23/07/2018-B.SC-MEDICAL SURGICAL-2-PAPER DONE-UPLOASD NO.2
23/07/2018-B.SC-MEDICAL SURGICAL-2-PAPER
kindly send your University paper’s Image watsapp us on 8485976407. we upload its solution immediately
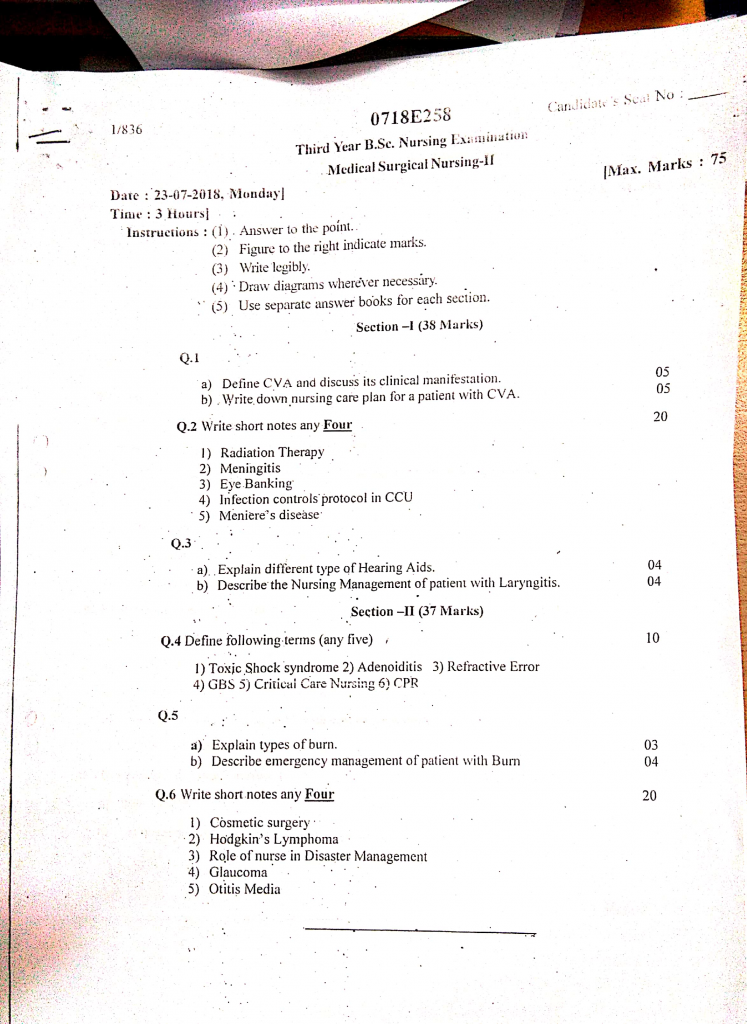
Section 1 (38 marks)
Q.1
1. Define CVA and discuss its clinical manifestation (5)
Definition
- A Cerebrovascular Accident (CVA), commonly referred to as a stroke, is a sudden onset of neurological deficit that results from an interruption in the cerebral blood flow due to either a blockage (ischemic stroke) or a rupture of blood vessels (hemorrhagic stroke) in the brain.
- It leads to loss of oxygen and nutrients to brain tissue, causing neuronal damage, brain ischemia, or cell death depending on the location and extent of damage.
- This condition is a medical emergency and can cause permanent disabilities or even death if not treated promptly.
Clinical Manifestations of CVA
The signs and symptoms of a CVA depend on the location of the lesion in the brain, extent of the damage, and type of stroke (ischemic vs. hemorrhagic). Here are the detailed manifestations:
1️⃣ Motor Deficits
- It is very common to observe sudden weakness or paralysis on one side of the body (hemiparesis or hemiplegia), typically contralateral to the affected hemisphere of the brain.
- It includes drooping of the mouth, inability to raise one arm, or leg weakness, which are classic signs.
- There is loss of fine motor control, causing difficulty in grasping or writing.
- Muscle tone may be hypotonic (flaccid) in early stages and then become hypertonic (spastic) in later stages.
- Reflexes such as the Babinski reflex may be abnormally positive on the affected side.
- Patients may experience difficulty in walking, frequent falls, and an unsteady gait due to poor balance.
2️⃣ Sensory Impairments
- Patients may report numbness, tingling, or decreased sensation on one side of the body.
- There is often impaired perception of temperature, pain, or touch, making the patient prone to injuries.
- Proprioception (sense of body position in space) is usually lost, leading to poor coordination and posture.
- In some patients, agnosia (inability to recognize objects, sounds, or sensations) may occur depending on cortical damage.
- There may be neglect syndrome, especially in right hemisphere strokes, where the patient ignores the left side of the body.
3️⃣ Visual Disturbances
- Hemianopia, especially homonymous hemianopia, is common – meaning loss of vision in the same half of both eyes.
- Patients may bump into objects or fail to see things on the affected side.
- Diplopia (double vision) may occur due to brainstem involvement or cranial nerve palsies.
- Visual-perceptual difficulties like difficulty judging distances or depth may affect reading and mobility.
4️⃣ Speech and Language Disorders
- It is often present in left hemisphere strokes, which dominate language function.
- Aphasia is a major symptom and occurs in various forms:
- Expressive Aphasia (Broca’s) – Patient can understand speech but cannot speak or write correctly.
- Receptive Aphasia (Wernicke’s) – Patient can speak fluently but with meaningless or nonsensical words; cannot understand spoken language.
- Global Aphasia – Severe form affecting both expression and comprehension.
- Dysarthria – Weakness or incoordination of the speech muscles causes slurred, slow, or unintelligible speech.
5️⃣ Cognitive and Behavioral Changes
- Patients often display confusion, poor memory, and difficulty concentrating on tasks.
- There may be impaired problem-solving and abstract thinking.
- Personality changes such as agitation, impulsivity, apathy, or depression are frequent.
- Emotional lability is common – patient may cry or laugh inappropriately due to loss of emotional control.
- Involvement of the frontal lobe may lead to poor judgment, loss of initiative, and social disinhibition.
6️⃣ Swallowing and Nutritional Problems
- Dysphagia (difficulty in swallowing) is common, especially in brainstem or cortical strokes.
- This increases the risk of aspiration pneumonia and malnutrition.
- Patients may also have weight loss, dehydration, or require tube feeding in severe cases.
7️⃣ Bladder and Bowel Dysfunction
- Some patients may develop urinary incontinence, retention, or a neurogenic bladder.
- Constipation or bowel incontinence may also occur due to immobility, medications, or neurological damage.
8️⃣ Altered Level of Consciousness
- (Especially in Hemorrhagic Stroke)
Large strokes, particularly hemorrhagic or brainstem strokes, may cause sudden loss of consciousness or even coma. - Other symptoms include severe headache, nausea, vomiting, and stiff neck, especially in subarachnoid hemorrhage.
- Seizures may occur during the acute phase of stroke, especially in cortical involvement.
9️⃣ Signs of Increased Intracranial Pressure (ICP) (Especially in Hemorrhagic Stroke)
- Patients may exhibit bradycardia, irregular respirations, and hypertension (Cushing’s triad).
- There may be pupil dilation on one side, papilledema, or loss of brainstem reflexes in severe cases.
2. Write down nursing care plan for a patient with CVA (5)
Impaired physical mobility related to neuromuscular dysfunction secondary to stroke
Goal :
The patient will maintain or improve physical mobility within limits of condition.
Nursing Interventions :
- It is important to assess muscle strength, tone, and coordination regularly in affected limbs.
- It is necessary to assist the patient in position changes every 2 hours to prevent pressure sores and contractures.
- It is advised to encourage active and passive range-of-motion exercises to maintain joint flexibility.
- It is helpful to collaborate with physiotherapists for ambulation and gait training using assistive devices.
- It is important to use supportive devices like footboards or splints to prevent foot drop.
Evaluation :
The patient participated in physiotherapy and demonstrated gradual improvement in limb movement and coordination.
Impaired verbal communication related to expressive or receptive aphasia
Goal :
The patient will express needs using available methods and show reduced frustration in communication.
Nursing Interventions :
- It is necessary to assess the type of aphasia (expressive, receptive, or global) to plan care.
- It is helpful to use communication aids such as picture boards, writing pads, or mobile apps.
- It is essential to speak slowly, clearly, and use simple sentences, allowing time for response.
- It is important to encourage the use of gestures, facial expressions, or nodding.
- It is advised to avoid correcting or interrupting the patient while trying to speak.
Evaluation :
The patient communicated needs using gestures and picture cards with reduced frustration.
Risk for aspiration related to impaired swallowing (dysphagia)
Goal :
The patient will remain free from aspiration and maintain a clear airway.
Nursing Interventions :
- It is important to assess for gag reflex and swallowing ability before offering food or fluids.
- It is necessary to position the patient in a high Fowler’s position during and after meals.
- It is advised to provide soft, thickened foods and avoid liquids that increase aspiration risk.
- It is important to have suction equipment readily available and monitor for signs of choking.
- It is essential to refer to a speech or swallowing therapist as needed.
Evaluation :
The patient tolerated oral feeding without coughing or choking and maintained adequate oxygenation.
Risk for impaired skin integrity related to immobility and reduced sensation
Goal :
The patient will maintain intact skin throughout hospitalization.
Nursing Interventions :
- It is necessary to perform daily skin assessments, especially on pressure-prone areas (sacrum, heels, elbows).
- It is advised to reposition the patient every 2 hours to relieve pressure and promote circulation.
- It is important to use pressure-relieving devices such as foam mattresses and heel protectors.
- It is essential to keep skin clean and dry, and apply moisture barriers to prevent breakdown.
- It is helpful to provide a nutritionally rich diet with protein and vitamins for skin healing.
Evaluation :
The patient’s skin remained intact with no signs of ulcer formation.
Self-care deficit (bathing, dressing, toileting) related to physical limitation
Goal :
The patient will gradually regain independence in performing self-care activities.
Nursing Interventions :
- It is important to assess the patient’s level of independence in daily activities using a checklist.
- It is necessary to assist with bathing, grooming, dressing, and toileting, while encouraging participation.
- It is advised to encourage use of unaffected limbs to perform tasks and promote autonomy.
- It is helpful to provide assistive devices like adaptive utensils, handrails, or grab bars.
- It is essential to praise efforts and progress to build self-confidence and motivation.
Evaluation :
The patient performed personal hygiene and dressing with minimal support using the unaffected hand.
