09/08/2017-PHARMA,PATHO,GENETICS-JUHI DONE-PAPER NO.6
PHARMA,PATHO,GENETICS-PAPER SOLUTION NO.6
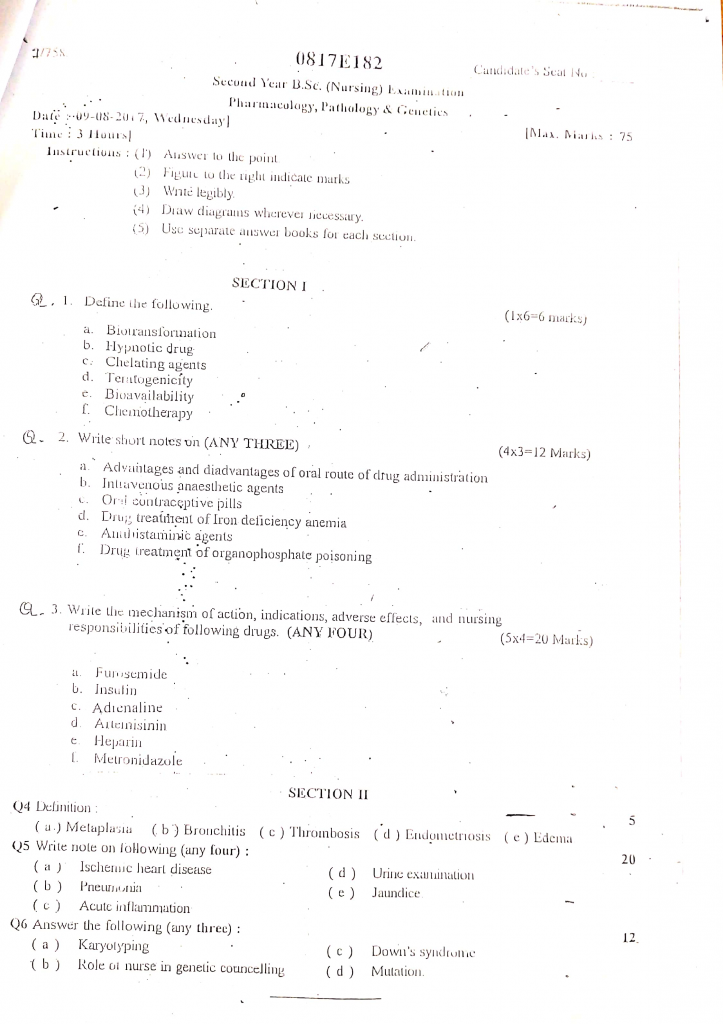
Section 1
Q.1 Define following (1×6=6 mark)
a. Biotransformation
- Biotransformation is the biochemical process by which the body chemically modifies drugs or foreign substances (xenobiotics), mainly in the liver, into more water-soluble and excretable forms through enzymatic reactions, primarily involving cytochrome P450 enzymes.
- It is also known as drug metabolism and usually occurs in two phases—Phase I (functionalization) and Phase II (conjugation).
b. Hypnotic drug
- Hypnotic drugs are medications that are primarily used to induce, maintain, or enhance sleep by depressing the central nervous system (CNS) activity.
- These drugs are commonly prescribed for short-term treatment of insomnia and other sleep disorders. They are also known as sleeping pills or sedative-hypnotics.
c. Chelating agent
- A chelating agent is a chemical substance that binds tightly with metal ions (like lead, mercury, iron) in the body to form a stable, non-toxic complex, which is then excreted through urine or feces.
- These agents are mainly used to treat heavy metal poisoning by removing toxic metals from the bloodstream.
d. Teratogenicity
- Teratogenicity is the ability of a substance, drug, or environmental factor to cause developmental abnormalities or congenital malformations in a developing fetus during pregnancy.
- Teratogens interfere with normal embryonic or fetal development, especially during the first trimester, which is the most critical period for organ formation (organogenesis).
e. Bioavailability
- Bioavailability is the proportion or percentage of an administered drug dose that reaches the systemic circulation in its active form and is available to produce a therapeutic effect.
- It is a key pharmacokinetic parameter that helps determine the onset, intensity, and duration of a drug’s action.
f. Chemotherapy
- Chemotherapy is the treatment of diseases, particularly cancer, using chemical substances or cytotoxic drugs that destroy or inhibit the growth and reproduction of cancerous cells.
- It works by targeting rapidly dividing cells, including both malignant and some healthy cells (like hair follicles and bone marrow), which often leads to side effects.
Q.2 Write short notes on (any three) (4×3=12 marks)
a. Advantages and disadvantages of oral route of drug administration
Advantages of Oral Route
Convenient and simple for the patient
➤ Oral administration is easy to perform without requiring special skills, training, or instruments. This enhances patient compliance and independence, especially in long-term treatments.
Non-invasive and painless
➤ Since it does not involve needles, there’s no pain, risk of bleeding, or infection. It avoids complications associated with parenteral routes (e.g., abscess, phlebitis).
Economical and cost-effective
➤ Oral drugs are cheaper to produce and purchase. It also eliminates the need for hospital visits or specialized administration, thus reducing healthcare costs.
Safe for long-term use
➤ Most chronic diseases like diabetes, hypertension, and asthma are managed with oral drugs that can be taken at home without supervision.
Wide variety of dosage forms available
➤ Tablets, capsules, liquids, suspensions, powders, lozenges, and chewable forms provide flexibility in formulation and patient preference.
Flexible dosing schedule
➤ Drugs can be formulated as sustained-release, extended-release, or enteric-coated tablets to ensure controlled and prolonged drug action.
Easy to store, transport, and handle
➤ Most oral medications have good shelf life, are stable at room temperature, and are easy to package and carry.
Psychologically acceptable
➤ Patients often feel more comfortable and in control when taking oral medication, as it does not involve invasive procedures.
Disadvantages of Oral Route
Slower onset of action
➤ Oral drugs must be digested and absorbed through the GI tract, which delays therapeutic effect, making it unsuitable for emergencies such as myocardial infarction or status epilepticus.
Not suitable for unconscious or vomiting patients
➤ Oral administration cannot be used if the patient is unconscious, delirious, unable to swallow, or experiencing persistent vomiting, which may lead to aspiration.
First-pass metabolism reduces efficacy
➤ Many drugs undergo significant hepatic metabolism (first-pass effect) before entering systemic circulation (e.g., propranolol, nitroglycerin), leading to reduced bioavailability.
Variable and unpredictable absorption
➤ Absorption can be influenced by presence of food, GI pH, motility, intestinal flora, drug interactions, and disease conditions (e.g., diarrhea or malabsorption syndromes).
Irritation to gastrointestinal mucosa
➤ Certain drugs like aspirin or iron supplements can irritate the gastric lining, causing ulcers, gastritis, or nausea.
Some drugs are destroyed by digestive enzymes or gastric acid
➤ Proteins like insulin and some peptides are degraded in the GI tract, making them ineffective orally.
Unpleasant taste or odor
➤ Drugs with bitter taste (e.g., metronidazole) may cause poor adherence, especially in children or elderly patients, unless taste-masked.
Risk of choking in certain populations
➤ Elderly, pediatric, or dysphagic (swallowing difficulty) patients may be at risk of choking with large tablets or capsules.
Drug interactions are more common
➤ Oral drugs may interact with food (e.g., calcium with tetracycline), other medications, antacids, or milk, altering the therapeutic effect.
b. Intravenous anestheic agents
Intravenous Anesthetic Agents
Definition
Intravenous anesthetic agents are the drugs that are administered directly into the bloodstream via IV route to produce rapid onset of anesthesia or sedation for short-term surgical or diagnostic procedures.
Classification of IV Anesthetic Agents
1. Barbiturates
- It includes agents like Thiopental sodium and Methohexital, which act as ultra-short-acting anesthetics.
- It is commonly used for the induction phase of general anesthesia due to its rapid onset (within 30 seconds).
2. Non-barbiturates
- This class includes Etomidate and Propofol.
- These are used for induction as well as maintenance of anesthesia.
3. Dissociative Anesthetics
- Ketamine is a commonly used dissociative agent.
- It causes analgesia, amnesia, and cataleptic state, with preservation of airway reflexes.
4. Benzodiazepines
- Includes Midazolam, Diazepam, and Lorazepam.
- These are used for pre-medication, sedation, and induction in minor procedures.
Mechanism of Action (MOA)
1. Barbiturates (e.g., Thiopental)
- It acts on the GABA-A receptor complex, increasing the duration of chloride channel opening, leading to CNS depression and unconsciousness.
2. Propofol
- It enhances GABAergic neurotransmission, leading to hypnotic effect and smooth induction of anesthesia without significant analgesia.
3. Ketamine
- It acts as an NMDA receptor antagonist, blocking excitatory neurotransmission.
- It causes a trance-like state with profound analgesia and amnesia.
4. Etomidate
- It also enhances GABA-A activity, providing hypnotic effects with minimal cardiovascular depression.
5. Benzodiazepines (e.g., Midazolam)
- It enhances GABA-A receptor activity, increasing the frequency of chloride channel opening, producing sedation, anxiolysis, and amnesia.
Indications of IV Anesthetic Agents
- It is used for induction of general anesthesia.
- It is useful in short diagnostic or therapeutic procedures (e.g., endoscopy, cardioversion).
- It is administered during minor surgeries requiring sedation without general anesthesia.
- It is often used for rapid sequence intubation (RSI) in emergency settings.
- It is used in ICU sedation for mechanically ventilated patients.
Adverse Effects of IV Anesthetics
- Hypotension and cardiovascular depression (esp. with Propofol and Thiopental).
- Respiratory depression or apnea, especially during rapid administration.
- Adrenal suppression (especially with Etomidate).
- Delirium or hallucinations on recovery from Ketamine.
- Injection site pain (commonly seen with Propofol).
- Laryngospasm or bronchospasm in hypersensitive individuals.
Contraindications
- Known allergy to the agent (e.g., egg allergy with Propofol).
- Porphyria (contraindicated with Barbiturates).
- Uncontrolled hypertension (Ketamine raises BP).
- Raised intracranial pressure (Propofol preferred over Ketamine).
- Severe cardiac conditions (use with caution due to cardiovascular depression).
Nursing Responsibilities
1. Pre-procedural Preparation
- It is the nurse’s responsibility to ensure that informed consent is taken from the patient or guardian, and that the patient is mentally and physically prepared for the anesthesia procedure.
- The nurse must verify that the patient has followed NPO guidelines for 6–8 hours and assess for history of allergies, past anesthetic complications, or existing systemic illnesses such as asthma, epilepsy, or cardiac conditions.
