09/07/2022-B.SC-CHILD HEALTH NURSING-PAPER (DONE)-UPLOAD NO.1
09/07/2022-B.SC-CHILD HEALTH NURSING-PAPER-UPLOAD NO.1
(KINDLY SEND YOUR UNIVERSITY PAPER IMAGE WATS APP ON – 8485976407 – WE PROVIDE ITS SOLUTION AS PER YOUR NEED)
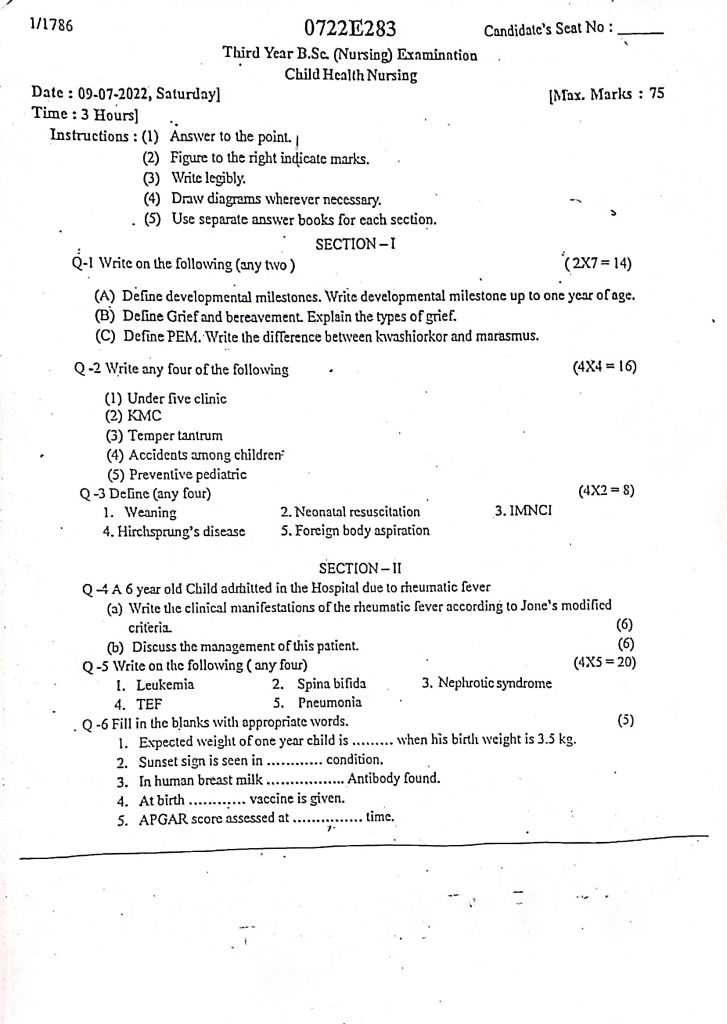
SECTION-I
Q-1 Write on the following (any two) (2X7-14)
(A) Define developmental milestones. Write developmental milestone up to one year of age.
Developmental milestone
Developmental milestones are age-specific functional skills or tasks that most children can do at a certain age range. These milestones reflect a child’s physical, cognitive, social, emotional, and communication development, and serve as important indicators of overall growth and neurological health.
Developmental milestones up to one year of age
📅 At Birth (0 Month)
- The newborn lies in a flexed position with the arms and legs drawn close to the body, and shows complete head lag when pulled to sit.
- Shows strong primitive reflexes including the Moro reflex, palmar grasp, rooting, and sucking.
- Fine motor activity is involuntary, with tightly clenched fists and reflex hand closure.
- Crying is the only form of language expression, mainly in response to hunger or discomfort.
- Socially, the baby prefers human faces, becomes quiet when comforted, and briefly stares at contrasting objects.
- Shows startle reflex to loud sounds and may respond to touch by blinking or moving limbs.
📅 1 Month
- The baby can slightly lift the head when prone, and the head may wobble side to side.
- Hands remain in a closed position most of the time, with occasional jerky arm movements.
- Makes soft vowel sounds, may coo briefly, and listens intently to human voices.
- Begins to make eye contact with caregivers, may follow slow-moving objects within a limited range.
- Recognizes mother’s voice, and calms when picked up or soothed.
- Shows brief alert periods, usually after feeding.
📅 2 Months
- Holds the head up more steadily while lying on the tummy and may lift the chest slightly with arm support.
- Hands begin to open more frequently, and the baby can bring hands toward the mouth.
- Makes cooing and gurgling sounds, especially when spoken to or when content.
- Shows a true social smile, indicating pleasure upon seeing a familiar face.
- Follows objects with eyes from side to midline, and may track movement briefly.
- Becomes quiet and attentive to soft music or a familiar voice.
📅 3 Months
- The baby has much better head control, can hold the head up and centered during tummy time, and lifts the chest higher.
- Starts to bat at objects and may briefly grasp a toy when placed in hand.
- Vocalizes more varied coos and vowel-like sounds, showing enjoyment through pitch and tone changes.
- Smiles spontaneously and recognizes familiar caregivers, responding to voice and touch.
- Shows excitement by waving arms and kicking when stimulated.
- Begins to visually track toys and express curiosity about new faces.
📅 4 Months
- The baby is able to roll from tummy to back, props self up on elbows, and maintains head steadily in vertical position.
- Reaches out intentionally for dangling toys, brings hands together at midline, and holds a rattle with brief control.
- Laughs aloud and continues bubbling and cooing during interaction.
- Becomes more expressive with facial gestures, and smiles at own reflection in the mirror.
- Enjoys interactive games like “pat-a-cake” and anticipates being picked up when arms are extended.
- Shows early awareness of surroundings by turning head toward new voices.
📅 5 to 6 Months
- Begins to roll both ways, bears weight on legs when held upright, and sits briefly with support.
- Transfers objects hand-to-hand, reaches for toys actively, and uses the whole palm to grasp objects.
- Babbles repetitive syllables like “ba-ba” and “ma-ma” (without meaning), and enjoys sound-making toys.
- Shows attachment to caregivers, responds to familiar people with excitement, and shows wariness of strangers.
- Looks around with interest, tries to reach for distant objects, and understands simple cause-effect relationships.
- May become frustrated if toys are taken away, showing emotional reactions more clearly.
📅 7 to 8 Months
- Sits well without support, leans forward to reach, and may begin crawling or scooting.
- Uses a raking motion to pick up small objects, bangs toys together, and may attempt to feed self.
- Understands “no”, responds to own name, and imitates speech sounds with greater variation.
- Shows clear signs of stranger anxiety, clings to parents, and may cry when left alone.
- Plays interactive games like peek-a-boo, recognizes familiar faces in photos or mirrors.
- Starts to explore objects by shaking, banging, and dropping to observe reactions.
📅 9 Months
- Pulls to stand holding furniture and starts cruising sideways, crawling is faster and more purposeful.
- Develops a refined pincer grasp, allowing picking up of tiny items like cereal between thumb and index finger.
- Says “mama” or “dada” non-specifically, understands simple instructions and gestures like “give me” or “come here.”
- Shows separation anxiety, follows caregiver around, and enjoys clapping and waving hands.
- Understands the concept of object permanence—searches for dropped or hidden toys.
- Begins to show independent personality traits, like preferences for food or toys.
📅 10 to 11 Months
- Cruises confidently holding furniture, may stand briefly without support, and attempts to stoop and recover balance.
- Can put objects into a container and remove them, scribbles with a crayon if offered.
- Responds to one-step verbal commands, says 1–2 meaningful words, and imitates adult tones and phrases.
- Exhibits imitation behavior, such as pretending to talk on a toy phone or brushing a doll’s hair.
- Points to desired objects, expresses dislike by turning head or throwing toys.
- Demonstrates simple problem-solving skills, like turning objects to fit or exploring how doors open.
📅 12 Months (1 Year)
- Walks with one hand held or independently, stands alone with confidence, and may climb onto low furniture.
- Uses mature pincer grasp, stacks 2–3 blocks, and turns pages of a book (2–3 at a time).
- Says 1–3 clear words with meaning, understands 5–10 simple words, and uses gestures like pointing, waving, and nodding.
- Follows simple commands like “give that to me” or “come here,” and imitates words during songs.
- Engages in symbolic or pretend play, such as feeding a doll or pretending to sleep.
- Shows increasing independence, resists diaper changes, explores surroundings, and may exhibit tantrum-like behavior when frustrated.
(B) Define grief and bereavement. Explain the types of grief.
Grief
Grief is a natural emotional response to loss, particularly the loss of a loved one. It includes a wide range of emotions, thoughts, and behaviors experienced when someone or something important is lost. It is not a disorder, but a normal part of life, allowing individuals to adjust and cope with the reality of the loss.
Types of grief
Normal (Uncomplicated) Grief
- Normal grief is the typical emotional and behavioral response to the loss of a loved one or something significant in life, where the grieving person experiences a range of emotions such as sadness, crying, anxiety, anger, guilt, and even temporary withdrawal from daily activities.
- This type of grief follows a predictable pattern of emotional processing, gradually lessens over time, and eventually allows the individual to adjust to life without the person or object lost, while still maintaining their ability to function in personal, social, and occupational roles.
Anticipatory Grief
- Anticipatory grief occurs before an actual loss takes place and is commonly seen when a loved one is terminally ill, aging, or when a major life change (like divorce or amputation) is expected.
- The grieving individual starts to emotionally prepare for the impending loss by experiencing feelings of sadness, anxiety, anger, or even guilt while the person is still alive, often resulting in a mix of hope and helplessness.
- This process may help some people cope more effectively once the loss actually occurs, but for others, it may cause prolonged emotional distress.
