease.
- It reduces or eliminates the need for long-term medications or surgery.
- It is useful in treating diseases with no known effective treatment.
- It may improve quality of life and life expectancy in individuals with life-threatening genetic disorders.
Limitations / Disadvantages of Gene Therapy
- It carries risk of immune response or rejection of the introduced gene.
- It may cause insertional mutagenesis, potentially leading to cancer.
- It is currently expensive and not widely accessible.
- It involves ethical concerns, especially in germline therapy.
- The long-term effects and safety of gene therapy are still being studied.
Nursing Management in Gene Therapy
✅ 1. Pre-Treatment Preparation and Education
- It is the responsibility of the nurse to educate the patient and family about gene therapy procedures, risks, and benefits.
- It is essential to obtain informed consent after thoroughly explaining experimental nature and possible outcomes.
- It is important to assess the patient’s understanding and psychological readiness for the therapy.
✅ 2. Monitoring During and After Therapy
- It is necessary to monitor vital signs, allergic reactions, and immune responses during gene delivery.
- It is the duty of the nurse to observe for signs of infection, inflammation, or infusion-related complications.
- It is also important to document adverse effects or therapy failure and report promptly to the physician.
✅ 3. Post-Therapy Care and Support
- It is essential to provide emotional and psychological support for patients undergoing experimental treatments.
- It is the nurse’s role to ensure follow-up appointments for gene expression studies and clinical assessments.
- It is necessary to encourage adherence to infection prevention precautions and lifestyle modification as advised.
✅ 4. Ethical and Legal Considerations
- It is crucial to maintain confidentiality and bioethics when dealing with genetic information.
- It is also required to respect patient autonomy and cultural beliefs regarding genetic modifications.
b) Application of genetics in nursing
1️⃣ Genetic Risk Assessment and Counseling
- It is the responsibility of the nurse to collect a complete family history (three-generation pedigree) to assess hereditary risks for genetic diseases like cancer, diabetes, and cardiovascular disorders.
- It is used to identify individuals or families at risk for inherited conditions such as thalassemia, cystic fibrosis, Huntington’s disease, and hemophilia.
- The nurse plays a role in referring patients to genetic counselors or specialists when high risk is detected based on genetic screening.
2️⃣ Prenatal and Reproductive Health Nursing
- Genetics is applied in antenatal care to detect congenital or chromosomal disorders (e.g., Down syndrome, neural tube defects) through screening like triple test, amniocentesis, or chorionic villus sampling.
- Nurses assist in educating pregnant women about genetic testing options and implications of positive results.
- Nurses help in explaining the results of prenatal genetic testing, helping parents make informed decisions.
3️⃣ Newborn Screening and Pediatric Nursing
- Genetics is applied in newborn screening programs for early detection of genetic/metabolic disorders like phenylketonuria (PKU) or congenital hypothyroidism, which can be treated early.
- The nurse plays a key role in informing parents, collecting samples, and following up with results and referrals.
- Pediatric nurses use genetic information to identify inherited diseases early and coordinate appropriate care or specialist referrals.
4️⃣ Oncology and Genetic Disorders
- Genetic testing helps identify hereditary cancer syndromes, such as BRCA1 and BRCA2 mutations in breast and ovarian cancer.
- Oncology nurses support patients by explaining genetic risk, testing procedures, and possible outcomes.
- Nurses also assist in screening family members of patients with known genetic predispositions.
5️⃣ Pharmacogenomics and Personalized Medicine
- Nurses use genetic knowledge to understand how an individual’s genetic makeup influences their response to drugs (e.g., warfarin sensitivity, clopidogrel metabolism).
- Pharmacogenetics helps the nurse and healthcare team to select the most effective drug and avoid adverse drug reactions.
- Nurses must monitor and educate patients on genotype-based medication dosing or selection.
6️⃣ Genetic Testing and Ethical Considerations
- Nurses must understand genetic testing types (diagnostic, predictive, carrier, newborn, pharmacogenomic testing) and guide patients accordingly.
- Nurses help in protecting patient confidentiality, ensuring informed consent, and advocating for non-discriminatory genetic policies.
- The nurse must provide emotional support and psychological preparation for patients undergoing genetic testing.
7️⃣ Role in Education and Awareness
- Nurses are responsible for educating patients and the community about inheritance patterns, genetic diseases, and the importance of early screening.
- They help in disseminating genetic knowledge to reduce stigma and promote preventive health behavior.
- Nurses organize community-level awareness campaigns about inherited diseases like sickle cell anemia or thalassemia in high-risk populations.
c) Morphology of myocardial infarction
The morphology of myocardial infarction includes the structural changes that occur in the heart muscle due to ischemic injury, which can be observed grossly (with the naked eye) and microscopically (under a microscope). These changes occur in a time-dependent manner.
A. Gross Morphological Changes of MI (Macroscopic Changes)
These are the changes seen by the naked eye on the external surface or cross-section of the heart, varying with time since infarction.
0–6 Hours Post-Infarction:
- It is usually not possible to detect any significant gross change during this early phase.
- In some cases, pallor of the myocardium may be noticed on special staining.
6–12 Hours:
- The infarcted area may appear slightly darker than surrounding tissue.
- Mottling or blotchy discoloration may start to appear due to sluggish blood flow.
12–24 Hours:
- The area becomes dark red-blue due to blood stagnation and edema.
- Tissue is slightly softened and congested.
1–3 Days:
- The infarcted area becomes pale yellow or tan, especially in the center.
- A reddish hyperemic border may surround the necrotic area due to inflammation.
