Second Year Post Basic (Nursing) B.Sc.March-2023-Mental Health Nursing(PAPER NO.7)
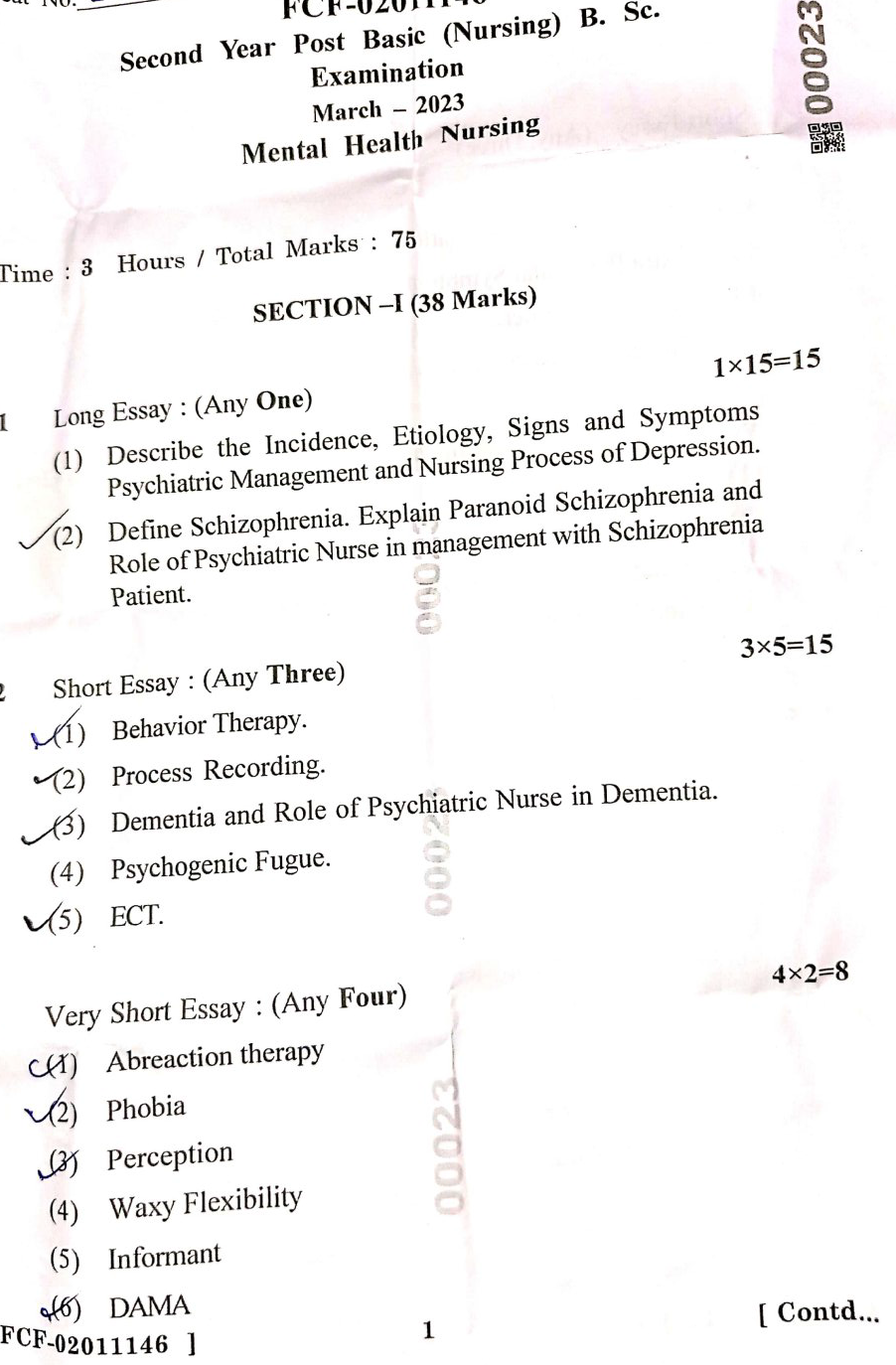
SECTION-I
I. Long Essay: (Any One)1×15-15
(1) Describe the Incidence, Etiology, Signs and Symptoms Psychiatric Management and Nursing Process of Depression.
Depression: Incidence, Etiology, Signs and Symptoms, Psychiatric Management, and Nursing Process
1. Incidence of Depression:
Depression is a widespread mental health disorder affecting individuals across all age groups. According to the World Health Organization (WHO), more than 264 million people globally suffer from depression. In India, the National Mental Health Survey reports a lifetime prevalence of depression of about 5.25% in the general population. The incidence is higher in women compared to men, and depression is a leading cause of disability worldwide.
2. Etiology of Depression:
Depression is a multifactorial disorder, with the following key causes:
- Biological Factors:
- Genetic Predisposition: Family history of depression increases the risk.
- Neurotransmitter Imbalance: Deficiencies or imbalances in neurotransmitters like serotonin, norepinephrine, and dopamine.
- Hormonal Changes: Changes in hormone levels during pregnancy, postpartum, or menopause.
- Chronic Medical Conditions: Conditions like diabetes, heart disease, and chronic pain.
- Psychosocial Factors:
- Stressful Life Events: Loss of a loved one, relationship problems, unemployment.
- Childhood Trauma or Abuse: Early experiences of neglect, abuse, or trauma can predispose individuals to depression.
- Negative Thinking Patterns: Persistent pessimism, low self-esteem, and feelings of worthlessness.
- Environmental Factors:
- Social Isolation: Lack of social support or isolation.
- Economic Hardships: Financial instability or poverty.
- Substance Abuse: Alcohol or drug abuse can contribute to or exacerbate depression.
3. Signs and Symptoms of Depression:
Depression can manifest with a variety of emotional, cognitive, and physical symptoms, including:
- Emotional Symptoms:
- Persistent sadness or low mood.
- Feelings of hopelessness or worthlessness.
- Irritability or frustration, even over minor matters.
- Loss of interest or pleasure in activities once enjoyed (anhedonia).
- Cognitive Symptoms:
- Difficulty concentrating, remembering, or making decisions.
