😡PAPER NO.1-B.Sc. (NURSING)- SEPTEMBER:-2019PHARMACOLOGY, PATHOLOGY & GENETICS (DONE-UPLOAD)
PAPER SOLUTION NO.1-B.Sc. (NURSING)- SEPTEMBER:-2019-PHARMACOLOGY, PATHOLOGY & GENETICS (BKNMU)
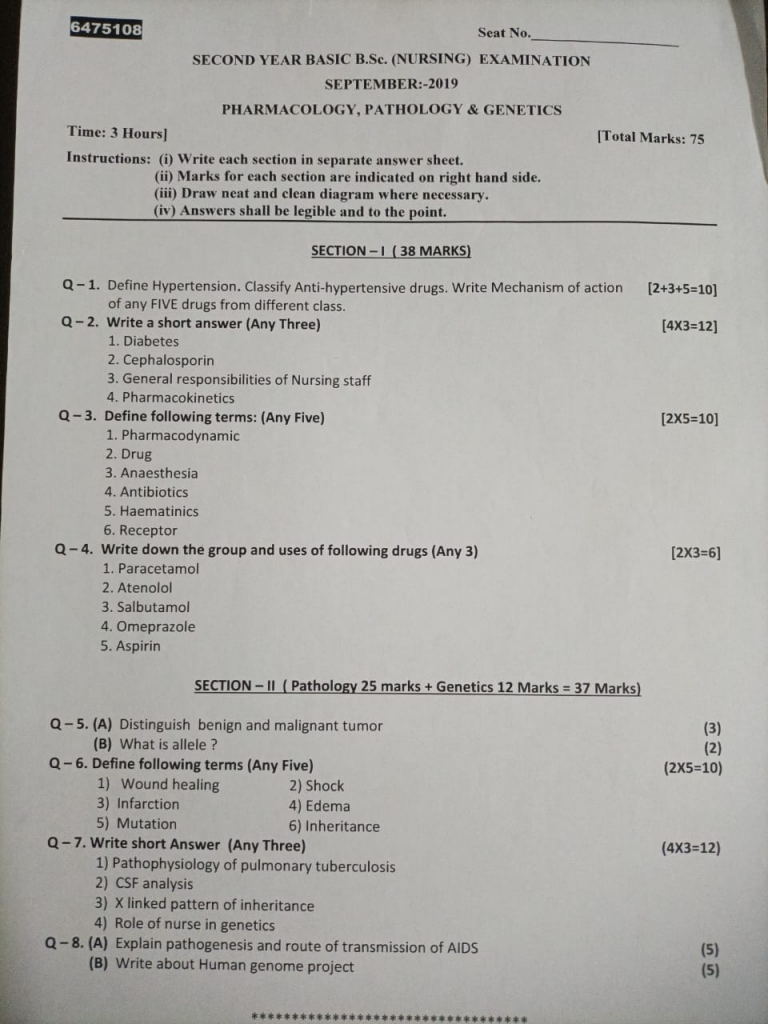
🔸 SECTION-1🔸
🔸Q-1. Define Hypertension. Classify Anti-hypertensive drugs. Write Mechanism of action of any FIVE drugs from different class.
- Definition of Hypertension Hypertension, commonly known as high blood pressure, is a chronic medical condition characterized by persistently elevated blood pressure levels. Blood pressure is measured as the force exerted by circulating blood on the walls of blood vessels, and it is typically expressed as two values:
- systolic blood pressure (the pressure when the heart beats) over diastolic blood pressure (the pressure when the heart rests between beats).
- Hypertension is generally defined as having a blood pressure reading of 130/80 mmHg or higher.
- Classification of Anti-Hypertensive Drugs Anti-hypertensive drugs are classified into several categories based on their mechanisms of action:
1.Diuretics
Examples: Hydrochlorothiazide, Furosemide, Spironolactone
Mechanism of Action: Diuretics increase the excretion of sodium and water from the body, which reduces blood volume and decreases blood pressure. Thiazide diuretics work primarily on the distal convoluted tubule, while loop diuretics act on the ascending loop of Henle and potassium-sparing diuretics act on the collecting duct.
2.ACE Inhibitors
Examples: Lisinopril, Enalapril, Ramipril
Mechanism of Action: ACE inhibitors block the enzyme angiotensin-converting enzyme (ACE), which prevents the conversion of angiotensin I to angiotensin II. Angiotensin II is a potent vasoconstrictor that increases blood pressure, so inhibiting its formation leads to vasodilation and reduced blood pressure.
3.Angiotensin II Receptor Blockers (ARBs)
Examples: Losartan, Valsartan, Irbesartan
Mechanism of Action: ARBs block the angiotensin II receptors (AT1 receptors) on blood vessels, preventing angiotensin II from causing vasoconstriction and increasing blood pressure.
4.Calcium Channel Blockers
Examples: Amlodipine, Diltiazem, Verapamil
Mechanism of Action: Calcium channel blockers inhibit calcium entry into vascular smooth muscle and cardiac cells. This results in vasodilation and reduced cardiac output, both of which lower blood pressure.
5.Beta-Blockers
Examples: Metoprolol, Atenolol, Carvedilol
Mechanism of Action: Beta-blockers block beta-adrenergic receptors in the heart and blood vessels. This reduces heart rate, cardiac output, and the release of renin from the kidneys, which ultimately lowers blood pressure.
