24/07/2019-B.SC-MEDICAL SURGICAL-2-UPLOAD-PAPERNO.1
ADULT HEALTH NURSING-2-UPLOAD-PAPER SOLUTION NO.1
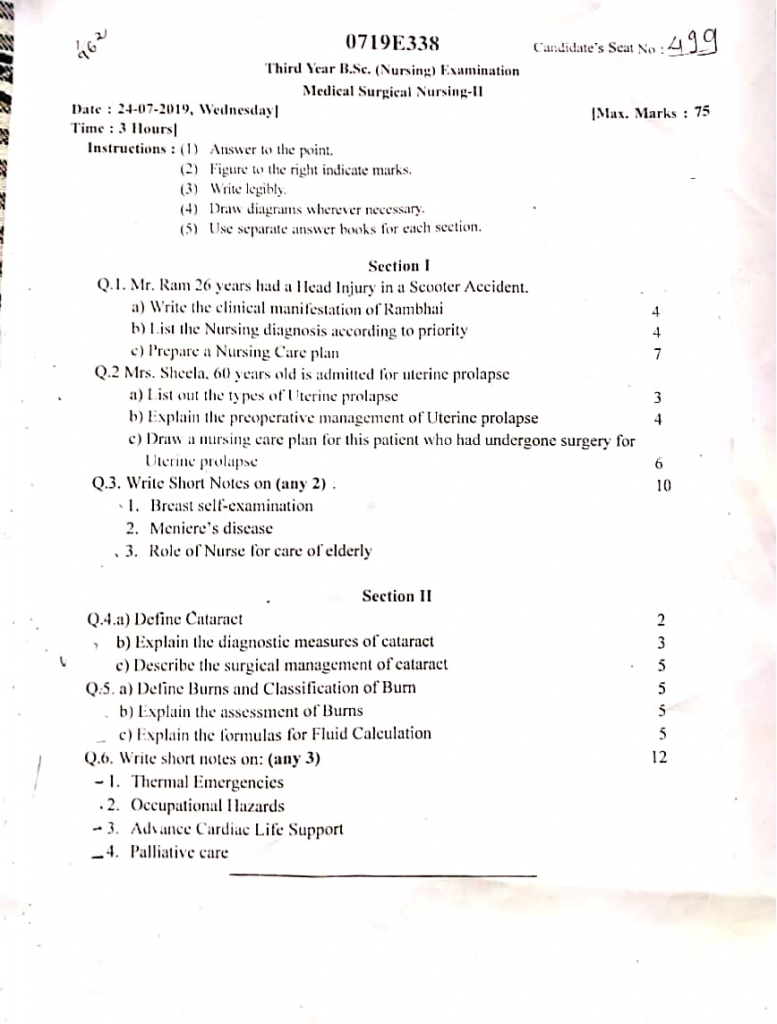
Section 1
Q.1 Mr. Ram 26 years had a head injury in a scooter accident.
1. Write the clinical manifestation of rambhai (4)
- It is observed that Mr. Ram has altered level of consciousness, which may range from confusion and disorientation to unconsciousness depending on the severity of the head injury.
- It is noted that Mr. Ram is experiencing projectile vomiting, which is a classical sign of increased intracranial pressure and requires immediate neurological assessment.
- It is evident that Mr. Ram had a history of transient loss of consciousness following the accident, indicating possible cerebral concussion or contusion.
- It is seen that Mr. Ram may have bleeding from the ear or nose, which can suggest a base of skull fracture and needs urgent evaluation.
- It is possible that Mr. Ram shows signs of pupillary changes, such as unequal pupils (anisocoria) or sluggish reaction to light, which may reflect pressure on cranial nerves.
- It is also noticed that Mr. Ram may complain of severe headache, which is a common symptom due to trauma, swelling, or internal bleeding.
- It is likely that Mr. Ram may show weakness or paralysis of limbs, depending on the area of the brain affected (hemiparesis or hemiplegia).
- It is seen that Mr. Ram may demonstrate abnormal posturing, such as decerebrate or decorticate postures, which are serious signs of brain stem involvement.
- It is expected that Mr. Ram may experience seizures or convulsions, due to cortical irritation following trauma.
- It is common that Mr. Ram may have external signs of injury, like scalp laceration, bruising (e.g., Battle’s sign or raccoon eyes), or swelling over the head.
2. List the nursing diagnosis according to priority (4)
- Ineffective cerebral tissue perfusion related to cerebral edema or bleeding
- Risk for increased intracranial pressure related to head trauma
- Impaired physical mobility related to decreased level of consciousness or motor deficit
- Acute pain related to tissue trauma and swelling
- Risk for aspiration related to altered level of consciousness
- Impaired verbal communication related to brain injury
- Risk for infection related to open wound or invasive devices
- Disturbed sensory perception related to neurological impairment
- Risk for disturbed sleep pattern related to hospital environment and pain
- Anxiety (family) related to critical condition and uncertain prognosis
3. Prepare a nursing care plan (7)
Ineffective cerebral tissue perfusion related to cerebral edema
Goal :
Mr. Ram will maintain adequate cerebral perfusion as evidenced by stable GCS and normal vital signs.
Nursing Interventions :
- Monitor Glasgow Coma Scale (GCS) every 2–4 hours.
- Elevate head of bed to 30° to reduce intracranial pressure (ICP).
- Administer osmotic diuretics like mannitol as prescribed.
- Provide supplemental oxygen to maintain SpO₂ > 95%.
- Reduce external stimulation (lights, noise, visitors).
- Maintain fluid balance chart and restrict fluids if prescribed.
- Monitor serum electrolytes to prevent imbalances that can affect brain function.
- Assess for changes in pupil size and responsiveness every shift.
Risk for increased intracranial pressure (ICP)
Goal :
Mr. Ram will not show signs of increased ICP (no vomiting, no pupil changes).
Nursing Interventions :
- Assess for early signs of increased ICP (headache, vomiting, behavior change).
- Avoid neck flexion, straining, coughing, and suctioning.
- Monitor blood pressure, pulse pressure, and respiratory pattern closely.
- Ensure HOB remains elevated unless contraindicated.
- Notify physician of any rapid changes in condition.
- Keep the room quiet and dim to minimize sensory overload.
- Administer anticonvulsants to prevent seizure-related ICP spikes.
- Monitor for Cushing’s triad: bradycardia, irregular respirations, and widening pulse pressure.
Acute pain related to tissue injury
Goal :
Mr. Ram will verbalize pain relief and appear comfortable.
Nursing Interventions :
- Assess pain level using appropriate pain scale.
- Administer prescribed analgesics like acetaminophen or opioids.
- Use non-pharmacological measures like ice pack if indicated.
- Maintain quiet and dim lighting to reduce discomfort.
- Reassess pain after medication for effectiveness.
- Provide gentle head positioning to avoid strain.
- Offer emotional support and reassurance.
- Teach relaxation techniques such as deep breathing if patient is conscious.
Impaired physical mobility
Goal :
Mr. Ram will maintain joint flexibility and skin integrity.
Nursing Interventions :
- Reposition every 2 hours to prevent pressure injuries.
- Perform passive range-of-motion (ROM) exercises twice daily.
- Use pressure-relieving mattress or foam pads.
- Monitor skin for redness, breakdown, or ulceration.
- Encourage physiotherapy as condition improves.
- Place splints or footboards to prevent foot drop.
- Maintain nutritional intake to support tissue healing.
- Assess for signs of DVT: calf pain, swelling, and warmth.
Risk for aspiration
Goal :
Mr. Ram will remain free from aspiration episodes.
Nursing Interventions :
- Maintain semi-Fowler’s or lateral position.
- Keep NPO status until gag reflex is assessed.
- Provide suctioning as required.
- Monitor for coughing, wet voice, or respiratory distress.
- Use nasogastric feeding only after proper placement verification.
- Refer to speech therapist for swallowing evaluation.
- Provide oral hygiene to reduce bacterial colonization.
- Monitor respiratory rate, sounds, and SpO₂ continuously.
Impaired verbal communication
Goal :
Mr. Ram will demonstrate effective alternative communication methods.
Nursing Interventions :
- Use picture boards, writing tools, or simple gestures.
- Speak slowly, clearly, and maintain eye contact.
- Allow extra time for patient to respond.
