26/07/2017-B.SC-MEDICAL SURGICAL-1 DONE-UPLOAD NO.5
AHN-1-PAPER SOLUTION NO.5
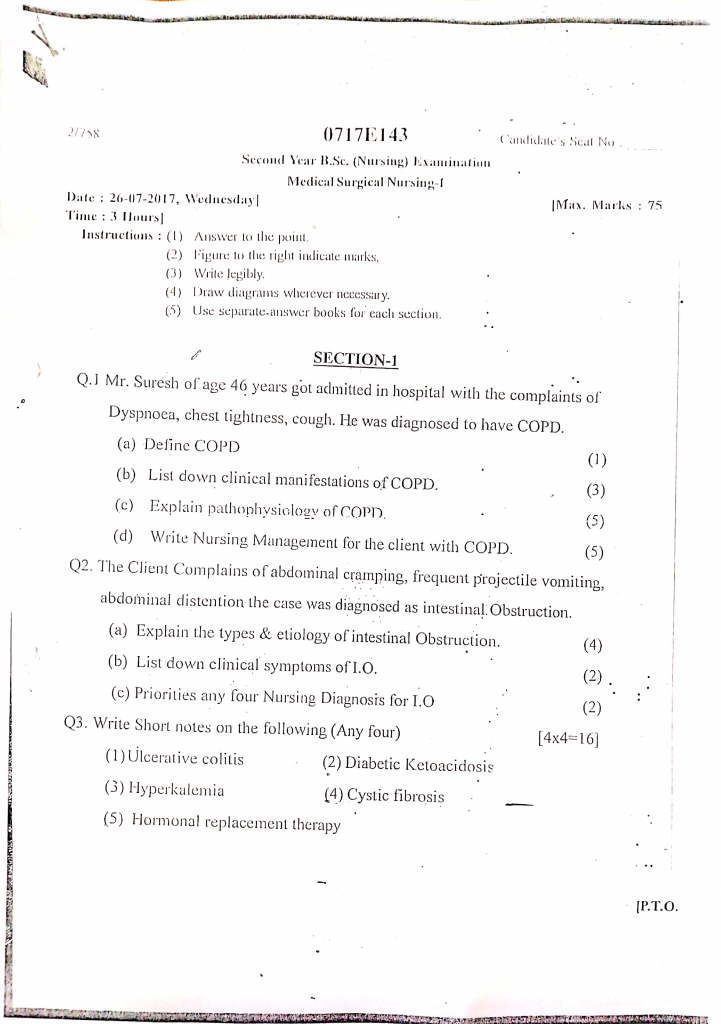
Section 1
Q.1 Mr. Suresh of age 46 years got admitted in the hospital with the complaints of dyspnoea, chest tightness, cough. He was diagnosed to have COPD.
a) Define COPD (1)
COPD is a progressive, irreversible lung disease characterized by chronic airflow limitation that is not fully reversible. It includes conditions like chronic bronchitis and emphysema, which cause obstruction of the airways and impair gas exchange, leading to breathlessness, cough, and sputum production.
b) List down clinical manifestations of COPD (3)
- Chronic productive cough
- Progressive dyspnea (shortness of breath)
- Excessive sputum production
- Wheezing and chest tightness
- Frequent respiratory infections
- Cyanosis (bluish lips/nails)
- Barrel-shaped chest
- Use of accessory muscles for breathing
- Fatigue and weakness
- Unintentional weight loss
- Pursed-lip breathing
- Prolonged expiration
- Signs of right-sided heart failure
- Anxiety and restlessness
- Digital clubbing
c) Expain pathophysiology of COPD (5)
1. Exposure to Irritants
- It is caused by chronic exposure to harmful particles and gases such as cigarette smoke, industrial fumes, air pollutants, and dust.
- It especially affects individuals with prolonged exposure to biomass fuel smoke used for cooking in poorly ventilated homes.
- It initiates repeated damage to airway epithelial cells, beginning the inflammatory process.
2. Chronic Inflammation
- It leads to the recruitment of neutrophils, macrophages, and CD8+ T-cells, which release enzymes (e.g., elastase) that degrade lung tissue.
- It increases the release of pro-inflammatory cytokines (e.g., TNF-alpha, IL-8), worsening the inflammation.
- This continuous inflammation disrupts normal lung repair mechanisms and promotes irreversible tissue damage.
