12/07/2022-B.SC-NURSING REAERCH-PAPER DONE-upload no.1
12/07/2022-B.SC-NURSING REAERCH-PAPER
kindly send your University paper’s Image watsapp us on 8485976407. we upload its solution immediately
Section 1 (50 marks)
Q.1 a) Define quantitative Research. (2+8=10)
Quantitative research is a systematic investigation that primarily focuses on collecting and analyzing numerical data to identify patterns, test hypotheses, and make predictions. It is used to quantify variables, measure relationships between them, and present findings using statistical methods.
b) Explain the steps of quantitative research study
✅ 1. Identifying and Defining the Research Problem
- The first step involves selecting a nursing or clinical problem that requires investigation, such as low immunization rates or poor patient compliance.
- The researcher must ensure that the problem is clearly stated, focused, and researchable using quantitative methods.
- The problem should highlight a knowledge gap or an unmet need in nursing practice or policy.
- Itbis important to define the research problem in operational terms to guide the direction of the study.
- A well-defined problem leads to specific research objectives and hypotheses.
✅ 2. Review of Literature
- This step includes collecting information from books, scholarly articles, journals, and electronic databases like PubMed, CINAHL, and Scopus.
- The literature review helps in understanding current knowledge, identifying gaps, and refining the problem statement.
- It assists in identifying theoretical frameworks or models suitable for developing the conceptual framework.
- Literature review prevents duplication of efforts and ensures the research is built on a solid foundation.
- It also aids in the selection of valid and reliable research tools.
✅ 3. Formulating Objectives and Hypotheses
- Based on the problem and literature review, the researcher formulates clear, measurable, and achievable objectives.
- Objectives help in focusing the study by stating what the researcher intends to find out.
- Hypotheses are framed as testable statements that predict a relationship between variables (e.g., “There is a significant difference in knowledge scores before and after intervention”).
- Both directional and non-directional hypotheses may be developed depending on the research question.
- Well-written objectives and hypotheses form the foundation of study design and analysis.
✅ 4. Selecting an Appropriate Research Design
- Research design is the blueprint of the study and determines how the study will be conducted.
- Common quantitative designs include descriptive, experimental, quasi-experimental, and correlational designs.
- The design must align with the research objectives, population, and hypothesis.
- It guides the selection of sampling technique, data collection methods, and statistical tools.
- A good research design ensures validity, reliability, and generalizability of the results.
✅ 5. Defining Population and Selecting Sampling Technique
- The population refers to the entire group of individuals who meet the study criteria (e.g., diabetic patients, nursing students).
- The sample is a representative subset selected from the population for data collection.
- Sampling methods include probability sampling (e.g., simple random, stratified) and non-probability sampling (e.g., convenience, purposive).
- The sample size must be large enough to allow for statistical validity and error control.
- Clear inclusion and exclusion criteria must be defined to ensure uniformity in sample selection.
✅ 6. Developing and Validating the Research Tool
- A tool or instrument (e.g., questionnaire, checklist, rating scale) is developed based on research variables and objectives.
- The tool must have clear, concise, and unbiased items to ensure accurate data collection.
- Validity (face, content, construct) ensures the tool measures what it’s supposed to measure.
- Reliability (test-retest, internal consistency) ensures the tool produces consistent results.
- A pilot test is conducted on a small group to refine tool content and language.
✅ 7. Data Collection Procedure
- After ethical clearance and participant consent, data is collected systematically using the approved tool.
- The same procedure is followed for all participants to maintain uniformity and reliability.
- Tools may be administered through interviews, self-reports, or observation.
- Confidentiality, accuracy, and neutrality must be maintained during data collection.
- All collected data should be recorded promptly and securely.
✅ 8. Data Analysis and Interpretation
- Data is first organized through tabulation, coding, and cleaning to remove errors.
- Descriptive statistics (mean, percentage, standard deviation) are used to summarize the data.
- Inferential statistics (t-test, chi-square, ANOVA) are used to test hypotheses and determine significance.
- Statistical software like SPSS, R, or Excel is often used.
- The data interpretation must be linked back to the objectives and hypothesis.
✅ 9. Presentation of Findings
- The analyzed results are presented in the form of tables, charts, graphs, and narratives.
- Each finding should be explained in clear terms related to the objectives.
- Unexpected findings or limitations should also be reported transparently.
- Results should be compared with findings from previous studies.
- The implications for nursing care or practice must be discussed.
✅ 10. Conclusion and Recommendations
- The conclusion should summarize the main findings and answer the research question or hypothesis.
- It should also explain the practical implications for nursing practice, education, or policy-making.
- Based on findings, recommendations are made for future research or intervention.
- Limitations of the study should be acknowledged.
- The study should end with a scientific justification of its value.
✅ 11. Dissemination of Research Findings
- This step involves sharing research outcomes with academic, clinical, and policy-making communities.
- Results can be disseminated through research reports, nursing journals, seminars, or conferences.
- Sharing knowledge contributes to evidence-based practice and improved patient care.
- The researcher must maintain ethical standards and accuracy while presenting findings.
- It also supports nursing professional development and policy reforms.
Q.2 a) Define problem statement. (2+4+4=10)
A problem statement is a clear, concise, and focused description of the issue or concern that needs to be addressed through research or investigation. It identifies the existing gap in knowledge or practice, outlines the context and significance of the problem, and provides the basis for setting research objectives and questions.
b) Describe the sources of research problem
✅ 1. Clinical Practice / Nursing Experience
- Nurses work closely with patients and are frequently exposed to recurring challenges in care delivery, such as delayed wound healing or medication errors.
- These clinical observations help nurses identify gaps between theory and practice, which can be converted into research questions.
- Repeated documentation of adverse events or variations in patient outcomes can highlight problems needing further exploration.
- Day-to-day care issues—such as improper positioning, lack of compliance, or staff shortage—often generate practical research topics.
- Clinical audits, patient feedback, and incident reporting systems can also indicate areas where nursing interventions need scientific evaluation.
- Example : A nurse observing poor pain control in post-operative patients may research the effectiveness of non-pharmacological methods like guided imagery.
✅ 2. Review of Literature
- Reviewing existing research articles, journals, reports, and theses helps identify what is already known and where the gaps exist.
- Literature can reveal inconsistencies in findings, such as one study supporting and another denying the effectiveness of a nursing intervention.
- It also identifies under-researched populations or settings, such as elderly care in rural areas.
- The review often highlights limitations of previous studies, which can be addressed in future research.
- Reading systematic reviews and meta-analyses can also point to areas needing more robust evidence.
- Example : If few studies exist on nurse-led asthma education for teenagers, that becomes a potential research problem.
✅ 3. Theories and Nursing Models
- Established nursing theories like Orem’s, Roy’s, or Neuman’s model offer structured concepts that researchers can test or modify in specific contexts.
- Unexplored or untested relationships between theoretical constructs can become rich sources of research problems.
- Theories also help in identifying predictors, mediators, and outcomes that need empirical validation.
- When theory is applied in practice, it may not always yield the expected result—this gap leads to a researchable problem.
- Theoretical frameworks can suggest hypothetical relationships (e.g., self-care and quality of life) that can be tested through research.
- Example : Using Roy’s adaptation model, a nurse may study the coping patterns of stroke patients in home care.
✅ 4. Personal Interest or Experience
- A nurse may develop a strong interest in a topic based on personal clinical experiences, emotional connections, or community background.
- Topics derived from personal interest often lead to higher motivation, deeper insight, and stronger commitment in conducting research.
- Nurses working in specialized areas like ICU, pediatrics, or psychiatry often notice problems not visible in general care.
- Personal experiences such as witnessing a misdiagnosis or suffering due to lack of resources can trigger a research question.
- Self-interest ensures that the topic is meaningful and relevant to the researcher, improving the quality and depth of the study.
- Example : A nurse who has cared for cancer patients may develop interest in researching the effectiveness of music therapy in reducing chemotherapy-induced nausea.
✅ 5. Social and Public Health Issues
- Community health nurses often encounter prevailing social issues like malnutrition, substance abuse, or reproductive health problems.
- These larger public health challenges become research problems when they affect nursing care delivery or require community intervention.
- Social taboos, lack of awareness, or limited access to healthcare can be researched for their impact on health-seeking behavior.
- Government health missions or WHO reports also indicate priority areas that need evidence-based solutions.
- Topics like school absenteeism due to menstruation or maternal anemia are socially significant and highly relevant in nursing research.
- Example : Studying the impact of health education on menstrual hygiene practices among adolescent girls in slum areas.
✅ 6. Policy and Administrative Problems
- Nurses involved in leadership roles or hospital administration often face issues in staffing, scheduling, workload distribution, or patient safety.
- These operational concerns can be scientifically studied to recommend policy improvements and workflow redesign.
- High nurse-to-patient ratios or job dissatisfaction can be explored through surveys and statistical analysis.
- Nursing audits and quality assurance programs may reveal inefficiencies or adverse trends requiring intervention.
