23/01/2019-B.SC-CHILD HEALTH NURSING-PAPER (DONE)-UPLOAD NO.2
23/01/2019-B.SC-CHILD HEALTH NURSING-PAPER NO.2
(KINDLY SEND YOUR UNIVERSITY PAPER IMAGE WATS APP ON – 8485976407 – WE PROVIDE ITS SOLUTION AS PER YOUR NEED)
SECTION-I
Q-1 Write on the following.(any two) (2×7-14)
(A) A three years child admitted with the complains of severe breathing difficulties and high grade fever. Write the nursing management of above patient
Case Overview
A 3-year-old child is admitted with severe breathing difficulty (dyspnea) and high-grade fever, which may indicate an acute lower respiratory tract infection such as pneumonia, bronchiolitis, or acute bronchitis. This is a medical emergency that requires immediate and focused nursing care to prevent respiratory failure, hypoxia, and sepsis.
Nursing management
Ineffective Breathing Pattern related to inflammatory process in the lungs as evidenced by increased respiratory rate, nasal flaring, use of accessory muscles, and breathlessness.
Nursing intervention :
- Assess and monitor respiratory rate, depth, pattern, and effort every 1–2 hours.
- Place the child in semi-Fowler’s or high Fowler’s position to promote lung expansion.
- Provide humidified oxygen therapy via nasal prongs or mask as prescribed to maintain SpO₂ ≥ 95%.
- Monitor oxygen saturation continuously using pulse oximeter.
- Suction airway gently if secretions are obstructing breathing, especially in case of bronchiolitis.
- Encourage deep breathing by offering play-based breathing exercises (e.g., blowing bubbles).
- Administer prescribed bronchodilators (e.g., salbutamol) and nebulization as ordered.
- Observe for signs of worsening distress like chest retractions, cyanosis, grunting.
Hyperthermia related to infection as evidenced by body temperature > 39°C, flushed skin, and irritability.
Nursing Interventions :
- Monitor body temperature every 2–4 hours using appropriate thermometer method.
- Administer prescribed antipyretics (e.g., paracetamol) as per pediatric dose.
- Encourage fluid intake to prevent dehydration and aid in temperature regulation.
- Provide tepid sponge bath and remove excess clothing to enhance heat loss.
- Monitor for signs of febrile seizure, especially in children under 5 years.
- Keep the room well-ventilated but warm enough to avoid chilling.
- Document response to fever management measures and antipyretics.
Ineffective Airway Clearance related to increased mucus production and inflammation as evidenced by cough, noisy breathing, and wheezing.
Nursing Interventions :
- Encourage coughing (in older children) or gently perform chest physiotherapy as indicated.
- Administer mucolytic and expectorant medications as prescribed.
- Perform postural drainage therapy if ordered by physician.
- Maintain adequate hydration to loosen respiratory secretions.
- Observe and record the nature, amount, and frequency of sputum or nasal discharge.
- Use suctioning cautiously to prevent trauma and maintain a patent airway.
- Educate parents on breathing support techniques like steam inhalation if appropriate.
Risk for Deficient Fluid Volume related to fever, tachypnea, and reduced oral intake.
Nursing Interventions :
- Monitor input and output accurately to assess hydration status.
- Offer small sips of water, ORS, or fluids frequently to maintain hydration.
- Monitor signs of dehydration such as dry lips, sunken eyes, and poor skin turgor.
- Administer IV fluids as prescribed if oral intake is not possible or sufficient.
- Assess daily weight and urine specific gravity to track hydration status.
Activity Intolerance related to respiratory distress and fever as evidenced by fatigue and reluctance to move or play.
Nursing Interventions :
- Encourage rest and avoid unnecessary physical activity until breathing stabilizes.
- Provide calm, quiet environment to conserve energy.
- Group nursing activities together to minimize exertion and promote adequate rest.
- Use age-appropriate methods (toys, stories) to provide psychological support.
- Monitor level of fatigue and response to care to adjust activity levels accordingly.
Parental Anxiety related to child’s acute illness and hospitalization.
Nursing Interventions :
- Explain the child’s diagnosis, treatment plan, and expected recovery pattern to the parents in simple terms.
- Allow parents to stay with the child and participate in care as appropriate.
- Provide regular updates and answer their queries patiently.
- Encourage expression of emotions and offer emotional reassurance.
- Involve parents in basic care activities to reduce their sense of helplessness.
Risk for Infection Spread related to communicable respiratory illness.
Nursing Interventions :
- Maintain standard precautions such as hand hygiene and use of PPE while handling the child.
- Isolate the child (if indicated) to prevent cross-infection in pediatric ward.
- Dispose of contaminated tissues and materials appropriately.
- Educate parents on cough hygiene and infection control practices at home.
- Disinfect toys, surfaces, and commonly touched items regularly.
Knowledge Deficit (Parent) related to management of respiratory illness and home care.
Nursing Interventions :
- Teach parents to recognize signs of respiratory distress such as fast breathing, chest retractions, or bluish lips.
- Demonstrate use of nebulizers or inhalers if prescribed for home use.
- Explain importance of medication adherence and completion of antibiotics if ordered.
- Emphasize proper nutrition, hydration, and hygiene practices at home.
- Provide written instructions or pictorial handouts for home care and emergency signs.
(B) Define growth and development. Explain the principles of growth and development.
Growth
Growth is a quantitative increase in the size, height, weight, or mass of the body or any of its parts. It refers to physical changes and can be measured in units (like centimeters or kilograms). Example : Increase in height or weight of a child.
Development
Development is a qualitative improvement in the functioning or capabilities of the individual. It refers to the maturation of physical, emotional, intellectual, and social abilities. Example : A child learning to speak, walk, or develop social skills.
Principles of growth and development
1. Principle of continuty
- Growth and development are continuous processes that start from conception and continue throughout life.
- Although the rate of growth may vary during different life stages (rapid during infancy, slow during middle childhood), it never completely stops.
- Example : Physical growth occurs rapidly during infancy and adolescence but continues subtly even in adulthood through cellular renewal.
2. Principle of Orderly Progression (Sequential Development)
- Development follows a definite, predictable sequence.
- This is also called the Cephalocaudal (head to toe) and Proximodistal (center to periphery) patterns.
- Example : A child first gains control over head movements before developing control over limbs.
3. Principle of Individual Differences
- Every child is unique and grows at their own pace.
- Influencing factors : Genetics, nutrition, environment, cultural background, and health conditions.
- Example : Some children may start walking at 10 months, while others may take 14-15 months.
4. Principle of Directionality
- Growth and development occur in specific directions:
- Cephalocaudal Direction : From head to toe (e.g., head control before standing).
- Proximodistal Direction : From the center of the body to outward extremities (e.g., control of arms before fingers).
- General to Specific : Broad motor skills develop before refined skills (e.g., grasping before writing).
5. Principle of Integration
- Simple skills gradually combine to form complex behaviors.
- Example : A child first learns to hold a pencil, then scribble, and later forms letters and words.
6. Principle of Interrelation of Growth and Development
- Physical, mental, emotional, social, and moral developments are interrelated.
- Example : A healthy child with good nutrition is likely to show better concentration and social skills.
7. Principle of Critical Periods
- Certain periods in life are especially important for specific types of development; these are known as critical or sensitive periods.
- Example : Language development is most critical between 2 to 5 years of age.
8. Principle of Maturation and Learning
- Development depends both on maturation (biological growth) and learning (environmental influences).
- Maturation provides the readiness, while learning helps in acquiring skills.
- Example : A child cannot learn to write before the muscles of the fingers are mature enough for fine motor control.
9. Principle of Predictability
- Growth patterns are predictable to a certain extent.
- Example : The eruption of primary teeth usually begins at around 6 months of age; the adolescent growth spurt typically starts around 10-12 years in girls and 12-14 years in boys.
10. Principle of Holistic Development
- Growth and development are holistic, affecting the body as a whole rather than isolated parts.
- Physical, intellectual, emotional, and social developments are interconnected and influence each other.
11. Principle of Uneven Development
- Different parts of the body and different abilities develop at uneven rates.
- Example : A child’s legs may grow faster during one phase, leading to a lanky appearance during adolescence.
12. Principle of Regression
- Sometimes, children may show temporary regression in behavior or skills during periods of stress or emotional disturbance.
- Example : A toilet-trained child may start bedwetting after the birth of a sibling.
13.Principle of Environment and Heredity
- Both genetic inheritance (heredity) and environmental factors play a crucial role in growth and development.
- Example : A child may have inherited a tall stature genetically, but poor nutrition can hinder growth.
(C) Define acute glomerulonephritis. Describe the nursing management
Acute Glomerulonephritis (AGN)
Acute Glomerulonephritis (AGN) is a sudden-onset inflammatory condition of the glomeruli — the filtering units of the kidneys — characterized by decreased glomerular filtration, hematuria (blood in urine), proteinuria, edema, and hypertension. It commonly occurs after a streptococcal infection (post-streptococcal glomerulonephritis) and leads to temporary but serious impairment of kidney function.
Nursing management og acute glomerulonephritis
✅ 1. Nursing Diagnosis : Excess Fluid Volume Related to decreased glomerular filtration and sodium retention as evidenced by facial edema, weight gain.