- It is essential for the nurse to arrange all pre-anesthetic checklists, label the drugs clearly, and set up emergency equipment like oxygen cylinders, suction apparatus, and crash carts at the bedside before administering any IV anesthetic.
2. Drug Administration and Monitoring
- The nurse should assist the anesthetist by setting up the IV line properly, checking the patency of the vein, and ensuring correct identification and dosage of the anesthetic drug prior to administration.
- During drug administration, the nurse must observe for any immediate local reactions such as pain, swelling, or redness at the injection site, and report any signs of extravasation or infiltration promptly.
- It is the duty of the nurse to document the exact drug name, dose, time, and route of administration clearly in the patient’s clinical record, along with the initial response of the patient.
3. Continuous Monitoring of Vital Functions
- The nurse must closely monitor and record the patient’s blood pressure, pulse rate, respiratory rate, and oxygen saturation every 5–15 minutes during and after the anesthesia to detect any abnormal changes.
- It is essential that the nurse remains vigilant for signs of respiratory depression, bradycardia, hypotension, or arrhythmias, and initiates emergency support as needed.
- The nurse should regularly assess the patient’s level of consciousness, muscle tone, and pupil size to determine the depth and effect of anesthesia and prevent overdose or underdose.
4. Emergency Preparedness and Response
- It is the nurse’s duty to ensure that all emergency resuscitation drugs like Flumazenil, Atropine, Epinephrine, and Naloxone are available, correctly labeled, and within expiry date.
- The nurse must be trained to initiate Basic Life Support (BLS) or assist in Advanced Cardiac Life Support (ACLS) if the patient shows signs of collapse or arrest during anesthetic use.
- The nurse must check that emergency devices like defibrillators, laryngoscopes, endotracheal tubes, and bag-mask ventilators are available and functional at the patient’s bedside before anesthesia begins.
5. Post-Anesthesia Recovery and Documentation
- After the procedure, the nurse should continuously monitor the patient for return of protective airway reflexes, consciousness, and stable vital signs, and provide oxygen if necessary.
- The nurse must observe and manage post-anesthetic side effects like nausea, vomiting, restlessness, shivering, or hallucinations, particularly when drugs like Ketamine are used.
- The nurse should complete accurate documentation of the anesthesia period, including all monitoring data, complications, patient outcomes, and nursing interventions during the recovery phase.
c. Oral contraceptive pills
Definition
- Oral contraceptive pills (OCPs) are hormonal medications taken orally by women to prevent pregnancy.
- These pills contain synthetic forms of estrogen and/or progesterone, which work by inhibiting ovulation and altering the uterine environment.
- They are among the most effective, reversible, and convenient methods of contraception when taken correctly.
Types of Oral Contraceptive Pills
A. Combined Oral Contraceptive Pills (COCs)
- Contain both estrogen (usually ethinylestradiol) and progestin (like levonorgestrel).
- Taken for 21 days continuously followed by 7 days break or placebo pills.
- Most commonly used and highly effective if taken regularly.
- Examples : Mala-D, Mala-N (India), Ovral, Yasmin.
B. Progestin-Only Pills (POPs) (Mini Pills)
- Contain only progestin, no estrogen.
- Preferred in lactating women or those with contraindications to estrogen.
- Pills must be taken at the same time daily without break.
- Examples: Cerazette, Micronor.
C. Emergency Contraceptive Pills (ECPs)
- High-dose progestin taken within 72 hours of unprotected sex to prevent pregnancy.
- Examples: Levonorgestrel (iPill), Ulipristal acetate (EllaOne).
Mechanism of Action of OCPs
- Inhibition of ovulation: The hormones suppress release of FSH and LH, preventing the ovary from releasing an egg.
- Thickening of cervical mucus: Progestin makes the mucus thick and sticky, preventing sperm entry.
- Alteration of endometrial lining: The uterine lining becomes unfavorable for implantation of a fertilized egg.
- Decreased tubal motility: Reduces the movement of egg and sperm within the fallopian tubes.
Advantages / Benefits of OCPs
- Highly effective (99% with perfect use) when taken regularly.
- Provides reversible contraception – fertility returns soon after discontinuation.
- Regulates menstrual cycle, reduces dysmenorrhea and menorrhagia.
- Offers protection against ovarian and endometrial cancer.
- Decreases incidence of ectopic pregnancy, PID, and benign breast disease.
- Improves acne and premenstrual symptoms in some users.
Side Effects / Adverse Effects
- Nausea, vomiting, headache
- Breast tenderness and weight gain
- Mood changes and breakthrough bleeding
- Mild hypertension and edema
- Rare but serious: Venous thromboembolism, stroke, myocardial infarction, especially in smokers over 35 years
Contraindications of OCPs
Absolute Contraindications :
- History of thromboembolic disease or stroke
- Liver disease or liver tumors
- Breast cancer or estrogen-sensitive cancers
- Undiagnosed vaginal bleeding
- Pregnancy
Relative Contraindications :
- Migraine with aura
- Smokers above 35 years
- Uncontrolled hypertension or diabetes
- Gallbladder disease
Nursing Responsibilities in OCP Use
A. Patient Assessment and Counseling
- The nurse must assess the patient’s medical and menstrual history before recommending or administering OCPs.
- The nurse should screen for contraindications like thrombosis, hypertension, or liver disease.
- Provide detailed counseling about how to use OCPs, their effectiveness, side effects, and what to do if a dose is missed.
B. Monitoring and Education
- Instruct the patient to take the pill daily at the same time, and never miss a dose.
- Teach the patient to use backup contraception (e.g., condoms) if pills are missed or if taking antibiotics.
- Advise regular BP monitoring, weight check, and review visits every 3–6 months.
C. Emergency Preparedness and Follow-Up
- Inform about warning signs: ACHES – Abdominal pain, Chest pain, Headache, Eye problems, Severe leg pain (may indicate clot).
- Ensure the patient has access to follow-up care in case of side effects or complications.
- Promote compliance and support, especially among adolescents and new users.
d. Drug treatment of iron deficiency anemia
Oral Iron Therapy (First Line Treatment)
- It is the most affordable and effective mode of treatment for correcting iron deficiency anemia in mild to moderate cases.
- Common preparations include Ferrous Sulfate (20% elemental iron), Ferrous Gluconate (12%), and Ferrous Fumarate (33%), usually taken once or twice daily.
- It is absorbed mainly in the duodenum and upper jejunum, and requires an acidic environment for optimal absorption.
- The nurse should advise patients to avoid taking iron with milk, tea, antacids, or calcium supplements, as these can reduce iron absorption.
- Long-term oral therapy (up to 3–6 months) is needed even after hemoglobin normalizes to replenish iron stores in bone marrow and liver.
Parenteral Iron Therapy (Intramuscular or Intravenous)
- It is indicated for patients with severe anemia, inflammatory bowel disease, gastric bypass, or when oral therapy fails.
- Ferric Carboxymaltose is a newer IV preparation with the advantage of larger single-dose infusion (up to 1000 mg), reducing number of hospital visits.
- Intramuscular iron should be injected deep into gluteal muscle using a long needle and Z-track technique to minimize skin staining.
- It is essential to calculate the total iron requirement using standard formulas based on hemoglobin deficit and body weight before starting therapy.
- Nurses must observe for signs of hypersensitivity reactions, hypotension, or bronchospasm, especially with Iron Dextran, which may require test dosing.
Blood Transfusion (In Severe Anemia)
- It is used only in emergency situations to rapidly increase oxygen-carrying capacity, such as in pregnancy with Hb < 7 g/dL, congestive heart failure, or shock.
- Each unit of packed red blood cells (PRBCs) increases hemoglobin by about 1 g/dL and hematocrit by 3%.
- Blood transfusion must be administered slowly and with close vital sign monitoring, to avoid volume overload or transfusion reactions.
- It should always be followed by definitive iron therapy to restore iron stores, as transfusion only provides temporary correction.
- Informed consent, cross-matching, and screening for infections (HIV, HBV, HCV) are mandatory before transfusion.
Erythropoiesis-Stimulating Agents (ESAs)
- They act by stimulating bone marrow to increase red blood cell production, especially beneficial in anemia of chronic disease or renal failure.
- These drugs are ineffective without adequate iron, so they must be given in combination with IV iron or oral iron supplementation.
- Side effects may include hypertension, headache, flu-like symptoms, and thromboembolic events, so patients must be monitored regularly.
- Doses are adjusted according to baseline hemoglobin levels, and the goal is to maintain Hb between 10–11.5 g/dL to avoid complications.
- ESAs should be used cautiously in patients with cancer, as they may promote tumor progression if not carefully monitored.
e. Antihistaminic agent
Definition
- Antihistamines are defined as drugs that block or reduce the effects of histamine at histamine receptors in the body, thereby alleviating allergic and inflammatory symptoms.
- These agents are primarily used in the treatment of allergies, urticaria, rhinitis, and anaphylactic reactions.
Types / Classification
Antihistamines are classified based on the type of histamine receptor they block:
✅ A. H1 Receptor Antagonists (Used in allergy and respiratory conditions)
First Generation H1 Antihistamines :
- It crosses the blood-brain barrier and causes sedation.
- Examples include diphenhydramine, chlorpheniramine, hydroxyzine, promethazine.
Second Generation H1 Antihistamines :
- It is non-sedating or less sedating due to poor penetration into the brain.
- Examples include loratadine, cetirizine, levocetirizine, fexofenadine.
✅ B. H2 Receptor Antagonists (Used in acid-peptic disorders)
- It blocks H2 receptors in the stomach lining, reducing gastric acid secretion.
- Examples include ranitidine (now banned in many countries), famotidine, cimetidine.
Mechanism of Action (H1 Antihistamines)
- It works by competitively binding to H1 histamine receptors on effector cells in the respiratory tract, skin, and blood vessels.
- It prevents histamine from binding to its receptor, thereby reducing capillary dilation, itching, bronchoconstriction, and mucus secretion.
- First-generation drugs also cross the blood-brain barrier and block histaminergic signals in the CNS, producing sedation and anti-nausea effects.
- Second-generation drugs selectively bind to peripheral H1 receptors and are long-acting with minimal drowsiness.
Indications / Therapeutic Uses
- It is used in the treatment of allergic rhinitis (hay fever), urticaria (hives), conjunctivitis, and eczema.
- It is beneficial in managing anaphylaxis (as an adjunct to epinephrine).
- It is given for motion sickness, vertigo, and nausea/vomiting (e.g., promethazine).
- It is prescribed in common cold and flu to relieve sneezing and rhinorrhea.
- It is also used in insect bite allergies and food/drug allergic reactions.
- H2 blockers are used in peptic ulcers, GERD, and Zollinger-Ellison syndrome.
