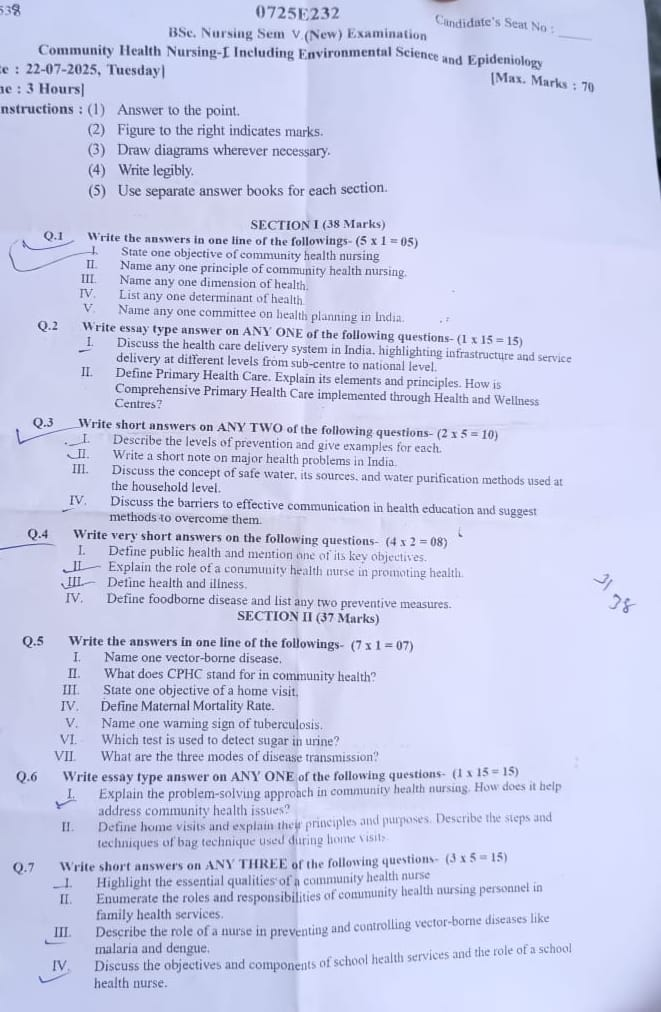
B.SC-COMMUNITY PAPER SOLUTION-22/07/2025 (G.U) NURSING SEM-V-PAPER SOLUTION NO.06
PAPER SOLUTION NO.06 – (22/07/2025 – G.U))
SECTION 1
Q.1 Write the answers in one line of the followings- (5 X1 = 5)
I.State one objective of community health
👉 To promote, protect, and maintain the health of the population by preventing diseases, prolonging life, and improving quality of life through organized efforts of society, health services, and individuals.
II.Name any one principle of community health nursing
👉 The principle of “Equitable Distribution of Health Services”, which means health services should be made available to all individuals in the community regardless of their socio-economic status, gender, age, or geographic location.
III.Name any one dimension of health
👉 Physical Dimension – It refers to the proper functioning of the body and its systems, maintaining normal body weight, good nutrition, regular exercise, and absence of disease or disability.
IV. List any one determinant of health
👉 Environmental Factors – It includes physical, chemical, biological, and socio-cultural surroundings such as clean air, safe water, proper sanitation, and safe housing, which directly affect an individual’s health.
V. Name any one committee on health planning in India.
👉 The Bhore Committee (1946) – It was the first major health planning committee in India, which laid the foundation for the public health system and recommended the integration of preventive and curative services.
Q.2 Write essay type answer on ANY ONE of the following questions- (1 X 15 = 15)
1.Discuss the health care delivery system in India, highlighting and service delivery at different levels from sub-centre to national level.
The Health Care Delivery System in India refers to the organized structure of services, personnel, institutions, and facilities established by the government and private sectors to deliver health care to the population. It aims to ensure availability, affordability, accessibility, acceptability, and quality health care to every individual.
India’s health care system is designed to provide universal, equitable, and need-based health care, especially for the rural, tribal, and underserved populations, through a three-tiered structure integrated with national health programs and public health policies.
🎯 OBJECTIVES OF HEALTH CARE DELIVERY SYSTEM IN INDIA
- ✅ It aims to provide preventive, promotive, curative, and rehabilitative health care services to all citizens without financial hardship.
- ✅ It is designed to reduce the burden of communicable and non-communicable diseases through early detection and timely treatment.
- ✅ It seeks to ensure maternal and child health, nutritional security, and reproductive health services in rural and urban areas.
- ✅ It promotes community participation and decentralization of health care services to local governance.
- ✅ It supports the implementation of national and international health goals, including Universal Health Coverage (UHC) and Sustainable Development Goals (SDGs).
🏥 STRUCTURE OF HEALTH CARE DELIVERY SYSTEM IN INDIA
India follows a three-tier model that includes Primary, Secondary, and Tertiary levels of care, each having a distinct role in service delivery.
🔹 1. SUB-CENTRE (SC)
Peripheral-level health unit – The first point of contact
📌 Staffing
- 1 Female Health Worker (ANM)
- 1 Male Health Worker (MPW-M)
- Under the supervision of Health Assistants at the PHC level.
📌 Population Coverage
- 5,000 people in plain areas
- 3,000 people in tribal/hilly/difficult areas
📌 Functions and Services Provided
- It provides maternal and child health (MCH) services, including ANC, PNC, and immunization.
- It carries out family welfare services like contraceptive distribution and motivation for sterilization.
- It conducts home visits, community-based nutrition education, and early childhood care.
- It helps in communicable disease surveillance and health promotion activities.
- It works on sanitation, safe water practices, and health education.
- It acts as the link between the community and the higher-level health system.
🔹 2. PRIMARY HEALTH CENTRE (PHC)
First-level referral unit for sub-centres
📌 Staffing
- 1 Medical Officer
- 1 Staff Nurse
- Pharmacist, Lab Technician, Health Assistants (Male/Female), and Support Staff
📌 Population Coverage
- 30,000 people in plains
- 20,000 people in tribal/hilly regions
📌 Functions and Services Provided
- It provides curative outpatient services, including minor surgeries and treatment of common ailments.
- It implements Reproductive and Child Health (RCH) programmes, including safe deliveries and MTP.
- It monitors and supervises the functioning of sub-centres under its jurisdiction.
- It undertakes epidemic control measures, like malaria and dengue control.
- It runs health awareness campaigns, national programs, and school health services.
- It is the first level for referrals from sub-centres, managing slightly more complex cases.
🔹 3. COMMUNITY HEALTH CENTRE (CHC)
Secondary-level health care – Acts as a First Referral Unit (FRU)
📌 Staffing
- 4 Specialists: Surgeon, Physician, Obstetrician/Gynaecologist, and Paediatrician
- Nurses, Pharmacists, Radiographers, Lab Technicians, Admin staff
📌 Population Coverage
- 1.2 lakh in plains
- 80,000 in hilly/tribal areas
📌 Functions and Services Provided
- It provides specialist consultation and basic surgeries (e.g., caesarean, hernia).
- It manages referrals from PHCs and provides inpatient and emergency services.
- It includes lab diagnostics, X-rays, blood storage units, and ambulance services.
- It handles emergency obstetric and neonatal care (EmONC).
- It plays a supervisory role in national programmes and public health monitoring.
🔹 4. DISTRICT HOSPITAL (DH)
Key Secondary and Referral Care Centre
📌 Staffing and Infrastructure
- Super-specialists, General Physicians, Surgeons, Gynaecologists, Orthopaedics, Anaesthetists
- Nursing staff, paramedical staff, technicians, and administrative team
- 100+ beds with ICUs, Operation Theatres, Blood Banks, and Diagnostic Services
📌 Functions and Services Provided
- It acts as a referral hospital for all CHCs and PHCs in the district.
- It provides specialised treatment for medical, surgical, paediatric, psychiatric, and trauma cases.
- It offers 24×7 emergency care, intensive care, and obstetric management.
- It supports district-level disease surveillance and epidemic control measures.
- It also serves as a teaching and training site for nurses, ANMs, and other health professionals.
🔹 5. TERTIARY HEALTH CARE CENTRES (REGIONAL/NATIONAL LEVEL)
Highest Level of Health Care Delivery
📌 Examples
- AIIMS (All India Institute of Medical Sciences)
- PGIMER (Post Graduate Institute of Medical Education and Research)
- JIPMER (Jawaharlal Institute of Postgraduate Medical Education and Research)
- State Medical Colleges
📌 Functions and Services Provided
- Provides super-specialty services like cardiology, nephrology, oncology, neurosurgery, plastic surgery, etc.
- Offers advanced diagnostics, critical care, and transplant services.
- Functions as a centre for medical education, research, and innovation.
- Supports national policy development, programme evaluation, and health technology assessment.
- Acts as apex referral centres for complex or rare diseases.
🏛️ Role of Government in Health Care Delivery
🔸 Central Government
- Formulates national health policies, guidelines, and budget allocations.
