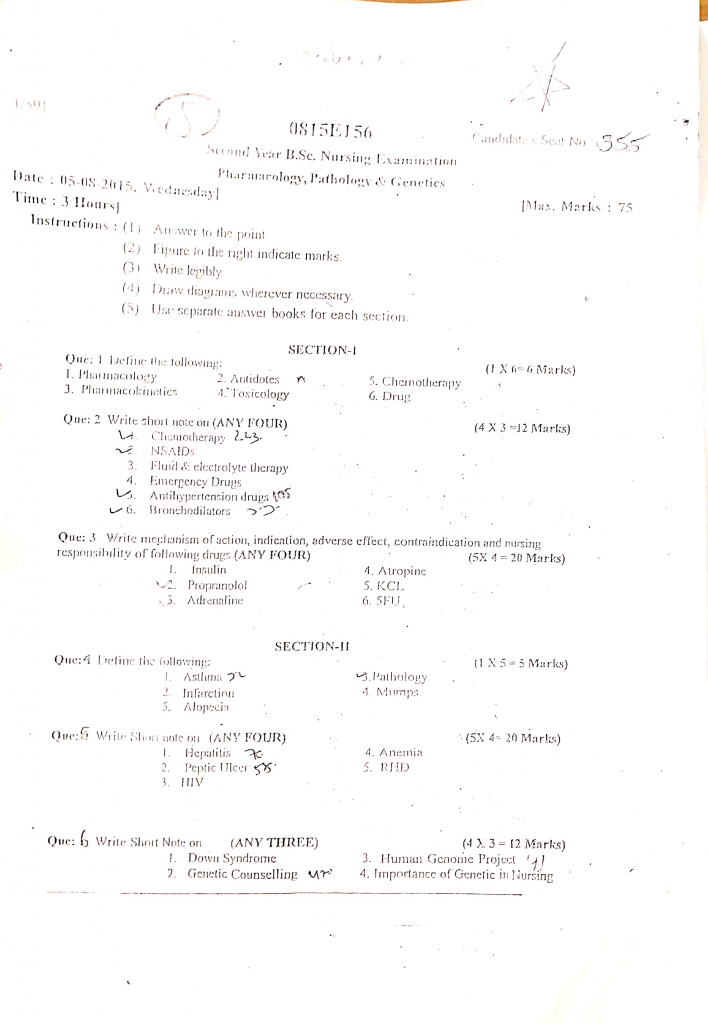
05/08/2015-PARMA,PATHO,GENETICS-JUHI DONE-PAPER NO-5
PARMA,PATHO,GENETICS-PAPER SOLUTION NO-5
Section 1
Q.1 Define the following (1×6=6)
1. Pharmacology
- Pharmacology is the branch of medical science that deals with the study of drugs, including their origin, composition, pharmacokinetics (absorption, distribution, metabolism, and excretion), pharmacodynamics (mechanism of action), therapeutic uses, and adverse effects on living organisms.
2. Antidotes
- An antidote is a substance that is used to neutralize, counteract, or reverse the effects of a poison or overdose of a drug in the human body.
- It is given in cases of poisoning or toxicity to prevent or reduce harm by either blocking the poison’s action, promoting its elimination, or directly binding with the toxin to render it harmless.
3. Pharmacokinetics
- Pharmacokinetics is the branch of pharmacology that deals with the movement of drugs within the body, specifically describing what the body does to the drug after administration.
4. Toxicology
- Toxicology is the branch of science that deals with the study of harmful effects of chemicals, drugs, or toxins on living organisms, including humans.
- It involves the identification, detection, nature, mechanisms, and treatment of toxic substances, and helps in understanding how poisons act, how much is dangerous, and how to manage or prevent poisoning in clinical and environmental settings.
5. Chemotherapy
- Chemotherapy is the branch of pharmacology that involves the use of chemical substances (drugs) to kill or inhibit the growth of microorganisms, parasites, or cancer cells without causing excessive damage to the host.
- It is mainly used in the treatment of infections (antibacterial, antiviral, antifungal) and malignancies (anticancer drugs) by targeting the disease-causing cells or organisms, often affecting their reproduction or metabolism.
6. Drug
- A drug is any chemical substance that, when administered to a living organism, produces a biological effect and is used for the prevention, diagnosis, treatment, or cure of diseases.
- It can modify physiological functions, either enhancing or inhibiting normal body processes, and is used in medical practice to restore health or relieve symptoms.
Q.2 Write short notes on (any four) (4×3=12)
1. Chemotherapy
Definition of Chemotherapy
- Chemotherapy refers to the use of chemical substances, particularly cytotoxic drugs, to treat diseases—most commonly cancer.
- It involves the administration of drugs that destroy or inhibit the growth and division of malignant (cancerous) cells.
- It can be curative, palliative, neoadjuvant (before surgery), or adjuvant (after surgery) depending on the goal of treatment.
Objectives of Chemotherapy
- It is used to cure cancer by eradicating all cancer cells from the body.
- It is used to shrink tumors before surgery or radiation (neoadjuvant therapy).
- It is used to kill any remaining cancer cells after surgery or radiation (adjuvant therapy).
- It is used to relieve symptoms and prolong survival in advanced cancers (palliative chemotherapy).
Classification of Chemotherapy Drugs
Chemotherapeutic agents are classified based on their mechanism of action:
1. Alkylating Agents
- These drugs damage DNA and prevent cell replication.
- Examples: Cyclophosphamide, Busulfan, Melphalan
2. Antimetabolites
- These drugs mimic normal substances and interfere with DNA and RNA synthesis.
- Examples: Methotrexate, 5-Fluorouracil (5-FU), Cytarabine
3. Anti-microtubule Agents (Mitotic Inhibitors)
- These drugs inhibit microtubule function, preventing cell division.
- Examples: Vincristine, Paclitaxel, Docetaxel
4. Topoisomerase Inhibitors
- These drugs interfere with enzymes involved in DNA replication.
- Examples: Etoposide, Irinotecan
5. Antitumor Antibiotics
- These drugs bind directly to DNA and inhibit essential enzymes.
- Examples: Doxorubicin, Bleomycin
6. Hormonal Agents
- These are used in hormone-sensitive cancers (e.g., breast or prostate cancer).
- Examples: Tamoxifen (anti-estrogen), Flutamide (anti-androgen)
7. Targeted Therapy and Monoclonal Antibodies
- These drugs target specific cancer cell markers.
- Examples: Imatinib, Trastuzumab (Herceptin), Rituximab
Common Side Effects of Chemotherapy
- Myelosuppression: Decrease in blood cell count (anemia, leukopenia, thrombocytopenia).
- Nausea and vomiting: Very common due to irritation of GI tract.
- Hair loss (alopecia): Results from damage to hair follicle cells.
- Mucositis and stomatitis: Painful inflammation of mucous membranes.
- Fatigue and weakness: Due to destruction of healthy cells.
- Increased risk of infection: Due to immune suppression.
- Neuropathy: Especially with vincristine and taxanes.
- Infertility: May affect reproductive organs.
Nursing Responsibilities in Chemotherapy
1. Pre-chemotherapy Assessment
- It is the nurse’s responsibility to assess the patient’s baseline health status, including CBC, renal, and liver function tests, before starting chemotherapy.
- It is essential to evaluate the presence of infection, allergies, and any contraindications for chemotherapy administration.
- The nurse must provide emotional support and psychological preparation to the patient and family before starting chemotherapy.
2. During Administration
- It is critical to ensure correct drug, dose, dilution, and route during chemotherapy administration under aseptic precautions.
- The nurse should monitor the IV site continuously for signs of extravasation or tissue necrosis during vesicant drug infusion.
- It is the nurse’s duty to be vigilant for any signs of hypersensitivity reactions or anaphylaxis during infusion and act promptly.
3. Post-Chemotherapy Monitoring
- It is important for the nurse to monitor for adverse effects like nausea, vomiting, fever, mucositis, or bone marrow suppression.
- The nurse should encourage hydration and intake of a balanced diet to support immune function and healing.
- The nurse must observe for signs of infection (e.g., fever, sore throat) and report to the physician immediately.
4. Patient Education and Counseling
- It is the responsibility of the nurse to educate the patient on expected side effects and when to seek help.
- It is important to instruct the patient on personal hygiene, infection prevention, and safe handling of body fluids post-chemotherapy.
- The nurse must guide the patient regarding fertility preservation options before starting therapy if appropriate.
2. NSAIDs
Definition of NSAIDs
- NSAIDs are a group of non-opioid, non-steroidal drugs that provide analgesic (pain-relieving), antipyretic (fever-reducing), and anti-inflammatory effects by inhibiting the synthesis of prostaglandins.
- These drugs are called “non-steroidal” because, unlike corticosteroids, they do not contain steroid structures, but still offer anti-inflammatory properties.
Mechanism of Action
- It is by inhibiting the activity of cyclooxygenase (COX) enzymes, mainly COX-1 and COX-2, which are responsible for converting arachidonic acid into prostaglandins.
- By reducing prostaglandin production, NSAIDs help in decreasing inflammation, pain sensation, and fever.