Q.2 Write short notes (any four) (20 marks)
1. Radiation therapy
Definition
- Radiation therapy is a clinical treatment method that involves the use of controlled, high-energy ionizing radiation, such as X-rays, gamma rays, or charged particles, to kill or damage cancer cells while minimizing harm to surrounding normal tissue.
- It works by causing breaks in the DNA strands of rapidly dividing cancer cells, thereby inhibiting their ability to multiply and survive.
- Radiation therapy may be used as a curative treatment, an adjuvant therapy after surgery, a neoadjuvant therapy before surgery, or as a palliative therapy in advanced cancer to relieve symptoms such as pain, bleeding, or obstruction.
Goals and Purposes of Radiation therapy
- To destroy or shrink cancerous tumors without harming surrounding normal tissues.
- To prevent recurrence of cancer after surgery or chemotherapy.
- To relieve symptoms like pain, bleeding, or obstruction in advanced cancers (palliative radiotherapy).
- To reduce tumor size before surgery to make it operable (neoadjuvant therapy).
- To kill microscopic residual cancer cells left after surgery (adjuvant therapy).
Types of Radiotherapy
A. External Beam Radiation therapy (EBRT)
- It is the most widely used form of radiotherapy where radiation beams are delivered from a machine outside the body, such as a linear accelerator (LINAC).
- The patient lies on a treatment couch while the radiation machine rotates around them to deliver beams precisely to the tumor site from various angles.
- Techniques such as 3D-CRT (Three-Dimensional Conformal Radiation Therapy) and IMRT (Intensity-Modulated Radiation Therapy) help to shape the radiation dose to fit the tumor.
- It is usually given in daily fractions (sessions) over several weeks.
B. Internal Radiation therapy (Brachytherapy)
- In this technique, a radioactive source is placed directly into or near the tumor using applicators, needles, seeds, or catheters.
- It may be temporary (high-dose rate) or permanent (low-dose rate), depending on cancer type.
- It delivers a very high localized dose while sparing surrounding normal tissues.
- It is commonly used in gynecological cancers, prostate cancer, and oral cavity cancers.
C. Systemic Radiation therapy (Radioisotope Therapy)
- This method involves swallowing or injecting radioactive substances, such as radioiodine (I-131), strontium-89, or samarium-153, that circulate in the bloodstream and selectively target cancer cells.
- It is especially useful in thyroid cancer, bone metastases, and neuroendocrine tumors.
- This method requires isolation precautions due to systemic radioactivity.
Indications of Radiation therapy
Radiation therapy is used to treat a wide variety of malignant tumors, including :
- Breast cancer
- Cervical and uterine cancer
- Prostate cancer
- Head and neck cancers (larynx, pharynx, tongue, mouth)
- Lung cancer
- Esophageal and gastric cancer
- Brain tumors (gliomas, metastases)
- Skin cancers (basal cell, squamous cell carcinoma)
- Lymphomas (Hodgkin and non-Hodgkin)
- Pediatric cancers (e.g., medulloblastoma, rhabdomyosarcoma)
Side Effects of Radiation therapy
It may vary depending on site and dose
Local Side Effects
- Skin irritation, redness, or burns over the radiation site
- Hair loss in the treated area
- Oral ulcers, dry mouth (in head/neck radiation)
- Difficulty swallowing or sore throat (esophageal radiation)
- Diarrhea or abdominal cramps (abdominal or pelvic radiation)
- Vaginal dryness or bleeding (pelvic radiation)
Systemic Side Effects
- Fatigue
- Nausea and vomiting
- Anorexia and weight loss
- Suppression of bone marrow (in long-term or high-dose therapy)
- Risk of secondary malignancy (rare, long-term effect)
Nursing Responsibilities in Radiation therapy
A. Before Radiation therapy (Pre-procedure Nursing Care)
- The nurse must educate the patient and family about the procedure, possible outcomes, and common side effects in a compassionate manner.
- It is important to provide psychological support and reduce fear and anxiety related to the word “radiation”.
- The nurse must assess the patient’s physical baseline — weight, nutritional status, skin integrity, hydration, and vital signs.
- She ensures that any metallic objects (jewelry, implants) are noted and removed if they interfere with therapy.
- If the radiation field includes the pelvic area, patients may be instructed to empty or fill the bladder before treatment.
B. During Radiation therapy (Intra-procedure Care)
- The nurse should assist in accurate positioning of the patient on the radiation table to ensure the beam targets only the tumor site.
- She must observe for immediate adverse reactions such as dizziness, shortness of breath, or skin burning.
- The nurse should follow strict radiation safety protocols, including shielding, lead walls, and maintaining safe distance.
- During brachytherapy, the nurse should limit time spent in the radiation room, stand behind shielding, and wear a radiation dosimeter badge.
- Emotional support is important, as isolation during radiation can be psychologically distressing for many patients.
C. After Radiation therapy (Post-procedure Nursing Care)
- The nurse should inspect the radiation-exposed skin daily and report any signs of ulceration, blisters, or infection.
- It is essential to instruct the patient not to scratch, shave, or apply lotions or powders on the treated skin unless prescribed.
- Dietary counseling is required to manage nausea, mouth sores, weight loss, or bowel irregularities.
- The nurse should monitor complete blood counts (CBC) regularly if bone marrow is exposed, to assess for anemia, neutropenia, or thrombocytopenia.
- She must provide emotional and social support, especially for patients dealing with altered body image, infertility, or fatigue.
- Patient and family should be educated on long-term care, follow-up visits, and signs of complications that must be reported immediately.
Radiation Safety Guidelines for Nurses
- Follow ALARA principle (As Low As Reasonably Achievable) for exposure time.
- Maintain safe distance, use protective lead aprons or barriers, and avoid direct contact with radiation sources.
- Use a radiation badge to monitor cumulative exposure.
- Pregnant nurses should avoid assignments involving direct radiation exposure.
- Educate patients and their visitors about radiation hygiene and home precautions post-brachytherapy or systemic therapy.
2. Meningitis
Definition of Meningitis
- It is an acute or chronic inflammation of the meninges, the protective membranes covering the brain and spinal cord.
- It occurs due to infection of the cerebrospinal fluid (CSF) by bacteria, viruses, fungi, or other microorganisms.
- It is a medical emergency that may cause brain swelling, increased intracranial pressure (ICP), and neurological deficits if not treated promptly.
Types of Meningitis
1️⃣ Bacterial Meningitis
- It is the most severe and life-threatening type, caused by bacteria like Streptococcus pneumoniae, Neisseria meningitidis, and Haemophilus influenzae.
- It is highly contagious and needs urgent antibiotic treatment.
- It may occur as secondary to ear infections, sinusitis, or skull trauma.
2️⃣ Viral Meningitis
- It is caused by enteroviruses, herpes simplex virus (HSV), or mumps virus.
- It is generally milder than bacterial type, and most people recover without complications.
- It is more common in children and young adults.
3️⃣ Fungal Meningitis
- It is caused by fungi like Cryptococcus neoformans, especially in immunocompromised individuals (e.g., HIV/AIDS).
- It is usually chronic and slow-developing, and treatment requires long-term antifungal therapy.
4️⃣ Tuberculous Meningitis (TBM)
- It is caused by Mycobacterium tuberculosis, and often secondary to pulmonary TB.
- It presents with gradual onset, and may lead to hydrocephalus and neurological deficits.
5️⃣ Aseptic (Non-infectious) Meningitis
- It is caused by drugs, autoimmune diseases, or cancer, not infection.
- It mimics infectious meningitis but CSF culture is negative.
Etiology
- Bacteria (e.g., Neisseria meningitidis, Streptococcus pneumoniae)
- Viruses (e.g., enterovirus, HSV, mumps virus)
- Fungi (e.g., Cryptococcus)
- Tuberculosis
- Head trauma or skull fracture
- Immunosuppression (e.g., HIV)
- Ear or sinus infections
- Neurosurgical procedures
Pathophysiology of Meningitis
1️⃣ Invasion of Pathogen into CNS
It occurs through bloodstream, sinuses, or direct trauma to the skull, allowing microorganisms to enter CSF.
2️⃣ Multiplication and Inflammation
It is in the subarachnoid space that pathogens multiply, causing release of inflammatory mediators.
3️⃣ Increased Blood-Brain Barrier Permeability
It is the inflammation that causes disruption of the blood-brain barrier, allowing more fluid and immune cells into CSF.
4️⃣ Cerebral Edema and Increased ICP
It results in brain swelling, impaired perfusion, and intracranial hypertension.
5️⃣ Neuronal Injury and Complications
It leads to cell death, seizures, hearing loss, or coma if not controlled early.
Clinical Manifestations
- Sudden high fever
- Severe headache
- Neck stiffness (nuchal rigidity)
- Photophobia
- Nausea and vomiting
- Seizures
- Altered consciousness
- Positive Kernig’s and Brudzinski’s signs
- Bulging fontanelle (in infants)
Diagnostic Evaluation
- Lumbar puncture (CSF analysis)
- CSF culture and sensitivity
- CBC (↑ WBCs)
- Blood cultures
- CT/MRI (to rule out increased ICP)
- Serum electrolytes
- C-reactive protein (CRP)
Management
1️⃣ Antibiotic Therapy (Bacterial Meningitis)
- It is vital to begin empiric IV antibiotics immediately, commonly Ceftriaxone, Cefotaxime, or Vancomycin.
- It is modified later based on CSF culture sensitivity results.
- It is necessary to treat for 7–21 days, depending on the pathogen.
2️⃣ Antiviral Therapy (Viral Meningitis)
- It is administered for HSV meningitis using Acyclovir or Ganciclovir.
- Supportive care is often sufficient for most viral causes.
3️⃣ Antifungal Therapy (Fungal Meningitis)
- It includes Amphotericin B or Fluconazole, especially in immunocompromised cases.
4️⃣ Antitubercular Therapy (TB Meningitis)
- It involves RIPE regimen (Rifampicin, Isoniazid, Pyrazinamide, Ethambutol) with corticosteroids for inflammation.
5️⃣ Corticosteroids
- It is used to reduce cerebral edema and decrease neurologic complications, particularly in bacterial and TB meningitis.
6️⃣ Seizure Control
- It is managed with antiepileptic drugs (e.g., Phenytoin) if seizures occur.
7️⃣ Fluid and Electrolyte Balance
- It is essential to prevent dehydration, SIADH, and maintain cerebral perfusion.
Nursing Management
1️⃣ Neurological Assessment
- It is essential to monitor Glasgow Coma Scale (GCS), pupil reaction, and signs of increased ICP.
- It is important to assess headache severity, behavior, and level of alertness regularly.
