21/01/2019-B.SC-MEDICAL SURGICAL-2-UPLOAD-PAPER NO.2
ADULT HEALTH NURSING PAPER SOLUTION NO.2
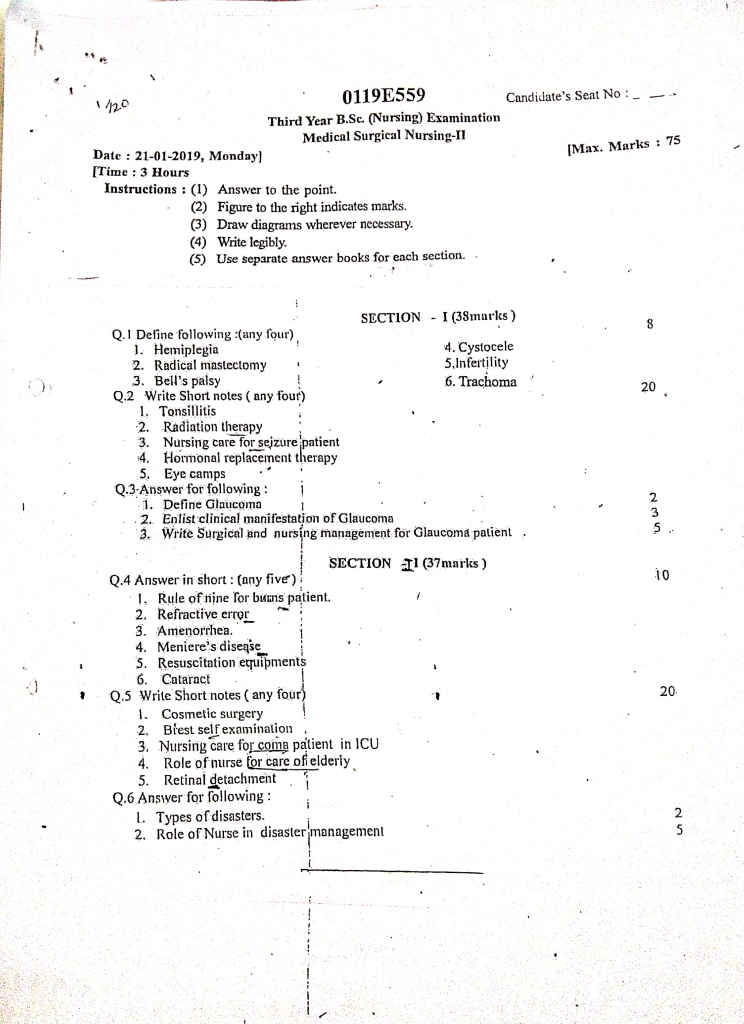
Section 1 (38 mark)
Q.1 Define following (any four) (8 mark)
1. Hemiplagia
- Hemiplegia is a neurological condition characterized by complete paralysis or severe weakness affecting one side of the body (either right or left).
- It usually results from damage to the brain or spinal cord due to conditions such as stroke, traumatic brain injury, brain tumor, or cerebral palsy.
- The affected side may experience loss of motor function, muscle control, and coordination.
2. Radical mastectomy
- Radical mastectomy is a surgical procedure performed for the treatment of breast cancer in which the entire breast tissue, underlying chest muscles (pectoralis major and minor), and nearby lymph nodes (usually axillary lymph nodes) are removed.
- It is considered an extensive type of breast surgery used when cancer has spread to surrounding tissues.
- Although now largely replaced by less invasive procedures, it is still used in advanced or recurrent cases.
3. Bells palsy
- Bell’s palsy is a sudden, temporary weakness or paralysis of the muscles on one side of the face due to inflammation or compression of the facial nerve (7th cranial nerve).
- It usually occurs without warning and affects facial expressions, eyelid movement, and sometimes taste sensation.
- The exact cause is unknown, but viral infections (like herpes simplex) are often linked.
4. Cystocele
- Cystocele is a medical condition in which the wall between a woman’s bladder and her vagina weakens, allowing the bladder to bulge or herniate into the vaginal canal.
- It is also referred to as anterior vaginal wall prolapse and is commonly caused by childbirth, heavy lifting, chronic coughing, or aging.
- It may result in urinary problems, discomfort, or a sensation of fullness in the pelvic area.
5. Infertility
Infertility is defined as the inability of a couple to conceive a child after one year of regular, unprotected sexual intercourse, or the inability to carry a pregnancy to a live birth. It can result from factors affecting the male, female, or both partners, including hormonal imbalances, anatomical problems, infections, or lifestyle factors. It is classified into :
Primary infertility : When a couple has never been able to conceive.
Secondary infertility : When a couple has conceived at least once but is now unable to conceive again.
6. Trachoma
- Trachoma is a chronic contagious eye infection caused by the bacterium Chlamydia trachomatis, which primarily affects the conjunctiva and cornea.
- It is characterized by repeated episodes of inflammation, leading to scarring of the inner eyelid, inward turning of the eyelashes (trichiasis), and potential corneal blindness.
- It is a major public health problem in many developing countries, particularly in areas with poor sanitation and limited access to clean water. It is the leading infectious cause of preventable blindness worldwide.
Q.2 Write short notes (any four) (20 marks)
1. Tonsilitis
Definition
- It is an acute or chronic inflammation and infection of the palatine tonsils, which are lymphoid tissues located on both sides of the throat.
- It is commonly caused by bacterial or viral pathogens and is most frequent in children aged 5–15 years.
Types of Tonsillitis
1️⃣ Acute Tonsillitis
- It is the sudden and rapid onset of inflammation in the tonsils.
- It usually occurs due to viral or bacterial infection and lasts for a short duration (5–10 days).
- Tonsils appear red, swollen, and may have white or yellow exudates.
- It is often associated with high fever, sore throat, and painful swallowing.
2️⃣ Chronic Tonsillitis
- It is a long-standing or frequently recurring infection of the tonsils.
- It leads to persistent throat discomfort, bad breath (halitosis), and enlarged lymph nodes.
- It may cause snoring, nasal voice, and difficulty swallowing over weeks or months.
- This type may require surgical removal (tonsillectomy) due to repeated episodes.
3️⃣ Recurrent Tonsillitis
- It refers to multiple episodes of acute tonsillitis occurring several times a year.
- Commonly seen in children with weakened immunity or chronic infections.
- The frequency is usually ≥7 episodes in 1 year, ≥5 in 2 consecutive years, or ≥3 in 3 consecutive years.
- May lead to impaired school attendance, poor sleep, and chronic fatigue.
4️⃣ Peritonsillar Abscess (Complication Type)
- Also called Quinsy, it is a pus-filled pocket that forms beside the tonsil.
- Causes severe throat pain, trismus (inability to open mouth), and uvular deviation.
- Requires urgent medical attention and drainage.
Etiology
- Caused mainly by Streptococcus pyogenes (Group A Streptococcus).
- Viral causes include adenovirus, influenza virus, Epstein-Barr virus.
- Risk factors include low immunity, poor hygiene, exposure to infections, and frequent cold/flu.
Pathophysiology of Tonsillitis
1️⃣ Entry of Pathogen
It is caused by viral or bacterial organisms entering the body through the mouth or nose, often via droplet infection.
2️⃣ Colonization
It is in this stage where microorganisms attach to the epithelial lining of the tonsils and begin multiplying.
3️⃣ Tissue Invasion
It is where pathogens invade the tonsillar crypts, triggering the local inflammatory process.
4️⃣ Immune Activation
It is through the release of cytokines and inflammatory mediators that white blood cells accumulate to fight the infection.
5️⃣ Inflammation and Swelling
It is due to vasodilation, fluid leakage, and cellular infiltration, leading to red, swollen, and painful tonsils.
6️⃣ Exudate Formation (in bacterial cases)
It is common to see pus or white patches on tonsils due to the collection of dead cells and bacteria.
7️⃣ Clinical Signs Appear
It is at this stage when fever, sore throat, dysphagia (difficulty in swallowing), and lymphadenopathy occur.
8️⃣ Recovery or Complication
It is after immune resolution that healing occurs; however, untreated cases may lead to abscess or chronic tonsillitis.
Clinical Manifestations
- Sore throat
- Pain while swallowing.
- Red and swollen tonsils with or without white patches (exudate).
- Fever
- Chills
- Malaise
- Tender, enlarged cervical lymph nodes.
- In children : vomiting or abdominal pain may occur.
Diagnosis
- History collection
- physical examination
- Throat swab for culture or rapid antigen detection test (RADT).
- Visual examination of throat using tongue depressor.
- CBC test may show elevated WBCs in bacterial infection.
Medical Management (Pharmacological)
1️⃣ Antibiotics
- It is recommended to give Penicillin V as the first-line antibiotic for streptococcal tonsillitis.
- It is suitable to use Amoxicillin-Clavulanate in penicillin-resistant cases.
- It is necessary to use Macrolides (like Azithromycin) in patients with penicillin allergy.
2️⃣ Analgesics/Antipyretics
- It is important to prescribe Paracetamol or Ibuprofen to relieve pain and reduce fever.
3️⃣ Local Treatment
- It is helpful to advise warm saline gargles or Betadine gargles to reduce throat discomfort.
Surgical Management (Tonsillectomy)
- It is indicated in recurrent tonsillitis (≥7/year) or chronic tonsillitis not responding to treatment.
- It is also required if peritonsillar abscess occurs or if there is airway obstruction due to enlarged tonsils.
- It is performed via cold knife dissection, electrocautery, or coblation techniques.
Nursing Management
1️⃣ Assessment
- It is essential to assess throat for redness, swelling, exudates, and voice changes.
- It is necessary to monitor temperature and signs of systemic infection.
- It is important to inspect for lymph node enlargement and signs of dehydration.
2️⃣ Medication Administration
- It is important to administer prescribed antibiotics (if bacterial) and antipyretics like paracetamol or ibuprofen.