Classification of NSAIDs
a) Non-selective COX Inhibitors
- These drugs act by blocking both COX-1 and COX-2 enzymes, thereby reducing prostaglandin formation throughout the body, which leads to both therapeutic effects and side effects.
- It is important to note that COX-1 inhibition is responsible for gastric irritation, so these drugs carry a higher risk of peptic ulcers and gastrointestinal bleeding.
- Examples: Aspirin, Ibuprofen, Naproxen, Diclofenac, Indomethacin, Ketoprofen.
b) Selective COX-2 Inhibitors (Coxibs)
- These drugs selectively inhibit only COX-2 enzyme, which is mainly induced during inflammation, thus reducing pain and swelling without much effect on the gastric mucosa.
- These are preferred in patients at risk of GI complications, but they carry a higher risk of cardiovascular side effects, such as myocardial infarction or stroke.
- Examples: Celecoxib, Etoricoxib, Parecoxib, Valdecoxib.
c) Salicylates
- These drugs are derived from salicylic acid and are among the oldest NSAIDs, with aspirin being the most widely used.
- Aspirin also has unique antiplatelet properties, making it valuable in the prevention of cardiovascular events like heart attack and stroke.
- Examples: Aspirin (Acetylsalicylic acid), Sodium salicylate, Choline magnesium trisalicylate.
d) Acetic Acid Derivatives
- These NSAIDs have a potent anti-inflammatory action and are commonly used in acute gouty arthritis or ankylosing spondylitis.
- These drugs have a higher incidence of CNS side effects, such as headache, dizziness, and confusion, especially in elderly patients.
- Examples: Indomethacin, Sulindac, Etodolac, Diclofenac sodium.
e) Enolic Acid Derivatives (Oxicams)
- These NSAIDs are known for their long half-life, which allows for once-daily dosing, improving patient compliance in chronic conditions.
- These drugs are commonly used in chronic inflammatory diseases like osteoarthritis and rheumatoid arthritis due to their slow onset and long duration.
- Examples: Piroxicam, Meloxicam, Tenoxicam, Lornoxicam.
Therapeutic Uses of NSAIDs
- It is widely used for relief of mild to moderate pain, such as headache, muscle pain, and toothache.
- It is commonly used to reduce fever in febrile illnesses.
- It is helpful in reducing inflammation in conditions like arthritis, bursitis, and tendinitis.
- It is used in rheumatoid arthritis, osteoarthritis, and gouty arthritis to reduce joint swelling and stiffness.
- Aspirin (a type of NSAID) is used in low doses for prevention of heart attacks and strokes due to its antiplatelet action.
Adverse Effects of NSAIDs
- It can cause gastric irritation, peptic ulcers, and GI bleeding due to COX-1 inhibition.
- It may lead to renal impairment by reducing prostaglandins that regulate renal blood flow.
- It may cause increased risk of bleeding due to platelet inhibition (especially aspirin).
- It may lead to hypersensitivity reactions like rashes, bronchospasm, or anaphylaxis.
- Long-term use may increase the risk of cardiovascular events, especially with selective COX-2 inhibitors.
Contraindications of NSAIDs
- It is contraindicated in patients with peptic ulcer disease or history of gastrointestinal bleeding.
- It should be avoided in patients with chronic kidney disease or heart failure.
- It is not recommended for asthmatic patients allergic to aspirin or NSAIDs.
- It should be used with caution during pregnancy, especially in the third trimester.
- NSAIDs are generally avoided in children with viral infections (especially aspirin, due to risk of Reye’s syndrome).
7️⃣ Nursing Responsibilities in NSAID Administration
a) Assessment and Evaluation
- It is important for the nurse to assess the patient’s history for any GI disorders, bleeding tendencies, or renal problems before administering NSAIDs.
- The nurse must evaluate pain levels and temperature before and after administration to assess therapeutic effectiveness.
b) Monitoring for Side Effects
- The nurse should monitor for signs of gastric discomfort, black tarry stools, hematuria, or epigastric pain, which may indicate GI bleeding.
- The nurse should also observe for skin rashes, wheezing, or difficulty breathing, which may indicate allergic reactions.
c) Patient Education
- It is the responsibility of the nurse to educate the patient to take NSAIDs with food or milk to reduce gastric irritation.
- The nurse must inform the patient to avoid alcohol and other ulcerogenic drugs like corticosteroids while on NSAIDs.
- Patients should be taught to report any unusual symptoms like abdominal pain, vomiting of blood, or ringing in the ears (especially with aspirin).
d) Safe Administration
- The nurse must verify the right dose and route and avoid giving NSAIDs in combination with other anticoagulants unless prescribed.
- The nurse should ensure appropriate spacing of doses and avoid overdose, especially in elderly patients.
3. Fluid and electrolyte therapy
Definition
- Fluid and electrolyte therapy is the medical and nursing intervention used to restore and maintain proper fluid volume and balance of essential electrolytes such as sodium, potassium, calcium, magnesium, chloride, phosphate, and bicarbonate in the body.
- It is most often used in conditions of dehydration, fluid overload, acid-base imbalance, and electrolyte disturbances, especially in hospitalized or critically ill patients.
Goals of Fluid and Electrolyte Therapy
- It is aimed at maintaining or restoring normal fluid volume in the intravascular, interstitial, and intracellular spaces.
- It is used to correct electrolyte imbalances such as hyponatremia, hypokalemia, or hypercalcemia.
- It is administered to support normal physiological functions, such as cardiac function, neural activity, and acid-base homeostasis.
- It helps in managing fluid losses due to diarrhea, vomiting, burns, surgery, or hemorrhage.
- It is also used to maintain hydration status during fasting, NPO (nothing by mouth) status, or post-operative care.
Types of Fluids Used
a) Crystalloids
- These are aqueous solutions of mineral salts or other water-soluble molecules, such as Normal Saline (0.9% NaCl), Ringer’s Lactate, and Dextrose solutions.
- It is used for volume replacement, maintenance fluids, and resuscitation.
b) Colloids
- These are solutions that contain large protein molecules like albumin, dextran, and hydroxyethyl starch.
- It is used to expand plasma volume by increasing oncotic pressure in conditions like shock or burns.
c) Electrolyte Supplements
- These include oral or intravenous preparations of sodium, potassium, calcium, magnesium, phosphate, etc., given to correct specific electrolyte deficiencies.
Indications for Fluid and Electrolyte Therapy
- It is indicated in dehydration or hypovolemia due to blood loss, diarrhea, vomiting, or burns.
- It is used in electrolyte disturbances such as hyponatremia, hyperkalemia, or hypocalcemia.
- It is essential during major surgeries, trauma, sepsis, renal failure, or prolonged fasting/NPO status.
- It is used in patients with vomiting, diarrhea, NG suction, or fever to maintain fluid balance.
Signs of Fluid and Electrolyte Imbalance
- It includes dry mucous membranes, low urine output, tachycardia, confusion, muscle weakness, cardiac arrhythmias, hypotension, or altered level of consciousness.
Nursing Management in Fluid and Electrolyte Therapy
a) Assessment and Monitoring
- It is the nurse’s responsibility to assess the patient’s hydration status, vital signs, weight changes, skin turgor, and intake-output balance regularly.
- The nurse must closely monitor lab values of serum electrolytes, blood urea nitrogen (BUN), creatinine, and arterial blood gases (ABGs).
b) Fluid Administration
- The nurse must ensure correct administration of IV fluids as per doctor’s order using aseptic techniques and regulate the IV flow rate accurately.
- The nurse should observe for signs of fluid overload like edema, crackles in lungs, or hypertension and immediately report them.
c) Electrolyte Supplementation
- It is the nurse’s role to administer oral or IV electrolyte preparations carefully and monitor for signs of toxicity or deficiency.
- For example, potassium should never be given IV push; it must be diluted and given slowly under strict supervision.
d) Patient Education
- The nurse should educate the patient and family regarding adequate oral fluid intake, dietary sources of electrolytes, and signs to report, such as muscle cramps, palpitations, or excessive fatigue.
e) Documentation
- It is the nurse’s duty to accurately document fluid intake, output, type of fluids given, rate of infusion, and any changes in patient’s condition during therapy.
4. Emergency drugs
Definition of Emergency Drugs
- Emergency drugs are life-saving medications used in acute, life-threatening conditions to stabilize vital signs and restore normal physiological functions.
- They are used during medical emergencies such as cardiac arrest, anaphylaxis, shock, respiratory failure, seizures, and severe hypotension.
- These drugs must be readily available in crash carts in ICU, emergency rooms, and operation theaters for immediate use.
Commonly Used Emergency Drugs
1. Adrenaline (Epinephrine)
- It is a potent sympathomimetic drug that stimulates alpha and beta-adrenergic receptors.
- It is used in anaphylactic shock, cardiac arrest, bronchospasm, and severe hypotension.
- It causes vasoconstriction, increases cardiac output, and dilates bronchial smooth muscle.
- Dose: 1 mg IV push every 3–5 minutes during CPR.