- Research on these issues supports better hospital policies and staffing models, improving nurse satisfaction and patient outcomes.
- Example : A study on the impact of night shift rotations on nurse burnout levels in critical care units.
✅ 7. Emerging Trends and Technological Advances
- New technologies in healthcare—like tele-nursing, electronic health records, or wearable devices—bring new unexplored research questions.
- Their integration in clinical practice often creates confusion, resistance, or adaptation challenges, which become areas of study.
- Nursing research can evaluate the effectiveness, usability, and outcomes of these technological tools.
- Technological shifts also raise questions about privacy, training, and digital literacy, especially among older nurses.
- Trends like climate change, pandemics, or digital mental health platforms open avenues for contemporary research topics.
- Example : Studying nurse satisfaction and patient safety before and after the introduction of electronic medical records.
c) Explain criteria for selecting a good research problem
A good research problem is the backbone of any research study. It must be carefully selected to ensure the study is meaningful, practical, ethical, and beneficial to the nursing or health field. The following are the detailed criteria for selecting a high-quality research problem :
1. Researchability and Feasibility
- The research problem must be capable of being investigated using scientific methods, such as observation, measurement, and analysis.
- It should be feasible to study with the available resources, including time, money, equipment, and personnel.
- The problem should match the researcher’s skill level and training, especially in nursing where clinical expertise is required.
- Example : Studying infection rates in post-operative patients using data from hospital records is feasible.
2. Significance and Relevance to Nursing Field
- The selected problem should be important and relevant to nursing practice, education, administration, or health policy.
- It should have the potential to improve patient outcomes, nursing care standards, or community health practices.
- Example : Exploring reasons for poor hand hygiene compliance among nurses can directly impact patient safety.
3. Novelty and Research Gap
- A good research problem should focus on a new issue or an area where current knowledge is insufficient.
- It should not simply duplicate past studies unless it addresses the problem in a new context or with improved methodology.
- The identification of a gap in the literature is essential to ensure the research is meaningful and contributes to existing knowledge.
- Example : Investigating the mental health of nursing students during online learning post-COVID is a current and original topic.
4. Ethical Acceptability
- The problem should be ethically sound and should not harm participants physically, emotionally, or socially.
- It must ensure informed consent, confidentiality, and voluntary participation.
- Research involving vulnerable groups like children, pregnant women, or elderly patients must be carefully planned with extra ethical safeguards.
- Example : A study on patient experiences of pain management should not expose them to additional pain or discomfort.
5. Clarity and Precision in Statement
- The problem must be clearly defined, specific, and understandable.
- Vague or overly broad topics can lead to confusion in the research process.
- A well-written problem statement helps in forming precise objectives, hypotheses, and choosing appropriate tools.
- Example : “The impact of daily exercise on blood sugar levels in elderly diabetic patients” is more specific than “Exercise and health.”
6. Availability of Supporting Literature and Data
- There should be sufficient existing literature to support the background of the study and justify the need for research.
- Also, reliable data sources (hospital records, health surveys, patient interviews) must be available for analysis.
- It is essential to confirm that data collection will be practical and ethical.
- Example : Researching maternal mortality trends in a specific district requires access to government health reports and hospital data.
Nursing Management / Application in Nursing
- Nurse researchers and practitioners should choose problems that focus on practical issues in patient care, hospital management, and nursing education.
- Selection of relevant problems helps in developing evidence-based protocols, enhancing staff training, and improving healthcare delivery.
- Nursing administrators can use research to improve workflow, reduce errors, and increase patient satisfaction.
- Example : A study on workload and burnout among ICU nurses can lead to improved staffing policies.
Q.3 a) Explain the steps of tool construction (4+4+2=10)
Tool construction is the systematic process of designing, developing, validating, and finalizing an instrument that collects data in a research study . It includes following steps :
✅ 1. Identifying the Purpose of the Tool
- The first step is to clearly define what the tool will measure, such as knowledge, attitude, skills, behaviors, or clinical symptoms.
- The purpose must align directly with the research objectives and variables.
- It should be decided whether the tool is for descriptive data (e.g., knowledge) or measurable outcomes (e.g., blood pressure).
- Knowing the tool’s purpose helps determine the type of items, scale format, and data analysis methods.
- Example : If the purpose is to assess stress levels, then a psychological rating scale (like Likert scale) may be suitable.
- In nursing, tools may assess pain intensity, anxiety, wound status, or medication adherence.
✅ 2. Deciding the Type of Tool and Method of Data Collection
- The researcher chooses the format of the tool: questionnaire, structured interview, observation checklist, or physiological test.
- This choice depends on the type of variable, population characteristics (age, literacy), and research design.
- Quantitative studies often use close-ended tools, while qualitative studies may use open-ended tools.
- The mode of administration (self-report vs. interviewer-administered) must also be selected.
- In nursing, tools may use scales like Likert, semantic differential, visual analog, or numeric rating.
- The chosen method should minimize bias and promote accurate responses.
✅ 3. Writing the Items or Questions
- Questions or statements are developed based on the variables and research objectives identified in the conceptual framework.
- Each item must be clear, precise, unambiguous, and free from bias or double meanings.
- The language should match the educational and cultural background of the target population.
- Items should be sequenced logically – starting from simple to complex, or general to specific.
- The number of questions must be sufficient to measure the variable comprehensively, but not so long that it causes fatigue.
- Example : In a tool measuring health awareness, include items covering definition, causes, prevention, and management.
✅ 4. Establishing Validity of the Tool
- Validity refers to how well the tool measures what it is intended to measure.
- Types include :
- Face validity: Does the tool appear suitable at face value?
- Content validity: Are the items adequate and representative of the content area?
- Construct validity: Does the tool measure the theoretical construct?
- Content validity is established by seeking opinions from subject matter experts (e.g., doctors, senior nurses, researchers).
- A content validity index (CVI) may be calculated to assess the degree of agreement among experts.
- Ensuring validity enhances the scientific credibility and clinical applicability of the tool.
- Example : A diabetes knowledge tool must include all essential areas like diet, exercise, insulin use, and complications.
✅ 5. Testing Reliability of the Tool
- Reliability refers to the consistency or dependability of the tool in producing stable results over time or across users.
- Types of reliability include :
- Test-retest reliability : Same test given at two time points.
- Inter-rater reliability : Two observers use the same tool.
- Internal consistency : How well items within the tool relate (e.g., Cronbach’s alpha).
- A pilot study is usually conducted to test reliability.
- Items that reduce reliability may be modified or deleted based on pilot results.
- Reliability scores are important to ensure that data collected is dependable for decision-making.
- In nursing, tools like pain scales must give reproducible scores regardless of who uses them.
✅ 6. Pre-Testing or Pilot Study
- A pilot test is conducted on a small representative sample (5–10% of study sample) to identify problems with wording, instructions, or sequencing.
- Pretesting helps to assess the feasibility, clarity, time required, and respondent comfort.
- Any confusing, leading, or ambiguous items are revised or eliminated.
- Feedback is obtained from both participants and experts.
- This step ensures the final tool is error-free and user-friendly.
- Pilot study also tests the scoring system and layout for final improvements.
✅ 7. Finalizing the Tool
- Based on expert feedback and pilot results, the final version of the tool is prepared.
- It includes clear instructions, a logical layout, appropriate font size, and response format.
- A cover page, consent statement, and confidentiality note are added for ethical compliance.
- The tool should be tested one last time for readability and flow.
- The finalized tool is then used in the main study and documented in the methodology section.
- Example : A checklist for neonatal care is finalized with 20 steps based on WHO guidelines and staff feedback.
b) Describe questionnaire as a tool for data collection
Definition
- A questionnaire is defined as a pre-formulated written or printed set of questions, which is used by researchers to obtain information from respondents in a consistent and standardized way regarding their opinions, behaviors, facts, or attitudes.
- It is one of the most commonly used tools for primary data collection in nursing and health-related research, as it can be used in both quantitative and qualitative studies.
- It is often self-administered, or sometimes conducted by a trained interviewer, and it may include closed-ended (structured) or open-ended (unstructured) questions.
Purpose of a Questionnaire
- To collect relevant data directly from the study participants in a structured and organized manner.
- To obtain standardized, comparable information from multiple respondents simultaneously.
- To explore individual views, knowledge, beliefs, experiences, and practices related to the research topic.
- To support the measurement of variables in the form of knowledge scores, attitude levels, or behavior patterns.
- To allow researchers to perform statistical analysis and draw meaningful conclusions based on the data gathered.
Types of Questionnaire
1️⃣ Structured Questionnaire (Closed-ended)
- This type of questionnaire contains pre-determined, fixed questions and answers that do not allow elaboration.
- It is used mainly in quantitative research for easy coding and statistical analysis.
- Example : “Have you received tetanus vaccination in the past 6 months? (Yes/No)”
2️⃣ Unstructured Questionnaire (Open-ended)
- This type of questionnaire includes broad, exploratory questions, allowing the respondent to express thoughts in their own words.