Complicated (Prolonged or Pathological) Grief
- Complicated grief is an intense and long-lasting form of grief that does not follow the normal course of healing and continues for more than six months or even years, severely impairing the individual’s ability to perform daily tasks.
- The person may experience persistent feelings of numbness, bitterness, disbelief, yearning for the deceased, and inability to accept the reality of the loss. This type of grief can lead to social withdrawal, depression, suicidal ideation, and may require medical or psychological treatment to help the person regain emotional balance.
Disenfranchised Grief
- Disenfranchised grief refers to grief that is not socially recognized or supported, where the loss is considered insignificant by others or is socially stigmatized. Examples include grieving over a miscarriage, the death of a pet, a partner in an extramarital or same-sex relationship, or a suicide.
- Since the loss is not acknowledged openly by society, the person may feel isolated, ashamed, or even denied the opportunity to mourn, making the grieving process more difficult and emotionally distressing.
Delayed Grief
- Delayed grief is a situation where the normal grief response is postponed, either intentionally or unintentionally, due to denial, emotional shock, or the need to manage urgent responsibilities such as caring for others or handling funeral arrangements.
- The emotional reaction may appear weeks, months, or even years later, often triggered by a related event or stressor, and can be more intense than if the grief had been expressed at the time of the loss. This unprocessed grief may lead to unexpected outbursts, physical symptoms, or psychological issues.
Chronic Grief
- Chronic grief is a type of grief in which the individual remains in a prolonged state of mourning without any significant reduction in the intensity of grief-related emotions. Unlike complicated grief, the person may still be able to function in their routine life but continues to feel profound sadness, loneliness, and longing for the deceased for years.
- The inability to move forward, frequent reminiscing, and avoidance of reminders of the loss are typical features, and without support or therapy, the individual may become emotionally stagnant or depressed.
Masked Grief
- Masked grief occurs when an individual experiences grief-related symptoms such as physical complaints (e.g., headaches, stomach pain), behavioral changes (e.g., irritability, substance abuse), or emotional disturbances, but does not recognize that these are related to the unresolved grief they are carrying.
- The grief is hidden or “masked” behind other conditions, and the person may be unaware that their suffering is due to a loss they have not fully processed. This type of grief may go unrecognized unless identified by a trained healthcare provider or counselor.
(C) Define PEM. Write the difference between kwashiorkor and marasmus.
Protein energy malnutrition
Protein Energy Malnutrition (PEM) is a nutritional disorder caused by a deficiency of protein and calories in the diet, especially in infants and young children. It commonly affects children under 5 years of age in low-income countries and results in growth failure, wasting, and weakened immunity. It includes mainly two condition kwashiorkor and marasmus.
Difference between kwashiorkor and marasmus
| Feature | Kwashiorkor | Marasmus |
|---|---|---|
| Definition | A form of severe protein deficiency with adequate or near-adequate calorie intake | A form of severe total energy deficiency, including both protein and calories |
| Age group affected | Commonly affects 1–3 years old, often after early weaning | Common in infants under 1 year, especially in cases of early cessation of breastfeeding |
| Onset | Sudden onset after infection or stress in a malnourished child | Gradual onset due to chronic starvation |
| Body weight | Weight may appear normal or slightly reduced due to edema | Weight is significantly reduced (less than 60% of expected weight) |
| Edema | Present (face, legs, feet) due to low plasma protein (hypoalbuminemia) | Absent, body appears emaciated |
| Muscle wasting | Mild to moderate, masked by edema | Severe, with visible ribs and thin limbs |
| Fat stores | Preserved, due to adequate energy intake | Depleted, due to overall energy deficiency |
| Appetite | Usually poor | Appetite is usually good |
| Skin changes | Flaky paint dermatosis, hyperpigmented, peeling patches | Skin may be dry and wrinkled, no dermatosis |
| Hair changes | Sparse, dry, depigmented hair; “flag sign” (bands of discoloration) | Thin, dry, and brittle hair without flag sign |
| Mental status | Lethargy, apathy, and irritability | Alert, irritable, and often hungry |
| Liver involvement | Fatty liver with hepatomegaly | No liver enlargement |
| Immune function | Severely compromised, prone to infections | Also compromised but less than Kwashiorkor |
| Mortality risk | High, especially if untreated or complicated by infection | Moderately high if not corrected |
Q-2 Write any four of the following (4X4-16)
(1) Under five clinic
An Under-Five Clinic is a specialized healthcare service unit designed to provide comprehensive preventive, promotive, curative, and educational health services to children below the age of five years. Its main objective is to monitor child growth and development, prevent and manage childhood illnesses, promote proper nutrition, ensure complete immunization, and educate mothers or caregivers to reduce child morbidity and mortality.
Objectives of Under-Five Clinic
- To ensure regular growth monitoring and early detection of malnutrition.
- To provide immunization services according to the national schedule.
- To offer early diagnosis and treatment of common childhood illnesses.
- To guide parents on proper nutrition and feeding practices.
- To provide family planning advice and promote maternal health education.
- To reduce the incidence of communicable and preventable diseases.
Components / Services of Under-Five Clinic
1️⃣ Growth Monitoring and Promotion
- Regularly measure and record weight, height/length, and head circumference.
- Use WHO Growth Charts or color-coded growth monitoring charts for easy identification of nutritional status.
- Monitor for failure to thrive, undernutrition, overweight, and obesity.
- Provide counseling to mothers on the importance of regular growth checks.
- Identify and manage children with Protein-Energy Malnutrition (PEM) early.
2️⃣ Immunization Services
- Administer vaccines as per National Immunization Schedule.
- Maintain the cold chain to ensure vaccine potency.
- Educate parents about the importance of completing immunization schedules and possible side effects.
- Conduct catch-up immunization sessions for defaulters.
- Monitor and manage any adverse events following immunization (AEFI).
3️⃣ Nutritional Services
- Counsel mothers on exclusive breastfeeding for the first 6 months.
- Guide on proper weaning practices starting at 6 months and balanced complementary feeding.
- Provide micronutrient supplementation like iron, folic acid, vitamin A, and zinc.
- Distribute deworming tablets periodically to prevent worm infestations.
- Educate mothers about low-cost, locally available nutritious foods to prevent malnutrition.
4️⃣ Curative Services
- Diagnose and manage common illnesses like diarrhea, acute respiratory infections, anemia, skin infections, and fever.
- Provide ORS and zinc supplementation for diarrhea cases.
- Early identification and management of pneumonia and other respiratory conditions.
- Administer first aid and provide referrals for serious conditions.
5️⃣ Health Education for Mothers and Caregivers
- Educate about personal hygiene, safe drinking water, and environmental sanitation to prevent infections.
- Counsel mothers on proper handwashing techniques to reduce the risk of diarrhea and respiratory infections.
- Provide information on recognizing danger signs in children (e.g., high fever, fast breathing, lethargy).
- Promote awareness about early child stimulation for cognitive development.
6️⃣ Family Welfare and Counseling Services
- Offer counseling on family planning methods suitable for the mother’s health and age.
- Educate about birth spacing benefits for maternal and child health.
- Provide support for postnatal care and breastfeeding counseling.
- Identify and refer mothers with postpartum depression or emotional distress.
- Promote male involvement in child health and family planning.
7️⃣ Developmental Monitoring
- Regularly assess milestones like motor, language, social, and cognitive development.
- Use developmental screening tools to identify delays early.
- Counsel parents about stimulating play activities and interaction for brain development.
- Follow up on children at risk of intellectual disabilities or learning problems.
8️⃣ Referral Services
- Recognize conditions requiring higher-level care like severe malnutrition, congenital anomalies, or severe infections.
- Facilitate timely referral to tertiary care centers or specialists.
- Ensure proper documentation and communication during referral.
- Encourage parents to comply with referral advice and attend follow-up visits.
9️⃣ Record Keeping and Follow-Up
- Maintain accurate and updated records of growth monitoring, immunizations, nutritional interventions, and illness management.
- Use Mother and Child Protection (MCP) cards for recording health data.
- Track defaulters and conduct home visits if necessary for follow-up.
- Prepare regular reports for health authorities to improve child health programs.
Role of the Nurse in Under-Five Clinic
1️⃣ Conduct Regular Growth Monitoring
Accurately measure and record the child’s weight, height, and head circumference, and plot them on growth charts to assess normal growth patterns.
2️⃣ Administer Immunizations Safely
Ensure timely vaccination as per the national immunization schedule, maintain cold chain management, and monitor for any post-vaccination reactions.
3️⃣ Provide Nutritional Counseling
Educate mothers and caregivers about breastfeeding, weaning, and the importance of balanced nutrition, including iron, vitamin A, and other micronutrients.
4️⃣ Conduct Health Education Sessions
Educate parents on hygiene, sanitation, prevention of infectious diseases, and common health issues affecting children under five.
5️⃣ Early Detection of Malnutrition and Illnesses
Identify children with signs of malnutrition, developmental delays, and common childhood illnesses such as respiratory infections, diarrhea, and anemia, and provide prompt management or referrals.
6️⃣ Monitor Developmental Milestones
Assess the child’s developmental progress, including motor, cognitive, and social skills, and counsel parents if any delays are observed.
7️⃣ Maintain Accurate Records
Keep systematic records of growth monitoring, immunization status, nutritional counseling, and any treatments provided for proper follow-up.
8️⃣ Family Planning Counseling
Educate mothers about spacing of children and provide information on available family planning methods to promote maternal and child health.
9️⃣ Promote Exclusive Breastfeeding
Encourage mothers to exclusively breastfeed their infants for the first six months and continue breastfeeding along with complementary foods thereafter.
