22/07/2013 MEDICAL SURGICAL NURSING 1 DONE-UPLOAD NO.9
AHN-1-PAPER SOLUTION NO.9
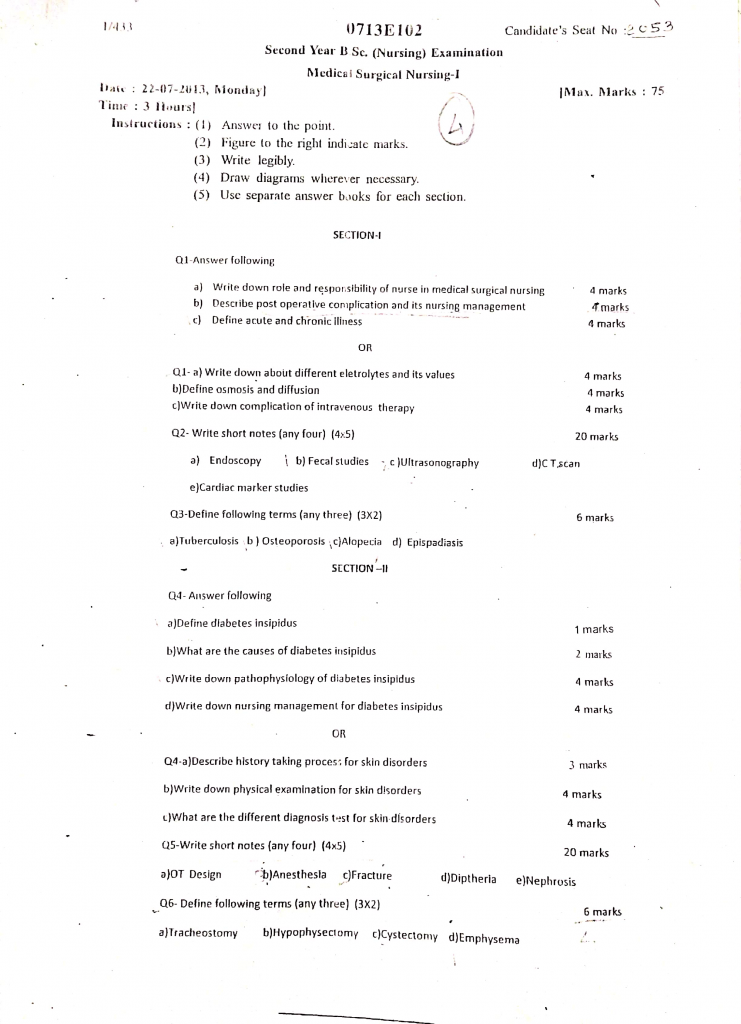
Section 1
Q.1 Answer following
a. Write down role and responsibility of nurse in medical surgical nursing (4 mark)
Role in Patient Assessment
- It is the responsibility of the nurse to perform comprehensive assessment of patient which includes physical, psychological, emotional, social, and spiritual aspects.
- It is done by collecting health history and performing systematic head-to-toe physical examination.
- It is also essential to monitor and document vital signs, level of consciousness, pain score, and other physiological parameters regularly.
Role in Planning and Implementing Care
- It is the duty of the nurse to develop an individualized nursing care plan based on assessment findings and patient needs.
- It is important to prioritize nursing diagnoses and formulate goals and expected outcomes.
- It is the responsibility of the nurse to implement evidence-based interventions to promote recovery and prevent complications.
Role in Medication Administration
- It is the nurse’s responsibility to safely administer prescribed medications via oral, parenteral, topical, inhalational, or other routes.
- It is also essential to check the right patient, right drug, right dose, right route, and right time (5 Rights of medication).
- It is the duty of the nurse to observe for adverse drug reactions and report them immediately to the physician.
Role in Preoperative and Postoperative Care
- It is the nurse’s role to prepare patients both physically and psychologically for surgical procedures.
- It is essential to ensure preoperative fasting, skin preparation, informed consent, and safe transfer to the OT.
- In the postoperative phase, it is the responsibility of the nurse to monitor airway, breathing, circulation, surgical site, pain level, and prevent complications such as infection and deep vein thrombosis.
Role in Maintaining Hygiene and Comfort
- It is the duty of the nurse to provide personal hygiene, maintain skin integrity, and ensure a clean and comfortable environment.
- It is also important to prevent pressure ulcers by frequent repositioning and providing appropriate support surfaces.
- It is the nurse’s role to provide comfort measures, manage pain, and ensure adequate rest and sleep for the patient.
Role in Nutrition and Hydration
- It is the responsibility of the nurse to assess nutritional status and collaborate with the dietician for an appropriate diet plan.
- It is essential to monitor oral intake, fluid balance, electrolyte status, and prevent dehydration and malnutrition.
- It is the nurse’s role to assist or feed patients who are unable to feed themselves.
Role in Patient and Family Education
- It is the responsibility of the nurse to provide health education regarding disease process, treatment, medications, and lifestyle modifications.
- It is also important to educate caregivers on how to provide home care, wound care, and manage medical equipment if needed.
- It is the role of the nurse to promote self-care and independence to enhance recovery.
Role in Infection Prevention and Control
- It is the nurse’s responsibility to follow strict infection control measures such as hand hygiene, use of PPE, sterilization, and safe waste disposal.
- It is important to educate patients and families on infection prevention strategies.
- It is also the nurse’s duty to monitor for signs of hospital-acquired infections and take appropriate actions if needed.
Role in Emotional and Psychological Support
- It is the responsibility of the nurse to provide emotional support and address the psychological needs of patients and families.
- It is also important to promote a positive environment, provide therapeutic communication, and reduce anxiety and stress during hospitalization.
- It is the role of the nurse to refer patients to mental health professionals when needed.
Role in Documentation and Reporting
- It is the nurse’s duty to maintain accurate, clear, and timely documentation of patient care.
- It is also essential to report significant changes in patient condition to the healthcare team promptly.
- It is important to participate in shift handover to ensure continuity of care.
Role in Coordination of Care
- It is the responsibility of the nurse to collaborate with physicians, physiotherapists, dieticians, social workers, and other members of the multidisciplinary team.
- It is also essential to coordinate discharge planning and arrange for necessary follow-up services and home care support.
Role in Emergency and Crisis Management
- It is the nurse’s duty to recognize early signs of clinical deterioration and respond quickly in emergencies.
- It is important to perform basic and advanced life support measures when required.
- It is also essential to assist in the management of code blue situations and provide care in disaster and mass casualty scenarios.
b. Describe post operative complication and its nursing management (4 mark)
- Postoperative complications are unwanted problems or adverse outcomes that occur after surgery.
- It may affect recovery, prolong hospital stay, increase cost, and even cause mortality if not managed properly.
- Complications can occur immediately (within 24 hours), early (first week) or late (weeks to months) after surgery.
Common Postoperative Complications
1️⃣ Respiratory Complications
- It includes atelectasis, pneumonia, bronchospasm, pulmonary embolism.
- It usually occurs due to immobility, shallow breathing, pain, general anesthesia, and preexisting lung disease.
2️⃣ Cardiovascular Complications
- It includes hypotension, hypertension, dysrhythmias, myocardial infarction, deep vein thrombosis (DVT), and pulmonary embolism.
3️⃣ Hemorrhage and Hypovolemic Shock
- It occurs due to excessive blood loss during or after surgery.
- It can lead to hypotension, tachycardia, pallor, cold and clammy skin, and decreased urine output.
4️⃣ Wound Complications
- It includes wound infection, dehiscence (wound opening), evisceration (protrusion of organs), hematoma, and seroma formation.
5️⃣ Fluid and Electrolyte Imbalance
- It may occur due to blood loss, inadequate fluid intake, vomiting, diarrhea, or diuretic use.
- It may cause dehydration, electrolyte disturbances (hyponatremia, hypokalemia), and acid-base imbalance.
6️⃣ Urinary Complications
- It includes urinary retention, urinary tract infection (UTI), and renal failure.
- It may occur due to anesthesia effects, pain, immobility, and decreased fluid intake.
7️⃣ Gastrointestinal Complications
- It includes paralytic ileus (absence of bowel movement), constipation, nausea and vomiting, abdominal distension.
- It may occur due to anesthesia, opioids, immobility, and decreased bowel motility.
8️⃣ Neurological Complications
- It includes delirium, confusion, agitation, anxiety, and stroke.
- It is commonly seen in elderly patients and those with preexisting neurological conditions.
9️⃣ Thromboembolic Complications
- It includes deep vein thrombosis (DVT) and pulmonary embolism (PE).
- It may occur due to immobility, hypercoagulable state, and venous injury during surgery.
Nursing Management of Postoperative Complications
1️⃣ Respiratory Complications
- It is the nurse’s role to encourage deep breathing, coughing, incentive spirometry, and early ambulation.
- It is also important to maintain oxygen therapy as prescribed and monitor respiratory rate, breath sounds, and oxygen saturation.
2️⃣ Cardiovascular Complications
- It is the responsibility of the nurse to monitor vital signs, ECG, and assess for signs of DVT.
- It is also essential to provide leg exercises, anti-embolism stockings, and ensure early mobilization.
- Nurse should promptly report signs of chest pain, shortness of breath, and abnormal ECG findings.
3️⃣ Hemorrhage and Hypovolemic Shock
- It is the nurse’s role to monitor surgical site for bleeding, assess vital signs, and maintain IV fluid replacement.
- It is important to report excessive drainage and prepare for blood transfusion if ordered.
- Nurse should maintain supine position with legs elevated in case of hypovolemic shock.
4️⃣ Wound Complications
- It is the nurse’s responsibility to maintain aseptic technique during wound care.
- It is also important to monitor wound drainage, signs of infection, and wound approximation.
- Nurse should reinforce wound dressing as needed and report signs of dehiscence or evisceration.
5️⃣ Fluid and Electrolyte Imbalance
- It is the nurse’s role to monitor fluid intake and output (I&O) accurately.
- It is essential to monitor serum electrolytes and report abnormal values.
- Nurse should administer IV fluids, electrolytes, and encourage oral intake as tolerated.
6️⃣ Urinary Complications
- It is the nurse’s responsibility to assess urinary output and monitor for signs of retention or infection.
- It is important to assist patient with early ambulation and toileting.
- If urinary retention occurs, bladder scanning and catheterization may be required under medical advice.
7️⃣ Gastrointestinal Complications
- It is the nurse’s duty to monitor bowel sounds, abdominal girth, and passage of flatus.
