11/07/2022-B.SC-MENTAL HEALTH-PAPER DONE
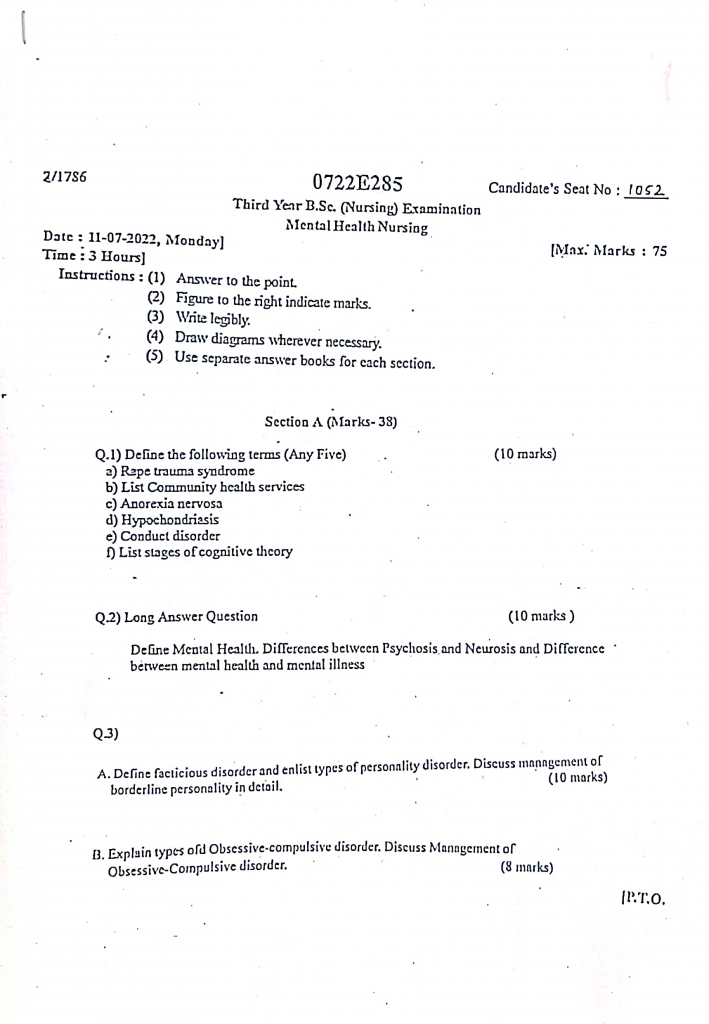
Section A (marks 38)
Q.1 Define the following terms (any five) (10 marks)
a) Rape truma syndrome
- Rape Trauma Syndrome is a psychological and physical response pattern that occurs in a survivor following a sexual assault or rape.
- It is a form of post-traumatic stress disorder (PTSD) that includes symptoms such as shock, denial, anxiety, fear, helplessness, sleep disturbances, flashbacks, depression, and social withdrawal.
- This syndrome reflects the emotional, behavioral, and physiological impact of the traumatic event on the victim.
b) List community health services
- Maternal and Child Health (MCH) Services
- Family Planning Services
- Immunization Services
- School Health Services
- Nutrition Services
- Communicable Disease Control Services
- Non-Communicable Disease (NCD) Services
- Environmental Sanitation Services
- Occupational Health Services
- Mental Health Services
- Home-based Care Services
- Emergency and Referral Services
- Health Education and Counseling Services
- Geriatric and Palliative Care Services
- Adolescent Health Services
- Reproductive and Sexual Health Services
- Disability and Rehabilitation Services
- Urban Health Services
- Tribal Health Services
- Telemedicine and E-health Services
c) Anorexia nervousa
- Anorexia Nervosa is a serious eating disorder characterized by an intense fear of gaining weight, a distorted body image, and self-imposed starvation, leading to significant weight loss and nutritional deficiencies.
- It primarily affects adolescents and young adults, especially females, and is often associated with emotional, psychological, and behavioral disturbances related to food and body shape.
d) Hypochondriasis
- Hypochondriasis is a psychological disorder in which a person has an excessive and persistent fear or belief of having a serious medical illness, despite repeated medical evaluations and reassurance showing no significant health problem.