- Negative or distorted thinking patterns (e.g., “I’m a failure”).
- Recurring thoughts of death or suicide.
- Difficulty in performing daily tasks.
- Physical Symptoms:
- Changes in appetite and weight (either increased or decreased).
- Sleep disturbances (insomnia or hypersomnia).
- Fatigue or loss of energy.
- Unexplained physical aches and pains (somatic symptoms).
- Psychomotor retardation (slowed speech or movement).
4. Psychiatric Management of Depression:
Effective management of depression often involves a combination of pharmacological, psychotherapeutic, and lifestyle interventions:
- Pharmacological Management:
- Antidepressants: These include selective serotonin reuptake inhibitors (SSRIs), such as fluoxetine and sertraline, serotonin-norepinephrine reuptake inhibitors (SNRIs), like venlafaxine, and tricyclic antidepressants (TCAs), such as amitriptyline.
- Mood Stabilizers: In cases of depression with mood instability, mood stabilizers like lithium may be used.
- Antipsychotics: In treatment-resistant cases, atypical antipsychotics (e.g., aripiprazole) may be added to antidepressant therapy.
- Electroconvulsive Therapy (ECT): Used for severe or treatment-resistant depression, especially when suicidal ideation is present.
- Psychotherapeutic Management:
- Cognitive Behavioral Therapy (CBT): Helps the patient identify and change negative thought patterns and behaviors that contribute to depression.
- Interpersonal Therapy (IPT): Focuses on improving interpersonal relationships and resolving conflicts that may contribute to depressive symptoms.
- Psychodynamic Therapy: Explores unresolved emotional conflicts and their impact on the individual’s current mental health.
- Mindfulness-Based Cognitive Therapy (MBCT): Combines mindfulness strategies with cognitive therapy to prevent relapse.
- Lifestyle and Support Interventions:
- Regular Physical Activity: Exercise can reduce depressive symptoms by releasing endorphins and improving mood.
- Healthy Diet: Nutritional support with a balanced diet helps maintain physical well-being.
- Social Support: Family therapy or group therapy may be beneficial to provide emotional support and reduce isolation.
5. Nursing Process for Depression:
The nursing process includes assessment, diagnosis, planning, implementation, and evaluation tailored to the care of individuals with depression.
- Assessment:
- Gather a comprehensive history of the patient, including medical, psychiatric, and psychosocial aspects.
- Assess the severity and duration of depressive symptoms using tools like the Hamilton Depression Rating Scale (HAM-D) or Patient Health Questionnaire-9 (PHQ-9).
- Evaluate the risk of self-harm or suicide.
- Monitor physical health parameters, including changes in sleep, appetite, weight, and energy levels.
- Nursing Diagnosis:
- Risk for Suicide related to hopelessness, worthlessness, and depression.
- Ineffective Coping related to stressful life situations and impaired cognitive functioning.
- Imbalanced Nutrition: Less Than Body Requirements related to loss of appetite and weight loss.
- Disturbed Sleep Pattern related to insomnia or hypersomnia.
- Social Isolation related to withdrawal and lack of interest in social activities.
- Planning:
- Collaborate with the patient and their family to create a plan of care focused on improving mood, coping strategies, and daily functioning.
- Develop short-term and long-term goals, such as reducing symptoms of depression, enhancing self-esteem, and preventing relapse.
- Plan for regular follow-ups to assess progress and modify the treatment plan as necessary.
- Implementation:
- Administer prescribed medications and monitor for side effects.
- Provide emotional support and actively listen to the patient’s concerns.
- Encourage participation in structured activities, including physical exercise or therapy sessions.
- Educate the patient about depression, treatment options, and the importance of adherence to therapy.
- Promote healthy lifestyle habits like sleep hygiene and balanced nutrition.
- Facilitate the patient’s engagement in support groups or family therapy.
- Evaluation:
- Regularly evaluate the patient’s progress toward achieving the set goals.
- Assess for improvement in mood, reduction in depressive symptoms, and enhancement in daily functioning.
- Reassess for suicidal ideation or self-harm risk.
- Ensure that the patient adheres to medication and therapy regimens.
- Revise the care plan if there is no improvement or worsening of symptoms.
By using a comprehensive approach involving medical treatment, psychotherapy, and supportive nursing care, the quality of life and prognosis for individuals with depression can improve significantly.
(2) Define Schizophrenia. Explain Paranoid Schizophrenia and Role of Psychiatric Nurse in management with Schizophrenia Patient.
Schizophrenia is a chronic and severe mental disorder that affects how a person thinks, feels, and behaves. Individuals with schizophrenia may seem like they have lost touch with reality, leading to significant distress for themselves and their loved ones. It is characterized by episodes of psychosis, including hallucinations, delusions, disorganized thinking, and impaired daily functioning.
Schizophrenia is typically categorized into different subtypes based on the dominant symptoms, such as paranoid schizophrenia, catatonic schizophrenia, disorganized schizophrenia, etc. It often manifests in late adolescence or early adulthood and requires long-term treatment.
Paranoid Schizophrenia:
Paranoid schizophrenia is one of the most common subtypes of schizophrenia, primarily marked by prominent delusions and auditory hallucinations. Individuals with this type generally have a better cognitive function compared to other subtypes of schizophrenia but struggle with paranoid thoughts and distrust of others.
Key Characteristics of Paranoid Schizophrenia:
- Delusions of Persecution or Grandeur:
- The person may believe that others are out to harm them or that they possess exceptional abilities or importance (e.g., thinking they are a famous person or being persecuted by the government).
- Auditory Hallucinations:
- Hearing voices that are not present is a common symptom. These voices may give commands, criticize the individual, or comment on their actions.
- Anxiety and Fear:
- Patients often experience intense anxiety, fear, or suspicion of people around them due to their delusions.
- Disorganized Thinking:
- Although paranoia dominates, these patients may still have disorganized speech and thoughts.
- Social Withdrawal:
- Due to their delusions, patients tend to withdraw from society and isolate themselves from others, believing that people are plotting against them.
- Hostility or Aggression:
- In some cases, the fear and delusions can lead to defensive or hostile behavior, although most individuals with schizophrenia are not violent.