🔟 Manage Minor Ailments and Provide First Aid
Provide curative services for common health issues and ensure early management of minor illnesses to prevent complications.
1️⃣1️⃣ Coordinate with Community Health Workers
Work in collaboration with ASHAs, ANMs, and anganwadi workers to ensure follow-up and community-level interventions for under-five children.
1️⃣2️⃣ Ensure Safe Waste Disposal
Follow biomedical waste management protocols during immunization and curative services to maintain clinic hygiene and prevent infections.
1️⃣3️⃣ Support and Counsel Parents Emotionally
Address parental concerns, provide emotional support, and reduce anxiety related to child illnesses or developmental issues.
(2) KMC
Definition
Kangaroo Mother Care (KMC) is a method of caring for preterm and low birth weight infants through skin-to-skin contact, exclusive breastfeeding, and early discharge with follow-up, which helps maintain the baby’s body temperature, promotes bonding, and improves survival rates.
Objectives of KMC
- To provide a natural thermal environment for the baby through skin-to-skin contact.
- To promote and support exclusive breastfeeding.
- To enhance emotional bonding between mother and baby.
- To reduce the risk of hypothermia, infections, and mortality in low birth weight infants.
- To encourage early discharge and community-based care with proper follow-up.
Components of Kangaroo Mother Care (KMC)
1️⃣ Skin-to-Skin Contact
Continuous and prolonged direct skin-to-skin contact between the mother (or other caregiver) and the baby.
Helps maintain the baby’s body temperature, stabilizes heart and respiratory rates, and promotes bonding.
2️⃣ Exclusive Breastfeeding
Encourages frequent and direct breastfeeding to ensure optimal nutrition and hydration.
Stimulates breast milk production and strengthens the baby’s immunity through maternal antibodies.
3️⃣ Early Discharge and Proper Follow-Up
Promotes early discharge from hospital when the baby is stable, with regular follow-up visits.
Follow-up includes monitoring the baby’s weight gain, feeding adequacy, growth, and developmental milestones.
Procedure of KMC
1️⃣ Ensure that the mother is healthy, willing, and properly counseled about the process.
2️⃣ Dress the baby in a diaper and cap and place him/her upright between the mother’s breasts in direct skin-to-skin contact.
3️⃣ Cover both mother and baby with a warm cloth or KMC wrap to maintain warmth.
4️⃣ Continue KMC for as many hours as possible each day, ideally minimum 6–8 hours daily.
5️⃣ Encourage exclusive breastfeeding whenever possible and monitor the baby’s feeding and weight gain.
6️⃣ Continue KMC until the baby reaches a weight of 2500 grams or shows stable growth.
Advantages of KMC
- Maintains the baby’s body temperature and prevents hypothermia.
- Enhances breastfeeding success and improves weight gain.
- Reduces the risk of hospital-acquired infections.
- Promotes early discharge from the hospital.
- Improves emotional bonding between mother and baby.
- Decreases neonatal morbidity and mortality.
Role of Nurse in Kangaroo Mother Care (KMC)
1️⃣ Educating and Counseling Mothers
The nurse plays a vital role in educating mothers and families about the importance, benefits, and techniques of KMC.
Provide psychological support to mothers who may feel anxious or insecure about handling preterm or low birth weight babies.
2️⃣ Preparation and Support for KMC
Assist the mother in maintaining personal hygiene and preparing for safe KMC practice.
Help the mother in proper positioning of the baby for effective skin-to-skin contact, ensuring the airway remains open and the baby is comfortable.
3️⃣ Monitoring Baby’s Condition
Regularly monitor the baby’s temperature, heart rate, respiratory rate, and oxygen saturation during KMC.
Observe for any signs of distress, hypothermia, or feeding difficulties.
4️⃣ Promoting Exclusive Breastfeeding
Encourage and assist mothers to initiate and maintain exclusive breastfeeding, offering support with latching and correct breastfeeding positions.
Educate mothers about the importance of frequent feeding to ensure adequate nutrition.
5️⃣ Ensuring Infection Control
Instruct mothers on proper hand hygiene before handling the baby.
Maintain a clean environment to reduce the risk of infections.
6️⃣ Documentation and Record Keeping
Accurately record the duration and frequency of KMC sessions.
Document the baby’s weight gain, feeding patterns, and vital signs to assess progress.
7️⃣ Coordination of Follow-Up Care
Ensure parents understand the importance of follow-up visits after discharge to monitor the baby’s growth and development.
Provide reminders for immunizations and growth monitoring schedules.
8️⃣ Involving Family Members
Encourage father and other family members to participate in KMC if the mother is unavailable, ensuring continuity of care.
9️⃣ Managing Complications Promptly
Recognize early signs of hypothermia, breathing difficulties, or poor feeding and take immediate action or refer to a higher center if necessary.
(3) Temper tantrum
Definition
A temper tantrum is an emotional outburst commonly seen in young children, characterized by behaviors such as crying, screaming, kicking, hitting, holding breath, or throwing objects, usually as a response to unmet needs, frustration, or inability to express emotions verbally. Typically seen between 1 to 4 years of age (Peak at 2–3 years).
Causes of Temper Tantrums
- Frustration or unmet desires (e.g., wanting a toy or attention).
- Hunger, fatigue, or discomfort.
- Desire for independence but lack of physical or verbal skills to express it.
- Attention-seeking behavior.
- Inconsistent discipline or parenting style.
- Stressful environment or sudden changes in routine.
Clinical manifestation
- Loud crying or screaming
- Hitting, kicking, or biting
- Throwing or breaking objects
- Rolling on the floor or stamping feet
- Breath-holding spells (in some cases)
- Refusal to follow instructions
- Clinging to caregivers intermittently
- Facial redness and restlessness
Management of Temper Tantrums
1️⃣ Remain Calm and Patient
Caregivers should control their emotions, respond calmly, and avoid shouting or physical punishment, as it may worsen the behavior.
2️⃣ Ignore Minor Tantrums
If the tantrum does not involve self-harm or danger, ignoring it helps prevent reinforcement of negative behavior.
3️⃣ Positive Reinforcement
Praise and reward the child for positive behavior and cooperation, encouraging desired actions through appreciation.
4️⃣ Provide Limited Choices
Offer simple choices to give the child a sense of control (e.g., “Would you like juice or milk?”), helping reduce frustration.
5️⃣ Use Distraction Techniques
Divert the child’s attention to a favorite toy, game, or activity before the tantrum escalates.
6️⃣ Establish Clear Rules and Consistent Discipline
Set firm, consistent boundaries and consequences for unacceptable behavior, ensuring the child understands expectations.
7️⃣ Maintain a Structured Routine
Follow a consistent daily schedule for meals, naps, and play to reduce unpredictability and irritability.
8️⃣ Ensure Basic Needs Are Met
Check if the child is hungry, tired, bored, or overstimulated, as these factors often trigger tantrums.
9️⃣ Teach Simple Communication Skills
Help children express their needs and emotions using words or gestures, especially in younger children with limited vocabulary.
🔟 Apply the Time-Out Technique
For severe or prolonged tantrums, place the child in a quiet, safe area for a short time to calm down and reflect.
1️⃣1️⃣ Model Appropriate Behavior
Demonstrate calm and respectful behavior in front of the child to encourage imitation of positive social responses.
1️⃣2️⃣ Avoid Triggers When Possible
Identify and avoid known situations or environments that commonly lead to tantrums.
1️⃣3️⃣ Reassure the Child After the Tantrum Ends
Comfort the child once they calm down, reinforcing that they are loved but that tantrums are not an acceptable way to express needs.
1️⃣4️⃣ Seek Professional Help if Necessary
If tantrums are frequent, severe, or associated with developmental concerns, refer the child for behavioral assessment or counseling.
Nurse’s Role in Managing Temper Tantrums
1️⃣ Assess the Child’s Behavior
Carefully observe and assess the frequency, duration, and triggers of temper tantrums to understand underlying causes such as hunger, fatigue, frustration, or emotional distress.
2️⃣ Educate Parents and Caregivers
Provide counseling to parents on the normal developmental phase of tantrums and guide them on how to handle such situations calmly and effectively.
3️⃣ Promote Positive Parenting Techniques
Teach caregivers the importance of positive reinforcement, consistent discipline, and the avoidance of physical punishment.
4️⃣ Encourage Consistent Routine
Advise parents to establish regular schedules for meals, sleep, play, and rest to reduce the likelihood of tantrums caused by fatigue or hunger.
5️⃣ Teach Distraction and Redirection Techniques
Guide parents on how to distract the child before tantrums escalate by offering alternative activities or engaging the child in play.
6️⃣ Monitor for Developmental or Behavioral Disorders
Assess if tantrums are excessive or prolonged and recommend further evaluation if there are signs of behavioral or developmental delays.
7️⃣ Demonstrate the Time-Out Technique
Educate caregivers on how to apply time-out methods appropriately and safely without harming the child emotionally or physically.
8️⃣ Provide Emotional Support to Parents
Offer reassurance to anxious or overwhelmed parents and support them in coping with challenging child behaviors.
9️⃣ Model Calm and Positive Behavior
During clinical interactions, demonstrate calm communication and effective behavior management techniques for parents to observe and learn.
(4) Accidents among children
Definition
Accidents among children refer to unintentional injuries that occur suddenly and can cause physical harm, disability, or even death. These incidents are a major cause of morbidity and mortality in children worldwide.
Common Causes of Accidents in Children
Falls : From beds, stairs, balconies, playground equipment, or while learning to walk.
Burns and Scalds : Due to hot liquids, open flames, electrical appliances, or fireworks.