- Runs vertical national health programmes (e.g., National TB Elimination Programme, NACP, RMNCH+A).
- Supervises apex institutions and provides technical assistance.
🔸 State Government
- Implements health programmes and manages human resources, state hospitals, and logistics.
- Handles district and block-level institutions, hiring of medical staff, and budget utilization.
🏥 Private Sector and Voluntary Organizations
- Includes clinics, nursing homes, diagnostic centres, and corporate hospitals.
- Plays a major role in urban and tertiary health care services.
- NGOs support health education, community outreach, rehabilitation, and program implementation.
- Many PPP (Public-Private Partnership) models have emerged under NHM for diagnostics, ambulance services, etc.
🔗 Linkages and Referral System
- Sub-centres refer cases to PHCs
- PHCs refer to CHCs
- CHCs refer to District Hospitals
- District Hospitals refer to Medical Colleges/Tertiary Centres
👉 This structured referral mechanism ensures continuity of care, appropriate use of resources, and patient safety.
📌 Challenges in the Health Care Delivery System
- Inadequate infrastructure and shortage of trained human resources in rural areas
- Poor accessibility in tribal and remote areas
- Underutilization of primary and secondary care centres
- Unequal distribution of health resources between urban and rural populations
- High out-of-pocket expenditure in private care
II. Define Primary Health Care. Explain its elements and principles. How is Comprehensive Primary Health Care implemented through Health and Wellness Centres?
👉 As per the Alma-Ata Declaration (1978) by WHO and UNICEF:
“Primary Health Care is essential health care made universally accessible to individuals and families in the community by means acceptable to them, through their full participation and at a cost that the community and the country can afford to maintain.”
🔹 It emphasizes universal access, community involvement, equity, and inter-sectoral coordination.
🔹 It is not just the first level of care, but a philosophy of health care delivery that emphasizes health promotion, disease prevention, and addressing the determinants of health.
🟠 II. ELEMENTS OF PRIMARY HEALTH CARE
As per WHO, there are eight essential components which together define the scope of PHC:
1️⃣ Health Education on Prevailing Health Problems and Prevention Methods
- Educating people about personal hygiene, disease prevention, and healthy practices.
- Mass campaigns, school health education, and folk media help in awareness.
- Focus on behavioral change communication (BCC) for health-seeking behavior.
2️⃣ Promotion of Food Supply and Proper Nutrition
- Nutrition education for mothers, children, adolescents, and elderly.
- Promotion of kitchen gardens, community nutrition programs, and use of locally available food.
- Linkages with ICDS, POSHAN Abhiyan, and mid-day meal schemes.
3️⃣ Adequate Supply of Safe Water and Basic Sanitation
- Access to safe drinking water, clean toilets, solid waste management.
- Prevention of waterborne and fecal-oral diseases like cholera, hepatitis A, diarrhea.
- Supported by schemes like Swachh Bharat Abhiyan.
4️⃣ Maternal and Child Health Including Family Planning
- Provision of ANC, PNC, safe delivery services, immunization, and growth monitoring.
- Family planning services include counseling, spacing methods, and sterilization.
- Focus on reducing maternal and infant mortality.
5️⃣ Immunization Against Major Infectious Diseases
- Immunization services under Universal Immunization Programme (UIP).
- Includes vaccines for polio, measles, DPT, Hepatitis B, rotavirus, COVID-19, etc.
- Special drives like Mission Indradhanush improve vaccine coverage.
6️⃣ Prevention and Control of Locally Endemic Diseases
- Local diseases like malaria, leprosy, TB, filariasis, and dengue are targeted.
- Activities include vector control, health surveillance, and early treatment.
7️⃣ Appropriate Treatment for Common Diseases and Injuries
- Provides basic medical care for fever, diarrhea, wounds, RTIs, skin infections, etc.
- Uses Essential Drug Lists and Standard Treatment Guidelines.
- Referrals are made to higher facilities for complications.
8️⃣ Provision of Essential Medicines
- Stocking of essential and generic drugs like antibiotics, antipyretics, antihypertensives.
- Ensures uninterrupted access to life-saving medications at no or low cost.
- Follows the Jan Aushadhi scheme principles and national drug policy.
🔵 III. PRINCIPLES OF PRIMARY HEALTH CARE
1️⃣ Equitable Distribution
- All individuals, regardless of economic status, caste, gender, or geography, should receive the same quality of care.
- PHC must reach the rural, tribal, slum, and underdeveloped areas with equal effort as urban areas.
2️⃣ Community Participation
- Health services must involve the community as active partners, not passive recipients.
- Mechanisms include Village Health Sanitation and Nutrition Committees (VHSNCs) and ASHA workers.
- Participation improves ownership, sustainability, and responsiveness.
3️⃣ Inter-sectoral Coordination
- Health outcomes are influenced by sectors like education, food, water supply, sanitation, housing, and employment.
- PHC must work with Panchayati Raj Institutions, Women & Child Development, Rural Development, etc.
4️⃣ Appropriate Technology
- Use of scientific, simple, cost-effective, and culturally acceptable technology suited to local needs.
- Examples: ORS, zinc tablets, digital hemoglobin meters, mobile health vans, and telemedicine.
🟣 IV. IMPLEMENTATION OF COMPREHENSIVE PRIMARY HEALTH CARE (CPHC) THROUGH HEALTH AND WELLNESS CENTRES (HWCs)
🔷 Background
Under the Ayushman Bharat Mission (2018), the Government of India launched Health and Wellness Centres (HWCs) to strengthen PHC.
- Goal: To transform existing Sub-Centres and Primary Health Centres into functional HWCs delivering CPHC.
- Target: Operationalize 1.5 lakh HWCs by expanding services and workforce.
🧑⚕️ V. KEY FEATURES OF HEALTH AND WELLNESS CENTRES
1️⃣ Expanded Package of 12 Comprehensive Services
- Maternal and child health
- Family planning and reproductive health
- Adolescent health care
- Communicable diseases
- Non-communicable diseases (NCDs)
- Elderly care
- Mental health
- Emergency care
- Oral health
- Eye and ENT care
- Palliative care
- Health promotion and wellness activities
2️⃣ Team-Based Care Model
Each HWC is staffed with:
- Community Health Officer (CHO) – a trained nurse or AYUSH professional
- ANM/MPW (M/F)
- ASHA workers
- Pharmacist/Lab technician where applicable
This ensures people-centered, continuous care, and community linkage.
3️⃣ Wellness and Health Promotion Focus
- Promotion of Yoga, meditation, lifestyle modification, nutrition education.
- Conducting weekly wellness sessions, health days, school programs.
- Special attention to mental well-being and positive health behavior.
4️⃣ Digital Health and Telemedicine
- Integration with Ayushman Bharat Digital Mission (ABDM).
- Teleconsultations with doctors at PHCs and higher levels.
- Electronic health records, mobile apps for patient registration and tracking.
5️⃣ Free Essential Drugs and Diagnostics
- HWCs supply free medicines for NCDs, maternal care, pain relief, and infections.
- Point-of-care diagnostics for blood sugar, hemoglobin, pregnancy tests, urine tests, BP monitoring, etc.
📊 VI. IMPACT OF HWCs AND PHC REFORMS IN INDIA
✅ Over 1.6 lakh HWCs are operational as of 2025.
✅ More than 50 crore people have access to CPHC.
✅ ASHA workers and CHOs have improved screening for hypertension, diabetes, cancer.
✅ Improved outreach to tribal and underserved areas.
✅ Reduced patient load on secondary and tertiary hospitals by treating early at the primary level.
Primary Health Care is the foundation of a resilient health system and the gateway to Universal Health Coverage. With its holistic approach, it not only cures illness but also promotes wellness, equity, and community empowerment. The introduction of Health and Wellness Centres under Ayushman Bharat has been a milestone reform in India’s health sector, enabling the shift from selective to comprehensive care.
To ensure long-term success, there must be continued focus on:
- Strengthening infrastructure and workforce
- Sustained funding and supply chain
- Digital inclusion and health literacy
- Effective monitoring and evaluation
Q.3 Write short answers on ANY TWO of the following questions (2 X 5 = 10)
I.Describe the levels of prevention and give examples for each
Prevention in public health refers to actions aimed at reducing the risk of disease, minimizing its impact, or delaying its progression. The concept of levels of prevention was introduced by Leavell and Clark (1965) and is widely used in community health nursing and epidemiology.
There are four recognized levels of prevention:
- Primordial Prevention
- Primary Prevention
- Secondary Prevention
- Tertiary Prevention
Each level targets a specific stage in the natural history of disease – from preventing the risk itself to reducing disability and restoring function.
🔵 1. PRIMORDIAL PREVENTION
🧾 Definition:
It refers to preventing the emergence of risk factors in a population before they appear.
🧾 Focus:
- Targets social, economic, environmental, and behavioral conditions leading to risk factor development.
- Often applied at policy or societal level.
🧾 Examples:
- Promotion of healthy lifestyle in children to prevent future obesity and diabetes.