2️⃣ Seizure and Safety Precautions
- It is necessary to pad side rails, keep suction ready, and avoid bright light and loud noise.
- It is the nurse’s role to record seizure duration and response to medication.
3️⃣ Infection Control
- It is vital to isolate the patient (droplet precautions) until 24 hours after starting antibiotics.
- It is necessary to use personal protective equipment (PPE) and hand hygiene strictly.
4️⃣ Monitoring and Medication
- It is important to administer IV antibiotics on time, monitor vital signs, and ensure fluid balance.
- It is necessary to assess for side effects of corticosteroids and antibiotics.
5️⃣ Hydration and Nutrition
- It is essential to ensure adequate fluid intake, especially if vomiting or fever is present.
- It may be necessary to provide enteral feeding if patient has decreased consciousness.
6️⃣ Psychosocial and Family Support
- It is helpful to explain the illness process and precautions to caregivers.
- It is important to provide emotional support and answer family concerns compassionately.
7️⃣ Health Education
- It is necessary to teach about vaccinations (e.g., meningococcal, pneumococcal, Hib).
- It is advised to seek early treatment for ear or sinus infections to prevent spread.
- It is important to follow-up for neurological sequelae such as hearing loss or cognitive delay.
3. Eye banking
Definition of Eye Banking
- Eye banking is a systematic and regulated medical service that involves the collection, preservation, evaluation, and distribution of human eyes or corneal tissue donated after death for the purpose of restoring vision through corneal transplantation, and for research and education.
- Eye banks work under strict legal, medical, and ethical guidelines, and play a vital role in the treatment of corneal blindness, which is the second most common cause of blindness in India after cataract.
Objectives of Eye Banking
- It is the primary objective of eye banks to collect and preserve donated human eyes in a safe and sterile manner.
- It is aimed at evaluating and screening the collected corneas to ensure suitability for transplantation.
- It is essential to distribute the healthy corneas to hospitals and surgeons for corneal graft surgeries.
- It is also the objective to create public awareness about eye donation, to reduce the gap between demand and supply of donor tissue.
- It serves as a training center for ophthalmic staff, and provides materials for corneal research and academic purposes.
Functions of Eye Bank
1️⃣ Collection of Donated Eyes
- It is the responsibility of the eye bank to collect eyes from registered and voluntary donors after death.
- The donation must occur within 6 hours of death, and proper informed consent must be obtained from the next of kin.
- Eye banks often operate through Hospital Cornea Retrieval Programs (HCRP) and home collection services.
2️⃣ Evaluation and Screening of Donor Eyes
- After collection, it is essential to perform a medical evaluation to rule out any infectious diseases such as HIV, Hepatitis B, C, sepsis, or rabies.
- Eye banks use specular microscopy, slit-lamp examination, and serology tests to assess the quality of corneal tissue.
- It is important to classify corneas as suitable for therapeutic use, research, or educational purposes.
3️⃣ Preservation and Storage
- It is essential to preserve donor corneas in sterile preservation media such as McCarey-Kaufman (MK) medium, Optisol-GS, or Cornisol.
- These media help to store corneas for 7–14 days depending on the solution used.
- Preservation must be done under controlled temperature (4°C) and sterile conditions.
4️⃣ Distribution and Transplantation
- It is the duty of the eye bank to allocate corneas to certified ophthalmic surgeons based on urgency and priority.
- Documentation must be maintained for traceability, utilization, and surgical outcomes.
- Emergency cases like corneal perforation or ulceration are given priority for transplantation.
5️⃣ Education and Public Awareness
- Eye banks conduct regular awareness programs, rallies, seminars, and health talks to promote eye donation.
- They collaborate with NGOs, schools, hospitals, and religious leaders to encourage voluntary pledging.
- Campaigns like Eye Donation Fortnight (August 25 – September 8) are observed to boost community participation.
Eligibility for Eye Donation
- Any person, regardless of age, gender, or religion, can donate eyes after death.
- People with cataracts, spectacle use, hypertension, or diabetes can still donate their corneas.
- Individuals with communicable diseases like HIV/AIDS, hepatitis, septicemia, and active cancers are not eligible for donation.
Legal and Ethical Guidelines
- Eye donation is regulated in India by the Transplantation of Human Organs and Tissues Act, 1994 (THOTA).
- Consent must be obtained ethically and in writing by trained personnel.
- No financial or commercial transactions are allowed in the donation or allocation of eye tissues.
- Eye banks must ensure confidentiality, respect, and dignity of the donor.
Role of Nurse in Eye Banking
- It is the duty of the nurse to motivate and counsel grieving families about the importance of eye donation.
- It is necessary for the nurse to identify potential donors in hospital ICUs, wards, or emergency departments, especially when brain death or death is declared.
- The nurse should immediately inform the eye bank team upon patient death to ensure timely retrieval.
- It is important to assist with documentation, consent process, and ensure privacy and comfort for the donor family.
- Nurses also play a major role in community health campaigns, school visits, and health melas to educate the public about myths and facts related to eye donation.
- During preservation, the nurse may help in eye enucleation, applying dressing, and maintaining sterile protocol.
4. Infection controls protocols in CCU
It is important to understand that the critical care unit (ICU/CCU/NICU/PICU) involves care of patients who are critically ill and often on life support systems, invasive monitoring, or long-term hospitalization.
Due to this, these patients are at high risk of acquiring infections, especially nosocomial infections (hospital-acquired infections). Therefore, a comprehensive infection control protocol is essential to ensure patient safety, prevent cross-contamination, and promote healing.
INFECTION CONTROL PROTOCOLS IN ICU
1️⃣ It is mandatory to practice strict Hand Hygiene at all levels
- It is the most effective and primary method of preventing the spread of microorganisms in the ICU.
- It is essential to perform handwashing with soap and water when hands are visibly soiled and to use alcohol-based hand rub when hands are not visibly dirty.
- As per WHO’s 5 Moments for Hand Hygiene, it is compulsory to clean hands :
- Before touching a patient
- Before a clean/aseptic procedure
- After body fluid exposure
- After touching a patient
- After touching patient surroundings
2️⃣ It is necessary to use Personal Protective Equipment (PPE)
- PPE includes gloves, gowns, surgical/N95 masks, face shields, shoe covers, and caps.
- It is important to use appropriate PPE based on the risk of exposure to body fluids or infectious material.
- It is mandatory to follow the correct donning (putting on) and doffing (removing) sequence to prevent self-contamination.
- PPE should be disposed of in biohazard containers after use.
3️⃣ It is critical to follow Aseptic Techniques during all invasive procedures
- In procedures like urinary catheterization, central line insertion, suctioning, tracheostomy care, wound dressing, and IV infusion, it is essential to use sterile gloves, sterile drapes, and antiseptic solution.
- It is required to maintain a no-touch technique and ensure only sterile instruments and items are used.
4️⃣ It is important to maintain Environmental Hygiene in the ICU
- It is mandatory that the surfaces, bed rails, trolleys, and equipment are cleaned and disinfected daily with 1% sodium hypochlorite.
- It is important to clean ventilators, infusion pumps, ECG machines, and monitors with alcohol wipes after each use.
- It is vital to maintain proper air ventilation using HEPA filters in ICU setup.
5️⃣ It is essential to prevent Ventilator-Associated Pneumonia (VAP)
- VAP is one of the most common infections in ventilated patients.
- Nursing actions to prevent VAP include:
- Keeping the head of the bed elevated to 30–45 degrees
- Performing oral care with chlorhexidine every 4 hours
- Using closed suction systems
- Avoiding unnecessary ventilator disconnections
- Checking and emptying ventilator tubing condensate safely
6️⃣ It is important to prevent Central Line-Associated Bloodstream Infection (CLABSI)
- Central lines can introduce organisms directly into the bloodstream.
- Prevention protocols include:
- Using full sterile barrier precautions during insertion
- Cleaning insertion site daily with chlorhexidine solution
- Changing dressings with sterile technique
- Monitoring the site for redness, pus, or swelling daily
7️⃣ It is essential to prevent Catheter-Associated Urinary Tract Infections (CAUTI)
Nurses must :
- Insert urinary catheters only when absolutely necessary
- Ensure aseptic insertion and maintenance of closed drainage system
- Perform daily perineal hygiene
- Remove catheters as early as possible to reduce risk
8️⃣ It is vital to follow Biomedical Waste Management Protocols
- It is important to dispose of all waste, including PPE, needles, dressings, etc., as per color-coded segregation rules:
- Yellow bag – Infectious waste
- Red bag – Contaminated plastic
- White container – Sharps like needles
- Blue bag – Glassware
- It is mandatory not to recap needles and to use needle destroyers or puncture-proof containers.
9️⃣ It is required to practice Isolation and Barrier Nursing Techniques
- Patients with highly contagious infections like MRSA, TB, COVID-19, C. difficile must be isolated in separate rooms.
- Nursing care involves :
- Using separate equipment for each patient
- Wearing PPE before entry and discarding before exit
- Labeling the patient room as “Infection Precaution”
- Limiting visitors and instructing them on precautions
🔟 It is important to follow Surveillance and Reporting Systems
Infection control nurses must :
- Monitor infection trends like VAP, CAUTI, CLABSI
- Report outbreaks to the hospital infection control committee
- Collect specimens for culture sensitivity and track resistance patterns
- Conduct root cause analysis for each hospital-acquired infection
1️⃣1️⃣ It is necessary to ensure Staff Education and Training
- Regular workshops, infection control audits, and training sessions must be conducted.
- Nurses must stay updated with national guidelines (e.g., CDC, WHO, NCDC India) and follow hospital protocols.
- It is encouraged to create a culture of safety and accountability in critical care areas.
5. Meniers disease
Definition of Ménière’s Disease
- It is a chronic inner ear disorder characterized by episodic vertigo, sensorineural hearing loss, tinnitus, and a feeling of fullness in the ear.
- It is associated with excess endolymphatic fluid (endolymph hydrops) in the inner ear, affecting the balance and hearing mechanisms.
- It is a relapsing and remitting condition, commonly affecting individuals between 40 to 60 years of age.
Types of Ménière’s Disease
1️⃣ Classical (Typical) Ménière’s Disease
- It is the form where all 4 major symptoms (vertigo, hearing loss, tinnitus, and ear fullness) are present.
- It occurs in repeated episodes, with symptoms resolving partially between attacks.
- It typically starts unilaterally, but may progress to bilateral involvement in 10–40% of cases.
2️⃣ Cochlear Ménière’s Disease
- It presents mainly with hearing symptoms, such as tinnitus and hearing loss, without vertigo.