Road Traffic Accidents (RTA) : As pedestrians, cyclists, or passengers without proper restraints.
Poisoning : Accidental ingestion of medications, household cleaning agents, kerosene, or pesticides.
Drowning : In bathtubs, buckets, water tanks, swimming pools, or open water bodies.
Choking and Suffocation : Due to small toys, coins, nuts, or plastic bags obstructing airways.
Cuts and Lacerations : From sharp objects like knives, scissors, or glass.
Electrical Injuries : From uncovered sockets or exposed electrical wires.
Animal Bites and Stings : Dog bites, snake bites, insect stings, or bee attacks.
Foreign Body Aspiration : Inhalation of small objects like beads, food particles, or buttons into the respiratory tract.
Preventive Measures
1️⃣ Ensure Adequate Supervision
- Always supervise young children, especially during playtime, near water bodies, and in the kitchen or bathroom.
- Assign a responsible adult when parents are unavailable.
- Be extra vigilant during high-risk activities like climbing stairs, bathing, or eating.
2️⃣ Create a Safe Home Environment
- Install window guards and safety grills to prevent falls from heights.
- Use child safety gates on staircases and balconies.
- Ensure floors are dry and non-slippery to prevent slips and falls.
- Keep sharp objects, knives, scissors, and glass items out of reach of children.
- Use corner protectors on sharp-edged furniture.
3️⃣ Prevent Burns and Scalds
- Keep hot liquids, cooking appliances, and heated objects away from children.
- Turn pot handles inward while cooking and avoid carrying hot drinks near children.
- Keep matches, lighters, and fireworks out of children’s reach.
- Educate children about the dangers of fire and hot objects.
4️⃣ Prevent Poisoning
- Store medicines, cleaning agents, insecticides, and chemicals in locked cabinets.
- Use child-resistant caps on medicine bottles.
- Avoid transferring harmful liquids like kerosene into drinking water bottles.
- Educate children never to taste unknown substances.
5️⃣ Prevent Drowning
- Never leave children unattended near bathtubs, water tanks, buckets, swimming pools, or open water bodies.
- Cover water tanks and pits properly.
- Enroll children in basic swimming lessons if age-appropriate.
- Use life jackets and floatation devices when near water.
6️⃣ Prevent Choking and Suffocation
- Keep small toys, coins, buttons, peanuts, and beads out of reach of infants and toddlers.
- Avoid giving small, hard foods like nuts and popcorn to very young children.
- Supervise children while eating and discourage talking or playing during meals.
- Keep plastic bags and balloons away to prevent suffocation.
7️⃣ Road Safety Measures
- Teach children basic road safety rules like looking both ways before crossing and using pedestrian crossings.
- Ensure children use car seats, seat belts, and helmets when traveling.
- Never allow children to sit in the front seat of vehicles without proper restraints.
8️⃣ Electrical Safety
- Install safety covers on electrical outlets.
- Keep electrical appliances and cords out of reach.
- Educate children not to touch electrical switches and devices with wet hands.
9️⃣ Prevent Animal Bites and Stings
- Teach children to avoid playing with stray animals.
- Keep pets vaccinated, especially against rabies.
- Ensure the living environment is free from mosquito breeding sites and keep children protected from insect bites.
🔟 Education and Awareness
- Educate children about personal safety and avoiding dangerous situations.
- Conduct safety awareness programs in schools and communities.
- Encourage parents to learn basic first aid measures and keep emergency numbers handy.
Role of Nurse in Prevention and Management of Accidents Among Children
1️⃣ Health Education to Parents and Caregivers
Educate families about common household hazards and how to create a safe environment for children.
Counsel parents on age-appropriate supervision and preventive practices during high-risk activities like bathing and outdoor play.
2️⃣ Promoting Environmental Safety
Assess home environments for potential dangers such as unprotected staircases, open water tanks, uncovered electrical outlets, and sharp objects.
Suggest modifications like using corner protectors, childproof locks, window guards, and anti-slip mats.
3️⃣ First Aid Training
Provide demonstrations on basic first aid techniques for burns, cuts, fractures, choking, and poisoning.
Educate parents on the importance of keeping a well-stocked first aid kit at home.
4️⃣ Community Awareness Programs
Organize community-level awareness campaigns on topics such as road safety, drowning prevention, safe handling of fireworks, and animal bite prevention.
5️⃣ Early Identification of High-Risk Families
Identify families living in unsafe environments or practicing neglectful parenting and collaborate with social services for necessary interventions.
6️⃣ Counseling on Use of Safety Devices
Educate about the proper use of car seats, seat belts, helmets, and child-resistant packaging for medications and chemicals.
7️⃣ Emergency Preparedness
Ensure that emergency contact numbers are accessible to parents and caregivers, and teach them how to respond promptly in case of an accident.
8️⃣ Monitoring and Reporting Accidental Injuries
Maintain accurate records of accidental injuries in children and report cases of frequent accidents for further investigation.
(5) Preventive pediatric
Definition
Preventive Pediatrics is a branch of pediatrics focused on the prevention of diseases, promotion of health, and early detection of developmental abnormalities in children from birth through adolescence. It aims to ensure optimal physical, mental, and social well-being of children.
Objectives of Preventive Pediatrics
- Prevent common childhood illnesses and nutritional deficiencies.
- Promote healthy growth and development.
- Educate parents and caregivers on child health and safety.
- Prevent disability and ensure early detection of health problems.
- Reduce childhood morbidity and mortality rates.
Components of Preventive Pediatrics
1️⃣ Antenatal Preventive Care
- Focuses on maternal health during pregnancy to ensure a healthy newborn.
- Includes regular antenatal check-ups, immunization (e.g., Tetanus toxoid), balanced diet, and folic acid supplementation.
- Prevention of congenital anomalies through proper maternal care.
2️⃣ Postnatal and Neonatal Preventive Care
- Early initiation and promotion of exclusive breastfeeding for the first 6 months.
- Administration of Vitamin K injection to prevent bleeding disorders.
- Early screening for congenital disorders (e.g., congenital hypothyroidism, hearing tests).
3️⃣ Infant and Child Preventive Care
- Immunization as per National Immunization Schedule to protect against preventable diseases.
- Regular growth monitoring and developmental screening.
- Nutritional counseling to prevent malnutrition and micronutrient deficiencies.
- Promotion of safe hygiene and sanitation practices.
4️⃣ Adolescent Preventive Care
- Health education on puberty changes, personal hygiene, and reproductive health.
- Counseling on mental health, substance abuse prevention, and healthy lifestyle practices.
- Vaccination against HPV and hepatitis B as per guidelines.
Preventive Measures in Pediatric Practice
Immunization : Timely vaccination against diseases like polio, measles, diphtheria, pertussis, and tetanus.
Growth and Development Monitoring : Regular assessment using growth charts and milestone evaluations.
Nutrition Promotion : Educating about balanced diets, breastfeeding, and proper weaning practices.
Injury and Accident Prevention : Creating safe environments and educating caregivers about accident prevention.
Health Education : Teaching children and families about hygiene, sanitation, oral health, and personal safety.
Early Detection of Disorders : Routine screenings for vision, hearing, anemia, and congenital anomalies.
Role of Nurse in Preventive Pediatrics
1️⃣ Health Education to Parents and Caregivers
Educate parents about the importance of exclusive breastfeeding, balanced nutrition, immunization schedules, hygiene, and safe parenting practices.
Provide counseling on the prevention of common childhood diseases, malnutrition, and the importance of early developmental stimulation.
2️⃣ Promoting and Administering Immunizations
Ensure that children receive all vaccines as per the National Immunization Schedule (NIS).
Maintain proper cold chain management for vaccine storage and handle Adverse Events Following Immunization (AEFI) effectively.
3️⃣ Growth and Development Monitoring
Regularly assess and record children’s weight, height, head circumference, and developmental milestones.
Identify early signs of growth faltering, malnutrition, or developmental delays and refer cases as needed.
4️⃣ Screening and Early Detection
Participate in health screening programs for congenital anomalies, vision and hearing problems, anemia, and dental caries.
Facilitate early diagnosis and timely intervention to prevent long-term complications.
5️⃣ Nutritional Counseling
Guide mothers on exclusive breastfeeding for the first 6 months and appropriate weaning practices after 6 months.
Educate on micronutrient supplementation (Iron, Vitamin A, and Iodine) and encourage the use of locally available nutritious foods.
6️⃣ Accident and Injury Prevention
Advise families on creating safe home environments and supervise play areas to prevent common childhood accidents like falls, burns, poisoning, and drowning.
Educate about the use of safety devices such as helmets, car seats, and safety gates.
7️⃣ Promoting Adolescent Health
Conduct counseling sessions on personal hygiene, reproductive health, menstrual hygiene management, prevention of substance abuse, and mental health support for adolescents.
8️⃣ Organizing Community Health Programs
Participate in community outreach activities like Pulse Polio campaigns, school health programs, and anemia control programs.
Create awareness about the prevention of infectious diseases and sanitation practices.
9️⃣ Record Keeping and Follow-Up
Maintain accurate records of immunization, growth monitoring, developmental assessments, and follow-up visits.
Track defaulters and ensure children receive missed vaccinations or nutritional interventions.
🔟 Advocacy and Policy Support
Advocate for child-friendly health policies and participate in developing and implementing child health programs at the community level.
Q-3 Deline (any four) (4X2-8)
1. Weaning
Weaning is the gradual process of introducing semi-solid and solid foods to an infant’s diet while reducing and eventually stopping breastfeeding or bottle feeding, usually starting around 6 months of age, when breast milk alone is no longer sufficient to meet the baby’s nutritional needs.