- It is now referred to as Illness Anxiety Disorder in DSM-5 and is characterized by preoccupation with bodily symptoms, frequent doctor visits, and heightened health-related anxiety that interferes with daily functioning.
e) Conduct disorder
- Conduct Disorder is a behavioral and emotional disorder seen in children and adolescents, characterized by a persistent pattern of aggressive, defiant, and antisocial behavior that violates societal norms, rules, and the basic rights of others.
- The individual often shows behaviors such as lying, stealing, physical aggression, truancy, destruction of property, and lack of remorse, which significantly impair social, academic, and family functioning.
f) List stages of cognitive theory
- Sensorimotor Stage (Birth to 2 years)
- Preoperational Stage (2 to 7 years)
- Concrete Operational Stage (7 to 11 years)
- Formal Operational Stage (11 years and above)
Q.2 Long answer question (10 mark)
a) Define mental health. Difference between psychosis and neurosis and difference between mental health and mental illness.
Definition of Mental Health
- Mental health is a state of emotional, psychological, and social well-being in which an individual can cope with the normal stresses of life, work productively, and contribute to their community.
- It is not just the absence of mental illness, but also the presence of positive mental functioning such as resilience, emotional stability, and clear thinking.
- According to the World Health Organization (WHO), mental health is : “A state of well-being in which the individual realizes his or her own abilities, can cope with the normal stresses of life, can work productively, and is able to make a contribution to his or her community.”
- Mental health includes positive self-esteem, ability to form relationships, adaptability to changes, and an understanding of reality.
Difference between Psychosis and Neurosis
| 🔹 Point of Difference | 🧠 Psychosis | 💭 Neurosis |
|---|---|---|
| 1. Definition | A severe mental disorder involving loss of contact with reality | A mild mental disorder with retained reality perception |
| 2. Insight | Absent or severely impaired | Present or partially impaired |
| 3. Reality Testing | Disturbed – patient believes delusions or hallucinations are real | Intact – patient knows their thoughts are irrational |
| 4. Perception | Hallucinations and delusions are commonly present | No hallucinations or delusions |
| 5. Thought Process | Disorganized, illogical, or bizarre | Coherent, logical but anxious or obsessive |
| 6. Emotional Expression | Inappropriate, flat, or exaggerated | Controlled but often anxious or depressed |
| 7. Behavior | Bizarre, unpredictable, or aggressive | Avoidant, ritualistic, or anxious behaviors |
| 8. Functioning in Society | Severely impaired personal, social, and occupational functioning | Partially affected, can often function independently |
| 9. Examples | Schizophrenia, Mania, Delusional disorder | Phobias, OCD, Anxiety disorders, Depression (mild) |
| 10. Treatment | Requires antipsychotics and possibly hospitalization | Treated with psychotherapy and antidepressants |
Difference between Mental Health and Mental Illness
| 🔹 Point of Difference | 🌟 Mental Health | 🚨 Mental Illness |
|---|---|---|
| 1. Definition | A positive state of well-being, enabling effective coping and functioning | A clinically diagnosable disorder causing distress or impairment |
| 2. Functioning | Performs daily roles effectively and adaptively | Difficulty or inability to perform daily activities |
| 3. Cognitive Abilities | Thinking is rational, logical, and clear | Thinking may be irrational, disorganized, or delusional |
| 4. Emotional State | Stable, resilient emotions | Mood disturbances, emotional instability or numbness |
| 5. Behavior | Socially appropriate and constructive | May be bizarre, harmful, or withdrawn |
| 6. Social Relationships | Able to form and maintain healthy relationships | Often has relationship conflicts or isolation |
| 7. Reality Perception | Accurately interprets reality | May experience hallucinations or distorted beliefs |
| 8. Response to Stress | Copes effectively using healthy strategies | Poor stress management, breakdown under pressure |
| 9. Duration | Ongoing, dynamic and adaptive state | May be acute, episodic, or chronic, requiring treatment |
| 10. Examples | Resilience, empathy, problem-solving, self-confidence | Schizophrenia, Depression, OCD, PTSD, Bipolar disorder |
Q.3
a) Define factitious disorders and enlist types of personality disorder and discuss management of borderline personality in detail (10 marks)
Definition of Factitious Disorders
- Factitious disorder is a type of mental illness in which a person deliberately and consciously produces, feigns, or exaggerates physical or psychological symptoms.