- It is the nurse’s role to ensure full antibiotic course is completed.
- It is essential to observe for drug allergies or side effects during treatment.
3️⃣ Symptom Relief
- It is necessary to encourage warm saline gargles to reduce throat pain.
- It is beneficial to apply warm compresses over the neck for comfort.
- It is helpful to use humidifiers to ease throat irritation.
4️⃣ Hydration and Nutrition
- It is crucial to encourage oral fluid intake like warm soups, juices, and water.
- It is advisable to provide soft, bland, and non-irritating foods.
- It is important to monitor intake-output and prevent dehydration.
5️⃣ Rest and Recovery
- It is essential to provide bed rest during the febrile phase.
- It is necessary to ensure a calm, quiet environment to promote healing.
- It is important to limit physical activity until recovery is complete.
6️⃣ Health Education
- It is the nurse’s duty to teach proper hand hygiene and cough etiquette.
- It is important to educate parents (in pediatric cases) about signs of recurrence.
- It is advisable to inform about complications like rheumatic fever or abscess.
- It is necessary to discuss tonsillectomy indications in chronic or recurrent cases.
7️⃣ Monitoring for Complications
- It is vital to monitor for signs of airway obstruction like stridor or drooling.
- It is important to watch for signs of quinsy, high fever, and difficulty swallowing.
- Immediate referral is needed if respiratory distress or severe pain develops.
2. Radiation therapy
Definition
- Radiation therapy is a clinical treatment method that involves the use of controlled, high-energy ionizing radiation, such as X-rays, gamma rays, or charged particles, to kill or damage cancer cells while minimizing harm to surrounding normal tissue.
- It works by causing breaks in the DNA strands of rapidly dividing cancer cells, thereby inhibiting their ability to multiply and survive.
- Radiation therapy may be used as a curative treatment, an adjuvant therapy after surgery, a neoadjuvant therapy before surgery, or as a palliative therapy in advanced cancer to relieve symptoms such as pain, bleeding, or obstruction.
Goals and Purposes of Radiation therapy
- To destroy or shrink cancerous tumors without harming surrounding normal tissues.
- To prevent recurrence of cancer after surgery or chemotherapy.
- To relieve symptoms like pain, bleeding, or obstruction in advanced cancers (palliative radiotherapy).
- To reduce tumor size before surgery to make it operable (neoadjuvant therapy).
- To kill microscopic residual cancer cells left after surgery (adjuvant therapy).
Types of Radiotherapy
A. External Beam Radiation therapy (EBRT)
- It is the most widely used form of radiotherapy where radiation beams are delivered from a machine outside the body, such as a linear accelerator (LINAC).
- The patient lies on a treatment couch while the radiation machine rotates around them to deliver beams precisely to the tumor site from various angles.
- Techniques such as 3D-CRT (Three-Dimensional Conformal Radiation Therapy) and IMRT (Intensity-Modulated Radiation Therapy) help to shape the radiation dose to fit the tumor.
- It is usually given in daily fractions (sessions) over several weeks.
B. Internal Radiation therapy (Brachytherapy)
- In this technique, a radioactive source is placed directly into or near the tumor using applicators, needles, seeds, or catheters.
- It may be temporary (high-dose rate) or permanent (low-dose rate), depending on cancer type.
- It delivers a very high localized dose while sparing surrounding normal tissues.
- It is commonly used in gynecological cancers, prostate cancer, and oral cavity cancers.
C. Systemic Radiation therapy (Radioisotope Therapy)
- This method involves swallowing or injecting radioactive substances, such as radioiodine (I-131), strontium-89, or samarium-153, that circulate in the bloodstream and selectively target cancer cells.
- It is especially useful in thyroid cancer, bone metastases, and neuroendocrine tumors.
- This method requires isolation precautions due to systemic radioactivity.
Indications of Radiation therapy
Radiation therapy is used to treat a wide variety of malignant tumors, including :
- Breast cancer
- Cervical and uterine cancer
- Prostate cancer
- Head and neck cancers (larynx, pharynx, tongue, mouth)
- Lung cancer
- Esophageal and gastric cancer
- Brain tumors (gliomas, metastases)
- Skin cancers (basal cell, squamous cell carcinoma)
- Lymphomas (Hodgkin and non-Hodgkin)
- Pediatric cancers (e.g., medulloblastoma, rhabdomyosarcoma)
Side Effects of Radiation therapy
It may vary depending on site and dose
Local Side Effects
- Skin irritation, redness, or burns over the radiation site
- Hair loss in the treated area
- Oral ulcers, dry mouth (in head/neck radiation)
- Difficulty swallowing or sore throat (esophageal radiation)
- Diarrhea or abdominal cramps (abdominal or pelvic radiation)
- Vaginal dryness or bleeding (pelvic radiation)
Systemic Side Effects
- Fatigue
- Nausea and vomiting
- Anorexia and weight loss
- Suppression of bone marrow (in long-term or high-dose therapy)
- Risk of secondary malignancy (rare, long-term effect)
Nursing Responsibilities in Radiation therapy
A. Before Radiation therapy (Pre-procedure Nursing Care)
- The nurse must educate the patient and family about the procedure, possible outcomes, and common side effects in a compassionate manner.
- It is important to provide psychological support and reduce fear and anxiety related to the word “radiation”.
- The nurse must assess the patient’s physical baseline — weight, nutritional status, skin integrity, hydration, and vital signs.
- She ensures that any metallic objects (jewelry, implants) are noted and removed if they interfere with therapy.
- If the radiation field includes the pelvic area, patients may be instructed to empty or fill the bladder before treatment.
B. During Radiation therapy (Intra-procedure Care)
- The nurse should assist in accurate positioning of the patient on the radiation table to ensure the beam targets only the tumor site.
- She must observe for immediate adverse reactions such as dizziness, shortness of breath, or skin burning.
- The nurse should follow strict radiation safety protocols, including shielding, lead walls, and maintaining safe distance.
- During brachytherapy, the nurse should limit time spent in the radiation room, stand behind shielding, and wear a radiation dosimeter badge.
- Emotional support is important, as isolation during radiation can be psychologically distressing for many patients.
C. After Radiation therapy (Post-procedure Nursing Care)
- The nurse should inspect the radiation-exposed skin daily and report any signs of ulceration, blisters, or infection.
- It is essential to instruct the patient not to scratch, shave, or apply lotions or powders on the treated skin unless prescribed.
- Dietary counseling is required to manage nausea, mouth sores, weight loss, or bowel irregularities.
- The nurse should monitor complete blood counts (CBC) regularly if bone marrow is exposed, to assess for anemia, neutropenia, or thrombocytopenia.
- She must provide emotional and social support, especially for patients dealing with altered body image, infertility, or fatigue.
- Patient and family should be educated on long-term care, follow-up visits, and signs of complications that must be reported immediately.
Radiation Safety Guidelines for Nurses
- Follow ALARA principle (As Low As Reasonably Achievable) for exposure time.
- Maintain safe distance, use protective lead aprons or barriers, and avoid direct contact with radiation sources.
- Use a radiation badge to monitor cumulative exposure.
- Pregnant nurses should avoid assignments involving direct radiation exposure.
- Educate patients and their visitors about radiation hygiene and home precautions post-brachytherapy or systemic therapy.
3. Nursing care for seizure patient
- Seizures are episodes of abnormal electrical activity in the brain, often resulting in changes in motor activity, consciousness, sensation, or behavior.
- Nursing care focuses on safety, observation, emergency preparedness, post-seizure support, and patient education.
1. Pre-Ictal Phase Nursing Responsibilities (Before Seizure Begins)
- The nurse identifies and records the patient’s aura or pre-seizure symptoms such as dizziness, visual changes, tingling sensations, or anxiety.
- She ensures the environment is safe and clutter-free, removing sharp objects, loose wires, or anything that may cause injury.
- The nurse keeps bed in a low position, raises padded side rails, and ensures oxygen and suction are available at the bedside.
- She administers prescribed antiepileptic medications (e.g., phenytoin, carbamazepine, valproate) on time and watches for therapeutic levels.
- The nurse educates the patient to alert staff if an aura begins, and avoid standing or walking alone during this time.
- She ensures IV access is maintained, especially in ICU, for rapid medication administration during prolonged seizures.
2. Ictal Phase Nursing Responsibilities (During Seizure Activity)
- The nurse must remain calm and stay with the patient, ensuring immediate safety and avoiding unnecessary panic.
- She positions the patient in a side-lying position to prevent aspiration and support drainage of saliva or vomitus.
- The nurse supports the head with a pillow or folded blanket to prevent head trauma from banging against hard surfaces.
- She does not insert anything into the patient’s mouth (like fingers, spoon, or gauze), as it may cause choking or dental injury.
- The nurse loosens tight clothing around the neck or waist to promote airway comfort.
- She observes and records the onset, duration, body part involved first, type of movements, eye deviation, cyanosis, and whether the patient lost bladder/bowel control.
- The nurse calls for emergency assistance if seizure lasts more than 5 minutes (status epilepticus) or if another seizure begins before recovery.
- She administers emergency anticonvulsants (e.g., lorazepam, diazepam, midazolam IV or IM) if prescribed.
3. Post-Ictal Phase Nursing Responsibilities (After Seizure Ends)
- The nurse ensures airway patency by continuing the patient in a side-lying position and suctioning if needed.
- She monitors vital signs, consciousness level, pupil reactions, and respiratory status every 15–30 minutes until stable.
- She performs a quick neurological assessment to evaluate post-seizure deficits such as limb weakness, disorientation, or speech difficulty.
- The nurse documents the entire seizure episode, including triggers, type, duration, postictal confusion, and response to treatment.
- She allows the patient to rest in a quiet, low-stimulation environment, turning off bright lights or noise to promote calm.
- The nurse offers emotional support and reassurance, as patients may feel anxious, embarrassed, or fearful.