3–7 Days:
- The infarct appears soft, yellow-tan, with clearer demarcation.
- Tissue breakdown is prominent, increasing risk of cardiac rupture.
7–10 Days:
- The infarct remains yellow and soft, but now has more distinct red granulation tissue at the borders.
- This is the phase of active healing.
10–14 Days:
- The yellow center is gradually replaced by gray-white fibrous tissue at the margins.
- Scar formation begins.
2–8 Weeks:
- The infarcted zone is progressively replaced by firm, fibrous, white scar.
- The myocardial wall may become thin.
After 8 Weeks:
- The healing is complete and the area is replaced by dense collagenous scar tissue.
- The ventricle may show deformity or aneurysm in some cases.
B. Microscopic Morphological Changes (Histological Changes)
These are changes that occur at the cellular level and are visible under a microscope, depending on the time since ischemia started.
0–6 Hours:
- No clear histological changes are visible with routine stains.
- Ultrastructural changes like mitochondrial swelling and myofibril relaxation seen under electron microscopy.
6–12 Hours:
- Beginning of coagulative necrosis in myocardial fibers.
- Cytoplasm becomes more eosinophilic (pink) due to protein denaturation.
- Nuclear changes like pyknosis (shrinkage) may begin.
12–24 Hours:
- Definite coagulative necrosis becomes evident.
- Neutrophil infiltration begins between dead myocytes.
- Loss of nuclei and striations in affected fibers.
1–3 Days:
- Extensive neutrophilic infiltration dominates the tissue.
- Myocytes are completely necrotic with no nuclei or cross-striations.
- This is the peak phase of acute inflammation.
3–7 Days:
- Macrophages replace neutrophils and begin phagocytosis of necrotic tissue.
- Myocardium is very soft; this is the highest risk period for myocardial rupture.
7–10 Days:
- Granulation tissue appears at margins, with new capillaries and fibroblasts.
- Macrophages continue clearing the dead tissue.
10–14 Days:
- Fibroblasts increase collagen production.
- Granulation tissue matures, and cellular inflammation decreases.
2–8 Weeks:
- Progressive replacement by dense collagen fibers.
- Few inflammatory cells remain; scar tissue forms.
8 Weeks:
- The infarcted area is replaced completely by acellular dense fibrous scar.
- Function of affected myocardium is permanently lost.
d) Karotyping of m genes
Definition of Karyotyping
- It is a laboratory technique used to visualize the complete set of chromosomes of an individual under a microscope.
- It is performed on metaphase chromosomes to detect chromosomal abnormalities in number or structure.
- It is useful for detecting genetic disorders, sex chromosome abnormalities, and chromosomal mutations.
What are M Genes?
- “M genes” are not a formally recognized group of genes; here, the ‘M’ likely refers to “mitotic” phase or male/female chromosomes (X/Y) often studied in karyotyping.
- In some literature, M may denote “Mutated Genes”, “Mitochondrial Genes”, or genes involved in Meiosis/Mitosis regulation.
- The karyotyping process studies all genes located on the chromosomes including M-gene regions (such as MHC, mitochondrial sequences, or specific disease-linked mutations).
Procedure of Karyotyping
Sample Collection
It is done from blood, amniotic fluid, bone marrow, or chorionic villi.
Cell Culture
Collected cells are cultured in a medium to promote cell division, especially until the metaphase stage.
Arresting Metaphase
Colchicine or another spindle inhibitor is used to stop cells in metaphase, as this is when chromosomes are most condensed and visible.
Hypotonic Treatment
The cells are treated with hypotonic solution to swell them, which helps to spread out the chromosomes.
Fixation and Slide Preparation
Cells are fixed with methanol-acetic acid and spread on microscope slides.
Staining
Slides are stained using Giemsa stain (G-banding), Q-banding, or R-banding to differentiate chromosome regions.
Microscopic Examination
A cytogeneticist arranges chromosomes into a karyogram – a standard format of chromosomes arranged in pairs.
Uses and Applications of Karyotyping
- It is used to detect chromosomal disorders such as Down syndrome (trisomy 21), Turner syndrome (monosomy X), and Klinefelter syndrome (XXY).
- It is helpful in identifying translocations, deletions, duplications, and inversions in chromosomes.
- It is used for prenatal diagnosis of genetic abnormalities in the fetus.
- It is utilized in cancer diagnosis, especially in identifying Philadelphia chromosome in chronic myeloid leukemia (CML).
- It aids in infertility evaluations, recurrent miscarriages, or developmental delays in children.
Limitations of Karyotyping
- It may not detect small gene mutations or single nucleotide changes.
- It requires cells to be actively dividing, which may take time in culture.
- It is a labor-intensive and time-consuming process.
- It has lower resolution compared to molecular techniques like FISH or PCR.
Nursing Responsibilities in Karyotyping
✅ 1. Pre-Test Preparation
- It is essential for the nurse to explain the purpose of karyotyping to the patient or guardian in a language they understand.
- It is necessary to obtain informed consent, especially in prenatal or invasive procedures like amniocentesis.
- It is the nurse’s duty to assist in the collection of blood or other tissue samples using aseptic technique.
✅ 2. During Procedure
- It is important to handle samples carefully to avoid contamination or cell damage.
- It is required to label samples properly and ensure timely transport to the cytogenetics laboratory.
✅ 3. Post-Test Support and Follow-Up
- It is the responsibility of the nurse to provide emotional support if chromosomal abnormalities are found.
- It is important to refer the patient for genetic counseling based on the test results.
- It is essential to maintain confidentiality and privacy of genetic information.