- It is characterized by the intentional production of symptoms to assume the sick role and gain attention, sympathy, or care — without any external incentives (like financial gain, as seen in malingering).
- It is also known as Munchausen Syndrome in its severe form.
- The behavior is repetitive, compulsive, and driven by a deep psychological need to be seen as ill.
Enlistment of Types of Personality Disorders
According to the DSM-5 (Diagnostic and Statistical Manual of Mental Disorders, 5th edition), Personality Disorders are grouped into three clusters:
Cluster A – Odd or Eccentric Disorders
These disorders are characterized by social withdrawal, paranoid thoughts, and unusual behavior.
1️⃣ Paranoid Personality Disorder
2️⃣ Schizoid Personality Disorder
3️⃣ Schizotypal Personality Disorder
Cluster B – Dramatic, Emotional, or Erratic Disorders
These disorders involve impulsivity, emotional instability, and intense interpersonal relationships.
4️⃣ Antisocial Personality Disorder
5️⃣ Borderline Personality Disorder
6️⃣ Histrionic Personality Disorder
7️⃣ Narcissistic Personality Disorder
Cluster C – Anxious or Fearful Disorders
These disorders are associated with high levels of anxiety, fearfulness, and insecurity.
8️⃣ Avoidant Personality Disorder
9️⃣ Dependent Personality Disorder
🔟 Obsessive-Compulsive Personality Disorder (OCPD)
Management of Borderline Personality Disorder (BPD)
Borderline Personality Disorder (BPD) is a complex mental health condition that is characterized by a long-standing pattern of emotional instability, interpersonal difficulties, impulsivity, distorted self-image, and an intense fear of abandonment. Individuals with BPD often experience rapid shifts in mood and behavior, leading to significant impairment in personal, social, and occupational functioning. Therefore, the management of BPD requires a comprehensive, multi-disciplinary, and long-term approach that involves psychological therapies, pharmacological support, nursing care, and family involvement.
Psychological Management (Psychotherapy)
a) Dialectical Behavior Therapy (DBT)
- Dialectical Behavior Therapy (DBT) is considered the most effective and evidence-based form of psychotherapy for managing Borderline Personality Disorder.
- It was specifically developed for individuals with BPD and is focused on helping patients develop skills in mindfulness, emotional regulation, interpersonal effectiveness, and distress tolerance.
- DBT teaches the patient to become aware of their intense emotions, manage impulsive behavior, and reduce self-harming tendencies by replacing maladaptive coping mechanisms with healthier strategies.
b) Cognitive Behavioral Therapy (CBT)
- Cognitive Behavioral Therapy (CBT) helps patients recognize and correct distorted patterns of thinking, irrational beliefs, and self-defeating behaviors.
- It assists the patient in understanding the connection between their thoughts, feelings, and actions, thereby improving self-awareness and promoting logical and goal-directed behavior.
c) Mentalization-Based Therapy (MBT)
- Mentalization-Based Therapy aims to enhance the individual’s ability to understand their own mental state and the mental states of others.
- It focuses on developing the capacity for “mentalization” – the ability to reflect on thoughts and feelings – which helps patients regulate their emotions and reduce interpersonal conflicts.
d) Schema-Focused Therapy
- Schema-focused therapy works on identifying and altering long-standing maladaptive core beliefs, or schemas, that the patient may have developed during early life.
- This therapy aims to restructure negative thought patterns that contribute to the patient’s low self-worth and instability in relationships.
Pharmacological Management
Although there is no single medication approved to cure BPD, pharmacological treatment is often used to manage co-occurring symptoms such as mood swings, anxiety, depression, and impulsivity.
a) Selective Serotonin Reuptake Inhibitors (SSRIs)
SSRIs such as Fluoxetine, Sertraline, and Escitalopram are frequently prescribed to treat underlying symptoms of depression, anxiety, and irritability, which are common in BPD.
b) Mood Stabilizers
Mood stabilizers such as Valproate, Lithium, and Lamotrigine are used to help manage mood dysregulation, aggression, and impulsive behavior by stabilizing emotional fluctuations.
c) Atypical Antipsychotics
Second-generation (atypical) antipsychotics like Olanzapine, Quetiapine, or Risperidone may be prescribed to address paranoid thinking, anger outbursts, and dissociative symptoms that sometimes occur in BPD.
d) Anxiolytics (Anti-Anxiety Medications)
Benzodiazepines may be used cautiously and for short durations to reduce severe anxiety or agitation; however, their use must be monitored closely due to the risk of dependency or misuse, especially in impulsive patients.