3. Airway Changes
- It causes bronchiolar wall thickening, smooth muscle hypertrophy, and fibrosis which narrow the airway lumen.
- It leads to airflow limitation, especially during expiration.
- Recurrent inflammation and repair cycles promote remodeling of the airway structure.
4. Alveolar Destruction (Emphysema)
- It results in the breakdown of elastin and connective tissue in alveolar walls due to protease-antiprotease imbalance.
- Alveoli coalesce to form larger air spaces (bullae), which are inefficient for gas exchange.
- It reduces lung compliance and elastic recoil, causing air trapping.
5. Mucus Hypersecretion (Chronic Bronchitis)
- It is due to goblet cell hyperplasia and enlargement of submucosal glands in bronchi.
- It contributes to chronic productive cough, especially in the early morning.
- The retained secretions can promote bacterial colonization and recurrent infections.
6. Air Trapping & Hyperinflation
- It causes progressive lung overdistension, increasing the effort needed for ventilation.
- It shifts the diaphragm into a flattened position, reducing its mechanical efficiency.
- It leads to the characteristic “barrel chest” appearance in severe COPD.
7. Gas Exchange Abnormalities
- Due to alveolar destruction and ventilation-perfusion (V/Q) mismatch, oxygen cannot effectively enter the blood.
- It leads to hypoxemia (↓PaO₂) and in advanced stages hypercapnia (↑PaCO₂).
- Over time, it causes respiratory acidosis and compensatory mechanisms like polycythemia.
8. Pulmonary Hypertension
- Chronic hypoxia induces vasoconstriction of pulmonary arteries, increasing pulmonary vascular resistance.
- It promotes vascular remodeling and smooth muscle hypertrophy in pulmonary vessels.
- It puts increased strain on the right side of the heart, progressing toward cor pulmonale.
9. Cor Pulmonale (Right-Sided Heart Failure)
- The right ventricle must work harder to pump blood through the constricted pulmonary vessels.
- Over time, the right heart becomes hypertrophied and eventually dilated, leading to failure.
- It results in peripheral edema, ascites, hepatomegaly, and jugular vein distension (JVD).
10. Progressive Functional Decline
- It reduces lung capacity, leading to exercise intolerance, fatigue, and dyspnea at rest.
- It increases susceptibility to acute exacerbations, often requiring hospitalization.
- Patients may develop depression and anxiety, further impacting quality of life.
d) Wrte nursing management of client with COPD (5)
Impaired Gas Exchange related to alveolar-capillary membrane changes and airflow limitation
Goal : Patient will maintain optimal gas exchange
Nursing Interventions :
- Monitor respiratory rate, depth, and SpO₂ regularly
- Administer supplemental oxygen as prescribed (low-flow if CO₂ retainer)
- Position patient in high Fowler’s or tripod position to facilitate lung expansion
- Teach pursed-lip breathing and diaphragmatic breathing
- Encourage incentive spirometry use
- Provide bronchodilators, corticosteroids, and nebulization therapy as ordered.
- Assess for cyanosis, restlessness, confusion (signs of hypoxia)
Ineffective Airway Clearance related to excessive mucus production and weak cough effort
Goal : Patient will maintain a clear airway with effective cough and normal breath sounds.
Nursing Interventions :
- Assess respiration rate and pattern
- Encourage fluid intake (if not contraindicated) to thin secretions
- Provide high fowler or fowler position to the patient
- Provide chest physiotherapy and postural drainage as indicated
- Encourage coughing and deep breathing exercisesSuction airway if necessary (esp. in acute phase)
- Administer expectorants or bronchodilators as ordered
Activity Intolerance related to imbalance between oxygen supply and demand
Goal : Patient will perform activities of daily living (ADLs) without excessive fatigue or dyspnea.
Nursing Interventions :
- Assess tolerance to activity and fatigue level
- Plan activities with rest periods
- Provide assistance with ADLs as needed
- Educate energy conservation techniques
- Administer medications like bronchodilators prior to activities
Imbalanced Nutrition less than Body Requirements related to anorexia, dyspnea during eating, increased metabolic demand as evidenced by weight loss, poor appetite
Goal : patient has improve nutritional level
Nursing Interventions :
- Assess nutritional status using weight trends and dietary history.
- Provide high-protein, high-calorie, small frequent meals.
- Encourage rest before meals to reduce fatigue while eating.
- Avoid gas-forming foods that increase bloating and dyspnea.