Adverse Effects (Side Effects)
First-Generation H1 Antihistamines :
- It causes sedation, drowsiness, dizziness, dry mouth, blurred vision, and constipation.
- It may also cause urinary retention and confusion in elderly patients.
Second-Generation H1 Antihistamines :
- It may cause headache, fatigue, dry mouth, and nausea but generally well-tolerated.
H2 Blockers
- It may cause diarrhea, headache, dizziness, gynecomastia (rare with cimetidine).
Contraindications
- t is contraindicated in patients with known hypersensitivity to antihistamines.
- It should be used with caution in patients with glaucoma, prostate hypertrophy, peptic ulcer, or seizure disorders.
- First-generation antihistamines are contraindicated in elderly patients due to CNS depression.
7. Nursing Responsibilities
Assessment and Monitoring
- It is the nurse’s responsibility to assess for signs of allergic reaction, airway patency, skin rashes, and itching before administering the drug.
- It is necessary to monitor for side effects such as sedation, dizziness, or hypotension, especially in elderly patients.
Safety and Sedation Precautions
- It is important to advise patients on first-generation antihistamines to avoid driving or operating heavy machinery due to drowsiness.
Hydration and Comfort
- It is essential to encourage increased fluid intake to reduce dryness of mouth and throat.
- It is helpful to offer sugar-free candy or ice chips to manage dry mouth.
Education
- It is the nurse’s duty to educate patients to avoid alcohol and CNS depressants while on antihistamines.
- It is advised to inform patients to take second-generation antihistamines during the day due to their non-sedating property.
Documentation and Reporting
- It is important to document time of administration, effectiveness, and any side effects, and report adverse reactions immediately.
f. Drug treatment of organophosphate poisioning
1. Atropine (Anticholinergic Agent)
- It is the primary drug used in the management of organophosphate poisoning, as it antagonizes muscarinic effects of excess acetylcholine.
- It works by blocking acetylcholine at muscarinic receptors, thus reducing bronchorrhea, bradycardia, hypotension, and salivation.
- The initial adult dose is usually 1.8–3 mg IV, repeated every 5–10 minutes until signs of atropinization appear (i.e., dry mouth, dilated pupils, and increased heart rate).
- Large and repeated doses may be needed due to continued release of acetylcholine.
- It does not reverse neuromuscular symptoms (i.e., muscle weakness or paralysis) caused by nicotinic stimulation.
2. Pralidoxime (Oxime Therapy or Cholinesterase Reactivator)
- Pralidoxime (also called 2-PAM) is given to reactivate cholinesterase enzymes that have been inactivated by organophosphates.
- It works by cleaving the bond between the organophosphate and acetylcholinesterase, particularly effective if given within the first 24–48 hours of poisoning.
- It helps reverse both muscarinic and nicotinic effects, especially muscle weakness and respiratory depression.
- Usual adult dose is 1–2 g IV infused over 15–30 minutes, may be repeated every 4–6 hours, or given as a continuous infusion.
- It is ineffective once “aging” of the enzyme has occurred (irreversible binding), so early administration is crucial.
3. Benzodiazepines (e.g., Diazepam or Lorazepam)
- It is used to control seizures or convulsions that may occur due to excessive CNS stimulation.
- Diazepam also has neuroprotective effects, and is sometimes used prophylactically in moderate-to-severe cases.
- It may be given IV or rectally, depending on the condition of the patient and available access.
4. Supportive and Symptomatic Medications
- Oxygen therapy may be administered in cases of respiratory distress or hypoxia.
- Bronchodilators (e.g., salbutamol) may be used if there is bronchospasm.
- IV fluids may be given to manage hypotension and support circulation.
- Anti-emetics may be needed if the patient has nausea or vomiting.
5. Activated Charcoal (if within 1 hour of ingestion)
- If the patient presents within 60 minutes of ingestion and is conscious or has a protected airway, activated charcoal may be given to limit further absorption.
- Usual dose is 1 g/kg orally or via nasogastric tube.
Q.3 Write the mechanism of action, indication, adverse effects and nursing responsibilies of following drugs (any four) (5×4=20 mark)
a. Frusemide
Mechanism of Action of Lasix (Furosemide)
- It is a potent loop diuretic that works primarily in the ascending limb of the loop of Henle in the nephron of the kidney.
- It inhibits the sodium-potassium-chloride (Na⁺/K⁺/2Cl⁻) co-transporter, which blocks the reabsorption of sodium and chloride ions.
- This action leads to increased excretion of sodium, chloride, potassium, calcium, and water, causing a powerful diuretic (urine-producing) effect.
- It results in a rapid decrease in blood volume and preload, which helps in reducing blood pressure and relieving pulmonary congestion or edema.
- It causes vasodilation of the blood vessels in the kidneys even before diuresis begins, helping to improve renal blood flow.
Indications of Lasix (Furosemide)
- Congestive Heart Failure (CHF) with pulmonary edema
- Acute and chronic renal failure
- Liver cirrhosis with ascites
- Hypertension (especially in patients with fluid overload)
- Hypercalcemia
- Pulmonary edema (emergency use)
- Nephrotic syndrome
- Cerebral edema (with other supportive care)
Adverse Effects of Lasix (Furosemide)
- Hypokalemia (low potassium levels)
- Hyponatremia (low sodium levels)
- Dehydration and hypotension
- Dizziness, headache
- Muscle cramps and weakness
- Ototoxicity (hearing loss at high doses or rapid IV push)
- Hyperuricemia and gout attacks
- Metabolic alkalosis
Contraindications of Lasix (Furosemide)
- Hypersensitivity to furosemide or sulfa drugs
- Anuria (absence of urine production)
- Severe electrolyte imbalance (especially low potassium/sodium)
- Hepatic coma or severe liver disease (relative contraindication)
- Pregnancy and lactation (use with caution)
- Dehydrated or hypotensive patients
Nursing Responsibilities While Administering Lasix (Furosemide)
1️⃣ Pre-administration Assessment
- The nurse must assess baseline blood pressure, pulse rate, respiratory status, and oxygen saturation before giving the drug.
- It is necessary to review serum electrolytes (Na⁺, K⁺, Cl⁻, Ca²⁺) and renal function tests (BUN, creatinine).
2️⃣ During Administration
- The nurse must administer IV doses slowly (e.g., 20 mg/min) to avoid ototoxicity.
- Oral Lasix should be given in the morning to prevent nocturia (urination at night).
- The nurse should ensure that the patient has easy access to a bathroom due to increased urine output.
3️⃣ Monitoring
- It is important to monitor daily weight, intake/output, and signs of fluid volume deficit.
- The nurse should watch for symptoms of hypokalemia such as muscle weakness, fatigue, or ECG changes.
- Vital signs must be monitored for signs of orthostatic hypotension or sudden drop in BP.
4️⃣ Patient Education
- The nurse must teach the patient to take the drug in the morning and avoid taking it late in the day.
- The nurse should advise the patient to report signs of dizziness, irregular heartbeat, muscle cramps, or tinnitus.
- It is important to advise potassium-rich diet or supplements (e.g., banana, orange juice), unless contraindicated.
5️⃣ Lab Follow-up
- The nurse must follow-up with regular blood tests to monitor electrolytes and kidney function.
- Urinalysis and blood pressure readings should be documented and evaluated regularly.
b. Insulin
Mechanism of Action of Insulin
- Insulin is a naturally occurring hormone produced by the beta cells of the pancreas (Islets of Langerhans), essential for glucose metabolism and energy utilization.
- It acts by binding to insulin receptors on the surface of target cells (like muscle, fat, and liver), which triggers cellular uptake of glucose from the bloodstream.
- In the liver, insulin promotes glycogen synthesis and inhibits gluconeogenesis, helping to store excess glucose and reduce blood sugar levels.
- In muscle and adipose tissue, it enhances glucose uptake, protein synthesis, and fat storage, helping maintain energy balance.
- Insulin also prevents the breakdown of fats and proteins by inhibiting lipolysis and proteolysis, preserving body tissues.
- Exogenous (injected) insulin mimics natural insulin and is used to control hyperglycemia in diabetes mellitus, especially in Type 1 and insulin-dependent Type 2 diabetes.
Indications of Insulin
- Type 1 Diabetes Mellitus
- Type 2 Diabetes Mellitus (when oral hypoglycemics are ineffective)
- Diabetic ketoacidosis (DKA)
- Hyperosmolar hyperglycemic state (HHS)
- Gestational diabetes
- Hyperkalemia (short-term emergency use)
- Perioperative or critical care glycemic control
Adverse Effects of Insulin
- Hypoglycemia (most common; signs include sweating, shakiness, confusion)
- Weight gain
- Lipodystrophy at injection site (lipoatrophy or lipohypertrophy)
- Allergic reaction (rare)
- Hypokalemia (due to shift of potassium into cells)
- Injection site pain or redness
- Insulin resistance (long-term use)
Contraindications of Insulin
- Hypoglycemia (do not administer if blood sugar is already low)
- Hypersensitivity to insulin or formulation components
- Caution in renal or hepatic impairment
- Avoid abrupt discontinuation (risk of DKA)
- Use with caution in patients with adrenal or pituitary disorders
Nursing Responsibilities While Administering Insulin
1️⃣ Assessment Before Administration
- The nurse must check the patient’s blood glucose level using a glucometer before administering insulin, and ensure it is within the appropriate range for injection.
- It is essential to verify the correct type, dosage, and timing of insulin as prescribed, because using the wrong type can cause serious hypo- or hyperglycemia.
2️⃣ Proper Preparation and Technique
- The nurse should ensure insulin is drawn into the syringe correctly, avoiding air bubbles, and if mixing insulins, clear insulin (short-acting) should be drawn before cloudy (intermediate-acting) to avoid contamination.
- It is important to rotate injection sites (abdomen, thighs, arms) to prevent lipodystrophy and ensure proper absorption.
3️⃣ Monitoring and Hypoglycemia Management
- The nurse must closely monitor for signs and symptoms of hypoglycemia (e.g., sweating, confusion, irritability, tremors), especially in patients who are NPO or after exercise.
- In case of hypoglycemia, the nurse should immediately administer fast-acting carbohydrates orally, or IV glucose/glucagon if the patient is unconscious.
4️⃣ Patient Education
- The nurse must teach the patient to self-monitor blood glucose regularly, recognize signs of hypoglycemia and hyperglycemia, and manage them appropriately.
- It is important to instruct the patient on correct storage of insulin, which should be refrigerated when unopened and used within a specified period once opened (usually 28 days at room temp).
5️⃣ Diet and Timing Coordination
- The nurse must ensure that meals are available shortly after administering rapid-acting insulin, as skipping meals can result in hypoglycemia.