- It is used in qualitative research for exploring deep experiences, feelings, and perceptions.
- Example : “What challenges did you face during your hospital stay?”
3️⃣ Semi-Structured Questionnaire
- It combines both open-ended and closed-ended questions, allowing researchers to gather quantitative data with descriptive elaboration.
- It is useful in mixed-method research designs.
Types of Questions Used in Questionnaires
Open-ended questions – allow free expression of opinions
Example : “What are your concerns about hospital cleanliness?”
Closed-ended questions – have fixed response options
Example : “Do you feel safe in your ward? (Yes/No)”
Multiple Choice Questions (MCQs) – more than two options
Example : “How do you commute to hospital? (a) Bus (b) Bike (c) Walk (d) Other”
Likert Scale – measures strength of attitude/opinion
Example: “Rate the quality of care: Very Poor – Poor – Neutral – Good – Very Good”
Dichotomous Questions – two choices only (Yes/No, True/False)
Steps in Designing a Questionnaire
- Define the research problem and objectives clearly.
- Identify the type of information needed to address the objectives.
- Select appropriate question types (open/closed, rating, etc.).
- Draft the questions using simple, neutral, and clear language.
- Arrange the questions in a logical sequence, starting with general questions and ending with sensitive or specific ones.
- Conduct a pilot test (pre-test) with a small group to check for clarity and usability.
- Make necessary revisions based on feedback, and finalize the tool for data collection.
- Include an introductory note or instructions for the respondent along with a consent statement.
Characteristics of a Good Questionnaire
- All questions must be relevant to the research problem.
- Questions should be clear, short, and free from ambiguity.
- Avoid leading, double-barreled, or biased questions.
- Should be logically arranged for smooth flow.
- Language used must be simple, culturally appropriate, and understandable by the target population.
- Should ensure anonymity and confidentiality of respondents.
- Must be pre-tested (pilot tested) before actual use in the field.
- Should be easy to analyze and interpret once data is collected.
Advantages of Questionnaire as a Data Collection Tool
- It is a cost-effective and time-saving method to collect data from a large population.
- It can be administered without the presence of the researcher, especially in mailed or online surveys.
- It enables standardization, ensuring that each respondent gets the same questions.
- It is useful for collecting quantitative data that is easy to tabulate and analyze statistically.
- It reduces interviewer bias, especially when it is self-administered.
Disadvantages or Limitations
- May have a low response rate, especially in postal or online forms.
- Cannot be used effectively with illiterate or non-cooperative participants.
- Respondents may misunderstand questions or provide inaccurate information.
- It does not allow probing or clarification, unlike interviews.
- Some questions may be skipped or left unanswered, leading to incomplete data.
Use of Questionnaire in Nursing Research
- Used to assess patient knowledge, attitudes, or behaviors (e.g., in health education studies).
- Widely used in KAP studies (Knowledge, Attitude, Practice).
- Helps to evaluate satisfaction of patients, caregivers, or nursing students.
- Used to measure pre-test and post-test knowledge levels in intervention studies.
- Important in community health surveys, disease surveillance, and epidemiological research
c) Discuss advantage & disadvantages
Advantages of Questionnaire as a Data Collection Tool
- It is a cost-effective and time-saving method to collect data from a large population.
- It can be administered without the presence of the researcher, especially in mailed or online surveys.
- It enables standardization, ensuring that each respondent gets the same questions.
- It is useful for collecting quantitative data that is easy to tabulate and analyze statistically.
- It reduces interviewer bias, especially when it is self-administered.
Disadvantages or Limitations
- May have a low response rate, especially in postal or online forms.
- Cannot be used effectively with illiterate or non-cooperative participants.
- Respondents may misunderstand questions or provide inaccurate information.
- It does not allow probing or clarification, unlike interviews.
- Some questions may be skipped or left unanswered, leading to incomplete data.
Q.4 Write short notes for the following any four (4×5=20)
1.Review of Literature.
Definition
- A Review of Literature is a critical summary and analysis of existing research studies, scholarly articles, books, journals, and other documents that are related to the research problem.
- It is conducted to gain in-depth knowledge about the topic, identify research gaps, and provide context and justification for the new study.
- It helps in developing theoretical and conceptual frameworks and refining research tools.
Purpose of Review of Literature
- It helps the researcher to gain comprehensive knowledge about the selected research problem.
- It identifies gaps or inconsistencies in previous studies, justifying the need for new research.
- It prevents duplication of earlier work and provides direction for further study.
- It helps to formulate research questions, hypotheses, and objectives clearly.
- It supports in selecting the appropriate research design, methodology, and tools.
- It provides a basis for comparison of the current findings with previous studies.
- It guides in interpreting results and placing them in the context of what is already known.
Main Types of Review of Literature
1️⃣ Narrative Review (Traditional Review)
- It is a qualitative summary of previously published research on a particular topic.
- It does not follow a strict protocol and is often written in essay format.
- It is used to give background information, highlight trends, and identify gaps.
- It may be subjective and prone to researcher bias.
- Example : Reviewing general studies on “Nurse burnout in hospital settings.”
2️⃣ Systematic Review
- It is a highly structured and scientific method of reviewing literature.
- It follows a clear and pre-defined protocol including inclusion and exclusion criteria.
- It uses objective and reproducible methods to identify, evaluate, and summarize findings.
- It aims to eliminate bias and provide reliable evidence.
- Example : A systematic review of randomized controlled trials on hand hygiene practices to prevent hospital-acquired infections.
3️⃣ Meta-Analysis
- It is a subset of a systematic review that uses statistical methods to combine the results of multiple studies.
- It is used to calculate a pooled estimate or effect size.
- It is applied when studies use similar methodologies and outcome measures.
- Example : Meta-analysis of various studies assessing the effectiveness of cognitive behavioral therapy in managing depression in adolescents.
4️⃣ Scoping Review
- It is used to map the existing literature on a broad topic.
- It helps identify key concepts, research gaps, and types of evidence.
- It does not assess the quality of the included studies.
- It is useful in exploratory phases of research.
- Example : Scoping review on available telehealth services for rural populations in India.
5️⃣ Integrative Review
- It includes both experimental and non-experimental studies.
- It allows for the integration of diverse types of data (qualitative and quantitative).
- It aims to summarize past empirical or theoretical literature to provide a comprehensive understanding.
- Example : Integrative review of both qualitative interviews and quantitative surveys on patient satisfaction in ICU.
6️⃣ Critical Review
- It involves a detailed analysis and evaluation of previous literature.
- It aims to challenge existing assumptions or conclusions.
- It includes a critical discussion of strengths and weaknesses of existing literature.
- Example : Critical review of ethical practices followed in clinical nursing research studies.
7️⃣ Theoretical Review
- It focuses on theories and theoretical concepts related to the topic.
- It analyzes the frameworks, models, and philosophical foundations.
- It is often used to refine or propose a new theory.
- Example : Theoretical review of Orem’s Self-Care Theory and its application in chronic illness care.
8️⃣ Rapid Review
- It is conducted in a short time frame using simplified methods of a systematic review.
- It provides quick evidence for decision-making, often used in policy or emergency settings.
- Example : Rapid review during a pandemic to assess the impact of PPE usage on nurse safety.
9️⃣ Umbrella Review (Review of Reviews)
- It reviews previously conducted systematic reviews and meta-analyses.
- It gives a broad and high-level summary of evidence on a topic.
- It is useful when multiple systematic reviews are available.
- Example : Umbrella review on mental health interventions for post-partum depression.
Sources of Review of Literature:
1. Primary Sources
- These are firsthand, original reports of facts or findings.
- They are created by researchers who conducted the study.
- Considered the most reliable and authentic for evidence-based practice.
- It provides detailed methodology, data, analysis, and conclusions
- It helps in understanding the research design and result interpretation
Examples :
- Theses and dissertations
- Conference proceedings (presenting original findings)
- Research reports by institutions
- Clinical trials
2. Secondary Sources
- These sources analyze, interpret, or summarize information from primary sources.
- They are not original research but rather a review or evaluation of existing studies.
- It is useful for building background knowledge.
- It Offers a broad overview of a topic
- It helps in identifies trends, gaps, and theoretical perspectives
Examples :
- Review articles
- Systematic reviews or meta-analysis
- Nursing textbooks
- Theoretical framework chapters
3. Tertiary Sources
- These are tools or reference materials that help in locating both primary and secondary sources.
- They do not contain original content but provide direction for finding it.
- Provides access to wide-ranging literature
- It helps in conducting effective literature search
Examples :
- Bibliographies
- Indexing and abstracting services
- Databases and directories
- Online search engines
Steps in Conducting a Review of Literature
- Identify the topic and research problem precisely.
- Search relevant literature using online databases, journals, libraries, etc.
- Select the relevant studies based on inclusion and exclusion criteria.
- Organize the studies thematically or chronologically.