- It may be an early stage or partial form of Ménière’s disease.
3️⃣ Vestibular Ménière’s Disease
- It involves primarily vertigo and balance disturbances without significant hearing loss.
- It may occur as an isolated balance disorder, especially in early stages.
Etiology
- Idiopathic (unknown cause)
- Excess endolymphatic fluid (hydrops)
- Viral infections (e.g., herpes virus)
- Autoimmune inner ear disease
- Allergies or food sensitivities
- Head or ear trauma
- Genetic predisposition
- Migraine-associated vertigo
Pathophysiology of Ménière’s Disease
1️⃣ Excess Endolymph Production or Impaired Absorption
It is the overproduction or blocked drainage of endolymph fluid in the membranous labyrinth that causes inner ear pressure.
2️⃣ Distension of Inner Ear Structures
It is the stretching of the endolymphatic sac and duct, which affects hair cells of cochlea and vestibular apparatus.
3️⃣ Abnormal Nerve Signal Transmission
It is due to the pressure and damage on sensory receptors, leading to distorted hearing and balance signals to the brain.
4️⃣ Recurrent Episodes of Vertigo and Hearing Disturbances
It causes temporary or progressive sensory deficits, with inflammatory or autoimmune responses possibly contributing.
5️⃣ Progressive Degeneration
It may lead to permanent hearing loss, chronic tinnitus, and debilitating balance issues if untreated.
Clinical Manifestations
- Recurrent episodes of vertigo (lasting 20 min to hours)
- Tinnitus (ringing or buzzing in ear)
- Sensorineural hearing loss (initially fluctuating, then permanent)
- Feeling of fullness or pressure in affected ear
- Nausea, vomiting (during vertigo episodes)
- Loss of balance or unsteadiness
- Anxiety and fatigue after attacks
Diagnostic Evaluation
- History collection
- Physical examination
- Audiometry (sensorineural hearing loss)
- Electronystagmography (ENG)
- Glycerol dehydration test
- Electrocochleography
- MRI (to rule out acoustic neuroma)
- History of ≥2 spontaneous vertigo episodes lasting ≥20 min
- Clinical symptom assessment
Medical Management
1️⃣ Lifestyle and Dietary Modifications
- It is advised to follow a low-sodium diet (<1500 mg/day) to reduce fluid retention.
- It is important to avoid caffeine, alcohol, and tobacco, which can aggravate symptoms.
- It is helpful to manage stress, as stress can trigger episodes.
2️⃣ Pharmacologic Therapy
- It includes Diuretics (e.g., hydrochlorothiazide) to reduce endolymphatic fluid pressure.
- Antihistamines (e.g., meclizine) and anticholinergics (e.g., scopolamine) help in controlling vertigo.
- Antiemetics (e.g., promethazine) are used during acute attacks to control nausea and vomiting.
- Benzodiazepines (e.g., diazepam) may be used short-term for severe vertigo episodes.
3️⃣ Vestibular Rehabilitation Therapy (VRT)
- It is a physical therapy program designed to improve balance, coordination, and adaptation to motion sensitivity.
- It is especially helpful in chronic or post-attack recovery phases.
4️⃣ Invasive Procedures and Surgery (for Refractory Cases)
- Intratympanic steroid injections may reduce inflammation and vertigo.
- Intratympanic gentamicin (ototoxic) may reduce vertigo but risk hearing loss.
- Endolymphatic sac decompression surgery is done to relieve fluid pressure.
- Vestibular nerve sectioning or labyrinthectomy is used in severe, drug-resistant cases.
Nursing Management
1️⃣ Assessment and Monitoring
- It is important to assess the frequency, duration, and severity of vertigo attacks.
- It is necessary to evaluate for hearing changes, tinnitus intensity, and gait stability.
- It is essential to monitor vital signs during an acute attack (risk of fall, hypotension due to vomiting).
2️⃣ Fall Prevention and Safety
- It is crucial to keep the patient in bed during vertigo attacks to prevent injury.
- It is advised to remove fall hazards, provide assistive devices, and ensure safe mobility during recovery.
- It is necessary to teach patients to move slowly when changing positions.
3️⃣ Medication Management
- It is the nurse’s responsibility to administer prescribed diuretics, anti-vertigo agents, and antiemetics.
- It is important to monitor fluid and electrolyte levels, especially during diuretic therapy.
- It is necessary to educate the patient about side effects, including drowsiness and dry mouth.
4️⃣ Psychosocial and Emotional Support
- It is essential to provide reassurance, as patients may feel anxious or depressed due to unpredictable attacks.
- It is helpful to involve family members in care and educate them about the condition.
- It is advised to provide support for occupational or vocational limitations if the disease becomes chronic.
5️⃣ Dietary and Lifestyle Education
- It is important to teach the importance of a low-sodium, caffeine-free diet.
- It is necessary to advise avoiding alcohol, smoking, and excess salt or sugar intake.
- It is helpful to emphasize stress reduction techniques, such as yoga, meditation, or breathing exercises.
6️⃣ Patient Education and Follow-up
- It is vital to teach patients about identifying triggers, recording symptom diaries, and adhering to treatment.
- It is necessary to inform about the importance of regular ENT check-ups and audiometry follow-up.
- It is helpful to explain that Ménière’s disease is manageable, but not completely curable.
Q.3
1. Explain different types of hearing aids (4)
- A hearing aid is a small electronic device worn in or behind the ear that amplifies sound for individuals with hearing loss.
- It consists of a microphone (to receive sound), amplifier (to increase the sound), and receiver (to send amplified sound to the ear).
Different Types of Hearing Aids
1️⃣ Behind-The-Ear (BTE) Hearing Aid
- It is worn behind the pinna (ear) and connected to a custom ear mold via a small plastic tube.
- It is suitable for mild to profound hearing loss and is most commonly prescribed for all age groups.
- It is larger in size, making it easier to handle, clean, and adjust especially for elderly patients.
- It supports multiple sound programs, Bluetooth connectivity, and directional microphones.
- It has longer battery life and is often more durable than smaller styles.
2️⃣ In-The-Ear (ITE) Hearing Aid
- It is custom-fitted into the outer ear bowl (concha) and is visible but compact.
- It is suitable for mild to severe hearing loss, and includes manual volume control and telecoil features.
- It is larger than canal devices, which makes it easier to insert and remove for patients with reduced dexterity.
- It may pick up more wind noise, which could affect outdoor hearing clarity.
- It may not be ideal for very small ear canals or excessive earwax.
3️⃣ In-The-Canal (ITC) Hearing Aid
- It fits partially into the ear canal, making it less visible than ITE aids.
- It is used for mild to moderately severe hearing loss and offers natural sound amplification.
- It is custom-molded and fits tightly, reducing wind and external noise.
- It is smaller than ITE, but may be harder to handle or clean, especially for elderly.
- ITC aids may not be suitable for individuals with chronic ear infections.
4️⃣ Completely-In-Canal (CIC) Hearing Aid
- It is placed deep into the ear canal, making it nearly invisible when worn.
- It is ideal for mild to moderate hearing loss and cosmetically preferred by young adults.
- It uses the natural shape of the ear to direct sound efficiently into the canal.
- It is more vulnerable to moisture, sweat, and earwax, which may damage internal components.
- Battery life is shorter due to small size and limited battery capacity.
5️⃣ Receiver-In-Canal (RIC) / Receiver-In-The-Ear (RITE) Hearing Aid
- It has the receiver (speaker) inside the ear canal while the rest of the device sits behind the ear.
- It provides clearer and more natural sound with less distortion.
- Suitable for mild to severe hearing loss, and is a lightweight, discreet option.
- It offers open-fit technology, which keeps the ear canal more ventilated.
- Many models come with rechargeable batteries, Bluetooth connectivity, and noise cancellation features.
6️⃣ Bone-Anchored Hearing Aid (BAHA)
- It is a surgically implanted device that bypasses the middle and outer ear by conducting sound through bone vibration to the inner ear.
- It is used in patients with conductive hearing loss, mixed hearing loss, or single-sided deafness (SSD).
- Suitable for those with malformed ears, chronically draining ears, or atresia (closed ear canal).
- The device consists of a small titanium implant, an abutment, and a detachable sound processor.
- It may be magnet-based (invisible under skin) or abutment-based (visible post).
- Provides excellent sound clarity in cases where regular hearing aids are not effective.
7️⃣ Body-Worn Hearing Aid
- The microphone and amplifier are located in a small device worn on the body, with a wire leading to the earpiece.
- It is typically used in profound hearing loss or by individuals who cannot tolerate behind-the-ear designs.
- Though rarely used today, it offers high-powered amplification.
- It is easier to operate, especially for those with vision or dexterity issues.
- It is often used in low-resource settings or pediatric populations for ease of handling.
8️⃣ Digital Hearing Aids
- These devices use digital signal processing (DSP) to convert sound into digital code, adjust it, and convert it back.
- They automatically adjust volume and background noise based on the environment.
- Available in all styles (BTE, ITE, CIC, etc.) with customizable settings.
- Offers features like directional microphones, Bluetooth pairing, feedback suppression, and remote control via mobile apps.
- Digital aids provide clearer, crisper sound quality and are preferred over analog models.
2. Describe the nursing management of patient with laryngitis (4)
1️⃣ Airway and Breathing Support
- It is essential to monitor the patient’s airway patency and observe for signs of upper airway obstruction, such as stridor or gasping.
- It is important to maintain the patient in a semi-Fowler’s or high Fowler’s position to reduce laryngeal edema and facilitate breathing.
- It is necessary to provide humidified air or steam inhalation 2–3 times daily to help moisten the airways and reduce inflammation.
- It is also advised to encourage the patient to breathe through the nose instead of the mouth to filter and humidify air naturally.
- In severe cases, be prepared to assist with emergency airway support or oxygen therapy.
2️⃣ Voice Rest and Communication
- It is necessary to advise complete voice rest – no talking, whispering, or singing – to prevent vocal cord strain.
- It is helpful to provide communication aids such as whiteboards, mobile apps, or writing tools to avoid verbal effort.
- It is important to explain that whispering strains the larynx more than speaking softly, and should be avoided.
- Educate the patient that repeated vocal misuse during laryngitis can lead to chronic hoarseness or nodules.
- It is also advised to limit conversation even in writing-intensive roles, to avoid throat-clearing habits.
3️⃣ Hydration and Nutrition
- It is essential to maintain adequate oral fluid intake (2–3 liters/day) to loosen mucus and soothe the throat.