- Implementation of national policies to reduce air pollution.
- Banning sale of tobacco to minors.
- Discouraging sedentary behavior through active school programs.
🟠 2. PRIMARY PREVENTION
🧾 Definition:
It aims to prevent the occurrence of disease or injury by controlling risk factors or enhancing resistance.
🧾 Focus:
- Applied before the onset of disease.
- Involves health promotion and specific protection.
🧾 Examples:
✳️ Health Promotion:
- Health education on balanced diet, exercise, and personal hygiene.
- Encouraging breastfeeding and immunization.
- Alcohol and smoking cessation programs.
✳️ Specific Protection:
- Vaccination programs (e.g., BCG, DPT, Hepatitis B).
- Use of mosquito nets or repellents to prevent malaria.
- Fluoridation of water to prevent dental caries.
- Wearing helmets and seat belts to prevent injuries.
🟡 3. SECONDARY PREVENTION
🧾 Definition:
It focuses on early detection and prompt treatment of disease to halt progression and prevent complications.
🧾 Focus:
- Disease has already occurred but is in early stage, often asymptomatic.
- Prevents development of severe or chronic conditions.
🧾 Examples:
- Screening programs:
- Pap smear for cervical cancer
- Mammography for breast cancer
- Blood pressure and blood sugar checks
- Early treatment of hypertension to prevent heart attack.
- Treating STIs early to prevent infertility.
- Isolation and treatment of tuberculosis patients.
🔴 4. TERTIARY PREVENTION
🧾 Definition:
It refers to limiting disability, restoring function, and rehabilitating individuals with chronic or irreversible conditions.
🧾 Focus:
- Applied after disease has advanced, aims at minimizing suffering and maximizing potential.
- Focuses on rehabilitation, support, and improving quality of life.
🧾 Examples:
- Physiotherapy and speech therapy after a stroke.
- Dialysis for chronic kidney disease.
- Prosthetic rehabilitation after limb amputation.
- Counseling and vocational training for mentally challenged individuals.
- Use of insulin and diabetic foot care in diabetic patients to prevent complications.
II.Write a short note on major health problems in India
India is the most populous country in the world as of 2023, with a population of over 1.43 billion people. The country is experiencing a dual burden of disease – both communicable and non-communicable diseases are prevalent. This is further complicated by urbanization, poverty, environmental degradation, lack of awareness, and poor access to health care services in rural and remote areas.
🔹 According to the National Family Health Survey (NFHS-5, 2019–21) and recent data from MoHFW and WHO (2023–24), India’s major health issues are multifaceted and demand urgent public health action.
🔴 1. Communicable Diseases (Infectious Diseases)
📌 Current Data:
- Tuberculosis (TB):
– India accounts for 27% of global TB cases.
– As per India TB Report 2024, over 24 lakh cases were reported in 2023.
– Drug-resistant TB is an emerging challenge. - Vector-borne Diseases (Malaria, Dengue, Chikungunya):
– Dengue cases have increased with over 1.3 lakh cases in 2023, mostly in urban areas.
– Malaria cases have declined due to active surveillance but still persist in tribal and forested regions. - HIV/AIDS:
– Estimated 2.4 million people living with HIV in India.
– Prevalence rate is 0.21% among adults (NACO, 2023). - Diarrheal Diseases:
– Major cause of morbidity and mortality in children under 5.
– Linked to unsafe drinking water, poor sanitation, and low ORS usage. - Leprosy:
– India reported over 75,000 new leprosy cases in 2023 (highest globally), especially in Bihar, Chhattisgarh, and Odisha.
🟠 2. Non-Communicable Diseases (NCDs)
👉 India is undergoing an epidemiological transition, with NCDs now accounting for 66% of all deaths (ICMR, 2024).
📌 Key NCDs and Stats:
- Hypertension:
– Around 24% of men and 21% of women (NFHS-5) have elevated BP.
– Often undiagnosed in rural areas. - Diabetes Mellitus:
– Over 101 million Indians have diabetes (ICMR–INDIAB, 2023).
– 77 million more are prediabetic. - Cancer:
– 14 lakh new cases diagnosed annually.
– Most common: oral cancer (in men), breast and cervical cancer (in women). - Mental Health Disorders:
– Over 7.5% of the population suffers from mental illnesses.
– Depression, anxiety, substance abuse, and suicide are major issues, especially among youth.
🟡 3. Nutritional Problems
India faces a dual nutritional burden: undernutrition in children and overnutrition in adults.
📌 NFHS-5 Data:
- Child undernutrition:
– 35.5% children under 5 are stunted.
– 19.3% are wasted, and 32.1% underweight. - Anemia:
– Found in 57% of women (15–49 yrs) and 67% of children (6–59 months). - Obesity:
– Rising in urban areas: 24% of women and 22% of men are overweight or obese. - Vitamin and mineral deficiencies:
– Vitamin A, Iodine, Zinc, and Iron deficiencies remain common in rural children and pregnant women.
🔵 4. Maternal and Child Health Problems
Despite improvement, India still has significant challenges in maternal and child health.
📌 Current Indicators:
- Maternal Mortality Ratio (MMR):
– 97 per 100,000 live births (SRS 2023) – declining, but still high in states like Assam, UP, and MP. - Infant Mortality Rate (IMR):
– 28 per 1,000 live births (SRS 2023) – highest in rural and tribal regions. - Neonatal Mortality Rate (NMR):
– 20 per 1,000 live births - Low Birth Weight (LBW):
– 18% of all live births (NFHS-5)
📌 Issues:
- Poor ANC/PNC coverage in certain districts
- Institutional deliveries improving (88.6%) but still gaps in quality care
- Unmet need for family planning – 9.4% (NFHS-5)
🟣 5. Environmental and Occupational Health Problems
📌 Key Environmental Hazards:
- Air Pollution:
– WHO reports 10 of the world’s most polluted cities are in India.
– Linked to COPD, asthma, cardiac issues, and lung cancer. - Water Pollution and Sanitation:
– Only 70% of rural households have improved sanitation.
– Contaminated water leads to diarrhea, hepatitis A/E. - Occupational Diseases:
– Found in mining, factories, agriculture (e.g., silicosis, pesticide toxicity).
– Lack of protective equipment and awareness.
🟤 6. Population Explosion and Urbanization
📌 Current Data:
- India’s population (2024): Over 1.43 billion
- Urban population: 35.4% (Census Estimate)
- Slum population: Over 65 million, lacking basic health, water, and housing.
📌 Health Impact:
- Overcrowding, unemployment, and strain on health resources
- Rise in non-communicable and communicable diseases in urban slums
- Increase in lifestyle disorders and mental health conditions
✅ CONCLUSION
India faces multiple overlapping health challenges – from old infectious diseases to emerging lifestyle and environmental threats. While national programs like Ayushman Bharat, NHM, and POSHAN Abhiyan are improving access and coverage, sustained efforts are needed.
Health professionals, especially nurses, have a crucial role in:
- Educating communities
- Screening and early detection
- Preventing complications
- Promoting sanitation, nutrition, and safe practices
With community-based interventions, policy implementation, and technology integration, India can make significant progress toward achieving Universal Health Coverage and SDG Goal 3 – Good Health and Well-being.
III. Discuss the concept of safe water, its sources, and water purification methods used ar the household level.
Water is an essential natural resource for life, health, food, and sanitation. However, unsafe and contaminated water continues to be a leading cause of illness and death, especially in developing countries like India. According to WHO, over 2 billion people globally lack access to safe drinking water. Contaminated water leads to waterborne diseases like diarrhea, typhoid, cholera, and hepatitis, particularly affecting children under five.
Therefore, understanding the concept of safe water, its sources, and simple household-level purification methods is essential for improving community health and preventing disease outbreaks.
🔵 II. CONCEPT OF SAFE WATER
🧾 Definition of Safe Water
Safe water refers to water that is free from harmful physical, chemical, and biological contaminants, making it fit for human consumption and domestic use.
🧾 Key Characteristics of Safe Water:
- Microbiologically Safe – Free from disease-causing organisms (bacteria, viruses, parasites).
- Chemically Safe – No hazardous substances like arsenic, lead, fluoride, nitrates, or pesticides.
- Physically Acceptable – Clear, colorless, odorless, and tasteless.
- pH Level – Should be between 6.5 to 8.5, as per BIS standards.
- Turbidity – Should be below 5 NTU (Nephelometric Turbidity Units).
Unsafe water can transmit diseases such as cholera, dysentery, typhoid, polio, and hepatitis A/E, which collectively account for millions of preventable deaths each year.
🟠 III. SOURCES OF WATER
Water for human use comes from various natural and artificial sources, broadly classified into surface water, groundwater, and rainwater.
🔹 1. Surface Water Sources
These sources collect water on the surface of the Earth and are usually replenished by rainfall.
- Rivers and Streams
➤ Large flowing bodies of freshwater, used in cities and villages.
➤ Often polluted by sewage, industrial effluents, and agricultural runoff. - Lakes and Ponds
➤ Natural or man-made depressions that store water.