2. Hirchsprung’s disease
Hirschsprung’s disease is a congenital disorder characterized by the absence of ganglion cells in the distal colon or rectum, leading to impaired intestinal motility and functional intestinal obstruction.
3. Neonatal resuscitation
Neonatal resuscitation is the immediate set of life-saving interventions provided to a newborn who does not initiate or maintain spontaneous breathing at birth. It includes steps to establish airway, support breathing, and circulation.
4. Foreign body aspiration
Foreign body aspiration is the inhalation of any object (solid or liquid) into the respiratory tract, typically into the larynx, trachea, or bronchus, causing partial or complete airway obstruction. It is a common emergency in children, especially between 6 months and 5 years.
5. IMNCI
IMNCI stands for Integrated Management of Neonatal and Childhood Illness.
It is a comprehensive child health strategy developed by WHO and UNICEF, adapted for India by the Government of India, to reduce mortality, morbidity, and disability in children under five years of age, especially from preventable and treatable illnesses.
SECTION-II
Q.4 A) 6 year old Child adrhitted in the Hospital due to rheumatic fever
(a) Write the clinical manifestations of the rheumatic fever according to Jone’s modified criteria. (6)
The Jones Criteria classify the manifestations into Major and Minor Criteria, supported by evidence of a recent Group A Streptococcal Infection.
Major Criteria (Primary Clinical Manifestations)
1️⃣ Carditis (Pancarditis)
- Involvement of the heart including endocarditis, myocarditis, and pericarditis.
- Clinical signs: Tachycardia, new or changing heart murmurs (especially mitral regurgitation), pericardial friction rub, and signs of heart failure (dyspnea, edema).
2️⃣ Polyarthritis (Migratory)
- Painful, swollen, and red large joints (commonly knees, ankles, elbows, and wrists).
- Migratory in nature; inflammation subsides in one joint and moves to another.
3️⃣ Chorea (Sydenham’s Chorea)
- Involuntary, purposeless, jerky movements primarily involving the face, hands, and feet.
- Emotional lability and muscle weakness are often present.
4️⃣ Erythema Marginatum
- Non-itchy, pink, or red rash with serpiginous (wavy) margins, commonly seen on the trunk and proximal limbs.
- Rash is transient and often unnoticed.
5️⃣ Subcutaneous Nodules
- Painless, firm nodules over bony prominences or tendons (e.g., elbows, knees, scalp, spine).
- Typically associated with severe carditis.
Minor criteria
✅ Clinical Criteria
1️⃣ Fever
- ≥38.5°C (101.3°F) in high-risk populations.
- ≥38.0°C (100.4°F) in low-risk populations.
2️⃣ Arthralgia
- Joint pain without signs of inflammation (swelling or redness).
- Note: In high-risk populations, polyarthralgia can be considered equivalent to major criteria.
✅ Laboratory Criteria
3️⃣ Elevated Acute Phase Reactants
- Erythrocyte Sedimentation Rate (ESR): ≥30 mm/hour.
- C-Reactive Protein (CRP): ≥3 mg/dL or 30 mg/L.
4️⃣ Prolonged PR Interval on ECG
- Indicates first-degree heart block.
- Must be age-appropriate and not explained by other conditions.
Note
Diagnosis requires 2 Major Criteria or 1 Major + 2 Minor Criteria, along with evidence of a recent streptococcal infection.
(b) Discuss the management of this patient. (6)
1️⃣ The child should be hospitalized if there are severe symptoms, especially the presence of carditis, congestive heart failure, or Sydenham’s chorea, and strict bed rest must be maintained during the acute phase to minimize cardiac workload and prevent complications.
2️⃣ To eliminate the underlying Group A Streptococcal infection, a single dose of intramuscular Benzathine Penicillin G should be administered at a dosage appropriate for the child’s weight, and if the child is allergic to penicillin, alternative antibiotics like Azithromycin or Erythromycin should be prescribed.
3️⃣ For controlling the inflammatory manifestations such as fever and arthritis, the child should be given high-dose Aspirin (80–100 mg/kg/day in divided doses) until the fever and joint symptoms subside, after which the dose should be gradually tapered based on clinical response.
4️⃣ In cases where the child presents with severe carditis or symptoms of heart failure, the administration of corticosteroids such as Prednisolone at a dose of 1–2 mg/kg/day is indicated, and the steroids should be tapered gradually once clinical improvement is noted to avoid relapse.
5️⃣ If the child develops Sydenham’s chorea, supportive care and reassurance should be provided to both the child and parents, and in severe cases, medications like Sodium Valproate or Carbamazepine should be prescribed to control involuntary movements, with Haloperidol being considered if other medications fail.
6️⃣ In the presence of cardiac failure, the child should be managed with appropriate heart failure treatment including diuretics like Furosemide to reduce fluid overload, and Digoxin or ACE inhibitors may be added to improve cardiac function if needed under close medical supervision.
7️⃣ After the acute phase, the child should be started on secondary prophylaxis with Benzathine Penicillin G intramuscular injections every 3 to 4 weeks to prevent recurrences, and the duration of prophylaxis should be determined based on whether carditis or residual heart disease is present.
8️⃣ The nurse should provide emotional support and counseling to the child and family, educate them about the importance of regular prophylaxis and follow-up, and ensure that parents understand the need for long-term antibiotic injections to prevent future attacks.
9️⃣ During hospitalization, the nurse should also monitor the child’s vital signs regularly, observe for signs of cardiac decompensation such as increased respiratory rate, edema, or cyanosis, administer all medications accurately as per the prescribed schedule, and maintain proper documentation.
🔟 Nutritional support should be ensured by encouraging the child to take a well-balanced, high-calorie, and high-protein diet, and the nurse should provide instructions for maintaining good hygiene to prevent further infections that could precipitate a relapse of rheumatic fever.
Nursing Management of Rheumatic Fever
1️⃣ Monitor vital signs frequently, including temperature, heart rate, respiratory rate, and blood pressure to detect early signs of deterioration.
2️⃣ Ensure the child maintains complete bed rest during the acute phase to reduce cardiac workload and prevent exacerbation of symptoms.
3️⃣ Administer antibiotics, anti-inflammatory medications, and corticosteroids as prescribed and monitor for possible drug side effects such as gastric irritation or bleeding.
4️⃣ Observe for signs of congestive heart failure, including breathlessness, facial puffiness, pedal edema, decreased urine output, and cyanosis.
5️⃣ Provide a calm and safe environment, especially for children with Sydenham’s chorea, to prevent accidental falls or injuries from involuntary movements.
6️⃣ Encourage the intake of a nutritious, high-calorie, and high-protein diet to promote tissue repair and recovery, and monitor daily weight and hydration status.
7️⃣ Educate parents about the importance of adhering to the complete antibiotic course and the necessity of long-term secondary prophylaxis with regular Benzathine Penicillin injections to prevent recurrence.
8️⃣ Advise parents to recognize early signs of recurrence, such as joint pains, fever, shortness of breath, or unusual body movements, and seek immediate medical attention if observed.
9️⃣ Provide emotional and psychological support to relieve the child’s anxiety and fear, especially in cases of prolonged hospitalization or chorea symptoms.
🔟 Assist the child with activities of daily living, ensuring energy conservation while gradually encouraging mild activities during the recovery phase.
1️⃣1️⃣ Educate parents on maintaining good hygiene practices to prevent recurrent streptococcal infections, including regular handwashing and avoiding contact with infected individuals.
1️⃣2️⃣ Ensure that the child receives all age-appropriate immunizations as per schedule to strengthen immunity and prevent other infections.
1️⃣3️⃣ Arrange for regular follow-up visits and educate parents on the importance of continuous health monitoring and echocardiography if advised by the physician.
1️⃣4️⃣ Provide guidance on proper storage of medications and maintaining a safe home environment to prevent accidental drug intake or injuries.
1️⃣5️⃣ Maintain accurate and up-to-date records of medication administration, vital signs, laboratory investigations, and the child’s progress to assist in planning ongoing care.
Q-5 Write on the following (any four) (4X5=20)
1. Leukemia
Definition
Leukemia is a group of malignant disorders involving the blood-forming tissues of the body, particularly the bone marrow and lymphatic system, characterized by the uncontrolled proliferation of abnormal white blood cells (leukocytes).
Classification of Leukemia
Leukemia is broadly classified based on the speed of progression and the type of blood cells involved, resulting in four major types.
Acute Lymphoblastic Leukemia (ALL)
It is a rapidly progressing cancer that originates from immature lymphoid cells, commonly affecting children, and is characterized by the accumulation of lymphoblasts in the bone marrow and blood.
Acute Myeloid Leukemia (AML)
It is an aggressive form of leukemia that arises from immature myeloid cells, frequently occurring in adults, and leads to the rapid production of non-functional myeloblasts that suppress normal hematopoiesis.
Chronic Lymphocytic Leukemia (CLL)
It is a slowly progressing malignancy that originates from mature-looking but dysfunctional B lymphocytes, usually affecting older adults, and is often discovered incidentally through routine blood tests.
Chronic Myeloid Leukemia (CML)
It is a slowly progressing leukemia of the myeloid lineage, commonly associated with a genetic abnormality known as the Philadelphia chromosome, which leads to the overproduction of mature and semi-mature granulocytes.
Etiology (Causes)
- Genetic mutations (e.g., Philadelphia chromosome in CML)
- Radiation exposure
- Chemical exposure (e.g., benzene)
- Chemotherapy drugs
- Viral infections (e.g., HTLV-1)
- Genetic disorders (e.g., Down syndrome)
Pathophysiology of Leukemia
- Genetic mutation occurs in bone marrow stem cells.