- It is important to promote early oral intake as tolerated and encourage early ambulation.
- Nurse should administer antiemetics, prokinetic agents, and provide high-fiber diet to prevent constipation.
8️⃣ Neurological Complications
- It is the nurse’s role to perform neurological assessments and monitor for changes in consciousness or behavior.
- It is important to provide orientation, reorient confused patients, and ensure a safe environment to prevent injury.
- Nurse should report persistent confusion, agitation, or neurological deficits immediately.
9️⃣ Thromboembolic Complications
- It is the nurse’s responsibility to encourage leg exercises, early ambulation, and use compression stockings.
- It is also important to monitor for signs of DVT (calf pain, swelling) and PE (chest pain, dyspnea).
- Nurse should administer anticoagulants as prescribed and ensure patient education about DVT prevention.
c. Define acute and chronic illness (4 mark)
Acute Illness
- Acute illness is defined as a disease or health condition that develops suddenly, progresses rapidly, and usually has a short duration — typically lasting from a few hours to a few days or weeks.
- It is often caused by infection, trauma, injury, inflammation, or sudden physiological imbalance.
- It usually shows prominent signs and symptoms that prompt the person to seek immediate medical attention.
- Acute illnesses can be self-limiting (resolve on their own) or may require medical or surgical treatment.
- Examples of acute illness include: fever, pneumonia, appendicitis, acute gastroenteritis, urinary tract infection, heart attack, stroke.
Chronic Illness
- Chronic illness is defined as a long-term disease or condition that develops gradually, progresses slowly, and typically persists for more than 3 months to a lifetime.
- It is usually caused by genetic factors, environmental influences, unhealthy lifestyle, or age-related degenerative changes.
- Chronic illnesses are not curable, but they can often be managed or controlled through lifestyle changes, medications, and rehabilitation.
- It is characterized by periods of remission (improvement) and exacerbation (worsening).
- Chronic illness often affects quality of life, requires long-term care, and can have psychosocial and economic impact on the patient and family.
- Examples of chronic illness include: diabetes mellitus, hypertension, asthma, chronic kidney disease, rheumatoid arthritis, heart failure, chronic obstructive pulmonary disease (COPD).
Or
Q.1 Answer following
a. Write down about different electrolyes and it values (4mark)
- Electrolytes are charged minerals (ions) present in body fluids, which are essential for maintaining fluid balance, acid-base balance, neuromuscular activity, and cellular function.
- It is important for nurses to monitor electrolyte levels in patients, as imbalances can lead to life-threatening complications.
- The main electrolytes are found in extracellular fluid (ECF) and intracellular fluid (ICF).
Different Electrolytes and Their Normal Values
1️⃣ Sodium (Na⁺)
- It is the primary extracellular cation and helps maintain fluid balance, nerve conduction, and muscle contraction.
- It plays a key role in maintaining extracellular osmolarity and blood pressure regulation.
- It also supports acid-base balance through the sodium-bicarbonate exchange mechanism.
- Normal value: 135–145 mEq/L.
- Disorders include hyponatremia and hypernatremia, which can cause confusion, seizures, coma.
2️⃣ Potassium (K⁺)
- It is the primary intracellular cation and essential for nerve impulse conduction, cardiac rhythm regulation, and muscle function.
- It also influences acid-base balance by shifting between intracellular and extracellular compartments.
- Potassium is critical for maintaining resting membrane potential of all excitable tissues, including the heart and skeletal muscles.
- Normal value: 3.5–5.0 mEq/L.
- Imbalances such as hypokalemia or hyperkalemia can lead to life-threatening arrhythmias.
3️⃣ Calcium (Ca²⁺)
- It is essential for bone and teeth formation, blood clotting, muscle contraction, and nerve transmission.
- Calcium also plays an important role in hormone secretion and enzyme activation.
- It helps regulate cardiac electrical activity, influencing the plateau phase of the cardiac action potential.
- Normal value: 8.5–10.5 mg/dL.
- Disorders include hypocalcemia (tetany, seizures) and hypercalcemia (renal stones, cardiac arrhythmia).
4️⃣ Magnesium (Mg²⁺)
- It acts as a cofactor for many enzymatic reactions and supports neuromuscular function and cardiac rhythm.
- It also influences parathyroid hormone secretion, thereby indirectly affecting calcium metabolism.
- Magnesium is essential for DNA and RNA synthesis and energy production through ATP metabolism.
- Normal value: 1.5–2.5 mEq/L or 1.8–3.0 mg/dL.
- Imbalances such as hypomagnesemia can cause tetany, seizures, and arrhythmias, while hypermagnesemia can depress neuromuscular activity.
5️⃣ Chloride (Cl⁻)
- It is the major extracellular anion and helps maintain osmotic pressure, acid-base balance, and fluid balance.
- Chloride is also important in maintaining electrical neutrality of cells by balancing positive cations like sodium.
- It is involved in the formation of hydrochloric acid (HCl) in the stomach, which is essential for digestion.
- Normal value: 95–105 mEq/L.
- Disorders include hypochloremia (metabolic alkalosis) and hyperchloremia (metabolic acidosis).
6️⃣ Bicarbonate (HCO₃⁻)
- It is a key component of the body’s buffer system, helping maintain acid-base balance.
- It is regulated mainly by the kidneys and is involved in transporting CO₂ in the blood.
- Bicarbonate helps neutralize excess acids and is crucial in preventing metabolic acidosis or alkalosis.
- Normal value: 22–26 mEq/L.
- Alterations in bicarbonate levels are seen in conditions like renal failure, COPD, and diabetic ketoacidosis.
7️⃣ Phosphate (PO₄³⁻)
- It is necessary for energy metabolism (ATP formation), bone mineralization, and cellular function.
- It also plays a role in acid-base buffering and is important for the structural integrity of cell membranes (as phospholipids).
- Phosphate is required for oxygen delivery to tissues via its role in 2,3-DPG (diphosphoglycerate) in red blood cells.
- Normal value: 2.5–4.5 mg/dL.
- Disorders include hypophosphatemia (muscle weakness, respiratory failure) and hyperphosphatemia (seen in renal failure).
b. Define osmosis and diffusion (4 mark)
Definition of Osmosis
- Osmosis is defined as the passage or movement of water molecules from an area of lower solute concentration (higher water concentration) to an area of higher solute concentration (lower water concentration) across a semi-permeable membrane.
- It is a passive process that does not require any energy (ATP).
- Osmosis continues until equilibrium is reached, where the concentration of solutes on both sides of the membrane becomes equal.
- It helps maintain fluid balance between intracellular and extracellular compartments.
- It is an essential mechanism for regulating cell volume and preventing cell shrinkage or swelling.
- Osmosis also plays a key role in capillary exchange, where water moves between blood plasma and interstitial fluid.
- Example: Movement of water into red blood cells or plant root cells.
Definition of Diffusion
- Diffusion is defined as the movement of particles (solutes or gases) from an area of higher concentration to an area of lower concentration until equilibrium is achieved.
- It is also a passive process that does not require energy (ATP).
- Diffusion helps substances like oxygen, carbon dioxide, and nutrients move across cell membranes or in body fluids.
- The rate of diffusion depends on temperature, concentration gradient, surface area, and size of molecules.
- Diffusion allows for the equal distribution of molecules throughout a given space or medium.
- It is a crucial process for gas exchange in lungs, where oxygen diffuses from alveoli to blood and carbon dioxide diffuses from blood to alveoli.
- Example: Exchange of oxygen and carbon dioxide between alveoli and blood capillaries in the lungs.
c. Write down complication of intravenous therapy (4 mark)
- Intravenous therapy is the administration of fluids, medications, blood products, or nutrients directly into the bloodstream through a vein.
- Though IV therapy is widely used, it is associated with several local and systemic complications.
- Nurses play a vital role in preventing, identifying, and managing these complications.
Complications of IV Therapy
1️⃣ Infiltration
- It occurs when IV fluid leaks into the surrounding tissue instead of the vein.
- It is usually caused by improper IV catheter placement or dislodgement.
- Signs include swelling, coolness, discomfort, and blanching around the IV site.
- Severe infiltration can cause tissue damage.
2️⃣ Phlebitis
- It is defined as inflammation of the vein at the IV insertion site.
- It can be caused by mechanical trauma, chemical irritation, or infection.
- Signs include redness, warmth, pain, and palpable cord along the vein.
- If left untreated, it may progress to thrombophlebitis.
3️⃣ Extravasation
- It occurs when vesicant (tissue-damaging) drugs leak into the surrounding tissue.
- It causes severe tissue injury, blistering, necrosis, and ulceration.
- Prompt recognition and management are essential to minimize permanent tissue damage.
4️⃣ Infection (Local or Systemic)
- Local infection can occur at the IV insertion site, leading to redness, warmth, purulent discharge, and pain.
- If bacteria enter the bloodstream, it can cause systemic infection or sepsis, which is life-threatening.
- Strict aseptic technique is necessary to prevent this complication.
5️⃣ Hematoma
- It is a localized collection of blood under the skin due to vein puncture or trauma.
- It presents as bruising, swelling, and discoloration around the IV site.
- Large hematomas can cause pain and compression of surrounding tissues.
6️⃣ Air Embolism
- It occurs when air enters the vein and travels to the heart or lungs, causing blockage of blood flow.
- It is a rare but potentially fatal complication.
- Signs include sudden dyspnea, chest pain, cyanosis, hypotension, and loss of consciousness.
- Prompt action is needed to prevent cardiovascular collapse.
7️⃣ Speed Shock
- It occurs when IV medications are administered too rapidly, causing toxic effects.
- Signs include flushing, dizziness, hypotension, irregular pulse, and cardiac arrest.
- Nurses must follow proper rate of administration to prevent this complication.
8️⃣ Fluid Overload
- It occurs when excessive fluid is infused, especially in elderly or cardiac-compromised patients.
- It leads to pulmonary edema, hypertension, dyspnea, crackles in lungs, and distended neck veins.
- Careful monitoring of IV rate and fluid balance is required.
9️⃣ Thrombosis
- It is the formation of a blood clot inside the vein.
- It can obstruct blood flow and may result in pain, swelling, and dysfunction of the affected limb.
- There is also a risk of embolism if the clot dislodges.
10️⃣ Allergic Reaction
- It may occur due to IV medications, fluids, or latex used in IV equipment.
- Symptoms include rash, itching, wheezing, shortness of breath, and in severe cases, anaphylaxis.