➤ Stagnant water may harbor algae, mosquitoes, and bacteria. - Reservoirs and Dams
➤ Constructed to store water from rivers for irrigation and drinking.
➤ Water is treated in filtration plants before supply.
🔹 2. Groundwater Sources
Water stored below the Earth’s surface in aquifers; usually cleaner than surface water but may have mineral contamination.
- Wells (Dug or Open)
➤ Shallow and vulnerable to contamination from pit latrines and surface runoff. - Tube Wells and Bore Wells
➤ Deep wells fitted with pumps to extract water from aquifers.
➤ Safer but may contain fluoride, arsenic, or iron depending on geography. - Springs
➤ Natural outlets where underground water flows to the surface.
➤ Usually safe if the source is protected from animals and waste.
🔹 3. Rainwater
- Collected using rooftop or surface catchment systems.
- Can be very pure but requires proper storage and filtering to prevent microbial growth.
🟡 IV. HOUSEHOLD METHODS OF WATER PURIFICATION
Since not all homes have access to treated water, simple and cost-effective purification methods can help ensure safe drinking water at the household level.
These methods remove physical impurities, pathogens, and in some cases chemical contaminants.
✅ A. Physical Methods
1. Boiling
- Water should be boiled for 10–15 minutes.
- It kills bacteria, viruses, protozoa, and some worms.
- Simple and effective but requires fuel or electricity.
- Boiled water must be stored in clean, covered containers to prevent re-contamination.
2. Sedimentation
- Water is allowed to stand undisturbed so that heavier particles settle at the bottom.
- Clear water is poured off from the top.
- Often used as the first step before boiling or chlorination.
3. Filtration
- Simple methods include:
- Cloth filtration (removes visible particles).
- Ceramic filters or biosand filters (remove bacteria and suspended particles).
- Commercial gravity-based filters (no electricity required).
✅ B. Chemical Methods
1. Chlorination
- Involves adding chlorine tablets or bleaching powder.
- Chlorine kills most bacteria and viruses.
- Standard dose: 0.5 grams per 20 liters of water; wait 30 minutes.
- Effective and affordable, but may leave a slight taste or smell.
2. Alum (Aluminum Sulfate) for Coagulation
- Used to remove muddy water or suspended solids.
- Added in small quantity (about 1g per liter), stirred, and allowed to settle.
- Followed by filtration and/or boiling.
3. Potassium Permanganate (KMnO₄)
- Sometimes used in very small quantities for disinfection and odor removal.
- Overuse can cause toxicity, so it must be used cautiously.
✅ C. Biological and Solar Methods
1. Solar Disinfection (SODIS)
- Water is stored in clear PET bottles and placed in direct sunlight for 6–8 hours.
- UV rays and heat destroy bacteria and viruses.
- Ideal for sunny rural areas; simple and sustainable.
2. Use of Moringa (Drumstick) Seeds
- Ground seeds act as natural coagulants to remove turbidity.
- Also have mild antibacterial properties.
- Useful where chemical coagulants are not available.
✅ D. Modern Domestic Water Purification Systems
1. UV Water Purifiers
- Use ultraviolet light to kill microorganisms.
- Require electricity; do not remove dissolved salts or chemicals.
- Effective for municipal water with low TDS.
2. RO (Reverse Osmosis) Systems
- Force water through a semi-permeable membrane to remove dissolved solids, heavy metals, and microorganisms.
- Removes fluoride, lead, arsenic, nitrates, etc.
- Requires regular maintenance and electricity.
3. RO + UV + UF Combined Systems
- Provide multi-stage filtration and ensure comprehensive purification.
- Useful for households using groundwater or borewell sources with high TDS and hardness.
🟣 V. STORAGE AND HANDLING OF DRINKING WATER
Even after purification, water can get contaminated if not stored or handled properly.
Key Practices:
- Use clean, narrow-mouthed containers with lids.
- Store water off the ground and in a shaded area.
- Use ladles or taps to draw water—avoid dipping hands or cups.
- Clean containers daily with soap and water.
Safe water is essential for human survival, public health, and economic development. Given the wide variety of contaminants in Indian water sources, household-level purification methods are crucial, especially in rural, tribal, and low-income urban areas where piped treated water is not available. By adopting simple, cost-effective, and sustainable methods, families can protect themselves from waterborne diseases and promote a healthier environment.
IV. Discuss the barriers to effective communication in health education and suggest methods to overcome them.
Communication is the foundation of health education, as it helps in transmitting correct health information, motivating behavioral change, and building trust with individuals and communities. However, effective communication often faces various barriers that hinder understanding, acceptance, and implementation of health advice.
In health education, these barriers may arise due to cultural, linguistic, psychological, environmental, or personal factors. Identifying and overcoming these obstacles is essential for delivering clear, impactful, and respectful health messages.
🔵 II. BARRIERS TO EFFECTIVE COMMUNICATION IN HEALTH EDUCATION
Barriers can be classified into various categories:
✅ A. Physical Barriers
These are obstacles in the environment or setting that interfere with message delivery.
- Noise and disturbances in clinics or community areas.
- Poor acoustics or lighting during health sessions.
- Distance between speaker and audience.
- Faulty equipment (e.g., microphone, visual aids).
- Inadequate seating or ventilation in the meeting area.
✅ B. Physiological Barriers
These are related to health problems of the communicator or receiver.
- Hearing or speech impairments in the audience.
- Fatigue or illness of the communicator or recipient.
- Cognitive disorders or mental fatigue that affect understanding.
- Language processing issues due to age or neurological issues.
✅ C. Psychological and Emotional Barriers
These barriers arise due to emotions, attitudes, or mental state of the participants.
- Fear, anxiety, or shyness in participants.
- Prejudices or preconceived notions about health topics (e.g., stigma around HIV, mental illness).
- Lack of interest or motivation to learn.
- Low self-esteem or distrust in the educator.
- Stress, anger, or emotional distress affecting message reception.
✅ D. Cultural and Social Barriers
These are due to cultural norms, beliefs, and social structures that influence communication.
- Differences in language, dialect, or accent.
- Health beliefs or taboos (e.g., misconceptions about contraception).
- Gender barriers in conservative communities.
- Educational background and literacy levels.
- Caste, religion, or class divisions that restrict free interaction.
✅ E. Semantic (Language) Barriers
These arise from differences in language, vocabulary, or interpretation of words.
- Use of technical or medical jargon unfamiliar to laypeople.
- Misinterpretation of commonly used words.
- Language mismatch between health educator and community.
- Lack of translation or regional language support in materials.
✅ F. Organizational or Structural Barriers
These are due to inadequate planning or improper channel selection.
- Unclear objectives of health education sessions.
- One-way communication without feedback.
- Overcrowded or rushed sessions with little interaction.
- Use of inappropriate communication aids for the target group.
- Poor time management during awareness programs.
🟡 III. METHODS TO OVERCOME COMMUNICATION BARRIERS IN HEALTH EDUCATION
Overcoming these barriers requires a planned, inclusive, and adaptive approach to health communication:
✅ A. Enhance the Physical Environment
- Conduct sessions in quiet, well-lit, ventilated, and spacious areas.
- Ensure comfortable seating arrangements and minimize distractions.
- Use functioning audio-visual aids and teaching materials.
✅ B. Use Simple and Clear Language
- Avoid complex medical terms and jargon.
- Use local language or dialect familiar to the audience.
- Provide translated handouts, posters, or flipbooks when necessary.
- Use pictorial messages or symbols for low-literate groups.
✅ C. Encourage Feedback and Interaction
- Use two-way communication methods – ask questions, invite opinions.
- Provide opportunities for audience clarification and discussion.
- Apply interactive methods like role plays, stories, and demonstrations.
✅ D. Respect Cultural and Social Values
- Be culturally sensitive – understand the beliefs and customs of the group.
- Involve local leaders, elders, or influencers to gain trust.
- Avoid judgmental or confrontational approaches during education.
- Adapt messages to fit the cultural context and values of the audience.
✅ E. Address Psychological Readiness
- Build rapport and trust before starting the session.
- Motivate participants through real-life success stories and positive reinforcement.
- Handle emotions and sensitive topics with empathy and confidentiality.
- Be non-threatening, friendly, and respectful in communication.
✅ F. Use Appropriate Educational Methods
- Choose communication methods based on age, literacy, and interests.
- Use audio-visual aids, demonstrations, charts, and models.
- Apply folk media, street plays, posters, and local songs in rural areas.
- Combine group discussions, lectures, and hands-on practice for effectiveness.
✅ G. Improve Planning and Structure
- Define clear, realistic goals for the session.
- Choose the right time, place, and audience size.
- Prepare a structured outline and rehearse the delivery.
- Evaluate the session and modify future approaches based on feedback.
Effective communication is the core of health education, but it can be obstructed by various barriers if not addressed. These barriers can lead to misunderstanding, misinformation, and resistance to healthy behavior change. By using culturally appropriate, clear, and inclusive communication techniques, and by adapting to the needs of the audience, health educators can ensure message clarity, promote behavior change, and improve community health outcomes.