- She checks for injuries sustained during the seizure—tongue bite, bruises, head trauma, or dislocated limbs.
- The nurse assesses bladder/bowel incontinence, provides hygiene care, and ensures privacy and dignity.
4. Long-Term & General Nursing Management
- The nurse ensures strict compliance with long-term antiepileptic medication regimens, and observes for side effects like drowsiness or gum overgrowth (e.g., with phenytoin).
- She provides lifestyle counseling to help avoid triggers: sleep deprivation, flashing lights, skipping meals, and emotional stress.
- The nurse encourages regular neurological follow-up, EEG tests, and medication level monitoring.
- She educates the patient and family on how to respond to seizures at home: keeping calm, protecting the head, and timing the episode.
- The nurse promotes dietary support such as a ketogenic diet (in children or refractory epilepsy), as advised.
- She advises against driving, swimming alone, or using heavy machinery unless seizure-free for a medically approved period.
- The nurse encourages wearing medical identification bracelets with diagnosis and emergency instructions.
5. Hospital/ICU-Specific Seizure Precaution Measures
- The nurse ensures a seizure warning sign is placed at the patient’s bedside.
- She places padded side rails, removes restraints or restraints are padded to avoid injury.
- The nurse ensures oxygen cylinder, Ambu bag, suction machine, oral airways, and emergency drugs are within reach.
- She keeps airway adjuncts and IV diazepam or lorazepam ready, especially for patients with frequent seizures.
- The nurse includes seizure activity as part of the nursing care plan, shift reports, and ICU handovers.
- She coordinates with the team for neurology referrals, imaging (CT/MRI), and EEG scheduling.
4. Hormonal replacement therapy
Definition
- Hormonal Replacement Therapy (HRT) is a medical treatment in which female sex hormones like estrogen and/or progesterone are administered artificially to compensate for hormonal deficiency, especially in menopausal or postmenopausal women, to relieve symptoms and prevent long-term complications such as osteoporosis.
- It is also used in conditions of premature ovarian failure, surgical menopause, or hormonal imbalances, and sometimes in males with androgen deficiency.
Types of Hormonal Replacement Therapy
1️⃣ Estrogen Therapy
- Estrogen is the primary hormone used in HRT and is essential for managing vasomotor symptoms (like hot flashes and night sweats), vaginal atrophy, and osteoporosis prevention.
- It is given to women who have undergone hysterectomy, as they are not at risk for endometrial cancer.
- Estrogen can be administered in various forms such as oral tablets (e.g., conjugated equine estrogen), transdermal patches (e.g., estradiol), topical gels, or vaginal rings.
- It works by replenishing the low estrogen levels in postmenopausal women, thereby maintaining bone density, vaginal health, and mood stabilization.
2️⃣ Progesterone / Progestin Therapy
- Progesterone (or its synthetic version, progestin) is used in combined HRT for women who still have an intact uterus, to protect the endometrium from the stimulating effects of estrogen and prevent endometrial hyperplasia or cancer.
- It is usually given along with estrogen in cyclical (monthly) or continuous regimens.
- Progesterone may be administered orally (e.g., medroxyprogesterone acetate), vaginally, or through intrauterine devices like levonorgestrel-releasing IUDs.
- It helps in regulating menstrual-like bleeding and ensures hormonal balance, reducing the risk of uterine abnormalities.
3️⃣ Estrogen + Progesterone Combination Therapy
- Combined therapy includes both estrogen and progesterone and is suitable for women with a uterus to reduce menopausal symptoms while ensuring protection of the endometrium.
- It is available as oral pills, transdermal patches, or combinations that mimic natural cycles.
- This combination helps to manage hot flashes, vaginal dryness, irritability, sleep disturbance, and mood fluctuations.
- It also provides bone protection and reduces the risk of fractures in postmenopausal women.
4️⃣ Tibolone
- Tibolone is a synthetic steroid with estrogenic, progestogenic, and androgenic effects and is prescribed to postmenopausal women as an alternative to traditional HRT.
- It helps in the reduction of menopausal symptoms, improves sexual function, and prevents bone loss.
- It is taken as a once-daily oral tablet and is particularly useful in women who are more than 12 months postmenopausal.
- Tibolone does not induce cyclical bleeding, which improves compliance in many women.
Indications of HRT
- It is used to relieve menopausal symptoms such as hot flashes, mood swings, insomnia, vaginal dryness, and fatigue.
- It is used in osteoporosis prevention and treatment in postmenopausal women.
- It is prescribed in cases of premature menopause or ovarian insufficiency, often seen in younger women.
- It is used in surgical menopause following bilateral oophorectomy (removal of ovaries).
- It may also be used in hypogonadism or Turner’s syndrome to induce puberty in adolescent girls.
Contraindications of HRT
- It is contraindicated in patients with a history of breast or endometrial cancer, due to risk of recurrence.
- It should not be given in patients with unexplained vaginal bleeding, which needs evaluation first.
- It is avoided in active or past thromboembolic disease like DVT or pulmonary embolism.
- It should not be used in patients with severe liver disease or dysfunction.
- It is contraindicated in women with known or suspected pregnancy.
Benefits of HRT
- It significantly reduces vasomotor symptoms such as hot flashes and night sweats.
- It improves genitourinary symptoms, like vaginal dryness, urinary urgency, and discomfort during intercourse.
- It helps in preserving bone density, thus preventing fractures and osteoporosis.
- It may improve mood, sleep, and overall quality of life in postmenopausal women.
- In some cases, it may help in cognitive function and memory, although evidence is mixed.
Risks and Side Effects of HRT
- It increases the risk of venous thromboembolism (blood clots), especially in older women or those with risk factors.
- Prolonged use, particularly of combined HRT, can raise the risk of breast cancer.
- It may cause bloating, breast tenderness, nausea, and headache in some women.
- It can lead to irregular bleeding during the early months of therapy.
- In some cases, gallbladder disease and stroke risk may be slightly increased.
Nursing Responsibilities in Hormonal Replacement Therapy (HRT):
- Assess complete medical, surgical, menstrual, and family history before starting HRT.
- Educate the patient about the purpose, types, dosage, route, and duration of hormone therapy.
- Explain possible side effects like nausea, breast tenderness, bloating, and breakthrough bleeding.
- Monitor vital signs, weight, blood pressure, and any signs of fluid retention or edema.
- Observe for early warning signs like chest pain, leg swelling, shortness of breath, or abnormal vaginal bleeding.
- Ensure proper administration of oral tablets, transdermal patches, vaginal creams, or rings.
- Encourage compliance by helping patients understand their dosing schedule and regimen (cyclic or continuous).
- Instruct the patient to avoid smoking and alcohol during HRT due to increased cardiovascular risk.
- Promote regular screening including mammograms, Pap smears, liver function tests, and bone density scans.
- Provide emotional and psychological support regarding body image changes and menopause-related distress.
- Encourage calcium and vitamin D intake, physical activity, and healthy lifestyle for bone protection.
- Maintain accurate and confidential documentation of all patient interactions, side effects, and progress.
5. Eye camps
Definition of Eye Camps
- It is a temporary, organized, outreach health service program conducted in rural or underserved areas to screen, diagnose, and treat eye disorders, especially cataract, refractive errors, and preventable blindness.
- It is conducted in collaboration with NGOs, government hospitals, and ophthalmology specialists to promote eye care awareness and visual health in the community.
Objectives of Eye Camps
- It is aimed at early detection and treatment of eye diseases like cataract, glaucoma, trachoma, refractive errors, etc.
- It is designed to provide free or subsidized eye surgeries, especially for poor or elderly patients.
- It helps in spreading awareness about eye hygiene, nutrition, and prevention of blindness.
- It works to increase community participation in eye health and promote health-seeking behavior.
- It helps in referring complicated cases to base hospitals for advanced management.
Types of Eye Camps
General Eye Screening Camps – It is conducted to screen general public for common eye problems.
Cataract Surgery Camps – It is organized specifically to identify and operate cataract cases.
School Eye Camps – It is held in schools to screen children for refractive errors and provide glasses.
Glaucoma Detection Camps – It is arranged to measure intraocular pressure (IOP) and diagnose glaucoma.
Specialized Camps – It may focus on diabetic retinopathy, squint, or corneal diseases with specialist intervention.
Activities Conducted in an Eye Camp
- Pre-camp awareness and publicity through posters, loudspeakers, health talks, and community leaders.
- Registration of patients, history taking, and recording demographic details.
- Initial screening by optometrists or trained health workers for visual acuity.
- Eye examination by ophthalmologist using slit-lamp, torchlight, or ophthalmoscope.
- Distribution of spectacles for those with refractive errors.
- Identification of operable cataract cases and transport arrangement for surgery.
- Free surgical treatment (e.g., cataract surgery) at base hospital or mobile operation theatre.
- Follow-up and post-operative care after surgery to prevent complications.
Advantages of Eye Camps
- It is cost-effective and accessible to poor and elderly populations.
- It provides mass-level screening and awareness in remote areas.
- It helps in early detection and prevention of avoidable blindness.
- It builds community trust and encourages utilization of health services.
- It supports national blindness control programs and public-private partnerships.
Limitations or Challenges
- It may lack sufficient follow-up care or monitoring after surgery.
- There is sometimes a risk of infection or poor outcomes if sterility is not maintained.
- Trained personnel and equipment may not be consistently available.
- Transportation and communication problems in rural areas may affect turnout.
- Cultural beliefs or fear of surgery may prevent some from utilizing services.
Government Initiatives Supporting Eye Camps
- National Programme for Control of Blindness (NPCBVI) – Supports eye camps for cataract surgery and childhood blindness.
- District Blindness Control Society (DBCS) – Coordinates camps at district level.
- Ayushman Bharat and PMJAY – Provide financial assistance for surgeries.
- Vision 2020 Initiative – A global campaign aiming at eliminating avoidable blindness by promoting such camps
Nursing Responsibilities in Eye Camps
A. Before the Camp (Preparation Phase)
- Participate in planning and organizing meetings with healthcare teams and NGOs.