Goals :
Reduce fluid overload and prevent complications
Nursing Interventions :
- Monitor intake and output every 4 hours
- Record daily weight at the same time each day
- Restrict oral fluids and sodium-rich foods as per prescription
- Administer prescribed diuretics and observe response
- Assess for lung sounds (rales) and respiratory effort every shift
- Elevate edematous limbs to reduce swelling
- Maintain semi-Fowler’s position if respiratory distress is present
- Check for abdominal distension or ascites, and measure abdominal girth if indicated
- Use strict fluid balance charting to prevent overload
Risk for Imbalanced Nutrition Less than Body Requirement related to dietary restrictions, anorexia, nausea as evidenced by poor oral intake, fatigue, delayed healing
Goals :
Promote adequate nutrition to meet healing demands
Nursing Interventions :
- Provide frequent small meals that are low in salt and moderate in protein
- Encourage nutrient-dense foods such as fruit purees, rice, boiled vegetables
- Monitor for vomiting or nausea and provide antiemetics if prescribed
- Record calorie intake and compare with energy needs
- Collaborate with dietician for individualized renal diet plan
- Involve parents in meal planning and preparation at home
Risk for Infection related to immunosuppression, skin breakdown, urinary stasis as evidenced by elevated WBC count, open skin areas, exposure to invasive devices
Goals :
Prevent infection and maintain asepsis
Nursing Interventions :
- Enforce hand hygiene before and after patient contact
- Monitor temperature and WBC count daily
- Inspect urinary meatus and skin folds for signs of infection
- Keep perineal area dry and clean after urination
- Encourage daily bathing with gentle antiseptic solution
- Use aseptic technique during medication and IV administration
- Limit visitors during acute phase to reduce exposure to pathogens
Activity Intolerance related to fatigue, anemia, fluid retention as evidenced by tiredness during play, reduced physical activity
Goals :
Maintain rest while preventing deconditioning
Nursing Interventions :
- Provide bed rest during the acute phase
- Space nursing activities to prevent exertion
- Provide quiet environment to encourage sleep
- Encourage age-appropriate activities when stable (e.g., puzzles, books)
- Monitor for fatigue or shortness of breath during movement
- Support psychosocial needs by involving parents in calming the child
Knowledge Deficit (Parent) Related to Disease Condition related to lack of prior exposure or understanding of AGN as evidenced by repeated questions, non-compliance, anxiety
Goals :
Improve understanding and promote compliance with treatment
Nursing Interventions :
- Educate about AGN cause, course, and management using simple language
- Demonstrate ORS preparation and home BP monitoring if needed
- Provide printed educational material about diet and medication
- Discuss importance of follow-up appointments and lab tests
- Reinforce completing the full course of antibiotics
- Encourage caregiver to maintain a symptom diary
Risk for impaired skin integrity
Goals :
Preserve skin integrity and prevent pressure sores
Nursing Interventions :
- Turn the child every 2 hours and encourage repositioning
- Apply protective barrier creams over edematous or pressure areas
- Use soft bedding and avoid wrinkles in linen
- Inspect skin over bony prominences and pressure points daily
- Massage areas not red or inflamed to promote circulation
- Keep skin dry and hydrated, especially in perineal area
✅ 7. Documentation and Follow-Up
- Record all interventions, observations, and patient responses.
- Report any worsening signs (e.g., hematuria, severe hypertension, anuria) to the physician.
- Prepare discharge summary and reinforce need for regular follow-up with a pediatric nephrologist or physician.
Q-2. Write short note (Any Four) (4×4-16)
1. Importance of child health nursing.
1. Promotes Early Detection and Prevention of Illness
- Helps in early identification of common illnesses like upper respiratory tract infections, skin conditions, or diarrhea, which if untreated may lead to complications.
- Allows for timely referral to pediatricians or specialists when abnormalities in growth, behavior, or immunity are observed.
- Guides routine screening programs such as newborn hearing test, eye screening, and congenital disease detection in infants.
2. Ensures Proper Growth and Development Monitoring
- Assesses child’s physical, cognitive, and psychosocial milestones through standardized developmental charts and tools.
- Detects signs of failure to thrive, developmental delays, or behavioral concerns at an early stage for immediate intervention.
- Promotes the concept of well-child visits, which are routine health checks aimed at monitoring overall child progress.
3. Provides Age-Appropriate Health Education
- Educates caregivers on nutrition, immunization, hygiene, accident prevention, and child safety appropriate to the child’s age and developmental stage.
- Enhances parental confidence and skills in managing common childhood conditions at home.
- Guides adolescent children on puberty, mental health, and substance abuse prevention, promoting responsible health behavior.
4. Plays a Crucial Role in Immunization Services
- Administers vaccines as per the National Immunization Schedule (NIS) and educates parents about the need for booster doses.
- Helps in cold chain maintenance, documentation, and tracking of immunization defaulters to reduce vaccine-preventable disease burden.
- Assists in mass immunization campaigns like pulse polio and Measles-Rubella campaigns in schools and communities.
5. Manages Common Pediatric Illnesses and Conditions
- Provides nursing care for acute and chronic childhood conditions like asthma, infections, malnutrition, and congenital disorders.
- Supports medication administration, oxygen therapy, hydration, and nutritional rehabilitation under medical guidance.
- Offers home care instructions to reduce hospitalization rates and recurrence of illness.
6. Promotes Nutrition and Prevents Malnutrition
- Conducts nutritional assessment using tools like MUAC (mid-upper arm circumference), weight-for-age, and dietary recall.
- Educates parents about balanced diet, exclusive breastfeeding, and proper weaning practices.
- Collaborates with nutritionists and health workers to identify SAM/MAM children and initiate proper management.
7. Supports Mental and Emotional Health of Children
- Assists in identifying issues like ADHD, autism spectrum disorders, anxiety, school refusal, and adjustment disorders.
- Provides a therapeutic environment, play therapy, and emotional support to help children express their feelings.
- Coordinates with school counselors and child psychologists for behavioral therapy or mental health services.
8. Acts as a Link Between Child, Family, and Health System
- Bridges the communication gap by explaining complex medical information to parents in understandable language.
- Helps in continuity of care, arranging follow-up visits, rehabilitation, or long-term support systems.
- Collaborates with ASHA, ANMs, social workers, and pediatricians for community-based child health outreach.
9. Provides Emergency and Critical Care Support
- Trained to identify signs of respiratory distress, high fever, seizures, shock, or poisoning in children.
- Delivers first-line emergency care, maintains airway, breathing, circulation, and prepares child for emergency interventions.
- Monitors children in pediatric ICU, HDU, or neonatal units and responds rapidly to condition changes.
10. Contributes to Reducing Infant and Child Mortality
- Implements evidence-based protocols, such as those under IMNCI, to treat diarrhea, pneumonia, and neonatal sepsis effectively.
- Educates communities about safe delivery, newborn care, breastfeeding, and danger signs, thus improving early health outcomes.
- Supports public health goals like Sustainable Development Goals (SDGs) for reducing under-five mortality rate.
11. Plays a Role in Special Child Care and Disability Support
- Provides specialized nursing care for children with cerebral palsy, congenital heart defects, Down syndrome, or epilepsy.
- Facilitates rehabilitation therapies (e.g., speech, occupational, physical therapy) and connects families with special education services.
- Supports parents emotionally and practically in coping with long-term disabilities and chronic care.
12. Encourages Community Participation and Health Awareness
- Conducts school health programs, awareness rallies, and home visits for child health promotion.
- Engages families in growth monitoring sessions, immunization drives, and parenting workshops.
- Strengthens community capacity by involving local leaders, mothers’ groups, and volunteers in child health promotio
2. Phototherapy
Phototherapy is a common therapeutic procedure used in neonatology to treat neonatal hyperbilirubinemia (jaundice). It involves the exposure of the infant’s skin to a specific wavelength of blue light, which helps in the breakdown of unconjugated bilirubin into water-soluble isomers that can be excreted through bile and urine without liver conjugation.
Definition
Phototherapy is defined as the use of visible blue spectrum light, typically between wavelengths of 420–470 nanometers, to reduce serum bilirubin levels in newborns with jaundice.
Indications of Phototherapy
- Used in neonates with physiological jaundice when bilirubin levels exceed normal limits based on age and weight.
- Indicated in pathological jaundice due to blood group incompatibility (Rh or ABO), sepsis, or G6PD deficiency.
- Recommended in preterm infants with even lower levels of bilirubin due to higher risk of kernicterus.
- Used when total serum bilirubin (TSB) approaches phototherapy threshold as per Apgar and Bhutani nomogram.
- Sometimes used prophylactically in infants at high risk for severe hyperbilirubinemia.
Mechanism of Action
- Phototherapy reduces bilirubin through three main mechanisms:
- Photoisomerization: Converts bilirubin into lumirubin and other isomers that can be excreted without liver conjugation.
- Structural Isomerization: Breaks down bilirubin to non-toxic forms that are excreted in bile.
- Photooxidation: Produces oxidized products that are excreted in urine and bile.
Types of Phototherapy
Conventional Phototherapy : Fluorescent lamps with blue/white light placed 30–45 cm above the baby.
LED Phototherapy : Emits a specific wavelength with higher intensity and lower heat, more efficient than conventional light.
Fiberoptic Phototherapy (Bili-blanket) : Used for mild jaundice; light is delivered via a fiberoptic pad wrapped around the baby.
Double-Surface Phototherapy : Lights are applied both above and below the infant for maximum skin exposure.
Procedure of Phototherapy
- Infant is undressed except for the diaper and eye protection, placed under the phototherapy unit.
- Light intensity, distance, and wavelength are adjusted as per manufacturer’s recommendation.
- Infant is repositioned every 2–3 hours to ensure uniform light exposure.
- Eye pads are checked and cleaned regularly to prevent irritation or displacement.
- Temperature and hydration are monitored closely during therapy.