6.Alpha-1 Blockers
Examples: Prazosin, Doxazosin, Terazosin
Mechanism of Action: Alpha-1 blockers inhibit alpha-1 adrenergic receptors on vascular smooth muscle, causing vasodilation and a reduction in blood pressure.
7.Alpha-2 Agonists
Examples: Clonidine, Methyldopa
Mechanism of Action: Alpha-2 agonists stimulate alpha-2 adrenergic receptors in the central nervous system, which decreases sympathetic nervous system activity and lowers blood pressure.
8.Direct Renin Inhibitors
Examples: Aliskiren
Mechanism of Action: Direct renin inhibitors prevent renin from converting angiotensinogen to angiotensin I, thus reducing the production of angiotensin II and lowering blood pressure.Each class of anti-hypertensive drugs has a unique mechanism of action that targets different aspects of the blood pressure regulation system, allowing for a range of therapeutic strategies to manage hypertension.
Q-2. Write a short answer (Any Three)
🔸1.Diabetes
Diabetes is a chronic metabolic disorder characterized by elevated blood glucose (sugar) levels. This condition occurs either due to insufficient insulin production, inadequate insulin action, or both.
Types of Diabetes
- 1.Type 1 Diabetes:
Cause: Autoimmune destruction of insulin-producing beta cells in the pancreas.
Onset: Typically develops in childhood or early adulthood.
Management: Requires lifelong insulin therapy, along with monitoring blood glucose levels, diet, and exercise.
- 2.Type 2 Diabetes:
Cause: Insulin resistance combined with insufficient insulin production.
Onset: Usually develops in adults over the age of 45, though increasing numbers of younger individuals are being diagnosed.
Management: Often managed through lifestyle changes (diet and exercise), oral medications, and sometimes insulin.
- 3.Gestational Diabetes:
Cause: Insulin resistance that occurs during pregnancy.
Onset: Develops during pregnancy and typically resolves after childbirth.
Management: Requires monitoring of blood glucose levels and lifestyle adjustments during pregnancy; women are at higher risk of developing type 2 diabetes later in life.
- 4.Other Specific Types:
Includes conditions resulting from genetic mutations, diseases of the pancreas, or secondary to medications.
Symptoms
Common symptoms include:
- Frequent urination
- Excessive thirst
- Unexplained weight loss
- Fatigue
- Blurred vision
- Slow-healing sores Complications
If poorly managed, diabetes can lead to severe complications:
Cardiovascular Disease: Increased risk of heart disease and stroke.
Neuropathy: Nerve damage that can lead to pain, tingling, or loss of sensation.
Retinopathy: Damage to the blood vessels in the retina, potentially leading to blindness.
Nephropathy: Kidney damage that can progress to kidney failure.
Foot Problems: Increased risk of infections and ulcers.
Diagnosis Diagnosis is typically based on blood tests such as:
- Fasting Blood Glucose Test
- Oral Glucose Tolerance Test
- Hemoglobin A1c Test (average blood glucose levels over 2-3 months)
- Management
Effective management involves:
Monitoring Blood Glucose Levels: Regular checks to manage blood sugar.
Medications: Insulin or oral medications to control blood sugar levels.
Diet: A balanced diet with controlled carbohydrate intake.
Exercise: Regular physical activity to help regulate blood sugar.
Education: Ongoing education about the condition and self-care strategies.
Prevention
- For Type 2 diabetes, lifestyle modifications can significantly reduce the risk:
- Maintain a healthy weight.
- Eat a balanced diet rich in fruits, vegetables, and whole grains.
- Engage in regular physical activity.
- Avoid smoking and limit alcohol consumption.
- Early detection and proactive management are essential to managing diabetes effectively and preventing complications.
🔸2.Cephalosporin
Cephalosporins are a group of broad-spectrum antibiotics used to treat various bacterial infections. They are derived from the fungus Acremonium (formerly called Cephalosporium).
Classification Cephalosporins are classified into generations based on their spectrum of activity and development over time:
1.First-Generation Cephalosporins:
Examples: Cephalexin, Cefazolin.
Coverage: Effective against Gram-positive bacteria (like Staphylococcus and Streptococcus) and some Gram-negative bacteria.
Common Uses: Skin infections, preoperative prophylaxis, and uncomplicated urinary tract infections (UTIs).
2.Second-Generation Cephalosporins:
Examples: Cefuroxime, Cefoxitin.
Coverage: Broader Gram-negative coverage compared to first-generation, with some Gram-positive activity.
Common Uses: Respiratory infections, sinusitis, and some intra-abdominal infections.
3.Third-Generation Cephalosporins:
Examples: Ceftriaxone, Ceftazidime.
Coverage: More effective against Gram-negative bacteria, with some also targeting Gram-positive bacteria.
Common Uses: Severe infections like pneumonia, meningitis, and complicated UTIs.
4.Fourth-Generation Cephalosporins:
Examples: Cefepime.
Coverage: Broad-spectrum activity against both Gram-positive and Gram-negative bacteria.
Common Uses: Hospital-acquired infections, including severe infections like febrile neutropenia.
5.Fifth-Generation Cephalosporins:
Examples: Ceftaroline.
Coverage: Effective against Gram-positive bacteria, including methicillin-resistant Staphylococcus aureus (MRSA), and some Gram-negative bacteria.
Common Uses: Skin infections, community-acquired pneumonia.
Mechanism of Action
Cephalosporins inhibit bacterial cell wall synthesis by binding to penicillin-binding proteins (PBPs), which are crucial for cell wall formation. This leads to bacterial cell lysis and death.