- Collaborate with a dietitian for individualized nutrition plans.
- Monitor serum albumin and prealbumin levels.
- Consider nutritional supplements (e.g., protein shakes).
Anxiety related to breathlessness and fear of suffocation
Goal : Patient will verbalize reduced anxiety and demonstrate relaxation techniques.
Nursing Interventions :
- Stay with patient during episodes of breathlessnessUse calm, reassuring Communication
- Teach relaxation techniques (e.g., guided imagery, controlled breathing)
- Encourage expression of fears
- Avoid sudden changes in care or routine
Q.2 The client complaints of abdominal cramping, frequent projectile vomiting, Abdominal distension the cause was diagnosed as intestinal obstruction.
a) Explain the types and etiology of intestinal obstruction (4)
Types of Intestinal Obstruction
A. Based on Mechanism
1️⃣ Mechanical Obstruction
- It occurs due to a physical blockage that prevents intestinal contents from passing through.
- The obstruction may be caused by tumors, adhesions, volvulus, hernias, intussusception, impacted feces, foreign bodies, strictures.
- It may lead to intestinal ischemia and necrosis if blood supply is compromised.
- Mechanical obstruction often presents with colicky abdominal pain and visible peristaltic waves.
2️⃣ Functional Obstruction (Paralytic Ileus)
- It occurs due to loss of normal peristaltic movement of the intestine, without a physical blockage.
- It is often caused by abdominal surgery, infections, metabolic disorders, or certain drugs.
- The bowel sounds are usually absent or decreased, differentiating it from mechanical obstruction.
- It may be associated with generalized abdominal distention and minimal or no colicky pain.
B. Based on Location
1️⃣ Small Bowel Obstruction (SBO)
- The blockage occurs in the small intestine (duodenum, jejunum, ileum).
- It is more common than large bowel obstruction.
- It causes rapid onset of symptoms like vomiting, cramping, and dehydration.
- It has a higher risk of causing electrolyte imbalances and metabolic alkalosis.
2️⃣ Large Bowel Obstruction (LBO)
- The blockage occurs in the colon or rectum.
- It is often associated with colon cancer or diverticulitis.
- It presents with progressive abdominal distension, constipation, and late vomiting.
- The risk of perforation is higher in LBO, especially in cases of volvulus or cancer.
C. Based on Degree
1️⃣ Partial Obstruction
- Some gas and liquid can still pass through the intestine.
- The patient may experience intermittent symptoms and partial relief after passing gas or stools.
- It may be managed conservatively if no signs of strangulation are present.
2️⃣ Complete Obstruction
- There is total blockage of intestinal flow, requiring urgent intervention.
- It is associated with severe, continuous pain, absent bowel sounds, and inability to pass stool or gas.
- Without prompt treatment, it can lead to peritonitis, septic shock, and death.
ETIOLOGY OF INTESTINAL OBSTRUCTION
Mechanical Causes (Physical Blockage)
- Postoperative adhesions (scar tissue)
- Hernias (inguinal, umbilical)
- Tumors (benign or malignant)
- Volvulus (twisting of intestine)
- Intussusception (telescoping of bowel)
- Fecal impaction
- Strictures (Crohn’s disease, radiation)
- Foreign bodies
Functional Causes (Paralytic Ileus)
- Postoperative state (after abdominal surgery)
- Peritonitis
- Electrolyte imbalances (hypokalemia)
- Medications (opioids, anticholinergics)
- Neurological disorders (spinal cord injury, Parkinson’s disease)
b) List down clinical manifestations of I.O. (2)
- Abdominal pain – colicky or continuous
- Abdominal distension
- Vomiting – may be bilious or feculent
- Constipation – absence of stool or gas
- Failure to pass flatus
- Bowel sounds – hyperactive early, absent later
- Dehydration signs – dry mouth, low urine output
- Tachycardia and hypotension (in severe cases)
- Signs of peritonitis – if perforation occurs
- Restlessness and anxiety due to pain and discomfort
c) Prioritise any four nursing diagnosis of I.O. (2)
1️⃣ Acute Pain related to intestinal distension and increased peristalsis
- It is the highest priority as patients with I.O. often experience severe colicky abdominal pain due to bowel distension and obstruction.
- The nurse should assess pain characteristics, intensity, and duration, and administer prescribed analgesics.