- Phototherapy is continued until serum bilirubin level falls to a safe range, monitored via periodic blood tests.
Advantages of Phototherapy
- Non-invasive, painless, and effective treatment for jaundice.
- Reduces the need for exchange transfusion, thereby minimizing risk.
- Can be started in hospital or home settings in selected mild cases (especially with Bili-blankets).
- Helps in preventing bilirubin encephalopathy and kernicterus, which are life-threatening complications.
Complications and Side Effects
- Dehydration due to increased insensible fluid loss.
- Diarrhea and skin rashes due to increased bilirubin breakdown.
- Hyperthermia or hypothermia due to improper light regulation.
- Bronze baby syndrome in infants with cholestasis.
- Retinal damage if eyes are not protected properly.
Nursing responsibility during photo therapy
Assess and monitor the newborn’s vital signs at regular intervals
- Monitor temperature, heart rate, respiratory rate, and oxygen saturation every 2–4 hours to detect early signs of distress.
- Watch closely for hypothermia or hyperthermia since phototherapy can interfere with the newborn’s thermoregulation.
Ensure proper positioning and skin exposure
- Place the infant in a supine position with minimal clothing, usually only a diaper, to maximize skin exposure.
- Reposition the baby every 2 to 3 hours to ensure even exposure to light and reduce the risk of pressure sores or burns.
Protect the newborn’s eyes adequately
- Cover the newborn’s eyes with clean, well-fitted eye patches or eye shields to prevent retinal damage from intense light.
- Remove eye covers during feeding, parent bonding, and assessments to avoid prolonged covering and monitor for signs of eye irritation.
Monitor fluid balance and prevent dehydration
- Observe for signs of fluid loss such as dry lips, reduced skin turgor, sunken fontanelles, and decreased urine output.
- Encourage frequent breastfeeding or formula feeding to compensate for increased insensible water loss.
- Administer IV fluids if ordered in case of poor oral intake or excessive fluid loss.
Assess stool pattern and urine output
- Monitor for increased frequency and loose greenish stools, which indicate the breakdown and excretion of bilirubin.
- Keep a record of urinary output and evaluate diaper weight if needed to ensure adequate hydration.
Maintain hygiene and prevent infection
- Change diapers frequently and clean the perineal area to prevent diaper rash or skin irritation.
- Maintain aseptic techniques when handling the baby and any IV lines or feeding equipment to prevent hospital-acquired infections.
Observe and document skin condition regularly
- Inspect the baby’s skin every shift for rashes, burns, or signs of ‘bronze baby syndrome’, especially in cholestatic jaundice.
- Monitor for erythema or blistering, which may indicate overheating or excessive light exposure.
Monitor bilirubin levels as per schedule
- Ensure blood samples are taken before initiating therapy and at prescribed intervals (usually every 12–24 hours) to evaluate therapy effectiveness.
- Document and report any rise in bilirubin levels despite therapy, which may suggest the need for escalated care like exchange transfusion.
Provide psychological support and education to parents
- Explain the purpose, procedure, and benefits of phototherapy to parents to alleviate fear and confusion.
- Reassure parents that jaundice is common and treatable, and answer all their queries with patience.
- Instruct on continuing breastfeeding, as it helps in bilirubin elimination.
Support thermoregulation and environmental control
- Maintain room temperature to avoid chilling or overheating.
- Cover the newborn with a light blanket during feeds or handling to prevent temperature fluctuations.
Ensure accurate documentation and communication
- Record start and stop times of therapy, bilirubin levels, feeding, I/O, skin assessment, and any unusual observations.
- Report signs of worsening jaundice, persistent fever, seizures, or poor feeding promptly to the pediatrician.
3. Initial steps of resuscitation
1. Ensure Scene and Self-Safety
- Before initiating resuscitation, it is important to assess the environment for safety hazards to both the nurse and the patient.
- Confirm that resuscitation equipment such as suction devices, oxygen source, bag and mask, laryngoscope, and radiant warmer is ready and functioning.
- Ensure the presence of assistance or call for help immediately to activate the resuscitation team.
2. Provide Warmth and Control Temperature
- Newborns are highly vulnerable to heat loss, so immediately place the baby under a radiant warmer to prevent hypothermia.
- Gently remove wet clothes or linen and wrap the baby in a warm, dry towel.
- Use pre-warmed towels or blankets to cover the baby, especially the head, to maintain body heat.
3. Position the Head and Airway
- Position the neonate in a supine posture with the head in a neutral (sniffing) position, which opens the airway.
- In neonates, a rolled towel under the shoulders may be used to maintain proper airway alignment.
- Avoid hyperextension or flexion of the neck as it may obstruct the airway and impair ventilation.
4. Clear the Airway
- Gently suction the mouth first, followed by the nose, using a bulb syringe or suction catheter to remove secretions, amniotic fluid, blood, or meconium.
- In meconium-stained amniotic fluid, suction should be performed only if the baby is non-vigorous (no cry, poor tone).
- Avoid deep or repeated suctioning which may cause trauma, bradycardia, or apnea.
5. Dry the Baby and Provide Tactile Stimulation
- Gently dry the baby thoroughly using a soft towel to stimulate crying and breathing.
- Replace the wet towel immediately with a dry and warm towel to avoid further heat loss.
- Provide tactile stimulation by rubbing the back or flicking the soles of the feet to encourage spontaneous breathing.
- Avoid vigorous stimulation or slapping which can injure the baby.
6. Assess the Infant’s Breathing and Heart Rate
- Look at the chest movement to assess if the baby is breathing spontaneously and effectively.
- Count the heart rate for 6 seconds and multiply by 10 using a stethoscope placed over the precordium or umbilical cord pulsations.
- If the baby is apneic, gasping, or heart rate is <100 bpm, proceed to positive pressure ventilation (PPV) immediately.
- If the heart rate is below 60 bpm, chest compressions must be started along with PPV.
7. Provide Positive Pressure Ventilation (PPV)
- Begin PPV with room air using a self-inflating bag and an appropriate-sized face mask if the baby is apneic or has a low heart rate.
- Ensure that the mask fits snugly over the nose and mouth to prevent air leaks.
- Observe for visible chest rise with each ventilation to confirm effective air entry.
- Reassess heart rate and respiration every 30 seconds after initiating PPV.
- Adjust technique or equipment if chest movement is inadequate or heart rate does not improve.
8. Administer Oxygen as Needed
- If available, attach oxygen to the bag and deliver 21–30% oxygen in term neonates, and up to 40–60% in preterm infants.
- For older infants and children, give high-flow oxygen using a mask or nasal cannula depending on the severity of respiratory failure.
- Monitor SpO₂ with a pulse oximeter, especially for preterm babies who require titrated oxygen therapy.
9. Call for Additional Help and Prepare for Advanced Support
- Activate the emergency code or call for help from the pediatric resuscitation team if available.
- Prepare for advanced interventions such as chest compressions, endotracheal intubation, or medication (e.g., epinephrine) administration if the infant’s condition does not improve.
- Keep emergency drugs and crash cart ready near the resuscitation area.
10. Provide Continuous Monitoring and Reassessment
- Continuously assess respiratory effort, heart rate, color, tone, and oxygen saturation.
- Document all the steps performed, including time of birth, time resuscitation was started, and the infant’s response to each intervention.
- Observe for improvement in color (from bluish to pink), spontaneous cry, and normalized breathing pattern.
4. Behavioral problems in children.
Definition
- Behavioral problems in children refer to patterns of disruptive, harmful, or socially unacceptable behavior that negatively impact the child’s learning, development, and relationships.
- It is considered a behavioral issue when the actions are persistent, inappropriate for the child’s age, and interfere with daily functioning.
- These problems may arise due to emotional distress, poor parenting, environmental stressors, neurological disorders, or developmental delays.
Common Types of Behavioral Problems in Children
Attention Deficit Hyperactivity Disorder (ADHD) :
- It is characterized by inattention, impulsivity, and hyperactivity, and affects academic performance and relationships.
- It is commonly seen in school-age children and may persist into adolescence.
Oppositional Defiant Disorder (ODD) :
- It is a pattern of angry, argumentative, and defiant behavior toward authority figures.
- It is often accompanied by irritability and low frustration tolerance.
Conduct Disorder :
- It includes aggressive behavior, lying, stealing, destroying property, and serious rule violations.
- It is a more severe condition and may lead to antisocial behavior later in life.
Anxiety Disorders :
- It includes separation anxiety, social anxiety, and specific phobias.
- It is presented as excessive fear, avoidance, and withdrawal.
Temper Tantrums and Aggression :
- It is common in toddlers, but if persistent and intense, it may indicate emotional dysregulation.
- It is usually triggered by frustration or unmet needs.
Autism Spectrum Disorders (ASD) :
- It includes communication difficulties, repetitive behaviors, and poor social interaction.
- Behavioral issues may arise due to sensory sensitivities or changes in routine.
Habit Disorders :
- It includes thumb-sucking, nail-biting, head banging, or hair-pulling.
- It may be a response to stress, anxiety, or attention-seeking behavior.
Enuresis and Encopresis :
- It is involuntary passage of urine or stool beyond the age of expected control.
- It may be linked to psychological distress, family conflict, or medical issues.
Causes and Contributing Factors
- It is due to genetic or neurobiological abnormalities (e.g., in ADHD or autism).
- It is often triggered by inconsistent parenting, harsh discipline, or neglect.
- It may be associated with parental conflict, divorce, or domestic violence.
- It is caused by exposure to trauma, abuse, or early life stress.