- It is beneficial to offer warm fluids like soups or herbal teas with honey to reduce throat discomfort.
- It is advised to avoid caffeinated, carbonated, or acidic beverages as they may irritate the throat lining.
- Encourage a nutrient-rich, soft diet to promote healing and avoid pain during swallowing.
- In case of painful swallowing, cold liquids like ice chips may be temporarily soothing.
4️⃣ Pain and Symptom Relief
- It is necessary to administer analgesics (e.g., paracetamol or ibuprofen) to manage sore throat and fever.
- It is helpful to perform or advise warm saline gargles 3–4 times daily to reduce inflammation and microbial load.
- It is important to monitor for progression of pain, fever, or inability to swallow, which may indicate complications like abscess.
- Throat lozenges or sprays containing benzocaine may be provided for temporary relief.
- Cold compress around the neck may be applied to reduce local swelling, if tolerated.
5️⃣ Medication Administration and Monitoring
- It is essential to administer prescribed antibiotics only if a bacterial infection is confirmed.
- It is necessary to give antitussives or mucolytics for dry cough and to promote rest.
- In allergic laryngitis, administer antihistamines or anti-allergic medications and monitor for drowsiness or side effects.
- In chronic cases, inhaled corticosteroids or proton-pump inhibitors may be prescribed (if reflux-related); ensure adherence.
- Observe for side effects or allergic reactions to prescribed medications and report them promptly.
6️⃣ Patient Education and Health Promotion
- It is important to educate the patient to avoid smoking, passive smoke, and exposure to dust, fumes, or chemicals.
- It is necessary to advise the patient to rest the voice even after recovery, to prevent recurrence.
- Teach the importance of using a soft, relaxed voice and voice modulation techniques if they are a professional voice user (e.g., teacher/singer).
- Recommend humidifiers at home, especially during dry seasons, to prevent recurrence.
- Promote flu vaccination and proper hand hygiene to reduce the risk of upper respiratory infections.
7️⃣ Monitoring and Follow-up
- It is necessary to monitor vital signs, respiratory rate, and SpO₂, especially if breathing difficulties are reported.
- Assess voice quality and swallowing ability daily, and note any signs of worsening hoarseness.
- It is important to document daily observations on throat pain, fever, voice tone, and medication compliance.
- Arrange for ENT referral if hoarseness or symptoms persist beyond 2–3 weeks, or if chronic laryngitis or vocal cord lesions are suspected.
- Educate the patient about the possibility of needing laryngoscopy or voice therapy during follow-up.
Section 2
Q.4 Define the following terms (any five) (10 marks)
1. Toxic shock syndrome
- It is a rare but life-threatening condition caused by bacterial toxins, most commonly from Staphylococcus aureus or Streptococcus pyogenes.
- Toxic shock syndrome is a serious systemic infection that results from the release of toxins into the bloodstream, often linked to tampon use, surgical wounds, or skin infections.
- It is characterized by sudden onset of high fever, low blood pressure, rash, and multi-organ dysfunction, due to the body’s extreme immune response to bacterial exotoxins.
2. Adenoiditis
- It is an inflammation or infection of the adenoids, which are lymphatic tissues located in the upper part of the throat behind the nose (nasopharynx).
- Adenoiditis is a condition in which the adenoids become swollen or infected, interfering with normal breathing and ear drainage.
- It is usually caused by bacterial or viral pathogens, and it commonly occurs in children, leading to symptoms such as nasal blockage, mouth breathing, and snoring.
3. Refrective error
It is a common visual disorder in which the eye is unable to properly focus light on the retina, resulting in blurred or distorted vision. It is caused by abnormalities in the shape of the cornea, lens, or eyeball length, leading to improper refraction of light rays. In short, refractive error refers to a condition in which the eye does not bend (refract) light correctly, making it difficult to see clearly at various distances.
Examples include :
- Myopia (Nearsightedness)
- Hyperopia (Farsightedness)
- Astigmatism
- Presbyopia
4. GBS
- It is an acute, rapidly progressive autoimmune disorder in which the body’s immune system mistakenly attacks the peripheral nerves, leading to muscle weakness, numbness, and sometimes paralysis.
- In which the myelin sheath covering the nerves is damaged, disrupting the nerve signals, usually starting in the legs and ascending upwards (ascending paralysis).
- It is also known as an acute inflammatory demyelinating polyradiculoneuropathy (AIDP), which is the most common form of GBS.
5. Critical care nursing
- It is a specialized area of nursing practice that involves the care of patients with life-threatening conditions who require comprehensive and continuous monitoring, advanced medical interventions, and skilled nursing support in intensive care units (ICUs) or emergency settings.
- It is also known as Intensive Care Nursing because it focuses on managing patients with severe and complex illnesses such as multi-organ failure, shock, sepsis, or major surgeries.
- In critical care nursing, the nurse is trained to work with advanced technologies (like ventilators, monitors, and life-support systems) and is part of a multidisciplinary team to stabilize and support critically ill patients.
6. CPR
- CPR (Cardiopulmonary Resuscitation) is a life-saving emergency procedure that combines chest compressions and rescue breaths to maintain circulation of oxygenated blood to the brain and vital organs when a person’s heart has stopped beating (cardiac arrest) or they have stopped breathing.
- It is intended to temporarily support circulation and breathing until advanced medical help becomes available. CPR helps in preserving brain function, preventing tissue death, and increasing survival chances in sudden cardiac arrest.
Q.5
1. Explain types of burns (3)
Burns are classified based on the depth of tissue damage into the following major types :
1️⃣ Superficial Burn (First-Degree Burn)
- It is a type of burn that involves only the epidermis, which is the outermost layer of the skin.
- It causes redness, mild swelling, pain, and a dry surface without the formation of blisters.
- It usually results from sunburn, brief contact with hot objects, or mild scalds.
- The healing occurs within 3 to 7 days, and it typically does not leave scars.
- It may be associated with mild discomfort or tenderness, but no permanent tissue damage.
2️⃣ Partial-Thickness Burn (Second-Degree Burn)
- It is a deeper type of burn that involves both the epidermis and part of the dermis (the second layer of the skin).
- It presents with blisters, intense redness, swelling, and moist or weepy skin, and is usually very painful.
- It can occur due to scald injuries, flames, or prolonged contact with hot objects.
- Healing may take 10 to 21 days depending on the depth, and scarring or pigmentation may develop.
- It is further divided into:
- Superficial partial-thickness burn (heals faster, less scarring)
- Deep partial-thickness burn (slower healing, possible scarring or surgical intervention needed)
3️⃣ Full-Thickness Burn (Third-Degree Burn)
- It is the most severe type of burn that destroys the entire epidermis and dermis, and may extend into subcutaneous tissue.
- The affected area may appear dry, leathery, waxy, white, charred, or brown, and is usually painless due to nerve ending destruction.
- It can result from prolonged flame exposure, chemical burns, or electrical burns.
- Spontaneous healing is not possible, and surgical intervention with skin grafting is usually required.
- It always results in permanent scarring and functional loss if not properly treated.
4️⃣ Fourth-Degree Burn (Extended Deep Burn)
- It is a very severe form of burn that involves damage beyond the skin layers into underlying tissues, such as muscles, tendons, and bones.
- The burned area appears charred, black, or exposed, and there is complete loss of sensation and function.
- It often occurs in high-voltage electrical injuries, major fire accidents, or explosions.
- It requires multiple surgical procedures, amputations, and leads to long-term disability or even death.
- Recovery is prolonged and often associated with severe complications such as infections and organ failure.
2. Describe emergency management of patient with burns (4)
1️⃣ Ensure Scene Safety and Stop Burning Process
- It is very important to first ensure the safety of both the patient and rescuer before approaching the burn site.
- It is essential to remove the patient from the source of burn—fire, heat, chemicals, or electricity.
- It is required to stop the burning process by applying cool (not cold) running water for 10–20 minutes.
- It is necessary to remove tight clothing, belts, jewelry, and burned clothing that is not stuck to the skin.
- It is important not to apply ice or butter, as they can worsen tissue damage.
2️⃣ A – Airway Management
- It is crucial to assess the airway immediately, especially in burns involving the face, neck, or chest.
- It is essential to observe for hoarseness, stridor, singed nasal hairs, or carbon-stained sputum indicating inhalation injury.
- It is necessary to administer 100% humidified oxygen via a non-rebreather mask.
- If airway swelling is suspected, it is important to prepare for early intubation or tracheostomy.
3️⃣ B – Breathing Support
- It is essential to monitor respiratory rate, depth, chest expansion, and oxygen saturation continuously.
- In case of inhalation injury or carbon monoxide poisoning, high-flow oxygen is mandatory.
- It is important to be alert for chest burns that restrict movement, which may require escharotomy.
4️⃣ C – Circulation and Fluid Replacement
- It is necessary to check peripheral pulses, capillary refill, and blood pressure to assess perfusion.
- It is essential to insert two large-bore IV cannulas in unburned areas.
- It is important to begin fluid resuscitation using the Parkland Formula :
👉 4 mL × body weight (kg) × % TBSA burned = total fluid in 24 hours
👉 Give half in first 8 hours, remaining in next 16 hours. - It is required to insert a Foley catheter to monitor hourly urine output (target: 0.5–1 mL/kg/hr).
5️⃣ D – Disability / Neurological Status
- It is necessary to assess the Glasgow Coma Scale (GCS) to detect altered mental status.
- It is important to monitor for hypoxia-induced confusion, drowsiness, or coma.
- If carbon monoxide poisoning is suspected, assess carboxyhemoglobin levels and provide oxygen therapy or consider hyperbaric oxygen.
6️⃣ E – Exposure and Estimation of Burn Severity
- It is essential to completely expose the patient to assess all injuries, while preventing hypothermia.
- It is necessary to cover the patient with clean, dry sheets to protect from infection and reduce heat loss.
- It is important to calculate Total Body Surface Area (TBSA) using Rule of Nines or Lund-Browder chart.
- It is important to assess depth of burns: superficial, partial thickness, or full thickness.
7️⃣ Pain Management
- It is necessary to administer intravenous analgesics (e.g., morphine) to manage severe pain.
- Oral pain medications are not suitable in early emergency phase due to delayed absorption.
- Continuous pain assessment is required throughout care.
8️⃣ Infection Prevention and Tetanus Prophylaxis
- It is essential to maintain strict aseptic technique during all wound care and IV insertions.
- It is necessary to administer tetanus toxoid injection if immunization is not updated.
- Prophylactic antibiotics are not given unless signs of infection are present.