- The nurse should also educate the patient to maintain a consistent diet and physical activity routine, and report any illness that could affect glucose control.
6️⃣ Double-checking and Documentation
- It is mandatory for the nurse to double-check insulin doses with another licensed nurse, especially for pediatric or critical care patients, and to document the dose, time, site, and blood glucose levels accurately.
7️⃣ Lab Monitoring and Long-term Care
- The nurse should coordinate with the physician for monitoring HbA1c levels, serum potassium, and renal function, especially in long-term insulin users.
c. Adrenaline
Mechanism of Action of Adrenaline
- Adrenaline is a potent non-selective adrenergic agonist that stimulates alpha (α1), beta-1 (β1), and beta-2 (β2) receptors throughout the body.
- By stimulating β1 receptors in the heart, it increases heart rate (positive chronotropic effect), enhances cardiac contractility (positive inotropic effect), and raises cardiac output and blood pressure.
- Through activation of β2 receptors in the lungs, it causes bronchodilation, making it highly effective in acute asthma and anaphylaxis.
- By stimulating α1 receptors in blood vessels, it causes vasoconstriction, which increases systemic vascular resistance and helps raise blood pressure in hypotensive states.
- It also inhibits the release of histamine and other inflammatory mediators during allergic reactions, making it the drug of choice in anaphylaxis.
- In emergency settings, adrenaline helps to restore spontaneous circulation during cardiac arrest by improving perfusion to vital organs.
Indications of Adrenaline
- Anaphylaxis (severe allergic reactions)
- Acute asthma attack (bronchospasm unresponsive to other drugs)
- Cardiac arrest (as part of Advanced Cardiac Life Support)
- Severe hypotension or shock (as a vasopressor)
- Local vasoconstriction (with local anesthetics to prolong action)
- Glaucoma (open-angle, rarely used now)
- Upper airway obstruction (epiglottitis, croup – racemic form)
Adverse Effects of Adrenaline
- Tachycardia and palpitations
- Hypertension
- Headache and dizziness
- Tremors and anxiety
- Arrhythmias or ventricular fibrillation
- Hyperglycemia (due to glycogenolysis)
- Tissue necrosis if extravasated during IV use
- Insomnia or restlessness (with repeated doses)
Contraindications of Adrenaline
- Hypersensitivity to epinephrine
- Uncontrolled hypertension
- Hyperthyroidism (relative contraindication)
- Narrow-angle glaucoma
- Severe cardiac disease (e.g., angina, arrhythmia – relative)
- Inhalational use in patients with closed-angle glaucoma
Nursing Responsibilities While Administering Adrenaline
1️⃣ Emergency Preparedness and Assessment
- The nurse must ensure emergency equipment (oxygen, suction, defibrillator) is readily available, especially when administering adrenaline during cardiac arrest or anaphylaxis.
- It is vital for the nurse to assess baseline vital signs, ECG, and respiratory status prior to administration to evaluate patient condition and anticipate adverse effects.
2️⃣ Correct Dose, Route, and Technique
- The nurse should strictly follow the prescribed route—IM for anaphylaxis, IV for cardiac arrest, SC for mild allergy, and inhalation for croup—because incorrect route may cause serious harm.
- It is crucial to check the correct concentration before administration (e.g., 1:1000 for IM; 1:10,000 for IV in cardiac arrest), as overdose may lead to fatal arrhythmias or severe hypertension.
3️⃣ Monitoring After Administration
- The nurse must closely monitor heart rate, blood pressure, oxygen saturation, and respiratory effort continuously during and after adrenaline administration.
- The nurse should be vigilant for early signs of toxicity, such as chest pain, severe hypertension, or arrhythmias, and take immediate action if such signs appear.
4️⃣ Injection Safety and Site Care
- For IM injection (e.g., EpiPen), the nurse must administer into the mid-anterolateral thigh, not into the buttock, and hold for 10 seconds to ensure full dose delivery.
- In IV use, the nurse must ensure patency of vein and avoid extravasation, as adrenaline leakage can cause local tissue necrosis.
5️⃣ Patient and Family Education
- The nurse must teach patients at risk for anaphylaxis how to use auto-injector (EpiPen), store it correctly, and carry it at all times.
- The nurse should instruct the patient to seek immediate medical help after adrenaline use, even if symptoms improve, as a biphasic allergic reaction may occur.
6️⃣ Documentation and Double-Check
- The nurse must document the exact time, dose, route, reason for administration, and patient’s response, especially in emergency cases for legal and medical accuracy.
- It is mandatory for the nurse to double-check the drug and dilution, especially during high-stress emergencies like resuscitation, to avoid life-threatening errors.
d. Artemisinin
Mechanism of Action of Artemisinin
- Artemisinin and its derivatives work by generating reactive free radicals inside Plasmodium-infected red blood cells when they interact with the heme iron released by hemoglobin digestion.
- These free radicals cause damage to essential proteins and membranes of the malaria parasite, ultimately leading to parasite death.
- Artemisinin is most active during the early ring stage and trophozoite stage of Plasmodium falciparum, making it highly effective in reducing parasite biomass rapidly.
- It has a fast onset of action but a short half-life, so it is often used in combination with longer-acting antimalarials (e.g., lumefantrine, mefloquine) in Artemisinin-based Combination Therapy (ACT) to prevent resistance.
- Artemisinin does not affect dormant liver stages (hypnozoites) of P. vivax or P. ovale, so primaquine is used along with it for radical cure.
Indications of Artemisinin
- Uncomplicated Plasmodium falciparum malaria
- Severe or complicated malaria (especially artesunate IV)
- Multidrug-resistant malaria
- Malaria in endemic areas where ACT is recommended
- Used in combination therapy (e.g., artemether-lumefantrine, artesunate-mefloquine)
Adverse Effects of Artemisinin
- Nausea and vomiting
- Dizziness and headache
- Anorexia or abdominal discomfort
- Mild rash or allergic reaction
- Transient elevation of liver enzymes
- Rare: neutropenia or hemolysis
- QT prolongation (especially with artemether-lumefantrine)
- Neurotoxicity in high or prolonged doses (animal studies)
Contraindications of Artemisinin
- Known hypersensitivity to artemisinin or its derivatives
- First trimester of pregnancy (relative; artesunate may still be used in severe malaria if benefits outweigh risks)
- Severe liver disease (use with caution)
- Patients with cardiac arrhythmia (if used with QT-prolonging agents)
- Not recommended for monotherapy (due to risk of resistance)
Nursing Responsibilities While Administering Artemisinin
1️⃣ Pre-treatment Assessment
- The nurse must assess the patient’s history of malaria, previous antimalarial drug use, liver function, and allergy status before initiating artemisinin treatment.
- It is essential to verify correct body weight to calculate the precise dose, especially in pediatric and underweight patients.
2️⃣ Correct Drug and Route Administration
- The nurse must ensure the correct artemisinin derivative is used based on severity of malaria—IV artesunate for severe cases and oral ACT for uncomplicated malaria.
- When preparing IV artesunate, the nurse should follow strict dilution and reconstitution instructions, and administer the drug over the correct time period to avoid local reaction or systemic shock.
3️⃣ Monitoring During Therapy
- The nurse should closely monitor the patient for signs of clinical improvement, such as reduced fever, improved consciousness, and increased urine output.
- It is necessary to observe for adverse effects such as nausea, dizziness, allergic reactions, or cardiac symptoms, especially in co-morbid or elderly patients.
4️⃣ Preventing Resistance and Educating the Patient
- The nurse must educate the patient to complete the full ACT course even if symptoms improve early, as premature stopping can lead to drug resistance.
- The nurse should also teach the patient to avoid re-infection by using mosquito nets, repellents, and avoiding exposure to mosquito breeding areas, especially during evenings and night.
5️⃣ Post-treatment Follow-up
- The nurse should schedule follow-up blood smears (thick and thin) to confirm parasite clearance, especially in areas with known resistance.
- It is also important to monitor liver enzymes and CBC during and after treatment in prolonged or repeated therapy cases.
6️⃣ Storage and Handling
- The nurse should store artemisinin derivatives in cool, dry conditions, and check expiration dates carefully, as these compounds degrade rapidly in heat and moisture.
7️⃣ Documentation and Reporting
- The nurse must document dose, time, patient response, adverse effects, and follow-up plans, and report any suspected treatment failure or resistance to local health authorities for epidemiological tracking.
e. Heparin
Mechanism of Action of Heparin
- Heparin is an indirect anticoagulant that works by activating antithrombin III, a natural inhibitor of several clotting factors.
- Once activated, antithrombin III inactivates thrombin (factor IIa) and factor Xa, thereby inhibiting the conversion of fibrinogen to fibrin, which is essential for clot formation.
- By preventing the formation of fibrin, heparin halts the progression of existing clots and prevents the formation of new thrombi but does not dissolve existing clots.
- Unfractionated Heparin (UFH) acts on both factor IIa and Xa, whereas LMWH acts more selectively on factor Xa.
- Heparin works rapidly when given intravenously, and its action is reversed with protamine sulfate, a heparin antidote.
Indications of Heparin
- Deep Vein Thrombosis (DVT) prevention and treatment
- Pulmonary Embolism (PE)
- Acute Coronary Syndrome (e.g., myocardial infarction)
- Atrial fibrillation with embolism risk
- During dialysis and open-heart surgery (to prevent clotting)
- Prevention of clotting in central venous lines
- Disseminated Intravascular Coagulation (DIC) (with caution)
Adverse Effects of Heparin
- Bleeding (internal or external)
- Heparin-Induced Thrombocytopenia (HIT)
- Osteoporosis (with long-term use)
- Skin rashes or injection site irritation
- Hyperkalemia (due to aldosterone suppression)
- Hypersensitivity reactions
- Bruising or hematoma at injection site
Contraindications of Heparin
- Active bleeding or hemorrhagic disorders
- Recent surgery or trauma (e.g., CNS, eye, spinal)
- Severe hypertension (uncontrolled)
- Heparin-induced thrombocytopenia (HIT) history
- Liver or kidney dysfunction (use with caution)
- Alcoholism or peptic ulcer disease
- Known hypersensitivity to heparin
Nursing Responsibilities While Administering Heparin
1️⃣ Assessment Before Administration
- The nurse must assess the patient’s baseline coagulation profile, including aPTT (activated partial thromboplastin time) for UFH and platelet count to detect risk of bleeding or thrombocytopenia.
- It is essential for the nurse to check for any history of bleeding disorders, recent surgery, or peptic ulcers, which increase bleeding risk.
2️⃣ Correct Dose and Route Handling
- The nurse should confirm the correct form, dose, and route (IV or SC) as ordered, because heparin is never given IM due to risk of hematoma.