- Immediate discontinuation of the IV and emergency management is needed.
Q.2 Write short notes on (any four) [20 mark]
a. Endoscopy
Definition
- Endoscopy is a diagnostic and therapeutic medical procedure in which a flexible tube with a camera and light source (called an endoscope) is inserted into the body to directly visualize internal organs and structures.
- It helps doctors to examine, diagnose, take biopsies, and sometimes treat conditions affecting the gastrointestinal tract, respiratory tract, and other internal areas.
- It is a minimally invasive procedure and can be performed under local, sedation, or general anesthesia.
Purpose of Endoscopy
- It is used to diagnose diseases of the digestive tract, airways, urinary tract, and joints.
- It helps in biopsy collection of suspicious tissues for histopathological examination.
- It is performed to remove foreign bodies, polyps, or small tumors.
- It is used to control bleeding, such as gastric or esophageal varices.
- It is used to place stents in narrowed passages (e.g., esophagus or bile duct).
Types of Endoscopy
1️⃣ Gastrointestinal (GI) Endoscopy
Upper GI Endoscopy (Esophagogastroduodenoscopy – EGD)
- It is performed to visualize the esophagus, stomach, and duodenum for diagnosing ulcers, gastritis, and tumors.
- It can also be used for therapeutic interventions such as dilation of strictures and control of bleeding varices.
Colonoscopy
- It is used to visualize the entire colon (large intestine) and rectum for screening colon cancer, and detecting polyps or inflammatory bowel disease.
Sigmoidoscopy
- It is a shorter version of colonoscopy used to visualize the sigmoid colon and rectum for diagnosis of hemorrhoids, polyps, and rectal tumors.
2️⃣ Respiratory Tract Endoscopy
- Bronchoscopy is performed to visualize the trachea, bronchi, and lungs.
- It is used to diagnose lung infections, tumors, foreign bodies, and to obtain bronchial washings or biopsy.
- It is also used for therapeutic procedures such as removal of secretions or tumors.
3️⃣ Urinary Tract Endoscopy
- Cystoscopy is performed to visualize the bladder and urethra for diagnosing bladder tumors, stones, strictures, and infections.
- It is also used for removal of small tumors, and placement of ureteric stents.
4️⃣ Joint Endoscopy
- Arthroscopy is performed to visualize the interior of joints, commonly knee, shoulder, elbow, ankle, and hip.
- It is used both for diagnostic purposes (assessing ligament injuries, cartilage damage) and therapeutic procedures (removal of loose bodies, repair of joint structures).
- It offers a minimally invasive alternative to open joint surgery.
5️⃣ Other Types of Endoscopy
- Laparoscopy is used to visualize the abdominal and pelvic organs through small incisions in the abdomen.
- It is used for diagnosing gynecological conditions, appendicitis, endometriosis, and for performing surgeries such as cholecystectomy and hysterectomy.
- Hysteroscopy is performed to visualize the uterine cavity for diagnosing polyps, fibroids, uterine adhesions, and abnormal uterine bleeding.
- It can also be used for therapeutic procedures such as polypectomy or fibroid removal.
Indications for Endoscopy
- Persistent abdominal pain or discomfort.
- Unexplained weight loss.
- Difficulty swallowing (dysphagia).
- Bleeding from gastrointestinal or respiratory tract.
- Persistent diarrhea or constipation.
- Screening for cancer (colon cancer, esophageal cancer).
- Removal of polyps, foreign bodies, or early cancers.
Contraindications of Endoscopy
- Severe cardiac or respiratory instability.
- Uncorrected bleeding disorders.
- Recent myocardial infarction.
- Perforation of the organ being examined.
- Patient’s refusal or non-cooperation.
Complications of Endoscopy
- Bleeding at the site of biopsy or polyp removal.
- Perforation of the organ wall.
- Infection.
- Reaction to sedation or anesthesia.
- Sore throat, nausea, or vomiting after procedure.
Nursing Responsibilities in Endoscopy
1️⃣ Before Procedure
- It is the nurse’s responsibility to obtain informed consent from the patient after explaining the purpose, risks, and procedure of endoscopy.
- The nurse must ensure the patient is kept NPO (nil per os) for at least 6–8 hours before an upper GI endoscopy to prevent aspiration.
- It is the nurse’s role to provide psychological support and alleviate anxiety by explaining what the patient can expect during and after the procedure.
- The nurse should assess patient’s allergy history, particularly to local anesthetics, iodine, or sedatives.
- It is essential to review laboratory values such as coagulation profile, platelet count, and renal function tests before the procedure.
- The nurse should ensure that all pre-procedure checklists are completed, and the patient has voided urine before the procedure.
2️⃣ During Procedure
- It is the nurse’s duty to assist in positioning the patient correctly according to the type of endoscopy being performed (e.g., left lateral for upper GI endoscopy).
- The nurse must closely monitor vital signs, oxygen saturation, and level of consciousness throughout the procedure.
- The nurse should remain vigilant for signs of complications such as respiratory distress, hypotension, or arrhythmias during the procedure.
- It is the nurse’s responsibility to ensure that emergency equipment (oxygen, suction, resuscitation kit) is readily available during the procedure.
- The nurse should provide comfort and reassurance to the patient during conscious sedation.
- The nurse should assist the physician with specimen collection (biopsy) and maintain proper labeling and transport of the specimen to the laboratory.
3️⃣ After Procedure
- It is the nurse’s responsibility to monitor the patient for bleeding, perforation, or aspiration, especially during the immediate post-procedure period.
- The nurse should keep the patient NPO until the gag reflex returns after an upper GI endoscopy to prevent aspiration.
- It is essential for the nurse to observe for abdominal pain, bloating, difficulty breathing, or chest discomfort — signs that may indicate complications.
- The nurse should frequently monitor vital signs and oxygen saturation post-procedure.
- The nurse should provide clear post-procedure instructions, including dietary advice and activity limitations as per medical advice.
- The nurse should educate the patient to report delayed complications such as fever, vomiting blood, or black tarry stools.
- It is the nurse’s duty to document the entire procedure clearly, including patient condition, vital signs, sedation given, and any complications encountered.
b. Fecal studies
Definition
- Fecal studies refer to a group of laboratory tests performed on a stool (feces) sample to evaluate and diagnose gastrointestinal (GI) tract disorders, infections, malabsorption syndromes, and occult (hidden) bleeding.
- It is a non-invasive diagnostic method and is commonly used in clinical settings to assist in diagnosing a variety of GI conditions.
Purpose of Fecal Studies
- It is used to detect the presence of intestinal infections caused by bacteria, viruses, parasites, or fungi.
- It helps in screening for occult (hidden) blood in stool, which may indicate colon cancer or polyps.
- It is used to evaluate malabsorption disorders, such as steatorrhea (fatty stools).
- It assists in identifying inflammatory bowel disease (IBD) such as Crohn’s disease or ulcerative colitis.
- It is used to detect digestive enzyme deficiencies.
- It also helps monitor the effectiveness of treatment for certain GI infections.
Types of Fecal Studies
1️⃣ Fecal Occult Blood Test (FOBT)
- This test detects hidden (occult) blood in the stool that is not visible to the naked eye.
- It is used to screen for colon cancer, polyps, and GI bleeding.
- The test may be done using guaiac-based tests or immunochemical tests (FIT), which have improved sensitivity.
- Multiple stool samples over several days are often required for accurate diagnosis.
2️⃣ Fecal Culture
- It is performed to detect bacterial infections such as Salmonella, Shigella, Campylobacter, and Clostridium difficile.
- The stool sample is cultured in the lab to identify specific pathogens.
- It helps guide antibiotic therapy in cases of infectious diarrhea.
- Fecal culture is also useful in investigating outbreaks of foodborne illness in communities or hospitals.
3️⃣ Ova and Parasite (O&P) Examination
- It is used to identify parasitic infections such as Giardia, Entamoeba histolytica, and helminths (worms).
- Multiple stool samples may be needed as parasites are shed intermittently.
- The test requires special preservation techniques to maintain parasite morphology.
- Concentration and staining techniques are used in the lab to improve the detection rate of parasites.
4️⃣ Fecal Fat Test
- It measures the amount of fat in the stool and is used to diagnose malabsorption syndromes such as celiac disease, chronic pancreatitis, and cystic fibrosis.
- Increased stool fat indicates steatorrhea.
- The test may involve qualitative (Sudan stain) or quantitative measurement of fat excretion over 72 hours.
- It helps assess the effectiveness of pancreatic enzyme replacement therapy in patients with exocrine pancreatic insufficiency.
5️⃣ Fecal Calprotectin and Lactoferrin
- These are inflammatory markers measured in stool.
- Elevated levels suggest inflammatory bowel disease (IBD) such as Crohn’s disease or ulcerative colitis.
- They help differentiate between IBD and irritable bowel syndrome (IBS).
- Fecal calprotectin is also used to monitor disease activity and response to treatment in patients with known IBD.
6️⃣ Other Specialized Tests
- Fecal pH: Used to evaluate carbohydrate malabsorption and lactose intolerance.
- Fecal elastase: Measures pancreatic enzyme activity — low levels suggest exocrine pancreatic insufficiency.
- Fecal DNA testing: Detects DNA mutations associated with colon cancer.
- Fecal DNA testing is a non-invasive screening alternative to colonoscopy for average-risk individuals.
- Fecal reducing substances test: Used to identify carbohydrate malabsorption in infants and children with chronic diarrhea.
Nursing Responsibilities in Fecal Studies
1️⃣ Before Sample Collection
- It is the nurse’s responsibility to explain the purpose, importance, and procedure of fecal study clearly to the patient.
- The nurse must instruct the patient to avoid certain foods (like red meat, beets), vitamin C, and non-steroidal anti-inflammatory drugs (NSAIDs) before the fecal occult blood test (FOBT) to prevent false positive results.
- The nurse should verify doctor’s orders and ensure correct type of stool test is requested (e.g., FOBT, culture, O&P test, fecal fat).
- It is essential to provide the patient with a clean, dry, labeled stool collection container to avoid contamination of the specimen.
- The nurse should assess for any recent barium studies or antibiotic therapy, which may interfere with fecal test results and report this to the physician.
2️⃣ During Collection
- The nurse should educate the patient or caregiver on the correct technique for stool collection, ensuring that the stool does not get contaminated with urine, water, or toilet paper.
- It is the nurse’s responsibility to wear gloves and follow standard precautions to prevent the spread of infection.