- Critically evaluate each study in terms of method, findings, strengths, and weaknesses.
- Summarize key findings and identify research gaps.
- Write a comprehensive review using proper referencing style (APA/MLA/Vancouver).
Key Guidelines While Writing a Literature Review
- Begin with a broad overview and narrow down to specific studies.
- Maintain objectivity and critical thinking while evaluating literature.
- Avoid plagiarism by citing all sources properly.
- Use paraphrasing and summarizing instead of copying text directly.
- Ensure the review is up-to-date, relevant, and comprehensive.
Importance of Review of Literature In Nursing Research
- It provides in-depth background knowledge and understanding of the research topic.
- It helps to identify research gaps and justifies the need for new studies.
- It supports the formulation of research problems, objectives, and hypotheses.
- It assists in developing a theoretical or conceptual framework for the study.
- It guides the selection of appropriate research design, tools, and methodology.
- It helps in constructing or modifying data collection tools like questionnaires.
- It prevents duplication of previous research efforts and encourages originality.
- It aids in data interpretation and comparison with past findings.
- It promotes evidence-based practice in nursing care and clinical decision-making.
- It improves the validity, credibility, and academic quality of the research project.
2.Rating scale
Definition
- It is a structured measuring instrument that allows participants to express the degree of their response to a particular item or statement.
- It is used to convert qualitative judgments into quantitative values that can be analyzed statistically.
- It is especially applicable in nursing research for measuring variables like stress level, pain score, satisfaction, or compliance.
Characteristics of a Good Rating Scale
- It is clear, concise, and easy to understand for all participants, including patients and healthcare workers.
- It is logically arranged and ensures uniform interpretation.
- It is composed of relevant items that are directly aligned with research objectives.
- It is balanced in structure, including an equal range of positive and negative options.
- It is designed using culturally appropriate and non-offensive language.
Types of Rating Scales
It is classified into the following types :
A. Numerical Rating Scale (NRS)
- It is a numeric scale, usually ranging from 0 to 10, used to assess intensity of symptoms, especially pain.
- Example: “Rate your pain from 0 (no pain) to 10 (worst pain imaginable).”
B. Likert Scale
- It is a widely used psychometric scale that measures attitudes or levels of agreement.
- Example : “Strongly Agree – Agree – Neutral – Disagree – Strongly Disagree”
C. Semantic Differential Scale
- It is a bipolar rating scale used to rate concepts between opposite adjectives.
- Example : “Satisfied ⬜⬜⬜⬜⬜ Dissatisfied”
D. Graphic Rating Scale
- It is a visual analog scale where respondents mark a point along a line representing a continuum.
- Example : A horizontal line from “No anxiety” to “Severe anxiety”.
E. Descriptive Rating Scale
- It is a scale with verbal descriptors for each point.
- Example : 1 = Poor, 2 = Fair, 3 = Good, 4 = Very Good, 5 = Excellent.
Advantages of Rating Scales
- It is helpful in converting subjective data into objective form.
- It is time-efficient and easy to administer in clinical and research settings.
- It is suitable for large population studies as it can be used in online or printed format.
- It is ideal for descriptive and inferential analysis, especially using statistical tools.
- It is useful in monitoring changes in symptoms or attitudes over time.
Disadvantages / limitations
- It is subject to response bias, where participants may give socially acceptable answers.
- It is affected by central tendency bias, where many participants avoid extreme ratings.
- It is limited in capturing complex feelings, especially with only 3- or 5-point scales.
- It is language- and literacy-dependent, possibly reducing effectiveness in rural or low-education settings.
Steps in Developing a Rating Scale
- It is important to first identify the variable that needs to be measured (e.g., satisfaction, pain, stress).
- It is followed by deciding the appropriate type of scale (Likert, NRS, etc.).
- It is necessary to formulate clear, relevant, and unbiased items.
- It is advisable to keep a consistent format and equal spacing between options.
- It is crucial to conduct pilot testing to check validity and readability.
- It is finalized only after expert validation and reliability assessment.
Nursing Implications / Nursing Management Use
✅ 1. Assessment of Patient Symptoms and Conditions
- It is used by nurses to assess subjective symptoms like pain, fatigue, anxiety, depression, and stress using standard scales (e.g., Pain Scale, GAD-7, PHQ-9).
- It helps in early identification of worsening symptoms and timely nursing interventions.
- It improves patient monitoring and supports individualized care plans.
✅ 2. Evaluation of Patient Satisfaction and Experience
- It is applied in patient satisfaction surveys to measure the quality of nursing care, hospital environment, and communication.
- It helps hospital administrators and nurse managers understand the strengths and gaps in service delivery.
- It enhances patient-centered care, as feedback can guide service improvements.
✅ 3. Performance Appraisal of Nursing Staff
- It is used in staff evaluation tools to rate clinical competence, punctuality, communication skills, and adherence to protocols.
- It helps nursing supervisors make informed decisions about training needs, promotions, and recognition.
- It supports fair and consistent performance management.
✅ 4. Evaluation of Nursing Education Outcomes
- It is used by nurse educators to assess students’ performance during clinical postings, simulation labs, or skill-based evaluations.
- It helps in grading students objectively on criteria like communication, technique, and patient safety.
- It supports continuous academic assessment and improvement in teaching strategies.
✅ 5. Measurement of Attitudes and Behavioral Change
- It is used in health education programs to evaluate the effect of counseling or teaching by measuring pre- and post-intervention attitudes.
- It helps in assessing compliance to health promotion behaviors like smoking cessation, diet adherence, or medication use.
- It provides measurable evidence of behavioral change in the community or hospital setting.
✅ 6. Nursing Research Data Collection
- It is used in research projects to collect data on variables like stress, burnout, resilience, workload, or satisfaction.
- It ensures standardized and quantifiable data for statistical analysis.
- It strengthens the reliability and validity of research findings in evidence-based practice.
✅ 7. Tool in Quality Assurance and Audits
- It is used during internal audits to assess protocol compliance, infection control practices, or documentation accuracy.
- It supports quality improvement initiatives by identifying low-performing areas needing corrective action.
- It contributes to accreditation standards and hospital rating programs (e.g., NABH, JCI).
✅ 8. Community Health Nursing Applications
- It is used by community health nurses during surveys and home visits to assess awareness, nutritional status, and maternal health practices.
- It helps in ranking priority needs and evaluating community-based interventions.
- It supports public health planning and evaluation of outreach programs.
✅ 9. Tool for Emotional and Mental Health Assessment
- It is used by psychiatric nurses to measure psychological variables like mood, sleep quality, suicidal ideation, or emotional stability.
- It helps guide therapeutic communication and appropriate mental health referrals.
- It assists in documentation and psychiatric care planning.
✅ 10. Documentation and Legal Protection
- It is part of clinical records that provide objective documentation of patient condition over time.
- It is useful in legal situations to show standardized assessment and nursing decisions.
- It supports continuity of care, especially in shift changes or referrals.
3.Reliability of research tool
Definition of Reliability
- Reliability refers to the extent to which a research instrument consistently measures what it is intended to measure over time, across different settings, or between different observers.
- It is the degree of consistency, repeatability, and stability of the scores obtained by using the tool under similar conditions.
- A reliable tool produces similar results every time it is used in the same context with the same population, indicating that the measurement is free from random errors.
Importance of Reliability in Nursing Research
- Reliability ensures the credibility and scientific rigor of the research findings by reducing errors.
- It helps the nurse researcher to collect accurate, consistent, and dependable data for clinical decision-making.
- In tools used for assessing patient conditions (e.g., pain scales, anxiety scales, depression scores), reliability ensures fair and repeatable evaluation.
- Reliable tools contribute to evidence-based practice and help nurses in planning interventions based on dependable data.
- Reliability is closely linked with validity because a tool cannot be valid unless it is first reliable.
Types of Reliability
✅ 1. Test-Retest Reliability
- This type of reliability refers to the stability of results over time, i.e., the tool yields similar results when it is administered to the same group of participants at two different times.
- The time interval between the two tests should not be too long (to avoid memory loss) or too short (to avoid memory recall).
- Example : A knowledge questionnaire on breastfeeding is given to 30 nursing mothers today and again after 5 days—the correlation between both scores determines test-retest reliability.
✅ 2. Inter-Rater Reliability (Inter-Observer Reliability)
- This type of reliability is used to determine the degree of agreement or consistency between two or more observers rating the same event or behavior.
- It is particularly important when the measurement involves observation, scoring, or rating clinical procedures.
- Example : Two staff nurses independently evaluate pressure ulcer stages in ICU patients using the same scale—their agreement rate indicates inter-rater reliability.
✅ 3. Internal Consistency Reliability
- Internal consistency measures how well the items within a tool are related to each other, meaning whether they all assess the same construct or concept.
- It is usually tested using Cronbach’s Alpha, where a value above 0.70 is considered acceptable.
- Example : A 10-item anxiety scale should consistently reflect various dimensions of anxiety and not irrelevant topics.