2️⃣ Risk for Deficient Fluid Volume related to vomiting and third-space fluid shift
- It is a critical diagnosis because persistent vomiting, bowel stasis, and fluid sequestration in the bowel lumen can lead to hypovolemia and electrolyte imbalance.
- The nurse must monitor fluid intake/output, vital signs, and administer IV fluids as prescribed.
3️⃣ Imbalanced Nutrition: Less than Body Requirements related to inability to ingest and absorb nutrients
- Due to vomiting and impaired bowel function, patients are unable to meet their nutritional needs.
- The nurse should monitor nutritional status, body weight, and collaborate with a dietitian to provide appropriate nutritional support.
4️⃣ Anxiety related to acute illness, hospitalization, and fear of complications or surgery
- Many patients with I.O. feel anxious and fearful due to the sudden onset of symptoms and possible need for surgery.
- The nurse should provide emotional support, clear communication about care plans, and encourage family involvement.
Q.3 Write short notes on the following (any four) (4×4=16)
a) Ulcerative colitis
Definition
Ulcerative colitis is a chronic inflammatory bowel disease (IBD) that causes inflammation and ulcer formation in the mucosal and submucosal layers of the colon and rectum.
It typically begins in the rectum and may extend continuously throughout the entire colon, leading to bloody diarrhea, abdominal pain, and systemic symptoms.
Causes (Etiology)
- Exact cause unknown
- Possible genetic factors
- Abnormal immune response
- Environmental triggers (infections, diet, stress)
- Family history of IBD
Pathophysiology
- The disease begins with inflammation in the mucosal layer of the rectum.
- The inflammation spreads proximally in a continuous manner to involve other parts of the colon.
- It leads to ulceration, edema, and bleeding in the colonic mucosa.
- This results in the production of pus, mucus, and blood in the stool.
- Over time, fibrosis and scarring may develop, leading to loss of elasticity and function of the colon.
- Chronic inflammation may also increase the risk of colorectal cancer in long-standing cases.
Clinical Manifestations
- Bloody diarrhea with mucus
- Abdominal pain and cramping
- Urgency to defecate, tenesmus
- Weight loss, fatigue
- Fever in severe cases
Diagnostic Evaluation
- History and physical exam
- Colonoscopy with biopsy (gold standard)
- Stool tests (rule out infection)
- CBC (anemia, WBC count)
- CRP, ESR (inflammation markers)
- Abdominal imaging (for complications)
Medical Management
- Aminosalicylates (5-ASA) such as sulfasalazine or mesalamine are used to reduce inflammation.
- Corticosteroids like prednisone are used in moderate to severe flares.
- Immunomodulators (azathioprine, 6-mercaptopurine) help maintain remission.
- Biologic agents (infliximab, adalimumab) target specific immune pathways and are used in refractory cases.
- Antibiotics may be used if secondary infection is suspected.
- In severe cases or complications, surgical management (colectomy) may be necessary.
Surgical Management
- Surgery is indicated in refractory disease, toxic megacolon, perforation, or dysplasia/cancer.
- Total proctocolectomy with ileal pouch-anal anastomosis (IPAA) is the preferred procedure.
- Permanent ileostomy may be required in some cases.
Nursing Management
Assessment and Monitoring
- The nurse must regularly assess frequency and characteristics of stools.
- Monitor for signs of dehydration, electrolyte imbalance, and nutritional status.
- Monitor vital signs for fever or hypotension.
Medication Administration
- Administer prescribed medications and monitor for side effects.
- Ensure adherence to medication regimen to maintain remission.
Dietary Care
- Encourage a low-residue, high-protein, high-calorie diet during flare-ups.
- Avoid trigger foods such as dairy, spicy foods, and caffeine.
Hydration and Skin Care
- Maintain adequate hydration, especially if diarrhea is severe.
- Provide skin care around the anal area to prevent irritation from frequent stools.
Emotional and Psychological Support
- Offer psychological support, as stress may exacerbate symptoms.
- Educate the patient on coping strategies and support group participation.
Post-Operative Care
- If surgery is performed, the nurse must provide stoma care education and psychosocial support.
b) Diabetic ketoacidosis
Definition
Diabetic ketoacidosis is an acute, life-threatening complication of uncontrolled diabetes mellitus, characterized by hyperglycemia, metabolic acidosis, and ketonemia. It occurs due to an absolute or relative deficiency of insulin, leading to increased lipolysis and production of ketone bodies.