2. Atropine Sulfate
- It is an anticholinergic drug that blocks the parasympathetic nervous system.
- It is used in bradycardia, asystole, and organophosphate poisoning.
- It increases heart rate by blocking vagal effects on the heart.
- Dose: 0.5 mg IV every 3–5 minutes (maximum 3 mg) for bradycardia.
3. Adenosine
- It is an antiarrhythmic drug that slows conduction through the AV node.
- It is used for treating supraventricular tachycardia (SVT).
- It may cause brief asystole but restores sinus rhythm rapidly.
- Dose: 6 mg IV bolus, may repeat with 12 mg.
4. Amiodarone
- It is a Class III antiarrhythmic drug used in ventricular tachycardia, ventricular fibrillation, and atrial fibrillation.
- It prolongs the action potential and refractory period of the cardiac muscle.
- Dose: 300 mg IV bolus during CPR, followed by 150 mg if needed.
5. Nitroglycerin (NTG)
- It is a vasodilator used in acute coronary syndrome, angina, and acute heart failure.
- It reduces preload and myocardial oxygen demand.
- Dose: 0.3–0.6 mg sublingual every 5 minutes, or IV infusion.
6. Sodium Bicarbonate
- It is an alkalinizing agent used in metabolic acidosis, hyperkalemia, or overdose of tricyclic antidepressants.
- It restores acid-base balance by buffering excess hydrogen ions.
- Dose: 1 mEq/kg IV bolus in emergencies.
7. Dopamine
- It is a vasopressor and inotropic agent used in shock and heart failure.
- It improves cardiac output and renal perfusion depending on the dose.
- Low dose: increases renal perfusion; high dose: causes vasoconstriction.
- Dose: 2–20 mcg/kg/min IV infusion.
8. Dobutamine
- It is a beta-1 agonist used in acute heart failure and cardiogenic shock.
- It increases myocardial contractility with less effect on heart rate and blood pressure.
- Dose: 2–10 mcg/kg/min IV infusion.
9. Hydrocortisone / Dexamethasone
- These are corticosteroids used in severe allergic reactions, anaphylaxis, and adrenal crisis.
- They reduce inflammation and improve blood pressure in shock.
- Dose: Hydrocortisone 100 mg IV stat; Dexamethasone 4–8 mg IV.
10. Diazepam / Lorazepam / Midazolam
- These are benzodiazepines used in status epilepticus, convulsions, and acute anxiety states.
- They act on GABA receptors in the CNS to produce sedation and stop seizures.
- Dose: Diazepam 5–10 mg IV; Lorazepam 4 mg IV for seizures.
11. Naloxone (Narcan)
- It is a specific opioid antagonist used to reverse the effects of opioid overdose.
- It rapidly restores respiratory function in opioid-induced respiratory depression.
- Dose: 0.4–2 mg IV/IM/subcutaneous every 2–3 minutes.
12. Glucose 50% (Dextrose)
- It is used in hypoglycemia, unconscious diabetic patients, and insulin overdose.
- It provides immediate energy and restores blood glucose levels.
- Dose: 25–50 ml of Dextrose 50% IV push.
13. Furosemide (Lasix)
- It is a loop diuretic used in pulmonary edema, acute heart failure, and hypertensive crisis.
- It promotes diuresis and reduces fluid overload and venous return.
- Dose: 20–40 mg IV slowly.
Nursing Responsibilities in Emergency Drug Administration
- It is essential for the nurse to identify signs of clinical deterioration quickly and initiate emergency protocols as per ACLS/BLS guidelines.
- It is the nurse’s responsibility to prepare, label, and administer emergency drugs accurately under aseptic precautions during resuscitation or crisis.
- The nurse must continuously monitor the patient’s vital signs, ECG, and response to the drug to prevent overdose or complications.
- It is important for the nurse to ensure the crash cart is regularly stocked and checked, including expiration dates and availability of all emergency drugs.
- It is the duty of the nurse to document the drug name, dose, route, time, and patient’s response precisely after every emergency intervention.
5. Antihypertension drugs
Definition
It is a class of medications used to lower elevated blood pressure (hypertension) and reduce the risk of complications such as stroke, myocardial infarction, kidney failure, and heart failure.
Classification of Antihypertensive Drugs (Based on Mechanism of Action)
Diuretics
- It is used to reduce blood volume by increasing urine output.
- Example: Hydrochlorothiazide, Furosemide
Beta-Adrenergic Blockers (Beta-Blockers)
- It blocks beta receptors in heart and vessels, reducing heart rate and cardiac output.
- Example: Atenolol, Metoprolol, Propranolol
Calcium Channel Blockers (CCBs)
- It inhibits calcium influx into vascular smooth muscle, causing vasodilation.
- Example: Amlodipine, Verapamil, Diltiazem
Angiotensin-Converting Enzyme (ACE) Inhibitors
- It prevents conversion of angiotensin I to angiotensin II, a vasoconstrictor.
- Example: Enalapril, Ramipril, Lisinopril
Alpha-Adrenergic Blockers
- It blocks alpha receptors in arterioles causing vasodilation.
- Example: Prazosin, Doxazosin
Centrally Acting Alpha-2 Agonists
- It decreases sympathetic activity by acting on central nervous system.
- Example: Clonidine, Methyldopa
Direct Vasodilators
- It directly relaxes the vascular smooth muscles.
- Example: Hydralazine, Minoxidil
Renin Inhibitors
- It inhibits renin and reduces the formation of angiotensin I.
- Example: Aliskiren
Indications of Antihypertensive Drugs
- It is used in treatment of essential (primary) hypertension.
- It is given in cases of secondary hypertension due to renal or endocrine causes.
- It is indicated in hypertensive emergencies (e.g., labetalol I.V.).
- It is used in chronic heart failure to reduce cardiac workload.
- It is used to prevent complications like stroke, heart attack, kidney failure.
Adverse Effects
- Hypotension (Low BP)
- Bradycardia (slow heart rate) – especially with beta blockers
- Dizziness or syncope
- Electrolyte imbalance (e.g., hypokalemia with diuretics)
- Dry cough (common with ACE inhibitors)
- Peripheral edema (especially with CCBs)
- Fatigue and weakness
- Hyperkalemia (with ACE inhibitors, ARBs)
- Sexual dysfunction (noted with beta blockers)
Contraindications
- Pregnancy – especially ACE inhibitors, ARBs, and renin inhibitors
- Bronchial asthma – beta blockers are avoided
- Severe renal failure – need dose adjustment
- Heart block – avoid beta blockers or some CCBs
- Hypotension or volume depletion
Nursing Responsibilities
✅ 1. Monitoring and Assessmen
- It is the responsibility of the nurse to regularly monitor the patient’s blood pressure and heart rate before and after administering antihypertensive medications.
- It is important to assess the patient for signs of hypotension like dizziness, fainting, or confusion, especially in the initial days of therapy.
✅ 2. Patient Education and Compliance
- It is the nurse’s duty to educate the patient about the importance of lifelong adherence to antihypertensive therapy, even if symptoms are not present.
- The nurse should also instruct the patient to avoid sudden position changes to reduce risk of orthostatic hypotension.
✅ 3. Dietary and Lifestyle Advice
- The nurse should advise the patient to follow a low-sodium, heart-healthy diet along with prescribed medications.
- It is important to counsel the patient on limiting alcohol, quitting smoking, and managing stress, which help improve drug effectiveness.
✅ 4. Monitoring for Adverse Effects
- It is necessary to observe and report any side effects such as persistent dry cough (ACE inhibitors), swelling, or irregular heartbeat to the physician promptly.
- Electrolyte levels, especially potassium and sodium, should be checked periodically when the patient is on diuretics or ACE/ARB drugs.
✅ 5. Drug-Specific Instructions
- It is the responsibility of the nurse to administer the medication at the same time each day, preferably with food if required to reduce gastric upset.
- The nurse should avoid abrupt withdrawal of beta blockers to prevent rebound hypertension or angina.
6. Bronchodilators
Definition
- It is a class of respiratory drugs that help relax and widen (dilate) the bronchial passages in the lungs, making breathing easier by reducing airway resistance.
- It is commonly used in the treatment of asthma, chronic obstructive pulmonary disease (COPD), bronchitis, and other obstructive lung diseases.
Classification of Bronchodilators (based on mechanism)
Beta-2 Adrenergic Agonists
These drugs stimulate β2-receptors in bronchial smooth muscles, causing bronchodilation.
➤ Short-acting (SABA):
▪️ Salbutamol (Albuterol)
▪️ Terbutaline
➤ Long-acting (LABA):
▪️ Salmeterol
▪️ Formoterol
Anticholinergics (Muscarinic Antagonists)
These drugs block acetylcholine at muscarinic receptors, leading to bronchodilation.
➤ Short-acting (SAMA):
▪️ Ipratropium bromide
➤ Long-acting (LAMA):
▪️ Tiotropium bromide
Methylxanthines
These drugs inhibit phosphodiesterase, leading to increased cAMP and smooth muscle relaxation.