- Document effective communication techniques used.
- Involve family members in interpretation and support.
- Use yes/no questions to simplify interaction.
- Observe nonverbal cues like facial expressions or eye movement.
- Offer reassurance even if the patient cannot reply.
Risk for infection
Goal :
Mr. Ram will remain free from infection during hospital stay.
Nursing Interventions :
- Use strict hand hygiene and PPE.
- Monitor temperature and WBC count.
- Change dressings with aseptic technique.
- Observe wound sites for redness, swelling, or discharge.
- Administer antibiotics as prescribed.
- Ensure timely catheter and IV site care.
- Provide perineal care if incontinent.
- Educate family about infection prevention during visits.
Disturbed sensory perception
Goal :
Mr. Ram will respond appropriately to sensory stimuli.
Nursing Interventions :
- Orient patient to time, place, and person regularly.
- Provide familiar objects or family voice recordings.
- Reduce environmental noise and dim lights.
- Limit number of visitors to avoid confusion.
- Encourage simple verbal stimulation during care.
- Monitor for hallucinations or confusion.
- Use clocks and calendars to help reorientation.
- Maintain consistent caregiving staff when possible.
Risk for disturbed sleep pattern
Goal :
Mr. Ram will report improved rest and show signs of sleep.
Nursing Interventions :
- Cluster nursing activities to avoid frequent sleep interruption.
- Maintain quiet and dark environment at night.
- Provide comfort measures like soft pillow or warm blanket.
- Limit caffeine intake and avoid unnecessary monitoring at night.
- Offer warm drinks or relaxation before sleep (if allowed).
- Encourage family to speak softly during visits.
- Avoid unnecessary alarms and noise from machines.
- Administer sleep aids if prescribed.
Q.2 Mrs. Sheela 60 years old is admitted for uterine prolepse
1. List out the types of uterine prolepse (3)
Uterine prolapse is classified into three main degrees based on the extent to which the uterus descends through the vaginal canal:
1️⃣ First-Degree Uterine Prolapse
- It is the mildest form of prolapse, where the uterus descends slightly, but the cervix remains within the vaginal canal and does not reach the vaginal opening.
- This type may be asymptomatic or cause mild pelvic pressure, especially when standing or coughing.
2️⃣ Second-Degree Uterine Prolapse
- In this type, the uterus descends further down, and the cervix protrudes at or near the vaginal opening, particularly on straining or standing.
- The patient may complain of a visible bulge, backache, urinary frequency, or difficulty during intercourse.
3️⃣ Third-Degree Uterine Prolapse (Complete Prolapse)
- This is the most severe form, where the entire uterus, including the cervix, protrudes outside the vaginal opening and is visible externally.
- The condition is often associated with difficulty in walking, sitting, urinary retention, and ulceration of the exposed tissue.
2. Explain the preoperative management of uterine prolepse (4)
Preoperative management of uterine prolapse involves a series of nursing and medical interventions that are aimed at optimizing the patient’s physical and psychological condition, preventing complications, and preparing the patient for surgery such as vaginal hysterectomy or pelvic floor repair.
1️⃣ Comprehensive Patient Assessment Must Be Performed
- It is important for the nurse or physician to take a detailed medical, surgical, obstetric, and gynecological history, including the duration and severity of prolapse symptoms.
- A general physical examination and pelvic examination must be done to assess the degree of prolapse, vaginal health, and presence of any ulceration or infection.
2️⃣ Necessary Laboratory and Diagnostic Investigations Should Be Conducted
- Blood investigations such as complete blood count (CBC), blood sugar levels, urine analysis, blood group, and coagulation profile should be done to assess overall fitness for surgery.
- ECG and chest X-ray may be advised in women over 40 years to rule out any underlying cardiopulmonary conditions.
- Pelvic ultrasound or urodynamic studies may be ordered to evaluate associated pathologies like cystocele, rectocele, or urinary incontinence.
3️⃣ Vaginal Hygiene and Local Infections Should Be Treated
- Any vaginal discharge, infection, or ulceration must be treated with appropriate antibiotics, antiseptic vaginal douches, or estrogen creams to improve tissue healing before surgery.
- Local estrogen therapy may be given in postmenopausal women to improve the tone and vascularity of the vaginal tissues.
4️⃣ Bowel Preparation and Bladder Care Must Be Initiated
- The bowel must be emptied using mild laxatives, enemas, or rectal suppositories the night before surgery to avoid straining and reduce bowel handling.
- The patient should be instructed to void urine before shifting to the operation theatre, and a urinary catheter may be inserted as per protocol.
5️⃣ Preoperative Consent and Psychological Preparation Are Essential
- The procedure must be explained clearly to the patient and family, including the type of surgery, risks, expected outcomes, and recovery.
- Obtain written informed consent after explaining the nature of the surgical procedure and possible complications.
- Psychological support and reassurance must be given to reduce anxiety and address fears about uterus removal, sexual function, or body image.
6️⃣ Preoperative Fasting and Medication Instructions Must Be Followed
- The patient must remain nil by mouth (NPO) for at least 6–8 hours prior to surgery to prevent aspiration under anesthesia.
- Preoperative medications, such as antibiotics, sedatives, and antacids, should be given as prescribed by the surgeon or anesthetist.
7️⃣ Skin Preparation and Personal Hygiene Should Be Maintained
- Shaving or clipping of the perineal and abdominal area may be performed to reduce infection risk.
- A preoperative antiseptic bath using betadine or chlorhexidine solution is encouraged for skin hygiene.
8️⃣ Anesthesia Assessment Must Be Completed
- A pre-anesthetic check-up (PAC) must be done to assess airway, allergies, comorbidities, and anesthesia risks.
- The anesthetist may decide between regional (spinal or epidural) or general anesthesia, depending on the case and patient condition.
9️⃣ Preoperative Teaching Should Be Provided
- Teach the patient about deep breathing exercises, leg movements, and post-operative care routines to reduce complications like DVT and pneumonia.
- Explain the importance of pelvic floor exercises (Kegel’s) after surgery to strengthen pelvic support.
3. Draw a nursing care plan for this patient who had undergone surgery for uterine prolepse (6)
Assessment Data
- Patient complains of pain in the lower abdomen post-hysterectomy.
- Presence of urinary catheter and surgical dressing in the perineal region.
- Observed restricted mobility and mild emotional distress.
- Reports concern about future physical ability and body image.
- Needs education on postoperative care and recovery at home.
Acute Pain related to surgical intervention as evidenced by patient’s verbal report and guarded movements.
Goal :
- The patient will report a decrease in pain level from 8/10 to 3/10 within 24–48 hours postoperatively.
Nursing Interventions :
- Assess pain characteristics using a numeric rating scale every 4 hours.
- Administer prescribed analgesics as per physician’s order to reduce pain and improve comfort.
- Encourage relaxation techniques such as guided breathing or music therapy to reduce pain perception.
- Position the patient comfortably with a supportive pillow under knees to relieve abdominal pressure.
- Monitor the surgical site for swelling, bleeding, or signs of infection that may worsen pain.
- Educate the patient about the importance of early pain reporting to avoid escalation.
- Use non-drug methods like warm compresses and maintain a calm environment for rest.
- Observe for side effects of analgesics like nausea or rashes and inform the doctor.
Evaluation :
- Patient reported relief in pain, showed improved participation in activities, and required fewer analgesics over 48 hours.
Risk for Infection related to surgical incision and urinary catheter.
Goal :
- The patient will remain free from infection, with no fever, purulent discharge, or wound complications during hospitalization.
Nursing Interventions :
- Practice strict hand hygiene before and after patient contact.
- Perform surgical dressing change using aseptic technique and prescribed antiseptics.
- Observe for fever, redness, or foul-smelling discharge at incision site.
- Administer prophylactic antibiotics as ordered and monitor for adverse reactions.
- Maintain the urinary drainage bag below bladder level and ensure catheter is not obstructed.
- Reinforce perineal hygiene, especially after toileting or lochia discharge.
- Instruct the patient and attendants in proper handwashing and pad changing.
- Encourage fluid intake to prevent urinary tract infection unless contraindicated.
Evaluation :
- No signs of infection noted; temperature remained normal, and the incision site was clean and dry on review.
Impaired Physical Mobility related to post-surgical discomfort and restricted movement.