- Leads to uncontrolled production of abnormal WBCs (leukemic blasts).
- These abnormal cells fail to mature and accumulate in the bone marrow.
- Normal cell production (RBCs, platelets, normal WBCs) is suppressed.
- This lead to Anemia (due to ↓ RBCs), Bleeding (due to ↓ platelets), Infections (due to ↓ functional WBCs)
- Leukemic cells may spread to other organs (e.g., CNS, liver, spleen).
- Results in organ enlargement, bone pain, fever, and immune dysfunction.
Clinical Manifestations
- Fatigue and weakness
- Fever and infections
- Pallor (pale skin)
- Bleeding and bruising – petechiae, epistaxis, bleeding gums (from thrombocytopenia)
- Bone and joint pain
- Weight loss and appetite loss
- Swollen lymph nodes
- Enlarged spleen and liver
- Night sweats and chills
- Headache, vomiting, blurred vision
Diagnostic Evaluation
- History collection
- Physical examination
- Complete blood count (CBC)
- Peripheral blood smear
- Bone marrow aspiration and biopsy
- Cytogenetic studies
- Flow cytometry
- Lumbar puncture
Management of leukemia
General Management
The child or adult diagnosed with leukemia should be hospitalized during the acute phase of illness or whenever complications arise, such as severe infections, bleeding tendencies, or chemotherapy-induced side effects, and the healthcare team must provide continuous monitoring and supportive care to stabilize the patient’s condition.
Medical Management
✅ A. Chemotherapy
The primary treatment for leukemia involves the administration of multi-phase chemotherapy regimens, beginning with the induction phase to achieve remission, followed by the consolidation or intensification phase to destroy any residual cancer cells, and finally, a maintenance phase to prevent relapse, using various chemotherapeutic agents such as Vincristine, Methotrexate, Cyclophosphamide, Cytarabine, and Doxorubicin, adjusted according to the type and severity of leukemia.
✅ B. Radiation Therapy
Radiation therapy is employed in cases where there is central nervous system involvement or localized tumor masses, and it is often used alongside chemotherapy to enhance treatment effectiveness, particularly in cases of acute lymphoblastic leukemia with CNS infiltration.
✅ C. Targeted Therapy
In specific leukemia types like Chronic Myeloid Leukemia (CML) and Philadelphia chromosome-positive Acute Lymphoblastic Leukemia (ALL), targeted therapy using agents such as Imatinib mesylate, a tyrosine kinase inhibitor, is administered to block abnormal cell signaling pathways and control disease progression.
✅ D. Immunotherapy and Biological Therapy
For certain resistant or relapsed cases, advanced treatment options like Monoclonal Antibody Therapy (e.g., Rituximab) and newer technologies such as CAR-T cell therapy are used to boost the immune system’s ability to fight leukemia cells effectively.
✅ E. Hematopoietic Stem Cell Transplant (HSCT)
In high-risk or relapsed cases of leukemia, especially AML and CML, a hematopoietic stem cell transplant (bone marrow transplant) may be performed after intensive chemotherapy or radiation therapy to replace the damaged bone marrow with healthy donor cells, offering a potential cure.
Nursing management
1️⃣ Monitor vital signs and laboratory parameters frequently to detect early signs of infection, bleeding tendencies, anemia, and electrolyte imbalances.
2️⃣ Administer chemotherapy, antibiotics, analgesics, and antiemetics accurately as prescribed, and observe closely for side effects like nausea, vomiting, bone marrow suppression, alopecia, and mucositis.
3️⃣ Implement strict infection prevention protocols, including maintaining a sterile environment, practicing hand hygiene, using personal protective equipment (PPE), and enforcing reverse isolation for neutropenic patients.
4️⃣ Assess for bleeding manifestations, such as petechiae, purpura, hematuria, melena, and gum bleeding, and apply bleeding precautions by avoiding injections, minimizing invasive procedures, and handling the child gently.
5️⃣ Promote nutritional support by encouraging a high-protein, high-calorie, vitamin-rich diet, providing small and frequent meals, and arranging for parenteral or enteral nutrition if the child cannot tolerate oral feeding.
6️⃣ Encourage adequate fluid intake to prevent dehydration and assist in flushing out toxins from chemotherapy, unless restricted due to complications like renal impairment.
7️⃣ Provide emotional and psychological support to reduce anxiety and fear related to prolonged hospitalization, physical changes, and treatment side effects, using therapeutic communication techniques.
8️⃣ Educate parents and caregivers on recognizing danger signs such as persistent fever, unexplained bruising, extreme fatigue, and breathlessness, and advise them on when to seek immediate medical attention.
9️⃣ Support the child in managing body image disturbances by preparing them for alopecia and providing options like scarves, caps, or wigs, and encouraging acceptance of temporary changes.
🔟 Ensure oral hygiene to prevent mucositis by using soft toothbrushes, antiseptic mouthwashes, and avoiding spicy or acidic foods that may irritate the oral mucosa.
1️⃣1️⃣ Monitor for tumor lysis syndrome by assessing for signs like muscle cramps, arrhythmias, and altered urine output, and ensure appropriate hydration and administration of medications like Allopurinol.
1️⃣2️⃣ Assist the child with activities of daily living to conserve energy and prevent fatigue while promoting gradual mobilization during recovery phases.
1️⃣3️⃣ Coordinate with multidisciplinary teams, including oncologists, dietitians, psychologists, and social workers, to provide holistic care.
1️⃣4️⃣ Maintain accurate and detailed documentation of all nursing interventions, medication administration, fluid balance, and patient responses to facilitate continuity of care and treatment evaluation.
2. Spinal bifida
Definition
Spina bifida is a congenital neural tube defect characterized by the incomplete closure of the vertebral column and spinal cord during fetal development, leading to varying degrees of spinal and neurological abnormalities.
Causes of Spina Bifida
- Folic acid deficiency during early pregnancy
- Genetic predisposition (family history)
- Maternal diabetes and obesity
- Use of antiepileptic drugs (e.g., valproic acid)
- Exposure to radiation or heat in early pregnancy
- Alcohol and substance abuse
- Advanced maternal age
- Other nutritional deficiencies (e.g., zinc)
Types of spina bifida
1️⃣ Spina Bifida Occulta
It is the mildest and most common form where there is a small defect or gap in the vertebral arch, but neither the spinal cord nor the meninges protrude through the opening, and it often remains unnoticed without any visible signs or neurological symptoms.
2️⃣ Meningocele
It occurs when the meninges (protective membranes covering the brain and spinal cord) herniate through the vertebral defect, forming a visible fluid-filled sac on the back, but the spinal cord itself remains in its normal position, leading to fewer or no neurological problems in many cases.
3️⃣ Myelomeningocele (Meningomyelocele)
It is the most severe form in which both the meninges and the spinal cord protrude through the spinal defect, resulting in a visible sac on the back and significant neurological impairments such as paralysis of the lower limbs, loss of bladder and bowel control, and frequently associated complications like hydrocephalus.
Pathophysiology of Spina Bifida
1️⃣ During the 3rd to 4th week of embryonic life, the neural tube fails to close properly due to genetic factors, nutritional deficiencies (especially folic acid), or environmental influences.
2️⃣ This incomplete closure results in a defect in the vertebral arches, allowing protrusion of meninges, spinal cord, or both depending on the severity.
3️⃣ The defect leads to exposure and potential damage to the neural tissues, affecting nerve conduction and resulting in motor, sensory, and autonomic dysfunctions.
4️⃣ Associated complications such as hydrocephalus, paralysis, and neurogenic bladder develop based on the level and severity of the defect.
Clinical amnifestation
- Visible swelling or sac on the back (in meningocele or myelomeningocele)
- Paralysis or weakness in lower limbs
- Loss of bowel and bladder control (neurogenic bladder)
- Hydrocephalus (accumulation of CSF in the brain)
- Orthopedic deformities (e.g., clubfoot, scoliosis)
- Sensory loss below the level of the defect
- Learning difficulties (in some cases)
- Skin breakdown or pressure ulcers due to immobility
Diagnostic evaluation
- History collection
- Physical examination
- Maternal Serum Alpha-Fetoprotein (MSAFP)
- Ultrasound
- Amniocentesis
- MRI/CT Scan
- X-ray Spine
Management
General Management
- Early diagnosis through prenatal screening (Ultrasound, MSAFP levels) and postnatal assessment is crucial to plan timely interventions.
- Provide emotional support and counseling to parents upon diagnosis to help them understand the condition and available treatment options.
Medical Management
- Immediate care of the sac (in case of meningocele or myelomeningocele) involves covering the exposed area with a sterile, moist, non-adherent dressing to prevent infection.
- Administer prophylactic antibiotics to prevent meningitis and other infections before surgical intervention.
- Monitor for hydrocephalus, which is a common associated condition, and plan for early management if detected.
Surgical Management
- Surgical closure of the defect is typically performed within 24–48 hours after birth to prevent infection and further neurological damage.
- In cases of hydrocephalus, Ventriculoperitoneal (VP) shunt placement may be required to manage cerebrospinal fluid accumulation.
- Corrective surgeries may also be needed later for orthopedic deformities such as clubfoot or scoliosis.
Supportive and Rehabilitation Management
- Initiate physical therapy and rehabilitation early to improve mobility and prevent muscle atrophy or joint contractures.
- Provide orthotic devices, braces, and wheelchairs if necessary to support movement and improve independence.
- Implement bowel and bladder management programs, including scheduled voiding, clean intermittent catheterization, and dietary modifications to prevent constipation.