- Common Indications
Respiratory Tract Infections: Pneumonia, bronchitis.
Skin and Soft Tissue Infections: Cellulitis, abscesses.
Urinary Tract Infections: Cystitis, pyelonephritis.
Bone and Joint Infections: Osteomyelitis, septic arthritis.
Intra-abdominal Infections: Peritonitis, diverticulitis.
Surgical Prophylaxis: Prevention of infections in surgical procedures.
- Side Effects
Common side effects include: Gastrointestinal issues: Nausea, diarrhea.
Allergic reactions: Rash, itching, anaphylaxis.
Superinfections: Overgrowth of non-susceptible organisms like Candida.
- Considerations
Allergies: Patients with penicillin allergies may also be allergic to cephalosporins.
Renal Function: Dosage adjustments may be needed in patients with kidney impairment.
Drug Interactions: Cephalosporins can interact with other medications, so informing healthcare providers of all current medications is important.
🔸3.General responsibilities of Nursing staff
Nursing staff play a critical role in the healthcare system, providing care and support to patients in various settings. Their responsibilities can be broadly categorized into several general areas:
- 1.Patient Care
Assessment: Conducting comprehensive assessments of patients’ physical, emotional, and psychological conditions.
Planning: Developing individualized care plans based on patient needs, preferences, and medical conditions.
Implementation: Administering medications, performing procedures, and delivering treatments as prescribed.
Monitoring: Observing patients for changes in health status, and documenting and reporting these changes to the healthcare team.
Evaluation: Reviewing the effectiveness of care plans and making adjustments as needed.
- 2.Communication
Patient Interaction: Providing compassionate, empathetic, and effective communication with patients and their families.
Team Collaboration: Coordinating with doctors, specialists, and other healthcare professionals to ensure cohesive patient care.
Education: Educating patients and families about health conditions, treatment options, and self-care techniques.
- 3.Documentation
Record Keeping: Maintaining accurate and up-to-date patient records, including medical history, treatment plans, and progress notes.
Reporting: Documenting incidents, patient responses to treatments, and any deviations from care plans.
- 4.Patient Advocacy
Representation: Advocating for the patient’s rights, preferences, and needs within the healthcare system.
Ethical Care: Ensuring that care is provided in an ethical manner, respecting patients’ dignity and autonomy.
5.Health Promotion and Prevention
Preventive Care: Offering vaccinations, screenings, and preventive measures to maintain health and prevent disease.
Health Education: Providing information on topics like nutrition, exercise, and lifestyle changes for disease prevention and health maintenance.
- 6.Emergency Response
Critical Care: Responding to medical emergencies, including administering first aid, performing CPR, and stabilizing patients.
Crisis Management: Managing acute situations and coordinating with emergency response teams when necessary.
- 7.Administrative Duties
Scheduling: Managing patient appointments, coordinating referrals, and handling administrative paperwork.
Inventory Management: Ordering and managing medical supplies and equipment, ensuring that necessary resources are available.
- 8.Professional Development
Continued Education: Engaging in ongoing education and training to stay current with medical advancements and best practices.
Certification: Maintaining professional certifications and licensure required for the nursing role.
- 9.Quality Improvement
Safety Initiatives: Participating in quality improvement programs aimed at enhancing patient care and safety.
Feedback: Providing feedback on practices and procedures to improve patient outcomes and the work environment.
- 10.Ethics and Compliance
Regulatory Adherence: Following legal and regulatory standards for patient care and documentation.
Ethical Standards: Upholding the ethical principles of nursing, including honesty, integrity, and respect for patients’ rights.
🔸4.Pharmacokinetics
- Pharmacokinetics is the branch of pharmacology that studies how a drug is absorbed, distributed, metabolized, and excreted in the body. It provides insights into the time course of drug actions and their effects, helping optimize dosing regimens and therapeutic outcomes. The primary components of pharmacokinetics are often summarized by the acronym ADME:
- 1.Absorption
Definition: The process by which a drug moves from the site of administration into the bloodstream.
Factors Affecting Absorption:
Route of Administration: Oral, intravenous, intramuscular, subcutaneous, etc.
Drug Formulation: Tablets, capsules, injections, etc.
Physiochemical Properties: Solubility, stability, and permeability of the drug.
Biological Factors: Gastric pH, presence of food, gastric emptying time.
- 2.Distribution
Definition: The process by which a drug spreads from the bloodstream to various tissues and organs.
Factors Affecting Distribution:
Blood Flow: Higher blood flow areas like the liver and kidneys receive more drug.
Plasma Protein Binding: Drugs can bind to proteins like albumin, affecting their free (active) concentration.
Tissue Permeability: Drug penetration into tissues based on properties like lipid solubility.
Volume of Distribution (Vd): The theoretical volume into which the drug distributes; it helps estimate drug dosing.
- 3.Metabolism
Definition: The chemical alteration of a drug by the body, primarily in the liver.
Phases of Metabolism:
Phase I: Chemical modifications like oxidation, reduction, or hydrolysis (e.g., via cytochrome P450 enzymes).
Phase II: Conjugation reactions that make the drug more water-soluble for excretion (e.g., glucuronidation, acetylation).
Factors Affecting Metabolism:
Enzyme Activity: Genetic variations, drug interactions, and liver function.
Age and Health Status: Metabolic rate varies with age, health, and disease states.