Course and Prognosis:
- Paranoid schizophrenia tends to have a more stable course, and with proper treatment, individuals can maintain functional lives, but without management, it can lead to severe dysfunction.
Role of the Psychiatric Nurse in Managing Schizophrenia:
The management of a patient with schizophrenia requires a comprehensive and multidisciplinary approach. The psychiatric nurse plays a vital role in providing care, education, and support to both the patient and their family. Below is a detailed explanation of the psychiatric nurse’s role:
1. Assessment:
- Psychiatric and Mental Health Assessment: The nurse must thoroughly assess the patient’s mental health status, including mood, thoughts, behaviors, and perception.
- Suicide and Self-Harm Risk: Assess the patient for potential suicide risk or danger to self or others, especially during active phases of paranoia or psychosis.
- Physical Health Monitoring: Due to the side effects of antipsychotic medications, regular assessment of physical health (e.g., weight, blood sugar, and cholesterol levels) is necessary.
- Substance Use Assessment: Patients with schizophrenia may have co-occurring substance use issues, which the nurse should monitor.
2. Establishing a Therapeutic Relationship:
- Building Trust: Patients with paranoid schizophrenia often exhibit mistrust and suspicion. The nurse needs to build a relationship based on trust, maintaining clear communication, and ensuring that the patient feels safe.
- Non-Confrontational Approach: The nurse should avoid challenging delusions or hallucinations directly as this could escalate the patient’s fear or anxiety. Instead, acknowledging their feelings without agreeing with the delusion is a more effective approach.
- Consistent Interaction: Consistency in care helps build trust and minimize anxiety. Regular check-ins, maintaining routines, and being available for the patient are essential.
3. Medication Administration and Monitoring:
- Administer Antipsychotic Medications: Nurses are responsible for ensuring that patients take their prescribed medications. Antipsychotics like Risperidone, Olanzapine, or Haloperidol are commonly prescribed.
- Monitor Side Effects: Side effects of antipsychotics can include weight gain, sedation, tardive dyskinesia (involuntary movements), and metabolic changes. Regular monitoring and reporting any side effects to the doctor are essential.
- Medication Adherence: Many patients with schizophrenia may stop taking medications due to side effects or because they do not believe they are ill. The nurse’s role includes educating patients and families about the importance of medication adherence.
4. Psychoeducation:
- For the Patient: Educate the patient about schizophrenia, its symptoms, the role of medication, and coping strategies. Patients need to understand their condition and how to manage it.
- For Family Members: Involving the family in the treatment process is crucial. The nurse can educate them about the illness, how to provide support, and what to do in case of an emergency (e.g., recognizing early signs of relapse).
- Symptom Management: Teach the patient and their family how to identify early warning signs of relapse (e.g., increased paranoia, hearing voices) and strategies for seeking help.
5. Managing Hallucinations and Delusions:
- Distraction Techniques: Encourage patients to engage in activities that can divert their attention from hallucinations or delusions, such as listening to music, reading, or exercising.
- Reality Orientation: Gently reorient the patient to reality when they express delusional thoughts, without confronting the delusion directly (e.g., “I know you feel scared, but I don’t see anyone trying to harm you”).
- Calming Techniques: Teach patients relaxation techniques, like deep breathing or progressive muscle relaxation, to reduce anxiety caused by delusions or hallucinations.
6. Communication Skills Training:
- Social Skills Training: Individuals with schizophrenia often struggle with social interactions. The nurse can help teach them communication techniques to improve their relationships and interactions with others.
- Role-Playing: Role-playing scenarios can help patients learn how to communicate effectively and respond to social situations, which can help reduce their social isolation.
7. Providing a Safe and Structured Environment:
- Structured Routine: Establishing a daily routine helps reduce anxiety and keeps patients grounded. The nurse can help organize the patient’s day with activities that are meaningful and engaging.
- Safe Environment: Ensure that the patient is in a safe environment free of triggers that could exacerbate their paranoia or hallucinations.
- Crisis Intervention: If a patient is at risk of harming themselves or others, the nurse must take immediate action by using de-escalation techniques and possibly arranging hospitalization if necessary.
8. Encouraging Social Interaction:
- Group Therapy: The nurse can encourage patients to participate in group therapy sessions, which provide an opportunity to interact with others and develop social skills in a supportive environment.
- Community Integration: Helping patients reintegrate into their community by involving them in vocational training, job placements, or social groups.
9. Relapse Prevention:
- Long-Term Care Planning: Schizophrenia is a lifelong condition, and relapse is common. Nurses play a crucial role in developing a relapse prevention plan, which includes regular follow-up appointments, medication management, and support systems.
- Crisis Planning: Establish a crisis plan that includes emergency contact numbers, early warning signs, and steps to take in case of a psychiatric emergency.
10. Evaluation:
- Evaluate Progress: Regularly assess the patient’s progress in terms of symptom reduction, social integration, medication adherence, and coping skills.
- Monitor for Relapse: Nurses should continue to monitor for any signs of relapse and adjust the care plan accordingly.
- Family Feedback: Regular feedback from the patient’s family can help in making necessary adjustments to the treatment plan.
2 Short Essay: (Any Three)3×5-15
(1) Behavior Therapy.
Definition:
Behavior therapy is a type of psychotherapy that focuses on changing maladaptive behaviors. It is based on the principles of learning, specifically classical and operant conditioning, as well as social learning theory. Behavior therapy assumes that all behaviors, including abnormal ones, are learned and can therefore be unlearned or modified through therapeutic interventions.
Principles of Behavior Therapy
The main goal of behavior therapy is to replace undesirable behaviors with more adaptive ones. The key principles include:
- Classical Conditioning: This involves learning through association. Techniques like exposure therapy and systematic desensitization are based on classical conditioning. For example, in treating phobias, patients are gradually exposed to the feared object while being taught relaxation techniques.
- Operant Conditioning: This refers to learning through reinforcement and punishment. Desired behaviors are reinforced (e.g., through praise or rewards), while undesirable behaviors are either ignored or punished. Token economies are often used in clinical settings, where patients earn tokens for positive behavior.