Goal :
- The patient will gradually regain mobility and ambulate with minimal assistance within 3 days post-surgery.
Nursing Interventions :
- Assist the patient with turning and repositioning every 2 hours to prevent pressure injuries.
- Encourage leg exercises and ankle movements while in bed to prevent DVT.
- Help the patient to sit on the bed edge and walk slowly with support.
- Provide verbal encouragement to boost confidence in early mobilization.
- Educate the patient about avoiding heavy lifting and long standing post-discharge.
- Perform deep breathing exercises to prevent respiratory complications from immobility.
- Ensure obstacle-free pathways to prevent falls and accidents during walking.
- Collaborate with physiotherapy services if ambulation is delayed beyond expected recovery.
Evaluation :
- The patient was able to walk short distances with support by the third postoperative day.
Disturbed Body Image related to surgical removal of uterus and change in reproductive identity.
Goal :
- The patient will demonstrate positive coping and verbalize acceptance of physical changes by discharge.
Nursing Interventions :
- Provide non-judgmental emotional support and a listening ear to explore patient’s fears.
- Normalize the emotional reaction and offer reassurance about sexual and social functioning.
- Involve supportive family members or spouse in counseling sessions if patient consents.
- Offer information about pelvic floor exercises and resumption of sexual activity after recovery.
- Provide access to psychological counseling or support groups if patient expresses emotional distress.
- Involve the patient in small daily choices to promote a sense of control over her body.
- Give realistic reassurance that femininity is not defined solely by the uterus.
- Provide leaflets or videos explaining recovery stages to reduce anxiety.
Evaluation :
- The patient reported improved self-confidence, interacted positively, and showed psychological readiness for discharge.
Deficient Knowledge related to postoperative self-care and discharge regimen.
Goal :
- The patient will demonstrate understanding of self-care measures and verbalize key discharge instructions correctly.
Nursing Interventions :
- Educate the patient about perineal care, hygiene, and pad changes after surgery.
- Explain warning signs like excessive bleeding, discharge, or fever that require medical attention.
- Instruct about activity limitations, including avoiding lifting, intercourse, and prolonged standing.
- Provide written discharge instructions in simple language with pictorial guides.
- Explain the importance of follow-up visits and when to seek emergency care.
- Include family members or caregivers in teaching sessions to ensure home support.
- Encourage the patient to repeat back key points to confirm understanding.
- Offer contact information for post-discharge queries or complications.
Evaluation :
- The patient and caregiver were able to explain all self-care instructions, and agreed to attend follow-up appointments.
Q.3 Write short notes (any two) (10 marks)
1. Breast self examination
Definition
- It is a simple, non-invasive method in which a woman examines her own breasts regularly for any unusual changes in appearance or texture, in order to detect breast abnormalities such as lumps, skin dimpling, or nipple discharge, which may be an early sign of breast cancer.
- It is a procedure by which a woman systematically inspects and palpates her breasts using her own hands and eyes to detect any changes or abnormalities.
- It is considered a primary screening method for breast cancer, especially in low-resource settings.
- It is a preventive health measure recommended for women starting from 20 years of age, performed once every month.
- It helps in developing awareness of normal breast consistency, so changes can be quickly identified.
PURPOSE / OBJECTIVES OF BSE
- To detect early signs of breast cancer such as lumps, pain, or skin changes.
- To enable a woman to become familiar with the normal structure and texture of her breasts.
- To promote responsibility and self-awareness about breast health.
- To serve as a supplement to clinical breast examination (CBE) and mammography.
- To identify any visible or palpable abnormality so that medical care can be sought promptly.
IDEAL TIME FOR BSE
- In menstruating women, the best time to perform BSE is 7 to 10 days after the onset of menstruation, when breast tissue is least tender or swollen.
- In post-menopausal women, BSE should be performed on the same date every month to maintain regularity.
- Women on oral contraceptives are advised to perform BSE on a fixed day during their pill cycle.
- It should be performed monthly, as regular checks help recognize new or unusual changes more easily.
STEPS OF BREAST SELF-EXAMINATION
BSE involves visual inspection and manual palpation in both standing and lying positions.
A. VISUAL INSPECTION (Performed in front of a mirror)
- The woman should undress from the waist up and stand in front of a mirror with arms relaxed at her sides.
- She should inspect for any visible asymmetry, lumps, swelling, or skin changes such as dimpling, puckering, or redness.
- Next, she should raise both arms overhead and observe for the same changes again.
- Then she should press her hands firmly on her hips and slightly bend forward to contract the chest muscles.
- In each step, she should carefully observe both breasts for nipple changes (e.g., inversion, retraction, discharge).
B. MANUAL PALPATION (Using finger pads for touch examination)
While Standing or Bathing
- With the skin wet and soapy (which improves finger glide), she should raise her right arm.
- Using the pads of the three middle fingers of the left hand, she should palpate the right breast in small, circular motions.
- She should follow a pattern (circular, vertical strip, or wedge) to ensure full coverage of the breast tissue.
- The axillary area (underarm) should be palpated thoroughly for any enlarged lymph nodes.
- The process should be repeated for the left breast using the right hand.
While Lying Down
- She should lie on her back with a small pillow under her right shoulder and place her right arm behind her head.
- With her left hand, she should feel the right breast using gentle pressure at various depths (light for surface, medium for mid-level, and firm for deep tissue).
- She should move her fingers in a systematic manner, from the outer edge toward the nipple.
- The same steps should be repeated on the left side using the right hand.
- Lastly, she should gently squeeze each nipple to check for any discharge or fluid.
WHAT TO LOOK FOR DURING BSE
- New lump or mass in the breast or underarm area.
- Thickened areas or firm nodules that feel different from surrounding tissues.
- Changes in the shape or size of the breast.
- Skin changes like puckering, dimpling, or orange-peel texture (peau d’orange).
- Nipple abnormalities, including retraction, inversion, discharge (especially bloody or clear), or crusting.
- Persistent localized pain or tenderness in one breast or armpit.
- Swelling, warmth, or redness on the skin of the breast.
ADVANTAGES OF BSE
- It is cost-free, simple, and non-invasive.
- It empowers women to take responsibility for their own breast health.
- It helps in early detection, which improves treatment outcomes.
- It increases self-awareness and confidence in recognizing physical changes.
- It is especially useful in rural and resource-limited settings where mammography may not be available.
LIMITATIONS OF BSE
- BSE is not a substitute for clinical breast examination or mammography.
- It may lead to false alarms and unnecessary anxiety due to benign lumps.
- It may miss deep or small tumors, especially in obese women.
- Some women may lack confidence or proper technique in performing BSE correctly.
- It may cause delay in seeking medical care if symptoms are ignored or misinterpreted.
NURSING RESPONSIBILITIES IN PROMOTING BSE
✅ 1. Health Education and Awareness
- It is the nurse’s responsibility to create awareness about breast cancer and the importance of early detection through regular BSE.
- The nurse should explain that early-stage breast cancer often does not cause pain, so regular self-checks are essential.
- It is important to conduct individual or group education sessions during outpatient visits, health camps, antenatal clinics, and community health programs.
- The nurse should provide accurate, culturally sensitive information, especially in rural or less educated populations.
- Educational materials like charts, leaflets, posters, videos, or breast models should be used during teaching sessions.
✅ 2. Demonstration of Technique
- The nurse must demonstrate the correct steps of BSE practically, using breast models or visual aids.
- Each woman should be taught the systematic method of inspection and palpation, covering the entire breast and axillary area.
- The nurse must explain the importance of using finger pads, circular motion, and varying pressure for accurate palpation.
- She should teach women how to choose a fixed day each month for the examination and integrate it into their routine.
- The nurse should give clear, repeated instructions to ensure the woman learns the technique correctly.
✅ 3. Encouraging Routine Practice and Adherence
- It is the nurse’s duty to motivate and remind women to perform BSE every month consistently.
- She should help the woman overcome fear, embarrassment, or shyness, especially among adolescents or newly married women.
- The nurse can suggest using a calendar, diary, or phone alarm to remind them of their monthly BSE schedule.
- Women should be encouraged to include BSE as a regular part of their personal hygiene or self-care routine.
- Reinforcement during each follow-up visit helps to develop confidence and habit formation.