Q.4 Write very short answers on the following questions (4 X2 = 8)
I.Define public health and mention one of its key objectives
Public Health:
It is the science and art of preventing disease, prolonging life, and promoting health through organized efforts of society, communities, and individuals.
One key objective:
👉 To prevent and control the spread of diseases in the population.
II.Explain the role of a conununity health nurse in promoting health
1️⃣ Health Education and Awareness
– The community health nurse plays a major role in educating individuals, families, and groups about hygiene, nutrition, immunization, and prevention of communicable and non-communicable diseases.
2️⃣ Disease Prevention and Early Detection
– The nurse conducts screening camps, home visits, and monitors growth charts, vital signs, and health indicators to detect diseases early and prevent complications.
3️⃣ Immunization Services
– The nurse ensures that all children and pregnant women in the community receive timely vaccines as per the Universal Immunization Programme.
4️⃣ Promotion of Safe Water and Sanitation Practices
– Educates the community on hand hygiene, water purification, proper waste disposal, and sanitary latrine use to prevent infections.
5️⃣ Maternal and Child Health (MCH) Care
– Provides antenatal and postnatal care, promotes exclusive breastfeeding, monitors child growth, and gives family planning counseling.
6️⃣ Support for National Health Programs
– Actively participates in programs like RCH, NCD control, tuberculosis elimination, and malaria prevention, promoting health at the grassroots level.
III Define health and illness.
✅ Health:
Health is a state of complete physical, mental, and social well-being, and not merely the absence of disease or infirmity.
(– World Health Organization, 1948)
✅ Illness:
Illness is a subjective experience of feeling unwell or unhealthy, which may or may not be due to a diagnosed disease. It reflects how a person perceives and responds to a health problem.
IV. Define foodborne disease and list any two preventive measures.
✅ Definition of Foodborne Disease:
A foodborne disease is an illness caused by consuming contaminated food or beverages, typically due to the presence of harmful bacteria, viruses, parasites, or toxins.
✅ Two Preventive Measures:
1️⃣ Ensure proper cooking and storage of food
→ Cook food thoroughly and keep perishable items refrigerated to prevent bacterial growth.
2️⃣ Practice good personal and kitchen hygiene
→ Wash hands before handling food and keep utensils and surfaces clean to avoid cross-contamination.
SECTION II
Q.5 Write the answers in one line of the followings- (7 X1 = 7)
I.Name one vector-borne disease.
👉 Malaria – It is transmitted by the female Anopheles mosquito, which carries the Plasmodium parasite.
II. What does CPHC stand for in community health?
👉 Comprehensive Primary Health Care
It refers to the delivery of holistic, need-based, and expanded health services that go beyond maternal and child health, including non-communicable diseases, mental health, elderly care, oral health, and emergency services, especially through Health and Wellness Centres (HWCs) under the Ayushman Bharat Mission.
III.State one objective of a home visit
👉 To provide need-based nursing care, health education, and follow-up services to individuals and families in their own home environment.
IV. Define Maternal Mortality Rate.
Maternal Mortality Rate is defined as:
👉 The number of maternal deaths due to pregnancy-related causes per 1,00,000 live births during a given time period, usually one year.
📌 Formula:
MMR = (Number of maternal deaths / Number of live births) × 100,000
📌 It reflects the quality of maternal health services and is a key indicator of health system effectiveness.
V. Name one warning sign of tuberculosis
👉 Persistent cough lasting more than 2 weeks, often with blood-tinged sputum.
VI. Which test is used to detect sugar in urine”
👉 Benedict’s Test
It is a chemical test used to detect the presence of glucose (reducing sugar) in urine, which may indicate conditions like diabetes mellitus.
Ask ChatGPT
VII. What are the three modes of disease transmission?
1️⃣ Direct Transmission
👉 Occurs through direct contact with an infected person, such as touching, kissing, sexual contact, or droplet spread (e.g., influenza, COVID-19).
2️⃣ Indirect Transmission
👉 Occurs through contaminated objects (fomites), food, water, or blood transfusion (e.g., hepatitis B, typhoid).
3️⃣ Vector-Borne Transmission
👉 Occurs when insects or animals (like mosquitoes, ticks) carry and transmit pathogens (e.g., malaria, dengue).
Q.6 Write essay type answer on ANY ONE of the following questions (1X15 = 15)
I.Explain the problem-solving approach in comumunity health nursing. How does it help address community health issues?
Community Health Nursing aims to improve the health status of individuals, families, and entire populations through organized health services. Due to the diversity of health problems and varying socio-cultural contexts, a problem-solving approach is essential in identifying, addressing, and managing community health challenges effectively.
This approach is a systematic, evidence-based, and community-centered process that helps in understanding root causes of problems, designing appropriate interventions, and evaluating outcomes. It not only strengthens health service delivery but also enhances community participation and self-reliance.
🔵 II. DEFINITION OF PROBLEM-SOLVING APPROACH
The problem-solving approach in community health nursing can be defined as:
“A logical, structured, and continuous process of identifying health problems in the community, analyzing their causes, formulating action plans, implementing appropriate interventions, and evaluating outcomes to promote community well-being.”
It is based on the public health model and closely follows the nursing process (assessment, diagnosis, planning, implementation, and evaluation) tailored to the community level rather than individuals alone.
🟡 III. STEPS OF THE PROBLEM-SOLVING APPROACH IN COMMUNITY HEALTH NURSING
Each step in the process builds upon the previous one and ensures that the nurse’s actions are targeted, purposeful, and measurable.
1️⃣ Community Health Assessment
This is the foundational step, where the nurse collects comprehensive data about the community to identify existing health conditions and resources.
🔹 Key Methods of Assessment:
- Household surveys and census data
- Observation of sanitation, housing, nutrition
- Interviews and focus group discussions
- Review of health records from sub-centres or PHCs
- Participatory techniques like social mapping, transect walks
🔹 Information Collected:
- Demographics: age, sex, literacy, occupation
- Morbidity and mortality data
- Availability of health services, roads, schools
- Environmental conditions: waste disposal, drainage, water supply
- Cultural practices, health beliefs, taboos
2️⃣ Diagnosis or Identification of Community Health Problems
Based on data, the nurse identifies key health problems, their determinants, and priority levels.
🔹 Example Diagnoses:
- High prevalence of diarrhea among under-five children due to contaminated water.
- Increased adolescent pregnancy rates due to lack of awareness and contraception.
- Low immunization coverage due to fear and cultural myths.
🔹 Prioritization Criteria:
- Magnitude and severity of the problem
- Vulnerability of the affected group
- Community demand and readiness
- Availability of resources
- Feasibility of intervention
3️⃣ Planning
Planning is the blueprint for action, ensuring that goals are realistic, measurable, and community-oriented.
🔹 Components of Planning:
- Goal: Broad statement of desired change
👉 Example: “To reduce anemia among adolescent girls in XYZ village.” - Objectives: Specific, measurable steps
👉 “To increase hemoglobin levels in 60% of girls within 6 months.” - Activities:
– Iron and folic acid (IFA) tablet distribution
– Nutrition education
– Cooking demonstrations - Resources Needed:
– Personnel, funds, materials, logistics - Time Frame and Responsibility:
– Assign roles to health workers and community volunteers.
4️⃣ Implementation
Implementation means putting the plan into action through community participation and coordinated effort.
🔹 Activities may include:
- Organizing health education sessions in schools, homes, or community halls.
- Conducting immunization drives or screening camps.
- Distributing sanitary kits, contraceptives, or nutrition supplements.
- Demonstrating safe practices like hand washing, ORS preparation.
- Engaging local influencers and volunteers for better outreach.
Implementation should be flexible to adapt to real-time challenges or community feedback.
5️⃣ Evaluation
Evaluation determines whether the program achieved its intended outcomes and identifies areas for improvement.
🔹 Types of Evaluation:
- Formative – done during implementation to guide improvements
- Summative – done at the end to assess overall impact
🔹 Evaluation Methods:
- Comparing baseline and post-intervention data
- Community feedback sessions
- Observation of behavioral changes
- Health indicators like immunization rate, anemia prevalence
Evaluation ensures accountability, builds evidence for success, and guides replication or scale-up of programs.
🟣 IV. IMPORTANCE OF PROBLEM-SOLVING APPROACH IN ADDRESSING COMMUNITY HEALTH ISSUES
✅ 1. Identifies Real Needs, Not Assumptions
– Avoids guesswork by using data-driven decisions, improving the relevance of interventions.
✅ 2. Promotes Targeted and Efficient Use of Resources
– Ensures time, funds, and manpower are directed toward the most pressing and solvable problems.
✅ 3. Facilitates Community Involvement
– Engages the population in problem identification, planning, and implementation, which increases ownership and sustainability.
✅ 4. Supports Measurable Outcomes
– By setting clear objectives and indicators, it allows for quantifiable evaluation of success or failure.