- Assist in survey and selection of the location based on need and accessibility.
- Help prepare logistics, such as registration sheets, IOP machines, Snellen charts, medications, sterilized surgical instruments.
- Coordinate with local leaders, school teachers, ASHA and Anganwadi workers to mobilize the population.
- Assist in pre-camp publicity through posters, banners, and announcements.
B. During the Camp (Implementation Phase)
- Perform basic vision screening, record findings and guide patients to examination counters.
- Assist ophthalmologists during eye examinations, IOP measurements, and slit-lamp setup.
- Administer prescribed eye drops or ointments, and counsel on their usage.
- Provide pre-operative preparation for cataract surgery candidates (cleaning, instilling pupil-dilating drops, taking consent).
- Maintain infection control practices and manage instrument sterilization.
- Counsel patients on eye drop instillation techniques and follow-up visits.
- Record data and statistics of number of patients seen, surgeries done, spectacles distributed, etc.
C. After the Camp (Post-camp Follow-up)
- Participate in follow-up visits to operated patients for wound care, suture check, and vision testing.
- Educate patients on recognizing complications such as eye pain, redness, or blurred vision post-surgery.
- Collect feedback and evaluation to improve future camps.
- Assist in report preparation and documentation.
- Ensure referred patients reach hospitals for further care.
Benefits and Importance of Eye Camps
- Eye camps reduce the burden of preventable blindness, especially in underserved populations.
- They help in early detection of chronic eye diseases like glaucoma and diabetic retinopathy.
- Improve access to quality eye care services in remote and inaccessible areas.
- Provide health education and create awareness about the importance of regular eye checkups.
- Offer low-cost or free surgical services like cataract surgery to poor patients.
- Promote community participation in eye health and strengthen public-private partnerships in healthcare.
Q.3 Answer the following
1. Define glucoma (2)
- Glaucoma is a group of chronic eye conditions in which there is increased intraocular pressure (IOP) that causes damage to the optic nerve.
- This damage to the optic nerve can gradually lead to visual field defects and may result in permanent blindness if not treated on time.
- It is one of the leading causes of preventable blindness worldwide, especially among the elderly.
2. Enlist clinical manifestation of glucoma (3)
✅ Open-Angle Glaucoma (Chronic)
- Gradual loss of peripheral vision (tunnel vision)
- Painless and progressive vision loss
- Halos around lights (in late stage)
- Difficulty seeing in dim light or night vision
- Frequent changes in eyeglass prescription
- Mild eye ache or strain after prolonged reading
- Increased intraocular pressure (IOP) on examination
- Headaches or blurred vision during the day
✅ Angle-Closure Glaucoma (Acute)
- Sudden severe eye pain (often one-sided)
- Redness of eye and decreased visual acuity
- Colored halos or rainbow rings around lights
- Nausea and vomiting due to raised IOP
- Fixed mid-dilated pupil (non-reactive to light)
- Eye feels hard on palpation
- Frontal headache or brow pain
- Photophobia and excessive tearing
3. Write surgical and nursing management for glucoma patient (5)
Surgical Management of Glaucoma
Surgery is indicated when intraocular pressure (IOP) is not adequately controlled by medications or laser therapy. The goal is to improve aqueous humor drainage and reduce IOP.
✅1. Laser Surgeries
Laser procedures are non-incisional, outpatient techniques aimed at reducing intraocular pressure by improving fluid drainage or reducing aqueous production.
Laser Trabeculoplasty
- It is most commonly used in Primary Open-Angle Glaucoma (POAG).
- A laser beam is applied to the trabecular meshwork, stimulating the tissue to improve outflow of aqueous humor.
- Common techniques include Argon Laser Trabeculoplasty (ALT) and Selective Laser Trabeculoplasty (SLT).
- The procedure is usually done under topical anesthesia and lasts about 10–15 minutes.
- It may be repeated after months or years if IOP rises again.
- Post-procedure anti-inflammatory drops are often prescribed to control inflammation.
Laser Peripheral Iridotomy
- Typically used in Angle-Closure or Narrow-Angle Glaucoma.
- A small hole is made in the peripheral iris, allowing aqueous humor to bypass the blocked trabecular meshwork.
- It helps to equalize pressure between anterior and posterior chambers of the eye.
- The procedure is usually done prophylactically in the fellow eye as well.
- Transient blurring of vision or photophobia may occur post-treatment.
- The patient may be pretreated with IOP-lowering medications before the laser to prevent a pressure spike.
Cyclophotocoagulation (CPC)
- This is a laser treatment targeting the ciliary body epithelium, where aqueous humor is produced.
- It is reserved for advanced, painful, or refractory glaucomas where vision is already compromised.
- Can be done transsclerally or endoscopically depending on eye condition.
- It reduces intraocular pressure by decreasing aqueous production, not outflow.
- May require multiple sessions depending on response.
- Risk of inflammation, vision loss, or hypotony (too low IOP) exists, so it is used cautiously.
✅ 2. Conventional Surgeries
These involve incisional techniques to create new outflow pathways or implant devices to reduce IOP, especially in cases resistant to medical and laser therapy.
Trabeculectomy
- This is the most frequently performed incisional surgery for glaucoma.
- A scleral flap is created to form a new drainage pathway for aqueous humor into a filtering bleb under the conjunctiva.
- Reduces IOP significantly and may eliminate the need for medications.
- Antifibrotic agents like mitomycin-C or 5-FU are used intraoperatively to prevent scarring.
- Complications include hypotony, bleb infection (blebitis), and choroidal effusion.
- Post-op care includes frequent follow-up and IOP monitoring to ensure bleb function.
Glaucoma Drainage Implants (Tube Shunt Surgery)
- Used when trabeculectomy fails or is contraindicated (e.g., uveitis, neovascular glaucoma, pediatric glaucoma).
- A silicone tube is inserted into the anterior chamber, connected to a reservoir plate placed beneath the conjunctiva.
- Helps drain excess aqueous humor externally and controls IOP long-term.
- Common devices: Ahmed, Molteno, and Baerveldt implants.
- Surgery is more complex and requires longer surgical time and healing.
- Postoperative care involves monitoring tube patency, inflammation, and endothelial cell count.
Minimally Invasive Glaucoma Surgery (MIGS)
- MIGS refers to a set of modern, less invasive techniques designed for mild-to-moderate glaucoma.
- Uses tiny stents, shunts, or trabecular meshwork ablation via small incisions.
- Procedures are often combined with cataract surgery for optimal results.
- Examples include : iStent, Hydrus Microstent, XEN Gel Stent
Nursing Management of Glaucoma Patient
✅ A. Preoperative Nursing Care (Before Glaucoma Surgery)
- The nurse assesses the extent of vision loss, type of glaucoma (open or angle-closure), and impact on activities of daily living.
- She ensures that IOP-reducing medications are given on time (e.g., timolol, pilocarpine, acetazolamide).
- The nurse encourages the patient to lie with the head slightly elevated to reduce intraocular pressure.
- She educates the patient to avoid coughing, straining, or Valsalva maneuvers, which can further increase IOP.
- She provides psychological support, addressing fears of blindness or surgery.
- The nurse confirms that pre-op investigations (RBS, BP, ECG, consent) are completed.
- She assists in maintaining strict asepsis during pre-op eye care and eye drop instillation.
- The nurse assesses patient’s understanding of postoperative limitations, like avoiding eye rubbing or strenuous activities.
- She ensures documentation of allergies, especially to anesthesia or antibiotics, is complete and updated.
- The nurse explains the purpose of eye drops (miotics) given preoperatively to constrict pupils, helping reduce IOP.
✅ B. Postoperative Nursing Care (After Glaucoma Surgery)
- The nurse regularly monitors vital signs and pain level, reporting any unusual symptoms immediately.
- She observes the operated eye for redness, swelling, excessive discharge, or sudden vision loss, which could indicate complications.
- She positions the patient on the non-operative side, with the head slightly elevated.
- The nurse reinforces the correct method of applying prescribed antibiotic, steroid, or anti-inflammatory eye drops, preventing contamination.
- She teaches the patient to avoid bending, sneezing, lifting heavy weights, or reading for long periods.
- She applies eye shields or protective goggles, especially at night, to prevent accidental injury.
- She checks the patency of the filtration bleb (in trabeculectomy patients) and monitors IOP as per ophthalmologist’s orders.
- The nurse monitors for hyphema (blood in anterior chamber), shallow anterior chamber, or corneal edema.
- She ensures post-op follow-up visits are scheduled and attended for tonometry and visual field tests.
- She promotes adequate hydration and soft diet to prevent straining during bowel movements.
✅ C. General Nursing Care and Patient Education
- The nurse educates the patient about the chronic nature of glaucoma, emphasizing that lifelong treatment and monitoring are essential.
- She provides guidance on adherence to eye drop schedules, even when there are no symptoms.
- She advises on avoiding over-the-counter medications (like antihistamines) that may increase IOP in angle-closure glaucoma.
- The nurse teaches the patient to recognize warning signs of increased IOP—blurred vision, colored halos, eye pain—and report them immediately.
- She refers patients with advanced vision loss to low-vision aids, mobility training, or social support programs.
- She encourages family members to get routine eye exams, since glaucoma often has a genetic component.
- She advises the patient to limit screen time, take breaks during reading, and use adequate lighting to reduce eye strain.
- The nurse promotes use of large-print reading material or audio books in patients with significant vision loss.
- She encourages a diet rich in antioxidants (vitamin A, C, E, zinc) and regular moderate physical activity.
- She discusses coping strategies and emotional support resources for patients anxious about vision loss or dependency.
Section 2 (37 marks)
Q.4 Answer in short (any five) (10 marks)
1. Rule of nine for burn patient
The Rule of Nines is a clinical tool used to estimate the percentage of total body surface area (TBSA) that has been burned in a patient with burn injuries. It helps in guiding fluid resuscitation, determining severity of burns, and planning medical or surgical management.