- It is important to rotate subcutaneous injection sites (e.g., abdomen) and avoid rubbing the area post-injection to prevent bruising.
3️⃣ Monitoring During Therapy
- The nurse must monitor aPTT levels regularly (for UFH) and adjust the dosage according to protocol to maintain therapeutic range (typically 1.5 to 2.5 times control).
- The nurse should observe closely for any signs of bleeding, such as hematuria, melena, bleeding gums, or bruising, and report them promptly.
4️⃣ Antidote and Emergency Readiness
- The nurse should ensure protamine sulfate is readily available in case of heparin overdose or uncontrolled bleeding.
- It is important to have emergency equipment ready if the patient is receiving IV heparin during invasive procedures or high-risk situations.
5️⃣ Patient Education and Safety
- The nurse must educate the patient to report any signs of bleeding, avoid activities that may cause injury, and not take aspirin or NSAIDs unless prescribed.
- It is necessary to advise the patient not to massage injection sites, and to inform all healthcare providers of ongoing heparin therapy.
6️⃣ Documentation and Double-Check Protocol
- The nurse must double-check heparin doses and pump settings with another nurse, especially in IV continuous infusion, as errors can cause fatal bleeding.
- Accurate documentation of dose, time, site of administration, lab results, and patient response is essential for legal and safety reasons.
7️⃣ Lab Coordination and Communication
- The nurse should coordinate frequent lab tests (aPTT, platelet count) with the laboratory and communicate critical values to the physician promptly.
- In case of low platelet counts or abnormal aPTT values, the nurse must withhold the next dose and notify the doctor to avoid complications.
f. Metronidazole
Mechanism of Action of Metronidazole
- Metronidazole is a prodrug that becomes active only inside anaerobic organisms (bacteria or protozoa) where low oxygen tension exists.
- Inside the microorganism, it is reduced by electron transport proteins to form cytotoxic nitroso free radicals that disrupt DNA helical structure, leading to strand breakage and inhibition of nucleic acid synthesis.
- This DNA damage causes cell death of anaerobic bacteria and protozoa, making it a bactericidal and protozoacidal drug.
- It is highly effective against anaerobic bacteria (e.g., Bacteroides, Clostridium) and protozoa (e.g., Entamoeba histolytica, Giardia lamblia, Trichomonas vaginalis).
- Metronidazole is well absorbed orally, penetrates tissues effectively including the CNS, and is excreted in urine, making it suitable for deep tissue infections.
Indications of Metronidazole
- Amoebiasis (intestinal and hepatic)
- Giardiasis
- Trichomoniasis
- Anaerobic bacterial infections (e.g., pelvic, dental, brain abscess)
- Clostridium difficile colitis (pseudomembranous colitis)
- Bacterial vaginosis
- Surgical prophylaxis for colorectal or gynecological procedures
- H. pylori infection (in combination therapy)
Adverse Effects of Metronidazole
- Metallic or bitter taste in mouth
- Nausea, vomiting, abdominal cramps
- Headache or dizziness
- Dry mouth or dark-colored urine
- Peripheral neuropathy with prolonged use
- Seizures (rare, at high doses)
- Disulfiram-like reaction with alcohol (flushing, vomiting)
Contraindications of Metronidazole
- Hypersensitivity to metronidazole or nitroimidazoles
- First trimester of pregnancy (especially high-dose use)
- Chronic alcoholism (due to disulfiram-like reaction)
- History of seizures or CNS disease (relative contraindication)
- Severe hepatic impairment (use with caution)
Nursing Responsibilities While Administering Metronidazole
1️⃣ Assessment Before Administration
- The nurse must assess the patient’s history of drug allergy, alcohol use, pregnancy status, and neurological symptoms before starting metronidazole therapy.
- It is essential to review baseline liver function tests (LFTs) and monitor for any pre-existing CNS disorders that may worsen with this drug.
2️⃣ Correct Route, Dose, and Timing
- The nurse should verify and administer the correct form of metronidazole—oral, IV, or vaginal—based on the diagnosis and doctor’s prescription.
- IV doses must be infused slowly over 30–60 minutes, and oral doses should be given with food to reduce gastrointestinal irritation.
3️⃣ Monitoring for Side Effects
- The nurse must monitor for nausea, vomiting, abdominal pain, headache, or dizziness, especially in prolonged use, and assess for signs of peripheral neuropathy (e.g., tingling or numbness).
- The nurse should also observe for urine discoloration (brown or reddish) and reassure the patient that this is harmless and temporary.
4️⃣ Patient and Family Education
- The nurse must instruct the patient to strictly avoid alcohol during and for at least 48 hours after completion of therapy, as it can cause a disulfiram-like reaction (vomiting, flushing, palpitations).
- It is important to educate the patient on completing the full course of medication even if symptoms subside, to avoid recurrence or resistance.
5️⃣ Drug Interaction and Documentation
- The nurse must assess for drug interactions, particularly with warfarin (increased bleeding risk) and phenytoin or lithium (toxicity risk), and report any signs of adverse drug reactions.
- The nurse should ensure accurate documentation of dose, route, side effects, and patient education provided, especially when used in infection control cases like C. difficile colitis.
6️⃣ Infection Control Measures
- The nurse should follow isolation precautions if the patient is being treated for infections like C. difficile or bacterial vaginosis to prevent transmission.
7️⃣ Evaluation and Follow-up
- It is necessary for the nurse to evaluate the effectiveness of therapy by monitoring for relief of symptoms (e.g., fever, diarrhea, vaginal discharge) and notify the physician if symptoms persist or worsen.
Section 2
Q.4 Definition (5)
a. Metaplasia
- Metaplasia is a reversible change in which one type of adult, fully differentiated cell is replaced by another type of adult cell that is better able to withstand the adverse environment or stress.
- It usually occurs as an adaptive response to chronic irritation or inflammation. It is most commonly seen in epithelial tissues, such as the transformation of columnar epithelium to squamous epithelium in the respiratory tract due to smoking.
b. Bronchitis
- Bronchitis is an inflammation of the bronchial tubes (bronchi), which are the air passages that carry air to the lungs, resulting in cough, mucus production, and difficulty in breathing.
- It may be acute or chronic, depending on the duration and cause.
c. Thrombosis
- Thrombosis is the pathological process of formation of a blood clot (thrombus) within a blood vessel, which obstructs the normal flow of blood through the circulatory system.
- It can occur in arteries or veins, and may lead to serious complications like myocardial infarction, stroke, or deep vein thrombosis (DVT).
d. Endometriosis
- Endometriosis is a chronic gynecological condition in which the endometrial tissue (lining of the uterus) grows outside the uterine cavity, most commonly on the ovaries, fallopian tubes, and pelvic peritoneum.
e. Edema
- Edema is the abnormal accumulation of fluid in the interstitial spaces of tissues, leading to visible swelling in the affected body parts such as the legs, ankles, face, or lungs.
- It occurs due to an imbalance in fluid filtration and reabsorption, often associated with conditions like heart failure, kidney disease, liver cirrhosis, or inflammation.
Q.5 Write notes on folowing (any four) (20)
a) Ischemic heart disease
Definition
Ischemic Heart Disease (IHD) refers to a group of conditions where the heart muscle (myocardium) receives insufficient oxygen-rich blood due to narrowing or blockage of the coronary arteries, usually caused by atherosclerosis. It is a leading cause of angina, myocardial infarction (heart attack), and sudden cardiac death.
Etiology
- Atherosclerosis (main cause)
- Hypertension
- Diabetes mellitus
- Hyperlipidemia
- Smoking and sedentary lifestyle
- Family history of CAD
Pathophysiology
- Atherosclerosis develops in coronary arteries due to accumulation of lipid-laden plaques.
- These plaques cause progressive narrowing of the arterial lumen, reducing oxygen delivery to the myocardium.
- During increased demand (e.g., exercise, stress), the oxygen supply becomes insufficient, causing myocardial ischemia.
- If blood flow is severely reduced or completely blocked, myocardial infarction (heart muscle death) may occur.
- Prolonged ischemia weakens the myocardium, leading to arrhythmias, heart failure, or sudden cardiac arrest.
Clinical Manifestations
- Chest pain (angina) radiating to arm, jaw
- Shortness of breath
- Fatigue on exertion
- Palpitations
- Nausea or diaphoresis
- Asymptomatic in some cases (silent ischemia)
Diagnostic Evaluation
- ECG (ST changes, arrhythmias)
- Troponin levels (↑ in myocardial infarction)
- Lipid profile
- Echocardiogram (wall motion abnormality)
- Stress test (treadmill test)
- Coronary angiography (definitive)
Medical & Surgical Management
- Nitrates (e.g., nitroglycerin) are used to relieve anginal pain by dilating coronary arteries and reducing myocardial workload.
- Antiplatelet agents like aspirin help prevent thrombus formation over atherosclerotic plaques.
- Statins are prescribed to lower LDL cholesterol and slow progression of atherosclerosis.
- Beta-blockers and ACE inhibitors reduce myocardial oxygen demand and protect heart function.
- In severe or unstable cases, coronary revascularization procedures like percutaneous coronary intervention (PCI) with stent or coronary artery bypass graft (CABG) are performed.
Nursing Management of Ischemic Heart Disease (IHD)
1. Assessment and Monitoring
- Monitor for chest pain characteristics, including onset, location, intensity, radiation, and duration, and report any unrelieved pain immediately.
- Check vital signs, especially blood pressure, pulse rate, oxygen saturation, and ECG changes, at regular intervals.
- Observe for signs of heart failure, such as dyspnea, pedal edema, and crackles in the lungs.
- Monitor cardiac enzymes and troponin levels as prescribed to detect myocardial injury.
- Maintain a daily weight chart and intake-output record to assess fluid overload.
2. Medication Administration and Compliance
- Administer nitrates, beta-blockers, aspirin, statins, and anticoagulants as prescribed and monitor for side effects.
- Educate the patient about the purpose, dosage, and timing of medications and the importance of lifelong adherence.
- Observe for signs of hypotension or bradycardia after nitrate or beta-blocker administration.
- Encourage timely INR testing if the patient is on warfarin therapy.
- Keep rescue medication (sublingual nitroglycerin) at the bedside and teach proper usage during anginal episodes.
3. Activity Management and Lifestyle Modification
- Encourage rest during acute episodes and gradually increase activity level based on the patient’s tolerance.
- Educate about avoiding heavy lifting, stress, or strenuous exertion that could precipitate angina.
- Support adoption of a low-fat, low-sodium, heart-healthy diet and weight management strategies.
- Emphasize smoking cessation, alcohol moderation, and regular exercise tailored to the patient’s condition.
- Refer to cardiac rehabilitation programs for structured guidance and support.