- Modeling: In social learning theory, behaviors can be learned by observing others. In therapy, the therapist may model healthy behaviors for the patient to imitate.
Applications of Behavior Therapy
Behavior therapy is effective for a wide range of conditions, including:
- Anxiety Disorders: Systematic desensitization and exposure therapy help reduce anxiety by confronting the source of fear in a controlled manner.
- Depression: Behavioral activation encourages patients to engage in positive activities to combat the inactivity associated with depression.
- Addictions: Contingency management uses rewards to reinforce abstinence or sobriety.
- Obsessive-Compulsive Disorder (OCD): Exposure and response prevention (ERP) involves exposing patients to anxiety-provoking situations while preventing their usual compulsive behaviors.
(2) Process Recording.
Process recording is a tool used in psychiatric nursing to document the nurse-patient interaction, focusing on the communication process. It is an educational and evaluative tool that allows nurses to reflect on their communication skills and the effectiveness of their therapeutic interactions with patients.
Purpose of Process Recording
- Self-Reflection: Nurses use process recording to analyze their own communication techniques and improve future interactions with patients.
- Patient Understanding: The recording helps in understanding the patient’s thoughts, feelings, and behaviors during the interaction.
- Learning Tool: It serves as a learning tool for nursing students and professionals to enhance their therapeutic communication skills.
Components of Process Recording
- Verbatim Dialogue: The actual conversation between the nurse and the patient is recorded word for word.
- Nonverbal Behavior: Observations of nonverbal cues such as body language, facial expressions, and gestures.
- Nurse’s Feelings and Reactions: The nurse reflects on their own emotions and reactions during the interaction.
- Analysis of Interaction: This involves interpreting the patient’s responses and the effectiveness of the nurse’s communication strategies.
- Evaluation: The nurse evaluates whether therapeutic goals were met during the session.
(3) Dementia and Role of Psychiatric Nurse in Dementia.
Dementia is a progressive neurodegenerative disorder characterized by cognitive decline, memory impairment, and behavioral changes. Alzheimer’s disease is the most common form of dementia, followed by vascular dementia. Patients with dementia experience a decline in their ability to perform daily activities, requiring increasing levels of care over time.
Symptoms of Dementia
- Memory Loss: Especially for recent events or information.
- Language Problems: Difficulty finding words, forming coherent sentences, or understanding language.
- Disorientation: Confusion about time, place, and even familiar faces.
- Mood and Behavior Changes: Increased irritability, depression, or aggression.
- Poor Judgment: Difficulty making decisions or understanding consequences.
Role of Psychiatric Nurse in Managing Dementia
Psychiatric nurses play a key role in managing patients with dementia. Their responsibilities include:
- Assessment and Diagnosis:
- Psychiatric nurses assess cognitive functioning, monitor disease progression, and collaborate with the healthcare team to diagnose and create treatment plans for dementia patients.
- Behavioral Management:
- Nurses implement strategies to manage common behavioral symptoms like agitation, aggression, wandering, or sleep disturbances. They use non-pharmacological interventions such as redirecting the patient, offering calming environments, and using therapeutic touch.
- Medication Management:
- Psychiatric nurses monitor the administration of medications, including cholinesterase inhibitors (e.g., donepezil) and antipsychotics, ensuring that side effects are managed, and dosages are adjusted according to the patient’s condition.
- Patient and Family Education:
- Nurses educate patients and families about the disease, stages of progression, and caregiving strategies. They help families understand how to care for a loved one with dementia and manage their own stress and emotional burden.
- Creating a Safe Environment:
- Ensuring the patient’s environment is safe is crucial. Nurses may remove hazards, provide supervision, and ensure that the patient is in a familiar and structured environment to reduce confusion.
- Emotional Support:
- Psychiatric nurses offer emotional support to both patients and caregivers, addressing feelings of frustration, grief, and exhaustion associated with dementia.
(4) Psychogenic Fugue.
Psychogenic fugue, also known as dissociative fugue, is a rare dissociative disorder characterized by sudden, unexpected travel away from one’s usual surroundings, accompanied by an inability to recall past events and personal identity. It is triggered by psychological stress rather than medical conditions and often results in temporary amnesia.
Symptoms and Characteristics
- Sudden Travel: The individual may unexpectedly leave home or work and travel to a new location, often without any apparent reason or planning.
- Amnesia: The person experiences memory loss, specifically about their past life, personal identity, or important life events.
- Adoption of a New Identity: In some cases, the person may assume a new identity or engage in unfamiliar activities during the fugue state.
- Confusion and Disorientation: Once the fugue state ends, the individual may be confused about how they arrived at their new location and may have no memory of the fugue episode.
Causes
Psychogenic fugue is usually triggered by severe emotional or psychological trauma, such as the death of a loved one, abuse, or overwhelming stress. It is often seen as a defense mechanism to escape from painful memories or emotional distress.
Treatment and Management
- Psychotherapy: Cognitive-behavioral therapy (CBT) and other forms of psychotherapy help patients address the underlying psychological trauma.
- Medication: Antidepressants or anxiolytics may be prescribed to alleviate symptoms of anxiety or depression associated with the fugue state.
- Supportive Therapy: Involves family counseling, support groups, and long-term psychological care to help the individual recover and prevent recurrence.
(5) ECT.
Electroconvulsive therapy (ECT) is a medical treatment that involves inducing brief seizures in the brain through electrical stimulation. It is primarily used to treat severe mental health conditions like major depression, bipolar disorder, and schizophrenia, especially when other treatments such as medications or psychotherapy have failed.
Indications for ECT
- Severe Depression: ECT is highly effective in treating severe, treatment-resistant depression, particularly when there are symptoms like suicidal thoughts or refusal to eat or drink.
- Bipolar Disorder: ECT is used in cases of extreme mania or severe depressive episodes associated with bipolar disorder.
- Schizophrenia: Patients with treatment-resistant schizophrenia, particularly those with catatonic symptoms or severe psychosis, may benefit from ECT.
- Other Indications: ECT may also be used in cases of acute agitation, aggression, or in patients who cannot take medications due to side effects or pregnancy.