Nursing Management in Borderline Personality Disorder
1. Establishing a Therapeutic Nurse–Patient Relationship
- It is important for the nurse to build a trust-based, professional, and empathetic relationship with the patient to make them feel safe and understood.
- The nurse must remain emotionally neutral, nonjudgmental, and consistent in responses to reduce the patient’s fear of abandonment or rejection.
- Due to splitting behavior (idealizing some staff and devaluing others), the nurse should use team-based communication and set limits on dependency.
2. Maintaining Structure and Setting Firm Boundaries
- The nurse must provide a predictable, structured routine to help the patient feel secure and reduce emotional chaos.
- It is essential to establish and enforce clear behavioral limits in a calm and consistent manner to reduce manipulative behavior.
- The nurse should explain the rules and consequences clearly, while being careful not to punish or reject the patient emotionally.
3. Monitoring for Self-Harm and Suicide Risk
- Individuals with BPD often engage in self-injurious behaviors such as cutting, burning, or suicidal gestures during emotional crises.
- The nurse should perform regular risk assessments, monitor the patient’s mood, and observe for warning signs of self-harm.
- If needed, the nurse should implement one-to-one observation, initiate safety contracts, and remove access to harmful objects from the environment.
4. Providing Emotional Regulation and Coping Skill Training
- The nurse should assist the patient in recognizing emotional triggers, labeling emotions, and responding in a healthy manner.
- Techniques such as deep breathing, progressive muscle relaxation, grounding exercises, or journaling may be taught to help regulate intense emotions.
- Patients should be encouraged to channel emotional energy into constructive outlets like art therapy, music, or physical activity.
5. Educating the Patient About the Disorder and Treatment
- The nurse should educate the patient about the nature of BPD, its chronic course, emotional patterns, and the role of therapy and medications.
- It is essential to help the patient understand the importance of attending psychotherapy (like DBT) and maintaining consistency with prescribed medications.
- Teaching about warning signs of emotional crises and the use of safety plans can empower patients to manage their own condition.
🟩 6. Promoting Medication Compliance and Monitoring Side Effects
- The nurse must ensure that the patient is taking medications regularly as prescribed, especially antidepressants, mood stabilizers, or antipsychotics.
- The patient and family should be educated about expected benefits, side effects, and risks of abruptly stopping medications.
- The nurse should report any unusual changes in behavior, mood, or physiological responses to the psychiatrist for medication adjustment.
🟩 7. Supporting Social Skills and Interpersonal Functioning
- The nurse should facilitate group interaction sessions or role-playing to help the patient improve communication, trust, and emotional expression.
- Encourage positive relationships with peers and staff while discouraging unhealthy attachments or enmeshment.
- Teach the patient how to manage conflicts, express anger safely, and use “I” statements during disagreements.
8. Family Education and Involvement in Care
- The nurse should involve family members in therapy sessions to educate them about the patient’s condition, emotional instability, and triggers.
- Families should be taught to set consistent limits, avoid rescuing or enabling dysfunctional behavior, and provide emotional support without becoming overinvolved.
- The nurse should help families understand that empathy and structure must go hand in hand in managing a loved one with BPD.
9. Referral to Community Resources and Support Services
- The nurse should guide the patient to community mental health centers, crisis hotlines, DBT programs, and peer support groups for long-term help.
- Referral to vocational rehabilitation programs or occupational therapy may support reintegration into meaningful roles in society.
- The nurse may also connect the patient with non-governmental organizations (NGOs) or online support forums for continued motivation and support.
10. Maintaining Self-Awareness and Staff Support
- Nurses working with BPD patients should maintain strong professional boundaries and avoid personalizing the patient’s anger or praise.
- Due to emotional intensity and manipulative behavior, nurses may experience burnout, so regular team debriefings and emotional support are essential.