- The nurse must verify that the stool sample is of adequate quantity and is free from foreign materials.
- It is important to promptly label the specimen with the patient’s name, identification number, date, and time of collection.
- The nurse should ensure that the specimen is transported to the laboratory immediately or stored correctly (e.g., refrigeration if required) to maintain sample integrity.
- The nurse should reassure the patient and provide privacy and emotional support during the collection process.
3️⃣ After Collection
- The nurse should monitor test results and immediately report any abnormal findings (such as positive occult blood) to the physician.
- It is the nurse’s responsibility to provide post-test instructions and education to the patient regarding diet, hygiene, and any necessary follow-up tests.
- The nurse should document the date, time of collection, patient education provided, and any relevant observations in the patient’s medical record.
- The nurse must ensure proper disposal of used collection equipment according to infection control policies.
- It is important for the nurse to communicate clearly with the laboratory regarding any special handling or urgency required for specific fecal tests (e.g., urgent O&P exam for suspected parasitic infection).
- The nurse should maintain confidentiality of the patient’s health information throughout the testing process.
c. Ultrasonography
Definition
- Ultrasonography (USG) is a non-invasive diagnostic imaging technique that uses high-frequency sound waves to produce real-time images of internal organs, tissues, and blood flow.
- The sound waves are transmitted into the body using a device called a transducer, and the returning echoes are converted into visual images on a monitor.
- It is a safe and painless procedure as it does not involve ionizing radiation like X-rays or CT scans.
Purpose of Ultrasonography
- It helps in the diagnosis of various diseases and monitoring of treatment progress.
- It is widely used in obstetrics to assess fetal growth and development.
- It is used to evaluate abdominal organs such as liver, gallbladder, pancreas, kidneys, and spleen.
- It helps in detecting abnormal fluid collections, cysts, tumors, and stones.
- It is used to assess thyroid gland, breast tissues, and soft tissue masses.
- It helps guide needle aspiration, biopsies, and therapeutic procedures.
Types of Ultrasonography
1️⃣ Obstetric and Gynecologic Ultrasound
- It is used to monitor fetal growth, gestational age, fetal heartbeat, and amniotic fluid volume.
- It helps detect congenital anomalies and monitor high-risk pregnancies.
- It is used to evaluate uterine and ovarian pathologies such as fibroids, cysts, and endometrial thickness.
2️⃣ Abdominal Ultrasound
- It visualizes liver, gallbladder, bile ducts, pancreas, spleen, and kidneys.
- It is useful for diagnosing gallstones, liver cirrhosis, tumors, and hydronephrosis.
- It is often used to guide drainage of abdominal abscesses.
3️⃣ Cardiac Ultrasound (Echocardiography)
- It visualizes the structure and function of the heart chambers and valves.
- It is used to assess cardiac output, ejection fraction, and detect congenital heart diseases.
- It helps evaluate pericardial effusion and cardiac masses.
4️⃣ Thoracic Ultrasound
- It is used to evaluate the pleural cavity for pleural effusion and lung consolidation.
- It helps guide thoracentesis and pleural biopsies.
- It is used in the bedside assessment of critically ill patients.
5️⃣ Vascular Ultrasound (Doppler)
- It assesses blood flow in arteries and veins using Doppler technology.
- It helps detect deep vein thrombosis (DVT) and arterial occlusions.
- It is used to assess carotid artery disease and peripheral vascular disease.
6️⃣ Musculoskeletal Ultrasound
- It evaluates muscles, tendons, ligaments, and joints.
- It is useful in diagnosing soft tissue injuries, tendonitis, bursitis, and joint effusions.
- It can guide injections into joints or soft tissues.
Advantages of Ultrasonography
- It is non-invasive and does not use radiation.
- It provides real-time imaging, allowing assessment of organ motion and blood flow.
- It is portable, making it suitable for use in emergency rooms, ICUs, and bedside exams.
- It is relatively inexpensive compared to CT or MRI.
- It is safe during pregnancy.
Limitations of Ultrasonography
- It is limited in imaging air-filled organs such as lungs or bowel.
- It is operator-dependent — the quality of images depends on the skill of the technician.
- It has limited ability to visualize deep-seated organs in obese patients.
- Bone and air interfere with ultrasound waves, limiting its use for bony structures or lungs.
Nursing Responsibilities in Ultrasonography
1️⃣ Before Procedure
- The nurse should explain the procedure, purpose, and safety of USG to reduce patient anxiety.
- For abdominal ultrasound, the nurse should instruct the patient to fast (NPO) for 6–8 hours to reduce bowel gas and improve image quality.
- For pelvic ultrasound, the nurse should advise the patient to drink water and maintain a full bladder to enhance visualization of pelvic organs.
- The nurse should verify the doctor’s order and check for any contraindications.
- The nurse should review the patient’s previous imaging reports or relevant history to provide necessary clinical background to the radiologist or sonographer.
2️⃣ During Procedure
- The nurse should assist the patient in assuming the correct position on the examination table.
- The nurse should provide privacy and emotional support during the procedure.
- The nurse should monitor for any signs of discomfort or distress.
- The nurse should help in applying ultrasound gel on the skin and ensure the patient is comfortable.
- The nurse should assist in maintaining proper infection control measures during transvaginal or transrectal ultrasound procedures (using sterile covers and gel).
3️⃣ After Procedure
- The nurse should assist the patient in cleaning the gel after the procedure.
- The nurse should observe the patient for any discomfort or adverse reactions.
- The nurse should ensure the patient understands follow-up instructions.
- The nurse should document the procedure and communicate any special findings to the physician.
- The nurse should ensure that the USG report and images are safely sent to the concerned department or attached to the patient’s medical record for further review.
d. CT scan
Definition
- CT scan is a diagnostic imaging procedure that uses a combination of X-rays and computer technology to create detailed cross-sectional images of the body.
- It produces images of bones, soft tissues, blood vessels, and internal organs in greater detail than standard X-rays.
- CT scanning is a non-invasive and painless procedure and can be performed with or without contrast medium.
Purpose of CT Scan
- It helps diagnose a wide range of diseases and conditions.
- It is used to detect tumors, infections, fractures, and vascular diseases.
- It evaluates the extent of injuries in trauma patients.
- It is used to guide biopsies, drainage procedures, and radiation therapy planning.
- It is useful for detecting bleeding, stroke, and brain abnormalities.
- It helps in the staging and monitoring of cancer.
- It provides detailed images for preoperative assessment.
Types of CT Scan
1️⃣ CT Scan of the Head / Brain
- It is used to detect stroke, bleeding, tumors, skull fractures, and hydrocephalus.
- It helps evaluate head injury, headaches, and neurological symptoms.
- It is used to guide neurosurgical procedures.
2️⃣ CT Angiography (CTA)
- It visualizes blood vessels and detects aneurysms, blockages, and vascular malformations.
- It is used to evaluate coronary arteries, pulmonary arteries, and cerebral vessels.
- It helps assess peripheral arterial disease.
3️⃣ Abdominal and Pelvic CT Scan
- It evaluates abdominal organs such as liver, pancreas, kidneys, spleen, and bowel.
- It detects tumors, abscesses, stones, and inflammatory conditions.
- It is used for staging abdominal and pelvic cancers.
4️⃣ CT Chest / Thorax
- It detects lung nodules, masses, pleural effusion, and pulmonary embolism.
- It helps diagnose lung infections such as pneumonia and tuberculosis.
- It is useful in preoperative lung assessment.
5️⃣ CT Scan of Bones and Joints
- It detects fractures, bone tumors, joint abnormalities, and spinal conditions.
- It helps guide orthopedic surgery.
- It provides detailed images of complex fractures.
Advantages of CT Scan
- It provides high-resolution images of various tissues.
- It is a quick and widely available test.
- It can image bone, soft tissue, and blood vessels simultaneously.
- It is useful in emergency situations, such as trauma and stroke.
- It can be performed with contrast to enhance visualization of specific structures.
Limitations of CT Scan
- It exposes the patient to ionizing radiation.
- It may require the use of contrast media, which carries a risk of allergic reactions or kidney damage.
- It may not be suitable for pregnant women.
- It is less effective than MRI in imaging soft tissues of the brain and spinal cord.
Nursing Responsibilities in CT Scan
Before Procedure
- The nurse should explain the procedure, purpose, and possible sensations (such as warmth from contrast injection) to the patient.
- The nurse should assess for allergies to iodine or contrast agents.
- It is important to check renal function tests (serum creatinine, BUN) before administering contrast.
- The nurse should ensure informed consent is obtained.
- The nurse should instruct the patient to be NPO (nothing by mouth) for 4–6 hours before contrast-enhanced CT.
- The nurse should remove metal objects, jewelry, or dentures to avoid image artifacts.
During Procedure
- The nurse should assist the patient in correct positioning on the CT table.
- The nurse should provide privacy and emotional support during the scan.
- The nurse should monitor for any signs of contrast reaction (rash, itching, difficulty breathing).
- The nurse should ensure that emergency equipment is available in case of an anaphylactic reaction.
- The nurse should instruct the patient to remain still and follow breath-hold instructions to ensure clear images.
After Procedure
- The nurse should observe the patient for any delayed allergic reactions to contrast medium.
- The nurse should encourage oral fluid intake to promote contrast elimination from the body.
- The nurse should monitor urine output, especially in patients at risk of contrast-induced nephropathy.
- The nurse should document the procedure and report any adverse events to the physician.
- The nurse should provide follow-up instructions and ensure that the CT report reaches the referring doctor promptly.
e. Cardiac marker studies
Definition
- Cardiac marker studies are laboratory tests that measure specific enzymes, proteins, or molecules released into the blood when the heart muscle is damaged.
- These markers help in the diagnosis, assessment, and monitoring of patients with suspected acute myocardial infarction (AMI) or other cardiac conditions.
- Cardiac markers are an essential component of emergency cardiac care and help guide treatment decisions.
Purpose of Cardiac Marker Studies
- To aid in the early diagnosis of myocardial infarction (heart attack).
- To assess the extent and severity of cardiac muscle injury.
- To differentiate between cardiac and non-cardiac chest pain.
- To monitor progression of cardiac disease or response to therapy.
- To assist in risk stratification of patients with acute coronary syndrome (ACS).
Types of Cardiac Markers
1️⃣ Troponins (Troponin I and Troponin T)
- Troponins are proteins involved in the contractile mechanism of cardiac muscle.
- They are the most specific and sensitive markers for myocardial injury.