4. Patient and Family Education
- Explain the nature of ischemic heart disease, its risk factors, and warning signs of worsening condition or heart attack.
- Instruct on home monitoring of BP and pulse, and when to seek emergency help (e.g., unrelieved chest pain).
- Teach stress reduction techniques like deep breathing, yoga, or relaxation therapy.
- Provide a written medication schedule and discharge instructions for diet, activity, and follow-up care.
- Educate the family members about CPR and emergency response in case of sudden collapse.
Complications
- Myocardial infarction
- Arrhythmias (e.g., atrial fibrillation, ventricular tachycardia)
- Heart failure
- Cardiogenic shock
- Sudden cardiac death
b) Pneumonia
Definition of Pneumonia
- It is an acute inflammatory condition of the lung parenchyma, primarily affecting the alveoli, and it is usually caused by infection from bacteria, viruses, fungi, or aspiration of foreign substances.
- It is characterized by consolidation of the affected lung tissue, causing difficulty in breathing, cough, fever, and sputum production.
Etiology / Causes
- Bacterial infection (e.g., Streptococcus pneumoniae)
- Viral infection (e.g., influenza virus)
- Fungal infection (e.g., Pneumocystis jirovecii)
- Aspiration of food, vomitus, or fluids
- Inhalation of toxic substances
- Immunocompromised state (e.g., HIV/AIDS)
Pathophysiology of Pneumonia
- It begins when pathogens enter the lungs either through inhalation, aspiration, or bloodstream.
- These pathogens reach the alveolar sacs, where they multiply and cause inflammation.
- Inflammatory cells such as neutrophils and macrophages accumulate, releasing cytokines and enzymes.
- This leads to filling of alveoli with exudate and fluid, causing consolidation and impaired gas exchange.
- Hypoxia develops due to blocked oxygen exchange, leading to symptoms like breathlessness and cyanosis.
Clinical Manifestations / Signs & Symptoms
- Cough with or without sputum
- Fever with chills
- Shortness of breath
- Chest pain while breathing or coughing
- Fatigue and weakness
- Cyanosis (in severe cases)
Diagnostic Evaluation
- Chest X-ray (to detect lung consolidation)
- Sputum culture and sensitivity
- CBC – shows elevated WBCs
- Blood cultures
- Pulse oximetry/ABG – shows low oxygen
- CRP and ESR – elevated in inflammation
Medical Management
- Antibiotic therapy is initiated based on the causative organism; e.g., amoxicillin, azithromycin, or cephalosporins.
- Antipyretics like paracetamol are given to reduce fever and discomfort.
- Cough suppressants or expectorants may be prescribed to aid mucus clearance.
- Oxygen therapy is given in case of hypoxia or low oxygen saturation.
- IV fluids are administered to maintain hydration and manage hypotension.
- In severe cases, hospitalization and mechanical ventilation may be needed.
Nursing Management
✅ Respiratory Support
- It is essential to monitor the patient’s respiratory rate, depth, and effort regularly, especially during acute phases.
- The nurse must administer oxygen as per physician’s order and monitor SpO₂ levels using pulse oximeter.
- It is crucial to assist the patient with chest physiotherapy and incentive spirometry to enhance lung expansion.
- The nurse should encourage the patient to cough and take deep breaths to promote mucus clearance.
✅ Hydration and Nutrition
- The nurse must ensure adequate fluid intake, either oral or IV, to help loosen respiratory secretions.
- It is important to provide a nutritious, high-protein diet to boost immunity and support healing.
- In cases of poor oral intake, tube feeding or IV nutrition support may be required.
✅ Medication Administration
- The nurse should administer prescribed antibiotics on time, checking for side effects or allergic reactions.
- It is vital to record temperature, pain, and other vital signs before and after drug administration.
- The nurse must monitor the patient for therapeutic response, such as decreased fever and improved breathing.
✅ Positioning and Comfort
- It is advised to keep the patient in semi-Fowler’s position to aid lung expansion and ease breathing.
- The nurse must provide frequent back care and change of position to prevent bedsores.
- Comfort measures like warm fluids, steam inhalation, or use of humidifier may be encouraged if ordered.
✅ Health Education
- The nurse must educate the patient and family about completing the full course of antibiotics.
- It is important to teach proper cough etiquette and hygiene to prevent the spread of infection.
- The nurse should advise the patient on vaccination against pneumococcal pneumonia and influenza.
Complications
- Pleural effusion
- Lung abscess
- Respiratory failure
- Sepsis or septic shock
- Empyema
- Chronic lung disease (in repeated infections)
c) Acute inflammation
Definition
Acute inflammation is the immediate and early response of body tissues to injury, infection, or irritation, characterized by redness, heat, swelling, pain, and loss of function.
It is a protective mechanism aimed at removing the injurious agents and initiating tissue repair, usually lasting for a few hours to days.
Etiology
- Physical injury (cuts, burns, trauma)
- Infection (bacterial, viral, fungal)
- Chemical irritants or toxins
- Immune reactions (e.g., allergies)
- Thermal injury (heat or cold exposure)
Pathophysiology
- When tissue injury occurs, chemical mediators like histamine, prostaglandins, and cytokines are released by damaged cells, mast cells, and macrophages.
- These mediators cause vasodilation, leading to increased blood flow (redness and heat) at the site of injury.
- Capillary permeability increases, allowing plasma and leukocytes to move into the tissues, causing swelling (edema).
- Leukocytes (mainly neutrophils) migrate to the site via chemotaxis and start phagocytosis of microbes and dead cells.
- The inflammatory exudate accumulates, and tissue repair begins once the injurious agents are removed.
- If resolution occurs, tissue returns to normal; if not, inflammation may persist and progress to chronic inflammation.
Clinical Manifestations
- Redness (rubor)
- Heat (calor)
- Swelling (tumor)
- Pain (dolor)
- Loss of function (functio laesa)
- Fever (in systemic response)
- Local tenderness
Diagnostic Evaluation
- Complete blood count (↑ neutrophils)
- ESR and CRP (inflammatory markers)
- Culture and sensitivity (if infection suspected)
- X-ray or ultrasound (for internal inflammation)
- Physical examination of affected area
Medical & Surgical Management
- Nonsteroidal anti-inflammatory drugs (NSAIDs) such as ibuprofen or diclofenac are used to reduce inflammation and relieve pain.
- Antibiotics are prescribed when infection is the underlying cause of inflammation.
- In case of abscess formation, incision and drainage may be required to remove pus and allow healing.
- Cold compresses are used in the initial phase to reduce swelling, while warm compresses may help in later stages to enhance circulation.
- Rest, elevation, and immobilization of the affected part may be advised to minimize irritation and promote recovery.
Nursing Management
1. Assessment and Monitoring
- The nurse should assess the site of inflammation for redness, warmth, swelling, and pain, and document changes regularly.
- Monitor vital signs including temperature to detect any signs of systemic infection or fever.
2. Medication Administration
- Administer prescribed anti-inflammatory drugs, antibiotics, and analgesics, and observe for side effects like gastric irritation.
- Educate the patient on the importance of completing the full antibiotic course, even if symptoms improve.
3. Local Care and Comfort Measures
- Apply cold compresses during the early phase to reduce edema and pain, followed by warm compresses later to improve circulation and promote healing.
- Ensure the affected limb is elevated and immobilized if necessary to reduce swelling and pain.
4. Infection Control
- Maintain strict hand hygiene and wound care to prevent secondary infection.
- Monitor for signs of spreading infection such as increased redness, warmth, pus discharge, or fever.
5. Patient Education and Psychosocial Support
- Educate the patient on recognizing early signs of infection and when to seek medical help.
- Provide emotional reassurance, especially if the inflammation causes pain or functional limitations in daily activities.
Complications
- Abscess formation
- Cellulitis or spread of infection
- Chronic inflammation
- Tissue necrosis
- Sepsis (if systemic spread)
d) Urine examination
Definition of Urine Examination
- It is a diagnostic test in which urine is analyzed chemically, physically, and microscopically to detect various diseases, metabolic disorders, kidney function, and urinary tract abnormalities.
- It is non-invasive, quick, and economical, and it gives important clues to various systemic illnesses, especially renal and metabolic.
Types of Urine Examination
- Physical Examination of Urine
- Chemical Examination of Urine
- Microscopic Examination of Urine
- Bacteriological Examination of Urine
- 24-Hour Urine Collection
Physical Examination of Urine
It is used to assess the appearance and physical characteristics of urine sample:
- Color: It is normally pale yellow to amber; dark yellow may indicate dehydration or jaundice.
- Clarity: It is usually clear; turbidity may indicate pus cells, crystals, or bacteria.
- Odor: It is mildly aromatic; fruity smell indicates ketonuria, foul smell indicates infection.
- Specific Gravity: It is normally 1.005–1.030; high levels may indicate dehydration, low levels may suggest overhydration or renal impairment.
- Volume: Normal is 1200–1500 ml/day; oliguria, anuria, or polyuria indicates different pathologies.
- pH: Normal is 4.5–8.0; acidic urine in metabolic acidosis, alkaline in UTI or alkalosis.
Chemical Examination of Urine
It is done by using reagent strips (dipstick) or manual methods.
- Protein: It is not normally present; presence indicates proteinuria or renal disease.
- Glucose: It is absent in healthy individuals; presence suggests diabetes mellitus.
- Ketone Bodies: It is absent normally; presence indicates diabetic ketoacidosis or starvation.
- Bile Pigments (Bilirubin/Urobilinogen): Presence may indicate liver disease or hemolysis.
- Blood (Hematuria): Presence may suggest UTI, stones, trauma, or malignancy.
- Nitrites: It is formed by bacterial metabolism; positive in urinary tract infection.
- Leukocyte esterase: It indicates presence of pus cells and infection.
Microscopic Examination of Urine
- It is done under a microscope to detect cells, crystals, casts, and microorganisms.
- Red Blood Cells (RBCs): It is present in glomerulonephritis, trauma, stones.
- White Blood Cells (WBCs): It is present in infection and inflammation.
- Casts: Hyaline casts (normal), granular casts (nephritis), RBC casts (glomerulonephritis).
- Crystals: Calcium oxalate, uric acid, triple phosphate crystals suggest metabolic disorders.
- Bacteria/Yeast/Parasites: Indicates urinary tract infection or contamination.
6. Bacteriological Examination of Urine
- It is performed to isolate and identify pathogenic organisms, commonly in UTI.
- Midstream clean catch sample is ideal for culture.
- Colony count >100,000/ml indicates infection.
- Antibiotic sensitivity testing is done to choose effective antibiotics.
24-Hour Urine Collection Test
- It is done to quantify the total excretion of certain substances over 24 hours.