▪️ Theophylline
▪️ Aminophylline
Mechanism of Action (MOA)
- It is the action of bronchodilators to relax smooth muscles of the bronchial tree and expand airway diameter.
- Beta-2 agonists increase cyclic AMP via adenylate cyclase stimulation leading to smooth muscle relaxation.
- Anticholinergics block muscarinic receptors to prevent bronchoconstriction caused by parasympathetic stimulation.
- Methylxanthines inhibit phosphodiesterase, preventing breakdown of cAMP and enhancing bronchodilation.
Indications (Uses)
- It is primarily used in asthma (acute and chronic attacks).
- It is useful in chronic obstructive pulmonary disease (COPD) and emphysema.
- It is prescribed for acute bronchospasm (e.g., due to allergens or exertion).
- It is also used in chronic bronchitis and wheezing episodes.
- Theophylline may be used in nocturnal asthma or apnea of prematurity.
Adverse Effects
- Tachycardia and palpitations
- Nervousness, tremors, and restlessness
- Dry mouth and throat irritation (common with inhaled anticholinergics)
- Nausea, vomiting (especially with methylxanthines)
- Headache or insomnia
- Hypokalemia (with repeated beta-2 agonist use)
Contraindications
- Severe cardiac arrhythmias (especially with beta-agonists)
- Known hypersensitivity to drug components
- Hyperthyroidism (caution with sympathomimetics)
- Seizure disorders (caution with theophylline)
- Peptic ulcer (methylxanthines can worsen condition)
Nursing Responsibilities
✅ 1. Pre-Administration Assessment
- It is the duty of the nurse to assess the patient’s respiratory rate, lung sounds (wheezing/rhonchi), oxygen saturation, and peak expiratory flow rate (PEFR) before giving bronchodilators.
- The nurse must also review the history of asthma attacks or COPD exacerbations and check for any previous allergic reactions to the medications.
✅ 2. Drug Administration and Monitoring
- It is essential for the nurse to ensure that the correct form of drug is administered (inhaler, nebulizer, oral or IV) and that the patient is using proper technique for inhalation therapy.
- The nurse should monitor for onset of relief of dyspnea, improvement in breath sounds, and any signs of toxicity such as tremors, increased pulse rate, or nausea.
✅ 3. Patient Education
- The nurse must educate the patient to use bronchodilators exactly as prescribed, especially in the correct sequence when using multiple inhalers (e.g., bronchodilator before corticosteroid).
- It is important to teach the patient to rinse their mouth after inhalation, especially with anticholinergics, to prevent dry mouth and oral thrush.
- The patient should be informed about recognizing early signs of asthma attack and carrying a rescue inhaler at all times.
✅ 4. Monitoring for Side Effects and Toxicity
- The nurse should observe for symptoms of overdose such as tremors, irregular heartbeat, or confusion and report them immediately.
- In case of theophylline use, it is important to monitor serum drug levels periodically to avoid toxicity, as it has a narrow therapeutic index.
✅ 5. Dietary and Lifestyle Advice
- The nurse should counsel the patient to avoid caffeine-containing beverages when on methylxanthines like theophylline to prevent additive CNS stimulation.
- Smoking cessation should be advised as smoking increases metabolism of bronchodilators, reducing effectiveness.
Q.3 Write mechanism of action, indication, adverse effect, contraindication and nursing responsibilies of following drugs (any four)
1. Insulin
Mechanism of Action of Insulin
- Insulin is a naturally occurring hormone produced by the beta cells of the pancreas (Islets of Langerhans), essential for glucose metabolism and energy utilization.
- It acts by binding to insulin receptors on the surface of target cells (like muscle, fat, and liver), which triggers cellular uptake of glucose from the bloodstream.
- In the liver, insulin promotes glycogen synthesis and inhibits gluconeogenesis, helping to store excess glucose and reduce blood sugar levels.
- In muscle and adipose tissue, it enhances glucose uptake, protein synthesis, and fat storage, helping maintain energy balance.
- Insulin also prevents the breakdown of fats and proteins by inhibiting lipolysis and proteolysis, preserving body tissues.
- Exogenous (injected) insulin mimics natural insulin and is used to control hyperglycemia in diabetes mellitus, especially in Type 1 and insulin-dependent Type 2 diabetes.
Indications of Insulin
- Type 1 Diabetes Mellitus
- Type 2 Diabetes Mellitus (when oral hypoglycemics are ineffective)
- Diabetic ketoacidosis (DKA)
- Hyperosmolar hyperglycemic state (HHS)
- Gestational diabetes
- Hyperkalemia (short-term emergency use)
- Perioperative or critical care glycemic control
Adverse Effects of Insulin
- Hypoglycemia (most common; signs include sweating, shakiness, confusion)
- Weight gain
- Lipodystrophy at injection site (lipoatrophy or lipohypertrophy)
- Allergic reaction (rare)
- Hypokalemia (due to shift of potassium into cells)
- Injection site pain or redness
- Insulin resistance (long-term use)
Contraindications of Insulin
- Hypoglycemia (do not administer if blood sugar is already low)
- Hypersensitivity to insulin or formulation components
- Caution in renal or hepatic impairment
- Avoid abrupt discontinuation (risk of DKA)
- Use with caution in patients with adrenal or pituitary disorders
Nursing Responsibilities While Administering Insulin
1️⃣ Assessment Before Administration
- The nurse must check the patient’s blood glucose level using a glucometer before administering insulin, and ensure it is within the appropriate range for injection.
- It is essential to verify the correct type, dosage, and timing of insulin as prescribed, because using the wrong type can cause serious hypo- or hyperglycemia.
2️⃣ Proper Preparation and Technique
- The nurse should ensure insulin is drawn into the syringe correctly, avoiding air bubbles, and if mixing insulins, clear insulin (short-acting) should be drawn before cloudy (intermediate-acting) to avoid contamination.
- It is important to rotate injection sites (abdomen, thighs, arms) to prevent lipodystrophy and ensure proper absorption.
3️⃣ Monitoring and Hypoglycemia Management
- The nurse must closely monitor for signs and symptoms of hypoglycemia (e.g., sweating, confusion, irritability, tremors), especially in patients who are NPO or after exercise.
- In case of hypoglycemia, the nurse should immediately administer fast-acting carbohydrates orally, or IV glucose/glucagon if the patient is unconscious.
4️⃣ Patient Education
- The nurse must teach the patient to self-monitor blood glucose regularly, recognize signs of hypoglycemia and hyperglycemia, and manage them appropriately.
- It is important to instruct the patient on correct storage of insulin, which should be refrigerated when unopened and used within a specified period once opened (usually 28 days at room temp).
5️⃣ Diet and Timing Coordination
- The nurse must ensure that meals are available shortly after administering rapid-acting insulin, as skipping meals can result in hypoglycemia.
- The nurse should also educate the patient to maintain a consistent diet and physical activity routine, and report any illness that could affect glucose control.
6️⃣ Double-checking and Documentation
- It is mandatory for the nurse to double-check insulin doses with another licensed nurse, especially for pediatric or critical care patients, and to document the dose, time, site, and blood glucose levels accurately.
7️⃣ Lab Monitoring and Long-term Care
- The nurse should coordinate with the physician for monitoring HbA1c levels, serum potassium, and renal function, especially in long-term insulin users.
2. Propanolol
Mechanism of Action of Propranolol
- It is a non-selective beta-adrenergic receptor antagonist, which means it blocks both β1 and β2 receptors located in the heart, lungs, and blood vessels.
- By blocking β1 receptors, it decreases the heart rate, myocardial contractility, and cardiac output, which results in a reduction in blood pressure.
- It also reduces renin release from the kidneys, which leads to a decrease in angiotensin II and aldosterone production, thereby lowering blood pressure and fluid retention.
- By blocking β2 receptors in bronchial smooth muscle, it can cause bronchoconstriction, which is why it must be used cautiously in asthma patients.
- It has membrane-stabilizing activity similar to anti-arrhythmic drugs, making it effective in treating arrhythmias.
- It crosses the blood-brain barrier and affects the central nervous system, leading to reduced tremors and prevention of migraine headaches.
Indications of Propranolol
- Hypertension (High Blood Pressure)
- Angina pectoris (Chest Pain)
- Cardiac arrhythmias (e.g., atrial fibrillation)
- Myocardial infarction (Post-MI management)
- Migraine prophylaxis
- Essential tremors
- Hyperthyroidism symptoms (e.g., tachycardia)
- Anxiety (off-label use)
Adverse Effects of Propranolol
- Bradycardia (slow heart rate)
- Hypotension (low blood pressure)
- Bronchospasm or breathing difficulty (especially in asthma patients)
- Fatigue and dizziness
- Depression or mood changes
- Cold extremities (due to vasoconstriction)
- Impotence or sexual dysfunction
- Sleep disturbances or vivid dreams
Contraindications of Propranolol
- Bronchial asthma or COPD (due to risk of bronchospasm)
- Severe bradycardia or heart block
- Hypotension or cardiogenic shock
- Uncompensated heart failure
- Hypersensitivity to propranolol
- Peripheral arterial disease (with caution)
Nursing Responsibilities While Administering Propranolol
1️⃣ Assessment & Monitoring
- It is important for the nurse to assess baseline vital signs, especially heart rate and blood pressure before administering the drug.