Procedure
ECT is performed under general anesthesia. The patient’s vital signs are monitored, and a muscle relaxant is administered to prevent physical movements during the procedure. Electrodes are placed on the patient’s scalp, and a controlled electrical current is passed through the brain, inducing a brief seizure. The entire procedure takes about 5 to 10 minutes, though the seizure itself lasts only 30 to 60 seconds.
Mechanism of Action
While the exact mechanism of action is not fully understood, ECT is believed to work by altering brain chemistry. It is thought to affect neurotransmitter systems, including serotonin and dopamine, and enhance neuroplasticity, thereby improving mood and reducing psychotic symptoms.
Side Effects
- Short-term Memory Loss: Some patients experience temporary memory loss or confusion after ECT sessions.
- Headache or Muscle Aches: Mild physical discomfort is common after the procedure.
- Cognitive Effects: Although rare, some patients may experience longer-term cognitive side effects.
3 Very Short Essay: (Any Four)4×2=8
(1) Abreaction therapy
Abreaction therapy is a psychotherapeutic technique that involves the release of repressed emotions or memories by having the patient relive past traumatic experiences. This is typically achieved through the process of catharsis, where the individual is encouraged to express previously suppressed feelings, often accompanied by emotional discharge like crying or anger. The goal is to bring unconscious conflicts or trauma into the conscious mind, allowing for emotional healing and resolution. Abreaction is sometimes used in psychoanalysis or hypnotherapy, and it requires careful handling to avoid re-traumatizing the patient. While it can be effective for certain psychological issues like post-traumatic stress disorder (PTSD), its use has declined in favor of more structured therapies like Cognitive Behavioral Therapy (CBT).
(2) Phobia
A phobia is an intense, irrational fear of a specific object, situation, or activity that leads to avoidance behavior and significant distress. Unlike general fears, phobias are persistent and can disrupt daily life and functioning. Phobias are classified into three main types: specific phobias (e.g., fear of spiders, heights), social phobia (fear of social situations), and agoraphobia (fear of places where escape might be difficult). Phobias often arise from a combination of genetic, environmental, and psychological factors. Treatment typically involves Cognitive Behavioral Therapy (CBT), particularly exposure therapy, where the person is gradually exposed to the source of their fear in a controlled manner. In some cases, medications like anti-anxiety drugs or antidepressants may also be prescribed.
(3) Perception
Perception is the process through which sensory information from the environment is interpreted and organized by the brain to create a meaningful understanding of the world. It involves the integration of stimuli received through the five senses—sight, sound, taste, touch, and smell—into a coherent experience. Perception is subjective and can be influenced by past experiences, expectations, and emotional states. For example, two individuals may perceive the same event differently based on their prior knowledge or mood. Theories of perception include bottom-up processing (starting with raw sensory input) and top-down processing (where prior knowledge influences perception). Perception plays a crucial role in how we navigate and respond to our environment.
(4) Waxy Flexibility
Waxy flexibility is a symptom often associated with catatonia, a condition seen in psychiatric disorders like schizophrenia. In this state, the person’s body remains in a fixed position, and their limbs can be moved by someone else into awkward or rigid postures, which they will maintain for an extended period. The term “waxy” reflects the pliability of the individual’s muscles, resembling wax in how easily they can be manipulated. Despite being in uncomfortable positions, the person shows little to no resistance or discomfort. Waxy flexibility indicates severe impairment in motor function and often requires immediate medical and psychiatric intervention, typically through medications like antipsychotics or benzodiazepines.
(5) Informant
In a healthcare or psychological context, an informant is an individual, usually a family member, friend, or caregiver, who provides relevant information about the patient’s history, behavior, symptoms, or functioning. This is especially useful when the patient is unable or unwilling to provide accurate details due to factors such as cognitive impairment, altered mental status, or severe psychological conditions. The informant’s input can help clinicians make more accurate diagnoses and create appropriate treatment plans. In research settings, informants may also provide data for studies, contributing to the understanding of a particular condition or population.
(6)DAMA
Discharge Against Medical Advice (DAMA) refers to a situation where a patient chooses to leave a healthcare facility before the medical staff recommends discharge. This can occur for various reasons, including personal, financial, or emotional factors. When a patient opts for DAMA, they are typically required to sign a form acknowledging that they are leaving against professional advice and accepting the risks associated with early discharge, including potential complications or worsening of their condition. DAMA poses ethical and legal challenges for healthcare providers, who must balance respecting the patient’s autonomy with ensuring the patient understands the possible consequences of their decision.
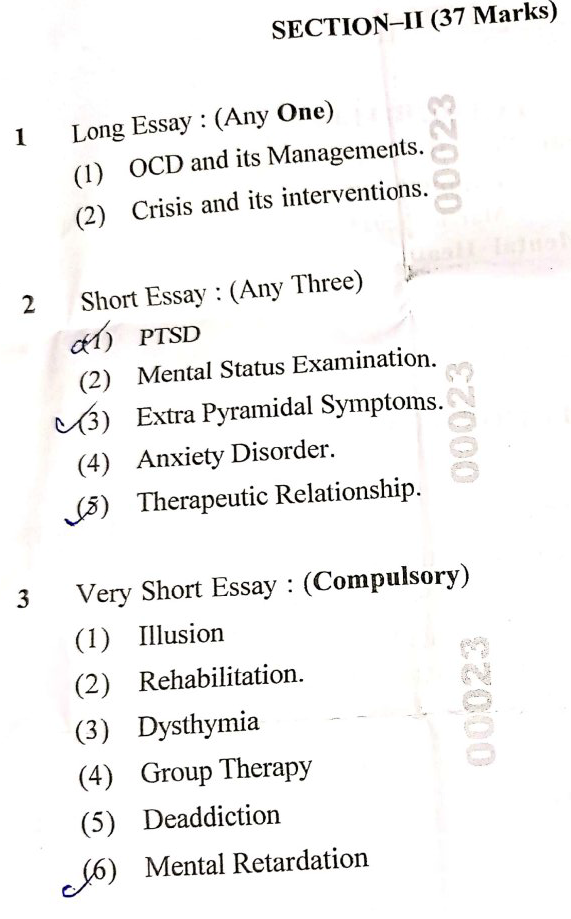
SECTION-II
1 Long Essay: (Any One)1×10=10
(1) OCD and its Managements.