Etiology
- Missed insulin dose
- Infection or stress (e.g., pneumonia, UTI)
- Newly diagnosed type 1 diabetes
- Myocardial infarction or surgery
- Use of steroids or beta-blockers
Pathophysiology
- In absence of insulin, glucose cannot enter the cells, resulting in cellular starvation despite high blood glucose.
- The body compensates by breaking down fats (lipolysis) for energy, producing free fatty acids.
- The liver converts these fatty acids into ketone bodies (acetoacetate, beta-hydroxybutyrate), causing ketonemia and ketonuria.
- Accumulation of ketones leads to metabolic acidosis, reflected in low blood pH and low bicarbonate levels.
- Hyperglycemia leads to osmotic diuresis, resulting in dehydration, electrolyte loss, and hypovolemia.
- If untreated, DKA can progress to coma, circulatory collapse, and death.
Clinical Manifestations
- Polyuria, polydipsia, dehydration
- Abdominal pain, nausea, vomiting
- Fruity breath odor (ketones)
- Kussmaul’s respiration
- Confusion or unconsciousness
Diagnostic Evaluation
- History collection
- Physical examination
- Blood glucose level (> 250 mg/dL)
- Serum ketone and urine ketone level (Positive serum and urine ketones)
- ABG analysis (Arterial pH < 7.3, low HCO₃)
- Elevated anion gap
- Serum electrolyte (↓Na⁺, ↓K⁺)
Management
1️⃣ Fluid Replacement
- Normal saline (0.9% NaCl) is administered to restore circulating volume.
- After initial bolus, switch to 0.45% saline based on hydration status.
- When glucose falls below 200 mg/dL, add 5% dextrose to prevent hypoglycemia.
2️⃣ Insulin therapy
- Administer IV regular insulin via infusion pump.
- Insulin promotes glucose uptake into cells and stops ketone production.
- Blood glucose is monitored hourly and insulin adjusted accordingly.
3️⃣ Electrolyte Replacement
- Potassium correction is critical even if serum potassium is high initially.
- Start K⁺ supplementation once urine output is adequate and levels fall <5.3 mEq/L.
- Monitor serum Na⁺, K⁺, Mg²⁺, phosphate frequently.
4️⃣ Acidosis Correction
- Most cases correct with fluids and insulin alone.
- Sodium bicarbonate IV is used only if pH < 6.9, with caution.
5️⃣ Treat Underlying Cause
- Start antibiotics if infection is suspected (e.g., UTI, pneumonia).
- Manage stressors like MI, surgery, trauma.
Nursing Management
1️⃣ Monitoring
- Monitor vital signs, level of consciousness, I&O, and capillary glucose hourly.
- Assess for signs of fluid overload or worsening acidosis.
- Monitor ECG for potassium-related arrhythmias.
2️⃣ Administer Medications
- Document dosage, response, and adverse effects.
- Administer IV insulin, fluids, electrolytes as per protocol.
- Watch for hypoglycemia as glucose drops.
3️⃣ Prevention of Complications
- Prevent cerebral edema with slow correction of hyperglycemia.
- Maintain aseptic technique with IV lines and catheters.
- Prevent pressure sores with regular repositioning.
4️⃣ Health Education
- Teach patient about glucose monitoring, diet, hydration, and medication adherence.
- Educate on early signs of DKA like nausea, fruity breath, increased urination.
- Stress importance of sick-day rules: never skip insulin even during illness.
Complications of DKA
- Cerebral edema (especially in children)
- Hypokalemia or hyperkalemia
- ARDS (acute respiratory distress syndrome)
- Severe hypotension or shock
- Coma or death if untreated
c) Hyperkalemia
Definition
- Hyperkalemia is a medical condition characterized by an abnormally high concentration of potassium (K⁺) in the blood, typically defined as a serum potassium level greater than 5.0 mEq/L.
- Potassium is vital for neuromuscular function and cardiac rhythm, so elevated levels can cause life-threatening arrhythmias and muscle dysfunction.