- The nurse must hold the dose and notify the physician if pulse is below 60 bpm or if systolic BP is less than 90 mmHg.
- The nurse should closely monitor for signs of heart failure, such as edema, dyspnea, weight gain, or crackles on auscultation.
2️⃣ Patient Safety
- It is necessary for the nurse to advise the patient to rise slowly from sitting or lying position to prevent orthostatic hypotension.
- The nurse must ensure that fall precautions are in place for elderly or weak patients receiving propranolol.
3️⃣ Respiratory Care
- It is essential to monitor for any signs of bronchospasm, wheezing, or breathing difficulty, especially in patients with a history of asthma or lung disease.
4️⃣ Patient Education
- The nurse should educate the patient not to abruptly stop the medication, as it may lead to rebound hypertension or angina.
- It is important to teach the patient about potential side effects like dizziness, fatigue, and cold extremities.
- The nurse must advise the patient to check pulse daily and report any unusual slowing.
5️⃣ Drug Interaction Monitoring
- The nurse should check for drug interactions with calcium channel blockers, digoxin, or insulin (as propranolol may mask hypoglycemia symptoms).
6️⃣ Lab and Follow-up
- The nurse should monitor blood glucose levels in diabetic patients as propranolol may mask signs of hypoglycemia.
- Liver function tests may be required in long-term use to evaluate hepatotoxicity.
3. Adrenaline
Mechanism of Action of Adrenaline
- Adrenaline is a potent non-selective adrenergic agonist that stimulates alpha (α1), beta-1 (β1), and beta-2 (β2) receptors throughout the body.
- By stimulating β1 receptors in the heart, it increases heart rate (positive chronotropic effect), enhances cardiac contractility (positive inotropic effect), and raises cardiac output and blood pressure.
- Through activation of β2 receptors in the lungs, it causes bronchodilation, making it highly effective in acute asthma and anaphylaxis.
- By stimulating α1 receptors in blood vessels, it causes vasoconstriction, which increases systemic vascular resistance and helps raise blood pressure in hypotensive states.
- It also inhibits the release of histamine and other inflammatory mediators during allergic reactions, making it the drug of choice in anaphylaxis.
- In emergency settings, adrenaline helps to restore spontaneous circulation during cardiac arrest by improving perfusion to vital organs.
Indications of Adrenaline
- Anaphylaxis (severe allergic reactions)
- Acute asthma attack (bronchospasm unresponsive to other drugs)
- Cardiac arrest (as part of Advanced Cardiac Life Support)
- Severe hypotension or shock (as a vasopressor)
- Local vasoconstriction (with local anesthetics to prolong action)
- Glaucoma (open-angle, rarely used now)
- Upper airway obstruction (epiglottitis, croup – racemic form)
Adverse Effects of Adrenaline
- Tachycardia and palpitations
- Hypertension
- Headache and dizziness
- Tremors and anxiety
- Arrhythmias or ventricular fibrillation
- Hyperglycemia (due to glycogenolysis)
- Tissue necrosis if extravasated during IV use
- Insomnia or restlessness (with repeated doses)
Contraindications of Adrenaline
- Hypersensitivity to epinephrine
- Uncontrolled hypertension
- Hyperthyroidism (relative contraindication)
- Narrow-angle glaucoma
- Severe cardiac disease (e.g., angina, arrhythmia – relative)
- Inhalational use in patients with closed-angle glaucoma
Nursing Responsibilities While Administering Adrenaline
1️⃣ Emergency Preparedness and Assessment
- The nurse must ensure emergency equipment (oxygen, suction, defibrillator) is readily available, especially when administering adrenaline during cardiac arrest or anaphylaxis.
- It is vital for the nurse to assess baseline vital signs, ECG, and respiratory status prior to administration to evaluate patient condition and anticipate adverse effects.
2️⃣ Correct Dose, Route, and Technique
- The nurse should strictly follow the prescribed route—IM for anaphylaxis, IV for cardiac arrest, SC for mild allergy, and inhalation for croup—because incorrect route may cause serious harm.
- It is crucial to check the correct concentration before administration (e.g., 1:1000 for IM; 1:10,000 for IV in cardiac arrest), as overdose may lead to fatal arrhythmias or severe hypertension.
3️⃣ Monitoring After Administration
- The nurse must closely monitor heart rate, blood pressure, oxygen saturation, and respiratory effort continuously during and after adrenaline administration.
- The nurse should be vigilant for early signs of toxicity, such as chest pain, severe hypertension, or arrhythmias, and take immediate action if such signs appear.
4️⃣ Injection Safety and Site Care
- For IM injection (e.g., EpiPen), the nurse must administer into the mid-anterolateral thigh, not into the buttock, and hold for 10 seconds to ensure full dose delivery.
- In IV use, the nurse must ensure patency of vein and avoid extravasation, as adrenaline leakage can cause local tissue necrosis.
5️⃣ Patient and Family Education
- The nurse must teach patients at risk for anaphylaxis how to use auto-injector (EpiPen), store it correctly, and carry it at all times.
- The nurse should instruct the patient to seek immediate medical help after adrenaline use, even if symptoms improve, as a biphasic allergic reaction may occur.
6️⃣ Documentation and Double-Check
- The nurse must document the exact time, dose, route, reason for administration, and patient’s response, especially in emergency cases for legal and medical accuracy.
- It is mandatory for the nurse to double-check the drug and dilution, especially during high-stress emergencies like resuscitation, to avoid life-threatening errors.
4. Atropine
Mechanism of Action of Atropine
- Atropine is a competitive antagonist of muscarinic acetylcholine receptors, mainly affecting the parasympathetic nervous system.
- It blocks the action of acetylcholine at muscarinic receptors in smooth muscles, exocrine glands, and the central nervous system, thereby inhibiting parasympathetic nerve impulses.
- In the heart, atropine blocks vagal stimulation of the SA node, resulting in increased heart rate (positive chronotropic effect) and improved AV conduction.
- In the respiratory tract, it reduces bronchial secretions and causes bronchodilation by relaxing smooth muscles of the airways.
- In the gastrointestinal and urinary systems, it reduces motility and secretions, causing smooth muscle relaxation.
- It also causes pupil dilation (mydriasis) and cycloplegia (loss of accommodation) by relaxing the sphincter muscle of the iris and the ciliary muscle.
Indications of Atropine
- Bradycardia (symptomatic)
- Pre-anesthetic medication (to reduce secretions)
- Organophosphate or nerve agent poisoning
- Pupil dilation during eye exams or surgery
- Reversal of muscarinic effects of anticholinesterases
- Irritable bowel syndrome or GI hypermotility (rare use)
- Asystole or pulseless electrical activity (as part of ACLS)
Adverse Effects of Atropine
- Dry mouth and dry eyes
- Tachycardia and palpitations
- Blurred vision and photophobia
- Urinary retention
- Constipation
- Confusion or hallucinations (especially in elderly)
- Hyperthermia (especially in children)
- Flushing and skin dryness
Contraindications of Atropine
- Glaucoma (especially narrow-angle)
- Prostatic hypertrophy causing urinary retention
- Myasthenia gravis
- Severe ulcerative colitis
- Paralytic ileus or bowel obstruction
- Hypersensitivity to atropine or belladonna alkaloids
Nursing Responsibilities While Administering Atropine
1️⃣ Assessment Before Administration
- The nurse must assess baseline vital signs, especially heart rate, respiratory status, and pupil size, before administering atropine to monitor for therapeutic and adverse effects.
- It is essential to review the patient’s history for glaucoma, urinary retention, or GI obstruction, as these are important contraindications to atropine use.
2️⃣ Correct Dose and Route Monitoring
- The nurse must ensure that atropine is administered through the correct route—IV for bradycardia, IM for pre-op, SC or IM for poisoning, and ophthalmic for eye exams—as per the condition being treated.
- IV doses should be given slowly over 1 minute, and the nurse should have resuscitation equipment ready in emergency use such as bradycardia or cardiac arrest.
3️⃣ Monitoring and Observation
- The nurse should closely monitor for improvement in heart rate (for bradycardia), pupil response (for ophthalmic use), and drying of secretions (for pre-operative use).
- It is important for the nurse to observe for signs of anticholinergic toxicity, such as confusion, hallucinations, dry skin, or rapid heart rate, and report them immediately.
4️⃣ Patient Education and Safety
- The nurse must instruct the patient that blurred vision and sensitivity to light may occur with eye use and to avoid driving or operating machinery until effects wear off.
- The nurse should teach the patient to increase fluid intake, chew sugarless gum, and use lubricating eye drops if dryness becomes uncomfortable during systemic therapy.
5️⃣ Special Precautions in Pediatrics and Elderly
- The nurse should use extreme caution when administering atropine to children, as they are more prone to hyperthermia and CNS excitation.
- Elderly patients should be monitored for confusion, agitation, or urinary retention, as these adverse effects are more common and more serious in this group.