Nursing management
1️⃣ Maintain a sterile and moist dressing over the exposed sac using normal saline-soaked non-adherent dressings to prevent drying and infection until surgical closure is performed.
2️⃣ Position the infant in a prone position with hips slightly flexed and legs abducted using padding to avoid pressure on the sac and prevent injury.
3️⃣ Monitor the sac regularly for signs of leakage, infection, or rupture, and report immediately if redness, swelling, or discharge is observed.
4️⃣ Observe for signs of increased intracranial pressure (ICP), such as bulging fontanelles, irritability, poor feeding, high-pitched cry, vomiting, or sunset sign, which may indicate associated hydrocephalus.
5️⃣ Monitor vital signs frequently, including temperature, as infants with open neural tube defects are at a higher risk of developing infections such as meningitis.
6️⃣ Administer prescribed antibiotics and other medications promptly to prevent or treat infections and manage associated complications.
7️⃣ Support bladder and bowel management by educating parents about clean intermittent catheterization techniques and scheduled bowel emptying to prevent constipation and urinary tract infections.
8️⃣ Collaborate with physiotherapists and occupational therapists to initiate early mobility exercises and prevent muscle atrophy, contractures, and deformities.
9️⃣ Provide meticulous skin care to prevent pressure ulcers, especially in areas with decreased sensation, and change the child’s position frequently to reduce pressure over bony prominences.
🔟 Educate parents on post-operative wound care after surgical correction, emphasizing signs of wound infection, CSF leakage, and shunt malfunction if a VP shunt has been placed.
1️⃣1️⃣ Offer emotional and psychological support to parents, helping them cope with feelings of guilt or anxiety, and provide information about the child’s prognosis and care plan.
1️⃣2️⃣ Facilitate early referral to social support services and special education programs to assist families in planning for long-term care and rehabilitation.
1️⃣3️⃣ Teach parents to identify signs of shunt malfunction such as headaches, vomiting, drowsiness, and swelling along the shunt tract, and advise seeking prompt medical attention if observed.
1️⃣4️⃣ Promote parental bonding by encouraging safe touch and interaction with the baby even when special positioning is required.
1️⃣5️⃣ Maintain accurate documentation of neurological assessments, dressing changes, parental education, and all nursing interventions to ensure continuity of care.
3. Nephrotic syndrome
Definition
Nephrotic Syndrome is a kidney disorder characterized by excessive protein loss in urine (proteinuria), leading to low blood protein levels (hypoalbuminemia), generalized body swelling (edema), and high blood lipid levels (hyperlipidemia).
Causes
- Primary (Idiopathic) Nephrotic Syndrome:
- Minimal Change Disease (Most common in children)
- Focal Segmental Glomerulosclerosis (FSGS)
- Membranous Nephropathy
- Secondary Nephrotic Syndrome:
- Diabetes Mellitus (Diabetic Nephropathy)
- Systemic Lupus Erythematosus (SLE)
- Infections: Hepatitis B, Hepatitis C, HIV, Malaria
- Amyloidosis
- Malignancies (Lymphoma, Leukemia)
- Drugs : NSAIDs, Penicillamine, Gold, Heroin
Pathophysiology
- Injury to the glomerular filtration barrier (podocytes and basement membrane).
- Increased permeability of the glomeruli → Massive protein loss in urine (proteinuria).
- Loss of plasma proteins, especially albumin → Hypoalbuminemia.
- Reduced oncotic pressure → Fluid moves into interstitial tissues → Edema formation.
- Liver compensates by increasing lipid synthesis → Hyperlipidemia.
- Loss of immunoglobulins and coagulation proteins → Increased risk of infections and thrombosis.
Clinical Manifestations
- Generalized Edema (Periorbital, pedal, ascites, pleural effusion)
- Proteinuria (Frothy or foamy urine)
- Hypoalbuminemia (Low serum albumin)
- Hyperlipidemia
- Weight gain due to fluid retention
- Fatigue and weakness
- Hypertension (Sometimes present)
- Increased susceptibility to infections
- Thromboembolic events (e.g., deep vein thrombosis)
Diagnostic Evaluation
- History collection
- Physical examination
- Urine Analysis
- Blood Tests
- Renal Function Tests
- Serological Tests
- Renal Biopsy
Management
General Measures
- Low-sodium and low-fat diet to control edema and hyperlipidemia.
- Moderate protein intake to replace lost proteins without overloading kidneys.
- Fluid restriction in cases of severe edema.
Pharmacological Treatment
- Corticosteroids : Prednisolone is the first-line drug to reduce proteinuria.
- Immunosuppressants : Cyclophosphamide or Cyclosporine in steroid-resistant cases.
- Diuretics : Furosemide to manage edema.
- ACE Inhibitors/ARBs : Enalapril or Losartan to reduce protein loss in urine.
- Statins : To manage hyperlipidemia.
- Anticoagulants : Heparin or Warfarin if there is a risk of thrombosis.
Advanced Management (If Required):
Dialysis or kidney transplantation in end-stage renal failure.
Nursing management
Monitoring and Assessment
- Monitor vital signs frequently, paying special attention to blood pressure, respiratory rate, and heart rate.
- Record daily weight at the same time each day using the same scale to monitor fluid retention accurately.
- Maintain a detailed intake and output chart, noting urine color, volume, and presence of frothy urine.
- Assess for signs of edema (periorbital puffiness, abdominal distension, sacral and pedal edema).
- Monitor for signs of infection, such as fever, cough, or abdominal tenderness.
Medication Administration
- Administer prescribed medications (e.g., corticosteroids like Prednisolone, diuretics, and ACE inhibitors) on time and as per correct dosage.
- Monitor for adverse effects of steroids (weight gain, hyperglycemia, mood changes) and diuretics (hypokalemia, dehydration).
- Educate parents about the importance of completing the full course of medications and not discontinuing treatment abruptly.
Infection Prevention
- Maintain strict hand hygiene before and after patient contact to reduce the risk of hospital-acquired infections.
- Encourage a clean environment by keeping the child’s room sanitized and limiting visitors.
- Administer vaccinations as advised (e.g., Pneumococcal, Influenza) to prevent opportunistic infections.
- Educate parents to avoid taking the child to crowded places and to report any signs of infection immediately.
Nutritional Management
- Provide a low-sodium diet to control edema and prevent fluid overload.
- Encourage a moderate-protein diet based on the child’s age and renal function status to replace protein losses.
- Offer nutritious, calorie-rich foods to prevent malnutrition, especially during prolonged illness.
- Ensure fluid restriction if prescribed, and teach parents how to measure and control the child’s daily fluid intake.
Psychological and Emotional Support
- Provide emotional reassurance to the child to reduce anxiety about hospitalization and frequent medical interventions.
- Encourage age-appropriate play activities to promote normal growth and development.
- Offer family counseling to help parents cope with the chronic nature of the disease and manage stress.
- Involve parents in care decisions to enhance their confidence and competence in home care after discharge.
4. TEF
Definition
Tracheoesophageal Fistula (TEF) is a congenital abnormal connection between the trachea and the esophagus, leading to the passage of food or fluids into the respiratory tract and resulting in serious respiratory complications if untreated.
Causes of TEF
- Congenital Malformation during 4th–6th week of embryonic life.
- Associated with VACTERL anomalies.
- Chromosomal disorders like Trisomy 13, 18, and 21 (Down Syndrome).
- Maternal polyhydramnios during pregnancy.
- Exposure to teratogenic drugs or environmental toxins.
- Rarely, acquired causes like trauma, foreign body ingestion, or prolonged intubation.
Types of Tracheoesophageal Fistula (TEF)
✅ 1. Type C (Most Common Type) – EA with Distal TEF
- The upper esophagus ends in a blind pouch (atresia), and the lower esophagus connects to the trachea.
- It occurs in about 85% of cases.
- Clinical Features: Excessive drooling, coughing, choking during feeds, and abdominal distension due to air in the stomach.
✅ 2. Type A – Isolated Esophageal Atresia (No TEF)
- The esophagus is interrupted with no connection to the trachea.
- Accounts for about 8% of cases.
- Clinical Features: Drooling of saliva, inability to pass a feeding tube, no gas in the abdomen.
✅ 3. Type E (H-Type Fistula) – TEF without Esophageal Atresia
- There is a direct fistula between the trachea and esophagus, but the esophagus is continuous.
- Accounts for about 4% of cases.
- Clinical Features: Recurrent pneumonia, coughing during feeding, but normal swallowing.
- Difficult to diagnose early because symptoms may be subtle.
✅ 4. Type B – EA with Proximal TEF (Rare)
- The upper esophagus connects to the trachea; the lower esophagus ends in a blind pouch.
- Extremely rare (about 1% of cases).
- Clinical Features: Choking and aspiration immediately after birth; abdomen remains flat due to no gas entry.
✅ 5. Type D – EA with Both Proximal and Distal TEF (Very Rare)
- Both ends of the esophagus are connected to the trachea via fistulas.
- Accounts for less than 1% of cases.
- Clinical Features: Severe respiratory distress, recurrent aspiration, and early onset of symptoms after birth.
Clinical Manifestations
- Excessive frothy saliva and drooling immediately after birth.
- Coughing and choking during feeding episodes.
- Cyanosis (bluish discoloration), especially while feeding or crying.
- Respiratory distress and noisy breathing due to aspiration.
- Recurrent aspiration pneumonia from swallowed milk or secretions entering the lungs.
- Abdominal distension due to air entering the stomach through the fistula.
- Inability to pass a nasogastric tube into the stomach (diagnostic clue).