- Troponins appear in the blood 3–6 hours after injury, peak at 12–24 hours, and remain elevated for 7–14 days.
- A rise in troponins indicates acute myocardial infarction (AMI) or cardiac muscle damage.
- High-sensitivity troponin (hs-Tn) tests can detect very small amounts of cardiac injury and allow earlier diagnosis.
2️⃣ Creatine Kinase-MB (CK-MB)
- CK-MB is an enzyme isoform specific to cardiac muscle.
- It rises in the blood 4–6 hours after myocardial injury, peaks at 18–24 hours, and returns to normal in 2–3 days.
- CK-MB is useful for detecting reinfarction (second heart attack) in patients with recent MI.
- It is less specific than troponin but still valuable in certain clinical situations.
- Serial measurement of CK-MB helps assess trend and ongoing myocardial damage.
3️⃣ Myoglobin
- Myoglobin is a small oxygen-binding protein found in muscle, including cardiac muscle.
- It is released rapidly after muscle injury, rising within 1–2 hours of MI and peaking at 6–9 hours.
- Myoglobin is a very early marker but is not specific to cardiac muscle — it may be elevated in skeletal muscle injury as well.
- It is mainly used to rule out MI in early stages.
- A normal myoglobin level in the first few hours after chest pain onset is a strong negative predictor for MI.
4️⃣ B-type Natriuretic Peptide (BNP) and NT-proBNP
- BNP and NT-proBNP are hormones released from the ventricles in response to increased pressure and volume overload.
- They are used to diagnose and monitor heart failure.
- Higher BNP levels correlate with worsening heart failure and poor prognosis.
- BNP helps differentiate cardiac from non-cardiac causes of dyspnea.
5️⃣ C-Reactive Protein (CRP) — High Sensitivity (hs-CRP)
- hs-CRP is an inflammatory marker that reflects systemic inflammation.
- It is not specific for myocardial injury but is useful in predicting cardiovascular risk.
- Elevated hs-CRP levels are associated with increased risk of atherosclerosis and coronary artery disease (CAD).
- hs-CRP helps in long-term risk assessment for future cardiac events.
Advantages of Cardiac Marker Studies
- Provides early and accurate diagnosis of myocardial infarction.
- Assists in monitoring therapeutic response and detecting reinfarction.
- Helps in risk stratification and prognosis of cardiac patients.
- Guides clinical decision-making in emergency settings.
- Allows serial measurements to track progression of myocardial injury.
Limitations of Cardiac Marker Studies
- Some markers lack cardiac specificity (e.g., myoglobin).
- Troponin may be elevated in non-ischemic conditions (e.g., renal failure, myocarditis).
- Delay in marker appearance may limit very early diagnosis.
- Elevated markers do not indicate the exact location of myocardial injury.
Nursing Responsibilities in Cardiac Marker Studies
Before Sample Collection
- The nurse should explain the purpose of the test and the importance of timely blood sampling to the patient.
- The nurse should verify doctor’s order and ensure proper test requisition.
- The nurse should assess for any contraindications to venipuncture.
- The nurse should label the sample correctly and record the time of collection accurately.
- The nurse should coordinate with the lab to ensure timely transport of samples, especially for serial marker measurements.
During Collection
- The nurse should perform venipuncture using aseptic technique.
- The nurse should collect samples in the appropriate tube as per laboratory guidelines (e.g., serum separator tube for troponins).
- The nurse should monitor for any signs of bleeding, hematoma, or vasovagal reaction during or after blood draw.
- The nurse should reassure the patient and provide emotional support, especially if the patient is anxious about the diagnosis.
After Collection
- The nurse should observe the patient for post-venipuncture complications.
- The nurse should document time of sample collection and any observations.
- The nurse should monitor and report results promptly to the healthcare team.
- The nurse should assist in preparing the patient for further interventions based on results (e.g., angiography, thrombolysis).
- The nurse should educate the patient and family about the significance of cardiac markers and their role in cardiac care.
Q.3 Define following terms (any three) [6 mark]
a. Tuberculosis
Tuberculosis is a chronic infectious disease caused by the bacterium Mycobacterium tuberculosis, primarily affecting the lungs (pulmonary TB), but it can also involve other organs (extrapulmonary TB), and is characterized by the formation of granulomas, caseous necrosis, and slow progressive symptoms like cough, fever, weight loss, and night sweats.
b. Osteoporosis
Osteoporosis is a chronic skeletal disorder characterized by low bone mass and deterioration of bone tissue, leading to increased bone fragility and a higher risk of fractures, particularly in the spine, hip, and wrist.
c. Alopecia
Alopecia is a condition characterized by partial or complete loss of hair from the scalp or any part of the body, which may be temporary or permanent, and can result from genetic factors, autoimmune disorders, medications, infections, or stress.
d. Epispadiasis
Epispadiasis is a rare congenital defect in which the urethral opening is located on the upper (dorsal) surface of the penis in males, or in the region of the clitoris or along the anterior vaginal wall in females, instead of its normal position, often associated with urinary incontinence and bladder exstrophy.
Section 2
Q.4 Answer the following
a. Define diabetes insipidus (1 mark)
- Diabetes Insipidus is a medical condition in which the body is unable to properly regulate water balance due to either a deficiency of antidiuretic hormone (ADH) or resistance of the kidneys to ADH action.
- It is characterized by the excretion of large volumes of dilute urine (polyuria) and excessive thirst (polydipsia), which can lead to dehydration if fluid intake does not keep up with fluid loss.
b. What are the causes of diabetes insipidus (2 mark)
1️⃣ Central Diabetes Insipidus (Deficient ADH Production)
- Head trauma
- Brain tumors (pituitary or hypothalamic)
- Neurosurgery involving the pituitary gland
- Infections (meningitis, encephalitis)
- Idiopathic (unknown cause)
- Genetic mutations affecting ADH synthesis
2️⃣ Nephrogenic Diabetes Insipidus (Renal Resistance to ADH)
- Genetic defects (in aquaporin-2 or V2 receptor)
- Chronic kidney disease
- Drugs (e.g., lithium, demeclocycline)
- Electrolyte imbalances (hypercalcemia, hypokalemia)
- Post-obstructive uropathy
c. Write down pathophysiology of diabetes insipidus (4 mark)
1️⃣ Normal Mechanism (What happens normally)
- It is the normal process where Antidiuretic Hormone (ADH), also called vasopressin, is released by the posterior pituitary gland.
- It is important to know that ADH binds to receptors on kidney tubules, especially in the collecting ducts, and promotes water reabsorption.
- It is through this mechanism that urine volume is reduced and body water balance is maintained.
2️⃣ Impairment in Diabetes Insipidus
- It is a condition where there is either decreased secretion of ADH (as seen in central or neurogenic DI) or
- It is due to impaired renal response to ADH (as seen in nephrogenic DI).
- It is also important to note that in gestational DI, placental enzymes degrade ADH.
- In all cases, the action of ADH on the kidneys is ineffective, causing water loss.
3️⃣ Failure of Water Reabsorption
- It is because the collecting ducts become impermeable to water when ADH is absent or ineffective.
- It is essential to understand that aquaporin-2 channels are not inserted into the collecting duct membranes, preventing water reabsorption.
- As a result, dilute urine continues to be produced, regardless of the body’s hydration status.
4️⃣ Excessive Water Loss (Polyuria)
- It is this impaired process that causes the kidneys to produce large volumes of hypotonic (dilute) urine.
- It is observed that urine volume can reach up to 3–20 liters/day depending on the severity.
- This chronic loss of free water leads to increased plasma osmolality and hypernatremia if fluid intake is inadequate.
5️⃣ Increased Thirst (Polydipsia)
- It is the body’s compensatory mechanism to prevent dehydration; osmoreceptors in the hypothalamus sense rising plasma osmolality.
- It is this stimulation that causes intense thirst (polydipsia), prompting the person to drink excessive amounts of water.
- If the thirst mechanism is impaired, such as in unconscious patients, the risk of severe dehydration and hypernatremia is very high.
6️⃣ Resulting Fluid and Electrolyte Imbalance
- It is important to note that persistent water loss leads to hemoconcentration, increased blood sodium levels, and hyperosmolar state.
- It is also accompanied by hypovolemia, low blood pressure, dry mucous membranes, and potential shock in severe cases.
- Without adequate treatment, this imbalance can cause neurological symptoms like irritability, seizures, or coma.
d. Write down nursing management of diabetes insipidus (4 mark)
1️⃣ Risk for Fluid Volume Deficit related to polyuria
- Monitor intake and output hourly and document.
- Assess for signs of dehydration: dry mucous membranes, poor skin turgor, hypotension.
- Administer IV fluids as prescribed (hypotonic solutions preferred).
- Encourage oral fluid intake frequently to compensate for losses.
- Monitor daily body weight for early detection of fluid loss.
- Assess vital signs (tachycardia, hypotension) frequently.
- Educate patient to report excessive thirst or increased urine output.
2️⃣ Risk for Electrolyte Imbalance related to excessive water loss
- Monitor serum sodium and potassium levels daily.
- Observe for hypernatremia symptoms: thirst, restlessness, confusion, seizures.
- Administer electrolyte replacements as prescribed.
- Educate patient on the importance of monitoring blood electrolytes regularly.
- Promote balanced nutrition to support electrolyte balance.
- Monitor for cardiac arrhythmias as electrolyte imbalance can affect the heart.
- Ensure fluid intake and electrolyte management is balanced during illness or activity.
3️⃣ Risk for Impaired Skin Integrity related to dehydration and frequent urination
- Perform regular skin assessment, especially over pressure points and perineal area.
- Provide perineal care after each urination to prevent skin breakdown.
- Use protective creams/barrier ointments as needed.
- Encourage wearing loose, breathable clothing to prevent skin irritation.
- Keep skin clean and dry; change wet garments promptly.
- Reposition immobile patients every 2 hours to prevent pressure sores.
- Maintain adequate nutrition to promote skin healing and integrity.
4️⃣ Deficient Knowledge related to disease process and management
- Explain the nature of Diabetes Insipidus and its chronic nature.
- Teach proper medication administration (desmopressin/DDAVP, if prescribed).
- Educate about early signs of dehydration and when to seek medical attention.
- Encourage consistent fluid intake during illness, heat, or travel.
- Explain the importance of routine follow-up visits and lab tests.
- Involve family in education and support, especially for elderly or dependent patients.
- Provide written discharge instructions regarding self-monitoring and emergency signs.