- 4.Excretion
Definition: The removal of the drug and its metabolites from the body.
Routes of Excretion:
Renal: Via urine (filtration, secretion, reabsorption processes in the kidneys).
Hepatic: Via bile and then feces.
Other: Sweat, saliva, and breast milk.
Factors Affecting Excretion:
Renal Function: Glomerular filtration rate, tubular secretion/reabsorption.
Liver Function:
Biliary excretion and metabolism.
pH of Urine: Affects drug reabsorption and elimination.
5.Pharmacokinetic Parameters Absorption Rate Constant (Ka): Rate at which a drug is absorbed into the bloodstream.
Bioavailability (F): Fraction of the administered dose that reaches systemic circulation.
Half-Life (t1/2): Time required for the drug concentration in the bloodstream to reduce by half.
Clearance (CL): Volume of blood cleared of the drug per unit time.
Peak Plasma Concentration (Cmax): Maximum concentration of the drug in the blood.
Time to Peak Concentration (Tmax): Time taken to reach Cmax.
Area Under the Curve (AUC): Total drug exposure over time.
Applications of Pharmacokinetics
Dosing Regimens : Designing effective dosing schedules to achieve therapeutic drug levels.
Drug Interactions: Predicting how drugs affect each other’s ADME processes.
Therapeutic Drug Monitoring: Adjusting dosages based on drug concentration measurements.
Drug Development: Designing new drugs with optimal ADME properties.
Q-3. Define following terms: (Any Five)
🔸1.Pharmacodynamic
- Pharmaco dynamics is a branch of pharmacology that explores the effects of drugs on the body and the mechanisms by which they exert their therapeutic and adverse effects. It focuses on understanding the relationship between drug concentrations at the site of action and the resulting physiological or biochemical responses. Here’s a detailed breakdown of pharmacodynamics:
Definition: The interaction between a drug and its specific target receptor, which triggers a biological response.
🔸2.Drug
- A drug is a substance used to diagnose, treat, cure, or prevent diseases and medical conditions, or to alleviate symptoms. Drugs can be natural or synthetic, and their effects are typically classified into several categories based on their uses and mechanisms of action. Here’s a comprehensive overview:
Definition: Drugs used to treat, cure, or manage diseases and medical conditions.
🔸3.Anaesthesia
- Anesthesia is a medical practice aimed at preventing pain and discomfort during surgical and medical procedures. It involves the use of medications and techniques to induce a temporary loss of sensation or consciousness. There are different types of anesthesia tailored to the needs of the patient and the procedure. Here’s an in-depth look at anesthesia, including its types, techniques, and applications.
Definition: A state of controlled unconsciousness where the patient is entirely unaware of the procedure.
🔸4.Antibiotics
- Antibiotics are medications used to prevent and treat bacterial infections. They work by targeting specific processes essential to bacteria but not to human cells, thereby eliminating or inhibiting the growth of bacteria. Here’s a detailed overview of antibiotics, including their classes, mechanisms of action, uses, and considerations.
Definition: A class of antibiotics derived from Penicillium fungi.
🔸5.Haematinics
- Haematinics are substances used to treat or prevent anemia by improving the production of red blood cells and increasing hemoglobin levels in the blood. They work by supplying essential nutrients required for red blood cell formation or by stimulating the bone marrow to produce more red blood cells. Here’s a comprehensive overview of haematinics, including their types, mechanisms of action, uses, and example.
Definition: Iron is a crucial component of hemoglobin in red blood cells, and its deficiency leads to iron-deficiency anemia.
🔸6.Receptor
- are specialized protein molecules located on the surface of or within cells that bind to specific molecules, called ligands, to initiate a biological response. Receptors play a critical role in cellular communication and the regulation of physiological processes. Here’s a detailed overview of receptors, including their types, mechanisms of action, and roles in pharmacology
Definition: Receptors are protein structures that recognize and bind specific chemical signals (ligands), which then trigger a series of biochemical events inside the cell.
Q-4. Write down the group and uses of following drugs (Any 3)
🔸1.Paracetamol
Group: Paracetamol is classified as an analgesic and antipyretic drug. It belongs to the non-opioid analgesics and is commonly used for its pain-relieving and fever-reducing effects.
Uses: Paracetamol is primarily used to alleviate mild to moderate pain such as headaches, muscle aches, and menstrual cramps. It is also effective in reducing fever associated with conditions like colds and influenza. Additionally, it can be used to manage osteoarthritis pain and as part of combination therapies for post-surgical pain. Paracetamol is preferred for its safety profile compared to NSAIDs for short-term use and is often recommended for children and individuals with gastrointestinal issues.
These references offer detailed information on the classification and uses of paracetamol.
🔸2.Atenolol
Group: Atenolol is a beta-blocker medication, specifically a selective beta-1 adrenergic antagonist.
Uses: Atenolol is primarily used to manage hypertension (high blood pressure) and angina pectoris (chest pain due to heart disease). It is also prescribed for the prevention of heart attacks and to treat chronic heart failure. Additionally, it can be used for arrhythmias (irregular heartbeats) and to improve outcomes in patients with myocardial infarction.
🔸3.Salbutamol
Group: Salbutamol is a beta-2 adrenergic agonist and falls under the category of bronchodilators.
Uses: Salbutamol is primarily used for the relief of bronchospasm associated with conditions like asthma and chronic obstructive pulmonary disease (COPD). It works by stimulating beta-2 adrenergic receptors in the bronchial smooth muscle, leading to relaxation of the muscles and improved airflow. Salbutamol is commonly used as a rescue inhaler for acute asthma attacks and to provide preventive relief from exercise-induced bronchoconstriction.