✅ 4. Split-Half Reliability
- In this method, the tool is split into two equal halves, such as dividing a 20-item questionnaire into odd and even questions, and both halves are tested for correlation of results.
- It tests the internal consistency of a tool without conducting it twice.
- Example : A self-care checklist given to patients is split into two sections, and both sets should give similar mean scores if the tool is reliable.
Nursing Responsibilities in Ensuring Reliability of Research Tool
✅ 1. Selection of a Scientifically Validated Tool
- Nurse researchers are responsible for choosing tools that have been previously tested and reported to have high reliability scores (e.g., Cronbach’s alpha, Kappa coefficient) in related research studies or populations.
- They must review existing literature, standardized nursing assessments, or psychological scales before finalizing a tool.
✅ 2. Pilot Testing to Assess Reliability
- Before using the tool in actual research, nurses must conduct a pilot study or pre-test with a small group of subjects to identify any flaws or inconsistencies in the tool.
- Based on the results, they should revise, remove, or improve items that may lower internal consistency.
✅ 3. Ensuring Consistent Data Collection Procedure
- Nurses must ensure that the tool is administered under the same conditions (setting, time, instructions) for all participants to eliminate variability.
- For example, if a pain scale is administered in a quiet room with the same explanation each time, the reliability increases.
✅ 4. Training Research Assistants and Co-Researchers
- If the study involves multiple data collectors or raters, the nurse must conduct training sessions so that all team members understand how to use the tool correctly.
- This increases inter-rater reliability and reduces subjectivity in assessments.
✅ 5. Maintaining Clarity and Simplicity of Tool Items
- The nurse researcher should carefully review each item in the tool to ensure it is clear, specific, culturally appropriate, and free from double meanings or jargon.
- This avoids participant confusion and improves internal consistency reliability.
✅ 6. Proper Scoring and Coding Practices
- Nurses must use accurate scoring methods and consistent coding systems while entering responses into data sheets or software, to maintain the uniformity of data.
- Miscalculation or inconsistent score assignment can damage the reliability of findings.
✅ 7. Regular Monitoring During Data Collection
- Throughout the study, nurse researchers must monitor for deviations in how the tool is being administered and correct them immediately.
- This includes checking for skipped questions, wrong instructions, or non-uniform interviewing techniques.
✅ 8. Periodic Review of Inter-Rater Scores
- If observation-based tools are being used, the nurse must check and compare ratings from multiple observers periodically to ensure consistency.
- Where disagreements occur, retraining or clarification should be done to correct the scoring pattern.
✅ 9. Documenting and Reporting Reliability Measures
- Nurses have a responsibility to report the reliability coefficient (e.g., Cronbach’s alpha, test-retest correlation) in the final research document, along with the type of reliability tested.
- This builds transparency, credibility, and allows other researchers to use or adapt the tool.
✅ 10. Applying Reliable Tools in Clinical Practice
- In evidence-based nursing practice, reliable tools must be selected for routine patient assessments such as pain scales, Braden scale, and anxiety screening tools.
- Nurses are responsible for using scientifically proven reliable tools in the clinical setting to provide safe, effective, and consistent patient care.
4.Steps of developing conceptual framework
- A conceptual framework is a logically developed structure that organizes ideas, variables, and their relationships to explain the research phenomenon and guide the study.
- In nursing, a conceptual framework helps to link theoretical knowledge with practical nursing problems to develop evidence-based care strategies.
- It is often based on existing nursing theories or models and is used to explain, predict, or understand phenomena in a scientific manner.
Steps of Developing a Conceptual Framework
✅ 1. Identification of the Research Problem
- The first step involves defining the area of interest or clinical issue that needs to be investigated in the study.
- The nurse researcher must clearly frame a research problem statement that is focused, researchable, and relevant to nursing care or public health.
- Itbis important to ensure that the problem chosen addresses a gap in knowledge or practice, such as poor pain assessment in postoperative care.
✅ 2. Conducting a Literature Review
- A detailed literature review helps the researcher to understand what has already been studied, which theories have been used, and what gaps still exist.
- It includes reviewing books, research articles, nursing journals, online databases like CINAHL, PubMed, etc.
- This step helps in identifying existing theoretical models or concepts that can be adopted or adapted to the current research problem.
✅ 3. Identification of Key Concepts and Variables
- The researcher then selects the major concepts related to the problem, such as knowledge, attitude, behavior, compliance, anxiety, etc.
- These concepts are classified into independent, dependent, moderating, or extraneous variables, and each variable is given a clear operational definition.
- This step helps in aligning the variables with the objectives and hypothesis of the study.
✅ 4. Establishing Relationships Among Concepts (Assumptions & Propositions)
- The researcher develops logical assumptions or propositions about how the variables are expected to relate to each other based on theory or prior evidence.
- Example : “Better health education (independent variable) improves medication adherence (dependent variable).”
- This step is important to form the foundation for research questions or hypotheses.
✅ 5. Designing a Visual Framework (Model Development)
- The concepts and variables are arranged in a diagrammatic format using arrows, blocks, and directional flows to indicate relationships.
- It visually explains the cause-effect pathways or interactions between variables.
- This model becomes a blueprint for tool development, data analysis, and interpretation.
✅ 6. Linking the Framework to Research Objectives and Hypotheses
- Each element in the conceptual framework must be linked to specific research objectives and hypotheses.
- It helps in guiding the development of the questionnaire, interview schedule, or checklist used in data collection.
- It provides a structure for organizing data and testing the expected relationships during data analysis.
✅ 7. Testing, Reviewing, and Refining the Framework
- After drafting the initial conceptual framework, it should be reviewed by subject experts or guides for logic, clarity, and alignment with objectives.
- If a pilot study is conducted, feedback can be used to modify or refine the conceptual framework.
- The finalized framework should be feasible, relevant to nursing practice, and adaptable during actual research.
Nursing Responsibilities in Developing a Conceptual Framework
✅ 1. Application of Nursing Theories
Nurses must apply appropriate nursing theories or models (such as Roy’s Adaptation Model, Orem’s Self-care Theory, or Neuman’s System Model) when developing the framework to ensure nursing relevance and scientific accuracy.
✅ 2. Identification of Nursing-Specific Variables
The nurse researcher should ensure that concepts included in the framework reflect key aspects of nursing care such as pain, patient satisfaction, hygiene practices, mobility, communication, etc.
✅ 3. Ensuring Patient-Centered Focus
The conceptual framework should be oriented toward improving patient outcomes, and nurses must ensure that the research reflects holistic patient care including physical, emotional, and social dimensions.
✅ 4. Ethical Consideration in Framework Design
Nurses must incorporate ethical principles while framing assumptions and relationships, especially in sensitive research areas like mental health, terminal illness, or pediatric care.
✅ 5. Linking Framework to Nursing Practice and Education
The framework developed should help nurses to translate theory into practice, guide curriculum development in nursing education, and influence policies in clinical settings.
✅ 6. Using Framework for Evidence-Based Practice
Nurses are responsible for ensuring that the conceptual framework supports the generation of evidence that can be used in bedside nursing, community health interventions, or healthcare programs.
5.Snowball sampling
Definition of Snowball Sampling
- Snowball sampling is a type of non-probability sampling technique, in which the researcher selects a few initial participants who fit the inclusion criteria and then asks those participants to identify or refer other individuals they know who also qualify for the study.
- It is called “snowball” because the number of participants grows like a snowball rolling downhill, gradually increasing in size through referrals or networks.
- This method is primarily used when the target population is difficult to locate or when a formal list or sampling frame is not available.
Characteristics / Features of Snowball Sampling
- It is a chain-referral technique where existing subjects help the researcher reach more potential subjects.
- It is non-random in nature and hence cannot claim to produce statistically generalizable results.
- This method is qualitative-friendly and especially useful for exploratory or descriptive research designs.
- Participants are selected based on personal networks and trust, which is particularly important in sensitive research areas.
- The final sample is not predetermined, and data collection continues until data saturation or the required sample size is achieved.
Steps of Snowball Sampling (Process)
- The researcher identifies and selects a few initial subjects who meet the eligibility criteria (called “seeds”).
- These initial participants are requested to nominate or refer other individuals within their network who also qualify.
- The referred individuals are contacted, assessed, and if found eligible, they are included in the study.
- These new participants again provide further referrals, and this referral chain continues.
- The process continues until enough data is collected, or no new referrals are available (called “sampling saturation”).
✅ Advantages of Snowball Sampling
- It is highly effective for studying hidden, marginalized, or hard-to-reach populations, such as drug abusers, sex workers, undocumented immigrants, or patients with rare diseases.
- It requires fewer resources and is less costly and time-consuming compared to random sampling techniques, especially when the target population is not easily accessible.
- The trust factor is high, because the referrals come from personal or social networks, making participants more likely to cooperate and provide honest information.
- It helps in building rapport and access to populations that may not respond to traditional data collection methods or surveys.