Obsessive-Compulsive Disorder (OCD) is a chronic and often debilitating mental health condition characterized by persistent, unwanted thoughts (obsessions) and repetitive behaviors or mental acts (compulsions) performed to reduce distress or prevent a feared outcome. It affects individuals across all age groups, impacting daily functioning, relationships, and quality of life.
Symptoms of OCD:
- Obsessions: Recurrent, intrusive thoughts, images, or urges that cause significant anxiety. Common obsessions include fear of contamination, harm, or a need for symmetry.
- Compulsions: Repetitive behaviors (e.g., handwashing, checking) or mental acts (e.g., counting, praying) performed to neutralize the anxiety triggered by obsessions. The individual often feels compelled to perform these actions even though they know it is excessive or irrational.
Etiology of OCD:
- Biological Factors: Imbalance of neurotransmitters like serotonin, dysfunction in certain brain regions (e.g., orbitofrontal cortex, basal ganglia), and genetic predisposition.
- Psychological Factors: Cognitive distortions, maladaptive thought patterns, and learned behaviors may play a role.
- Environmental Factors: Stressful or traumatic life events can trigger or exacerbate OCD symptoms.
Diagnosis:
Diagnosis is typically based on clinical interviews and assessments using diagnostic criteria from the DSM-5. OCD must be differentiated from other anxiety disorders and conditions with similar features.
Management of OCD:
- Psychotherapy:
- Cognitive-Behavioral Therapy (CBT): CBT, specifically Exposure and Response Prevention (ERP), is the gold standard for OCD treatment. ERP involves gradually exposing individuals to anxiety-provoking stimuli (obsessions) without allowing them to perform compulsions, helping them to tolerate distress and reduce compulsive behaviors over time.
- Cognitive Restructuring: Aims to help patients recognize and modify distorted thinking patterns that contribute to their OCD symptoms.
- Pharmacotherapy:
- Selective Serotonin Reuptake Inhibitors (SSRIs): Medications such as fluoxetine, sertraline, and fluvoxamine are commonly used to reduce OCD symptoms by increasing serotonin levels in the brain. Higher doses are often required than those used for treating depression.
- Tricyclic Antidepressants (TCAs): Clomipramine, a TCA, is another option for patients who do not respond to SSRIs.
- Antipsychotic Medications: In treatment-resistant cases, adding low-dose antipsychotic medications (e.g., risperidone, aripiprazole) may help.
- Psychoeducation and Family Therapy:
- Education about OCD helps patients and families understand the nature of the disorder, reducing stigma and promoting a supportive environment.
- Family therapy can be helpful in addressing family dynamics and reducing accommodation of OCD behaviors, which often reinforce symptoms.
- Lifestyle Modifications:
- Regular exercise, mindfulness, and stress management techniques can help reduce anxiety and improve overall mental health.
- Proper sleep hygiene is essential as poor sleep can exacerbate OCD symptoms.
- Other Interventions:
- Deep Brain Stimulation (DBS) and Transcranial Magnetic Stimulation (TMS): These are reserved for severe, treatment-resistant cases.
- Hospitalization: For acute exacerbations, especially when OCD severely impairs functioning or leads to self-harm or suicidal thoughts.
OCD is a complex disorder that requires a multifaceted approach to management, including psychotherapy, medication, and lifestyle changes. With early diagnosis and appropriate treatment, many individuals can achieve significant relief from symptoms and lead fulfilling lives.
(2) Crisis and its interventions.
A crisis is a significant emotional event or situation that disrupts an individual’s or a community’s normal functioning, often leading to an overwhelming sense of distress, helplessness, and confusion. Crises can arise from various sources such as natural disasters, accidents, personal loss, mental health issues, or sudden life changes. They require timely and effective intervention to prevent further psychological harm and help individuals regain a sense of control.
Types of Crises:
- Developmental Crisis: Occurs during normal life transitions or changes (e.g., adolescence, retirement, becoming a parent).
- Situational Crisis: Triggered by unexpected traumatic events such as accidents, death, or divorce.
- Existential Crisis: Involves deep personal questioning about life’s meaning or purpose, often occurring during major life changes.
- Community or Collective Crisis: Affects large groups or communities, such as natural disasters, terrorism, or economic crises.
Phases of Crisis:
- Pre-crisis: The individual may experience initial stress but is still functioning normally.
- Impact: The event occurs, causing shock, confusion, and overwhelming emotional responses.
- Crisis: The individual is unable to cope using usual methods, leading to disorganized behavior and emotional turmoil.
- Resolution: The individual begins to adapt, either positively by seeking help or negatively by avoiding the issue.
- Post-crisis: With or without intervention, the individual returns to a baseline or improved state, or remains impaired.
Symptoms of a Crisis:
- Emotional symptoms include anxiety, fear, confusion, anger, depression, or despair.
- Physical symptoms may manifest as headaches, fatigue, changes in sleep or appetite.
- Behavioral symptoms can include isolation, aggression, substance use, or suicidal thoughts.
Crisis Intervention:
Crisis intervention is a short-term therapeutic approach designed to provide immediate support and stabilization. The goal is to help the individual regain equilibrium, improve coping skills, and reduce the impact of the crisis.
Steps in Crisis Intervention:
- Assessment:
- The first step is to assess the severity of the crisis, the individual’s safety (risk of harm to self or others), and the available support systems.
- Understanding the nature of the crisis, the person’s coping mechanisms, and any prior history of mental health issues is critical.
- Establishing Rapport:
- Building trust and rapport with the individual is essential. Empathy, active listening, and non-judgmental support are key components.
- Encouraging open communication helps the individual feel understood and supported.
- Identifying Major Problems:
- Clarify the specific problems or stressors that triggered the crisis.
- Focus on the immediate issues rather than delving into long-standing problems, which can be addressed later.
- Exploring Feelings and Emotions:
- Provide a safe space for the individual to express their emotions. This validation of their feelings can help reduce emotional intensity.