9️⃣ Emotional and Psychological Support
- It is necessary to provide emotional support to the patient, as burns cause pain, fear, and psychological trauma.
- It is helpful to communicate with the family, explain the condition and expected care steps.
- Referrals to counselors or psychiatric professionals may be initiated early if needed.
1️⃣0️⃣ Documentation and Transfer
- It is essential to document initial assessment, TBSA, vital signs, fluids administered, and interventions in detail.
- For severe burns, early referral or transfer to a burn unit or tertiary care center is important.
- Ensure safe transport, with continuous monitoring of airway, breathing, and circulation.
Q.6 Write short notes (any four) (20 marks)
1. Cosmetic surgery
Definition of Cosmetic Surgery
- Cosmetic surgery is defined as a medical procedure aimed at improving or modifying the aesthetic appearance of an individual through surgical or minimally invasive techniques.
- Cosmetic surgery is a specialized field of plastic surgery that focuses on improving physical appearance through surgical and non-surgical techniques. It is generally elective and performed to enhance self-image, body proportion, or rejuvenate aging features.
- Unlike reconstructive surgery, which focuses on repairing defects or injuries, cosmetic surgery is performed electively and is not medically necessary.
- It may involve reshaping facial or body structures to achieve harmony, balance, and enhanced self-confidence.
Objectives / Purpose of Cosmetic Surgery
- The primary objective of cosmetic surgery is to improve the aesthetic appearance of a person and boost self-esteem.
- It is performed to reshape normal body features, remove unwanted fat or skin, or restore youthfulness by reducing signs of aging.
- It also helps in improving quality of life for individuals who may suffer from low self-confidence due to their appearance.
- In some cases, cosmetic surgery may be used for post-bariatric contouring (after massive weight loss) or gender-affirming surgeries.
Types of cosmetic surgery
🔷 A. Facial Cosmetic Surgery
Rhinoplasty (Nose reshaping): It improves the shape, size, and structure of the nose to enhance facial harmony.
Blepharoplasty (Eyelid surgery): Performed to remove sagging skin or fat deposits from the upper/lower eyelids.
Rhytidectomy (Facelift): Tightens loose skin, smoothens wrinkles, and rejuvenates facial appearance.
Chin and cheek implants: Enhance bone structure for a more defined facial contour.
Botox and dermal fillers: Non-surgical options to reduce fine lines and restore facial volume.
🔷 B. Body Contouring Surgery
Liposuction: Removes localized fat deposits from areas like thighs, abdomen, arms, and neck.
Abdominoplasty (Tummy Tuck): Removes excess abdominal skin and tightens muscles for a flatter stomach.
Buttock augmentation/lift: Enhances shape and size of buttocks using fat grafting or implants.
Arm and thigh lift: Removes sagging skin and fat following weight loss or aging.
🔷 C. Breast Cosmetic Procedures
Breast augmentation: Insertion of silicone or saline implants to increase breast size and fullness.
Breast lift (Mastopexy): Lifts and reshapes sagging breasts without changing volume.
Breast reduction: Removes excess tissue for comfort and proportion, often also improving posture and reducing back pain.
🔷 D. Hair and Skin Cosmetic Procedures
Hair transplantation: Surgical technique that moves hair follicles from a donor site to bald areas.
Chemical peels: Use of chemical solutions to remove damaged outer skin layers for smoother skin.
Laser resurfacing: Targets scars, age spots, wrinkles, and skin irregularities using laser technology.
Indications for Cosmetic Surgery
- Desire to improve physical appearance, body symmetry, or confidence.
- Presence of aesthetic dissatisfaction with features such as nose shape, breast size, or abdominal bulge.
- Aging signs like wrinkles, sagging skin, or eyelid drooping.
- Post-weight loss excess skin or deformities.
- Gender-affirming procedures for transgender individuals.
- Career or personal requirements (e.g., modeling, acting) where appearance plays a role.
Risks and Complications
- Like any surgical procedure, cosmetic surgery carries inherent risks which include:
- Infection at the incision site, leading to delayed healing.
- Hematoma or seroma formation, causing swelling and fluid accumulation.
- Scarring or keloid formation depending on healing tendencies.
- Nerve damage leading to temporary or permanent numbness or muscle weakness.
- Unsatisfactory results, possibly requiring revision surgery.
- Anesthesia complications, such as respiratory distress or allergic reactions.
- Emotional or psychological dissatisfaction, especially in unrealistic expectations.
Nursing Responsibilities in Cosmetic Surgery
Nurses play a crucial role in ensuring the safety, well-being, emotional comfort, and recovery of patients undergoing cosmetic surgery, both before and after the procedure.
✅ 1. Preoperative Nursing Responsibilities
- The nurse must collect a complete health history, including previous surgeries, allergies, current medications, past illnesses, and psychosocial background.
- She should assess the patient’s mental readiness and ensure they have realistic expectations regarding the results of the surgery.
- The nurse explains the purpose, steps, risks, recovery process, and costs of the cosmetic procedure in a clear, honest, and respectful manner.
- She ensures that informed consent is obtained, signed, and witnessed after the patient fully understands the procedure.
- The nurse performs preoperative investigations, including blood tests, ECG, chest X-ray, and any other ordered evaluations.
- She prepares the patient physically, including fasting instructions (NPO status), shaving or cleaning the surgical site, and administering prescribed premedications.
- She helps reduce preoperative anxiety by offering reassurance, answering questions, and supporting the patient’s emotional needs.
- The nurse verifies that the correct patient, correct site, and correct procedure are confirmed before transferring to the operation theater.
✅ 2. Intraoperative Nursing Responsibilities
- The nurse assists in maintaining a sterile environment in the operating room by ensuring all aseptic protocols are followed.
- She prepares and arranges sterile instruments, sutures, and dressings according to the type of cosmetic surgery planned.
- The nurse assists the surgeon by handing instruments and managing surgical equipment during the procedure.
- She continuously monitors the patient’s vital signs (BP, pulse, temperature, SpO₂) during surgery.
- The nurse ensures the patient is in a safe and appropriate surgical position, especially in surgeries involving the face or body contouring.
- She records intraoperative events, estimated blood loss, fluid administration, and anesthesia monitoring.
- The nurse ensures accurate sponge, instrument, and needle counts before wound closure.
✅ 3. Postoperative Nursing Responsibilities
- The nurse monitors vital signs closely in the immediate postoperative period and checks for any signs of complications like bleeding, hypotension, or hypoxia.
- She assesses the surgical wound site for bleeding, swelling, hematoma, infection, or poor healing and applies sterile dressings as per protocol.
- The nurse provides pain management through prescribed analgesics and non-pharmacologic methods such as ice packs or positioning.
- She educates the patient about postoperative self-care, including wound care, scar management, activity restrictions, and when to seek medical help.
- She helps the patient with early ambulation, depending on the surgery, to prevent complications such as deep vein thrombosis (DVT).
- The nurse monitors for psychological reactions such as emotional distress, disappointment, or body image concerns post-surgery.
- She reinforces the importance of follow-up visits and adherence to instructions regarding medication, rest, and hygiene.
- The nurse documents all nursing interventions, vital signs, dressing changes, medication administration, and patient responses in the nursing notes.
✅ 4. Emotional and Psychological Responsibilities
- The nurse provides emotional support before and after surgery, especially in patients undergoing visible facial or body changes.
- She ensures that the patient does not have unrealistic expectations and understands that healing and final results take time.
- The nurse may need to recognize signs of body dysmorphic disorder (BDD) and refer to counseling if needed.
- She promotes positive reinforcement and body image by reassuring the patient and celebrating recovery milestones.
✅ 5. Legal and Ethical Responsibilities
- The nurse ensures that all legal documents, including consent forms and pre-anesthetic checklists, are properly filled out.
- She must maintain confidentiality and privacy, especially in procedures involving sensitive areas.
- The nurse acts as a patient advocate, ensuring their rights, dignity, and autonomy are respected.
- She should report any ethical concerns, such as coercion or inadequate informed consent, to the healthcare team.
2. Hodgkins lymphoma
Definition of Hodgkin’s Lymphoma
- It is a malignant cancer of the lymphatic system, characterized by the presence of Reed–Sternberg cells (large abnormal B lymphocytes) in lymph nodes.
- It typically begins in a single lymph node group, most commonly in the cervical or mediastinal area, and spreads in an orderly fashion.
- It is a potentially curable form of lymphoma, especially when detected early and treated with chemotherapy and/or radiation therapy.
Types of Hodgkin’s Lymphoma
1️⃣ Nodular Sclerosis Hodgkin’s Lymphoma
- It is the most common subtype, especially among young adults and females.
- It shows fibrous bands in lymph nodes and lacunar-type Reed–Sternberg cells.
- It often involves mediastinal lymph nodes.
2️⃣ Mixed Cellularity Hodgkin’s Lymphoma
- It is commonly seen in older adults and those with HIV infection.
- It contains many Reed–Sternberg cells mixed with various inflammatory cells.
- It frequently presents with advanced-stage disease.
3️⃣ Lymphocyte-Rich Hodgkin’s Lymphoma
- It has many normal lymphocytes and few Reed–Sternberg cells.
- It has a favorable prognosis and is often diagnosed at an early stage.
4️⃣ Lymphocyte-Depleted Hodgkin’s Lymphoma
- It is a rare, aggressive form, seen in elderly or immunocompromised patients.
- It has few lymphocytes, but many abnormal cells, and often presents with advanced disease.
5️⃣ Nodular Lymphocyte Predominant Hodgkin Lymphoma (NLPHL)
- It is a distinct subtype, with “popcorn cells” instead of classic Reed–Sternberg cells.
- It usually involves peripheral lymph nodes, and has an indolent course, but may recur.
Etiology
- Epstein-Barr virus (EBV) infection
- Genetic predisposition/family history
- Immunosuppression (e.g., HIV/AIDS)
- Autoimmune disorders
- Prior radiation or chemotherapy
- Male gender (more common in males)
- Exposure to certain chemicals (e.g., pesticides)
Pathophysiology of Hodgkin’s Lymphoma
1️⃣ Origin in Lymph Node B-Cells
It arises from abnormal B lymphocytes in the germinal center of lymph nodes.
2️⃣ Formation of Reed–Sternberg Cells
It is the presence of binucleated or multinucleated giant cells, which is the hallmark of diagnosis.
3️⃣ Immune Cell Infiltration
It is the surrounding inflammatory cells (lymphocytes, eosinophils, plasma cells) that form the tumor mass along with Reed–Sternberg cells.