- It may develop due to peer pressure, bullying, or poor social support.
- It is sometimes related to screen overuse, sleep deprivation, or poor nutrition.
Signs and Symptoms
- Frequent temper outbursts, aggression, or defiance.
- Difficulty paying attention or sitting still.
- Withdrawal from social interaction or extreme shyness.
- Failure to follow rules, lying, or stealing.
- Repetitive behaviors or unusual movements.
- Poor academic performance and low self-esteem.
Nursing Management / Role of Nurse
Assessment and Identification :
- It is the nurse’s duty to assess behavioral patterns, duration, and severity.
- It is necessary to gather history from parents, teachers, and caregivers.
Health Education to Parents :
- It is to educate about normal child behavior vs. abnormal.
- It is to guide them on positive parenting, emotional bonding, and discipline.
Supportive Counseling :
- It is to offer emotional support to the child and family.
- It is to encourage open expression and develop trust through therapeutic communication.
Behavioral Modification Techniques :
- It is to use positive reinforcement, reward systems, and time-out techniques.
- It is to teach problem-solving and self-regulation.
Play Therapy and Recreational Activities :
- It is to use play as a medium for expression and emotional release.
- It is effective in children with fear, trauma, or communication issues.
Referral and Coordination :
- It is to refer severe cases to child psychologists, psychiatrists, or counselors.
- It is to collaborate with school teachers, social workers, and therapists.
School Health Involvement :
- It is to conduct screening programs and awareness campaigns.
- It is to guide teachers in managing difficult behavior in class.
Monitoring and Follow-Up :
- It is to track progress, adjust interventions, and provide long-term support.
5. Play Therapy
- Play therapy is a form of psychotherapy that uses play as a medium to help children express their feelings, thoughts, and experiences, especially when they are unable to do so through verbal communication.
- It is used for children who are dealing with emotional distress, trauma, anxiety, or behavioral problems, and it allows them to communicate in their natural language – play.
Objectives of Play Therapy
- It is to help the child express suppressed emotions such as anger, fear, confusion, and sadness through symbolic play.
- It is to provide emotional support and foster understanding and insight into the child’s inner world.
- It is to help the child develop social skills and build healthy relationships with others.
- It is to assist the child in coping with trauma, hospitalization, or illness in a supportive and safe environment.
- It is to enhance self-confidence, self-regulation, and adaptive behavior in the child.
Types of Play Therapy
Directive Play Therapy :
- It is a therapist-led method in which the play activities are structured, goal-oriented, and guided by the therapist.
- It is used when a specific problem or behavior is to be addressed, such as aggression, trauma-related fears, or inappropriate social behavior.
- Examples include: using a puppet show to discuss abuse, role-play to explore fears, or a board game to promote decision-making.
- It is best for children who need clear direction, have difficulty initiating activities, or are struggling with structured environments.
Non-Directive (Child-Centered) Play Therapy :
- It is based on the belief that children have the internal drive to resolve their own issues if provided a supportive environment.
- The child chooses the toys, sets the theme, and leads the play, while the therapist observes and reflects.
- The therapist offers minimal intervention, only helping the child feel heard and understood.
- It is useful for shy, withdrawn, anxious, or abused children, where building trust is essential.
- It fosters autonomy, self-confidence, and emotional release.
Structured Play Therapy :
- It is a systematic approach in which the play is designed with specific therapeutic goals in mind.
- The therapist plans sessions with predefined activities, such as emotion cards, sand play, or art activities.
- It is commonly used in clinical, educational, or hospital settings where time is limited, and therapy needs to be efficient.
- This type is helpful in children with learning disabilities or behavioral problems where repeated patterns can be observed and guided.
Therapeutic Play :
- It is used to help children overcome minor anxieties, stress, or adjustment issues, especially during hospitalization, surgery, or chronic illness.
- It includes use of medical dolls, storytelling, coloring, or breathing games to prepare a child for medical procedures.
- This type is more informal and is often used by pediatric nurses to reduce hospital-related anxiety or needle phobia.
- Its goal is emotional support, comfort, and distraction.
Group Play Therapy :
- It involves a small group of children engaging in therapeutic play under the supervision of a trained therapist.
- It helps children learn social interaction, turn-taking, cooperation, and conflict resolution.
- It is used for children with peer-related issues, social anxiety, or behavioral problems in school or community settings.
- Group dynamics allow the therapist to observe relational patterns, leadership traits, and emotional triggers.
Filial Therapy :
- It is a specialized type of play therapy in which parents are trained to conduct therapeutic play sessions with their own children.
- It strengthens parent-child bonding, improves emotional understanding, and empowers parents to support their child’s mental health.
- Parents are guided to use reflective listening and empathic play techniques.
- It is effective in managing family conflict, trauma recovery, or attachment disorders.
Sand Tray Play Therapy :
- It involves the use of a sandbox filled with sand and a collection of miniature toys and figures.
- Children create scenes or stories in the sand, which reflect their inner world, conflicts, or past experiences.
- It is especially helpful for children who are non-verbal, abused, or have suffered trauma, as it provides a non-threatening medium.
- It allows for symbolic expression and subconscious processing of emotional issues.
Digital or Virtual Play Therapy :
- It is a modern form of play therapy using technology like tablets, computers, or online games.
- It is especially useful in telehealth settings or during situations like the COVID-19 pandemic.
- It allows therapists to connect with tech-savvy children or adolescents through storytelling apps, interactive games, or digital drawings.
- Caution is required to maintain therapeutic control and avoid over-stimulation.
Indications / Uses of Play Therapy
- It is useful in children with anxiety disorders, phobias, or PTSD.
- It is helpful for children with developmental disorders like autism or ADHD.
- It is used in cases of abuse, neglect, grief, or family conflict.
- It is beneficial for children hospitalized with chronic illnesses or those undergoing medical procedures.
- It is effective in promoting emotional expression in children with speech or communication difficulties.
Benefits of Play Therapy
- It is to provide a safe emotional outlet for children who cannot express verbally.
- It is to help in emotional healing and psychological adjustment.
- It is to strengthen problem-solving and coping skills in children.
- It is to encourage creativity, imagination, and exploration.
- It is to build trust and therapeutic relationships between the child and therapist.
Role of nurse in play therpy
Assessment of the Child’s Needs
- It is the responsibility of the nurse to assess the child’s developmental stage, emotional status, behavioral issues, and psychosocial background before initiating play therapy.
- It is important for the nurse to identify underlying stressors or medical conditions that may influence play behavior.
- It is through observation and parental interviews that the nurse gathers relevant information to plan appropriate play activities.
Planning and Selection of Appropriate Play Materials
- It is the nurse’s role to choose age-appropriate, safe, culturally relevant, and therapeutic toys or play materials (e.g., soft toys, coloring books, dolls, medical kits).
- It is essential to plan structured or unstructured activities based on whether directive or non-directive play therapy is being used.
- It is the nurse’s duty to ensure materials do not promote aggression or fear and are clean and infection-free.
Creating a Safe and Supportive Environment
- It is the nurse’s role to provide a warm, welcoming, non-judgmental, and private setting where the child feels secure to express emotions.
- It is important for the nurse to remove any potential threats or distractions from the environment.
- It is crucial to maintain emotional and physical safety throughout the session.
Facilitation and Observation During the Session
- It is the duty of the nurse to gently guide, observe, and support the child during the play session, especially in structured play therapy.
- It is important to interpret play patterns, behaviors, and symbols which may give clues to the child’s emotional issues.
- It is vital that the nurse remains patient, calm, and empathetic, without forcing conversation or reactions.
Therapeutic Communication
- It is the nurse’s role to use therapeutic communication techniques such as active listening, reflection, and validation during or after the play session.
- It is important to build a trusting therapeutic relationship, especially in cases of abused or withdrawn children.
- It is necessary to respect the child’s pace of communication and not interrupt symbolic expression.
Family Education and Involvement
- It is the nurse’s responsibility to educate parents or caregivers about the benefits of play therapy and involve them when appropriate (as in filial therapy).
- It is to help parents understand the child’s needs, emotional state, and behavioral improvements through play therapy.
- It is also to train parents in supportive play techniques to continue therapy at home.
Documentation and Reporting
- It is the nurse’s duty to maintain detailed records of the play therapy sessions, including child behavior, interaction patterns, progress, and therapeutic outcomes.
- It is to report observations to the multidisciplinary team, such as pediatricians, psychologists, or social workers for integrated care.
- It is to document any signs of abuse or neglect revealed during therapy as per legal and ethical protocols.
Q-3. Define (Any Four) (4×2-8)
1. Birth Asphyxia
Birth asphyxia is a medical condition in which a newborn baby fails to initiate and sustain normal breathing at birth, leading to decreased oxygen supply (hypoxia) and increased carbon dioxide (hypercapnia) in the blood. It can cause serious damage to the brain and other vital organs if not managed promptly.
2. Cold Chain
The Cold Chain is a temperature-controlled supply chain system used for the storage, transportation, and distribution of vaccines and other temperature-sensitive medical products. It ensures that vaccines maintain their potency and effectiveness from the point of manufacture to the point of administration.
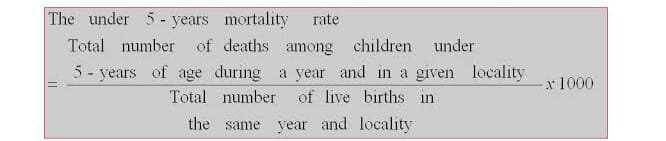
3. Under Five Mortality Rate
The Under-Five Mortality Rate (U5MR) refers to the probability of a child born in a specific year or period dying before reaching the age of five, expressed per 1,000 live births. It is a key indicator of child health and overall development in a country.