✅ 4. Assessment and Clarification
- The nurse should ask open-ended questions to assess the woman’s understanding of the BSE process.
- She must observe the woman’s demonstration, if possible, and correct any errors in hand movement, positioning, or technique.
- The nurse should evaluate whether the woman knows what signs to look for, such as lumps, nipple discharge, or skin changes.
- Misconceptions (e.g., BSE is not necessary without pain or symptoms) should be identified and corrected immediately.
✅ 5. Referral and Follow-Up Care
- If a woman finds any lump, change, or abnormality during BSE, the nurse must guide her to seek immediate medical evaluation.
- The nurse should assist in scheduling clinical breast examination, ultrasound, mammogram, or FNAC as advised.
- She must explain that not all lumps are cancerous, and further testing is necessary for accurate diagnosis.
- The nurse should provide emotional support and reduce anxiety during the waiting period for results.
- Documentation of the finding and referral must be done in the woman’s health record for future follow-up.
✅ 6. Role in Community and Public Health Settings
- Nurses working in community health centers, sub-centers, or urban health posts have a vital role in mass education about BSE.
- They can organize awareness camps during Breast Cancer Awareness Month (October) or local health events.
- Nurses should also involve ASHA, ANM, or women’s self-help groups in spreading awareness about breast self-examination.
- They can collaborate with NGOs and cancer screening programs to increase BSE practice coverage.
- Community-based teaching helps to reach underserved, tribal, and low-literacy populations.
2. Menieres disease
Definition of Ménière’s Disease
- It is a chronic inner ear disorder characterized by episodic vertigo, sensorineural hearing loss, tinnitus, and a feeling of fullness in the ear.
- It is associated with excess endolymphatic fluid (endolymph hydrops) in the inner ear, affecting the balance and hearing mechanisms.
- It is a relapsing and remitting condition, commonly affecting individuals between 40 to 60 years of age.
Types of Ménière’s Disease
1️⃣ Classical (Typical) Ménière’s Disease
- It is the form where all 4 major symptoms (vertigo, hearing loss, tinnitus, and ear fullness) are present.
- It occurs in repeated episodes, with symptoms resolving partially between attacks.
- It typically starts unilaterally, but may progress to bilateral involvement in 10–40% of cases.
2️⃣ Cochlear Ménière’s Disease
- It presents mainly with hearing symptoms, such as tinnitus and hearing loss, without vertigo.
- It may be an early stage or partial form of Ménière’s disease.
3️⃣ Vestibular Ménière’s Disease
- It involves primarily vertigo and balance disturbances without significant hearing loss.
- It may occur as an isolated balance disorder, especially in early stages.
Etiology
- Idiopathic (unknown cause)
- Excess endolymphatic fluid (hydrops)
- Viral infections (e.g., herpes virus)
- Autoimmune inner ear disease
- Allergies or food sensitivities
- Head or ear trauma
- Genetic predisposition
- Migraine-associated vertigo
Pathophysiology of Ménière’s Disease
1️⃣ Excess Endolymph Production or Impaired Absorption
It is the overproduction or blocked drainage of endolymph fluid in the membranous labyrinth that causes inner ear pressure.
2️⃣ Distension of Inner Ear Structures
It is the stretching of the endolymphatic sac and duct, which affects hair cells of cochlea and vestibular apparatus.
3️⃣ Abnormal Nerve Signal Transmission
It is due to the pressure and damage on sensory receptors, leading to distorted hearing and balance signals to the brain.
4️⃣ Recurrent Episodes of Vertigo and Hearing Disturbances
It causes temporary or progressive sensory deficits, with inflammatory or autoimmune responses possibly contributing.
5️⃣ Progressive Degeneration
It may lead to permanent hearing loss, chronic tinnitus, and debilitating balance issues if untreated.
Clinical Manifestations
- Recurrent episodes of vertigo (lasting 20 min to hours)
- Tinnitus (ringing or buzzing in ear)
- Sensorineural hearing loss (initially fluctuating, then permanent)
- Feeling of fullness or pressure in affected ear
- Nausea, vomiting (during vertigo episodes)
- Loss of balance or unsteadiness
- Anxiety and fatigue after attacks
Diagnostic Evaluation
- History collection
- Physical examination
- Audiometry (sensorineural hearing loss)
- Electronystagmography (ENG)
- Glycerol dehydration test
- Electrocochleography
- MRI (to rule out acoustic neuroma)
- History of ≥2 spontaneous vertigo episodes lasting ≥20 min
- Clinical symptom assessment
Medical Management
1️⃣ Lifestyle and Dietary Modifications
- It is advised to follow a low-sodium diet (<1500 mg/day) to reduce fluid retention.
- It is important to avoid caffeine, alcohol, and tobacco, which can aggravate symptoms.
- It is helpful to manage stress, as stress can trigger episodes.
2️⃣ Pharmacologic Therapy
- It includes Diuretics (e.g., hydrochlorothiazide) to reduce endolymphatic fluid pressure.
- Antihistamines (e.g., meclizine) and anticholinergics (e.g., scopolamine) help in controlling vertigo.
- Antiemetics (e.g., promethazine) are used during acute attacks to control nausea and vomiting.
- Benzodiazepines (e.g., diazepam) may be used short-term for severe vertigo episodes.
3️⃣ Vestibular Rehabilitation Therapy (VRT)
- It is a physical therapy program designed to improve balance, coordination, and adaptation to motion sensitivity.
- It is especially helpful in chronic or post-attack recovery phases.
4️⃣ Invasive Procedures and Surgery (for Refractory Cases)
- Intratympanic steroid injections may reduce inflammation and vertigo.
- Intratympanic gentamicin (ototoxic) may reduce vertigo but risk hearing loss.
- Endolymphatic sac decompression surgery is done to relieve fluid pressure.
- Vestibular nerve sectioning or labyrinthectomy is used in severe, drug-resistant cases.
Nursing Management
1️⃣ Assessment and Monitoring
- It is important to assess the frequency, duration, and severity of vertigo attacks.
- It is necessary to evaluate for hearing changes, tinnitus intensity, and gait stability.
- It is essential to monitor vital signs during an acute attack (risk of fall, hypotension due to vomiting).
2️⃣ Fall Prevention and Safety
- It is crucial to keep the patient in bed during vertigo attacks to prevent injury.
- It is advised to remove fall hazards, provide assistive devices, and ensure safe mobility during recovery.
- It is necessary to teach patients to move slowly when changing positions.
3️⃣ Medication Management
- It is the nurse’s responsibility to administer prescribed diuretics, anti-vertigo agents, and antiemetics.
- It is important to monitor fluid and electrolyte levels, especially during diuretic therapy.
- It is necessary to educate the patient about side effects, including drowsiness and dry mouth.
4️⃣ Psychosocial and Emotional Support
- It is essential to provide reassurance, as patients may feel anxious or depressed due to unpredictable attacks.
- It is helpful to involve family members in care and educate them about the condition.
- It is advised to provide support for occupational or vocational limitations if the disease becomes chronic.
5️⃣ Dietary and Lifestyle Education
- It is important to teach the importance of a low-sodium, caffeine-free diet.
- It is necessary to advise avoiding alcohol, smoking, and excess salt or sugar intake.
- It is helpful to emphasize stress reduction techniques, such as yoga, meditation, or breathing exercises.
6️⃣ Patient Education and Follow-up
- It is vital to teach patients about identifying triggers, recording symptom diaries, and adhering to treatment.
- It is necessary to inform about the importance of regular ENT check-ups and audiometry follow-up.
- It is helpful to explain that Ménière’s disease is manageable, but not completely curable.
3. Role of nurse for care of elederly
The role of the nurse in geriatric care includes holistic management of the elderly, addressing their physical, mental, emotional, and social needs while promoting independence and dignity.
✅ 1. Comprehensive Physical Assessment and Monitoring
- The nurse performs routine head-to-toe physical assessments to detect early signs of deterioration in elderly patients.
- She monitors chronic illnesses such as diabetes, hypertension, arthritis, and cardiac conditions through daily observations and scheduled investigations.
- The nurse evaluates the elderly person’s ability to perform ADLs (Activities of Daily Living) and determines the need for assistive support.
- She also screens for hearing loss, vision problems, oral health issues, and foot complications.