🔸4.Omeprazole
Group: Omeprazole is a proton pump inhibitor (PPI).
Uses: Omeprazole is primarily used to treat gastroesophageal reflux disease (GERD) and peptic ulcers. It works by inhibiting the proton pump in the stomach lining, which reduces the production of stomach acid. This action helps heal ulcers, manage acid reflux, and reduce acid-related discomfort. Omeprazole is also used in combination with antibiotics to treat Helicobacter pylori infection and to prevent NSAID-induced gastric ulcers.
🔸5.Aspirin
Group: Aspirin is classified as a non-steroidal anti-inflammatory drug (NSAID) and specifically an acetylsalicylic acid.
Uses: Aspirin is used for various medical conditions due to its anti-inflammatory, analgesic, and antipyretic properties. It is commonly prescribed for the management of pain and fever. Additionally, aspirin is used for the prevention of cardiovascular events such as heart attacks and stroke due to its ability to inhibit platelet aggregation. It is also utilized for chronic conditions like rheumatoid arthritis and osteoarthritis for its anti-inflammatory effects.
🔸SECTION-II🔸 (Pathology 25 marks + Genetics 12 Marks = 37 Marks)
Q-5.🔸 (A) Distinguish benign and malignant tumor
Benign tumors and malignant tumors are two distinct types of neoplasms with several key differences.
Growth Pattern: Benign tumors grow slowly and are well-circumscribed, meaning they have clear boundaries and do not invade surrounding tissues. They remain localized and do not spread to other parts of the body. In contrast, malignant tumors grow more rapidly and invade nearby tissues. They have an infiltrative growth pattern, meaning they invade and destroy adjacent tissues and can spread to distant organs through the bloodstream or lymphatic system.
Cellular Characteristics: Cells in benign tumors are well-differentiated and closely resemble normal tissue cells in both appearance and function. Their nuclei are typically normal in size and shape. Conversely, malignant tumor cells are poorly differentiated, with significant abnormalities in cell structure and function. They often exhibit irregular nuclei with a high nuclear-to-cytoplasmic ratio and show signs of pleomorphism, meaning there is significant variation in size and shape among the cells.
Metastasis: Benign tumors do not metastasize, meaning they do not spread to other parts of the body. They are generally localized and can often be completely removed with surgery. Malignant tumors, on the other hand, have the potential to metastasize, spreading cancer cells to distant sites through the bloodstream or lymphatic system, which complicates treatment and increases the risk of a poor prognosis.
Clinical Impact: Benign tumors are usually less life-threatening but can cause issues if they press on vital structures or organs. Treatment often involves surgical removal, and there is usually a low risk of recurrence if the tumor is completely excised. Malignant tumors are more dangerous due to their aggressive nature and potential to spread. They often require a combination of treatments such as surgery, chemotherapy, and radiation therapy, and they have a higher chance of recurrence or progression.
Histological Features: Histologically, benign tumors have a more uniform appearance with well-defined margins and less vascularity. Malignant tumors, in contrast, display a heterogeneous appearance with irregular borders and increased blood vessel formation. They also exhibit invasive growth patterns that can destroy surrounding tissues.
In summary, benign tumors are non-invasive and localized with a generally favorable outcome, while malignant tumors are aggressive, invasive, and capable of spreading to other body parts, often requiring more intensive treatment and management.
🔸(B) What is allele ?
An allele is a variant form of a gene found at a specific location on a chromosome. Alleles contribute to the genetic diversity within a population and determine various traits and characteristics.
Key Characteristics of Alleles
1.Gene Variants:
Alleles are different versions of a gene. For example, the gene for flower color in pea plants has different alleles for purple and white flowers.
2.Genetic Locus:
Each allele occupies a specific position on a chromosome called a locus. This locus is the same for all members of a species, but the alleles at that locus can vary.
3.Types of Alleles:
Dominant Alleles: These alleles express their trait even if only one copy is present. For instance, in the gene for flower color, a purple flower allele (P) is dominant over a white flower allele (p).
Recessive Alleles: These alleles express their trait only if two copies are present. For instance, a white flower color will only appear if both alleles are for white flowers (pp).
4.Homozygous vs. Heterozygous:
Homozygous: An organism has two identical alleles for a particular gene (e.g., PP or pp).
Heterozygous: An organism has two different alleles for a particular gene (e.g., Pp).
5.Expression of Traits:
Alleles contribute to the phenotype, which is the observable expression of traits. For example, the presence of the dominant purple allele (P) will result in purple flowers regardless of the presence of a white allele.
Examples of Alleles
Human Blood Groups:
The ABO blood group system involves three alleles: A, B, and O. The combinations of these alleles determine the blood group (e.g., AA or AO for type A blood).
Pea Plant Traits:
In pea plants, the gene for seed shape has two alleles: round (R) and wrinkled (r). The round allele is dominant, so a plant with Rr or RR will have round seeds.
Eye Color in Humans:
Alleles for eye color include brown (B), blue (b), and green (G). Brown is dominant over blue and green, while green is typically dominant over blue.
Genetic Inheritance
Mendelian Inheritance:
Gregor Mendel’s principles describe how alleles are inherited from one generation to the next. His work showed that each parent contributes one allele to the offspring, and the combination of these alleles determines the offspring’s traits.