4. Immunization
Immunization is the process by which a person is made immune or resistant to an infectious disease, typically by the administration of a vaccine. It stimulates the body’s immune system to recognize and fight pathogens (bacteria, viruses, etc.), preventing future infections.
5. Intussusceptions
Intussusception is a medical condition in which a part of the intestine slides into an adjacent part of the intestine, similar to how parts of a telescope slide into one another. This leads to intestinal obstruction, compromised blood supply, and can cause serious complications if not treated promptly.
SECTION-II
Q-4. (A) You are working as a staff nurse in primary health centre, how will you organize immunization clinic in your centre ? (6)
✅ Planning and Preparation (Before the Session)
- It is the responsibility of the staff nurse to assist in monthly and weekly microplanning of immunization sessions (fixed, outreach, and mobile).
- It is to prepare due-lists of children under 1 year, pregnant women, and dropouts using :
- Immunization register
- MCP (Mother and Child Protection) card
- Eligible couple and child tracking register
- It is to coordinate with ASHA and ANM to mobilize the beneficiaries on session days.
- It is to identify the session sites (PHC/sub-centers/anganwadis) and inform the community in advance.
✅ Vaccine and Logistics Management
- It is to ensure all vaccines are available in adequate quantity as per the National Immunization Schedule (e.g., BCG, OPV, Hepatitis B, Pentavalent, IPV, Measles-Rubella, Rotavirus, Td, PCV, JE where applicable).
- It is to verify and maintain the cold chain system :
- Store vaccines in Ice-Lined Refrigerator (ILR) at 2°C to 8°C.
- Transport vaccines using Vaccine Carriers with 4 conditioned ice packs for outreach sessions.
- It is to check expiry dates and Vaccine Vial Monitors (VVM) for color change before use.
- It is to arrange all essential supplies :
- Auto-disable (AD) syringes
- Hub cutter
- Anaphylaxis management kit
- MCP cards and registers
- Red and black color-coded bins
- Soap or sanitizer for hand hygiene
✅ Immunization Session Setup
- It is to select a clean, ventilated, well-lit area with adequate seating arrangements.
- Ensure separate areas for :
- Registration and counseling
- Vaccination and observation
- It is to follow infection control protocols, including :
- Hand hygiene
- Use of gloves
- Safe waste disposal after injection
✅ Pre-Vaccination Activities
- It is to screen the child/pregnant woman before immunization :
- Check for fever, contraindications, or previous AEFI history.
- It is to verify the due vaccine as per the child’s age using the MCP card or due-list.
- It is to explain the importance of vaccination to the caregiver, including :
- Benefits of vaccines
- Common side effects (mild fever, swelling)
- Importance of completing the full schedule
✅ Vaccine Administration
- It is the nurse’s duty to follow the “Five Rights” of immunization :
- Right vaccine
- Right dose
- Right route
- Right site
- Right child
- It is to administer vaccines as per standard protocols. :
- BCG and Measles/MR – intradermal (left upper arm)
- OPV – oral (2 drops)
- Pentavalent/DPT/PCV – intramuscular (anterolateral thigh)
- It is to record the time of vaccine administration, batch number, and date in the immunization register and MCP card.
✅ Post-Vaccination Observation and Care
- It is to observe every vaccinated child for at least 30 minutes for early detection of Adverse Events Following Immunization (AEFI).
- It is to inform mothers about minor side effects and how to manage them at home.
- It is to advise on when to return for the next scheduled vaccination.
✅ AEFI (Adverse Event Following Immunization) Management
- It is essential to be prepared for emergencies, such as anaphylaxis or fainting.
- It is to keep a well-stocked AEFI kit, which includes:
- Inj. Adrenaline 1:1000
- Airway, IV fluids, syringes, spirit, cotton
- It is to immediately manage and report the AEFI, using standard AEFI reporting formats, and notify the Medical Officer.
✅ Recording and reporting
- It is to update all records accurately, including :
- Child’s MCP card
- Immunization register
- Stock and usage register
- Daily and monthly reports (submitted to block or district program officer)
- It is to track and follow up with dropout cases, ensuring full immunization.
✅ Health Education and Community Involvement
- It is to counsel mothers/caregivers on :
- Importance of completing the full immunization schedule
- Exclusive breastfeeding
- Hygiene and nutrition
- Identifying danger signs post-vaccination
- It is to coordinate with ASHA, AWW, ANM for community mobilization, especially in outreach areas.
(B) Write the nursing management of four years child having severe dehydration (6)
Deficient Fluid Volume related to excessive fluid loss through diarrhea and vomiting as evidenced by dry mucous membranes, sunken eyes, low urine output, and lethargy.
Nursing intervention :
- Monitor vital signs (heart rate, respiratory rate, blood pressure, temperature) every 2–4 hours to assess hydration status.
- Assess signs of dehydration like decreased skin turgor, sunken fontanelle (if applicable), dry lips, and prolonged capillary refill time.
- Maintain a strict intake-output chart, including urine, stool, vomitus, and oral/IV intake.
- Administer intravenous fluids such as Ringer’s Lactate or Normal Saline as prescribed by the pediatrician.
- Start oral rehydration solution (ORS) when vomiting subsides and the child is alert enough to drink.
- Record body weight daily and compare with baseline to evaluate fluid restoration.
- Observe for improvement in urine output, alertness, and skin elasticity as indicators of rehydration.
- Elevate head slightly and keep child in a lateral position if semi-conscious to prevent aspiration.
- Keep emergency medications and resuscitation kit ready in case of sudden deterioration.
Risk for Electrolyte Imbalance related to ongoing fluid losses and impaired absorption.
Nursing Interventions :
- Monitor serum electrolytes (sodium, potassium, chloride, bicarbonate) regularly.
- Observe for signs of electrolyte imbalance such as muscle cramps, twitching, confusion, arrhythmias, or altered mental status.
- Administer potassium and other electrolytes only after confirming adequate urine output.
- Educate parents about signs of electrolyte disturbances and emphasize importance of follow-up labs.
- Record ECG changes if potassium imbalances are suspected.
- Encourage small amounts of ORS frequently to balance electrolyte intake.
- Collaborate with the physician to adjust IV fluid composition based on lab reports.
Imbalanced Nutrition: Less than Body Requirements related to poor intake and gastrointestinal loss as evidenced by fatigue, weight loss, and weakness.
Nursing Interventions :
- Resume oral feeding with bland, easily digestible foods once the child can tolerate.
- Encourage frequent small meals rather than large ones to prevent nausea or vomiting.
- Offer familiar foods preferred by the child to increase willingness to eat.
- Monitor daily weight and nutritional intake closely to evaluate improvement.
- Consult pediatric dietitian for individualized diet plan including energy-rich and nutrient-dense foods.
- Avoid forcing food, but gently encourage and reward food acceptance.
- Assess for any feeding problems such as difficulty chewing or swallowing.
- Offer fluids with a spoon or cup instead of bottle to avoid air intake.
Risk for Hypovolemic Shock related to excessive fluid volume loss.
Nursing Interventions :
- Monitor vital signs every 15–30 minutes in critical stage to detect early signs of shock.
- Look for warning signs such as cold extremities, weak pulse, hypotension, restlessness, or decreased consciousness.
- Ensure IV line patency for immediate fluid or drug administration.
- Keep emergency crash cart and oxygen supply readily available at the bedside.
- Notify physician immediately if signs of shock appear.
- Position child supine with legs elevated to improve perfusion if shock is suspected.
- Provide high-flow oxygen if signs of respiratory distress are present.
- Reduce unnecessary handling of the child to prevent added stress.
Anxiety (Parental) related to child’s acute condition and hospital environment.
Nursing Interventions :
- Provide clear and simple explanation to parents regarding the child’s condition and treatment plan.
- Encourage parents to stay with the child to provide comfort and reduce separation anxiety.
- Allow participation of parents in simple care tasks like feeding, holding, or comforting the child.
- Offer emotional support by listening to their concerns and answering questions patiently.
- Provide updates at regular intervals about the child’s progress.
- Offer information leaflets or visuals to explain dehydration and its prevention.
- Encourage discussion about fears or previous similar experiences.
- Create a calm and reassuring environment during hospital stay.
Risk for Impaired Skin Integrity related to frequent diarrhea, immobility, and dehydration.
Nursing Interventions :
- Clean perianal area gently after every loose stool using mild soap and water.
- Apply barrier creams such as zinc oxide to prevent skin irritation and rash.
- Change diapers or underclothes frequently to keep skin dry.
- Keep bedding clean and wrinkle-free to avoid friction injuries.
- Turn and reposition child every 2 hours if bedridden to prevent pressure ulcers.
- Use breathable cotton garments and allow air circulation to the affected area.
- Inspect skin every shift and document condition to detect early signs of breakdown.
Knowledge Deficit (Parent) related to lack of information about signs, prevention, and management of dehydration.
Nursing Interventions :
- Educate parents on causes of dehydration like diarrhea, fever, excessive sweating, and poor intake.
- Teach early signs of dehydration such as dry mouth, less urination, irritability, and sunken eyes.
- Demonstrate preparation and correct use of oral rehydration solution (ORS).
- Provide handwashing education and hygiene tips to prevent infections causing dehydration.
- Encourage timely medical consultation in case of persistent vomiting or diarrhea.
- Offer educational leaflets or pictorial charts for better understanding.
- Emphasize importance of proper fluid intake during illness or hot weather.