Adult Body Surface Area (BSA) Estimation – Rule of 9%:
Head and Neck – 9%
Each Upper Limb – 9% (4.5% front + 4.5% back)
Each Lower Limb – 18% (9% front + 9% back)
Front of the Trunk – 18%
Back of the Trunk – 18%
Perineum (Genital area) – 1%
2. Refrective error
It is a common visual disorder in which the eye is unable to properly focus light on the retina, resulting in blurred or distorted vision. It is caused by abnormalities in the shape of the cornea, lens, or eyeball length, leading to improper refraction of light rays. In short, refractive error refers to a condition in which the eye does not bend (refract) light correctly, making it difficult to see clearly at various distances.
Examples include :
- Myopia (Nearsightedness)
- Hyperopia (Farsightedness)
- Astigmatism
- Presbyopia
3. Amenorrhea
Amenorrhea is defined as the absence or cessation of menstruation in a woman of reproductive age for three or more consecutive menstrual cycles, or failure to begin menstruation by the age of 15 years (primary amenorrhea). It may be caused by pregnancy, hormonal disorders, stress, excessive exercise, or structural abnormalities. It is classified into :
Primary amenorrhea : When menstruation has not started by age 15.
Secondary amenorrhea : When a woman who had normal menstruation stops getting periods for 3 months or more.
4. Menieres disease
- It is a chronic disorder of the inner ear that affects balance and hearing, usually presenting with episodes of vertigo, tinnitus, hearing loss, and a feeling of fullness in the ear.
- Meniere’s disease is a progressive inner ear disorder that results in repeated episodes of dizziness and hearing problems, commonly affecting only one ear.
- It is believed to be caused by an abnormal accumulation of endolymphatic fluid in the inner ear (labyrinth), leading to sensory disturbances.
5. Resuctitation equipment
- Bag-valve-mask (Ambu bag)
- Oxygen cylinder with flow meter
- Suction machine with catheters
- Laryngoscope (with blades)
- Endotracheal tubes (ET tubes) – various sizes
- Oropharyngeal and nasopharyngeal airways
- Defibrillator (manual or AED)
- Intravenous (IV) cannulas – various sizes
- IV fluids (e.g., Normal Saline, Ringer Lactate)
- Emergency drug tray (e.g., epinephrine, atropine)
- Syringes and needles – various sizes
- Stethoscope
- Blood pressure monitor (sphygmomanometer)
- Pulse oximeter
- Cardiac monitor/ECG machine
- Face masks and nasal cannula
- Gloves, gowns, and protective eyewear
- Tourniquets
- Spinal board or stretcher
- Thermal blanket or warming device
6. Cataract
- Cataract is a medical condition in which the natural crystalline lens of the eye becomes progressively cloudy or opaque, leading to a decrease in vision clarity.
- It is commonly age-related, but can also be congenital, traumatic, or secondary to diseases like diabetes or long-term corticosteroid use.
- This opacification interferes with the passage of light through the lens, resulting in blurred or dim vision. It is the most common cause of reversible blindness globally, especially in elderly individuals.
Q.5 Write short notes (any four) (20 mark)
1. Cosmetic surgery
Definition of Cosmetic Surgery
- Cosmetic surgery is defined as a medical procedure aimed at improving or modifying the aesthetic appearance of an individual through surgical or minimally invasive techniques.
- Cosmetic surgery is a specialized field of plastic surgery that focuses on improving physical appearance through surgical and non-surgical techniques. It is generally elective and performed to enhance self-image, body proportion, or rejuvenate aging features.
- Unlike reconstructive surgery, which focuses on repairing defects or injuries, cosmetic surgery is performed electively and is not medically necessary.
- It may involve reshaping facial or body structures to achieve harmony, balance, and enhanced self-confidence.
Objectives / Purpose of Cosmetic Surgery
- The primary objective of cosmetic surgery is to improve the aesthetic appearance of a person and boost self-esteem.
- It is performed to reshape normal body features, remove unwanted fat or skin, or restore youthfulness by reducing signs of aging.
- It also helps in improving quality of life for individuals who may suffer from low self-confidence due to their appearance.
- In some cases, cosmetic surgery may be used for post-bariatric contouring (after massive weight loss) or gender-affirming surgeries.
Types of cosmetic surgery
🔷 A. Facial Cosmetic Surgery
Rhinoplasty (Nose reshaping): It improves the shape, size, and structure of the nose to enhance facial harmony.
Blepharoplasty (Eyelid surgery): Performed to remove sagging skin or fat deposits from the upper/lower eyelids.
Rhytidectomy (Facelift): Tightens loose skin, smoothens wrinkles, and rejuvenates facial appearance.
Chin and cheek implants: Enhance bone structure for a more defined facial contour.
Botox and dermal fillers: Non-surgical options to reduce fine lines and restore facial volume.
🔷 B. Body Contouring Surgery
Liposuction: Removes localized fat deposits from areas like thighs, abdomen, arms, and neck.
Abdominoplasty (Tummy Tuck): Removes excess abdominal skin and tightens muscles for a flatter stomach.
Buttock augmentation/lift: Enhances shape and size of buttocks using fat grafting or implants.
Arm and thigh lift: Removes sagging skin and fat following weight loss or aging.
🔷 C. Breast Cosmetic Procedures
Breast augmentation: Insertion of silicone or saline implants to increase breast size and fullness.
Breast lift (Mastopexy): Lifts and reshapes sagging breasts without changing volume.
Breast reduction: Removes excess tissue for comfort and proportion, often also improving posture and reducing back pain.
🔷 D. Hair and Skin Cosmetic Procedures
Hair transplantation: Surgical technique that moves hair follicles from a donor site to bald areas.
Chemical peels: Use of chemical solutions to remove damaged outer skin layers for smoother skin.
Laser resurfacing: Targets scars, age spots, wrinkles, and skin irregularities using laser technology.
Indications for Cosmetic Surgery
- Desire to improve physical appearance, body symmetry, or confidence.
- Presence of aesthetic dissatisfaction with features such as nose shape, breast size, or abdominal bulge.
- Aging signs like wrinkles, sagging skin, or eyelid drooping.
- Post-weight loss excess skin or deformities.
- Gender-affirming procedures for transgender individuals.
- Career or personal requirements (e.g., modeling, acting) where appearance plays a role.
Risks and Complications
- Like any surgical procedure, cosmetic surgery carries inherent risks which include:
- Infection at the incision site, leading to delayed healing.
- Hematoma or seroma formation, causing swelling and fluid accumulation.
- Scarring or keloid formation depending on healing tendencies.
- Nerve damage leading to temporary or permanent numbness or muscle weakness.
- Unsatisfactory results, possibly requiring revision surgery.
- Anesthesia complications, such as respiratory distress or allergic reactions.
- Emotional or psychological dissatisfaction, especially in unrealistic expectations.
Nursing Responsibilities in Cosmetic Surgery
Nurses play a crucial role in ensuring the safety, well-being, emotional comfort, and recovery of patients undergoing cosmetic surgery, both before and after the procedure.
✅ 1. Preoperative Nursing Responsibilities
- The nurse must collect a complete health history, including previous surgeries, allergies, current medications, past illnesses, and psychosocial background.
- She should assess the patient’s mental readiness and ensure they have realistic expectations regarding the results of the surgery.
- The nurse explains the purpose, steps, risks, recovery process, and costs of the cosmetic procedure in a clear, honest, and respectful manner.
- She ensures that informed consent is obtained, signed, and witnessed after the patient fully understands the procedure.
- The nurse performs preoperative investigations, including blood tests, ECG, chest X-ray, and any other ordered evaluations.
- She prepares the patient physically, including fasting instructions (NPO status), shaving or cleaning the surgical site, and administering prescribed premedications.
- She helps reduce preoperative anxiety by offering reassurance, answering questions, and supporting the patient’s emotional needs.
- The nurse verifies that the correct patient, correct site, and correct procedure are confirmed before transferring to the operation theater.
✅ 2. Intraoperative Nursing Responsibilities
- The nurse assists in maintaining a sterile environment in the operating room by ensuring all aseptic protocols are followed.
- She prepares and arranges sterile instruments, sutures, and dressings according to the type of cosmetic surgery planned.
- The nurse assists the surgeon by handing instruments and managing surgical equipment during the procedure.
- She continuously monitors the patient’s vital signs (BP, pulse, temperature, SpO₂) during surgery.
- The nurse ensures the patient is in a safe and appropriate surgical position, especially in surgeries involving the face or body contouring.
- She records intraoperative events, estimated blood loss, fluid administration, and anesthesia monitoring.
- The nurse ensures accurate sponge, instrument, and needle counts before wound closure.
✅ 3. Postoperative Nursing Responsibilities
- The nurse monitors vital signs closely in the immediate postoperative period and checks for any signs of complications like bleeding, hypotension, or hypoxia.
- She assesses the surgical wound site for bleeding, swelling, hematoma, infection, or poor healing and applies sterile dressings as per protocol.
- The nurse provides pain management through prescribed analgesics and non-pharmacologic methods such as ice packs or positioning.
- She educates the patient about postoperative self-care, including wound care, scar management, activity restrictions, and when to seek medical help.
- She helps the patient with early ambulation, depending on the surgery, to prevent complications such as deep vein thrombosis (DVT).
- The nurse monitors for psychological reactions such as emotional distress, disappointment, or body image concerns post-surgery.
- She reinforces the importance of follow-up visits and adherence to instructions regarding medication, rest, and hygiene.
- The nurse documents all nursing interventions, vital signs, dressing changes, medication administration, and patient responses in the nursing notes.
✅ 4. Emotional and Psychological Responsibilities
- The nurse provides emotional support before and after surgery, especially in patients undergoing visible facial or body changes.