Or
Q.4 Answer the following
a. Describe history taking process for skin disorder (3 mark)
It is a very important step where the nurse collects detailed information about the patient’s skin problem, general health, and lifestyle factors, which helps in diagnosing and planning treatment.
1️⃣ Identification Data
- It is necessary to begin by recording the patient’s name, age, gender, occupation, address, and contact information.
- It is also important to mention if the patient works in environments that may expose them to allergens or irritants.
2️⃣ Chief Complaints
- It is very important to ask the patient to describe their main skin-related problem in their own words.
- The nurse should note when the problem started, the nature of the lesions (rash, itching, swelling, ulcer, discoloration), and whether it is localized or generalized.
- It is also helpful to ask about any associated symptoms, such as pain, burning, scaling, bleeding, or discharge.
3️⃣ History of Present Illness
- It is essential to collect a detailed chronological history of how the skin problem evolved.
- The nurse should inquire about duration, progression, frequency, intensity, and any factors that aggravate or relieve the condition.
- It is important to ask about previous episodes of similar complaints.
- It is also useful to find out about previous treatments tried (topical creams, home remedies, medications) and their effectiveness.
4️⃣ Past Medical History
- It is necessary to ask about any previous illnesses or skin conditions such as eczema, psoriasis, dermatitis, or skin infections.
- It is also important to inquire about systemic diseases that may affect the skin, like diabetes, thyroid disease, liver disease, or autoimmune disorders.
- The nurse should ask about any history of allergies or known triggers.
5️⃣ Family History
- It is important to explore if there is a family history of skin diseases, such as psoriasis, atopic dermatitis, vitiligo, or autoimmune skin conditions.
- It is useful to know about hereditary patterns to aid in diagnosis.
6️⃣ Personal and Social History
- It is important to gather information about personal habits, such as bathing frequency, skin care routine, cosmetic use, and exposure to sun or chemicals.
- The nurse should ask about smoking, alcohol consumption, and nutritional status.
- It is also essential to ask about occupational hazards and exposure to allergens or infectious agents.
- The patient’s mental health status should also be considered, as stress can worsen some skin disorders.
7️⃣ Drug History
- It is very important to ask about current and past medications, including prescribed drugs, over-the-counter medications, and herbal or traditional remedies.
- The nurse should inquire about any history of drug allergies or adverse skin reactions to medications.
8️⃣ Environmental History
- It is essential to ask about any recent travel, change in climate, or contact with infected persons.
- It is also important to inquire about use of new soaps, detergents, clothing materials, or pets at home that may contribute to skin issues.
9️⃣ Psychosocial History
- It is helpful to assess the psychological impact of the skin disorder, including feelings of embarrassment, anxiety, depression, or social isolation.
- The nurse should also inquire about coping mechanisms and support systems available to the patient.
10️⃣ Summary and Clarification
- It is important for the nurse to summarize the key points of the history and clarify any doubts with the patient.
- It is also helpful to document all findings accurately and maintain confidentiality.
b. Write down physical examination for skin disorder (4 mark)
It is an essential part of the skin assessment process where the nurse or healthcare provider systematically observes and palpates the skin to identify any abnormalities in appearance, texture, or function.
1️⃣ General Inspection of the Skin
- It is important to start with a general inspection of the entire skin surface under good lighting.
- The nurse should look for any visible lesions, rashes, discolorations, dryness, or abnormal growths.
- It is also necessary to note whether the lesions are localized or generalized and whether they are symmetrical or asymmetrical.
2️⃣ Color of the Skin
- It is crucial to observe the color of the skin, as this can provide important diagnostic clues.
- The nurse should check for pallor, cyanosis, erythema, jaundice, or hyperpigmentation.
- It is also helpful to look for vitiligo, ecchymosis, or purpura.
3️⃣ Moisture Level
- It is important to assess the moisture content of the skin.
- The nurse should check whether the skin is excessively dry (xerosis) or overly moist, which could indicate sweating disorders or infections.
4️⃣ Temperature of the Skin
- It is necessary to palpate the skin to assess its temperature.
- The nurse should compare bilateral areas to check for warmth (which may indicate infection or inflammation) or coolness (which may suggest vascular insufficiency).
5️⃣ Texture of the Skin
- It is essential to evaluate the texture of the skin by gently palpating it.
- The nurse should note whether the skin feels smooth, rough, thickened (lichenification), thin, or leathery.
6️⃣ Turgor and Elasticity
- It is important to assess skin turgor to evaluate hydration status.
- The nurse should gently pinch the skin (usually on the forearm or sternum) and observe how quickly it returns to normal.
- Poor skin turgor is a sign of dehydration or aging.
7️⃣ Presence of Lesions
- It is necessary to thoroughly examine and describe any skin lesions present.
- The nurse should document the type of lesion (macule, papule, nodule, vesicle, pustule, plaque, ulcer), size, shape, color, border, distribution, and any associated features such as scaling or crusting.
- It is also helpful to check for secondary changes like excoriation or scarring.
8️⃣ Edema Assessment
- It is important to check for presence of edema.
- The nurse should palpate for pitting or non-pitting edema, and document its location and severity.
9️⃣ Examination of Hair
- It is necessary to inspect the scalp and hair for texture, quantity, distribution, and presence of lesions or infestations.
- The nurse should note any hair thinning, alopecia, dandruff, or scalp infections.
1️⃣0️⃣ Examination of Nails
- It is important to examine the nails for color, shape, thickness, and integrity.
- The nurse should observe for clubbing, spoon nails (koilonychia), pitting, ridging, or discoloration, which may be indicators of systemic diseases.
1️⃣1️⃣ Examination of Mucous Membranes
- It is essential to inspect the oral mucosa, lips, tongue, and conjunctivae.
- The nurse should look for pallor, cyanosis, ulcers, or pigmentary changes.
c. What are the different diagnosis test for skin disorder (4 mark)
It is very important to understand that a variety of diagnostic tests are used to identify and differentiate skin disorders, assess their severity, and guide appropriate treatment.
1️⃣ Physical Examination
- It is the first step where the healthcare provider conducts a detailed inspection and palpation of the skin, noting the type of lesion, distribution, color, texture, and presence of scales, ulcers, or nodules.
- It is essential to also examine the hair, nails, and mucous membranes.
2️⃣ Skin Biopsy
- It is a procedure where a small sample of skin tissue is removed for microscopic examination.
- It is used to diagnose skin cancers, chronic inflammatory skin conditions, infections, and autoimmune skin diseases.
- Different types include punch biopsy, excisional biopsy, and shave biopsy.
3️⃣ Patch Testing
- It is a test performed to identify allergens responsible for contact dermatitis.
- It is done by applying patches containing common allergens to the skin (usually the back) and observing for delayed hypersensitivity reactions after 48–72 hours.
4️⃣ Skin Prick Test (Allergy Testing)
- It is a test used to diagnose immediate-type allergic reactions (Type I hypersensitivity), such as those caused by pollens, dust mites, foods, or animal dander.
- It is done by applying a small drop of allergen extract to the skin and pricking it to observe for immediate wheal and flare reaction.
5️⃣ Wood’s Lamp Examination
- It is a diagnostic test where ultraviolet (UV) light is used to examine the skin.
- It is helpful in identifying fungal infections, bacterial infections, pigmentary disorders (such as vitiligo), and some skin tumors by observing fluorescence.
6️⃣ Tzanck Smear
- It is a microscopic test used to diagnose viral skin infections, particularly herpes simplex and varicella-zoster infections.
- It involves scraping the base of a vesicle and staining the cells to look for multinucleated giant cells.
7️⃣ Potassium Hydroxide (KOH) Preparation
- It is a simple test used to detect fungal infections of the skin, hair, or nails.
- A scraping of the lesion is treated with KOH, which dissolves keratin and allows fungal elements (hyphae) to be seen under a microscope.
8️⃣ Gram Stain and Bacterial Culture
- It is a laboratory test used to identify bacterial infections of the skin.
- A sample from a pustule or wound is stained and cultured to determine the bacterial species and guide antibiotic therapy.
9️⃣ Viral Culture and Polymerase Chain Reaction (PCR)
- It is a diagnostic method used to identify viral pathogens in skin lesions, such as herpes viruses or human papillomavirus (HPV).
- PCR is highly sensitive and can detect viral DNA in a skin sample.
10️⃣ Dermoscopy (Dermatoscopy)
- It is a non-invasive imaging technique where a dermatoscope (magnifying device with polarized light) is used to examine skin lesions.
- It is especially useful in the evaluation of pigmented lesions, melanomas, and vascular lesions.
11️⃣ Blood Tests
- It is important to conduct blood tests when systemic skin diseases are suspected.
- Tests may include complete blood count (CBC), autoantibody screening (such as ANA for lupus), thyroid function tests, liver and kidney function tests, and serologic tests for infections.
12️⃣ Skin Scrapings for Parasites
- It is a test performed by scraping the skin to identify ectoparasites like scabies mites or lice under the microscope.
Q.5 Write short notes on (any four) [20 mark]
a. OT design
It is the planned and systematic layout of the operation theatre, which ensures a safe, sterile, and efficient environment for performing surgical procedures.
1️⃣ Purpose of OT Design
- It is designed to maintain strict sterility and reduce the risk of infection during surgery.
- It is also intended to provide an environment that ensures patient safety, comfort for surgical teams, and optimum workflow.
2️⃣ Location of OT
- It is generally recommended to place the OT in a strategic location within the hospital, ideally close to ICU and emergency departments for quick patient transfer.
- It is usually kept in a separate, controlled zone to minimize traffic and contamination.
3️⃣ Zoning of OT Complex
- It is important to know that modern OT design is based on a zoning system to maintain aseptic conditions:
a) Protective Zone
- It is the outer zone of the OT complex, including changing rooms, waiting areas, and administrative offices.
- It is where staff and patients are prepared before entering the sterile areas.
b) Clean Zone
- It is the intermediate zone that includes preoperative areas, storage rooms, and scrub stations.
- It helps reduce the risk of contaminants entering the sterile area.
c) Sterile Zone
- It is the innermost zone where actual surgeries are performed.
- It consists of the operating room(s), sterile supply areas, and instrument preparation zones.
- Strict aseptic techniques are maintained here.
d) Disposal Zone
- It is the area for waste disposal and decontamination after surgery.
- Used instruments and materials are processed here.
4️⃣ Design of the Operating Room
- It is essential to ensure that the operating room has adequate space to accommodate surgical equipment, staff, and patient care devices.