- The nurse observes for signs of elder abuse or neglect, especially in dependent or bedridden patients.
✅ 2. Medication Administration and Safety
- The nurse is responsible for accurate timing, dosage, and route of administration of prescribed medications.
- She monitors for adverse drug effects, allergic reactions, or overdose—especially in patients on multiple medications.
- The nurse maintains a medication administration record (MAR) to track compliance and modifications.
- She collaborates with physicians for regular medication review and deprescribing when appropriate.
- The nurse provides patient and caregiver teaching on the purpose and potential side effects of medications.
✅ 3. Nutritional Care and Hydration
- The nurse assesses the nutritional status by monitoring weight trends, BMI, and lab indicators like albumin and hemoglobin.
- She identifies and addresses chewing difficulties, poor dentition, or loss of taste which affect food intake.
- The nurse ensures dietary modifications for specific illnesses, such as low-sodium for hypertension or diabetic-friendly meals.
- She promotes supplementation of vitamins and minerals as required by the aging body.
- The nurse encourages mealtime support, upright positioning, and slow feeding to reduce aspiration risk.
✅ 4. Mobility Support and Fall Prevention
- The nurse assists elderly patients with daily ambulation, physiotherapy routines, and walking exercises to maintain mobility.
- She provides training on safe use of assistive devices such as canes, walkers, or wheelchairs.
- The nurse evaluates environmental safety, including non-slippery floors, grab bars, and clutter-free pathways.
- She observes for signs of dizziness or hypotension that may lead to falls during standing or walking.
- The nurse participates in institutional fall-prevention programs and uses fall-risk scoring tools.
✅ 5. Psychosocial and Emotional Support
- The nurse recognizes signs of depression, anxiety, grief, or hopelessness, and provides emotional support.
- She encourages participation in social gatherings, spiritual groups, or elderly day-care programs to avoid isolation.
- The nurse builds a trust-based relationship that allows the elderly to express fears or past memories.
- She coordinates with social workers to provide support systems for financially or emotionally neglected elders.
- The nurse facilitates family counseling sessions to improve intergenerational relationships and caregiving harmony.
✅ 6. Cognitive Support and Mental Health Monitoring
- The nurse routinely assesses for confusion, memory loss, disorientation, and behavioral changes.
- She uses tools like the Mini-Mental State Examination (MMSE) for cognitive screening.
- The nurse introduces mental stimulation techniques such as reality orientation, name recall, date charts, and music therapy.
- She helps establish routines for consistency and reduced anxiety, especially for Alzheimer’s patients.
- The nurse involves family in behavioral therapy and home safety planning for patients with cognitive decline.
✅ 7. Skin Integrity and Hygiene Care
- The nurse performs daily skin inspections for pressure areas and uses a Braden scale for pressure ulcer risk assessment.
- She ensures regular cleansing, moisturizing, and protective barriers to keep skin soft and infection-free.
- The nurse uses special mattresses, cushions, and heel protectors to reduce prolonged pressure.
- She maintains proper perineal care and incontinence hygiene, especially in bedridden patients.
- The nurse teaches caregivers about pressure sore staging and early signs of breakdown.
✅ 8. Bladder and Bowel Management
- The nurse encourages regular toileting and maintains a timed voiding schedule to avoid incontinence.
- She observes for signs of urinary retention, infection, or constipation, especially in immobile or post-operative patients.
- The nurse promotes pelvic floor exercises in cooperative patients to strengthen sphincter control.
- She ensures safe and sterile catheter care and minimizes catheter use to prevent infections.
- The nurse maintains elimination charts and updates them during clinical shift reports.
✅ 9. Education and Health Counseling
- The nurse provides education on preventive health measures, such as vaccination, oral hygiene, and foot care in diabetics.
- She encourages lifestyle modifications including diet, sleep hygiene, and gentle physical activity.
- The nurse offers counseling regarding acceptance of aging, body image changes, and dependency issues.
- She assists in preparing legal documents like advanced directives, DNR orders, and wills when needed.
- The nurse empowers caregivers through training on safe handling, communication, and coping skills.
✅ 10. Collaboration and Rehabilitation Support
- The nurse works as part of a multidisciplinary team to ensure integrated geriatric care.
- She refers to occupational therapy for hand-function, grooming, and bathing adaptations.
- The nurse coordinates with home healthcare services, hospice, or old-age homes based on individual needs.
- She supports adaptive training with aids like grab bars, feeding spoons, dressing devices, and ensures elderly can live with dignity.
- The nurse participates in community geriatric programs and assists with elder welfare schemes and insurance.
Section 2
Q.4
1. Define cataract (2)
- Cataract is a medical condition in which the natural crystalline lens of the eye becomes progressively cloudy or opaque, leading to a decrease in vision clarity.
- It is commonly age-related, but can also be congenital, traumatic, or secondary to diseases like diabetes or long-term corticosteroid use.
- This opacification interferes with the passage of light through the lens, resulting in blurred or dim vision. It is the most common cause of reversible blindness globally, especially in elderly individuals.
2. Explain the diagnostic measure of cataract (3)
Cataract is a progressive clouding of the lens in the eye, leading to gradual visual impairment. The diagnosis of cataract involves both clinical evaluation and specialized eye investigations to assess the type, severity, and impact on vision.
1️⃣ Detailed Patient History Collection
- The ophthalmologist or nurse collects a complete history of visual symptoms, such as blurring of vision, difficulty seeing in bright light, glare at night, fading of colors, or seeing halos around lights.
- Information about risk factors, including age, diabetes, trauma, long-term steroid use, or family history of cataract, is also gathered.
2️⃣ Visual Acuity Testing
- The Snellen chart or near vision chart is used to assess how well the patient can see at a distance or close up.
- A decline in visual acuity (less than 6/9 or 20/40) without other causes often suggests cataract formation.
3️⃣ Slit Lamp Examination
- This is a specialized microscopic examination of the anterior eye structures using a slit lamp biomicroscope.
- It helps to visually inspect the lens for cloudiness, opacification, and to classify the cataract (e.g., nuclear, cortical, posterior subcapsular).
- It is considered the gold standard for diagnosing and grading the severity of cataracts.
4️⃣ Pupil Dilation (Mydriatic Eye Exam)
- Mydriatic drops (such as tropicamide) are instilled to dilate the pupil for better visualization of the entire lens and retina.
- This allows the examiner to detect even posterior cataracts or coexisting retinal conditions, such as diabetic retinopathy or macular degeneration.
5️⃣ Ophthalmoscopy (Fundus Examination)
- After pupil dilation, a direct or indirect ophthalmoscope is used to view the retina and optic nerve.
- If cataract is dense, the red reflex may be reduced or absent, and the posterior segment may not be visible — indicating the need for further tests like B-scan.
6️⃣ Tonometry (Intraocular Pressure Measurement)
- It is performed to rule out co-existing glaucoma, which can affect surgical outcomes.
- This is done using a tonometer (e.g., Goldmann applanation) to measure intraocular pressure (IOP) before planning cataract surgery.
7️⃣ Refraction and Retinoscopy
- A refraction test is done to check if changes in eyeglass prescription can temporarily improve vision.
- Retinoscopy helps determine if vision loss is due to cataract or other refractive errors.
8️⃣ B-Scan Ocular Ultrasonography (If Fundus Is Not Visible)
- When the cataract is mature or hypermature and prevents visualization of the retina, a B-scan ultrasound is done to rule out retinal detachment or tumors.
9️⃣ Biometry (A-Scan) for Intraocular Lens (IOL) Power Calculation
- Axial length and corneal curvature are measured using A-scan biometry or optical biometry.
- These values are used to calculate the power of intraocular lens (IOL) to be implanted during cataract surgery.
1️⃣0️⃣ Contrast Sensitivity and Glare Testing
- These tests assess how well the patient can see in low-light or high-glare conditions, which helps in early detection of posterior subcapsular cataract.
3. Describe the surgical management of cataract (5)
Cataract surgery is the definitive and most effective treatment for cataract, which is the clouding of the lens leading to vision loss. The surgery involves removal of the opaque lens and implantation of an artificial intraocular lens (IOL) to restore clear vision. Cataract surgery is generally performed as a day-care procedure under local or topical anesthesia and is highly successful with modern techniques.