- She ensures that the patient does not have unrealistic expectations and understands that healing and final results take time.
- The nurse may need to recognize signs of body dysmorphic disorder (BDD) and refer to counseling if needed.
- She promotes positive reinforcement and body image by reassuring the patient and celebrating recovery milestones.
✅ 5. Legal and Ethical Responsibilities
- The nurse ensures that all legal documents, including consent forms and pre-anesthetic checklists, are properly filled out.
- She must maintain confidentiality and privacy, especially in procedures involving sensitive areas.
- The nurse acts as a patient advocate, ensuring their rights, dignity, and autonomy are respected.
- She should report any ethical concerns, such as coercion or inadequate informed consent, to the healthcare team.
2. Brest self examination
Definition
- It is a simple, non-invasive method in which a woman examines her own breasts regularly for any unusual changes in appearance or texture, in order to detect breast abnormalities such as lumps, skin dimpling, or nipple discharge, which may be an early sign of breast cancer.
- It is a procedure by which a woman systematically inspects and palpates her breasts using her own hands and eyes to detect any changes or abnormalities.
- It is considered a primary screening method for breast cancer, especially in low-resource settings.
- It is a preventive health measure recommended for women starting from 20 years of age, performed once every month.
- It helps in developing awareness of normal breast consistency, so changes can be quickly identified.
PURPOSE / OBJECTIVES OF BSE
- To detect early signs of breast cancer such as lumps, pain, or skin changes.
- To enable a woman to become familiar with the normal structure and texture of her breasts.
- To promote responsibility and self-awareness about breast health.
- To serve as a supplement to clinical breast examination (CBE) and mammography.
- To identify any visible or palpable abnormality so that medical care can be sought promptly.
IDEAL TIME FOR BSE
- In menstruating women, the best time to perform BSE is 7 to 10 days after the onset of menstruation, when breast tissue is least tender or swollen.
- In post-menopausal women, BSE should be performed on the same date every month to maintain regularity.
- Women on oral contraceptives are advised to perform BSE on a fixed day during their pill cycle.
- It should be performed monthly, as regular checks help recognize new or unusual changes more easily.
STEPS OF BREAST SELF-EXAMINATION
BSE involves visual inspection and manual palpation in both standing and lying positions.
A. VISUAL INSPECTION (Performed in front of a mirror)
- The woman should undress from the waist up and stand in front of a mirror with arms relaxed at her sides.
- She should inspect for any visible asymmetry, lumps, swelling, or skin changes such as dimpling, puckering, or redness.
- Next, she should raise both arms overhead and observe for the same changes again.
- Then she should press her hands firmly on her hips and slightly bend forward to contract the chest muscles.
- In each step, she should carefully observe both breasts for nipple changes (e.g., inversion, retraction, discharge).
B. MANUAL PALPATION (Using finger pads for touch examination)
While Standing or Bathing
- With the skin wet and soapy (which improves finger glide), she should raise her right arm.
- Using the pads of the three middle fingers of the left hand, she should palpate the right breast in small, circular motions.
- She should follow a pattern (circular, vertical strip, or wedge) to ensure full coverage of the breast tissue.
- The axillary area (underarm) should be palpated thoroughly for any enlarged lymph nodes.
- The process should be repeated for the left breast using the right hand.
While Lying Down
- She should lie on her back with a small pillow under her right shoulder and place her right arm behind her head.
- With her left hand, she should feel the right breast using gentle pressure at various depths (light for surface, medium for mid-level, and firm for deep tissue).
- She should move her fingers in a systematic manner, from the outer edge toward the nipple.
- The same steps should be repeated on the left side using the right hand.
- Lastly, she should gently squeeze each nipple to check for any discharge or fluid.
WHAT TO LOOK FOR DURING BSE
- New lump or mass in the breast or underarm area.
- Thickened areas or firm nodules that feel different from surrounding tissues.
- Changes in the shape or size of the breast.
- Skin changes like puckering, dimpling, or orange-peel texture (peau d’orange).
- Nipple abnormalities, including retraction, inversion, discharge (especially bloody or clear), or crusting.
- Persistent localized pain or tenderness in one breast or armpit.
- Swelling, warmth, or redness on the skin of the breast.
ADVANTAGES OF BSE
- It is cost-free, simple, and non-invasive.
- It empowers women to take responsibility for their own breast health.
- It helps in early detection, which improves treatment outcomes.
- It increases self-awareness and confidence in recognizing physical changes.
- It is especially useful in rural and resource-limited settings where mammography may not be available.
LIMITATIONS OF BSE
- BSE is not a substitute for clinical breast examination or mammography.
- It may lead to false alarms and unnecessary anxiety due to benign lumps.
- It may miss deep or small tumors, especially in obese women.
- Some women may lack confidence or proper technique in performing BSE correctly.
- It may cause delay in seeking medical care if symptoms are ignored or misinterpreted.
NURSING RESPONSIBILITIES IN PROMOTING BSE
✅ 1. Health Education and Awareness
- It is the nurse’s responsibility to create awareness about breast cancer and the importance of early detection through regular BSE.
- The nurse should explain that early-stage breast cancer often does not cause pain, so regular self-checks are essential.
- It is important to conduct individual or group education sessions during outpatient visits, health camps, antenatal clinics, and community health programs.
- The nurse should provide accurate, culturally sensitive information, especially in rural or less educated populations.
- Educational materials like charts, leaflets, posters, videos, or breast models should be used during teaching sessions.
✅ 2. Demonstration of Technique
- The nurse must demonstrate the correct steps of BSE practically, using breast models or visual aids.
- Each woman should be taught the systematic method of inspection and palpation, covering the entire breast and axillary area.
- The nurse must explain the importance of using finger pads, circular motion, and varying pressure for accurate palpation.
- She should teach women how to choose a fixed day each month for the examination and integrate it into their routine.
- The nurse should give clear, repeated instructions to ensure the woman learns the technique correctly.
✅ 3. Encouraging Routine Practice and Adherence
- It is the nurse’s duty to motivate and remind women to perform BSE every month consistently.
- She should help the woman overcome fear, embarrassment, or shyness, especially among adolescents or newly married women.
- The nurse can suggest using a calendar, diary, or phone alarm to remind them of their monthly BSE schedule.
- Women should be encouraged to include BSE as a regular part of their personal hygiene or self-care routine.
- Reinforcement during each follow-up visit helps to develop confidence and habit formation.
✅ 4. Assessment and Clarification
- The nurse should ask open-ended questions to assess the woman’s understanding of the BSE process.
- She must observe the woman’s demonstration, if possible, and correct any errors in hand movement, positioning, or technique.
- The nurse should evaluate whether the woman knows what signs to look for, such as lumps, nipple discharge, or skin changes.
- Misconceptions (e.g., BSE is not necessary without pain or symptoms) should be identified and corrected immediately.
✅ 5. Referral and Follow-Up Care
- If a woman finds any lump, change, or abnormality during BSE, the nurse must guide her to seek immediate medical evaluation.
- The nurse should assist in scheduling clinical breast examination, ultrasound, mammogram, or FNAC as advised.
- She must explain that not all lumps are cancerous, and further testing is necessary for accurate diagnosis.
- The nurse should provide emotional support and reduce anxiety during the waiting period for results.
- Documentation of the finding and referral must be done in the woman’s health record for future follow-up.
✅ 6. Role in Community and Public Health Settings
- Nurses working in community health centers, sub-centers, or urban health posts have a vital role in mass education about BSE.
- They can organize awareness camps during Breast Cancer Awareness Month (October) or local health events.
- Nurses should also involve ASHA, ANM, or women’s self-help groups in spreading awareness about breast self-examination.
- They can collaborate with NGOs and cancer screening programs to increase BSE practice coverage.
- Community-based teaching helps to reach underserved, tribal, and low-literacy populations.
3. Nursing care for coma patient in ICU
A coma patient requires round-the-clock comprehensive nursing care focused on maintaining vital functions, preventing complications, and promoting recovery through a multidisciplinary and empathetic approach.
✅ 1. Airway Management and Respiratory Support
- The nurse ensures a patent airway using endotracheal tube or tracheostomy, depending on the coma level.
- She maintains oxygen therapy or mechanical ventilation settings, as prescribed by the physician.
- Performs frequent suctioning to clear secretions and prevent aspiration pneumonia.
- Regularly checks chest rise symmetry, breath sounds, and respiratory effort to detect changes.
- Administers humidified oxygen, chest physiotherapy, and postural drainage when indicated.
- She ensures closed suction systems are clean and functioning to avoid contamination.
✅ 2. Neurological Monitoring and Assessment
- Uses Glasgow Coma Scale (GCS) every 1–2 hours to evaluate consciousness level.
- Observes for pupil size, reaction to light, and symmetry to monitor cranial nerve function.
- Monitors for abnormal movements, posturing (decorticate, decerebrate), or seizures.
- Records intracranial pressure (ICP) if an ICP monitor is in place and ensures its functioning.
- Applies stimulus-response testing, like nail bed pressure, to detect motor response.
- Reports neurological deterioration signs such as Cushing’s triad (bradycardia, hypertension, irregular respirations).
✅ 3. Hemodynamic and Cardiovascular Monitoring
- Performs continuous monitoring of heart rate, BP, ECG, oxygen saturation, and CVP if indicated.
- Administers inotropic agents, antihypertensives, or fluids to stabilize cardiovascular status.
- Monitors for shock, arrhythmias, or fluid overload, especially in ventilated patients.
- Maintains accurate hourly input-output records, including NG feed, IV, and urine.
- Uses central line access care protocols to prevent line-related infections.
- Assists in preparing the patient for emergency interventions like defibrillation or transvenous pacing if needed.
✅ 4. Nutritional and Fluid Management
- Starts enteral feeding within 24–48 hours using a nasogastric or PEG tube.
- Monitors for feeding intolerance like high gastric residuals, vomiting, or bloating.