✅ 5. Improves Adaptability and Responsiveness
– If unexpected challenges arise, the plan can be modified promptly based on real-time assessment and feedback.
✅ 6. Builds Trust Between Health Workers and the Community
– Structured approach shows professionalism, which enhances credibility and cooperation.
🔵 V. ILLUSTRATIVE EXAMPLE
🔸 Situation:
High incidence of diarrheal disease in a slum community during monsoon.
🔸 Problem-Solving Steps Applied:
- Assessment – Found low hand hygiene, poor sanitation, and open defecation.
- Diagnosis – Community affected by contaminated water and lack of toilet facilities.
- Planning –
- Install community hand-washing stations.
- Conduct hygiene awareness sessions.
- Distribute ORS packets and chlorine tablets.
- Implementation – Health workers and volunteers carried out education campaigns and household visits.
- Evaluation – Within 3 months, diarrhea incidence dropped by 50%, and 70% of households adopted hand-washing practices.
The problem-solving approach is a cornerstone of effective community health nursing. It ensures that interventions are need-based, participatory, measurable, and impactful. By systematically assessing, diagnosing, planning, implementing, and evaluating health activities, community health nurses play a critical role in reducing disease burden, promoting healthy behavior, and empowering communities toward self-reliance.
This approach not only enhances service quality but also aligns with public health goals, national programs, and the vision of Universal Health Coverage.
II.. Define home visits and espiam they principles and purposes. Describe the steps and techniques of hag technique used during home visit
🟢 I. DEFINITION OF HOME VISITS
A home visit is a structured process in which a community health nurse or health worker visits the residence of an individual or family to assess their living conditions, provide direct health care, offer health education, and build a continuing relationship that supports wellness and disease prevention.
✅ According to WHO:
“A home visit is a purposeful interaction in the client’s home by a health professional to promote health, prevent illness, and provide care in the most natural and personal setting.”
It is one of the most effective outreach strategies used in rural, tribal, and underserved urban communities, ensuring that basic health services reach the doorstep of people in need.
🔵 II. PRINCIPLES OF HOME VISITS
The following key principles guide a professional and ethical home visit:
1️⃣ Planned and Goal-Oriented
– Every home visit must have a specific objective, such as immunization, follow-up care, or counseling. The nurse should prepare for the visit based on community needs and health priorities.
2️⃣ Need-Based and Client-Centered
– Services must be tailored to the individual or family’s needs, culture, socioeconomic status, and readiness to accept help.
3️⃣ Respect and Cultural Sensitivity
– The nurse must respect the family’s privacy, customs, and values. Always seek permission before entering or initiating interventions.
4️⃣ Participatory Approach
– The family should not be passive recipients but active participants in decision-making, learning, and care.
5️⃣ Continuity of Care
– A single visit is rarely sufficient; follow-up and long-term relationships are key to health improvement.
6️⃣ Scientific and Educational Focus
– Services provided during a home visit must be based on evidence-based practice, and health education should promote sustainable behavior change.
7️⃣ Accurate Documentation
– Everything observed, taught, or done during the visit must be clearly recorded, to ensure legal accountability and continuity of care.
🟠 III. PURPOSES OF HOME VISIT
Home visits serve multiple purposes that contribute to comprehensive community health:
✅ 1. Health Promotion
– Educating families on topics like personal hygiene, nutrition, immunization, and safe practices for maternal and child health.
✅ 2. Disease Prevention
– Early identification of risk factors and disease symptoms through screening, surveillance, and immunization efforts.
✅ 3. Curative and Basic Medical Care
– Providing wound care, medication, injections, and treatment for minor illnesses at home, especially where health facilities are far.
✅ 4. Rehabilitation and Follow-Up
– Post-discharge care for TB, stroke, leprosy, disability, or postnatal mothers who need continuous guidance and rehabilitation.
✅ 5. Building Trust and Rapport
– Strengthening nurse-family relationships for better health cooperation and compliance.
✅ 6. Environmental Assessment
– Observing and correcting hazards like unsafe water storage, open defecation, indoor smoke, and poor ventilation.
✅ 7. Data Collection and Health Record Updating
– Ensures accurate household health records, which help in micro-planning and program evaluation.
🟡 IV. STEPS OF A HOME VISIT
A professional home visit should follow these well-organized steps to ensure effectiveness:
🔹 1. Planning and Preparation
- Review the health records and prior visit notes.
- Set a clear objective for the visit (e.g., antenatal checkup, growth monitoring).
- Prepare kits and educational materials (BP apparatus, IFA tablets, flipcharts, ORS packets).
- Inform the family in advance if possible, especially for scheduled visits.
🔹 2. Approaching the Home and Building Rapport
- Greet the family courteously and introduce yourself with your designation and purpose.
- Observe non-verbal cues and attitudes of the family.
- Sit at eye-level and choose a comfortable, culturally appropriate space for discussion.
- Ensure to gain consent before beginning any procedure or assessment.
🔹 3. Comprehensive Family and Environmental Assessment
- Assess:
- Demographics: family size, age, occupation, education.
- Health status: signs of illness, nutritional deficiencies, disabilities.
- Immunization and antenatal care: schedule, completion, awareness.
- Living conditions: sanitation, water source, drainage, waste disposal.
- Behavioral factors: smoking, alcohol use, open defecation, food storage.
- Use observation, informal interviews, and visual examination to gather data.
🔹 4. Service Delivery and Interventions
- Provide necessary health care services as per the purpose of visit:
- Giving vaccines
- Checking BP and blood sugar
- Dressing wounds
- Distributing medications
- Counseling for contraception or breastfeeding
- Demonstrate correct methods (e.g., handwashing, ORS preparation).
🔹 5. Health Education and Behavior Change Communication (BCC)
- Deliver health education tailored to the family’s:
- Literacy level
- Cultural background
- Current health needs
- Use charts, pictures, pamphlets, role play, or verbal explanation to reinforce understanding.
- Encourage questions and discussion, especially with caregivers and decision-makers.
🔹 6. Recording and Reporting
- Record in family folder or register:
- Date, time, purpose
- Services provided
- Advice given
- Observations made
- Follow-up needed
- Submit data to PHC or Sub-Centre regularly.
🔹 7. Follow-Up and Referrals
- Schedule the next visit for follow-up of:
- Chronic illnesses
- High-risk pregnancies
- Immunization booster doses
- Refer the client to PHC/CHC for:
- Complicated cases
- Diagnostic services
- Specialist consultation
🟣 V. TECHNIQUES OF HAG METHOD IN HOME VISIT
The HAG technique is a practical approach used during home visits to ensure comprehensive assessment and intervention.
✅ H – Home Environment Assessment
- Observe:
- Housing structure: roof, walls, windows
- Cleanliness of kitchen and water source
- Toilet facilities and waste disposal
- Presence of mosquitoes, flies, animals
- Ventilation, overcrowding, cooking smoke
📌 Purpose: To identify environmental risk factors affecting family health.
✅ A – Ask and Assess Health Needs
- Use open-ended and respectful questions:
- “Has anyone been sick recently?”
- “Are all children immunized?”
- “Are you taking your medicines regularly?”
- Ask about:
- Nutrition and feeding practices
- Antenatal/postnatal visits
- Contraceptive use
- Chronic disease management
📌 Purpose: To understand medical and educational needs of the family.
✅ G – Give Health Education and Support
- Provide simple, need-based advice on:
- Hygiene and sanitation
- Safe motherhood
- Disease prevention
- Nutrition and infant care
- Drug compliance
- Demonstrate when possible (e.g., ORS, breast positioning, handwashing).
📌 Purpose: To promote self-care, awareness, and sustainable health behavior.
✅ VI. CONCLUSION
Home visits are a vital public health strategy in community health nursing, especially in low-resource settings. They allow the nurse to bridge the gap between health services and households, making care personal, preventive, promotive, and accessible.
By following scientific steps and using techniques like the HAG method, nurses ensure that home visits are not just routine, but transformative experiences that improve health knowledge, early disease detection, and behavior change—ultimately leading to a healthier, empowered community.
Q.7Write short answers on ANY THREE of the following questions- (5 X 5 = 15)
I. Highlight the essential qualities of a community health nurse
A community health nurse plays a critical role in promoting and maintaining the health of individuals, families, and communities in both rural and urban settings. Unlike hospital nurses, community health nurses work in the field, often in challenging conditions, delivering preventive, promotive, curative, and rehabilitative care.
To function effectively, a community health nurse must possess a unique combination of personal, professional, and ethical qualities that support client-centered, culturally appropriate, and resourceful care.
🔵 II. ESSENTIAL QUALITIES OF A COMMUNITY HEALTH NURSE
1️⃣ Professional Knowledge and Competence
- The nurse must have strong theoretical and practical knowledge of:
- Public health
- Epidemiology
- Family health care
- Maternal and child health
- Communicable and non-communicable diseases
- Should stay updated with national health programs, protocols, and innovations.
📌 Why important?
To provide scientific, evidence-based, and effective health services in the community.