6️⃣ Emergency Use and Antidote Support
- In organophosphate poisoning, the nurse must administer repeated doses of atropine until secretions dry up and be prepared to give pralidoxime (2-PAM) concurrently as a specific antidote.
7️⃣ Documentation and Communication
- The nurse must document dose, route, time, indication, response, and any adverse effects, and inform the healthcare team of any changes in vital signs or neurologic status.
5. KCL
Mechanism of Action of Potassium Chloride (KCl)
- Potassium chloride acts by replenishing potassium levels in the body, which is essential for normal cellular function, nerve impulse conduction, muscle contraction, and cardiac rhythm.
- Potassium is the major intracellular cation and plays a critical role in maintaining acid-base balance, osmotic equilibrium, and neuromuscular activity.
- KCl provides exogenous potassium to treat or prevent hypokalemia, a condition that can occur due to diuretics, vomiting, diarrhea, or chronic illness.
- It restores normal potassium-dependent enzymatic and electrophysiological activities, especially in the myocardium, where low potassium can cause arrhythmias or cardiac arrest.
- Potassium also influences the resting membrane potential of nerve and muscle cells, thus helping in nerve transmission and muscle function.
Indications of Potassium Chloride (KCl)
- Treatment and prevention of hypokalemia
- Replacement therapy in patients on diuretics (e.g., furosemide)
- Potassium loss due to prolonged vomiting, diarrhea, or gastric suction
- Electrolyte imbalance correction in DKA or renal tubular acidosis
- Prevention of digoxin toxicity (in hypokalemic patients)
- Maintenance in TPN (total parenteral nutrition) therapy
Adverse Effects of Potassium Chloride (KCl)
- Hyperkalemia (muscle weakness, arrhythmias, cardiac arrest)
- Nausea, vomiting, abdominal pain
- Diarrhea or GI irritation (oral form)
- Phlebitis or pain at IV site (IV form)
- ECG changes (peaked T waves, widened QRS)
- Paresthesia, confusion (due to electrolyte imbalance)
Contraindications of Potassium Chloride (KCl)
- Hyperkalemia (serum potassium > 5.5 mEq/L)
- Renal failure or anuria (no urine output)
- Addison’s disease (adrenal insufficiency)
- Severe tissue trauma or burns
- Concomitant use with potassium-sparing diuretics (e.g., spironolactone)
- Dehydration with oliguria
Nursing Responsibilities While Administering Potassium Chloride (KCl)
1️⃣ Assessment Before Administration
- The nurse must assess serum potassium level and renal function (BUN, creatinine, urine output) before giving KCl to prevent dangerous hyperkalemia.
- It is necessary to evaluate for signs of hypokalemia (e.g., fatigue, muscle cramps, weak pulse, ECG changes) and check medication history for potassium-altering drugs.
2️⃣ Preparation and Administration Guidelines
- The nurse should never give KCl undiluted or as IV push, as it may cause sudden cardiac arrest; it must always be diluted and infused slowly via IV drip or infusion pump.
- Oral KCl should be given with food or after meals to minimize gastric irritation, and sustained-release tablets should not be crushed or chewed.
3️⃣ Monitoring and Observation
- The nurse must monitor cardiac rhythm using ECG if the patient is on IV KCl, as it can cause arrhythmias if infused too rapidly.
- The nurse should also monitor for signs of hyperkalemia, including muscle weakness, bradycardia, paresthesia, and ECG changes (tall T-waves, wide QRS).
4️⃣ Patient and Family Education
- The nurse must instruct the patient to avoid potassium-rich foods (e.g., bananas, oranges, potatoes) during KCl therapy unless prescribed.
- The nurse should educate the patient to report signs of weakness, tingling, palpitations, or chest pain, which may indicate potassium imbalance.
5️⃣ IV Site and Drug Compatibility
- The nurse should assess IV site frequently for signs of phlebitis or infiltration, as KCl is irritating to veins and may cause tissue damage.
- It is important to check for drug compatibility before mixing KCl with other IV medications or fluids.
6️⃣ Documentation and Safety Protocols
- The nurse must document the exact dose, route, time, dilution, and patient’s response, especially if given intravenously under supervision.
- The nurse should always double-check with another nurse when preparing or administering concentrated KCl, as it is considered a high-alert medication.
7️⃣ Lab Coordination and Evaluation
- The nurse must coordinate follow-up lab tests, including repeat serum potassium levels, and notify the physician if levels are critically high or low.
- The nurse should evaluate the overall response to therapy, ensuring normalization of potassium levels and symptom relief without complications.
6. 5FU
Mechanism of Action of 5-Fluorouracil (5-FU)
- 5-FU is a cell cycle-specific antineoplastic drug that primarily acts during the S-phase of cell division, targeting rapidly dividing cancer cells.
- It is a pyrimidine analog that is converted inside cells into active metabolites, particularly fluorodeoxyuridine monophosphate (FdUMP).
- FdUMP binds to and irreversibly inhibits thymidylate synthase, an enzyme essential for the synthesis of thymidine, a nucleotide required for DNA replication.
- This blocks DNA synthesis and repair, leading to apoptosis (programmed cell death) of rapidly dividing malignant cells.
- 5-FU may also be incorporated into RNA as fraudulent nucleotides, disrupting protein synthesis, which adds to its antitumor effects.
Indications of 5-Fluorouracil (5-FU)
- Colorectal cancer (commonly used in combination regimens)
- Breast cancer
- Gastric (stomach) cancer
- Pancreatic cancer
- Esophageal cancer
- Head and neck cancers
- Topically for skin conditions like actinic keratosis and superficial basal cell carcinoma
Adverse Effects of 5-Fluorouracil
- Bone marrow suppression (leukopenia, anemia, thrombocytopenia)
- Gastrointestinal toxicity (nausea, vomiting, diarrhea, mucositis)
- Hand-foot syndrome (palmar-plantar erythrodysesthesia)
- Stomatitis and mouth ulcers
- Hair loss (alopecia)
- Photosensitivity and skin rash (especially with topical use)
- Cardiotoxicity (rare but serious)
- Neurotoxicity (confusion, ataxia – rarely)
Contraindications of 5-Fluorouracil
- Hypersensitivity to 5-FU or any of its components
- Severe bone marrow suppression
- Pregnancy and breastfeeding (teratogenic and toxic to fetus)
- Severe liver or renal dysfunction
- Known dihydropyrimidine dehydrogenase (DPD) deficiency (increased toxicity risk)
Nursing Responsibilities While Administering 5-Fluorouracil
1️⃣ Pre-administration Assessment
- The nurse must assess baseline complete blood count (CBC), liver and kidney function tests, and hydration status before administering 5-FU to identify any risk factors for toxicity.
- It is essential to check for previous history of hypersensitivity reactions, nutritional status, and presence of oral ulcers or GI complaints before therapy begins.
2️⃣ Proper Handling and Administration
- The nurse must prepare and administer 5-FU using chemotherapy precautions, including wearing gloves, mask, gown, and using a biological safety cabinet to avoid exposure.
- It is important to administer IV 5-FU through central venous access, especially for continuous infusions, to prevent extravasation and tissue necrosis.
3️⃣ Monitoring and Adverse Effects Management
- The nurse should closely monitor the patient for signs of bone marrow suppression, such as frequent infections, unexplained bruising, and fatigue.
- The nurse must observe for gastrointestinal side effects, such as diarrhea, mucositis, or vomiting, and notify the physician if symptoms are severe.
4️⃣ Oral and Skin Care
- It is essential to provide mouth care with a soft toothbrush and bland rinses to prevent or treat stomatitis and oral ulcers.
- For patients on topical 5-FU, the nurse should educate about skin irritation, sun protection, and proper hand hygiene after application.
5️⃣ Patient and Family Education
- The nurse must teach the patient to report symptoms like severe diarrhea, sore mouth, fever, or unusual bleeding immediately to prevent complications.
- The nurse should also explain contraceptive precautions, as 5-FU is teratogenic, and advise against pregnancy during and several months after therapy.
6️⃣ Follow-Up and Evaluation
- The nurse should ensure regular follow-up for blood tests, especially CBC every week during treatment cycles, and adjust treatment as per hematologic toxicity.
7️⃣ Documentation and Coordination
- The nurse must document dose, route, patient response, and side effects in the medical record and coordinate with oncology and pharmacy departments for drug scheduling and safety.
Section 2
Q.4 Define the following (1×5=5 mark)
1. Asthma
- Asthma is a chronic inflammatory disorder of the airways that causes recurrent episodes of wheezing, breathlessness, chest tightness, and coughing, particularly at night or early in the morning.
- It is characterized by airway hyperresponsiveness, bronchoconstriction, and reversible airflow obstruction, often triggered by allergens, infections, exercise, or environmental irritants.
2. Infarction
- Infarction is the process of tissue death (necrosis) that occurs due to a sudden and complete obstruction of the blood supply to a specific part of the body, usually caused by a thrombus, embolus, or severe vasospasm.