- Nurses should practice self-care and stress management techniques to sustain compassionate and effective caregiving.
b) Explain types of obsessive compulsive disorder. Discuss management of obsessive compulsive disorder (8 marks)
Obsessive-Compulsive Disorder is a chronic and long-lasting mental health disorder in which a person experiences unwanted, intrusive, and distressing thoughts (obsessions) and performs repetitive behaviors or mental acts (compulsions) to reduce the anxiety or fear related to these thoughts.
TYPES OF OBSESSIVE-COMPULSIVE DISORDER
OCD can manifest in various ways. Each type is based on the content of obsessions and the form of compulsions the individual experiences.
1️⃣ Contamination and Cleaning Type
- In this type, the person has an intense fear of germs, dirt, viruses, or harmful substances.
- It is one of the most common forms of OCD.
- Obsessions include thoughts like: “I touched something dirty, I might get sick.”
- Compulsions include excessive handwashing, cleaning surfaces, avoiding public places or touching people.
- This leads to excessive use of disinfectants and avoidance behavior that interferes with daily functioning.
2️⃣ Checking Type
- In this type, the person has persistent doubts that something bad will happen due to their carelessness or negligence.
- It includes obsessions like “Did I turn off the gas?”, “Did I lock the door?”, or “Will my family be harmed if I don’t check?”
- Compulsions include checking the stove, door locks, electrical appliances, emails, or body symptoms repeatedly.
- The checking behavior can take hours and cause significant delays or absenteeism.
3️⃣ Symmetry, Order, and Arranging Type
- This type involves a strong need for things to be aligned symmetrically or arranged in a certain order.
- Obsessions include thoughts that something terrible will happen if items are not placed “just right”.
- Compulsions include arranging items until they feel perfect, walking in certain patterns, or repeating words or numbers.
- It is commonly associated with magical thinking — a belief that arranging things a certain way will prevent harm.
4️⃣ Hoarding Type (Now classified as a related disorder in DSM-5)
- It involves difficulty in discarding or parting with possessions, even those with no value.
- Obsessions include thoughts like “What if I need this someday?”
- Compulsions include keeping useless items such as old newspapers, clothes, containers, etc.
- This results in cluttered living spaces and serious hygiene and safety issues.
5️⃣ Intrusive Thoughts Type (“Pure O” OCD)
- In this type, obsessions are purely mental and usually involve violent, sexual, or blasphemous themes.
- Examples include thoughts of harming others, shouting profanities in a temple, or engaging in immoral sexual acts.
- The compulsions are usually covert and include mental rituals like praying, counting, or avoiding certain thoughts.
- The person feels extreme guilt and shame but rarely acts on the thoughts.
6️⃣ Religious and Moral OCD (Scrupulosity)
- In this type, the person becomes obsessed with religious or moral perfection.
- Obsessions include fear of offending God, committing sin, or violating religious codes.
- Compulsions include repeated praying, confession, or avoiding spiritual practices due to fear of imperfection.
- This can lead to spiritual distress and social isolation.
7️⃣ Relationship OCD (ROCD)
- It is an emerging subtype in which the person constantly doubts the quality, compatibility, or value of their romantic relationship.
- Obsessions include “Do I really love my partner?” or “Is my partner right for me?”
- Compulsions include repeated questioning, checking feelings, comparing with others, or seeking reassurance from friends or partner.
- It creates emotional strain on relationships and can result in breakups due to unrealistic expectations.
MANAGEMENT OF OBSESSIVE-COMPULSIVE DISORDER
Management of OCD is multimodal, involving psychological therapy, medication, nursing care, and family involvement.
PSYCHOLOGICAL MANAGEMENT
✅ a) Cognitive Behavioral Therapy (CBT)
- CBT is the first-line treatment for OCD, especially effective in mild to moderate cases.
- It helps the patient identify irrational thoughts and learn healthier thought patterns.
- CBT corrects distorted beliefs and reduces fear attached to obsessions.
✅ b) Exposure and Response Prevention (ERP)
- ERP is a specialized CBT method where patients are gradually exposed to feared objects or thoughts without allowing them to perform compulsions.
- It helps reduce anxiety over time by breaking the obsession-compulsion cycle.
- Example: Making a patient touch a doorknob and preventing them from washing hands.
✅ c) Mindfulness and Acceptance Therapy
- It focuses on observing thoughts without judgment.
- It encourages acceptance of intrusive thoughts instead of fighting or suppressing them.