- It is used to estimate protein, creatinine, calcium, catecholamines, VMA.
- Accurate timing and proper collection is necessary to avoid errors.
- It helps assess kidney function and systemic disorders like Cushing’s syndrome.
Indications for Urine Examination
- It is used in diagnosis and monitoring of urinary tract infections.
- It is essential in screening for diabetes mellitus and gestational diabetes.
- It helps in diagnosis of renal disorders such as nephritis, glomerulonephritis, and failure.
- It assists in detection of liver diseases, hemolysis, and metabolic abnormalities.
- It is done routinely in antenatal care, pre-surgical assessment, and general checkups.
Nursing Responsibilities During Urine Examination
- Educating the patient: It is the nurse’s duty to explain to the patient the purpose, importance, and procedure of urine collection to ensure accurate results.
- Proper collection technique: It is the nurse’s responsibility to ensure that a clean, dry, and labeled sterile container is provided, and midstream urine is collected in case of infection screening.
- Timely transport to laboratory: It is essential for the nurse to ensure that the specimen is sent to the lab within 30–60 minutes, or stored properly to avoid bacterial overgrowth.
- Recording observations: The nurse should note and report the volume, color, odor, or any unusual finding to the physician immediately.
- Maintaining hygiene: It is crucial that the nurse advises the patient on perineal hygiene, especially in female patients, before urine collection.
- Documentation: It is important that the nurse records time of collection, reason for test, and patient condition in nursing notes for continuity of care.
- Follow universal precautions: The nurse should wear gloves, avoid direct contact with urine, and ensure hand hygiene before and after sample handling.
e) jaundice
Definition
Jaundice is a clinical condition characterized by yellow discoloration of the skin, sclera (whites of the eyes), and mucous membranes, resulting from elevated levels of bilirubin in the blood (hyperbilirubinemia), typically above 2.5 mg/dL.
Etiology
- Hemolysis (pre-hepatic causes)
- Hepatitis, cirrhosis (hepatic causes)
- Bile duct obstruction (post-hepatic or obstructive)
- Neonatal liver immaturity
- Genetic disorders (e.g., Gilbert’s syndrome)
Pathophysiology
- Bilirubin is a by-product of red blood cell breakdown, processed by the liver for excretion.
- In pre-hepatic jaundice, excessive RBC breakdown leads to overproduction of unconjugated bilirubin.
- In hepatic jaundice, liver cells are damaged (e.g., hepatitis), impairing the liver’s ability to conjugate and excrete bilirubin.
- In post-hepatic (obstructive) jaundice, bile flow is blocked due to gallstones, tumors, or strictures, causing conjugated bilirubin to leak into the bloodstream.
- The accumulation of bilirubin in blood and tissues results in yellowish discoloration and other systemic symptoms.
Clinical Manifestations
- Yellowing of skin and sclera
- Dark-colored urine
- Pale or clay-colored stools
- Fatigue and weakness
- Pruritus (itching)
- Nausea and poor appetite
Diagnostic Evaluation
- Serum bilirubin (total, direct, indirect)
- Liver function tests (ALT, AST, ALP)
- CBC (to check for hemolysis)
- Abdominal ultrasound or CT scan
- Hepatitis serology panel
Medical & Surgical Management
- Management depends on the underlying cause — antiviral drugs for hepatitis, antibiotics for infections, or steroids for autoimmune hepatitis.
- In obstructive jaundice, surgical interventions like ERCP (Endoscopic Retrograde Cholangiopancreatography) or cholecystectomy may be necessary.
- Phototherapy is used in neonatal jaundice to convert bilirubin into water-soluble forms for excretion.
- Supportive treatments include hydration, vitamin supplements (especially B complex and K), and high-carbohydrate diets.
- Liver transplant may be considered in cases of irreversible liver failure or advanced cirrhosis.
Nursing Management of Jaundice
1. Assessment and Monitoring
- Monitor skin and scleral color changes, and document progression or improvement in jaundice.
- Assess for signs of fatigue, anorexia, nausea, or itching, which may suggest worsening liver function.
- Check vital signs, especially temperature (for infections) and heart rate (for dehydration or anemia).
- Monitor daily input/output and stool/urine color to evaluate bile excretion.
- Report any signs of confusion, bleeding, or abdominal distension, indicating hepatic encephalopathy or worsening condition.
2. Medication Administration and Evaluation
- Administer prescribed medications such as antivirals, antibiotics, cholestyramine (for itching), or vitamin K (for clotting).
- Monitor for adverse drug reactions and educate the patient to avoid hepatotoxic drugs (e.g., paracetamol, alcohol).
- Evaluate effectiveness of treatment by observing bilirubin levels and symptom resolution.
- Educate about medication compliance, especially in chronic liver disease.
- In neonatal cases, monitor effectiveness of phototherapy and protect eyes with shields during treatment.
3. Nutritional and Hydration Support
- Provide a high-calorie, low-protein, low-fat diet, especially in hepatic jaundice, to reduce liver workload.
- Encourage small, frequent meals to maintain energy levels and reduce nausea.
- Ensure adequate fluid intake to promote bilirubin excretion and prevent dehydration.
- Supplement with vitamins (A, D, E, K) in fat malabsorption cases.
- Monitor for signs of malnutrition or vitamin deficiencies, especially in prolonged jaundice.
4. Health Education and Psychosocial Support
- Educate the patient and family about the cause, progression, and prevention of jaundice.
- Counsel on avoiding alcohol, smoking, and junk foods to protect liver health.
- Instruct on hygiene and infection control, especially in infectious hepatitis.
- Encourage follow-up visits, liver function monitoring, and timely reporting of new symptoms.
- Provide emotional support and address anxiety due to changes in appearance or chronic illness.
Complications
- Hepatic encephalopathy
- Liver failure
- Coagulopathy (bleeding disorders)
- Pruritus and skin breakdown
- Malnutrition
- Sepsis (in obstructive jaundice)
Q.6 Answer the following (any three) (12)
a) Karotyping
Definition
- It is a laboratory technique used to visualize the number, size, shape, and structure of chromosomes in a cell, usually during metaphase of mitosis.
- It is a process in which the complete set of chromosomes from a person is photographed and arranged in a standard format to detect chromosomal abnormalities.
- It is used especially in prenatal diagnosis, cancer studies, and detection of genetic disorders.
Purpose of Karyotyping
- It is used to detect chromosomal abnormalities such as trisomies, monosomies, deletions, duplications, or translocations.
- It is commonly done to diagnose congenital genetic disorders like Down syndrome, Turner syndrome, or Klinefelter syndrome.
- It helps in prenatal diagnosis when done on amniotic fluid or chorionic villi cells.
- It is used in infertility evaluations, recurrent miscarriages, or ambiguous genitalia assessment.
- It is helpful in cancer diagnosis, particularly in identifying chromosomal changes in leukemia and lymphoma.
Steps/Procedure of Karyotyping
Sample Collection:
It is usually done from peripheral blood, bone marrow, amniotic fluid, chorionic villi, or tissue biopsy.
Cell Culture:
It is the process in which white blood cells or fetal cells are cultured for 48–72 hours in a medium that promotes cell division.
Arresting Cells in Metaphase:
It involves adding colchicine or colcemid to stop the cell division at metaphase, where chromosomes are most visible.
Hypotonic Treatment:
The cells are placed in a hypotonic solution which causes the cells to swell, thus separating the chromosomes.
Fixation and Slide Preparation:
Cells are then fixed using methanol-acetic acid and spread onto a glass slide.
Staining of Chromosomes:
Chromosomes are stained using Giemsa stain (in G-banding), which gives a light and dark banding pattern for identification.
Microscopic Observation:
Under the microscope, metaphase spreads are observed, and photographs of chromosomes are taken.
Karyotype Arrangement:
The chromosomes are arranged in pairs (22 autosomal pairs and 1 sex chromosome pair) from largest to smallest, forming a karyogram.
Normal Human Karyotype
- A normal karyotype consists of 46 chromosomes arranged in 23 pairs.
- 22 pairs are autosomes (numbered 1 to 22).
- 1 pair is sex chromosomes (XX in females, XY in males).
Uses / Clinical Applications of Karyotyping
Prenatal Diagnosis:
It is used in pregnant women to detect chromosomal disorders in the fetus, like Trisomy 21 (Down syndrome), Trisomy 18, and Turner syndrome.
Infertility Evaluation:
It is used in both men and women to identify chromosomal causes of infertility, like Klinefelter syndrome (47,XXY) or Turner syndrome (45,X).
Cancer Diagnosis:
It helps in detecting chromosomal changes in hematologic malignancies, such as Philadelphia chromosome in chronic myeloid leukemia (CML).
Mental Retardation / Developmental Delay:
It is done in children with unexplained developmental delay, dysmorphic features, or intellectual disability to look for chromosomal abnormalities.
Sex Determination / Ambiguous Genitalia:
It is done in cases of intersex or ambiguous genitalia to confirm chromosomal sex (e.g., XX, XY, XO, XXY).
Advantages of Karyotyping
- It is highly accurate in detecting large-scale chromosomal abnormalities.
- It is helpful in confirming diagnosis of genetic disorders, especially congenital syndromes.
- It gives a visual record of the full chromosomal structure for further reference.
Limitations
- It cannot detect small genetic mutations or single gene disorders.
- It requires actively dividing cells, so it may not be suitable for all samples.
- It is time-consuming and takes several days to culture cells.
Nursing Responsibilities in Karyotyping
- It is the nurse’s responsibility to provide health education and counseling to the client and family members, explaining the purpose, benefits, and potential outcomes of karyotyping.
- It is essential for the nurse to obtain informed consent before collecting blood or amniotic fluid, ensuring that the patient is fully aware of the procedure and risks.
- The nurse must prepare and assist in sterile sample collection techniques, especially during procedures like amniocentesis or chorionic villus sampling.
- The nurse should maintain strict sample labeling and preservation, ensuring it reaches the genetic lab without contamination or delay.
- After the test, the nurse should support patients psychologically, especially if abnormal findings are detected, and refer them to genetic counseling or specialized services as needed.
b) Role of nurse in genetic counseling
1️⃣ Establishing Trust and Providing Psychological Support
- It is the nurse’s primary role to establish a warm, respectful, non-judgmental, and confidential relationship with individuals or couples undergoing genetic counseling, as this helps build emotional safety and trust during a potentially distressing or sensitive period.
- It is essential for the nurse to show empathetic listening, cultural sensitivity, and emotional validation, especially when the client expresses fears, guilt, confusion, or anxiety regarding the possibility of inherited disorders or risks to offspring.
- It is also the responsibility of the nurse to assure the client that their concerns are being taken seriously and to encourage open communication about family history, feelings, and expectations related to genetic health.