4️⃣ Lymphatic Spread
It spreads in a contiguous manner from one lymph node region to adjacent nodes (e.g., from neck to chest to abdomen).
5️⃣ Systemic Involvement in Advanced Stage
It may involve spleen, liver, bone marrow, and lungs, leading to constitutional symptoms (B symptoms) like fever, night sweats, and weight loss.
Clinical Manifestations
- Painless lymph node swelling (usually neck)
- Persistent fatigue
- Unexplained weight loss
- Night sweats
- Fever (Pel-Ebstein fever)
- Pruritus (itching)
- Alcohol-induced lymph node pain
- Hepatosplenomegaly (advanced cases)
Diagnostic Evaluation
- History collection
- Physical examination
- Lymph node biopsy (Reed–Sternberg cells)
- Complete blood count (CBC)
- ESR, LDH levels (for inflammation, tumor activity)
- Chest X-ray and CT scan
- PET scan (for staging and spread)
- Bone marrow biopsy (in late-stage cases)
Management
1️⃣ Chemotherapy (Main Treatment Modality)
- It is based on ABVD regimen – Adriamycin (Doxorubicin), Bleomycin, Vinblastine, Dacarbazine.
- It is given in cycles depending on disease stage and patient response.
- Other regimens include BEACOPP for advanced-stage or relapsed disease.
2️⃣ Radiation Therapy
- It is often combined with chemotherapy in early-stage disease to target affected lymph nodes.
- It is also used as palliative care in bulky or nonresponsive masses.
- Side effects include fatigue, skin changes, and risk of secondary malignancies.
3️⃣ Targeted Therapy and Immunotherapy
- It includes Brentuximab vedotin (anti-CD30 monoclonal antibody) for relapsed Hodgkin’s lymphoma.
- Checkpoint inhibitors like Nivolumab and Pembrolizumab are used in refractory cases.
4️⃣ Hematopoietic Stem Cell Transplant (HSCT)
- It is considered in relapsed or refractory Hodgkin’s lymphoma, after salvage chemotherapy.
- Autologous transplant (self-donor) is more common than allogeneic (donor).
5️⃣ Supportive Therapies
- It includes growth factors (G-CSF) to prevent neutropenia, antiemetics for nausea, and analgesics.
- Regular nutritional support, hydration, and infection prevention are critical during treatment.
Nursing Management
1️⃣ Assessment and Monitoring
- It is important to assess location and size of lymph nodes, B symptoms, and fatigue level.
- It is necessary to monitor CBC, liver and kidney functions, and treatment side effects.
- It is essential to observe for signs of infection, especially during neutropenic phases.
2️⃣ Medication and Chemotherapy Care
- It is the nurse’s role to administer chemotherapy safely, using central lines when appropriate.
- It is important to monitor for drug toxicities (e.g., Bleomycin – pulmonary, Adriamycin – cardiac).
- It is necessary to give pre-medications to prevent nausea, allergic reactions, or infusion reactions.
3️⃣ Infection Prevention
- It is critical to maintain neutropenic precautions, such as hand hygiene, mask use, and avoiding raw food or flowers.
- It is essential to educate the patient to report fever, sore throat, or unusual bleeding immediately.
- It is advisable to avoid crowded places and limit visitors during low WBC periods.
4️⃣ Nutrition and Hydration
- It is necessary to offer high-protein, high-calorie diets, especially during weight loss phases.
- It is important to encourage oral fluids to prevent dehydration and renal complications.
- It is helpful to manage nausea and mucositis with diet modifications and mouth care.
5️⃣ Psychosocial and Emotional Support
- It is important to address body image issues (e.g., hair loss) and emotional distress related to cancer diagnosis.
- It is the nurse’s duty to provide counseling, spiritual support, and refer to cancer support groups.
- It is essential to involve the family in care planning and decision-making.
6️⃣ Health Education and Follow-Up
- It is important to teach about treatment adherence, managing side effects, and signs of relapse.
- It is necessary to emphasize the importance of regular follow-up and cancer screenings.
- It is advised to educate about fertility preservation options prior to chemotherapy in young patients.
3. Role of nurse in disaster management
A nurse plays a multidimensional role during all four phases of disaster management: preparedness, response, recovery, and mitigation. Nurses are the backbone of healthcare delivery in emergencies, offering clinical care, emotional support, and leadership to individuals and communities affected by disasters.
1. Role of Nurse in Disaster Preparedness Phase
- This is the pre-disaster phase where planning, training, and organization take place to reduce the impact of the disaster.
- It is the nurse’s responsibility to actively participate in hospital disaster planning committees and contribute knowledge toward making realistic and effective response strategies.
- The nurse should attend regular disaster drills and mock codes, ensuring familiarity with evacuation routes, emergency procedures, and disaster protocols.
- The nurse must educate patients, families, and communities about disaster types common to their region (e.g., earthquakes, floods, fire) and how to respond to them.
- The nurse is responsible for preparing personal and institutional emergency kits, including first aid supplies, medications, sterile dressings, gloves, IV fluids, and emergency contact lists.
- The nurse collaborates with other healthcare professionals and local authorities to assess community risks and vulnerabilities and develop action plans.
- It is also vital for the nurse to assist in creating communication flowcharts, so everyone knows whom to contact and what to do during emergencies.
- The nurse may lead public education campaigns on hygiene, disease prevention, and personal safety during disasters.
2. Role of Nurse in Disaster Response Phase
- This phase occurs during or immediately after the disaster, where the focus is on saving lives, preventing complications, and minimizing injuries.
- It is the nurse’s immediate responsibility to perform triage, which involves sorting patients based on injury severity using color-coded tags (e.g., red for urgent, yellow for delayed).
- The nurse provides life-saving emergency care, including controlling hemorrhage, managing airway, performing CPR, administering IV fluids, and stabilizing fractures.
- The nurse assists in evacuation procedures, ensuring that critically ill patients are safely transported to emergency shelters or hospitals.
- The nurse should maintain infection control measures in temporary shelters or field hospitals by ensuring proper waste disposal, hand hygiene, and use of PPE.
- The nurse maintains accurate records of victims treated, including personal details, injuries, treatments provided, and referrals.
- It is the nurse’s duty to communicate with relatives, provide updates on victim status, and offer emotional reassurance.
- In mass casualty incidents, the nurse also coordinates with ambulance services, disaster relief workers, and military personnel to streamline care delivery.
3. Role of Nurse in Disaster Recovery Phase
- This phase involves returning the affected individuals and communities back to normal life and rebuilding healthcare services.
- The nurse assists in wound care, rehabilitation, follow-up of chronic conditions, and psychological counseling for trauma victims.
- It is the nurse’s duty to identify long-term care needs, such as orthopedic rehabilitation, prosthetics for amputees, or continued treatment for burns.
- The nurse provides grief counseling and emotional support for individuals who lost loved ones, homes, or jobs.
- Nurses help in restoring healthcare infrastructure, such as setting up mobile health units or reopening damaged clinics.
- The nurse participates in health assessments and surveillance, identifying outbreaks of communicable diseases post-disaster (e.g., diarrhea, malaria, leptospirosis).
- It is the nurse’s role to conduct home visits to check on elderly, disabled, or pregnant women affected by the disaster.
- The nurse assists in government relief work, such as filling forms for compensation, housing, or ration supply.
4. Role of Nurse in Mitigation Phase
- Mitigation involves reducing the long-term risk and impact of future disasters.
- The nurse works with public health teams to educate the community about preventive actions, like securing heavy furniture in earthquake-prone zones or using mosquito nets to prevent vector-borne diseases.
- It is the nurse’s responsibility to improve community resilience by encouraging regular drills, early warning alerts, and safe construction practices.
- Nurses may engage in health mapping and environmental risk assessments to identify high-risk zones and vulnerable populations.
- The nurse provides counseling on stress management and trauma recovery, helping communities build psychological strength.
- Nurses help evaluate existing disaster plans, suggest improvements, and participate in research to identify gaps in disaster response.
5. Ethical and Professional Role of Nurse in Disasters
- It is essential that nurses practice non-discriminatory care, giving equal attention to all affected individuals regardless of age, gender, caste, or financial status.
- Nurses must maintain patient confidentiality, even in chaotic environments like emergency shelters or open field hospitals.
- The nurse should demonstrate calm, leadership behavior, helping to reduce panic and maintain order.
- The nurse advocates for vulnerable populations like children, disabled persons, pregnant women, and elderly who are often overlooked during mass relief efforts.
- It is the nurse’s ethical duty to self-monitor for fatigue or burnout and seek help if needed, to ensure optimal care delivery.
6. Communication & Coordination Role
- Nurses should maintain clear, timely, and accurate communication with physicians, disaster teams, NGOs, and local authorities.
- They may serve as a liaison between victims and rescue agencies, helping victims understand available services.
- Nurses must report outbreaks or deaths to public health authorities immediately to activate containment measures.
- They are often responsible for collaborating with media teams, when assigned, to deliver public health messages or announcements.
7. Documentation and Evaluation Role
- The nurse must record all medical care provided, resources used, number of people assisted, and any referrals made.
- Documentation helps in financial audits, legal accountability, and future disaster policy formulation.
- Nurses should assist in post-disaster evaluation reports, offering suggestions for what worked well and what needs improvement.
- These reports contribute to national disaster database systems, enhancing preparedness for future events.
4. Glaucoma
Definition of Glaucoma
- It is a chronic progressive optic neuropathy in which increased intraocular pressure (IOP) damages the optic nerve, leading to irreversible vision loss.
- It is called the “silent thief of sight”, because most types of glaucoma do not show symptoms until significant vision is lost.
- It primarily affects the elderly, but may also occur in infants or younger adults.
Types of Glaucoma
1️⃣ Primary Open-Angle Glaucoma (POAG)
- It is the most common type, in which aqueous humor outflow through the trabecular meshwork is reduced, leading to gradual IOP rise.
- It is painless and asymptomatic in early stages, often detected during routine eye exams.
- It causes gradual loss of peripheral vision, progressing to tunnel vision.
2️⃣ Primary Angle-Closure Glaucoma (PACG)
- It occurs when the iris bulges forward, narrowing or blocking the drainage angle, resulting in sudden rise in IOP.
- It presents with sudden eye pain, headache, nausea, and blurred vision with halos.
- It is considered a medical emergency.
3️⃣ Normal-Tension Glaucoma
- It is a form where the optic nerve is damaged despite normal IOP levels.
- It is thought to be related to reduced blood flow to the optic nerve.
- It may be seen in people with migraines or low blood pressure.
4️⃣ Congenital Glaucoma
- It is present at birth due to developmental anomalies in the eye’s drainage system.