Causes
- Renal failure – decreased potassium excretion
- Potassium-sparing diuretics (e.g., spironolactone)
- Excess potassium intake (oral or IV)
- Adrenal insufficiency (e.g., Addison’s disease)
- Cell lysis – burns, trauma, tumor lysis
- Metabolic acidosis – shifts K⁺ out of cells
- Uncontrolled diabetes mellitus – insulin deficiency
- Drugs – ACE inhibitors, NSAIDs, heparin
- Blood transfusion-related hemolysis
- Lab error – pseudohyperkalemia
Clinical Manifestations
- Muscle weakness and flaccid paralysis
- Paresthesia (tingling or numbness)
- Nausea, vomiting, and abdominal cramps
- Bradycardia and hypotension
- ECG changes: peaked T-waves, wide QRS, flat or absent P waves
- Risk of ventricular fibrillation or cardiac arrest in severe cases
- Fatigue, confusion, and anxiety
- Respiratory muscle weakness (in advanced cases)
Diagnostic Evaluation
- History collection
- Physical examination
- Serum potassium level >5.0 mEq/L
- ECG monitoring for cardiac changes
- Renal function tests: BUN, Creatinine
- ABG: may show metabolic acidosis
- Blood glucose and insulin levels (in diabetics)
Medical Management
- Immediate treatment includes IV calcium gluconate, which stabilizes cardiac membranes.
- Insulin with glucose is given to shift potassium into cells and lower serum levels quickly.
- Beta-agonists (e.g., albuterol) may also help promote intracellular potassium uptake.
- Sodium bicarbonate is used if acidosis is present.
- Loop diuretics (e.g., furosemide) are administered to promote potassium excretion via urine.
- In severe cases, hemodialysis is the most effective way to remove excess potassium.
- Potassium binders (e.g., sodium polystyrene sulfonate or patiromer) are used to bind potassium in the gut for excretion.
NURSING MANAGEMENT OF PATIENT WITH HYPERKALEMIA
1. Assessment and Monitoring Responsibilities
- It is the nurse’s responsibility to assess the patient’s clinical condition regularly, including any signs of fatigue, muscle weakness, or numbness.
- She should monitor the patient’s cardiac status continuously using ECG, as hyperkalemia can cause fatal arrhythmias.
- The nurse must monitor serum potassium levels, along with renal function tests like BUN and creatinine.
- It is essential to observe for changes in mental status, respiratory pattern, or any flaccid paralysis, which may suggest worsening condition.
- The nurse should track intake and output records accurately to evaluate kidney function and guide fluid therapy.
2. Medication Administration
- The nurse should administer medications as prescribed, such as IV calcium gluconate, insulin with dextrose, sodium bicarbonate, or loop diuretics (like furosemide).
- She must monitor blood glucose levels after insulin administration to prevent hypoglycemia.
- If sodium polystyrene sulfonate (Kayexalate) is ordered, the nurse should monitor for bowel movement and assess for signs of constipation or diarrhea.
- She must prepare the patient for emergency dialysis, if indicated, and ensure that all emergency resuscitation equipment is available at bedside.
3. Dietary Management and Patient Education
- The nurse must educate the patient about potassium-restricted diets, advising to avoid foods high in potassium such as bananas, oranges, spinach, potatoes, tomatoes, coconut water, and dry fruits.
- She must encourage proper fluid intake unless restricted, and educate the patient on importance of regular monitoring of serum potassium levels.
- Educate patients with renal failure or diabetes about the risk factors and medication compliance to prevent recurrence of hyperkalemia.
4. Prevention of Complications and Safety Measures
- The nurse must ensure fall precautions and side railings if the patient is weak or dizzy.
- She should evaluate for signs of bradycardia, palpitations, and hypotension and report immediately.
- The nurse must collaborate with the multidisciplinary team, including physicians and dieticians, for coordinated care.
- Ensure the environment is calm and supportive, especially if the patient is anxious or confused due to electrolyte imbalance.
5. Documentation and Evaluation
- The nurse must document vital signs, ECG changes, potassium values, medications administered, and patient response carefully.
- She should evaluate the effectiveness of interventions and adjust care plans as needed.
- Ongoing communication with the healthcare team and family ensures that treatment goals are met and understood by all.
d) cystic fibrosis
Definition
Cystic Fibrosis is a chronic, inherited, autosomal recessive disorder that affects the exocrine glands, leading to the production of abnormally thick and sticky mucus, primarily affecting the respiratory, gastrointestinal, and reproductive systems.
Etiology
- Caused by mutation in CFTR gene (Cystic Fibrosis Transmembrane Conductance Regulator).
- Inherited in autosomal recessive pattern.
- Common mutation: ΔF508 gene deletion.
Pathophysiology
- The CFTR gene controls the movement of chloride and sodium ions across epithelial cells.