- Techniques such as reflective listening and summarization are useful to ensure the person feels heard.
- Generating and Exploring Alternatives:
- Encourage brainstorming of possible solutions and coping strategies.
- Help the individual evaluate the pros and cons of each option and select a plan of action that feels manageable.
- Developing an Action Plan:
- Create a clear, step-by-step plan for addressing the crisis.
- The action plan should include concrete goals, such as seeking medical or psychological help, contacting support systems, or removing oneself from a dangerous situation.
- Follow-up:
- Crisis intervention should include follow-up sessions to ensure the individual is recovering and not experiencing ongoing distress.
- Follow-up can help identify any unresolved issues and prevent future crises.
Techniques in Crisis Intervention:
- Cognitive Behavioral Techniques: Helping the individual identify and challenge negative thought patterns that contribute to their distress.
- Problem-Solving: Teaching the individual to break down overwhelming problems into smaller, manageable steps.
- Relaxation Techniques: Guided breathing, meditation, or mindfulness to reduce anxiety and restore emotional balance.
- Empowerment: Encouraging self-efficacy and promoting the individual’s ability to take control of their situation.
Special Considerations:
- Cultural Sensitivity: Interventions should be tailored to the individual’s cultural background, values, and beliefs.
- Ethical Considerations: Confidentiality, informed consent, and respecting the autonomy of the individual are important ethical principles.
- Multidisciplinary Approach: In some cases, collaboration with other professionals such as social workers, counselors, or legal experts may be necessary to address complex crises.
Crisis intervention plays a crucial role in helping individuals navigate through life-altering situations. By providing immediate support, stabilization, and practical solutions, crisis intervention can prevent long-term psychological harm and promote resilience and recovery.
2 Short Essay: (Any Three) 3×5=15
(1) PTSD
Post-Traumatic Stress Disorder (PTSD) is a mental health condition triggered by witnessing or experiencing a traumatic event, such as war, natural disasters, accidents, or violence. Individuals with PTSD often struggle with intense fear, helplessness, and anxiety, long after the trauma has passed.
Symptoms
PTSD symptoms are categorized into four groups:
- Re-experiencing: Flashbacks, nightmares, or intrusive thoughts related to the trauma.
- Avoidance: Avoiding places, people, or thoughts that remind the person of the trauma.
- Negative Changes in Thinking and Mood: Feelings of guilt, shame, or detachment from others.
- Hyperarousal: Increased irritability, difficulty sleeping, and being easily startled.
Treatment
Treatment for PTSD typically includes:
- Cognitive Behavioral Therapy (CBT): Focuses on changing negative thought patterns.
- Exposure Therapy: Helps individuals face and reduce fear associated with their trauma.
- Medications: Antidepressants and anti-anxiety medications help manage symptoms.
- PTSD is a serious mental health condition that can profoundly affect one’s quality of life. Early intervention with therapy and medications can help individuals regain control of their lives and manage symptoms more effectively.
(2) Mental Status Examination.
A Mental Status Examination (MSE) is a comprehensive assessment of a patient’s psychological functioning. It is used to evaluate various aspects of the patient’s mental health, including appearance, behavior, thought processes, and cognitive function.
Components of MSE
- Appearance: The patient’s physical appearance, grooming, and clothing.
- Behavior: Observations of motor activity, eye contact, and cooperation.
- Speech: Rate, volume, and tone of speech.
- Mood and Affect: The patient’s emotional state (mood) and how emotions are expressed (affect).
- Thought Process: The organization and flow of thoughts.
- Thought Content: Presence of delusions, obsessions, or suicidal thoughts.
- Perception: Hallucinations or illusions.
- Cognition: Orientation, attention, memory, and abstract thinking.
- Insight and Judgment: The patient’s awareness of their condition and decision-making abilities.
The MSE is a crucial tool for diagnosing psychiatric conditions and planning treatment. It provides a structured way for healthcare professionals to assess the mental functioning of a patient and guide the course of therapy.
(3) Extra Pyramidal Symptoms.
Extra Pyramidal Symptoms (EPS) are drug-induced movement disorders, often caused by the use of antipsychotic medications. These symptoms arise due to dopamine receptor blockade in the brain, particularly in the extrapyramidal system, which controls motor movements.
Types of EPS
- Dystonia: Involuntary muscle contractions that cause abnormal postures or twisting movements, often affecting the neck, face, and limbs.
- Parkinsonism: Symptoms resembling Parkinson’s disease, such as tremors, bradykinesia (slowness of movement), and muscle stiffness.
- Akathisia: A feeling of restlessness and an urgent need to move.
- Tardive Dyskinesia: Involuntary, repetitive movements, often affecting the face and mouth (e.g., lip smacking, grimacing).
Management of EPS
- Dose Adjustment: Reducing the dose of the antipsychotic medication.
- Medications: Anticholinergic drugs (e.g., benztropine) and beta-blockers are commonly used to manage EPS.
- Switching Medications: Moving to atypical antipsychotics, which have a lower risk of EPS, may be necessary.
EPS are significant side effects associated with antipsychotic medications and can severely affect a patient’s quality of life. Early recognition and management of EPS are essential in improving treatment outcomes for individuals on antipsychotics.
(4) Anxiety Disorder.
Anxiety disorders are a group of mental health conditions characterized by excessive, uncontrollable worry, fear, or nervousness. These disorders can significantly impact daily life, leading to avoidance behaviors and social isolation.
Types of Anxiety Disorders
- Generalized Anxiety Disorder (GAD): Persistent, excessive worry about various life aspects.
- Panic Disorder: Recurrent, unexpected panic attacks, with intense fear or discomfort.
- Social Anxiety Disorder: Extreme fear of being judged or embarrassed in social situations.
- Specific Phobias: Intense, irrational fear of specific objects or situations (e.g., heights, spiders).
- Obsessive-Compulsive Disorder (OCD): Recurrent intrusive thoughts (obsessions) and repetitive behaviors (compulsions).
- Post-Traumatic Stress Disorder (PTSD): Anxiety following a traumatic event (covered earlier).