- Administers TPN via central line if enteral route is contraindicated or ineffective.
- Calculates caloric, protein, and fluid requirements in consultation with dietitian.
- Maintains strict electrolyte monitoring (Na⁺, K⁺, Ca²⁺) and corrects imbalances.
- Flushes feeding tubes regularly to prevent clogging and ensures correct tube position.
✅ 5. Skin Integrity and Pressure Ulcer Prevention
- Repositions the patient every 2 hours using proper log-roll technique to prevent pressure ulcers.
- Uses pressure-relieving devices like air mattresses, foam cushions, and water beds.
- Inspects bony prominences (sacrum, heels, scapula) for redness, blisters, or skin breakdown.
- Keeps skin clean and dry, especially in incontinent patients.
- Applies barrier creams and follows a structured turning schedule.
- Educates caregivers and staff on pressure ulcer prevention protocols.
✅ 6. Eye and Mouth Care
- Provides eye lubrication drops to prevent corneal abrasions due to reduced blinking.
- Applies eye patches or closes eyelids manually in cases of incomplete lid closure.Performs oral hygiene every 4 hours using chlorhexidine or antiseptic solutions.
- Cleans the tongue, gums, and oral cavity to prevent ventilator-associated pneumonia (VAP).
- Keeps lips moisturized and crack-free using petroleum jelly.
- Monitors for mouth ulcers, dental caries, or bad breath as signs of infection.
✅ 7. Bowel and Bladder Management
- Monitors bowel movement patterns, reports constipation or diarrhea.
- Administers stool softeners or suppositories as needed.
- Ensures sterile urinary catheter insertion and care, monitors for signs of UTI.
- Maintains hourly urine output chart, especially for patients on diuretics or with kidney issues.
- Uses bladder scanners to monitor retention before catheterizing.
- Maintains perineal hygiene after bowel/bladder incontinence to prevent dermatitis.
✅ 8. Infection Control and Asepsis
- Practices strict hand hygiene and PPE (gloves, mask, gown) usage.
- Performs aseptic suctioning, catheterization, and dressing changes.
- Monitors for early signs of infection: fever, tachycardia, increased WBC, cloudy urine, or purulent sputum.
- Maintains daily device care logs (e.g., IV line, trach care, central line).
- Follows isolation precautions for immunocompromised or infected patients.
- Educates family and staff on infection control policies inside ICU.
✅ 9. Psychological and Emotional Support
- Talks to the comatose patient during procedures to provide comfort and orientation, as some patients can hear.
- Encourages family involvement with verbal reassurance and therapeutic touch.
- Updates the family on daily condition and changes in care plans.
- Supports family decision-making regarding end-of-life care and prognosis discussions.
- Maintains calm, low-noise ICU environment to promote healing.
- Refers to spiritual care providers or counselors based on family preference.
✅ 10. Documentation and Communication
- Documents vital signs, GCS, neuro and respiratory observations, intake/output, and interventions hourly or per protocol.
- Maintains shift-wise nursing notes and communication logs for the healthcare team.
- Uses flow charts for GCS, ICP, ventilator data, infection control audits.
- Reports abnormal changes immediately to physicians for timely intervention.
- Participates in daily ICU rounds to ensure coordinated care planning.
- Documents family updates, consent forms, and legal instructions carefully.
4. Role of nurse for care of elederly
The role of the nurse in geriatric care includes holistic management of the elderly, addressing their physical, mental, emotional, and social needs while promoting independence and dignity.
✅ 1. Comprehensive Physical Assessment and Monitoring
- The nurse performs routine head-to-toe physical assessments to detect early signs of deterioration in elderly patients.
- She monitors chronic illnesses such as diabetes, hypertension, arthritis, and cardiac conditions through daily observations and scheduled investigations.
- The nurse evaluates the elderly person’s ability to perform ADLs (Activities of Daily Living) and determines the need for assistive support.
- She also screens for hearing loss, vision problems, oral health issues, and foot complications.
- The nurse observes for signs of elder abuse or neglect, especially in dependent or bedridden patients.
✅ 2. Medication Administration and Safety
- The nurse is responsible for accurate timing, dosage, and route of administration of prescribed medications.
- She monitors for adverse drug effects, allergic reactions, or overdose—especially in patients on multiple medications.
- The nurse maintains a medication administration record (MAR) to track compliance and modifications.
- She collaborates with physicians for regular medication review and deprescribing when appropriate.
- The nurse provides patient and caregiver teaching on the purpose and potential side effects of medications.
✅ 3. Nutritional Care and Hydration
- The nurse assesses the nutritional status by monitoring weight trends, BMI, and lab indicators like albumin and hemoglobin.
- She identifies and addresses chewing difficulties, poor dentition, or loss of taste which affect food intake.
- The nurse ensures dietary modifications for specific illnesses, such as low-sodium for hypertension or diabetic-friendly meals.
- She promotes supplementation of vitamins and minerals as required by the aging body.
- The nurse encourages mealtime support, upright positioning, and slow feeding to reduce aspiration risk.
✅ 4. Mobility Support and Fall Prevention
- The nurse assists elderly patients with daily ambulation, physiotherapy routines, and walking exercises to maintain mobility.
- She provides training on safe use of assistive devices such as canes, walkers, or wheelchairs.
- The nurse evaluates environmental safety, including non-slippery floors, grab bars, and clutter-free pathways.
- She observes for signs of dizziness or hypotension that may lead to falls during standing or walking.
- The nurse participates in institutional fall-prevention programs and uses fall-risk scoring tools.
✅ 5. Psychosocial and Emotional Support
- The nurse recognizes signs of depression, anxiety, grief, or hopelessness, and provides emotional support.
- She encourages participation in social gatherings, spiritual groups, or elderly day-care programs to avoid isolation.
- The nurse builds a trust-based relationship that allows the elderly to express fears or past memories.
- She coordinates with social workers to provide support systems for financially or emotionally neglected elders.
- The nurse facilitates family counseling sessions to improve intergenerational relationships and caregiving harmony.
✅ 6. Cognitive Support and Mental Health Monitoring
- The nurse routinely assesses for confusion, memory loss, disorientation, and behavioral changes.
- She uses tools like the Mini-Mental State Examination (MMSE) for cognitive screening.
- The nurse introduces mental stimulation techniques such as reality orientation, name recall, date charts, and music therapy.
- She helps establish routines for consistency and reduced anxiety, especially for Alzheimer’s patients.
- The nurse involves family in behavioral therapy and home safety planning for patients with cognitive decline.
✅ 7. Skin Integrity and Hygiene Care
- The nurse performs daily skin inspections for pressure areas and uses a Braden scale for pressure ulcer risk assessment.
- She ensures regular cleansing, moisturizing, and protective barriers to keep skin soft and infection-free.
- The nurse uses special mattresses, cushions, and heel protectors to reduce prolonged pressure.
- She maintains proper perineal care and incontinence hygiene, especially in bedridden patients.
- The nurse teaches caregivers about pressure sore staging and early signs of breakdown.
✅ 8. Bladder and Bowel Management
- The nurse encourages regular toileting and maintains a timed voiding schedule to avoid incontinence.
- She observes for signs of urinary retention, infection, or constipation, especially in immobile or post-operative patients.
- The nurse promotes pelvic floor exercises in cooperative patients to strengthen sphincter control.
- She ensures safe and sterile catheter care and minimizes catheter use to prevent infections.
- The nurse maintains elimination charts and updates them during clinical shift reports.
✅ 9. Education and Health Counseling
- The nurse provides education on preventive health measures, such as vaccination, oral hygiene, and foot care in diabetics.
- She encourages lifestyle modifications including diet, sleep hygiene, and gentle physical activity.
- The nurse offers counseling regarding acceptance of aging, body image changes, and dependency issues.
- She assists in preparing legal documents like advanced directives, DNR orders, and wills when needed.
- The nurse empowers caregivers through training on safe handling, communication, and coping skills.
✅ 10. Collaboration and Rehabilitation Support
- The nurse works as part of a multidisciplinary team to ensure integrated geriatric care.
- She refers to occupational therapy for hand-function, grooming, and bathing adaptations.
- The nurse coordinates with home healthcare services, hospice, or old-age homes based on individual needs.
- She supports adaptive training with aids like grab bars, feeding spoons, dressing devices, and ensures elderly can live with dignity.
- The nurse participates in community geriatric programs and assists with elder welfare schemes and insurance.
5. Retinal detachment
Definition of Retinal Detachment
- It is a serious ophthalmologic condition in which the sensory retina separates from the underlying retinal pigment epithelium (RPE) within the eye.
- It is a condition that leads to loss of blood supply and nutrition to the photoreceptors, which may cause permanent vision loss if not treated promptly.
- It is considered a medical emergency that often requires surgical repair.
Types of Retinal Detachment
1️⃣ Rhegmatogenous Retinal Detachment
- It is the most common type, occurring due to a retinal tear or break.
- It is caused by vitreous fluid leaking under the retina, separating it from the RPE.
- It is often seen in older adults, especially those with high myopia or after cataract surgery.
2️⃣ Tractional Retinal Detachment
- It is caused by fibrous or vascular tissue pulling the retina away from the RPE.
- It is commonly seen in patients with proliferative diabetic retinopathy or retinopathy of prematurity (ROP).
- It is not associated with a retinal break or tear.
3️⃣ Exudative (Serous) Retinal Detachment
- It is due to fluid accumulation beneath the retina without any tear.
- It may result from inflammatory conditions, tumors, or hypertensive retinopathy.
- It usually requires treatment of the underlying systemic condition.
Etiology
- Retinal tear or hole
- High myopia (nearsightedness)
- Eye trauma
- Post-cataract surgery
- Diabetic retinopathy
- Inflammatory eye diseases
- Ocular tumors
- Family history of detachment
Pathophysiology of Retinal Detachment
1️⃣ Vitreous Degeneration or Trauma
It is due to aging or trauma, which causes liquefaction and shrinkage of the vitreous humor, leading to traction on the retina.