Disadvantages of Snowball Sampling
- The major drawback is that it introduces selection bias, since participants are not randomly chosen and tend to refer people similar to themselves (homogeneity bias).
- The sample may not be representative of the larger population, hence limiting generalizability of findings.
- It can violate confidentiality or privacy, especially when participants are uncomfortable referring others in sensitive studies.
- It depends heavily on initial contacts; if they are not diverse or well-connected, the resulting sample can be skewed or limited.
- It lacks control over sample size and structure, as growth of sample depends on willingness of participants to refer others.
Uses in Nursing and Health Research
- Snowball sampling is particularly useful in mental health nursing research, for accessing patients with psychiatric illness, suicidal ideation, or PTSD who may be reluctant to participate.
- It is helpful in community health nursing, especially when researching stigmatized or hidden groups like HIV-positive individuals, transgender people, or substance users.
- It is widely applied in qualitative research methods in nursing to explore beliefs, cultural norms, and behaviors of minority groups or tribal communities.
- In epidemiological studies conducted by nurses, snowball sampling assists in mapping transmission patterns of diseases like hepatitis B or tuberculosis within close-knit communities.
Nursing Management / Nursing Responsibilities
1. Ethical Responsibility of Informed Consent
- The nurse researcher has the responsibility to ensure that each participant in snowball sampling gives voluntary, informed, and written consent, which includes an understanding of the study’s purpose, procedures, possible risks, and the nature of referrals.
- It is the duty of the nurse to explain that participation is completely voluntary, and that individuals may withdraw at any time without penalty.
2. Maintaining Confidentiality and Privacy
- Nurses must maintain strict confidentiality of both the participants and the individuals they refer during snowball sampling, especially when dealing with sensitive or stigmatized populations such as HIV/AIDS, drug users, or mentally ill patients.
- Nurses must ensure that names, addresses, and personal details are kept secure and not shared without permission, thus maintaining ethical standards in research.
3. Ensuring Voluntary Referrals Without Coercion
- It is the nurse’s duty to make sure that participants who are asked to refer others are not pressured, influenced, or manipulated to provide names.
- The nurse must create a comfortable and respectful environment, where participants feel safe and empowered to either refer others or refuse without fear or guilt.
4. Culturally Sensitive Communication
- Nurses are responsible for using culturally appropriate, respectful, and sensitive language while interacting with diverse populations during the snowball sampling process.
- When dealing with tribal groups, sex workers, or LGBTQ+ communities, the nurse should demonstrate cultural humility and non-judgmental behavior to build trust and encourage participation.
5. Building Rapport with Initial Participants (“Seeds”)
- Nurses must take the time to establish strong rapport and trust with the first few participants, as these individuals serve as the foundation of the referral chain in snowball sampling.
- By ensuring a positive, respectful, and empathetic relationship, the nurse can increase the likelihood of referrals and honest participation.
6. Monitoring Sample Bias and Diversity
- Nurses involved in the research process should observe and document any bias emerging due to over-reliance on one network or social group, and try to reach diverse participants through new seeds if necessary.
- The nurse researcher should attempt to broaden recruitment chains to increase representativeness and reduce homogeneity of the sample.
7. Safe and Appropriate Data Collection
- It is the nurse’s responsibility to collect data in a safe, respectful, and private environment, ensuring that both the physical and emotional well-being of the participants is protected.
- Nurses must be trained to conduct interviews without leading questions, and must handle any emotional distress or disclosures (e.g., trauma, abuse) with professional support or referrals.
8. Ethical Referral Practices in Sensitive Research
- When researching topics like sexual abuse, domestic violence, HIV status, or substance use, the nurse must be extra cautious to avoid breaching privacy or putting referred individuals at risk.
- The nurse should seek consent from the new referral before mentioning who referred them, and never approach referred individuals without clear permission.
9. Documentation and Record Keeping
- Nurses must keep detailed, accurate, and secure records of the sampling process, including number of referrals, interview schedules, signed consent forms, and demographic details, while ensuring anonymity in public reporting.
- It is important to maintain a logbook or referral chart that shows the snowball chain for internal review while keeping identities confidential.
10. Collaborating with Community Health Workers or NGOs
- Nurses may coordinate with local health workers, NGOs, or peer educators to identify seeds and facilitate snowball referrals in a more ethical and effective manner, especially in field or community-based studies.
- Nurses should ensure that collaboration partners are also trained in confidentiality and ethical sampling procedures
Section II
Q 5 a) Explain Scale of measurement. (10+5=15)
Definition
- The scale of measurement refers to the system or rule that determines how a particular variable is classified, ranked, or measured, so that it can be quantitatively analyzed and interpreted in research.
- It is the foundation of statistical analysis because it determines what type of data you have, and thereby what kind of statistical techniques are suitable.
- In simple terms, a scale of measurement describes the relationship among the values that a variable can take and how these values can be manipulated mathematically.
Purpose of Using Scale of Measurement
- It is used to organize and classify data for accurate analysis and interpretation.
- It helps the researcher to choose appropriate statistical tools and tests.
- It provides a clear understanding of data type (qualitative or quantitative).
- It supports validity and reliability of data collection tools like questionnaires or rating scales.
- It is essential for ensuring that data are measured, compared, and reported meaningfully.
FOUR MAJOR TYPES OF SCALES OF MEASUREMENT
These four scales are arranged in order of increasing complexity and mathematical power.
1️⃣ NOMINAL SCALE
- Name Only, No Order, No Quantity
- It is the most basic and simplest level of measurement, where values are categorized but not ranked.
- The numbers or labels used are just symbolic codes to differentiate categories — they have no numerical meaning.
- There is no sense of greater or lesser between the categories.
- Only equality or inequality can be tested (e.g., Male ≠ Female).
- You can only count the frequency or calculate the percentage for each category.
- No addition, subtraction, or other mathematical functions can be used.
Examples :
- Blood Group : A, B, AB, O
- Gender : Male, Female, Other
- Religion : Hindu, Muslim, Christian, Sikh
- Hospital Wards: General, Private, ICU
Use in Nursing :
- Used in classifying patients by gender, blood type, diagnosis, or department.
2️⃣ ORDINAL SCALE
- Order Without Equal Interval
- It allows for ranking or ordering of variables based on a specific criterion, but the exact difference between the ranks is not known.
- The values indicate relative position, but not the magnitude of difference between them.
- It tells which is more or less, but not how much more or less.
- Mathematical operations like addition or averaging are not meaningful here.
- It allows the use of non-parametric tests in analysis.
Examples :
- Pain level : No Pain (1), Mild (2), Moderate (3), Severe (4)
- Satisfaction level : Very Dissatisfied to Very Satisfied
- Tumor Grade : Grade I, Grade II, Grade III
- Triage Level : Red (critical), Yellow (urgent), Green (stable)
Use in Nursing :
- Used in pain scales, anxiety scales, satisfaction surveys, and patient prioritization in emergencies.
3️⃣ INTERVAL SCALE
- Order + Equal Interval Without True Zero
- This scale allows measurement of the distance between values, meaning the intervals are equal.
- However, it does not have an absolute or true zero, so ratios are meaningless (e.g., 20°C is not twice as hot as 10°C).
- You can perform addition and subtraction, but not multiplication or division.
- Negative values can exist because zero does not mean “nothing.”
Examples :
- Temperature in Celsius or Fahrenheit
- IQ scores (e.g., 90, 110, 130)
- Date or Year (e.g., 1990, 2020)
- Standardized test scores (e.g., nursing entrance exams)
Use in Nursing :
- Used in temperature charting, psychological assessments, and educational measurements.
4️⃣ RATIO SCALE
- Order + Equal Interval + True Zero
- This is the most informative and powerful measurement scale, as it includes all characteristics of nominal, ordinal, and interval scales.
- It has a true and absolute zero point, meaning zero indicates complete absence of the quantity being measured.
- All mathematical operations can be applied: addition, subtraction, multiplication, division.
- Ratios make sense (e.g., a patient weighing 80 kg is twice as heavy as one weighing 40 kg).
Examples :
- Weight in kilograms or pounds
- Height in centimeters or inches
- Blood pressure (mmHg)
- Pulse rate (beats/minute)
- Urine output (ml)
- Oxygen saturation (%)
Use in Nursing
- Used to measure vital signs, lab values, fluid intake/output, anthropometric data, etc.
Why Is It Important in Nursing Research?
- It helps the nurse researcher understand the nature of collected data, whether it is categorical, ordered, or numerical.
- It guides the researcher to select the right statistical tests, such as chi-square, t-test, ANOVA, correlation, etc.
- It ensures validity and accuracy in result interpretation by using appropriate tools.
- It assists in tool development, such as designing questionnaires and rating scales.
- It prevents misuse of statistical analysis by defining how far mathematical operations can be applied to data.
- It is essential in constructing variables and assigning them values in a measurable form.