2️⃣ Effective Communication Skills
- Must be able to listen actively, speak clearly, and explain health messages in simple language.
- Should be able to converse in local dialects and use visual aids effectively.
- Should use non-verbal communication like gestures, body language, and facial expressions appropriately.
📌 Why important?
To build trust and rapport, enhance health education, and ensure compliance.
3️⃣ Cultural Sensitivity and Respect
- Must respect community values, traditions, customs, and religious beliefs.
- Should never judge or criticize people for their lifestyle or health beliefs.
- Should adapt health messages to be culturally acceptable.
📌 Why important?
To gain cooperation, build credibility, and provide inclusive care.
4️⃣ Empathy and Compassion
- Must show genuine concern and kindness toward people, especially the poor, sick, and marginalized.
- Must be patient with elderly, disabled, and illiterate clients.
- Should be able to offer emotional support during suffering or crisis.
📌 Why important?
To reduce fear, improve health-seeking behavior, and build trust.
5️⃣ Leadership and Teamwork Ability
- Must be able to:
- Lead health campaigns
- Supervise ASHAs, ANMs, and volunteers
- Work with Anganwadi workers, NGOs, and panchayat members
- Should encourage community participation and act as a role model.
📌 Why important?
To mobilize community resources, delegate tasks, and coordinate care effectively.
6️⃣ Decision-Making and Problem-Solving Skills
- Must be able to identify health problems, prioritize needs, and plan interventions independently.
- Should use logic and experience to make timely decisions in emergencies or resource-limited settings.
📌 Why important?
To respond promptly, prevent complications, and manage outbreaks or high-risk situations.
7️⃣ Organizational and Time Management Skills
- Must plan home visits, immunization sessions, school health checkups, and health education programs efficiently.
- Should maintain health records, registers, and reporting formats in a timely manner.
📌 Why important?
To ensure continuity of care, timely follow-up, and accurate data submission.
8️⃣ Adaptability and Flexibility
- Must be ready to:
- Work in remote or disaster-prone areas
- Visit homes in varying weather conditions
- Adjust to cultural, environmental, or political challenges
📌 Why important?
To serve the community under all circumstances and overcome unexpected challenges.
9️⃣ Ethical Integrity and Confidentiality
- Must maintain:
- Confidentiality of patient information
- Honesty and transparency in records and services
- Equal treatment regardless of gender, caste, or religion
📌 Why important?
To uphold professional ethics, gain respect, and ensure legal accountability.
🔟 Motivation and Self-Discipline
- Must be self-driven, organized, and proactive in reaching out to vulnerable groups.
- Should set personal goals for improving service quality and community satisfaction.
📌 Why important?
To work consistently and achieve health goals without constant supervision.
The role of a community health nurse is both challenging and rewarding, requiring a blend of scientific knowledge, soft skills, leadership, and compassion. These essential qualities enable the nurse to deliver equitable, holistic, and person-centered care to individuals and families in real-life, community settings.
By nurturing these qualities, a community health nurse becomes a change agent, a health advocate, and a lifeline for public health services, helping India progress toward universal health coverage and healthier communities.
II. Enumerate the roles and responsibilities of community health nursing personnel in family health services.
Family health services are the core focus of community health nursing, aimed at promoting and maintaining the health of individuals within the context of the family. Community health nursing personnel, including public health nurses, ANMs (Auxiliary Nurse Midwives), LHVs (Lady Health Visitors), and ASHAs, play a vital role in delivering comprehensive, preventive, promotive, curative, and rehabilitative care to families.
Their roles are directed toward improving family health outcomes, reducing maternal and child mortality, preventing disease, and promoting health-seeking behavior.
🔵 II. ROLES AND RESPONSIBILITIES OF COMMUNITY HEALTH NURSING PERSONNEL IN FAMILY HEALTH SERVICES
The responsibilities can be grouped under various service components:
1️⃣ Maternal Health Services
- Conduct antenatal care (ANC) visits – register pregnant women, check BP, weight, and fetal growth.
- Distribute iron, calcium, and folic acid tablets and provide nutritional counseling.
- Identify high-risk pregnancies and make timely referrals.
- Conduct postnatal visits to monitor the mother’s recovery and newborn care.
- Educate mothers about breastfeeding, danger signs, and rest after delivery.
- Assist in institutional deliveries or conduct home deliveries if needed.
2️⃣ Child Health Services
- Monitor growth and development using growth charts.
- Promote exclusive breastfeeding for the first 6 months and appropriate complementary feeding.
- Administer vaccines as per the Universal Immunization Programme (UIP).
- Identify and manage malnutrition and common illnesses like diarrhea and ARI.
- Promote Vitamin A supplementation, deworming, and hygiene practices.
- Educate parents on child safety, immunization schedules, and disease prevention.
3️⃣ Family Planning Services
- Provide counseling to eligible couples about spacing and permanent methods.
- Distribute oral contraceptive pills, condoms, and refer for IUD or sterilization.
- Maintain eligible couple registers and track contraceptive acceptance.
- Address myths and misconceptions related to family planning.
- Ensure follow-up care after sterilization or IUD insertion.
4️⃣ Adolescent and School Health
- Conduct health check-ups and awareness programs in schools.
- Educate adolescents about menstrual hygiene, nutrition, anemia, and reproductive health.
- Distribute Iron and Folic Acid tablets (IFA) under the WIFS programme.
- Identify and refer adolescents with behavioral, emotional, or physical issues.
- Promote life skill education and substance abuse prevention.
5️⃣ Nutrition Services
- Identify malnourished children and pregnant women during visits.
- Counsel on locally available nutritious foods and correct feeding practices.
- Link families with supplementary nutrition programs (ICDS, Anganwadi centers).
- Monitor weight gain in pregnancy and BMI of adults and adolescents.
- Participate in nutrition demonstration and awareness camps.
6️⃣ Health Education and Counseling
- Provide health teaching at individual, family, and group levels.
- Use audio-visual aids, charts, and folk media for illiterate populations.
- Educate on personal hygiene, sanitation, safe drinking water, ORS use, etc.
- Counsel families on healthy lifestyles, early treatment-seeking behavior, and compliance.
- Organize group meetings, mothers’ meetings, and community awareness sessions.
7️⃣ Disease Prevention and Control
- Conduct screening for communicable and non-communicable diseases.
- Promote vaccination, sanitation, and mosquito control to prevent malaria, dengue, etc.
- Identify suspected cases of TB, leprosy, COVID-19, or diarrhea outbreaks.
- Guide families on home isolation, medication adherence, and infection control.
- Refer and follow up for chronic illnesses like hypertension and diabetes.
8️⃣ Home Visits and Follow-Up Care
- Conduct regular home visits for vulnerable families, pregnant women, infants, and elderly.
- Provide basic nursing care, assess environmental sanitation, and promote home hygiene.
- Follow up on defaulters for immunization, ANC, and chronic disease care.
- Provide supportive counseling and care during illness or grief.
9️⃣ Record Keeping and Reporting
- Maintain:
- Eligible couple registers
- Maternal and child health records
- Immunization and nutrition charts
- Home visit records and referral slips
- Submit reports to PHC or Sub-centre for program evaluation and monitoring.
🔟 Coordination and Community Involvement
- Coordinate with:
- ASHA, Anganwadi workers, PRI members
- Village Health Sanitation and Nutrition Committees (VHSNCs)
- Health department staff, NGOs, and school teachers
- Motivate the community to participate in health days, camps, and government programs.
Community health nursing personnel serve as the backbone of India’s primary health care system, especially in the delivery of family-centered care. Their multifaceted role extends from clinical care to education, counseling, surveillance, and coordination.
By fulfilling their responsibilities with dedication, sensitivity, and skill, community health nurses help reduce maternal and child mortality, promote reproductive health, empower families, and contribute significantly to achieving Universal Health Coverage and Sustainable Development Goals.
III.Describe the role of a nurse in preventing and controlling vector-borne diseases like malaria and dengue.
Vector-borne diseases like malaria and dengue are major public health problems in India, especially during the monsoon and post-monsoon seasons. These diseases are transmitted by mosquito vectors – Anopheles (for malaria) and Aedes aegypti (for dengue). They lead to high morbidity, mortality, and increased burden on the health system.
Nurses, especially community health nurses, play a crucial role in prevention, early detection, control, and community education related to these diseases. Their involvement in surveillance, case management, environmental control, and health education is vital in controlling outbreaks.
🔵 II. ROLE OF A NURSE IN PREVENTION AND CONTROL OF MALARIA AND DENGUE
The role of the nurse can be explained under specific functions:
1️⃣ Health Education and Community Awareness
- Educate individuals and families on:
- Causes, transmission, symptoms, and complications of malaria and dengue.
- Importance of early reporting of fever to the nearest health facility.
- Avoiding mosquito bites using nets, repellents, and protective clothing.
- Using screens on windows and doors to prevent mosquito entry.