- Involve parents in observing and reporting the child’s symptoms and behavior.
Q-5 Write on the following (Any four) (4×5-20)
1.Principles of IMNCI
- IMNCI (Integrated Management of Neonatal and Childhood Illness) is a comprehensive approach developed by WHO and UNICEF and adapted by Govt. of India to improve child survival and reduce infant and child mortality.
- It focuses on the most common and life-threatening illnesses among children under 5 years, including neonatal infections, pneumonia, diarrhea, malaria, measles, and malnutrition.
Principles of IMNCI (Expanded with Multiple Subpoints)
Integration of Preventive and Curative Care
- It is to combine treatment and health promotion in one approach for better child survival.
- It addresses acute illnesses like pneumonia, diarrhea, and malaria, as well as chronic issues like malnutrition and anemia.
- It promotes preventive strategies such as immunization, vitamin A supplementation, hand hygiene, and exclusive breastfeeding.
- It integrates growth monitoring, developmental assessment, and nutrition education with illness management.
Syndromic Approach for Case Management
- It is based on recognition of symptoms and clinical signs, not on sophisticated laboratory tests, making it suitable for peripheral settings.
- It uses algorithms and flowcharts to help identify and classify the illness severity.
- It reduces diagnostic delay, allowing immediate action.
- It is practical and easy to use for ANMs, ASHAs, and nurses working in low-resource settings.
Inclusion of Neonatal Care (0–7 Days)
- India expanded IMCI to IMNCI by including care for the first 7 days of life, recognizing that more than 60% of under-five deaths occur in the neonatal period.
- It focuses on early breastfeeding, cord care, temperature maintenance, and sepsis detection.
- It teaches health workers to identify danger signs in newborns such as poor feeding, convulsions, hypothermia, and fast breathing.
- It promotes Home-Based Newborn Care (HBNC) by ASHAs during postnatal visits.
Early Recognition and Prompt Referral
- It trains health workers to detect danger signs early, such as chest indrawing, lethargy, convulsions, or inability to feed.
- It emphasizes urgency in referral of Pink category cases to higher health facilities.
- It ensures life-saving interventions are not delayed due to waiting for medical officers.
- It supports a strong referral linkage between Sub-center, PHC, CHC, and District Hospital.
Use of Standard Treatment Protocols
- It uses evidence-based, color-coded charts (Pink, Yellow, Green) for classification and action.
- It improves accuracy, consistency, and confidence in health workers.
- It standardizes care delivery across various levels of the health system.
- It eliminates unnecessary medication use and irrational prescriptions.
Strengthening Health Worker Skills
- It provides hands-on training for nurses, ANMs, MPHWs, and ASHAs on child assessment, classification, and treatment.
- It builds problem-solving and decision-making ability in frontline workers.
- It emphasizes supportive supervision and on-job mentorship for sustained skill development.
- It enhances capacity-building at the grassroots level, improving service quality in rural areas.
Improvement of Health System Support
- It aims to ensure availability of essential drugs, logistics, and job aids.
- It improves record-keeping, supervision, and data management systems.
- It builds a referral transport system and communication link for emergency transfer of sick children.
- It encourages public-private partnerships and community involvement to strengthen health delivery.
Promotion of Family and Community Practices
- It educates caregivers about nutrition, immunization, hygiene, early signs of illness, and care-seeking behavior.
- It promotes exclusive breastfeeding for 6 months and complementary feeding thereafter.
- It improves maternal awareness of ORS preparation, zinc use, handwashing, and danger signs.
- It motivates families to seek timely health care rather than waiting until serious complications arise.
Promotion of Cost-Effective and Accessible Care
- IMNCI aims to provide quality health services at low cost, using simple and available technology.
- It avoids unnecessary hospitalization by managing mild and moderate illnesses at home or PHC level.
- It reduces the economic burden on families by reducing drug misuse and preventing complications.
- It ensures equity in care, reaching children from underserved, poor, tribal, or remote areas.
Monitoring and Follow-Up of Sick Children
- IMNCI ensures that every treated child is followed up within 2–5 days to assess improvement.
- It promotes home visits by health workers for nutritional counseling and therapy compliance.
- It reduces recurrence of illness and helps track defaulters of immunization or nutrition programs.
- It improves accountability and continuity of care from facility to home.
2.Benefits of breast feeding.
Benefits of Breastfeeding to the Infant
Provides Optimal Nutrition :
- It is naturally designed to meet the nutritional needs of the infant.
- It contains the right balance of proteins (whey and casein), fats, lactose, water, vitamins, and minerals.
- The composition of breast milk changes over time to match the baby’s changing needs (colostrum, transitional, and mature milk).
Strengthens Immune System :
- Breast milk is rich in antibodies (especially secretory IgA) that protect the infant’s mucous membranes.
- It contains lactoferrin, lysozyme, macrophages, leukocytes, and cytokines which fight infections.
- It protects against respiratory tract infections, otitis media, gastroenteritis, and urinary tract infections.
Promotes Neurological Development :
- It provides long-chain polyunsaturated fatty acids (DHA, ARA) crucial for brain and retinal development.
- Studies show better cognitive scores and higher IQ in breastfed infants compared to formula-fed infants.
Prevents Allergies and Atopic Conditions :
- It reduces the risk of food allergies, eczema, asthma, and dermatitis, especially in genetically predisposed children.
- Breast milk promotes gut flora and provides immune tolerance to new foods.
Reduces Risk of Chronic Illnesses Later in Life :
- Breastfeeding is associated with a lower incidence of obesity, diabetes (Type 1 and Type 2), hypertension, and cardiovascular diseases in later life.
- It enhances metabolic programming which protects against adult diseases.
Prevents Sudden Infant Death Syndrome (SIDS) :
- Exclusive breastfeeding during the first 6 months significantly reduces the risk of SIDS, likely due to improved respiratory and cardiac function during sleep.
Ensures Emotional Security :
- Close physical and eye contact during breastfeeding promotes bonding and emotional attachment, which enhances psychosocial development.
Promotes Oral and Dental Development :
- The sucking motion during breastfeeding strengthens oral muscles and encourages proper alignment of teeth.
- It reduces the risk of malocclusion, dental caries, and speech disorders.
Benefits of Breastfeeding to the Mother
✅ 1. Promotes Uterine Involution and Reduces Postpartum Bleeding
- It is one of the most immediate benefits of breastfeeding, as the act of suckling stimulates the release of oxytocin hormone.
- Oxytocin causes rhythmic contractions of the uterus, helping it shrink back to its pre-pregnancy size.
- It reduces the risk of postpartum hemorrhage, uterine atony, and promotes healing of the uterine lining.
✅ 2. Acts as a Natural Contraceptive (Lactational Amenorrhea Method – LAM)
- It is a temporary birth spacing method based on exclusive breastfeeding.
- Prolactin levels increase during breastfeeding, suppressing the release of Gonadotropin-Releasing Hormone (GnRH), which delays ovulation.
- It can provide 98% protection from pregnancy during the first 6 months, if:
- The mother is exclusively breastfeeding,
- She has not resumed menstruation,
- The baby is under 6 months of age.
✅ 3. Reduces Risk of Breast and Ovarian Cancers
- It is a proven long-term benefit, as breastfeeding suppresses ovulation and reduces lifetime estrogen exposure, which is linked to hormone-related cancers.
- The longer a woman breastfeeds across her lifetime, the greater the protection from:
- Breast cancer
- Ovarian cancer
- Endometrial cancer
✅ 4. Aids in Postpartum Weight Loss
- It is an effective natural way to lose pregnancy weight.
- Breastfeeding burns approximately 500–600 extra calories per day to produce breast milk.
- Helps the mother gradually return to her pre-pregnancy weight without extreme dieting.
✅ 5. Reduces Risk of Postpartum Depression and Enhances Emotional Well-being
- It improves the mother’s psychological state by releasing hormones like:
- Prolactin – promotes relaxation and nurturing behavior.
- Oxytocin – fosters bonding and emotional calmness.
- It lowers stress hormones (cortisol), reducing the risk of postpartum blues and depression.
✅ 6. Promotes Mother-Baby Bonding
- It creates a strong emotional connection through skin-to-skin contact, eye contact, and closeness.
- Frequent interaction builds confidence in caregiving and fosters secure attachment between mother and baby.
✅ 7. Economical and Convenient
- It is free, requires no sterilization or preparation, unlike formula feeding.
- Reduces :
- Cost of artificial milk or feeding supplies
- Time spent preparing and cleaning bottles
- Medical expenses due to fewer infections in breastfed infants
✅ 8. Reduces the Risk of Chronic Diseases
- Long-term breastfeeding has been shown to reduce the mother’s risk of:
- Type 2 diabetes (especially in women with gestational diabetes)
- Hypertension and heart disease
- Rheumatoid arthritis and osteoporosis later in life
✅ 9. Empowers Women and Improves Maternal Confidence
- It gives mothers a sense of satisfaction and accomplishment, knowing they are providing optimal nutrition and protection to their baby.
- It enhances self-esteem, maternal identity, and reduces anxiety about infant care.
Benefits to the Family and Society
Reduces Healthcare Costs
Breastfed babies fall sick less often, resulting in fewer hospital admissions and medication costs for families and governments.
Improves Family Bonding
Breastfeeding promotes closer parent-infant interactions, enhancing family bonding and reducing child neglect.
Environmentally Friendly
It produces no waste, packaging, or pollution, making it an eco-friendly choice compared to formula feeding.