- The size of an operating room is usually around 400–600 square feet depending on the type of surgeries performed.
- It is recommended that walls, ceilings, and floors be made of smooth, seamless, and washable materials to prevent contamination.
- The room should have proper ventilation, usually with HEPA filters and positive pressure airflow, to ensure clean air circulation.
- It is important to install adequate lighting, including shadowless operating lights directly over the surgical field.
- It is also necessary to ensure that electrical outlets and gas pipelines (oxygen, nitrous oxide, suction) are safely and conveniently placed.
5️⃣ Ventilation System
- It is crucial that the OT has a well-designed ventilation system to maintain positive air pressure, which prevents contaminated air from entering the sterile zone.
- It is recommended to maintain 20–25 air changes per hour with HEPA filtration.
- It is also important to maintain the temperature (20–24°C) and humidity (50–60%) at appropriate levels.
6️⃣ OT Traffic Control
- It is important to control traffic flow in and out of the OT to minimize contamination risk.
- There should be dedicated entry and exit points for staff and equipment.
- It is advised to have restricted access to the sterile zone, with strict adherence to gowning and hand hygiene protocols.
7️⃣ Essential Components of OT Design
- The following elements must be included in the OT design:
- Operating table → Adjustable, radiolucent table for surgical procedures.
- Shadowless lights → For optimal illumination of the surgical field.
- Anesthesia machine → For safe administration of anesthesia.
- Surgical instrument trolley → To hold sterile surgical instruments.
- Suction apparatus → For clearing blood and secretions during surgery.
- Monitors and displays → For continuous patient monitoring.
- Handwashing stations → With elbow-operated taps near the entry to the sterile zone.
8️⃣ Safety Features
- It is important to include fire safety measures, including fire-resistant materials and accessible fire extinguishers.
- Electrical systems should be isolated and grounded to prevent electrical hazards.
- Adequate backup power supply must be ensured to avoid interruptions during surgery.
b. Anesthesia
Definition
- It is defined as a temporary and controlled loss of sensation or awareness, which is produced by administering anesthetic agents through various routes.
- It is used to allow patients to undergo surgical procedures or painful diagnostic interventions without discomfort or memory of the event.
Purpose of Anesthesia
- It is mainly given to relieve pain (analgesia), to prevent awareness during the procedure (amnesia), and to achieve muscle relaxation for better surgical access.
- It also helps in maintaining patient safety, physiological stability, and psychological comfort during invasive procedures.
Types of Anesthesia
It is classified into four major types based on the extent of sensation loss and the method of administration:
a) General Anesthesia
- It is a type of anesthesia that causes complete loss of consciousness and total body sensation, rendering the patient unaware and unresponsive.
- It is administered through inhalational agents or intravenous drugs.
- It is used for major surgical procedures such as abdominal, thoracic, cardiac, or neurological surgeries.
b) Regional Anesthesia
- It is a technique where sensation is blocked in a specific region of the body by administering anesthetic agents near nerve pathways.
- It includes:
- Spinal anesthesia → Injected into the subarachnoid space to block lower body sensation.
- Epidural anesthesia → Injected into the epidural space, used for labor analgesia and lower limb surgeries.
- Nerve block → Injected around a specific nerve or nerve plexus to block sensation in a targeted body area.
c) Local Anesthesia
- It is a type of anesthesia that produces loss of sensation in a small, localized area without affecting consciousness.
- It is often used for minor surgical or dental procedures, wound suturing, or skin biopsies.
d) Conscious Sedation (Monitored Anesthesia Care)
- It is a controlled state of depressed consciousness where the patient is relaxed but awake and can respond to commands.
- It is used for procedures such as endoscopy, minor orthopedic interventions, and diagnostic imaging.
Stages of General Anesthesia
- It is important to know that general anesthesia progresses through four stages:
- Stage I (Analgesia) → The patient experiences pain relief and drowsiness but is still conscious.
- Stage II (Excitement) → The patient may show irregular breathing, involuntary movements, and increased heart rate.
- Stage III (Surgical Anesthesia) → The patient reaches a state of deep unconsciousness, suitable for surgical procedures; reflexes are lost and muscles are relaxed.
- Stage IV (Overdose) → It is a dangerous stage of respiratory and cardiovascular depression, which must be avoided.
Common Complications of Anesthesia
- It is necessary to monitor the patient for the following complications:
- Nausea and vomiting postoperatively are very common.
- Sore throat may occur due to intubation.
- Allergic reactions to anesthetic agents may develop.
- Respiratory depression and hypotension may occur if anesthesia is not well balanced.
- In rare cases, malignant hyperthermia, a life-threatening condition, can develop.
- Awareness during anesthesia is a rare but concerning complication that should be avoided through proper dosing.
1️⃣ Pre-Anesthesia Responsibilities
- It is important for the nurse to conduct a complete pre-anesthetic assessment, including medical history, allergies, current medications, previous anesthesia experiences, and baseline vital signs.
- It is the nurse’s duty to verify that the patient has maintained NPO status (nothing by mouth) for the required number of hours to prevent aspiration risk during anesthesia.
- It is important to obtain informed consent for the procedure and anesthesia and ensure that all consent forms are correctly signed and documented.
- The nurse should provide emotional support and psychological preparation, addressing any fears or concerns expressed by the patient.
- It is necessary to ensure that jewelry, dentures, contact lenses, makeup, and nail polish are removed before shifting the patient to the operating room.
2️⃣ Intra-Anesthesia Responsibilities
- It is the nurse’s responsibility to assist the anesthetist during induction, maintenance, and emergence from anesthesia.
- It is very important for the nurse to continuously monitor vital signs, including heart rate, respiratory rate, blood pressure, oxygen saturation, and ECG readings, throughout the procedure.
- It is essential to observe the patient for signs of anesthesia complications, such as allergic reactions or respiratory depression.
- The nurse should assist in airway management, including positioning, suctioning, and providing oxygen as required.
- It is necessary to maintain aseptic technique to prevent infection during the procedure.
3️⃣ Post-Anesthesia Responsibilities
- It is important to transfer the patient to the Post-Anesthesia Care Unit (PACU) safely and position the patient to maintain an open airway (often in the lateral position initially).
- The nurse must perform frequent monitoring of vital signs until the patient is fully awake and stable.
- It is necessary to assess the patient for return of protective reflexes (gag, cough) and readiness for oral intake.
- The nurse should manage pain effectively by administering prescribed analgesics and evaluating their effectiveness.
- It is essential to monitor for postoperative nausea and vomiting and administer antiemetic medications if prescribed.
- The nurse should encourage early ambulation when appropriate to prevent complications such as deep vein thrombosis (DVT) and atelectasis.
c. Fracture
Definition of Fracture
- Fracture is defined as a break or disruption in the continuity of a bone, either partial or complete.
- It may occur due to direct trauma, twisting injury, repetitive stress, or disease-related weakness.
- Fracture healing depends on factors such as age, nutritional status, and blood supply to the bone.
Etiology
- Trauma / injury (fall, accident)
- Osteoporosis
- Bone tumors
- Overuse / stress fractures
- Congenital bone diseases
Types of Fracture
1️⃣ Closed (Simple) Fracture
- The bone breaks but does not pierce the skin.
- It is less prone to infection.
- Example: Hairline fracture of tibia after a fall.
2️⃣ Open (Compound) Fracture
- The broken bone end protrudes through the skin, causing an open wound.
- It carries a high risk of infection and requires urgent surgical care.
- Example: Compound fracture of femur in a road traffic accident.
3️⃣ Comminuted Fracture
- The bone is shattered into multiple fragments.
- It usually results from high-energy trauma such as car crashes.
- Example: Comminuted fracture of femur after a crush injury.
4️⃣ Greenstick Fracture
- One side of the bone bends, while the other side breaks.
- It is commonly seen in children due to soft, flexible bones.
- Example: Greenstick fracture of radius in a child after a playground fall.
5️⃣ Transverse Fracture
- The fracture line is horizontal across the bone.
- It occurs commonly due to direct blow or bending forces.
- Example: Transverse fracture of the humerus after a direct fall.
6️⃣ Oblique Fracture
- The fracture line runs at an angle across the bone.
- It is caused by a rotational or twisting force.
- Example: Oblique fracture of fibula due to sports injury.
7️⃣ Spiral Fracture
- The bone is twisted apart, producing a helical fracture line.
- It is commonly caused by rotational forces, often in sports.
- Example: Spiral fracture of tibia from skiing accident.
8️⃣ Impacted Fracture
- The broken ends of the bone are driven into each other.
- It is commonly seen in arm or leg injuries due to falls.
- Example: Impacted fracture of femoral neck in an elderly patient.
9️⃣ Compression Fracture
- The bone is compressed or crushed, leading to collapse.
- Commonly occurs in vertebrae of elderly patients with osteoporosis.
- Example: Compression fracture of thoracic vertebrae in an osteoporotic patient.
10️⃣ Pathological Fracture
- It occurs in a bone weakened by disease, such as cancer, infection, or osteoporosis.
- It may happen with minimal trauma or spontaneously.
- Example: Pathological fracture of femur in a patient with bone metastasis.
Clinical Manifestations
- Pain at the fracture site
- Swelling and bruising
- Deformity or abnormal positioning
- Loss of function or movement
- Crepitus (grating sound on movement)
- Shortening of the affected limb
Diagnostic Evaluation
- History collection
- Physical examination
- X-ray (confirm fracture and type)
- CT scan / MRI for complex fractures
- Bone scan for stress fractures
- CBC if blood loss suspected
Medical Management of Fracture
1️⃣ Initial Assessment & Stabilization
- The patient is assessed for life-threatening injuries (ABCs) first.
- The fractured limb is immobilized using splints or traction to prevent further damage.
- Neurovascular checks are done frequently.
2️⃣ Pain Management
- Analgesics such as paracetamol, NSAIDs, or opioids are used as needed.
- Positioning and cold application help reduce pain and swelling.
3️⃣ Reduction of Fracture
- Closed reduction is performed for simple fractures under sedation or anesthesia.
- Open reduction is required for complex or displaced fractures, followed by internal fixation.
4️⃣ Immobilization
- It includes cast application, splinting, or external fixation.
- Immobilization duration depends on type of fracture, age, and healing potential.
5️⃣ Surgery (ORIF)
- Open reduction and internal fixation are used for unstable fractures.
- Devices such as plates, screws, intramedullary rods, or external fixators are used to maintain alignment.