Punnett Squares:
These tools are used to predict the probability of an offspring inheriting particular alleles and therefore certain traits based on the parents’ genetic makeup.
Applications in Genetics
Genetic Disorders:
Alleles can be associated with genetic disorders. For instance, the allele for sickle cell anemia (S) is recessive, and individuals need two copies of this allele (SS) to express the disease.
Genetic Research:
Understanding alleles helps in genetic research, including the study of genetic variations, inheritance patterns, and the development of treatments for genetic diseases.
Q-6. Define following terms (Any Five)
🔸1) Wound healing
Wound healing is a complex biological process involving the repair of damaged tissue. It occurs in several phases:
1.Hemostasis and Inflammation:
Hemostasis: Immediately after injury, blood vessels constrict to minimize bleeding, and platelets aggregate to form a clot.
Inflammation: White blood cells migrate to the wound site to prevent infection and clear debris. This phase typically lasts for a few days.
2.Proliferation:
Cell Growth: New tissue forms as fibroblasts produce collagen, and epithelial cells cover the wound.
Angiogenesis: New blood vessels develop to supply nutrients and oxygen to the healing tissue.
3.Remodeling:
Maturation: Collagen fibers are reorganized, and the wound strengthens. This phase can last for months to years and results in tissue remodeling and scar formation.
Effective wound healing is influenced by factors like wound type, infection control, and overall health
🔸2) Shock
Shock is a critical condition characterized by inadequate blood flow to tissues and organs, leading to cellular and systemic dysfunction. It can be classified into several types, each with distinct causes and treatments:
- Definition:
Shock occurs when the body’s circulatory system fails to supply enough blood and oxygen to meet the metabolic needs of tissues, leading to cellular damage and organ failure. - Types of Shock:
Hypovolemic Shock: Caused by significant loss of blood or fluids, often from trauma, bleeding, or severe dehydration. - Cardiogenic Shock: Results from the heart’s inability to pump blood effectively, commonly due to heart attacks or severe heart failure.
- Distributive Shock: Includes septic shock, where severe infection causes widespread blood vessel dilation, and anaphylactic shock, caused by a severe allergic reaction.
- Obstructive Shock: Caused by physical obstruction of blood flow, such as from a pulmonary embolism or cardiac tamponade.
- Symptoms:
Common symptoms include low blood pressure, rapid heartbeat, weak pulse, confusion, and pale or cold skin. - Treatment:
Treatment depends on the shock type but generally involves fluid resuscitation, medications, and addressing the underlying cause of the shock.
🔸3) Infarction
Infarction refers to tissue death due to a lack of blood supply, often resulting from the obstruction of a blood vessel.
Definition: Infarction occurs when blood flow to a part of the body is reduced or stopped, leading to the death of tissue due to insufficient oxygen and nutrients.
Causes: It is commonly caused by thrombosis (blood clot), embolism (blockage by an object like fat or air), or vasospasm (narrowing of blood vessels).
Examples: Examples include myocardial infarction (heart attack) and cerebral infarction (stroke).
Consequences: The affected tissue undergoes necrosis, leading to potential loss of function in the affected organ.
🔸4) Edema
Edema is the abnormal accumulation of fluid in the interstitial spaces of tissues or cavities in the body.
Definition: Edema is characterized by swelling caused by excess fluid leakage from blood vessels into the surrounding tissues or cavities.
Causes:
1.Increased Hydrostatic Pressure: Often due to conditions like congestive heart failure or venous insufficiency, where elevated blood pressure in capillaries pushes fluid out into tissues.
2.Decreased Oncotic Pressure: Resulting from low levels of albumin in the blood, which may occur in nephrotic syndrome or liver disease.
3.Increased Capillary Permeability: Caused by inflammation or allergic reactions, allowing fluid to leak into tissues, as seen in allergic reactions or infectious diseases.
4.Lymphatic Obstruction: Blockage of lymph vessels can prevent fluid drainage, leading to edema, as seen in lymphedema.
Symptoms: Symptoms include visible swelling, pitting (leaving an indentation when pressed), and discomfort in the affected area.
Treatment: Management involves addressing the underlying cause, using diuretics to reduce fluid overload, and other supportive measures like elevation of the affected limbs.
🔸5) Mutation
Mutation refers to a permanent change in the DNA sequence of an organism’s genome.
Definition: A mutation is a genetic alteration that can affect gene function and lead to changes in an organism’s traits or health.
Types:
1.Point Mutation: A change in a single nucleotide base, which can be a substitution, insertion, or deletion. For example, sickle cell disease results from a point mutation in the hemoglobin gene.
2.Chromosomal Mutation:
Larger-scale changes such as deletions, duplications, or rearrangements of chromosome segments. Examples include Down syndrome, caused by an extra chromosome 21.
Effects:
Mutations can be neutral, beneficial, or harmful. For instance, some mutations lead to genetic disorders, while others may confer advantages such as antibiotic resistance in bacteria.
Causes: Mutations can be spontaneous or induced by external factors like radiation or chemicals M,
🔸6) Inheritance
Inheritance refers to the process by which genetic traits and characteristics are passed from parents to offspring through genes.
Definition:
Inheritance is the transmission of genetic information from one generation to the next, determining traits such as eye color, blood type, and susceptibility to certain diseases.
Types of Inheritance:
1.Mendelian Inheritance:
Dominant and Recessive Traits: Traits are determined by alleles, where dominant alleles mask the effects of recessive ones. For example, the gene for flower color in peas has dominant (P) and recessive (p) alleles.