- It manifests as enlarged eyes, excessive tearing, and light sensitivity in infants.
- It requires early surgical correction to prevent blindness.
5️⃣ Secondary Glaucoma
- It is caused by another eye condition such as uveitis, trauma, tumors, or prolonged steroid use.
- It may be open-angle or angle-closure, depending on the underlying pathology.
Etiology
- Increased intraocular pressure (IOP)
- Blocked aqueous humor drainage
- Family history of glaucoma
- Aging (above 40 years)
- Diabetes and hypertension
- Eye trauma or surgery
- Long-term corticosteroid use
- Congenital eye malformations
Pathophysiology of Glaucoma
1️⃣ Impaired Aqueous Humor Drainage
It is due to blockage or resistance in the trabecular meshwork or angle of anterior chamber, reducing aqueous outflow.
2️⃣ Rise in Intraocular Pressure (IOP)
It causes a gradual or sudden increase in pressure within the eye.
3️⃣ Compression of Optic Nerve Fibers
It is the high IOP that compresses the retinal ganglion cells and optic nerve, disrupting visual transmission.
4️⃣ Optic Nerve Ischemia and Degeneration
It leads to loss of blood supply, resulting in progressive optic nerve damage.
5️⃣ Irreversible Vision Loss
It begins with peripheral field defects, and in late stages, central vision may be lost, leading to blindness.
Clinical Manifestations
Open-Angle Glaucoma :
- Gradual peripheral vision loss
- No pain
- Poor night vision
- Tunnel vision (late stage)
Angle-Closure Glaucoma :
- Severe eye pain
- Redness and blurred vision
- Halos around lights
- Nausea and vomiting
- Sudden vision loss
Diagnostic Evaluation
- History collection
- Physical examination
- Tonometry (measures IOP)
- Ophthalmoscopy (optic disc evaluation)
- Visual field testing (perimetry)
- Gonioscopy (angle inspection)
- Pachymetry (corneal thickness)
- OCT (optic nerve imaging)
Medical & Surgical Management
1️⃣ Eye Drops (First-line Treatment)
- It includes Prostaglandin analogs (e.g., Latanoprost) to increase aqueous outflow.
- Beta-blockers (e.g., Timolol) are used to reduce aqueous production.
- Carbonic anhydrase inhibitors (e.g., Dorzolamide) lower IOP by decreasing fluid formation.
- Alpha agonists (e.g., Brimonidine) do both – reduce production and increase drainage.
2️⃣ Systemic Medications
- It includes oral Acetazolamide for emergency IOP control, especially in acute angle-closure glaucoma.
- Hyperosmotic agents (e.g., Mannitol IV) are given to rapidly reduce IOP.
3️⃣ Laser Procedures
- Laser trabeculoplasty is used in open-angle glaucoma to improve fluid drainage.
- Laser iridotomy is performed in angle-closure glaucoma to create a new drainage path.
- It is outpatient, quick, and often performed before or instead of surgery.
4️⃣ Surgical Management
- Trabeculectomy involves creating a new channel for aqueous outflow under the conjunctiva.
- Glaucoma drainage implants (shunts) may be used in complex or secondary glaucoma.
- Cyclophotocoagulation is used to reduce aqueous production in severe, uncontrolled cases.
Nursing Management
1️⃣ Assessment and Monitoring
- It is essential to assess the patient’s visual acuity, intraocular pressure monitoring records, and history of glaucoma symptoms.
- It is important to monitor for eye pain, photophobia, colored halos, or signs of medication intolerance.
- It is necessary to assess the psychological impact of visual impairment, especially in elderly patients.
2️⃣ Medication Administration
- It is the nurse’s responsibility to administer prescribed eye drops with strict attention to aseptic technique.
- It is important to educate the patient on how to instill eye drops properly, including punctal occlusion technique to avoid systemic absorption.
- It is essential to explain that medications control but do not cure glaucoma, and must be continued lifelong.
3️⃣ Post-Procedure and Surgical Care
- It is necessary to observe for post-operative complications such as eye pain, redness, sudden loss of vision, or purulent discharge.
- It is important to instruct the patient to sleep with head elevated, wear protective eye shields, and avoid sleeping on the operated side.
- It is advised to avoid coughing, straining during bowel movements, and exposure to dust or water after eye surgery.
4️⃣ Patient Safety and Environmental Adjustments
- It is helpful to keep the patient’s environment clutter-free to prevent accidents due to peripheral vision loss.
- It is recommended to install bright lighting, high-contrast labels, and non-slip flooring at home.
- It is necessary to refer to occupational therapy if vision is significantly impaired.
5️⃣ Psychosocial Support
- It is the nurse’s role to offer emotional reassurance, especially for patients facing permanent vision loss or surgery.
- It is helpful to connect patients with support groups for low vision or glaucoma education forums.
- It is important to involve family members in medication scheduling and transport for follow-up visits.
6️⃣ Health Education
- It is essential to emphasize the importance of regular follow-up appointments and monitoring intraocular pressure (IOP).
- It is advisable to inform about the need for lifelong therapy even when there are no visible symptoms.
- It is important to advise high-risk individuals (diabetics, hypertensives, family history of glaucoma) to get screened annually.
- It is the nurse’s responsibility to explain that sudden severe eye pain, nausea, and blurred vision can be signs of acute angle-closure glaucoma, requiring immediate medical attention.
5. Otitis media
Definition of Otitis Media
- It is an inflammation or infection of the middle ear cavity, which is located between the tympanic membrane (eardrum) and the inner ear.
- It commonly occurs due to blockage of the Eustachian tube, resulting in fluid build-up and infection.
- It is most frequent in infants and young children, but it can affect adults as well.
- It can be acute, chronic, or with effusion (fluid without active infection).
Types of Otitis Media
1️⃣ Acute Otitis Media (AOM)
- It is a sudden onset middle ear infection, usually following an upper respiratory tract infection.
- It is characterized by ear pain, fever, and bulging of the tympanic membrane.
- It may include fluid and pus accumulation in the middle ear.
2️⃣ Otitis Media with Effusion (OME)
- It is the presence of fluid in the middle ear without signs of active infection.
- It often follows AOM or occurs with Eustachian tube dysfunction.
- It may lead to hearing loss or a sense of fullness in the ear.
3️⃣ Chronic Suppurative Otitis Media (CSOM)
- It is a long-term infection of the middle ear with persistent ear discharge (otorrhea) through a perforated tympanic membrane.
- It may result in hearing loss, and sometimes cholesteatoma formation (abnormal skin growth in the ear).
Etiology
- Bacterial infection (e.g., Streptococcus pneumoniae, Haemophilus influenzae)
- Viral respiratory infections
- Eustachian tube dysfunction
- Exposure to smoke/allergens
- Bottle feeding in supine position
- Immature immunity in children
- History of upper respiratory tract infection (URTI)
Pathophysiology of Otitis Media
1️⃣ Eustachian Tube Dysfunction
It is commonly due to inflammation or blockage from a respiratory infection or allergy, impairing ventilation of the middle ear.
2️⃣ Negative Pressure and Fluid Accumulation
It is from blocked drainage that fluid builds up in the middle ear cavity, creating a medium for microbial growth.
3️⃣ Microbial Invasion
It is the bacteria or viruses that enter from the nasopharynx into the middle ear, initiating inflammation.
4️⃣ Inflammation and Exudate Formation
It leads to mucosal swelling, pus formation, and pressure on the eardrum, causing pain and potential rupture.
5️⃣ Chronic Infection (If Untreated)
It results in perforation, persistent discharge, and may cause ossicle damage and hearing impairment.
Clinical Manifestations
- Ear pain (otalgia)
- Fever
- Hearing loss or fullness in ear
- Irritability (in children)
- Tugging/pulling at the ear
- Purulent ear discharge (if perforated)
- Tinnitus or vertigo (sometimes)
Diagnostic Evaluation
- History collection
- Physical examination
- Otoscopic examination
- Tympanometry
- Hearing tests (audiometry)
- Culture of ear discharge (if present)
- CBC (to detect infection)
Management
1️⃣ Antibiotic Therapy
- It is common to prescribe Amoxicillin (first-line) or Amoxicillin-Clavulanate in bacterial cases.
- It is essential to complete the full antibiotic course to prevent complications.
- Macrolides (e.g., Azithromycin) may be used in penicillin-allergic patients.
2️⃣ Analgesics and Antipyretics
- It is important to manage pain and fever using Paracetamol or Ibuprofen.
- It improves comfort and feeding in children.
3️⃣ Decongestants and Antihistamines
- It may be used to relieve nasal congestion and improve Eustachian tube function, especially in allergic cases.
4️⃣ Myringotomy (Surgical Drainage)
- It is a minor surgical procedure to create an opening in the tympanic membrane to drain fluid.
- It is often done when there is persistent effusion or hearing loss.
5️⃣ Tympanostomy Tube Insertion
- It is the placement of ventilation tubes into the ear to prevent fluid build-up and recurrence of infection.
- It is considered for recurrent otitis media or chronic effusion lasting over 3 months.
6️⃣ Treatment of Chronic Suppurative Otitis Media (CSOM)
- It may require aural toilet (cleaning of ear discharge), topical antibiotics, and surgery like tympanoplasty or mastoidectomy in complicated cases.
Nursing Management
1️⃣ Assessment
- It is necessary to monitor ear pain, discharge, and hearing ability.
- It is important to assess temperature, signs of systemic infection, and behavioral cues in children.
2️⃣ Medication Administration
- It is the nurse’s role to administer antibiotics, antipyretics, and ear drops as prescribed.
- It is important to ensure adherence to the full antibiotic course.
- It is essential to monitor for adverse effects or allergy to medications.
3️⃣ Ear Care and Hygiene
- It is advised to keep the ear dry, especially in CSOM or post-myringotomy cases.
- It is essential to teach safe ear cleaning — no cotton buds or objects inside the ear.
- It is helpful to gently clean external discharge with sterile cotton.
4️⃣ Supportive and Comfort Care
- It is useful to apply warm compresses to reduce pain.
- It is necessary to ensure the child gets adequate fluids, rest, and comfort.
- It is important to prevent exposure to smoke, allergens, and cold air.
5️⃣ Health Education
- It is crucial to teach parents about early recognition of symptoms and when to seek care.
- It is important to discourage bottle feeding in lying down position.
- It is advisable to complete vaccinations (e.g., pneumococcal, influenza) to prevent AOM.
- It is necessary to explain the importance of follow-up for recurrent or chronic cases.