Diagnostic Evaluation
- History collection
- Physical examination
- NG tube test
- X-ray
- Contrast study
- Echocardiography
- Ultrasound
Management
✅ 1. Immediate Preoperative Management
Prevent Aspiration :
- Keep the baby nil per oral (NPO) (no oral feeds).
- Insert a Replogle tube (double-lumen tube) into the upper esophageal pouch to continuously suction secretions and prevent aspiration.
- Keep the infant in a semi-upright (head elevated) position to minimize reflux of secretions into the airway.
Maintain Airway and Oxygenation :
- Administer humidified oxygen if signs of respiratory distress are present.
- Monitor oxygen saturation (SpO₂) and provide ventilatory support if needed.
Hydration and Electrolyte Balance :
- Initiate intravenous fluids (IVF) to maintain hydration and correct electrolyte imbalances.
Antibiotic Therapy :
- Start broad-spectrum antibiotics to prevent or treat aspiration pneumonia.
✅ 2. Surgical Management (Definitive Treatment)
Timing of Surgery :
- Surgery is typically performed as soon as the infant is stabilized.
- In stable cases, immediate surgery is planned; in critically ill infants, surgery may be delayed after initial stabilization.
Surgical Procedure :
- Ligation of the fistula to close the abnormal connection between the trachea and esophagus.
- Primary anastomosis to reconnect the two ends of the esophagus if possible.
- In cases with long-gap atresia, staged repair or esophageal replacement procedures may be necessary.
✅ 3. Postoperative Management
Airway and Breathing :
- Closely monitor for respiratory distress and ensure airway patency.
- Provide oxygen support or mechanical ventilation if required.
Feeding Management :
- Start gastrostomy feeding if oral feeding is not possible initially.
- Gradually introduce oral feeds after confirming the integrity of esophageal repair (contrast study may be done before initiating oral feeds).
Monitor for Complications :
- Watch for signs of anastomotic leak, strictures, tracheomalacia, or recurrent fistula.
- Assess for signs of infection or sepsis.
Parental Counseling :
- Educate parents regarding postoperative care, feeding techniques, and recognizing complications.
- Explain the importance of follow-up visits for long-term monitoring.
5. Pneumonia
Definition
Pneumonia is an acute infection of the lungs characterized by inflammation of the alveoli, which may fill with fluid or pus, leading to difficulty in breathing and oxygen exchange. In children, it is a leading cause of morbidity and mortality, especially in children under 5 years.
Types of pneumonia
Pneumonia can be classified based on origin, causative agent, anatomical pattern, and risk group:
1. Based on Origin / Setting
✅ A. Community-Acquired Pneumonia (CAP)
- It is acquired outside hospital or healthcare setting
- Common pathogens : Streptococcus pneumoniae, Mycoplasma pneumoniae, viruses
✅ B. Hospital-Acquired Pneumonia (HAP)
- It occurs 48 hours or more after hospital admission
- More resistant organisms like Pseudomonas, MRSA
✅ C. Ventilator-Associated Pneumonia (VAP)
- It Develops 48–72 hours after endotracheal intubation
✅ D. Healthcare-Associated Pneumonia (HCAP) (less used now)
- In which patients from nursing homes, dialysis centers, or recent hospitalization develop pneumonia.
2. Based on Causative Agent
✅ A. Bacterial Pneumonia
- It is a most common type of pneumonia
- It occurs due to bacterial infection (e.g., Streptococcus pneumoniae, Klebsiella, Staphylococcus aureus)
✅ B. Viral Pneumonia
- It occurs due to viral infection.
- It is common in children and elderly (e.g., Influenza, RSV, SARS-CoV-2
✅ C. Fungal Pneumonia
- It occurs due to fungal infection.
- It is seen in immunocompromised individuals (e.g., Histoplasma, Aspergillus)
✅ D. Atypical Pneumonia
- It is caused by organisms like Mycoplasma, Chlamydophila, Legionella
- Symptoms are milder and extra-pulmonary
✅ E. Aspiration Pneumonia
- It occurs due to inhalation of oropharyngeal contents (vomit, food, saliva)
- Often involves anaerobic organisms
3. Based on Anatomical Involvement
✅ A. Lobar Pneumonia
- It Involves a single lobe of the lung
- It incldes classic consolidation pattern
✅ B. Bronchopneumonia
- In which patchy involvement of multiple lobes
- It starts in bronchi and spreads to alveoli
✅ C. Interstitial Pneumonia
- It involves alveolar walls and interstitium, not alveoli
- Often viral or atypical in origin
4. Based on Risk Factors
✅ A. Opportunistic Pneumonia
- It is most commonly seen in HIV/AIDS, cancer, transplant patients
- It is caused by organisms like Pneumocystis jirovecii
✅ B. Aspiration Pneumonia
- It is most commonly seen in patients with swallowing difficulties, stroke, unconsciousness
Pathophysiology of Pneumonia
1️⃣ Pathogens (bacteria, viruses, fungi) enter the lower respiratory tract via inhalation or aspiration.
2️⃣ They bypass lung defenses and infect the alveoli.
3️⃣ The immune system responds with inflammation and cytokine release.
4️⃣ Alveolar-capillary membrane becomes permeable, allowing fluid and pus to fill alveoli.
5️⃣ Gas exchange is impaired due to alveolar consolidation.
6️⃣ Hypoxemia and respiratory distress develop.
7️⃣ If untreated, complications like pleural effusion, empyema, or sepsis may occur.
Clinical Manifestations
- Fever and chills
- Cough (productive or dry)
- Tachypnea (rapid breathing)
- Chest in-drawing (retractions)
- Nasal flaring
- Grunting respiration
- Cyanosis (in severe cases)
- Poor feeding and irritability
- Crackles or diminished breath sounds on auscultation
Diagnostic Evaluation
- History collection
- Physical examination
- Chest X-ray
- Pulse oximetry
- Complete blood count (CBC)
- Blood culture
- Sputum culture
- Nasal swab PCR for pathogen identification (if needed)
Management
1. General Supportive Care
- Ensure the child has adequate rest and comfort.
- Maintain proper hydration through oral or intravenous fluids.
- Provide a nutrient-rich diet to support recovery and improve immunity.
- Keep the child in a semi-Fowler’s position to ease breathing.
- Use a humidified environment if there is thick sputum or respiratory distress.
2. Oxygen Therapy
- Administer humidified oxygen if the child shows signs of hypoxia (SpO₂ < 92%).
- Use nasal prongs, face mask, or oxygen hood based on the child’s age and condition.
3. Pharmacological Management
Antibiotic Therapy (Based on Severity and Organism Suspected) :
Mild pneumonia :
Amoxicillin (First-line oral antibiotic).
Macrolides (Azithromycin) if atypical organisms are suspected.
Severe Pneumonia :
Intravenous antibiotics like Ampicillin + Gentamicin or Ceftriaxone.
Modify antibiotics based on culture sensitivity reports.
Antipyretics :
Paracetamol or Ibuprofen to manage fever and discomfort.
Bronchodilators :
Salbutamol nebulization if there is associated wheezing or bronchospasm.
Mucolytics and Expectorants :
May be used to facilitate sputum clearance.
Vitamin and Mineral Supplementation :
Vitamin A and Zinc supplementation to enhance immunity and recovery.
4. Chest Physiotherapy
- Encourage deep breathing exercises and postural drainage if needed.
- Gently perform percussion and vibration techniques to help mobilize secretions.
5. Monitoring
- Continuously monitor respiratory rate, oxygen saturation (SpO₂), and temperature.
- Observe for signs of respiratory distress or cyanosis.
- Evaluate the effectiveness of antibiotics and modify treatment if necessary.
Nursing Management
1. Airway Clearance and Respiratory Support
- Maintain a clear airway by gentle suctioning of secretions if required.
- Position the child in a semi-Fowler’s or high Fowler’s position to promote easier breathing.
- Administer humidified oxygen therapy as per the physician’s order if signs of hypoxia are present.
- Encourage deep breathing exercises (age-appropriate) and chest physiotherapy to mobilize secretions.
- Monitor and record respiratory rate, effort, and oxygen saturation (SpO₂) regularly.
2. Monitoring Vital Signs and Clinical Status
- Frequently assess and record temperature, pulse, respiratory rate, and SpO₂ levels.
- Observe for signs of respiratory distress, such as nasal flaring, chest retractions, grunting, or cyanosis.
- Monitor for potential complications like pleural effusion or respiratory failure.
3. Medication Administration
- Administer prescribed antibiotics on time and monitor for adverse reactions.
- Provide antipyretics (e.g., Paracetamol) to manage fever.
- Administer bronchodilators (e.g., Salbutamol nebulization) if prescribed.
- Ensure correct technique for nebulization or inhaler use if applicable.
4. Nutrition and Hydration
- Encourage small, frequent, and nutrient-rich meals to maintain energy levels.
- Provide adequate oral fluids or administer IV fluids if the child is unable to drink adequately.
- Monitor for signs of dehydration such as dry mucous membranes and reduced urine output.
5. Comfort and Rest
- Provide a quiet and calm environment to ensure adequate rest.
- Use appropriate measures to reduce fever such as tepid sponging and maintaining a comfortable room temperature.
- Offer emotional support and reassurance to reduce anxiety in both the child and parents.
Q-6 Fill in the blanks with appropriate words. (5)
1. Expected weight of one year child is……….when his birth weight is 3.5 kg.
10.5kg
2. Sunset sign is seen in…………… condition.
Hydrocephalus
3. In human breast milk……………….Antibody found.
Immunoglobulin A (IgA)
4. At birth………… vaccine is given.
BCG, OPV-0, and Hepatitis B (birth dose)
5. APGAR score assessed at ……………… time
1 minute and 5 minutes after birth