1️⃣ Preoperative Preparation
- It is essential to conduct a complete eye examination including visual acuity test, slit-lamp examination, intraocular pressure measurement, and fundus evaluation.
- The power of the intraocular lens (IOL) to be implanted is calculated using A-scan biometry or optical coherence biometry.
- Patients are advised to stop using anticoagulants (if any) after physician approval and start antibiotic eye drops 1–2 days before surgery.
- The patient must fast for 4–6 hours, and the operative eye is dilated using mydriatic drops before surgery.
- A written informed consent is obtained after explaining the risks and benefits of surgery.
2️⃣ Types of Cataract Surgery
There are several types of surgical techniques depending on equipment availability, lens hardness, and surgeon preference:
A. Phacoemulsification (Modern Method)
- It is the most commonly performed and advanced technique for cataract surgery today.
- A very small incision (2.2 to 2.8 mm) is made at the edge of the cornea.
- A phaco probe is inserted through the incision, which uses ultrasound waves to emulsify (break down) the cloudy lens into small fragments.
- The emulsified lens is suctioned out and a foldable intraocular lens (IOL) is inserted through the same small incision.
- It is a stitch-less, bloodless, and fast-healing surgery with rapid recovery and minimal postoperative discomfort.
B. Manual Small Incision Cataract Surgery (SICS)
- This method involves making a slightly larger self-sealing incision (6–7 mm) on the sclera.
- The entire lens nucleus is removed manually without using phacoemulsification.
- A rigid PMMA intraocular lens is implanted.
- This technique is more affordable and commonly used in rural or low-resource settings with excellent outcomes.
C. Extracapsular Cataract Extraction (ECCE)
- In this older technique, a large incision (10–12 mm) is made, and the entire lens is removed, leaving the posterior capsule intact.
- A posterior chamber IOL is then implanted.
- This method is rarely used today and is reserved for very hard or mature cataracts where phaco is not possible.
D. Intracapsular Cataract Extraction (ICCE)
- It is an obsolete procedure in which the entire lens along with its capsule is removed.
- An anterior chamber IOL is placed in front of the iris.
- This technique has a higher risk of complications and is not commonly performed anymore.
3️⃣ Types of Intraocular Lenses (IOLs) Used
- During surgery, the natural lens is replaced with an IOL to restore vision:
- Monofocal IOL : Provides clear vision at one fixed distance, usually for distance vision.
- Multifocal IOL : Allows both near and distant vision but may cause glare or halos.
- Toric IOL : Corrects astigmatism.
- Aspheric IOL : Reduces optical aberrations and gives clearer vision, especially in younger patients.
4️⃣ Postoperative Management
- After surgery, an eye shield is placed to protect the eye, and the patient is observed for 1–2 hours before discharge.
- The patient is instructed to avoid touching or rubbing the eye, and to wear dark glasses during the day.
- Antibiotic-steroid combination eye drops are prescribed to prevent infection and inflammation.
- The patient is advised to avoid strenuous activities, bending, lifting heavy objects, or exposure to dust and water for a few weeks.
- Follow-up visits are scheduled to monitor visual recovery and detect any complications early.
Q.5
1. Define burns and classification of burns (5)
A burn is a form of traumatic injury that occurs when the body’s tissues are damaged due to thermal, chemical, electrical, or radiation exposure, leading to inflammation, cellular destruction, fluid loss, and increased risk of infection.
Classification of burns
Burns are classified based on the depth of tissue damage and the extent (surface area) affected.
1️⃣ Classification Based on Depth of Burn Injury
A. Superficial Burns (First-Degree Burns)
- It is a type of burn that affects only the epidermis, which is the outermost layer of the skin.
- It is commonly caused by mild sunburn or flash heat exposure.
- The skin appears red, dry, painful, and mildly swollen without any blister formation.
- The healing usually occurs within 3 to 7 days, and there is no scarring left behind.
B. Partial Thickness Burns (Second-Degree Burns)
- This burn involves both the epidermis and part of the dermis (the second layer of skin).
- It is caused by hot liquids, flames, or chemicals.
- The skin shows blisters, redness, swelling, wet or weepy appearance, and is extremely painful.
- Healing takes about 2 to 3 weeks and may result in scarring or changes in skin pigmentation.
C. Full Thickness Burns (Third-Degree Burns)
- It is a severe burn that destroys the entire epidermis and dermis, and may involve subcutaneous tissue, muscle, or even bone.
- It is usually caused by electric shock, fire, chemicals, or prolonged contact with hot objects.
- The burned skin may appear white, leathery, charred, brown or black, and the area is usually painless due to nerve destruction.
- These burns do not heal spontaneously and require surgical intervention such as skin grafting, and result in permanent scarring.
D. Fourth-Degree Burns (Deep Full-Thickness Burns)
- This is the most severe type of burn that extends into muscle, tendons, and even bone.
- It results from high-voltage electric injury or prolonged flame contact.
- The area is completely charred and dry, and there is no pain due to complete nerve damage.
- It has poor prognosis and always requires amputation or extensive surgical reconstruction.
2️⃣ Classification Based on Extent (Surface Area Affected)
Minor burns : In minor burns affected <10% of TBSA (in adults)
Moderate burns : In moderste burns affect 10–20% TBSA
Major burns : In major burns >20% TBSA, burns involving face, hands, feet, genitalia, or inhalation injury
2. Explain the assessment of burns (5)
- Assessment of burns area refers to the calculation of the percentage of Total Body Surface Area (TBSA) affected by burns.
- It helps in determining severity of burns, guiding fluid resuscitation, hospitalization needs, and treatment planning.
1. Rule of Nines (Wallace’s Rule of Nines)
- It is a quick and easy method used in emergency settings to estimate the total body surface area (TBSA) affected by burns in adults.
- The body is divided into regions that are multiples of 9%, which helps in fluid replacement calculation and burn severity assessment.
- Percentages in Adults :
1. Head and neck = 9%
2. Each arm (front and back) = 9%
3. Each leg (front and back) = 18%
4. Anterior trunk (chest + abdomen) = 18%
5. Posterior trunk (back + buttocks) = 18%
6. Perineum and genitalia = 1%
2. Lund and Browder Chart
- It is a more accurate method, especially in children and infants, because it adjusts for age-related body proportion differences.
- It provides detailed segmentation of body parts with percentage surface area based on age group.
- It considers age-specific variation in head and limb proportions.
- The chart is divided into small body segments, and the burned area is mapped for precise calculation.
- It is used in pediatric burn units or for extensive burns in adults.
- It is the gold standard for burn area assessment in clinical practice.
- Example :
- Head : 18% in infants vs 9% in adults
- Lower limb : 14% in infants vs 18% in adults
3. Lund and Browder Chart (Age-Specific Method)
- It is a more precise and accurate method for estimating Total Body Surface Area (TBSA) burned.
- This method modifies body percentage values based on the patient’s age, especially useful in infants and children, whose head and body proportions differ from adults.
- The body is divided into multiple anatomical areas, and each area has a different percentage depending on age (e.g., head accounts for more % in infants).
- A printed chart is used to shade the burned areas, and the TBSA is calculated using the age-specific values.
- Example : In a 5-year-old, the head might be considered 13%, but in an adult, it’s 9%.
- It i used in Pediatric burns, hospital settings, and documentation for surgical planning.
4. Rule of Palms (Palm Method / Hand Method)
- In modern hospitals, digital tools and software are used to calculate TBSA more accurately.
- It is a simple method where the patient’s own palm (with fingers) is estimated to be approximately 1% of TBSA.
- It is mostly used in small, patchy, scattered, or irregular burns, or when other methods are not feasible.
- It is Quick method and useful for minor burns or first aid assessment.
- It helps first responders, community health nurses, or emergency staff estimate burn size in the field or home settings.
- Example : If the burn area is the size of 3 palms, it is about 3% TBSA burned.
- 5. Computerized Methods and Burn Assessment Apps (Modern Method)
- These tools involve drawing burn areas on a digital body diagram, and the system automatically calculates the percentage.
- Some popular tools include BurnCase 3D, Mersey Burns App, and Smart Burn Calculator.
- These are used mainly in burn ICUs or trauma centers for detailed monitoring and surgical planning.
- It is Highly accurate, supports photographic evidence and monitoring.
- It Requires device, training, and software access.