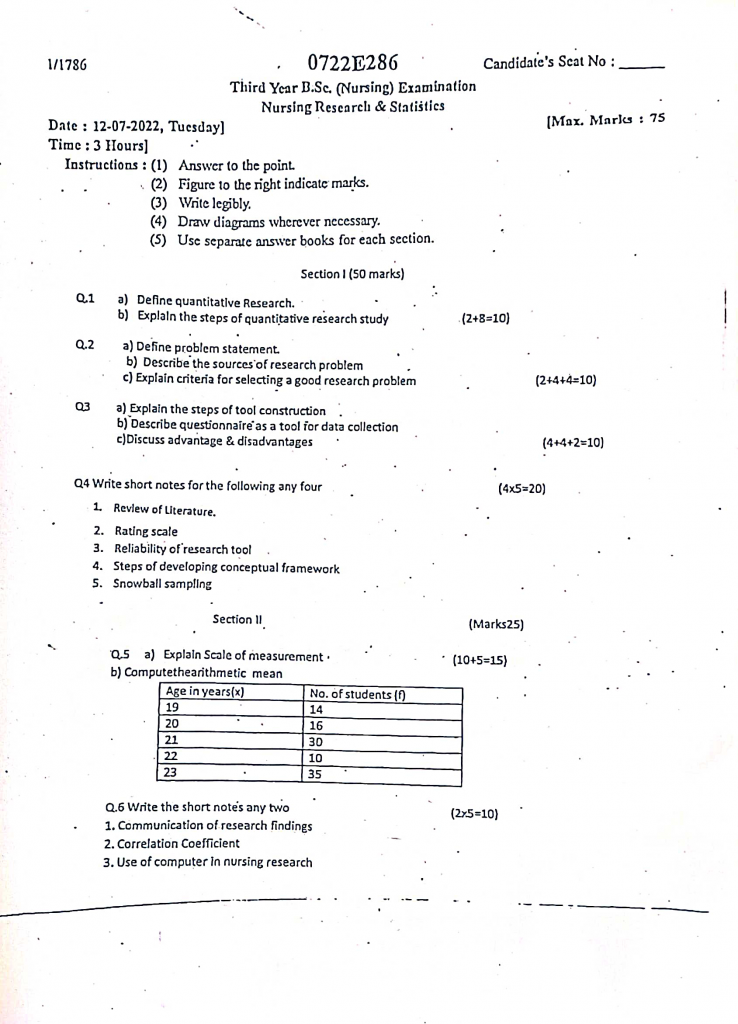
b) Computethearithmetic mean
Age in years(x) No. of students (I)
19 14
20 16
21 30
22 10
23 35
Answer
Formula for Arithmetic Mean (𝑥̄) :
𝑥̄ = ∑fx / ∑f
where :
𝑥 = Value of the variable (Age in years)
𝑓 = Frequency (No. of students)
𝑓𝑥 = Product of 𝑥 and 𝑓
Step-by-Step Calculation
| Age (x) | No. of Students (f) | fx = x × f |
|---|---|---|
| 19 | 14 | 266 |
| 20 | 16 | 320 |
| 21 | 30 | 630 |
| 22 | 10 | 220 |
| 23 | 35 | 805 |
| Σf = 105 | Σfx = 2241 |
Apply the formula :
𝑥̄ = ∑fx / ∑f
𝑥̄ = 2241/105
𝑥̄ = 21.34
Arithmetic Mean (Average age) = 21.34 years
Q.6 Write the short notes any two (2×5=10)
1.Communication of research findings
Definition
- Communication of research findings refers to the systematic process of conveying the outcomes, results, interpretations, and implications of a research study to the relevant individuals or institutions, such as research participants, academic communities, health professionals, policymakers, administrators, and the public.
- It is the final stage of the research process, where the knowledge gained from the study is shared with others for application, discussion, and further development.
- It is essential for ensuring that research contributes meaningfully to clinical practice, healthcare policy, and future investigations.
Purpose of Communicating Research Findings
- To disseminate new knowledge, evidence, or discoveries to nursing professionals, healthcare teams, and scientific communities.
- To influence and guide clinical practice, nursing education, and public health policy based on research evidence.
- To fulfill the ethical obligation of sharing results with participants and contributors.
- To allow peer evaluation, criticism, and validation of the study for transparency and scientific progress.
- To provide a base for further research, innovation, and evidence-based nursing practices.
- To enhance awareness and learning among students, nurses, and other professionals.
- To support decision-making in health programs and nursing management.
Importance of Communication of Research Findings in Nursing
- It is essential for evidence-based practice, where nurses apply research results to deliver high-quality care.
- It promotes transparency and academic honesty by sharing the methodology, data, and results openly.
- It helps nursing researchers gain recognition and professional growth through publication or presentation.
- It contributes to national and institutional health policies when shared with administrative or governmental bodies.
- It helps standardize nursing procedures and protocols across different institutions.
- It fosters collaboration and teamwork in multidisciplinary healthcare research.
- It enhances the scientific credibility and visibility of the nursing profession.
Methods or Channels of Communicating Research Findings:
1. Written Communication
- Written communication is the most widely used and formal method of presenting research findings, in which the researcher prepares a detailed report or document explaining the study background, objectives, methods, results, interpretations, and conclusions.
- This type of communication includes research dissertations or theses submitted by nursing students, project evaluation reports, technical summaries, and scientific research articles prepared for publication.
- The written method ensures that the research is permanently recorded, reviewed, and referred to by other researchers and healthcare professionals in the future.
2. Oral Communication
- Oral communication involves the verbal presentation of research results in front of a live audience, such as during academic seminars, faculty meetings, classroom teaching, research colloquiums, workshops, or professional conferences.
- It enables the researcher to explain their study face-to-face, and also allows immediate feedback, questions, and discussion, which helps in improving the clarity and depth of the findings.
- This method is especially useful when findings need to be shared quickly, or when the audience includes students, nurses, or administrators who benefit more from direct verbal explanation.
3. Poster Presentation
- A poster presentation is a visual and concise method of displaying research findings using printed or digital posters that include headings, graphs, tables, charts, bullet points, and key summaries.
- It is commonly used in college exhibitions, professional conferences, health science fairs, and symposiums, where researchers can interact informally with interested viewers and explain their study within a short time.
- This type of communication is best suited for quick overview and visual impact, especially when the audience prefers brief and to-the-point information.
4. Publication in Journals
- Publication in peer-reviewed national or international journals is considered the most professional and credible method of communicating research findings, as it involves expert review, formatting standards, and wide academic reach.
- This method involves submitting the full research manuscript, including abstract, introduction, literature review, methodology, results, discussion, conclusion, and references, to a scientific or nursing journal.
- Once accepted, the article is made available to researchers, practitioners, educators, and institutions globally, which helps the research to influence policy and practice on a larger scale.
5. Digital and Electronic Communication
- Digital communication refers to the use of internet and technology platforms to share research findings through emails, e-newsletters, webinars, blogs, online repositories, Google Scholar, YouTube, and academic websites.
- This method allows the findings to reach a wider audience rapidly, especially in situations like pandemics or global health issues, where quick knowledge sharing is vital.
- It is also useful for students and professionals who access research from mobile devices or digital libraries, thus promoting cost-effective, paperless, and borderless communication.
6. Conference Presentations and Workshops
- In this method, the researcher presents their study as part of scientific sessions, panel discussions, or breakout groups in state, national, or international conferences.
- Workshops may also involve interactive activities, where findings are demonstrated, applied, or debated, leading to collaborative learning and knowledge exchange.
- These platforms allow researchers to network with other professionals, receive peer feedback, and get recognition for their contributions.
Steps Involved in Communication of Research Findings
- Organize and interpret the results of the study clearly and systematically.
- Prepare a summary of key findings, conclusions, and implications.
- Choose an appropriate method or format of communication based on the audience (e.g., formal report, poster, oral talk).
- Ensure the content is accurate, unbiased, ethical, and easy to understand.
- Include tables, charts, and references as supporting evidence.
- Cite all sources properly to avoid plagiarism and maintain academic integrity.
- Submit or present the findings to relevant platforms — journals, conferences, institutions.
- Be ready to receive feedback or questions and engage in discussion for further improvement.
Target Audiences for Communication of Research Findings
- Nursing students and educators
- Clinical nurses and nurse administrators
- Hospital and public health policymakers
- Government and NGO health departments
- National and international journal readers
- Community health workers and program planners
2.Correlation Coefficient
Definition
- The correlation coefficient is defined as a statistical measure that expresses the strength and direction of a linear relationship between two quantitative (numerical) variables.
- It tells us how one variable changes when the other variable changes and whether these changes occur in the same direction or opposite direction.
- The correlation coefficient is denoted by the letter “r” and is most commonly calculated using Pearson’s method for parametric data and Spearman’s method for non-parametric data.
Range of Correlation Coefficient
- The value of the correlation coefficient always lies between –1 and +1.
- +1 indicates a perfect positive linear correlation.