2.Codominance and Incomplete Dominance:
Codominance: Both alleles express their traits simultaneously, as seen in AB blood type where both A and B an…
Q-7. Write short Answer (Any Three)
🔸1) Pathophysiology of pulmonary tuberculosis
Pathophysiology of pulmonary tuberculosis
Pulmonary tuberculosis (TB) is a chronic infectious disease caused by the bacterium Mycobacterium tuberculosis. The pathophysiology of pulmonary TB involves several stages, from initial infection to the manifestation of disease.
- Entry and Initial Infection
Transmission: TB is spread through airborne droplets from an infected individual.
Infection: Mycobacterium tuberculosis enters the respiratory tract and reaches the alveoli in the lungs.
- Immune Response and Formation of Granulomas
Phagocytosis: Macrophages in the alveoli engulf the bacteria. However, M. tuberculosis can evade destruction by residing within these macrophages.
Granuloma Formation: The immune system responds by forming a tubercle or granuloma, which is a cluster of macrophages, lymphocytes, and other immune cells aimed at containing the infection. This structure contains the bacteria and prevents further spread.
Primary Complex: The initial granuloma and regional lymph node involvement constitute the Ghon complex.
- Latent vs. Active TB
Latent TB: In many individuals, the immune response contains the bacteria, leading to a latent TB infection where the person is asymptomatic and non-contagious. However, the bacteria remain dormant.
Active TB: In some cases, especially if the immune system becomes compromised, the bacteria reactivate, leading to active disease characterized by symptoms such as chronic cough, hemoptysis, chest pain, and weight loss.
- Disease Progression
Pulmonary Inflammation: In active TB, the granulomas break down, leading to caseous necrosis (cheese-like appearance of dead tissue). The bacteria proliferate and cause further lung damage.
Cavitation: The formation of cavities in the lung tissue occurs due to the destruction of lung architecture by the bacteria. These cavities can facilitate further transmission of the bacteria through coughing.
- Clinical Manifestations
Symptoms: Persistent cough, chest pain, hemoptysis (coughing up blood), fever, night sweats, and weight loss.
Radiographic Findings: X-rays may reveal cavitary lesions, infiltrates, or nodular opacities consistent with TB.
- Diagnosis and Treatment
Diagnosis: Involves
tuberculin skin tests (Mantoux test), interferon-gamma release assays, sputum smear microscopy, and chest X-rays.
Treatment: Requires a combination of antibiotics such as isoniazid, rifampin, ethambutol, and pyrazinamide over a six-month period to eradicate the bacteria and prevent resistance
🔸2) CSF analysis
Cerebrospinal Fluid (CSF) Analysis is a diagnostic procedure used to assess the composition and properties of the CSF, which surrounds and protects the brain and spinal cord. The analysis helps diagnose a variety of neurological conditions.
1.Collection of CSF:
Procedure: CSF is collected through a lumbar puncture (spinal tap) performed in the lower back, typically between the L3-L4 or L4-L5 vertebrae.
Indications: Conditions like meningitis, multiple sclerosis, and subarachnoid hemorrhage.
- Components Analyzed:
Appearance:
Normal: Clear and colorless.
Abnormal: Turbid or cloudy in infections, yellow (xanthochromia) in hemorrhage, or pink/red in blood contamination.
Pressure:
Normal: 70-180 mm H₂O.
Elevated: May indicate increased intracranial pressure from conditions like meningitis or tumors.
Cell Count: Normal: 0-5 cells/µL (mainly lymphocytes).
Elevated: In infections (pleocytosis), inflammation, or malignancies.
Protein Levels:
Normal: 15-45 mg/dL.
Elevated: In infections, inflammation, or multiple sclerosis.
Glucose Levels:
Normal: 45-75 mg/dL.
Decreased: In bacterial meningitis, tuberculosis, or fungal infections.
Lactate Levels:
Normal : 1.1-2.6 mmol/L.
Elevated: Indicates anaerobic metabolism, seen in bacterial meningitis or brain abscesses.
Gram Stain and Culture:
Purpose: Detects bacterial pathogens.
Normal: No growth.
Abnormal: Positive in bacterial infections. - Clinical Significance:
Meningitis: CSF analysis helps identify the causative pathogen and differentiate between bacterial, viral, and fungal meningitis.
Subarachnoid Hemorrhage: CSF analysis can reveal the presence of blood or xanthochromia.
Multiple Sclerosis: Elevated protein levels and oligoclonal bands in CSF can indicate this condition.
Encephalitis: Analysis helps in identifying the cause and managing the treatment
🔸3) X linked pattern of inheritance
X-linked inheritance refers to the genetic transmission of traits or disorders linked to genes on the X chromosome. This pattern affects males and females differently due to their sex chromosomes, with females having two X chromosomes (XX) and males having one X and one Y chromosome (XY).
In X-linked recessive inheritance, the trait manifests in females only if both X chromosomes carry the recessive allele. In males, a single X chromosome with the recessive allele will express the trait. Affected males transmit the trait to all their daughters (making them carriers) but not to their sons. Females can be carriers of X-linked recessive traits if they have one affected X chromosome but do not show symptoms. Examples of X-linked recessive disorders include hemophilia A and Duchenne muscular dystrophy.