3. Explain the formulas for Fluid calculation (5)
Q.6 Write short notes (any three) (12 marks)
1. Thermal emergencies
Definition of Thermal Emergencies
- Thermal emergencies are acute or life-threatening conditions that occur due to excessive heat exposure (hyperthermia) or excessive cold exposure (hypothermia), which lead to disruption in normal body temperature regulation and can affect multiple organs.
- These emergencies may result from environmental, occupational, or accidental causes and need immediate assessment and intervention.
Classification of Thermal Emergencies
A. Heat-Related Emergencies (Hyperthermia)
1️⃣ Heat Cramps
- It is characterized by painful muscle cramps, usually in the legs or abdomen, due to excessive sweating and sodium loss during strenuous physical activity in hot conditions.
2️⃣ Heat Exhaustion
- It is a moderate heat illness that results from fluid and electrolyte depletion, presenting with profuse sweating, weakness, dizziness, and headache.
3️⃣ Heat Stroke (Sunstroke)
- It is the most severe and life-threatening condition of heat-related illnesses.
- It is characterized by core body temperature >40°C (104°F), with altered mental status, dry hot skin, and possible organ failure.
B. Cold-Related Emergencies (Hypothermia)
1️⃣ Mild Hypothermia
It occurs when the core body temperature falls below 35°C (95°F) and the patient experiences shivering, confusion, and lethargy.
2️⃣ Moderate to Severe Hypothermia
Body temperature drops below 32°C (90°F), leading to slowed pulse, respiration, unconsciousness, and eventually cardiac arrest if untreated.
3️⃣ Frostbite
- It is a localized cold injury where skin and underlying tissues freeze, most commonly affecting fingers, toes, ears, and nose.
- It can lead to tissue necrosis, gangrene, and loss of limb if not treated promptly.
Causes / Risk Factors
- Prolonged exposure to extreme temperatures (hot or cold).
- Working outdoors, especially in construction or agriculture without proper protective clothing.
- Elderly, infants, and chronically ill are more vulnerable due to poor thermoregulation.
- Excessive physical exertion without hydration in hot conditions.
- Alcohol, drug use, or psychiatric illness can impair judgment about temperature exposure.
- Poor housing or homelessness during winter or summer.
Signs and Symptoms
Heat-Related
- Increased body temperature, flushed skin
- Profuse sweating (in exhaustion) or absence of sweating (in heat stroke)
- Nausea, vomiting, fatigue
- Dizziness, fainting, altered mental status
- Tachycardia, hypotension
Cold-Related
- Pale, cold skin; shivering in early stages
- Numbness, tingling in extremities
- Slowed pulse, respiration, and impaired judgment
- Blue or black skin in frostbite
- Unconsciousness or cardiac arrest in severe hypothermia
Nursing Management of Thermal Emergencies
For Heat-Related Emergencies
- It is important to move the patient to a cool, shaded or air-conditioned environment immediately.
- The nurse must remove excessive clothing and apply cool compresses or tepid sponging.
- It is essential to administer oral fluids with electrolytes (if conscious) or IV fluids (for moderate to severe cases).
- For heat stroke, active cooling methods such as ice packs to groin and axillae, cool misting, or cold IV saline are vital.
- Monitor vital signs, urinary output, and watch for signs of shock or seizure.
- Ensure oxygen therapy and prepare for emergency airway management if altered consciousness is present.
For Cold-Related Emergencies
- It is crucial to remove the person from cold exposure and wet clothing.
- The nurse must initiate gradual rewarming using blankets, warm IV fluids, warm humidified oxygen.
- Avoid direct heat (like hot water bottles or heaters) which may damage the skin.
- For frostbite, immerse affected limbs in warm water (37°C–39°C) for 15–30 minutes.
- Do not rub or massage frostbitten areas, as this may worsen tissue damage.
- Monitor for arrhythmias, bradycardia, and mental status changes.
- Administer analgesics and antibiotics if needed.
Prevention Strategies
- It is essential to educate the public on weather-related precautions and hydration.
- Use of appropriate clothing and sun protection during summer is vital.
- Ensure access to shelter and heating during winter.
- Elderly and children should be monitored closely during temperature extremes.
- Workplaces must provide breaks, hydration, and cooling shelters in hot conditions.
2. Occupational hazards
Definition of Occupational Hazard
An occupational hazard refers to any condition, factor, or agent present in a work environment that may cause injury, disease, discomfort, or death to workers as a result of exposure during the course of employment. These hazards vary based on the type of job, industry, and working conditions and may affect physical, mental, or social well-being of the workers.
Classification and Types of Occupational Hazards
A. Physical Hazards
- These hazards are caused by exposure to physical environmental agents in the workplace.
- Workers may be exposed to excessive heat, cold, noise, vibration, ultraviolet radiation, and ionizing radiation.
- Example: Prolonged exposure to high decibel noise in industrial machinery can lead to noise-induced hearing loss.
- Other examples include heatstroke in furnace workers and frostbite in cold storage workers.
- Radiation exposure may lead to cancer or infertility, especially in X-ray departments or nuclear plants.
B. Chemical Hazards
- These hazards arise due to contact with harmful chemicals, gases, vapors, liquids, or solids during occupational work.
- Inhalation, ingestion, or skin contact can cause acute poisoning, respiratory issues, skin diseases, or cancer.
- Example: Benzene exposure in rubber industries may lead to blood disorders or leukemia.
- Agricultural pesticides may cause neurological symptoms or skin rashes in farm workers.
- Proper labeling, ventilation, and PPE use are essential for prevention.
C. Biological Hazards
- These involve exposure to infectious microorganisms such as bacteria, viruses, fungi, and parasites at work.
- Common among healthcare workers, lab technicians, veterinarians, and agriculture workers.
- Example: Needle stick injuries in nurses and doctors can lead to HIV, hepatitis B and C infection.
- Farmers may acquire zoonotic infections such as brucellosis or leptospirosis.
- Immunization, hand hygiene, and infection control protocols help reduce these hazards.
D. Mechanical Hazards
- These hazards result from machinery, moving parts, tools, and mechanical failure in industrial settings.
- They can cause cuts, fractures, amputations, crush injuries, or even death.
- Example: A factory worker’s hand getting trapped in a conveyor belt due to lack of safety guard.
- Improperly maintained machines or lack of emergency shutoff devices are common causes.
- Safety training and maintenance checks are vital to minimize risks.
E. Ergonomic Hazards
- These occur due to poor workstation design, repetitive movement, overexertion, and improper lifting techniques.
- Common in office staff, typists, drivers, dentists, and nurses performing bedside care.
- Can cause musculoskeletal disorders (MSDs), carpal tunnel syndrome, cervical spondylosis, and back pain.
- Example: Prolonged sitting in poor posture can cause chronic back and neck pain.
- Use of adjustable chairs, correct lifting posture, and rest breaks reduces ergonomic hazards.
F. Psychosocial Hazards
- These hazards arise from mental and emotional stress in the work environment.
- Causes include job insecurity, harassment, discrimination, poor work-life balance, overwork, and lack of support.
- Can lead to anxiety, depression, sleep disorders, burnout, and even suicide in extreme cases.
- Example: Nurses in ICU settings under constant stress may develop emotional exhaustion.
- Stress management programs, supportive supervision, and employee counseling are effective solutions.
Prevention and Control of Occupational Hazards
- Conduct regular workplace risk assessments and safety audits.
- Provide appropriate Personal Protective Equipment (PPE) to all workers.
- Ensure machine guards, exhaust fans, and proper ventilation in all work areas.
- Offer occupational health checkups and vaccinations (e.g., hepatitis B).
- Arrange safety training, mock drills, and fire response sessions regularly.
- Display hazard signs and safety instructions at high-risk areas.
- Promote safe lifting techniques and ergonomic furniture.
- Provide stress management and counseling services to reduce burnout.
- Encourage reporting of accidents, near misses, and unsafe practices.
- Maintain good housekeeping and cleanliness in all work zones.
- Enforce legal safety standards like OSHA, Factory Act, and ILO norms.
- Create a safety committee to monitor and implement health policies.