- It most commonly affects organs like the heart (myocardial infarction), brain (cerebral infarction), or lungs, and results in irreversible damage to the affected tissue if not treated promptly.
3. Pathology
- Pathology is the branch of medical science that deals with the study of the nature, causes, mechanisms, and effects of diseases in the body.
- It involves the examination of tissues, organs, body fluids, and autopsies to understand how diseases develop, progress, and affect normal bodily functions, and it forms the scientific foundation for diagnosis and treatment in clinical practice.
4. Mumps
- Mumps is an acute, contagious viral infection caused by the mumps virus (a paramyxovirus), which primarily affects the salivary glands, especially the parotid glands, leading to their painful swelling.
- It commonly occurs in children and adolescents and is transmitted through respiratory droplets or direct contact, and may be prevented by MMR vaccine (Measles, Mumps, Rubella).
5. Alopecia
- Alopecia is a medical condition characterized by partial or complete loss of hair from areas of the body where it normally grows, most commonly affecting the scalp.
- It can result from various causes such as genetic factors, autoimmune disorders (like alopecia areata), hormonal imbalances, nutritional deficiencies, medications, or stress, and may be temporary or permanent depending on the underlying cause.
Q.5 Write short notes on (any four) (5×4=20 mark)
1. Hepatitis
Definition
- Hepatitis is defined as an inflammation of the liver tissue, which may result from viral infections, toxins, autoimmune disorders, alcohol abuse, or certain medications.
- It leads to destruction or injury of liver cells, impairing normal liver functions such as metabolism, detoxification, and bile production.
Etiology / Causes
- Viral infections (Hepatitis A, B, C, D, E)
- Alcoholic liver disease
- Autoimmune hepatitis
- Drugs and toxins (e.g., paracetamol overdose, isoniazid)
- Metabolic disorders
- Blood transfusion with contaminated blood
- Poor sanitation and hygiene (in case of hepatitis A and E)
Pathophysiology
- The causative agent (mostly a hepatotropic virus) enters the liver either through bloodstream, oral ingestion, or direct contact with infected fluids.
- The virus invades hepatocytes, where it replicates, triggering an immune-mediated response.
- The body’s immune system, especially cytotoxic T-cells, attacks infected liver cells causing inflammation, hepatocellular necrosis, and cellular apoptosis.
- Depending on severity, this leads to liver swelling, impaired bile flow, and elevated liver enzymes in the blood.
- Chronic inflammation (especially in Hepatitis B and C) may lead to fibrosis, cirrhosis, and liver failure.
Clinical Manifestations / Signs and Symptoms
- Fatigue and malaise
- Anorexia and nausea
- Jaundice (yellowing of skin and eyes)
- Dark-colored urine
- Clay-colored stools
- Abdominal pain (especially in right upper quadrant)
- Low-grade fever (in viral hepatitis)
- Hepatomegaly and tenderness
Diagnostic Evaluation
- Liver function tests (elevated ALT, AST, bilirubin)
- Serologic tests (HBsAg, Anti-HCV, IgM Anti-HAV)
- Ultrasound of the liver
- Liver biopsy (in chronic cases)
- Prothrombin time and INR
- Complete blood count (CBC)
Medical and Surgical Management
- Rest and supportive therapy is essential in all types.
- Antiviral therapy is prescribed in chronic Hepatitis B or C (e.g., interferons, tenofovir, ribavirin).
- Immunoglobulin injection may be given as post-exposure prophylaxis for Hepatitis A and B.
- Steroids and immunosuppressants are given in autoimmune hepatitis.
- Liver transplant is considered in end-stage liver failure or fulminant hepatic failure.
- Avoidance of alcohol and hepatotoxic drugs is crucial in all types.
Nursing Management
✅ Monitoring and Assessment
- The nurse should regularly monitor vital signs, especially temperature and blood pressure, to detect early signs of liver decompensation or infection.
- It is important to observe for signs of jaundice, pruritus, and changes in urine or stool color, which indicate worsening liver function.
- The nurse must monitor laboratory results of liver enzymes and bilirubin levels to assess disease progression.
✅ Nutritional Support
- The nurse must ensure high-carbohydrate, low-fat, and moderate-protein diet to reduce hepatic workload.
- The patient should be encouraged to consume small, frequent meals to manage nausea and anorexia.
- Adequate hydration must be maintained, especially during vomiting or fever episodes.
✅ Medication Administration and Education
- The nurse must administer prescribed antiviral or immunosuppressive medications as ordered and observe for any side effects.
- It is important to educate the patient not to consume alcohol, herbal medications, or over-the-counter drugs without consulting a physician.
- The nurse should teach the patient about the importance of vaccination for Hepatitis A and B, especially in family members and healthcare workers.
✅Infection Control and Prevention
- The nurse should practice standard precautions including glove use, proper disposal of contaminated needles and body fluids, to prevent transmission.
- The nurse must ensure isolation precautions in acute hepatitis cases if needed.
- Proper handwashing and hygiene education should be reinforced to the patient and caregivers.
✅ Psychological and Emotional Support
- The nurse should provide emotional reassurance, as patients may experience fear due to jaundice, chronic illness, or risk of liver failure.
- It is necessary to promote compliance with long-term follow-up and therapy in chronic hepatitis.
Complications
- Chronic hepatitis
- Liver fibrosis and cirrhosis
- Hepatic encephalopathy
- Hepatocellular carcinoma (especially in HBV and HCV)
- Fulminant hepatic failure
- Portal hypertension and ascites
- Bleeding tendencies due to impaired clotting
2. Peptic ulcer
Definition
A peptic ulcer is a localized erosion or sore in the mucosal lining of the stomach, duodenum, or esophagus, caused by the action of gastric acid and pepsin, leading to tissue injury.
Etiology
- Helicobacter pylori infection
- Chronic NSAID use
- Smoking and alcohol use
- Stress
- Zollinger-Ellison syndrome
- Genetic predisposition
Pathophysiology
- Disruption of mucosal defenses occurs due to H. pylori infection, NSAID use, or other irritants, impairing protective mucus secretion.
- Increased gastric acid and pepsin activity penetrates the weakened mucosal layer, leading to erosion and ulcer formation.
- In response, local inflammation and edema occur, worsening mucosal injury.
- Without treatment, the ulcer can deepen, possibly causing bleeding, perforation, or pyloric obstruction.
- Healing requires restoring balance between aggressive factors (acid, pepsin) and protective factors (mucus, bicarbonate, blood flow).
Clinical Manifestations
- Epigastric pain (burning or gnawing)
- Pain relieved or worsened by food
- Nausea, vomiting
- Bloating
- Hematemesis or melena (in bleeding ulcers)
Diagnostic Evaluation
- History collection
- Physical examination
- Endoscopy (EGD) with biopsy → Gold standard
- Urea breath test / stool antigen test for H. pylori
- Barium meal X-ray
- CBC (anemia if bleeding)
- Occult blood test in stool
Medical Management
1️⃣ Eradication of H. pylori
Triple therapy:
- Proton pump inhibitor (PPI) +
- Clarithromycin +
- Amoxicillin or metronidazole (for 10–14 days)
2️⃣ Acid Suppression
- Proton pump inhibitors (PPIs): Omeprazole, pantoprazole — reduce acid secretion and promote healing.
- H2 receptor blockers: Ranitidine, famotidine — reduce acid production.
3️⃣ Mucosal Protection
- Sucralfate forms a protective barrier over the ulcer site.
- Misoprostol may be used to protect the mucosa, especially in NSAID-induced ulcers.
4️⃣ Lifestyle Modifications
- Avoid NSAIDs, alcohol, smoking, caffeine.
- Eat small frequent meals; avoid spicy and irritating foods.
- Manage stress with relaxation techniques.
Nursing Management
1️⃣ Pain Management
- Assess pain characteristics and provide prescribed analgesics and antacids.
- Monitor response to therapy.
2️⃣ Medication Administration
- Administer PPIs, antibiotics, H2 blockers, and protective agents as prescribed.
- Ensure compliance with full course of H. pylori eradication therapy.
3️⃣ Monitor for Complications
- Observe for GI bleeding: hematemesis, melena, hypotension.
- Watch for signs of perforation: sudden severe abdominal pain, rigidity, tachycardia.
4️⃣ Nutritional Support
- Encourage for nutritious, non-irritating diet.
- Monitor fluid intake/output, especially if vomiting or GI bleeding occurs.
5️⃣ Health Education
- Educate patient on the importance of medication adherence.
- Advise on lifestyle changes to prevent recurrence.
- Teach about early signs of complications and when to seek medical help.
3. HIV
Definition
- HIV stands for Human Immunodeficiency Virus, which is a retrovirus that attacks the body’s immune system, particularly the CD4+ T-helper cells (a type of white blood cell).
- It leads to progressive immune suppression, making the body vulnerable to opportunistic infections and certain cancers.
- If left untreated, HIV infection advances to AIDS (Acquired Immunodeficiency Syndrome), which is the end stage of the disease.