✅ d) Psychoeducation
- It involves educating the patient and family about OCD symptoms, treatment plan, and recovery path.
- It builds insight and cooperation from the client.
2. PHARMACOLOGICAL MANAGEMENT
✅ a) Selective Serotonin Reuptake Inhibitors (SSRIs)
- They are the first choice medications for OCD.
- Common SSRIs used: Fluoxetine, Sertraline, Fluvoxamine, Paroxetine.
- They help by increasing serotonin levels in the brain, thus reducing obsessions and compulsions.
- Therapeutic effect may take 8–12 weeks to appear.
✅ b) Tricyclic Antidepressants (TCA)
- Clomipramine is a potent TCA used for severe or resistant OCD.
- It blocks serotonin and norepinephrine reuptake, improving mood and reducing compulsive urges.
- It requires careful monitoring due to cardiac and anticholinergic side effects.
✅ c) Antipsychotic Augmentation
- Used in treatment-resistant OCD, especially when SSRIs alone are not effective.
- Common drugs: Risperidone, Aripiprazole, Quetiapine.
- They help by modulating dopamine, which is also involved in OCD pathophysiology.
NURSING MANAGEMENT
✅ 1. Assessment and Monitoring
- It is important to conduct initial and ongoing mental status examinations to assess the severity of obsessions and compulsions.
- It is essential to monitor the patient’s behavior pattern, duration of compulsions, and their impact on daily life.
- It is necessary to assess for comorbid conditions such as anxiety, depression, or suicidal ideation.
✅ 2. Therapeutic Communication and Trust Building
- It is essential to build a therapeutic and non-judgmental relationship to promote open discussion of distressing thoughts.
- It is vital to acknowledge the patient’s fears as real without reinforcing the rituals.
- It is necessary to provide emotional support during episodes of anxiety or compulsive urges.
✅ 3. Promoting Medication Adherence
- It is important to educate the patient about the role of medication, side effects, and the need for regular intake.
- It is essential to monitor for side effects of SSRIs and tricyclic antidepressants.
- It is helpful to maintain a medication chart or diary to ensure compliance.
✅ 4. Behavioral Support and Participation in Therapy
- It is necessary to encourage participation in Exposure and Response Prevention (ERP) sessions under professional guidance.
- It is important to reinforce non-compulsive behavior and praise small efforts in therapy.
- It is essential to gradually reduce the patient’s dependency on rituals through behavioral modification.
✅ 5. Family Involvement and Psychoeducation
- It is essential to involve family in therapy sessions to understand the disorder and avoid enabling behaviors.
- It is necessary to educate family members not to participate or assist in compulsions.
- It is important to guide family to provide structured routines and reduce stress at home.
✅ 6. Environment Modification and Safety Measures
- It is necessary to maintain a calm, structured, and low-stimulation environment to reduce anxiety.
- It is essential to remove triggers or stressors that may provoke obsessive thoughts.
- It is important to ensure patient safety, especially if the person has intrusive thoughts of self-harm or harming others.
✅ 7. Teaching Relaxation and Coping Skills
- It is essential to teach stress management techniques like deep breathing, yoga, or progressive muscle relaxation.
- It is helpful to introduce distraction strategies like journaling, art, or physical activities to reduce compulsive behavior.
- It is important to encourage mindfulness and grounding techniques for handling obsessive thoughts.
✅ 8. Providing Structure to Daily Routine
- It is vital to help the patient develop a consistent schedule to minimize unstructured time which may increase compulsions.
- It is necessary to assist in planning meaningful activities that promote self-esteem and independence.
- It is important to reinforce time limits for rituals to gradually reduce their duration.
✅ 9. Promoting Insight and Self-Awareness
- It is essential to encourage the patient to recognize the irrational nature of their obsessions over time.
- It is helpful to use cognitive worksheets or diaries to help track triggers, thoughts, and responses.
- It is important to motivate the patient to express feelings of fear, guilt, or shame associated with their compulsions.
✅ 10. Referral and Collaboration with Mental Health Team
- It is necessary to refer the patient to a psychiatrist or clinical psychologist for specialized cognitive therapies.
- It is essential to collaborate with social workers or case managers for long-term support and community resources.
- It is helpful to assist in follow-up planning and link with support groups for OCD patients.