3. Advance cardic life support
Definition of ACLS
Advanced Cardiac Life Support (ACLS) is a set of clinical protocols and interventions used to manage patients with life-threatening cardiovascular emergencies, such as cardiac arrest, arrhythmias, stroke, and acute coronary syndromes, by integrating high-quality CPR, defibrillation, airway management, intravenous medications, and advanced monitoring techniques.
Goals of ACLS
- To preserve brain function and vital organ perfusion during cardiac arrest or life-threatening cardiac events.
- To achieve Return of Spontaneous Circulation (ROSC) and stabilize the patient’s condition until definitive care is provided.
- To identify and treat reversible causes of cardiac arrest (such as 5 H’s and 5 T’s).
- To reduce morbidity and mortality through rapid and standardized treatment protocols.
Key Components of ACLS
✅ A. High-Quality CPR (Cardiopulmonary Resuscitation)
- Begin immediately with chest compressions if the patient is unresponsive and not breathing.
- Deliver compressions at a rate of 100–120 per minute with a depth of 5–6 cm (2 inches) in adults.
- Allow full chest recoil and minimize interruptions.
- Give 2 ventilations for every 30 compressions if an advanced airway is not in place.
✅ B. Airway Management
- Use bag-valve-mask (BVM) or advanced airway (like endotracheal tube or laryngeal mask airway).
- Confirm tube placement using capnography or chest movement.
- Provide 1 breath every 6 seconds (10 breaths per minute) when an advanced airway is placed.
✅ C. Cardiac Monitoring and Rhythm Recognition
- Attach the patient to a cardiac monitor/defibrillator to identify life-threatening rhythms :
1. Ventricular Fibrillation (VF)
2. Pulseless Ventricular Tachycardia (VT)
3. Asystole
4. Pulseless Electrical Activity (PEA) - Based on rhythm, follow appropriate algorithm for shockable vs. non-shockable rhythms.
✅ D. Defibrillation/Cardioversion
- Deliver unsynchronized shock for VF or pulseless VT (biphasic: 120–200 J; monophasic: 360 J).
- For tachycardias with a pulse, use synchronized cardioversion.
- Always announce “CLEAR” before shock and ensure no one is in contact with the patient.
✅ E. Medication Administration (During or after CPR)
- Epinephrine 1 mg IV/IO every 3–5 minutes is given in all cardiac arrests.
- Amiodarone 300 mg IV/IO bolus for refractory VF/pulseless VT (second dose: 150 mg).
- Other drugs include Atropine for bradycardia, Adenosine for SVT, and Lidocaine as alternative to Amiodarone.
- All drugs are followed by 20 ml normal saline flush and elevation of the limb.
ACLS Algorithms
ACLS follows specific treatment flowcharts :
- Cardiac Arrest Algorithm (shockable and non-shockable rhythms)
- Bradycardia Algorithm
- Tachycardia Algorithm
- Post-Cardiac Arrest Care Algorithm
- Acute Coronary Syndrome Algorithm
- Stroke Algorithm
Post-Resuscitation (Post-ROSC) Care
- Maintain adequate oxygenation (SpO₂ >94%) and ventilation.
- Monitor blood pressure and support with IV fluids/vasopressors if hypotensive.
- Obtain 12-lead ECG to identify myocardial infarction.
- Consider targeted temperature management (TTM) to improve neurological outcomes.
- Transfer to ICU or cardiac care unit for further management.
Nursing Role in ACLS
- Ensure early recognition of cardiac arrest and activation of emergency response team.
- Begin high-quality CPR immediately and use automated external defibrillator (AED) if available.
- Assist in airway insertion and ventilation during code blue.
- Prepare and administer IV medications as per doctor’s order.
- Maintain clear documentation of time, rhythm changes, drugs given, and patient response.
- Provide psychological support to patient’s relatives and assist in post-resuscitation care.
4. Palliative care
Definition of Palliative Care
- Palliative care is defined as a specialized form of medical and nursing care that focuses on relieving the suffering and improving the quality of life of patients who are facing serious, chronic, or life-limiting illnesses, such as cancer, end-stage organ failure, or neurological disorders.
- It addresses not only physical symptoms, but also the emotional, social, psychological, and spiritual needs of both the patient and their family.
Principles of Palliative Care
- It is the nurse’s and physician’s responsibility to relieve pain and other distressing symptoms such as breathlessness, nausea, and anxiety.
- Palliative care provides psychological, emotional, and spiritual support to the patient and their loved ones throughout the course of illness.
- It aims to affirm life and regard dying as a normal process, without either hastening or postponing death.
- It includes support systems to help patients live actively until death and support families to cope during illness and bereavement.
- Palliative care is applicable early in the course of illness, in combination with therapies that are intended to prolong life (like chemotherapy or dialysis).
- It emphasizes team-based care, involving doctors, nurses, counselors, social workers, and chaplains.
Goals of Palliative Care
- To improve the quality of life for patients and their families in the face of life-threatening illness.
- To provide symptom control, especially for pain, nausea, dyspnea, and insomnia.
- To provide holistic care by addressing the physical, emotional, spiritual, and social dimensions.
- To support the patient’s autonomy and decision-making regarding treatment choices.
- To assist in advance care planning such as Do Not Resuscitate (DNR) orders, living wills, or hospice referral.
- To provide bereavement support for family members after the death of a patient.
Conditions Where Palliative Care is Indicated
- Terminal cancer patients (most common group receiving palliative care).
- End-stage organ diseases such as congestive heart failure, chronic kidney failure, and liver cirrhosis.
- Progressive neurological diseases such as ALS, Parkinson’s disease, and dementia.
- Severe chronic respiratory illnesses like COPD.
- AIDS and other chronic infectious diseases in advanced stages.
- Geriatric patients with multiple comorbidities and reduced functional ability.
Key Components of Palliative Care
1️⃣ Physical Care
- Management of pain with opioids, NSAIDs, or adjuvant drugs.
- Control of symptoms like vomiting, constipation, breathlessness, or fatigue.
- Nutritional support and skin care to prevent pressure sores.
- End-of-life care including hydration and dignity in dying.
2️⃣ Psychological Support
- Helping the patient cope with fear, anxiety, depression, and grief.
- Providing mental health counseling and emotional reassurance.
- Supporting positive communication and acceptance of illness.
3️⃣ Spiritual and Cultural Care
- Respecting the religious beliefs, values, and spiritual needs of the patient and family.
- Assisting the patient to find peace and meaning during the terminal phase.
- Involving priests, spiritual leaders, or chaplains if desired.
4️⃣ Family and Social Support
- Helping families understand the patient’s condition and prepare for end-of-life issues.
- Educating them about care techniques at home and involving them in care decisions.
- Providing grief support after the patient’s death.
Nursing Role in Palliative Care
- It is the nurse’s responsibility to regularly assess the patient’s pain using standardized pain scales (such as Numeric Rating Scale or Visual Analog Scale) and administer prescribed analgesics, including opioids, promptly to ensure comfort.
- The nurse must provide empathetic listening and emotional reassurance by encouraging the patient to express their fears, concerns, and preferences about dying, without judgment.
- The nurse should ensure the patient’s right to dignity and privacy during personal care, procedures, and discussions, especially in terminal phases, preserving self-respect.
- The nurse actively participates in interdisciplinary team meetings, updating doctors, counselors, and social workers about the patient’s changing condition and preferences.
- It is the nurse’s duty to educate family members about home care techniques, including administering medications, turning the patient, and managing symptoms like breathlessness or delirium.
- The nurse ensures that advance directives, DNR (Do Not Resuscitate) orders, and end-of-life wishes of the patient are clearly understood, documented, and respected.
- The nurse supports spiritual needs by arranging access to spiritual leaders, rituals, or prayer time as requested by the patient or family, respecting cultural and religious beliefs.
- The nurse continuously monitors for signs of dying (such as decreased consciousness, apnea, or mottled skin) and prepares the family for a peaceful and dignified death.
- The nurse provides grief support and counseling during and after death, encouraging healthy coping and helping families understand that their emotional reactions are valid.
- It is also the nurse’s role to maintain accurate, confidential records of medications given, responses observed, patient condition changes, and communications with the family and team.
💥WELCOME TO MY NURSING APP FAMILY💥
KINDLY SEND YOUR UNIVERSITY PAPER FOR SAMPLE SOLUTION OR FOR MORE INFO CONTACT US ON-CALL/WATSAPP – 8485976407