6️⃣ Rehabilitation
- Physical therapy begins with range of motion (ROM) exercises as soon as possible.
- It helps in preventing stiffness, muscle atrophy, and regaining strength.
7️⃣ Prevention of Complications
- Measures include infection control, DVT prophylaxis, and pressure ulcer prevention.
- The patient is monitored for compartment syndrome and delayed union or nonunion of the fracture.
Nursing Management of Fracture Patient
1️⃣ Pain Management
- Pain level is assessed regularly using a pain scale.
- The nurse provides analgesics as prescribed and ensures comfortable limb positioning.
- Cold packs are applied in the acute phase to reduce swelling.
2️⃣ Immobilization Care
- The nurse ensures the cast or splint is properly positioned and not too tight.
- Frequent neurovascular checks (pulse, color, sensation, temperature, capillary refill) are performed.
- The patient is educated on cast care and signs of complications.
3️⃣ Prevention of Infection
- Aseptic technique is maintained during dressing changes.
- The surgical wound is monitored for redness, warmth, drainage, and foul odor.
- The patient is taught about personal hygiene and wound care.
4️⃣ Monitoring for Complications
- The nurse observes for deep vein thrombosis (DVT) signs, such as leg pain or swelling.
- Monitoring includes checking for pressure ulcers in immobilized patients.
- The nurse is alert for signs of fat embolism syndrome (dyspnea, confusion, petechiae).
5️⃣ Mobility and Rehabilitation
- The patient is encouraged to begin passive and active exercises as per doctor’s advice.
- The nurse assists with gradual ambulation when allowed.
- Coordination with physiotherapists is done to optimize recovery.
6️⃣ Nutritional Support
- The nurse ensures a diet rich in calcium, protein, and vitamin D to promote bone healing.
- Adequate fluid intake is encouraged to prevent constipation related to immobility.
- The patient is monitored for nutritional deficiencies.
7️⃣ Patient and Family Education
- The nurse teaches the patient about fracture healing, cast care, and activity restrictions.
- The family is educated about signs of infection, circulation problems, and when to seek help.
- The nurse emphasizes the importance of completing rehabilitation and attending follow-up visits.
d. Diptheria
Definition
Diphtheria is an acute, contagious bacterial infection caused by Corynebacterium diphtheriae, which primarily affects the mucous membranes of the throat and nose, producing a toxin that can cause systemic effects, particularly damage to the heart and nervous system.
Causative Agent
- Corynebacterium diphtheriae (gram-positive, non-motile, club-shaped bacillus)
- Toxigenic strains produce exotoxin responsible for systemic toxicity
Mode of Transmission
- Droplet infection (coughing, sneezing)
- Direct contact with respiratory secretions, skin lesions
- Fomites (rare)
Incubation Period
Typically 2 to 5 days
Pathophysiology
- Corynebacterium diphtheriae enters through the respiratory tract.
- Bacteria attach to mucosa and produce exotoxin.
- Toxin inhibits protein synthesis by blocking EF-2.
- Causes local cell death and necrosis.
- Pseudomembrane forms over tonsils/throat.
- Toxin enters bloodstream, spreads systemically.
- Affects heart (myocarditis), nerves (neuritis), and kidneys (tubular damage).
Clinical feature
- Sore throat and mild fever
- Thick grayish-white pseudomembrane over tonsils, pharynx, or larynx
- Difficulty swallowing (dysphagia)
- Hoarseness or voice change
- “Bull neck” appearance due to swollen lymph nodes and neck edema
- Breathing difficulty (if airway is blocked)
- Foul-smelling breath
Diagnostic Evaluation
- History collection
- Physical examination
- Throat swab culture on Löffler’s or tellurite medium
- Elek’s test for toxin detection
- PCR for gene encoding diphtheria toxin
- CBC : leukocytosis
Management
Diphtheria Antitoxin (DAT)
Diphtheria Antitoxin (DAT) is administered immediately to neutralize the circulating diphtheria toxin — it is the most important early treatment and should be given even before lab confirmation.
Antibiotic therapy
Antibiotic therapy is initiated with Penicillin G or Erythromycin for 14 days to eradicate the bacteria and prevent further toxin production.
Airway monitoring and supportive care
Airway monitoring and supportive care are provided — nurses should watch for signs of airway obstruction, be prepared for emergency airway management, and implement strict isolation to prevent the spread of infection.
Nursing management
- Maintain airway patency; monitor for signs of airway obstruction
- Administer oxygen therapy as needed
- Give prescribed antibiotics and diphtheria antitoxin promptly
- Monitor for signs of myocarditis (e.g., arrhythmias, chest pain)
- Maintain strict isolation precautions to prevent spread
- Provide nutritional support – soft, high-calorie diet
- Monitor fluid and electrolyte balance
- Educate patient and caregivers about hygiene and infection control
- Provide psychological support to reduce anxiety
- Observe for neurological complications (e.g., paralysis, cranial nerve involvement)
- Perform frequent oral care to prevent secondary infection in the throat
- Position patient in semi-Fowler’s to ease breathing
- Assist with suctioning if excessive secretions present
- Keep emergency airway equipment (e.g., tracheostomy tray) ready
- Encourage bed rest during the acute phase to prevent cardiac stress
Complications
- Myocarditis
- Respiratory failure
- Peripheral neuritis (e.g., palatal or limb paralysis)
- Renal failure
- Death (due to airway obstruction or toxin effects)
e. Nephrosis
Definition
Nephrosis (also known as Nephrotic Syndrome) is a non-inflammatory kidney disorder characterized by massive proteinuria (3.5 g/day), hypoalbuminemia, hyperlipidemia, and edema, due to damage to the glomerular filtration barrier.
Etiology
1. Primary (Idiopathic) Causes
- Minimal Change Disease (common in children)
- Focal Segmental Glomerulosclerosis (FSGS)
- Membranous Nephropathy
2. Secondary Causes
- Diabetes mellitus
- Systemic Lupus Erythematosus (SLE)
- Infections – Hepatitis B, Hepatitis C, HIV, Malaria
- Drugs – NSAIDs, gold salts, penicillamine
- Malignancies – Lymphoma, leukemia, solid tumors
- Amyloidosis
Pathophysiology
- Injury to glomerular podocytes and basement membrane.
- Increased glomerular permeability to proteins.
- Loss of albumin in urine (proteinuria).
- Decreased plasma oncotic pressure → edema.
- Liver compensates by increasing lipoprotein synthesis → hyperlipidemia.
Clinical manifestations
- Edema (periorbital, pedal, generalized)
- Frothy urine (due to proteinuria)
- Hypoalbuminemia
- Hyperlipidemia & lipiduria
- Weight gain
- Fatigue & weakness
- Oliguria (less urine output)
- Recurrent infections
- Thromboembolic risk (e.g., DVT)
- Mild hypertension
Diagnostic Evaluation
- History collection
- Physical examination
- Urine analysis – massive proteinuria
- Serum albumin – low
- Serum cholesterol & triglycerides – high
- Renal function tests
- Renal biopsy (to identify the underlying cause)
Management
Corticosteroids
Corticosteroids such as Prednisolone are the first-line treatment, especially in children with minimal change disease, as they help reduce inflammation and protein loss through the kidneys.
Diuretics
Diuretuics like Furosemide are prescribed to manage fluid overload and reduce edema by promoting excretion of excess water through the urine.
Angiotensin-converting enzyme (ACE)
(ACE) inhibitors or Angiotensin II receptor blockers (ARBs), such as Enalapril or Losartan, are used to reduce intraglomerular pressure and minimize proteinuria.
Statins
Statins like Atorvastatin may be given to manage hyperlipidemia associated with nephrotic syndrome and reduce cardiovascular risk.
Anticoagulants
Anticoagulant such as Heparin or Warfarin are considered if the patient has a high risk of thromboembolic events, as nephrosis can create a hypercoagulable state.
In steroid-resistant cases
In this cases immunosuppressive drugs such as Cyclophosphamide, Cyclosporine, or Tacrolimus are administered to control the underlying immune-mediated damage to the glomeruli.
Dietary management
It includes a moderate intake of protein to replace urinary losses without overburdening the kidneys, a low-sodium diet to control edema, and adequate calorie intake to maintain nutritional status.
Nursing management
- Monitor vital signs, daily weight, and intake/output (I/O)
- Assess and document edema (periorbital, pedal, sacral)
- Administer prescribed medications (steroids, diuretics, ACE inhibitors)
- Maintain low-sodium and moderate-protein diet
- Prevent infection with proper hygiene and isolation if needed
- Watch for signs of thromboembolism (e.g., leg pain, swelling)
- Educate about disease, medication adherence, and follow-up
- Provide emotional and psychological support to patient and family
- Monitor for adverse drug reactions (GI upset, immune suppression)
- Promote adequate rest and activity balance
- Encourage fluid restriction if ordered by physician
- Support skin care to prevent breakdown due to edema
- Encourage compliance with lab tests (urine protein, serum albumin, lipids)
- Coordinate with dietitian and social worker for holistic care
- Maintain aseptic technique during any invasive procedures
Complications
- Acute kidney injury
- Infections (peritonitis, cellulitis)
- Thromboembolism (DVT, renal vein thrombosis)
- Hypertension
- Chronic kidney disease
Q.6 Define following terms (any three) [6 mark]
a. Tracheostomy
Tracheostomy is a surgical procedure that involves creating an opening (stoma) in the anterior wall of the trachea (windpipe) to insert a tracheostomy tube, allowing direct access to the airway for breathing, suctioning, or mechanical ventilation, especially in cases of airway obstruction, respiratory failure, or prolonged intubation.
b. Hypophysectomy
Hypophysectomy is a surgical procedure involving the removal of the pituitary gland (hypophysis), usually performed to treat pituitary tumors, Cushing’s disease, or other hormonal disorders, and is commonly done through a transsphenoidal (nasal) approach or sometimes via a craniotomy.
c. Cystectomy
Cystectomy is a surgical procedure involving the removal of all or part of the urinary bladder, most commonly performed to treat bladder cancer, and may be classified as partial cystectomy (removal of a portion) or radical cystectomy (removal of the entire bladder along with surrounding structures like lymph nodes, prostate in males, or uterus in females).
d. Emphysema
Emphysema is a chronic obstructive pulmonary disease (COPD) characterized by permanent enlargement and destruction of the alveoli (air sacs) in the lungs, leading to reduced surface area for gas exchange, air trapping, and progressive breathlessness.