- –1 indicates a perfect negative linear correlation.
- 0 indicates no correlation at all between the two variables.
Types of Correlation Based on the Value of ‘r’
1️⃣ Perfect Positive Correlation (r = +1)
- A correlation coefficient of +1 indicates a perfect positive correlation, meaning that as one variable increases, the other also increases in a perfectly consistent and linear manner.
- In this relationship, every increase in one variable corresponds exactly to a proportional increase in the other.
- Example in nursing: A perfect relationship between hours of study and marks scored, assuming every extra hour studied results in a fixed increase in marks.
2️⃣ Strong Positive Correlation (r = +0.70 to +0.99)
- This indicates a strong direct relationship between two variables, meaning as one variable increases, the other tends to increase significantly.
- The values lie between +0.70 to +0.99, showing a high degree of association, though not perfect.
- Example : Height and weight in children — generally, taller children tend to weigh more.
3️⃣ Moderate Positive Correlation (r = +0.30 to +0.69)
- This range indicates a moderate but noticeable relationship, where increases in one variable are often associated with increases in the other, but not always consistently.
- It is statistically meaningful but shows some variability in the trend.
- Example: Number of antenatal visits and newborn health outcomes — more visits may lead to better outcomes, but with some exceptions.
4️⃣ Weak Positive Correlation (r = +0.01 to +0.29)
- This shows a weak or low positive relationship, where the variables move in the same direction, but the association is minimal and may not be statistically significant.
- Such a correlation suggests that other variables might be influencing the relationship.
- Example : Satisfaction with hospital food and overall hospital rating — slightly related, but not strongly.
5️⃣ No Correlation (r = 0)
- A correlation coefficient of zero implies no linear relationship between the two variables.
- Changes in one variable do not predict or affect changes in the other variable.
- Example: Blood group and intelligence level — no association exists.
6️⃣ Weak Negative Correlation (r = –0.01 to –0.29)
- This reflects a very slight inverse relationship, where as one variable increases, the other tends to decrease slightly, but not strongly enough to be highly relevant.
- It suggests a minimal and possibly non-significant trend.
- Example: Minor increase in exercise duration and a slight decrease in stress levels.
7️⃣ Moderate Negative Correlation (r = –0.30 to –0.69)
- This level indicates a moderate inverse relationship, meaning as one variable increases, the other decreases at a noticeable and somewhat consistent rate.
- The trend is stronger than weak correlation but still allows variability.
- Example: Increase in smoking frequency and decrease in lung function.
8️⃣ Strong Negative Correlation (r = –0.70 to –0.99)
- A strong negative correlation shows that as one variable increases, the other consistently decreases, and the relationship is significantly inverse.
- The value is close to –1, showing high predictive power, though not perfect.
- Example: Patient adherence to diet and blood sugar level — higher adherence is associated with significantly lower blood sugar.
9️⃣ Perfect Negative Correlation (r = –1)
- A correlation of –1 indicates a perfect inverse relationship, where every increase in one variable corresponds to a perfectly proportional decrease in the other.
- This is extremely rare in real-world data.
- Example (hypothetical): 100% adherence to a medication leads to a 100% reduction in symptoms.
Interpretation of the Value of ‘r’:
| Value of r | Meaning |
|---|---|
| +1 | Perfect positive correlation |
| +0.70 to +0.99 | Strong positive correlation |
| +0.30 to +0.69 | Moderate positive correlation |
| +0.01 to +0.29 | Weak positive correlation |
| 0 | No correlation |
| –0.01 to –0.29 | Weak negative correlation |
| –0.30 to –0.69 | Moderate negative correlation |
| –0.70 to –0.99 | Strong negative correlation |
| –1 | Perfect negative correlation |
Common Methods of Calculating Correlation
1️⃣ Pearson’s Product-Moment Correlation Coefficient (r):
- Used for interval or ratio scale data that is normally distributed.
- Measures the linear relationship between two continuous variables.
- Requires data to have no extreme outliers and a linear trend.
2️⃣ Spearman’s Rank Correlation Coefficient (ρ or rs):
- Used when data are ordinal, not normally distributed, or when outliers are present.
- It measures the monotonic relationship between two ranked variables.
- Commonly used in nursing research for Likert-scale responses or ranked scores.
Importance of Correlation Coefficient in Nursing Research
- It helps identify associations between clinical variables, such as age and recovery time.
- It supports predictive studies — for example, predicting infection risk based on hygiene score.
- It guides tool validation — like checking if knowledge scores correlate with practice scores.
- It contributes to evidence-based nursing practice by highlighting relationships in health behavior.
- It helps in data interpretation, providing meaning to raw numbers collected in fieldwork.
- It assists in hypothesis testing by supporting or rejecting relationships.
- It is useful in evaluating interventions — for example, the correlation between education and immunization uptake.
- It enhances research accuracy and helps in choosing correct statistical tests.
Practical Example in Nursing
- A researcher studying the relationship between the number of antenatal visits and birth weight of newborns may use the correlation coefficient.
- If r = +0.75, this would show a strong positive correlation, meaning more antenatal visits are associated with higher birth weight.
3.Use of computer in nursing research
In modern nursing research, computers play a crucial role in enhancing the accuracy, speed, and efficiency of the entire research process. Computers help researchers collect, store, analyze, interpret, and present data scientifically. The use of computers supports evidence-based nursing practice and advances clinical research outcomes.
1. Literature Review and Information Retrieval
- Computers provide access to millions of research articles and databases worldwide, allowing up-to-date and global literature searches.
- They enable use of Boolean search strategies (AND, OR, NOT) to refine search results.
- Researchers can bookmark, highlight, and organize references using citation managers (like Mendeley, EndNote).
- They support PDF downloading, annotation, and sharing of literature with colleagues.
- It helps in building a strong theoretical and conceptual foundation for the research problem.
2. Designing Research Tools and Questionnaires
- Computers allow the use of user-friendly interfaces to design digital surveys with closed, open-ended, Likert scale, or rating-type questions.
- Features like branching logic (showing or hiding questions based on previous answers) improve relevance of tools.
- Surveys designed using software (e.g., Google Forms, Qualtrics) can be embedded into emails or websites for quick response collection.
- Helps in saving paper, time, and printing costs, making the process eco-friendly.
- Allows real-time response monitoring and ensures higher participation.
3. Data Collection and Entry
- Researchers can collect data through online forms, mobile data collection apps (ODK, KoBoCollect), or tablets in field settings.
- Computers allow validation rules (e.g., number limits, required fields) to reduce entry errors.
- Immediate data syncing to cloud eliminates risk of data loss.
- Built-in tools help in tracking response rates, identifying missing data, and managing records.
- Enables simultaneous multi-user data entry in large-scale research projects.
4. Data Analysis and Statistical Processing
- Software like SPSS, R, Excel, and STATA allow calculation of both descriptive statistics (mean, median, SD) and inferential statistics (t-test, chi-square, ANOVA).
- Qualitative data analysis software (e.g., NVivo, Atlas.ti) helps in thematic coding and content analysis.
- Graphical representations like line graphs, pie charts, histograms enhance understanding and communication of results.
- Allows for advanced modeling (e.g., regression, path analysis, survival analysis).
- Makes it easy to perform data cleaning, transformation, and recoding.
5. Report Writing and Presentation
- Word processors (e.g., MS Word) help in writing well-structured reports with headings, tables, and citations.
- Citation software (e.g., Zotero, Mendeley) can automatically format references in APA, MLA, Vancouver, etc.
- Presentations can be created using PowerPoint, Prezi, Canva, with animations and visuals to improve engagement.
- Computers allow for multiple editing, version control, and document sharing.
- Researchers can collaboratively write papers with co-authors using Google Docs or MS Teams.
6. Communication and Collaboration
- Video conferencing tools (Zoom, Google Meet) help in virtual research meetings, expert interviews, and discussions.
- Email and cloud platforms are used to share datasets, draft documents, and feedback in real-time.
- Platforms like ResearchGate and Academia.edu help connect with global researchers.
- Communication with IRBs (Institutional Review Boards) for ethical approval can be managed digitally.
- Enables collaborative international studies and multicenter trials in nursing.
7. Data Storage and Backup
- Research data can be stored in organized folders and databases, with password protection for privacy.
- Backup systems (like external drives or cloud services) prevent data loss due to technical failures.
- Files can be encrypted and protected with multi-level security protocols.
- Cloud services allow access from anywhere, enabling remote work on research.
- Long-term storage allows for future reference, verification, or secondary analysis.
8. Ethical Compliance and Plagiarism Check
- Computers support plagiarism detection tools like Turnitin, Grammarly, and Copyscape, ensuring originality.
- Participant information can be stored with anonymization and coding systems for confidentiality.
- Secure digital systems help in tracking ethical approvals, consent forms, and audit trails.
- Data encryption tools protect against unauthorized access and breaches.
- Ethics software (e.g., IRBManager) is used to submit and monitor ethical applications.