Improves National Health Indicators:
Countries with high breastfeeding rates show lower infant mortality, higher school performance, and better economic productivity.
3.Essential new born care
- Essential Newborn Care (ENC) is defined as a set of comprehensive interventions provided to all newborns immediately after birth and during the first 28 days of life, regardless of place of birth or weight.
- It is aimed at reducing neonatal morbidity and mortality, promoting optimal growth and development, and preventing common complications such as infection, hypothermia, and birth asphyxia.
- It is a core part of the Reproductive, Maternal, Newborn, Child and Adolescent Health (RMNCH+A) strategy in India and recommended by WHO and UNICEF.
Objectives of Essential Newborn Care
- To reduce neonatal deaths by providing quality care at birth.
- To prevent complications like infection, hypothermia, and hypoglycemia.
- To support healthy growth, development, and early mother-infant bonding.
- To empower mothers and caregivers with knowledge of newborn care.
- To ensure early detection and referral of newborns with danger signs.
Components of Essential Newborn Care
✅ A. Immediate and Thorough Drying
- It is the first step after birth to remove amniotic fluid and stimulate breathing.
- The newborn is dried using a warm, clean, sterile towel immediately after birth before the cord is clamped.
- It helps prevent heat loss, which can lead to hypothermia.
✅ B. Skin-to-Skin Contact (Kangaroo Care)
- Baby should be placed on the mother’s bare chest or abdomen for skin-to-skin contact.
- This maintains warmth, supports bonding, and helps regulate the baby’s temperature, breathing, and heart rate.
✅ C. Early Initiation of Breastfeeding (within 1 hour)
- It provides colostrum, the first milk rich in antibodies and nutrients.
- Promotes immunity, prevents hypoglycemia, and encourages bonding.
- Suckling also stimulates oxytocin, which helps uterine contraction in the mother.
✅ D. Delayed Cord Clamping (1–3 minutes after birth)
- Delaying clamping allows placental blood to flow into the baby, increasing iron stores and reducing anemia.
- Cord is then clamped and cut with sterile equipment.
✅ E. Clean Cord Care
- No application of substances (like powders, oils, or antiseptics) unless medically indicated.
- Keep the cord stump clean, dry, and exposed to air to prevent infection (omphalitis).
✅ F. Thermal Protection
- Hypothermia is a leading cause of neonatal death.
- Newborns should be:
- Dried thoroughly
- Covered with a cap and blanket
- Kept close to the mother
- Delayed bathing for at least 24 hours
✅ G. Eye Care
- Eyes are cleaned with sterile gauze from inner to outer canthus.
- In some areas, prophylactic eye ointment (e.g., tetracycline) is applied to prevent ophthalmia neonatorum.
✅ H. Vitamin K Administration
- A single IM injection of 1 mg (term baby) or 0.5 mg (preterm baby) within 1 hour of birth.
- Prevents Vitamin K Deficiency Bleeding (VKDB), also known as hemorrhagic disease of the newborn.
✅ I. Weighing and Record Keeping
- Baby’s weight, length, head and chest circumference, and temperature should be recorded.
- Birth details like time, gender, and Apgar score (1 and 5 minutes) are documented.
✅ J. Immunization at Birth
- Newborn should receive the following vaccines before discharge :
- BCG – for tuberculosis
- OPV (0 dose) – for polio
- Hepatitis B (birth dose)
✅ K. Health Education to the Mother
- Teach mother about :
- Exclusive breastfeeding for 6 months
- Maintaining hygiene
- Recognizing newborn danger signs
- Importance of immunization and regular follow-up
Newborn Danger Signs (That Require Urgent Referral)
- Difficulty in feeding
- Fast or difficult breathing
- Convulsions
- Yellow discoloration of skin and eyes in first 24 hours
- Low body temperature
- Poor muscle tone or lethargy
- Umbilical redness or pus discharge
Role of Nurse in Essential Newborn Care given in detail
✅ 1. Preparation Before Delivery
- It is the responsibility of the nurse to prepare a clean, warm, and well-equipped delivery area, ensuring all supplies like sterile cord clamps, radiant warmers, towels, and resuscitation equipment are ready.
- It is essential to maintain infection control practices by following proper handwashing, sterile gloves, and use of clean delivery kits.
✅ 2. Immediate Care at Birth
- It is the nurse’s duty to receive the newborn in warm, sterile towels immediately after birth and begin gentle drying to prevent hypothermia.
- It is to assess the newborn’s breathing and color, and if necessary, initiate resuscitation following Neonatal Resuscitation Program (NRP) guidelines.
- It is to record the APGAR score at 1 and 5 minutes after birth.
✅ 3. Thermal Protection
- It is the nurse’s responsibility to prevent heat loss by :
- Placing the baby under a radiant warmer or on the mother’s chest for skin-to-skin contact.
- Covering the baby’s head with a warm cap and wrapping in a blanket.
- Delaying the first bath for at least 24 hours to maintain body temperature.
✅ 4. Early Initiation and Support of Breastfeeding
- It is the nurse’s duty to assist and encourage breastfeeding within the first hour of birth.
- It is to help the mother with proper positioning and attachment, ensuring the baby receives colostrum.
- It is to provide emotional support and build maternal confidence in exclusive breastfeeding.
✅ 5. Umbilical Cord Care
- It is the nurse’s role to clamp and cut the umbilical cord using sterile technique.
- It is to clean the cord area and keep it dry and exposed, avoiding any unprescribed substances.
- It is to observe the cord for signs of infection such as redness, pus, or foul smell.
✅ 6. Vitamin K Administration
- It is the nurse’s responsibility to administer 1 mg of Vitamin K intramuscularly to all term newborns (0.5 mg for preterm) within 1 hour of birth.
- It helps in preventing hemorrhagic disease of the newborn.
✅ 7. Monitoring and Assessment :
- It is to observe the newborn’s vital signs including temperature, heart rate, respiratory rate, and color regularly.
- It is to monitor urine and stool output, feeding adequacy, and general behavior of the baby.
- It is to detect early signs of complications like hypoglycemia, jaundice, or sepsis.
✅ 8. Immunization :
- It is the nurse’s role to administer the birth dose of vaccines such as:
- BCG – for tuberculosis
- OPV (Zero dose) – for poliomyelitis
- Hepatitis B (birth dose)
- It is also to document immunizations and inform the mother about the immunization schedule.
✅ 9. Health Education to the Mother and Family
- It is to educate the mother about exclusive breastfeeding, baby hygiene, thermal protection, and immunization.
- It is to counsel mothers on how to recognize newborn danger signs, such as :
- Poor feeding
- Difficulty breathing
- Yellowing of eyes and skin
- Cold hands and feet
- Convulsions or lethargy
- It is to provide instructions on follow-up visits, weight monitoring, and growth chart interpretation.
✅ 10. Documentation and Record Keeping
- It is the nurse’s responsibility to maintain accurate records of :
- Birth weight and measurements
- APGAR scores
- Time of breastfeeding initiation
- Medications and vaccines given
- It is also to document any complications or referrals made.
✅ 11. Referral and Emergency Management
- It is the nurse’s duty to identify high-risk newborns (preterm, low birth weight, birth asphyxia).
- It is to ensure timely referral to higher centers with proper stabilization and documentation.
- It is also to prepare transport with thermal protection and maintain oxygenation if needed.
4.Protein energy malnutrition
Definition
Protein Energy Malnutrition is a condition caused by a deficiency of protein and calories, mainly affecting infants and young children, leading to growth failure, muscle wasting, and increased risk of infections.
Causes
- Inadequate food intake (low protein and calorie diet).
- Poverty and poor socioeconomic status.
- Recurrent infections (diarrhea, measles, TB).
- Early weaning and improper complementary feeding.
- Lack of maternal education on nutrition.
- Large family size and food scarcity.
- Low birth weight and prematurity.
- Chronic illnesses (malabsorption, congenital diseases).
Types of Protein Energy Malnutrition (PEM)
1. Kwashiorkor
- Kwashiorkor is a form of severe malnutrition that occurs mainly due to inadequate protein intake despite sufficient calorie consumption, often seen in children between 1 to 3 years of age after early weaning from breast milk.
- Affected children typically present with generalized body swelling (edema), a rounded or “moon face” appearance, distended abdomen (pot belly), flaky paint-like skin lesions, and hair changes such as thinning, discoloration, and easy pluckability (flag sign).
- These children often appear apathetic, irritable, and suffer from frequent infections due to a compromised immune system.
2. Marasmus
- Marasmus is a severe form of malnutrition caused by a deficiency of both protein and calories, commonly affecting children below one year of age, especially in poor socioeconomic conditions.
- These children exhibit extreme wasting of muscles and fat, leading to a very thin, emaciated appearance with prominent ribs and sunken eyes.
- The skin becomes loose and wrinkled due to the loss of subcutaneous fat, and the child looks like a “skin and bones” case.
- Unlike kwashiorkor, there is no edema in marasmus, and the child often remains alert but irritable, and constantly hungry.
3. Marasmic-Kwashiorkor
- Marasmic-Kwashiorkor is a combined form of malnutrition where the child suffers from both severe energy (calorie) deficiency and protein deficiency simultaneously.
- This condition presents with features of both marasmus and kwashiorkor, where the child exhibits severe muscle wasting along with edema.
- These children are usually in a critical state, showing signs of extreme weakness, severe infections, impaired immunity, and poor healing of wounds.
- This type has a poor prognosis and requires immediate intensive nutritional and medical care.
4. Underweight (Mild to Moderate PEM)
- Underweight is a milder form of Protein Energy Malnutrition, where the child has low body weight for their age due to prolonged mild or moderate deficiency of essential nutrients, including proteins and calories.