- Conduct awareness sessions during school health programs, village meetings, and health camps using:
- Posters, flipcharts, pamphlets
- Role plays, group discussions, and demonstrations
📌 Purpose: To promote behavioral change and community participation in mosquito control.
2️⃣ Surveillance and Early Case Detection
- Participate in active and passive surveillance of fever cases.
- Conduct house-to-house visits in endemic or outbreak-prone areas.
- Identify suspected cases based on signs and symptoms:
- Malaria: Chills, fever with rigors, sweating, headache
- Dengue: High-grade fever, retro-orbital pain, body ache, rash, bleeding
- Collect blood smears or Rapid Diagnostic Tests (RDTs) for malaria detection.
- Report and refer suspected dengue cases for CBC and platelet count.
📌 Purpose: To detect and treat early, prevent complications, and reduce disease transmission.
3️⃣ Case Management and Nursing Care
- Administer antimalarial drugs as per national guidelines (ACT, Chloroquine, Primaquine).
- Monitor fever, hydration status, urine output, and vital signs.
- In dengue cases:
- Watch for warning signs: persistent vomiting, bleeding, abdominal pain, drop in BP.
- Ensure adequate fluid replacement and rest.
- Refer cases with low platelet counts or shock to higher centers.
- Educate the patient and caregiver on home care and danger signs.
📌 Purpose: To ensure prompt and safe treatment, prevent severe complications like cerebral malaria or dengue shock syndrome.
4️⃣ Vector Control and Environmental Sanitation
- Assist in identifying and eliminating mosquito breeding sites, such as:
- Open water tanks, discarded containers, stagnant water in pots, tires
- Water in coolers, flowerpots, construction sites
- Promote use of:
- Mosquito nets (especially insecticide-treated)
- Larvicides in water bodies (temephos, guppy fish)
- Fogging/spraying in outbreak areas
- Motivate the community to practice weekly dry-day – cleaning containers and draining standing water.
📌 Purpose: To break the life cycle of mosquitoes and reduce the vector population.
5️⃣ Collaboration with Local Authorities and NGOs
- Coordinate with:
- ASHAs, ANMs, Multipurpose Health Workers
- Gram Panchayats, Urban local bodies
- Accredited NGOs and health activists
- Assist in organizing anti-larval drives, sanitation campaigns, and mass awareness programs.
📌 Purpose: To enhance inter-sectoral collaboration and make prevention efforts more effective.
6️⃣ Training and Capacity Building
- Help train:
- ASHA workers, school teachers, and local volunteers on mosquito control, early diagnosis, and reporting.
- Update own knowledge on revised malaria/dengue treatment protocols and outbreak guidelines.
📌 Purpose: To build community-based capacity for long-term control.
7️⃣ Record-Keeping and Reporting
- Maintain accurate records of:
- Suspected and confirmed cases
- Laboratory reports
- Drug administration
- Health education sessions
- Home visits and environmental checks
- Submit weekly and monthly reports to PHC, Sub-Centre, or CHC.
📌 Purpose: For monitoring trends, planning interventions, and reporting outbreaks.
The nurse plays a central role in the multi-level prevention and control of vector-borne diseases like malaria and dengue. Through education, surveillance, treatment, environmental measures, and community involvement, nurses help reduce disease burden, save lives, and promote healthier living conditions.
In the face of climate change, urbanization, and changing vector behavior, the nurse’s knowledge, vigilance, and community presence become even more essential in keeping vector-borne diseases under control.
IV. Discuss the objectives and components of school health services and the role of a school health nurse.
School Health Services are a set of organized activities provided by the health and education sectors to improve and maintain the physical, mental, emotional, and social well-being of children in school age. These services act as a bridge between healthcare services and the education system, ensuring that children are healthy, active, and ready to learn.
School is the ideal setting for delivering health interventions as it covers the most formative years of life, and children are easily accessible through this setup. With the implementation of the Ayushman Bharat School Health Programme, the scope of school health has expanded significantly.
✅ II. OBJECTIVES OF SCHOOL HEALTH SERVICES
The essential objectives include:
1️⃣ To Promote Positive Health
– It is to ensure children attain optimum growth and development through timely interventions.
– Activities include health checkups, immunizations, and physical fitness promotion.
2️⃣ To Prevent Diseases
– Early identification of diseases such as vision problems, dental issues, nutritional deficiencies, and communicable diseases.
– Preventive education about hygiene and sanitation.
3️⃣ To Provide Early Diagnosis and Treatment
– Timely diagnosis through health screening and check-ups.
– Immediate treatment or referral helps reduce school absenteeism and future complications.
4️⃣ To Ensure Healthy Environment in Schools
– To monitor cleanliness, sanitation, safe water supply, and first-aid readiness.
– Ensuring the school premises are safe from hazards and infection risks.
5️⃣ To Educate Children on Health
– Health education on personal hygiene, nutrition, safety, reproductive health, and lifestyle diseases.
– Help children develop healthy behaviors and decision-making skills.
6️⃣ To Develop Health Consciousness
– Promote awareness about disease prevention, mental health, and substance abuse through health talks and activities.
✅ III. COMPONENTS OF SCHOOL HEALTH SERVICES
The following are the eight essential components of a comprehensive school health program:
1️⃣ Health Appraisal
– Initial and periodic check-ups for all students.
– Screening includes height, weight, BMI, vision, hearing, dental check, skin conditions, anemia, and mental health.
2️⃣ Treatment and Referral Services
– Minor ailments (e.g., fever, wounds, skin infections) are treated by the nurse or health officer.
– Referrals made to PHC/CHC/district hospitals for major problems (e.g., congenital heart defects, orthopedic issues, mental health disorders).
3️⃣ Immunization Services
– Integration with the Universal Immunization Programme (UIP).
– School-based vaccination campaigns – e.g., Measles-Rubella (MR), HPV (in adolescent girls), Tetanus-Diphtheria (Td).
– Maintenance of immunization registers.
4️⃣ Nutritional Services
– Height, weight, and hemoglobin monitoring.
– Iron-Folic Acid supplementation under Weekly Iron and Folic Acid Supplementation (WIFS).
– Deworming every 6 months.
– Monitoring the Mid-Day Meal Scheme for hygiene and nutrient content.
5️⃣ Health Education and Counseling
– Topics include:
- Menstrual hygiene management
- Personal cleanliness
- Balanced diet
- Physical activity
- Tobacco and alcohol prevention
- Road safety and mental health
– Methods: Role plays, peer education, posters, storytelling, puppet shows, video shows.
6️⃣ Mental Health Support
– Identification of children facing academic stress, behavioral problems, abuse, bullying, or substance use.
– Counseling sessions and referrals to trained psychologists or counselors.
7️⃣ School Environment Hygiene and Sanitation
– Assessment and maintenance of:
- Clean drinking water
- Separate clean toilets for boys and girls
- Proper drainage and waste management
- Safe classrooms and playgrounds
8️⃣ Maintenance of Records
– Health card for each child detailing:
- Anthropometry
- Screening results
- Immunization status
- Referrals
- Interventions provided
✅ IV. ROLE OF SCHOOL HEALTH NURSE
A school health nurse is the primary agent who implements, monitors, and evaluates health services and education in school settings. The nurse’s role is multidimensional:
🟢 1. Health Screening and Monitoring
– Conduct periodic health assessments.
– Identify physical, nutritional, developmental, and mental health issues.
– Maintain accurate and updated health records.
🟢 2. First Aid and Emergency Care
– Provide prompt care during injuries, allergic reactions, or illness.
– Maintain an equipped first aid room or box.
– Educate school staff on emergency procedures like CPR and wound dressing.
🟢 3. Referral and Follow-Up
– Ensure timely referral of complicated cases to higher health centers.
– Track treatment adherence and communicate with parents.
🟢 4. Health Promotion and Education
– Design and deliver age-appropriate health education sessions.
– Use interactive methods: charts, drama, quizzes, and role-plays.
– Promote hygienic practices among children such as:
- Hand washing
- Sanitary pad use
- Brushing teeth twice daily
🟢 5. Nutritional Surveillance
– Monitor nutritional status.
– Identify children with undernutrition, overweight, or anemia.
– Coordinate with authorities for mid-day meal improvements.
🟢 6. Environmental Health Monitoring
– Check sanitation, water safety, and food hygiene.
– Participate in school sanitation drives.
– Report health hazards like contaminated water or food poisoning.
🟢 7. Mental Health and Psychosocial Support
– Identify children with behavioral problems or trauma.
– Offer basic counseling or psychoeducation.
– Refer complex cases to psychologists or psychiatrists.
🟢 8. Parental and Teacher Collaboration
– Conduct awareness programs for parents.
– Train teachers on recognizing early signs of illness, abuse, or disabilities.
– Work as a liaison between school and local health authorities.
School health services form the foundation for a lifetime of healthy behaviors. Through regular screenings, education, and referrals, these services promote holistic child development and reduce health-related barriers to learning. The school health nurse plays a critical and dynamic role in ensuring the successful implementation of these services by acting as a caregiver, educator, counselor, and advocate for children’s health within the school setting.