- Mutation leads to dysfunction of chloride channels, resulting in dehydrated and viscous mucus in airways and ducts.
- Thick mucus obstructs the bronchi, pancreatic ducts, intestines, and reproductive tract.
- In the lungs, mucus causes airway obstruction, chronic infection, and bronchiectasis.
- In the pancreas, blockage prevents enzyme release, leading to malabsorption and malnutrition.
- Sweat glands excrete excessive salt, causing electrolyte imbalance.
- Progressive damage causes respiratory failure, the leading cause of death in CF patients.
Clinical Manifestations
- Persistent cough with thick sputum
- Frequent lung infections (pneumonia/bronchitis)
- Failure to thrive, poor weight gain
- Salty-tasting skin
- Bulky, greasy stools (steatorrhea)
- Digital clubbing
Diagnostic Evaluation
- History collection
- Physical examination
- Sweat chloride test (gold standard)
- Genetic testing for CFTR mutation
- Chest X-ray or CT (for bronchiectasis)
- Pulmonary function tests
- Stool analysis for fat content
Management
Airway Clearance Therapies
- Chest physiotherapy, postural drainage, and percussion help mobilize thick mucus.
- Mechanical vests or flutter devices improve mucus clearance.
- Nebulized saline and mucolytics (Dornase alfa) thin the mucus.
Antibiotic Therapy
- Inhaled antibiotics like tobramycin or aztreonam target Pseudomonas infections.
- Oral or IV antibiotics during acute exacerbations.
- Long-term macrolides (azithromycin) used for anti-inflammatory effect.
Pancreatic Enzyme Replacement Therapy (PERT)
- Oral enzymes (lipase, protease, amylase) taken with meals to aid digestion.
- Helps in improving weight and nutritional status.
Nutritional Support
- High-calorie, high-protein diet.
- Fat-soluble vitamin supplements (A, D, E, K).
- Salt supplementation especially in hot climates or during fever.
CFTR Modulators
- Targeted therapy (e.g., Ivacaftor, Lumacaftor, Tezacaftor, Elexacaftor) improves CFTR protein function in specific mutations.
- These drugs have revolutionized CF management in eligible patients.
Other Supportive Treatments
- Bronchodilators for wheezing.
- Anti-inflammatory agents (e.g., ibuprofen).
- Oxygen therapy for hypoxia.
- Lung transplantation in end-stage disease.
Nursing Management
Respiratory Support
- Assist in daily airway clearance techniques.
- Monitor for signs of respiratory distress and infection.
- Administer nebulizations and monitor oxygen saturation.
Nutritional Care
- Encourage high-calorie, protein-rich diet.
- Monitor weight and growth patterns.
- Ensure proper intake of enzymes and vitamins.
Medication Adherence
- Educate family about long-term medication use and CFTR modulators.
- Monitor for adverse effects and drug compliance.
Psychosocial Support
- Provide emotional support to child and family.
- Promote age-appropriate education and social interaction.
- Address body image concerns, especially in adolescents.
Infection Prevention
- Practice strict hand hygiene and isolation precautions.
- Educate on avoiding crowded places and contact with other CF patients.
Complications
- Bronchiectasis
- Respiratory failure
- CF-related diabetes mellitus
- Infertility (especially in males)
- Liver disease (biliary cirrhosis)
- Osteoporosis
e) Hormonal replacement therapy
Definition
- Hormonal Replacement Therapy (HRT) is a medical treatment in which female sex hormones like estrogen and/or progesterone are administered artificially to compensate for hormonal deficiency, especially in menopausal or postmenopausal women, to relieve symptoms and prevent long-term complications such as osteoporosis.
- It is also used in conditions of premature ovarian failure, surgical menopause, or hormonal imbalances, and sometimes in males with androgen deficiency.
Types of Hormonal Replacement Therapy
1️⃣ Estrogen Therapy
- Estrogen is the primary hormone used in HRT and is essential for managing vasomotor symptoms (like hot flashes and night sweats), vaginal atrophy, and osteoporosis prevention.
- It is given to women who have undergone hysterectomy, as they are not at risk for endometrial cancer.
- Estrogen can be administered in various forms such as oral tablets (e.g., conjugated equine estrogen), transdermal patches (e.g., estradiol), topical gels, or vaginal rings.
- It works by replenishing the low estrogen levels in postmenopausal women, thereby maintaining bone density, vaginal health, and mood stabilization.