- These children may not show dramatic symptoms like those seen in severe forms, but they experience delayed physical growth, slow development, decreased energy levels, and are more prone to recurrent infections due to weakened immunity.
- If not corrected early, this condition can progress to more severe forms of malnutrition.
Clinical Features
- Growth failure and stunted development.
- Severe weight loss or muscle wasting.
- Edema (present in kwashiorkor).
- Skin changes: hyperpigmentation, flaky paint dermatitis.
- Hair changes: thinning, discoloration, and easy pluckability.
- Poor wound healing and frequent infections.
- Delayed developmental milestones.
Management
📌 I. Immediate (Acute Phase) Management
This phase focuses on stabilizing the child’s critical condition, correcting deficiencies, and preventing complications.
Treat Hypoglycemia :
- Immediately provide 50 ml of 10% dextrose orally or IV if blood sugar is low.
- Start frequent small feeds to maintain normal glucose levels.
Correct Hypothermia :
- Keep the child warm using skin-to-skin contact (Kangaroo Mother Care) and warm clothing.
- Ensure the room is adequately heated.
Treat or Prevent Infections :
- Start empirical antibiotic therapy even if signs of infection are not obvious, as infections may be hidden.
- Common antibiotics : Amoxicillin, Ampicillin, or Gentamicin.
Correct Dehydration:
- Use low-osmolar ORS (ReSoMal) for rehydration.
- Avoid standard ORS as it may worsen electrolyte imbalance.
Correct Electrolyte Imbalance:
- Supplement potassium and magnesium to correct deficiencies.
- Avoid excessive sodium intake during this phase.
Treat Micronutrient Deficiencies :
- Provide Vitamin A, zinc, iron (after stabilization), folic acid, and multivitamins.
- Start iron only after the child begins to gain weight to avoid worsening infections.
📌 II. Nutritional Rehabilitation Phase
This phase focuses on gradual nutritional improvement and weight gain.
Start F-75 Formula :
- Low protein, low sodium diet initially to stabilize metabolism.
- Provide small, frequent feeds.
Transition to F-100 or Catch-Up Diet :
- After stabilization, shift to a high-energy, high-protein diet for rapid weight gain.
- Foods like milk-based formulas, eggs, pulses, oil, and locally available energy-dense foods.
Use of Ready-to-Use Therapeutic Foods (RUTF) :
- These are energy-dense, protein-rich pastes fortified with essential vitamins and minerals (e.g., Plumpy’Nut).
- Suitable for community-based management of severe malnutrition.
📌 III. Ongoing Care and Monitoring
Daily Monitoring :
- Monitor weight, temperature, hydration status, and signs of infections.
Psychosocial Stimulation :
- Encourage play and emotional bonding to promote mental and emotional recovery.
- Involve caregivers in interactive activities with the child.
Parental Counseling and Education :
- Educate caregivers on proper feeding practices, hygiene, and recognizing signs of relapse.
📌 IV. Follow-Up and Prevention of Relapse
- Ensure regular follow-up visits to monitor growth and development.
- Continue providing nutritional supplements as required.
- Promote immunization and regular health check-ups.
Prevention of Protein Energy Malnutrition (PEM)
1. Promotion of Exclusive Breastfeeding
- Encourage exclusive breastfeeding for the first 6 months of life to provide essential nutrients and immunity.
- Continue breastfeeding along with complementary feeding up to 2 years or beyond.
2. Timely and Adequate Complementary Feeding
- Introduce nutritious complementary foods at 6 months of age while continuing breastfeeding.
- Ensure the diet includes protein-rich foods like pulses, eggs, dairy products, meat, and energy-dense foods.
3. Nutrition Education for Mothers and Caregivers
- Educate families about the importance of a balanced diet and proper feeding practices.
- Teach mothers about locally available low-cost nutritious foods.
4. Control and Prevention of Infections
- Promote immunization as per national schedules to prevent diseases like measles, tuberculosis, and diarrhea.
- Ensure early detection and treatment of common infections to prevent nutritional depletion.
5. Regular Growth Monitoring and Health Check-ups
- Conduct regular growth monitoring using weight-for-age and MUAC measurements.
- Identify at-risk children early and provide timely interventions.
6. Improvement in Hygiene and Sanitation
- Promote safe drinking water, proper sanitation, and handwashing practices to prevent diarrheal diseases.
- Educate communities about food hygiene and safe food preparation.
7. Food Security and Poverty Alleviation Programs
- Implement government-supported programs like Mid-Day Meal Scheme, Integrated Child Development Services (ICDS), and Public Distribution System (PDS) to improve food availability.
- Ensure equitable access to food resources for underprivileged families.
8. Micronutrient Supplementation
- Provide supplementation of iron, folic acid, vitamin A, and zinc to children at risk.
- Fortification of commonly used foods (like salt, flour) with essential micronutrients.
9. Enhancing Maternal Nutrition
- Improve maternal nutrition during pregnancy and lactation to prevent low birth weight and early malnutrition in infants.
- Educate women about prenatal care and the importance of consuming iron, calcium, and folic acid supplements.
5.Kangaroo Mother Care.
Kangaroo Mother Care (KMC) is a method of caring for preterm and low birth weight infants through skin-to-skin contact, exclusive breastfeeding, and early discharge with follow-up, which helps maintain the baby’s body temperature, promotes bonding, and improves survival rates.
Objectives of KMC
- To provide a natural thermal environment for the baby through skin-to-skin contact.
- To promote and support exclusive breastfeeding.
- To enhance emotional bonding between mother and baby.
- To reduce the risk of hypothermia, infections, and mortality in low birth weight infants.
- To encourage early discharge and community-based care with proper follow-up.
Components of Kangaroo Mother Care (KMC)
1️⃣ Skin-to-Skin Contact
- Continuous and prolonged direct skin-to-skin contact between the mother (or other caregiver) and the baby.
- Helps maintain the baby’s body temperature, stabilizes heart and respiratory rates, and promotes bonding.
2️⃣ Exclusive Breastfeeding
- Encourages frequent and direct breastfeeding to ensure optimal nutrition and hydration.
- Stimulates breast milk production and strengthens the baby’s immunity through maternal antibodies.
3️⃣ Early Discharge and Proper Follow-Up
- Promotes early discharge from hospital when the baby is stable, with regular follow-up visits.
- Follow-up includes monitoring the baby’s weight gain, feeding adequacy, growth, and developmental milestones.
Procedure of KMC
1️⃣ Ensure that the mother is healthy, willing, and properly counseled about the process.
2️⃣ Dress the baby in a diaper and cap and place him/her upright between the mother’s breasts in direct skin-to-skin contact.
3️⃣ Cover both mother and baby with a warm cloth or KMC wrap to maintain warmth.
4️⃣ Continue KMC for as many hours as possible each day, ideally minimum 6–8 hours daily.
5️⃣ Encourage exclusive breastfeeding whenever possible and monitor the baby’s feeding and weight gain.
6️⃣ Continue KMC until the baby reaches a weight of 2500 grams or shows stable growth.
Advantages of KMC
- Maintains the baby’s body temperature and prevents hypothermia.
- Enhances breastfeeding success and improves weight gain.
- Reduces the risk of hospital-acquired infections.
- Promotes early discharge from the hospital.
- Improves emotional bonding between mother and baby.
- Decreases neonatal morbidity and mortality.
Role of Nurse in Kangaroo Mother Care (KMC)
1️⃣ Educating and Counseling Mothers
- The nurse plays a vital role in educating mothers and families about the importance, benefits, and techniques of KMC.
- Provide psychological support to mothers who may feel anxious or insecure about handling preterm or low birth weight babies.
2️⃣ Preparation and Support for KMC
- Assist the mother in maintaining personal hygiene and preparing for safe KMC practice.
- Help the mother in proper positioning of the baby for effective skin-to-skin contact, ensuring the airway remains open and the baby is comfortable.
3️⃣ Monitoring Baby’s Condition
- Regularly monitor the baby’s temperature, heart rate, respiratory rate, and oxygen saturation during KMC.
- Observe for any signs of distress, hypothermia, or feeding difficulties.
4️⃣ Promoting Exclusive Breastfeeding
- Encourage and assist mothers to initiate and maintain exclusive breastfeeding, offering support with latching and correct breastfeeding positions.
- Educate mothers about the importance of frequent feeding to ensure adequate nutrition.
5️⃣ Ensuring Infection Control
- Instruct mothers on proper hand hygiene before handling the baby.
- Maintain a clean environment to reduce the risk of infections.
6️⃣ Documentation and Record Keeping
- Accurately record the duration and frequency of KMC sessions.
- Document the baby’s weight gain, feeding patterns, and vital signs to assess progress.
7️⃣ Coordination of Follow-Up Care
- Ensure parents understand the importance of follow-up visits after discharge to monitor the baby’s growth and development.
- Provide reminders for immunizations and growth monitoring schedules.
8️⃣ Involving Family Members
- Encourage father and other family members to participate in KMC if the mother is unavailable, ensuring continuity of care.
Q-6. Fill in the blanks with appropriate words. (5)
1 .……………..is secreted during first three days after delivery.
Colostrum
2. A child start crawling at the age of ……….
6 to 9 months.
3. The anterior fontanel normal closes by ………months of age.
12 to 18 months
4. Ratio of chest compression and ventilation is…….for Neonate.
3:1 (3 compressions followed by 1 ventilation
5. ……………is the father of pediatrics.
Abraham Jacobi