2️⃣ Formation of Retinal Tear or Hole
It is at this stage that a small break develops, allowing fluid to pass through.
3️⃣ Subretinal Fluid Accumulation
It is this fluid that accumulates between the neurosensory retina and RPE, progressively lifting the retina away.
4️⃣ Photoreceptor Dysfunction
It is the separation from RPE that leads to ischemia and loss of photoreceptor function.
5️⃣ Progression to Permanent Vision Loss
It is in untreated cases that central vision is lost, especially if the macula is involved
Clinical Manifestations (Signs & Symptoms)
- Sudden floaters
- Flashing lights (photopsia)
- Curtain-like shadow over vision
- Painless vision loss
- Blurred or distorted central vision
- Reduced peripheral vision
Diagnostic Evaluation
- History collection
- Physical examination
- Ophthalmoscopy
- Slit-lamp examination
- Ultrasound B-scan
- Optical Coherence Tomography (OCT)
- Visual acuity test
- Visual field testing (perimetry)
Medical Management
1️⃣ Small Retinal Tears (Without Detachment)
- It is managed using laser photocoagulation or cryopexy, which creates a scar to seal the tear.
2️⃣ Rhegmatogenous Detachment
It is treated with :
- Pneumatic retinopexy : It involves injecting a gas bubble to press retina back in place.
- Scleral buckling : It involves placing a silicone band around the eye to relieve vitreous traction.
- Vitrectomy : It involves removing the vitreous gel and replacing it with gas or silicone oil.
3️⃣ Tractional Detachment
- It is usually treated with pars plana vitrectomy to remove the fibrous bands causing traction.
4️⃣ Exudative Detachment
- It is managed by treating the underlying condition, e.g., inflammation, tumor, or vascular disease.
Nursing Management
1️⃣ Assessment
- It is important to assess for visual disturbances, such as flashes of light, floaters, or visual field defects.
- It is necessary to monitor for any change in visual acuity and patient-reported loss of peripheral or central vision.
- It is essential to observe for signs of anxiety or fear, as vision loss may cause psychological distress.
2️⃣ Pre-operative Nursing Care
- It is crucial to instruct the patient to avoid straining or sudden head movements, which may worsen detachment.
- It is necessary to provide emotional support and educate the patient about the urgency of surgery.
- It is important to maintain NPO status if surgery is planned.
3️⃣ Post-operative Nursing Care
- It is essential to instruct the patient on proper head positioning, especially if intraocular gas is used (face-down position).
- It is vital to monitor for eye pain, discharge, redness, or signs of infection.
- It is necessary to administer eye drops as prescribed, including antibiotics and corticosteroids.
- It is important to advise the patient to avoid air travel until the intraocular gas is absorbed.
- It is essential to educate about gradual return of vision and the need for follow-up appointments.
4️⃣ Health Education
- It is the nurse’s duty to teach about risk factor control, including blood pressure and blood sugar management.
- It is important to instruct on recognizing early warning signs of recurrence or detachment in the other eye.
- It is helpful to provide information on visual aids and rehabilitative services if vision loss is permanent.
Complications
- It may lead to permanent blindness if not treated on time.
- It may result in proliferative vitreoretinopathy (PVR) or recurrent detachment after surgery.
- It may cause macular damage and loss of central vision.
Q.6 Answer the following
1. Types of disasters (2)
✅ 1. Natural Disasters
These are disasters that occur due to natural forces or phenomena without human interference.
- Earthquake
- Flood
- Cyclone / Hurricane / Typhoon
- Tsunami
- Landslide
- Volcanic eruption
- Drought
- Heat wave / Cold wave
✅ 2. Man-made (Anthropogenic) Disasters
These occur due to human activities, negligence, or intentional acts.
- Industrial accident
- Fire accident
- Transport accident (road, rail, air, sea)
- Nuclear disaster
- Building collapse
- War and terrorism
- Environmental degradation
✅ 3. Biological Disasters
These result from outbreaks or spread of diseases and toxins affecting humans, animals, or crops.
- Epidemic
- Pandemic
- Bioterrorism
- Zoonotic disease
- Insect infestation
- Toxin or poison exposure
✅ 4. Technological Disasters
A subset of man-made disasters that result from failures in technology or systems.
- Cyber attacks
- Dam failures
- Power grid failures
- Data leaks
2. Role of nurse in disaster management (5)
A nurse plays a multidimensional role during all four phases of disaster management: preparedness, response, recovery, and mitigation. Nurses are the backbone of healthcare delivery in emergencies, offering clinical care, emotional support, and leadership to individuals and communities affected by disasters.
1. Role of Nurse in Disaster Preparedness Phase
- This is the pre-disaster phase where planning, training, and organization take place to reduce the impact of the disaster.
- It is the nurse’s responsibility to actively participate in hospital disaster planning committees and contribute knowledge toward making realistic and effective response strategies.
- The nurse should attend regular disaster drills and mock codes, ensuring familiarity with evacuation routes, emergency procedures, and disaster protocols.
- The nurse must educate patients, families, and communities about disaster types common to their region (e.g., earthquakes, floods, fire) and how to respond to them.
- The nurse is responsible for preparing personal and institutional emergency kits, including first aid supplies, medications, sterile dressings, gloves, IV fluids, and emergency contact lists.
- The nurse collaborates with other healthcare professionals and local authorities to assess community risks and vulnerabilities and develop action plans.
- It is also vital for the nurse to assist in creating communication flowcharts, so everyone knows whom to contact and what to do during emergencies.
- The nurse may lead public education campaigns on hygiene, disease prevention, and personal safety during disasters.
2. Role of Nurse in Disaster Response Phase
- This phase occurs during or immediately after the disaster, where the focus is on saving lives, preventing complications, and minimizing injuries.
- It is the nurse’s immediate responsibility to perform triage, which involves sorting patients based on injury severity using color-coded tags (e.g., red for urgent, yellow for delayed).
- The nurse provides life-saving emergency care, including controlling hemorrhage, managing airway, performing CPR, administering IV fluids, and stabilizing fractures.
- The nurse assists in evacuation procedures, ensuring that critically ill patients are safely transported to emergency shelters or hospitals.
- The nurse should maintain infection control measures in temporary shelters or field hospitals by ensuring proper waste disposal, hand hygiene, and use of PPE.
- The nurse maintains accurate records of victims treated, including personal details, injuries, treatments provided, and referrals.
- It is the nurse’s duty to communicate with relatives, provide updates on victim status, and offer emotional reassurance.
- In mass casualty incidents, the nurse also coordinates with ambulance services, disaster relief workers, and military personnel to streamline care delivery.
3. Role of Nurse in Disaster Recovery Phase
- This phase involves returning the affected individuals and communities back to normal life and rebuilding healthcare services.
- The nurse assists in wound care, rehabilitation, follow-up of chronic conditions, and psychological counseling for trauma victims.
- It is the nurse’s duty to identify long-term care needs, such as orthopedic rehabilitation, prosthetics for amputees, or continued treatment for burns.
- The nurse provides grief counseling and emotional support for individuals who lost loved ones, homes, or jobs.
- Nurses help in restoring healthcare infrastructure, such as setting up mobile health units or reopening damaged clinics.
- The nurse participates in health assessments and surveillance, identifying outbreaks of communicable diseases post-disaster (e.g., diarrhea, malaria, leptospirosis).
- It is the nurse’s role to conduct home visits to check on elderly, disabled, or pregnant women affected by the disaster.
- The nurse assists in government relief work, such as filling forms for compensation, housing, or ration supply.
4. Role of Nurse in Mitigation Phase
- Mitigation involves reducing the long-term risk and impact of future disasters.
- The nurse works with public health teams to educate the community about preventive actions, like securing heavy furniture in earthquake-prone zones or using mosquito nets to prevent vector-borne diseases.
- It is the nurse’s responsibility to improve community resilience by encouraging regular drills, early warning alerts, and safe construction practices.
- Nurses may engage in health mapping and environmental risk assessments to identify high-risk zones and vulnerable populations.
- The nurse provides counseling on stress management and trauma recovery, helping communities build psychological strength.
- Nurses help evaluate existing disaster plans, suggest improvements, and participate in research to identify gaps in disaster response.
5. Ethical and Professional Role of Nurse in Disasters
- It is essential that nurses practice non-discriminatory care, giving equal attention to all affected individuals regardless of age, gender, caste, or financial status.
- Nurses must maintain patient confidentiality, even in chaotic environments like emergency shelters or open field hospitals.
- The nurse should demonstrate calm, leadership behavior, helping to reduce panic and maintain order.
- The nurse advocates for vulnerable populations like children, disabled persons, pregnant women, and elderly who are often overlooked during mass relief efforts.
- It is the nurse’s ethical duty to self-monitor for fatigue or burnout and seek help if needed, to ensure optimal care delivery.
6. Communication & Coordination Role
- Nurses should maintain clear, timely, and accurate communication with physicians, disaster teams, NGOs, and local authorities.
- They may serve as a liaison between victims and rescue agencies, helping victims understand available services.
- Nurses must report outbreaks or deaths to public health authorities immediately to activate containment measures.
- They are often responsible for collaborating with media teams, when assigned, to deliver public health messages or announcements.
7. Documentation and Evaluation Role
- The nurse must record all medical care provided, resources used, number of people assisted, and any referrals made.
- Documentation helps in financial audits, legal accountability, and future disaster policy formulation.
- Nurses should assist in post-disaster evaluation reports, offering suggestions for what worked well and what needs improvement.
- These reports contribute to national disaster database systems, enhancing preparedness for future events.
💥WELCOME TO MY NURSING APP FAMILY💥
KINDLY SEND YOUR UNIVERSITY PAPER FOR SAMPLE SOLUTION OR FOR MORE INFO CONTACT US ON-CALL/WATSAPP – 8485976407