Symptoms
- Physical: Rapid heartbeat, sweating, trembling, dizziness, shortness of breath.
- Psychological: Irrational fears, restlessness, difficulty concentrating, feelings of impending doom.
Treatment
- Cognitive Behavioral Therapy (CBT): Helps patients identify and change negative thought patterns.
- Medications: Antidepressants (SSRIs, SNRIs), benzodiazepines for short-term relief.
- Relaxation Techniques: Mindfulness, deep breathing, and yoga.
Anxiety disorders are highly treatable conditions. With proper therapy and medications, individuals can learn to manage their symptoms and lead fulfilling lives.
(5) Therapeutic Relationship.
A therapeutic relationship is the professional relationship between a healthcare provider, usually a nurse or therapist, and a patient. It is central to effective patient care, particularly in mental health settings. The relationship is built on trust, empathy, and mutual respect.
Key Components of a Therapeutic Relationship
- Trust: The patient must feel that they can confide in the healthcare professional without judgment.
- Empathy: Understanding and sharing the feelings of the patient help to create a supportive environment.
- Confidentiality: Maintaining the patient’s privacy is essential for building trust.
- Boundaries: Professional boundaries ensure that the relationship remains focused on the patient’s therapeutic needs.
- Active Listening: The nurse or therapist must actively listen to the patient’s concerns and validate their emotions.
Phases of Therapeutic Relationship
- Orientation Phase: The initial meeting where trust is established, and the patient’s needs are assessed.
- Working Phase: The nurse or therapist works with the patient to address issues, facilitate change, and provide support.
- Termination Phase: The relationship ends once the therapeutic goals have been met or the treatment plan is completed.
The therapeutic relationship is the cornerstone of effective patient care, particularly in mental health. By fostering trust, empathy, and respect, healthcare professionals can facilitate healing and help patients achieve their treatment goals.
3 Very Short Essay: (Compulsory) 6×2=12
(1) Illusion
An illusion is a misperception or misinterpretation of a real external stimulus. It differs from a hallucination, which is a perception in the absence of any external stimulus. Illusions occur when the brain misinterprets sensory information, leading to incorrect perceptions of reality.
Types of Illusions
- Optical Illusions: These involve the visual system, where objects may appear distorted in size, shape, or motion.
- Auditory Illusions: Misperception of sounds, such as hearing a voice or a sound that is not present.
- Tactile Illusions: A person may feel something on their skin that isn’t actually there.
Causes
Illusions can be caused by environmental factors, tiredness, stress, or psychiatric conditions like schizophrenia. They can also occur in normal individuals under certain circumstances, such as poor lighting or misleading stimuli.
( 3) Dysthymia
Dysthymia, also known as persistent depressive disorder, is a chronic form of depression that lasts for at least two years. The symptoms are less severe than major depression but are more enduring, often affecting a person’s daily functioning and quality of life.
Symptoms
- Chronic Low Mood: Feeling depressed most of the time, almost every day.
- Fatigue and Low Energy: Persistent tiredness that makes routine tasks difficult.
- Low Self-Esteem: A constant feeling of inadequacy or inferiority.
- Sleep and Appetite Changes: Disrupted sleep patterns and appetite changes, either increased or decreased.
Treatment
Treatment usually involves a combination of psychotherapy (e.g., cognitive behavioral therapy) and antidepressant medications. Patients are also encouraged to engage in regular physical activities and adopt a healthy lifestyle.
(2) Rehabilitation.
Rehabilitation refers to the process of helping individuals restore their abilities, function, or quality of life after an illness, injury, or addiction. It can be physical, psychological, or social, depending on the patient’s needs.
Types of Rehabilitation
- Physical Rehabilitation: Focuses on restoring physical function, often after surgery, stroke, or injury.
- Psychiatric Rehabilitation: Helps individuals with mental health issues regain their emotional balance and reintegrate into society.
- Substance Abuse Rehabilitation: Involves helping individuals recover from addiction and lead a substance-free life.
Importance
Rehabilitation is essential in enhancing a person’s independence, improving quality of life, and helping individuals regain their self-esteem. It also reduces the burden on caregivers and promotes long-term recovery.
(4) Group Therapy
Group therapy is a form of psychotherapy where multiple individuals with similar issues meet to discuss their concerns and experiences under the guidance of a therapist. It helps patients develop communication skills, gain support, and realize they are not alone in their struggles.
Benefits of Group Therapy
- Peer Support: Individuals gain support from others facing similar challenges, reducing feelings of isolation.
- Shared Experiences: Group members learn from each other’s experiences, gaining new perspectives on their own issues.
- Social Skills Development: Interacting in a group setting improves social and communication skills, especially for people with social anxiety.
Types of Group Therapy
- Cognitive Behavioral Group Therapy: Focuses on changing negative thinking patterns.
- Support Groups: These provide emotional support for conditions like addiction or chronic illness.
- Psychoeducational Groups: These teach participants about their condition and how to manage it.
(5) Deaddiction
Deaddiction refers to the process of overcoming addiction to substances like alcohol, drugs, or nicotine. Addiction is a chronic disease characterized by compulsive use of substances despite harmful consequences. Deaddiction programs aim to break this cycle through a combination of medical and psychological interventions.
Steps in Deaddiction
- Detoxification: The process of safely removing the addictive substance from the body.
- Counseling and Therapy: Cognitive Behavioral Therapy (CBT) and Motivational Interviewing are commonly used to address the psychological aspects of addiction.
- Support Groups: Groups like Alcoholics Anonymous (AA) or Narcotics Anonymous (NA) offer ongoing support for recovering addicts.
- Relapse Prevention: Focuses on teaching individuals how to avoid triggers and maintain long-term sobriety.
(6) Mental Retardation
💥☺☺☺ALL THE BEST ☺☺☺💥💪
નોંધ :-MCQ ANSWER APP ની યુનિક પેટર્ન માં બંને ભાષા માં આગળ paper solution /click here ની નીચે આપેલા છે. ” અ ” પર ક્લિક કરવાથી ભાષા ચેન્જ થશે.

IF ANY QUERY OR QUESTION,REVIEW-KINDLY WATSAPP US No. – 84859 76407