In X-linked dominant inheritance, one copy of the dominant allele on the X chromosome is sufficient for the trait to be expressed in both males and females. Affected males pass the trait to all their daughters but none of their sons. Affected females can pass the trait to both sons and daughters. Examples of X-linked dominant disorders include Rett syndrome and X-linked vitamin D-resistant rickets.
In pedigree analysis for X-linked recessive traits, there is a higher incidence of affected males, and the trait can skip generations. In X-linked dominant traits, both males and females can be affected, and the trait does not skip generations.
References
- Robbins Basic Pathology by Kumar, Abbas, and Aster
- Principles of Genetics by D. Peter Snustad and Michael J. Simmons
- Molecular Biology of the Gene by James D. Watson et al.
🔸4) Role of nurse in genetics
The role of the nurse in genetics encompasses a variety of responsibilities aimed at supporting patients and families through genetic assessment, counseling, and care.
Assessment and Identification of Genetic Risk
Nurses help identify patients who may be at risk for genetic conditions through the collection of family histories, assessing risk factors, and recognizing symptoms that may suggest a genetic disorder. They collaborate with genetic counselors and specialists to gather comprehensive family and medical histories to identify patterns of inheritance and potential genetic risks.
Genetic Counseling and Education
Nurses provide education to patients and families about genetic conditions, including explaining test results, discussing implications, and helping individuals understand their genetic risks. They support patients in making informed decisions about genetic testing and preventive measures.
Coordination of Care
Nurses coordinate care for patients undergoing genetic testing or treatment for genetic disorders. This includes scheduling appointments, managing follow-up care, and working with multidisciplinary teams to ensure comprehensive patient care. They also assist in organizing resources and referrals to genetic counselors, specialists, and support groups.
Support and Advocacy
Nurses offer emotional support to patients and families dealing with genetic conditions. They act as advocates, helping patients navigate the healthcare system, access necessary services, and advocate for their needs in various healthcare settings.
Research and Professional Development
Nurses engage in ongoing education and research to stay current with advancements in genetic medicine. They participate in research studies, attend professional development courses, and contribute to the development of new genetic testing methods and treatments.
Documentation and Record Keeping
Nurses maintain accurate and detailed records of genetic assessments, test results, and patient interactions. Proper documentation ensures continuity of care and supports clinical decision-making processes
Q-8. 🔸(A) Explain pathogenesis and route of transmission of AIDS
Pathogenesis of AIDS
Route of Transmission of AIDS
Pathogenesis of AIDS
AIDS (Acquired Immunodeficiency Syndrome) is caused by the human immunodeficiency virus (HIV). The pathogenesis of AIDS involves several stages, leading from initial infection to severe immune system damage.
HIV primarily infects CD4+ T lymphocytes, which are crucial for immune response. The virus binds to the CD4 receptor and co-receptors (CCR5 or CXCR4) on the surface of these cells. After entry, HIV undergoes reverse transcription to convert its RNA genome into DNA, which integrates into the host cell’s genome. This integration leads to the production of new viral particles, which eventually destroy the host CD4+ cells.
The chronic infection causes a gradual decline in CD4+ T cell counts, leading to immune system dysfunction. As the immune system weakens, the body becomes susceptible to opportunistic infections and certain cancers. The progression of HIV infection to AIDS is marked by a significant drop in CD4+ T cell counts and the occurrence of specific opportunistic infections or cancers.
Route of Transmission of AIDS
HIV is transmitted through several primary routes:
1.Sexual Contact: The most common route, involving the exchange of bodily fluids such as semen, vaginal secretions, or blood during unprotected sexual intercourse.
2.Blood Transfusion: Receiving blood products or organ transplants from an HIV-infected donor.
3.Needle Sharing: Sharing needles or syringes among drug users, which can introduce HIV from contaminated blood.
4.Mother-to-Child Transmission: HIV can be transmitted from an infected mother to her child during pregnancy, childbirth, or breastfeeding.
5.Occupational Exposure: Health care workers may be at risk through needle-stick injuries or exposure to HIV-contaminated blood.
HIV is not spread through casual contact, such as hugging or sharing utensils. Preventive measures include safe sex practices, needle exchange programs, and antiretroviral therapy for HIV-positive pregnant women to reduce mother-to-child transmission.
🔸(B) Write about Human genome project
Human Genome Project
The Human Genome Project was an international research initiative aimed at mapping and understanding all the genes of the human species. It was launched in 1990 and completed in 2003.
The primary goal of the Human Genome Project was to sequence the entire human genome, which consists of about 3 billion DNA base pairs. The project aimed to identify and map all the genes present in human DNA, which make up the complete genetic blueprint for human development and function. This monumental task involved determining the sequence of the 23 pairs of human chromosomes.
The project achieved several significant milestones. It successfully identified approximately 20,000-25,000 human genes and mapped the genetic variations among individuals. One of the key outcomes was the generation of a comprehensive reference genome that serves as a standard for comparing genetic sequences and studying genetic variations.
The Human Genome Project has had profound implications for various fields of biology and medicine. It has enabled the identification of genetic mutations associated with diseases, leading to advancements in diagnostic techniques and the development of targeted therapies. The knowledge gained has facilitated the growth of personalized medicine, where treatments are tailored to an individual’s genetic makeup.
Additionally, the Human Genome Project has fostered advancements in bioinformatics and genomics, establishing databases and computational tools that support ongoing genetic research and applications.
FOR MORE DETAILS KINDLY CONTACT US ON (CALL/WHATSAPP)-8485976407