2️⃣ Progesterone / Progestin Therapy
- Progesterone (or its synthetic version, progestin) is used in combined HRT for women who still have an intact uterus, to protect the endometrium from the stimulating effects of estrogen and prevent endometrial hyperplasia or cancer.
- It is usually given along with estrogen in cyclical (monthly) or continuous regimens.
- Progesterone may be administered orally (e.g., medroxyprogesterone acetate), vaginally, or through intrauterine devices like levonorgestrel-releasing IUDs.
- It helps in regulating menstrual-like bleeding and ensures hormonal balance, reducing the risk of uterine abnormalities.
3️⃣ Estrogen + Progesterone Combination Therapy
- Combined therapy includes both estrogen and progesterone and is suitable for women with a uterus to reduce menopausal symptoms while ensuring protection of the endometrium.
- It is available as oral pills, transdermal patches, or combinations that mimic natural cycles.
- This combination helps to manage hot flashes, vaginal dryness, irritability, sleep disturbance, and mood fluctuations.
- It also provides bone protection and reduces the risk of fractures in postmenopausal women.
4️⃣ Tibolone
- Tibolone is a synthetic steroid with estrogenic, progestogenic, and androgenic effects and is prescribed to postmenopausal women as an alternative to traditional HRT.
- It helps in the reduction of menopausal symptoms, improves sexual function, and prevents bone loss.
- It is taken as a once-daily oral tablet and is particularly useful in women who are more than 12 months postmenopausal.
- Tibolone does not induce cyclical bleeding, which improves compliance in many women.
Indications of HRT
- It is used to relieve menopausal symptoms such as hot flashes, mood swings, insomnia, vaginal dryness, and fatigue.
- It is used in osteoporosis prevention and treatment in postmenopausal women.
- It is prescribed in cases of premature menopause or ovarian insufficiency, often seen in younger women.
- It is used in surgical menopause following bilateral oophorectomy (removal of ovaries).
- It may also be used in hypogonadism or Turner’s syndrome to induce puberty in adolescent girls.
Contraindications of HRT
- It is contraindicated in patients with a history of breast or endometrial cancer, due to risk of recurrence.
- It should not be given in patients with unexplained vaginal bleeding, which needs evaluation first.
- It is avoided in active or past thromboembolic disease like DVT or pulmonary embolism.
- It should not be used in patients with severe liver disease or dysfunction.
- It is contraindicated in women with known or suspected pregnancy.
Benefits of HRT
- It significantly reduces vasomotor symptoms such as hot flashes and night sweats.
- It improves genitourinary symptoms, like vaginal dryness, urinary urgency, and discomfort during intercourse.
- It helps in preserving bone density, thus preventing fractures and osteoporosis.
- It may improve mood, sleep, and overall quality of life in postmenopausal women.
- In some cases, it may help in cognitive function and memory, although evidence is mixed.
Risks and Side Effects of HRT
- It increases the risk of venous thromboembolism (blood clots), especially in older women or those with risk factors.
- Prolonged use, particularly of combined HRT, can raise the risk of breast cancer.
- It may cause bloating, breast tenderness, nausea, and headache in some women.
- It can lead to irregular bleeding during the early months of therapy.
- In some cases, gallbladder disease and stroke risk may be slightly increased.
Nursing Responsibilities in Hormonal Replacement Therapy (HRT):
- Assess complete medical, surgical, menstrual, and family history before starting HRT.
- Educate the patient about the purpose, types, dosage, route, and duration of hormone therapy.
- Explain possible side effects like nausea, breast tenderness, bloating, and breakthrough bleeding.
- Monitor vital signs, weight, blood pressure, and any signs of fluid retention or edema.
- Observe for early warning signs like chest pain, leg swelling, shortness of breath, or abnormal vaginal bleeding.
- Ensure proper administration of oral tablets, transdermal patches, vaginal creams, or rings.
- Encourage compliance by helping patients understand their dosing schedule and regimen (cyclic or continuous).
- Instruct the patient to avoid smoking and alcohol during HRT due to increased cardiovascular risk.
- Promote regular screening including mammograms, Pap smears, liver function tests, and bone density scans.
- Provide emotional and psychological support regarding body image changes and menopause-related distress.
- Encourage calcium and vitamin D intake, physical activity, and healthy lifestyle for bone protection.
- Maintain accurate and confidential documentation of all patient interactions, side effects, and progress.