2️⃣ Taking a Detailed Family and Personal Genetic History
- It is the duty of the nurse to conduct a thorough assessment of the patient’s three-generation pedigree, which includes information about the health status of parents, siblings, children, aunts, uncles, and grandparents, as this helps identify any recurring genetic disorders or patterns of inheritance.
- It is important for the nurse to ask specific questions about miscarriages, stillbirths, developmental delays, congenital anomalies, infertility, consanguinity (marriage among blood relatives), early deaths, or any unusual health conditions in the family.
- It is also the nurse’s role to record any exposure to environmental teratogens, medications, radiation, or infections during pregnancy, which may contribute to genetic abnormalities.
3️⃣ Educating the Client and Family About Genetic Concepts
- It is the nurse’s professional responsibility to educate the individual or family about the nature of the suspected or diagnosed genetic disorder, including modes of inheritance (autosomal dominant, autosomal recessive, X-linked, mitochondrial, multifactorial), possible symptoms, progression, and implications.
- It is necessary for the nurse to use simple, non-technical language along with charts, diagrams, and visual aids like Punnett squares or pedigree trees to explain how a gene mutation may be inherited or occur spontaneously.
- It is the nurse’s role to help the client understand the purpose, procedures, and results of genetic testing (such as amniocentesis, chorionic villus sampling, karyotyping, DNA analysis), including possible risks, benefits, limitations, and ethical dilemmas associated with such testing.
4️⃣ Referral to Specialized Genetic Services
- It is the nurse’s duty to identify when the case requires specialized evaluation and refer the individual or couple to clinical geneticists, genetic counselors, or prenatal diagnostic centers for further genetic assessment and advice.
- It is also the responsibility of the nurse to help the client schedule, prepare for, and understand follow-up appointments with specialists, ensuring they have full access to support services like social work, psychological counseling, and medical genetics.
- The nurse plays a coordination role in communicating between the client and different healthcare team members involved in genetic care to ensure continuity of care and appropriate follow-up.
5️⃣ Supporting Informed Decision-Making and Autonomy
- It is essential for the nurse to ensure that the client or couple has all the accurate information needed to make a well-informed decision regarding their reproductive choices, genetic testing, or medical management options.
- The nurse should always respect the client’s autonomy, religious values, cultural beliefs, and moral framework, even if the decision (e.g., to terminate or continue a genetically affected pregnancy) does not align with the nurse’s personal values.
- It is the nurse’s ethical responsibility to protect the client from pressure, coercion, or misinformation, and to obtain written informed consent prior to any genetic testing or intervention.
6️⃣ Participating in Community Education and Genetic Screening Programs
- It is the nurse’s public health role to actively participate in community-based genetic screening and education programs, especially in regions with high prevalence of disorders like thalassemia, sickle cell anemia, Tay-Sachs disease, or Down syndrome.
- The nurse must educate at-risk populations, especially young couples, about the importance of pre-marital screening, antenatal screening, and voluntary genetic testing for early identification and prevention of inherited diseases.
- It is also the responsibility of the nurse to organize awareness campaigns, health talks, and school health programs to improve understanding of genetic health, especially among women of reproductive age and adolescents.
7️⃣ Maintaining Confidentiality and Ethical Standards
- It is the nurse’s legal and professional responsibility to ensure complete confidentiality of the client’s genetic information, which must not be shared with anyone — including insurance companies, employers, or relatives — without the individual’s written consent.
- It is essential for the nurse to store genetic reports securely, document sessions accurately, and maintain a record of counseling discussions, test results, and patient preferences.
- The nurse must follow all guidelines related to bioethics, patient rights, and human dignity, as outlined by national and international health authorities.
c) Down syndrome
Definition
- Down syndrome is a genetic chromosomal disorder that occurs due to the presence of an extra copy of chromosome 21, leading to 47 chromosomes instead of the normal 46.
- It is also known as Trisomy 21, and it results in intellectual disability, distinctive facial features, and various developmental and health problems.
Etiology / Causes
- Nondisjunction during meiosis (most common)
- Translocation of chromosome 21
- Mosaicism (partial trisomy 21)
- Increased maternal age (above 35 years)
- Family history of chromosomal abnormalities
Pathophysiology
- It begins with an error in cell division during the formation of the egg or sperm, most often due to nondisjunction.
- As a result, the fertilized egg ends up with three copies of chromosome 21 instead of the usual two.
- This extra chromosome leads to overexpression of genes, which affects physical and cognitive development.
- The overexpressed genes disrupt the normal development of the brain, heart, musculoskeletal system, and other organs.
- The presence of this genetic abnormality causes delayed milestones, intellectual disability, hypotonia, and congenital anomalies like heart defects.
Clinical Features / Signs and Symptoms
- Flat facial profile and slanted eyes
- Small head and short neck
- Protruding tongue and small mouth
- Hypotonia (poor muscle tone)
- Short stature and short fingers
- Intellectual disability (mild to moderate)
- Delayed growth and development
- Congenital heart defects (e.g., AV septal defect)
Diagnostic Evaluation
- Prenatal screening tests (triple test, quad screen)
- Ultrasound during pregnancy
- Amniocentesis and chorionic villus sampling (CVS)
- Karyotyping – confirms Trisomy 21
- Echocardiography – to detect congenital heart disease
- Developmental screening tests
Medical and Surgical Management
- There is no cure for Down syndrome; treatment is supportive and symptom-based.
- Cardiac surgery may be needed for structural heart defects.
- Hearing aids or eye correction may be required for sensory defects.
- Speech therapy, occupational therapy, and physiotherapy are provided to promote development.
- Special education programs and individualized teaching support cognitive growth.
- Regular health checkups are essential to monitor for complications like hypothyroidism or infections.
Nursing Management
✅ Physical Care and Monitoring
- The nurse must assess growth and development regularly using standardized growth charts for Down syndrome.
- It is important to monitor for signs of cardiac distress, respiratory infections, or feeding difficulties, especially in infancy.
- The nurse should provide supportive care for hypotonia including proper positioning, range-of-motion exercises, and safety precautions.
✅ Developmental Support
- It is necessary to encourage early intervention programs such as physiotherapy, occupational therapy, and language development.
- The nurse should assist parents in creating a structured, stimulating environment for the child’s learning.
- It is essential to promote independence in self-care activities as per the child’s abilities.
✅ Family Support and Education
- The nurse must provide emotional support to the family, especially after diagnosis.
- It is important to educate parents about the nature of the condition, prognosis, and expectations.
- The nurse should refer families to genetic counseling and support groups.
- Parents should be taught about the importance of routine health screening and vaccination.
✅ Prevention of Complications
- The nurse must be vigilant for signs of respiratory infections, sleep apnea, and feeding difficulties.
- Proper hygiene, handwashing, and environmental cleanliness should be promoted.
- Eye and hearing tests should be done regularly as part of routine care.
Complications
- Congenital heart defects (e.g., atrioventricular septal defect)
- Intellectual and developmental delays
- Hearing and visual impairment
- Frequent respiratory infections
- Hypothyroidism
- Gastrointestinal disorders (e.g., duodenal atresia)
- Increased risk of leukemia
- Alzheimer’s disease in later life
d) Mutation
Definition of Mutation
- It is defined as a permanent alteration or change in the nucleotide sequence of DNA within a gene or chromosome of an organism.
- It may occur spontaneously or due to environmental factors, such as radiation, chemicals, or viruses.
- It can result in genetic disorders, altered protein synthesis, or may have no effect at all on the organism.
- Mutations may be inherited from parents or acquired during the life of an individual (somatic mutation).
Types of Mutation
1️⃣ Based on Cell Type Involved
Germline Mutation
- It occurs in reproductive cells (sperm or egg).
- It is inheritable and passed on to offspring.
- It plays a major role in hereditary genetic disorders.
Somatic Mutation
- It occurs in non-reproductive body cells.
- It cannot be inherited, and affects only the individual.
- It can lead to conditions such as cancer or localized tissue damage.
2️⃣ Based on Type of Genetic Change
Point Mutation
- It is the mutation where a single nucleotide base is substituted.
- Example: Sickle cell anemia caused by substitution of adenine (A) with thymine (T).
Insertion Mutation
- It is a mutation where one or more extra nucleotide bases are added into a DNA sequence.
- It often causes frameshift mutation, altering all downstream amino acids.
Deletion Mutation
- It involves the loss of one or more nucleotide bases from a DNA sequence.
- Like insertion, it may also result in frameshift and abnormal protein synthesis.
Duplication Mutation
- It involves repetition of a section of DNA, resulting in extra copies of a gene.
- It may lead to conditions like Charcot-Marie-Tooth disease.
Inversion Mutation
- It is the mutation where a segment of DNA is reversed end to end.
- It can disrupt gene expression.
Translocation Mutation
- It occurs when a segment of one chromosome breaks off and attaches to another chromosome.
- Example: Chronic Myeloid Leukemia (CML) is associated with Philadelphia chromosome translocation.
Causes of Mutation (Etiology)
- Spontaneous errors during DNA replication
- Ionizing radiation (e.g., X-rays, gamma rays)
- Ultraviolet (UV) light exposure
- Chemical mutagens (e.g., benzene, formaldehyde)
- Biological agents (e.g., viruses)
- Errors in meiosis and mitosis
Effects / Consequences of Mutation
- It can cause genetic disorders (e.g., cystic fibrosis, sickle cell anemia).
- It may disrupt protein function or synthesis, leading to non-functional proteins.
- It may result in cancer, when it affects oncogenes or tumor suppressor genes.
- It can be beneficial, neutral, or harmful, depending on the type and location.
- Some mutations may contribute to evolutionary changes over generations.
Diagnosis of Genetic Mutations
- Karyotyping – to detect chromosomal abnormalities.
- Polymerase Chain Reaction (PCR) – to amplify and analyze DNA sequences.
- DNA Sequencing – to identify exact mutations at nucleotide level.
- Fluorescent In Situ Hybridization (FISH) – to detect chromosomal translocations or deletions.
- Newborn Screening – for early detection of inherited disorders.
Prevention & Counseling in Nursing
- It is important to avoid exposure to mutagens like radiation and toxic chemicals.
- Genetic counseling should be provided to families with history of genetic disorders.
- Nurses should support prenatal diagnostic testing (e.g., amniocentesis) and help patients understand their results.
- Genetic nursing includes educating individuals about inherited diseases, treatment options, and risk of transmission.
Importance of Mutation in Nursing and Healthcare
- It helps nurses understand the basis of inherited diseases.
- It guides gene therapy, personalized medicine, and pharmacogenomics.
- It allows nurses to provide better patient education and emotional support.
- Nurses can collaborate in genetic screening, early detection, and patient referral.