Etiology / Causes
- Transmission through unprotected sexual contact with an infected person
- Sharing of contaminated needles or syringes
- Transfusion of infected blood or blood products
- Mother-to-child transmission during childbirth or breastfeeding
- Needlestick injuries or exposure in healthcare workers
Pathophysiology
- HIV enters the body and targets CD4+ T-lymphocytes, binding to specific receptors using the gp120 protein.
- After entering the cell, HIV uses reverse transcriptase enzyme to convert its RNA into DNA.
- This viral DNA gets integrated into the host’s genome using the integrase enzyme and begins to replicate.
- The virus continues to produce more viral particles, killing CD4+ cells in the process.
- Over time, CD4 count declines, weakening the immune response, leading to increased risk of opportunistic infections, malignancies, and neurological disorders.
- When CD4 count falls below 200 cells/mm³ or AIDS-defining illness develops, the individual is considered to have AIDS.
Clinical Features / Signs and Symptoms
- Fever, night sweats, weight loss
- Fatigue and malaise
- Chronic diarrhea
- Oral thrush (candidiasis)
- Generalized lymphadenopathy
- Skin rashes or lesions
- Opportunistic infections (e.g., tuberculosis, pneumocystis pneumonia)
- Neurological symptoms in advanced stages
Diagnostic Evaluation
- ELISA (Enzyme-linked Immunosorbent Assay) – screening test
- Western blot or PCR test – confirmatory test
- CD4+ T-cell count – to monitor disease progression
- HIV viral load (RNA PCR) – to assess treatment response
- CBC, LFT, RFT – to evaluate systemic involvement
- Tests for opportunistic infections – e.g., TB, hepatitis, etc.
Medical Management
- The cornerstone of treatment is ART (Antiretroviral Therapy) — combination of 3 or more drugs from different classes:
- NRTIs (e.g., zidovudine, lamivudine)
- NNRTIs (e.g., efavirenz, nevirapine)
- PIs (e.g., lopinavir, ritonavir)
- Integrase inhibitors (e.g., dolutegravir)
- Cotrimoxazole prophylaxis is given to prevent certain opportunistic infections like Pneumocystis jirovecii pneumonia.
- Vaccination against hepatitis B, influenza, and pneumococcus is recommended.
- Regular monitoring of CD4 count and viral load is essential for therapy success.
- Treatment for associated infections (e.g., anti-TB, antifungals) is also provided.
Nursing Management
✅ Monitoring and Assessment
- The nurse should monitor vital signs, weight, temperature, and signs of infection on a daily basis.
- It is essential to assess for skin lesions, oral thrush, or signs of TB, which may indicate opportunistic infections.
- The nurse should regularly evaluate adherence to ART therapy and document any side effects.
✅ Infection Control and Prevention
- The nurse must follow standard precautions and use PPE (gloves, masks) to prevent occupational exposure.
- The patient should be educated on safe sex practices, use of condoms, and avoidance of needle sharing.
- Nurses must educate caregivers and family members about universal precautions.
✅ Nutritional and Emotional Support
- The nurse must ensure adequate high-protein, calorie-rich diet to prevent weight loss and maintain immunity.
- It is important to monitor fluid intake and hydration, especially during diarrhea or fever.
- Emotional and psychological support should be provided to help with stigma, depression, or anxiety.
- The nurse should assist in referring the patient to support groups or counseling centers.
✅ Health Education and Adherence
- The nurse must educate the patient on lifelong adherence to ART to achieve viral suppression.
- It is crucial to explain importance of regular follow-up, CD4 monitoring, and early reporting of symptoms.
- For pregnant women, education about PMTCT (Prevention of Mother-to-Child Transmission) protocols is necessary.
Complications
- Acquired Immunodeficiency Syndrome (AIDS)
- Opportunistic infections (e.g., TB, CMV, candidiasis)
- Neurological complications (HIV encephalopathy)
- Malignancies (Kaposi sarcoma, lymphoma)
- Wasting syndrome
- ART-related side effects (e.g., lipodystrophy, hepatotoxicity)
- Social stigma, mental health disorders, and isolation
4. Anemia
Definition of Anemia
- Anemia is a condition in which there is a deficiency in the number of red blood cells (RBCs), hemoglobin concentration, or both, which results in reduced oxygen-carrying capacity of the blood to meet the body’s tissue demands.
- It is typically diagnosed when the hemoglobin level falls below 13 g/dL in men and below 12 g/dL in women, as per WHO criteria.
Etiology / Causes of Anemia
- It is caused by nutritional deficiencies (iron, vitamin B12, folic acid).
- It occurs due to blood loss (trauma, menstruation, GI bleeding).
- It may result from bone marrow suppression or failure.
- It is associated with chronic diseases like kidney failure or cancer.
- It is also caused by increased destruction of RBCs (hemolytic anemia).
Pathophysiology of Anemia
- In anemia, a reduction in red blood cell mass or hemoglobin leads to decreased oxygen delivery to tissues.
- The body tries to compensate through increased cardiac output, respiratory rate, and erythropoietin production, stimulating bone marrow.
- If anemia persists, tissue hypoxia worsens, leading to fatigue, pallor, and organ dysfunction.
- In severe cases, it may result in cardiovascular strain, angina, and heart failure due to chronic hypoxia.
Clinical Manifestations of Anemia
- Fatigue, weakness, and shortness of breath
- Pallor of skin, conjunctiva, and mucous membranes
- Dizziness, headache, and cold extremities
- Palpitations and rapid heartbeat (tachycardia)
- Brittle nails and hair loss (in nutritional anemias)
Diagnostic Evaluation
- Complete Blood Count (CBC) – ↓ Hemoglobin, Hematocrit, RBC count
- Peripheral Blood Smear – shape and size of RBCs
- Serum iron, ferritin, TIBC – for iron deficiency
- Vitamin B12 and folic acid levels
- Bone marrow aspiration (in severe or unexplained anemia)
Medical Management of Anemia
a) Iron Deficiency Anemia
- It is treated with oral or intravenous iron supplements, such as ferrous sulfate.
- Vitamin C is given to enhance iron absorption.
b) Megaloblastic Anemia (Vitamin B12 or Folic Acid Deficiency)
- It is managed with parenteral or oral vitamin B12 and folic acid supplementation.
c) Aplastic or Bone Marrow Failure Anemia
- It may require immunosuppressive therapy, bone marrow transplant, or blood transfusions.
d) Hemolytic Anemia
- It is treated by steroids, immunosuppressants, or splenectomy, depending on cause.
e) Anemia due to Chronic Diseases
- It is managed by treating the underlying condition and recombinant erythropoietin injections if needed.
Nursing Management of Anemia
a) Nutritional Care
- It is important to encourage intake of iron-rich foods such as green leafy vegetables, jaggery, dates, liver, and eggs.
- The nurse must educate the patient about vitamin B12 and folic acid dietary sources, such as dairy, fish, meat, and legumes.
b) Monitoring and Observation
- It is the nurse’s duty to monitor hemoglobin levels, vital signs, and signs of hypoxia such as pallor and breathlessness.
- It is essential to observe for complications like cardiac strain or signs of bleeding in severe anemia.
c) Medication Administration
- The nurse should administer iron and vitamin supplements as prescribed, and educate the patient to avoid taking iron with milk or antacids, which impair absorption.
- Iron injections should be given using the Z-track technique to prevent skin staining.
d) Energy Conservation
- The nurse must advise the patient to take frequent rest periods and avoid strenuous activities until symptoms improve.
- It is necessary to ensure oxygen therapy, if prescribed, to relieve dyspnea and improve oxygenation.
e) Patient Education
- It is important to teach compliance with medications, regular follow-up testing, and dietary modifications.
- Female patients should be educated about menstrual hygiene and managing heavy menstrual flow to prevent recurring anemia.
Complications of Untreated Anemia
- It may lead to heart failure due to increased cardiac workload.
- Severe anemia may result in fetal growth retardation in pregnant women.
- Chronic anemia causes cognitive and developmental delays in children.
- It can cause weakened immunity and increased infection risk.
5. RHD
Definition
- Rheumatic heart disease (RHD) is defined as a chronic condition affecting the heart valves, caused by permanent damage following an episode or multiple episodes of acute rheumatic fever (ARF).
- It is an immune-mediated inflammatory condition, primarily involving the mitral and aortic valves, resulting in valvular stenosis or regurgitation.
Etiology / Causes
- Acute rheumatic fever (post Group A beta-hemolytic streptococcal throat infection)
- Recurrent untreated or partially treated streptococcal pharyngitis
- Poor socio-economic and sanitary conditions
- Lack of access to medical care and antibiotics
- Genetic predisposition in some populations
Pathophysiology
- After an episode of Group A Streptococcal pharyngitis, the immune system generates antibodies against the bacteria.
- These antibodies cross-react with proteins in the heart tissue (molecular mimicry), especially the valves, myocardium, and pericardium.
- This leads to inflammatory lesions (Aschoff bodies) and valvulitis, particularly involving the mitral valve (most common).
- Over time, this causes fibrosis, thickening, and deformity of the heart valves, leading to valvular stenosis or regurgitation.
- This disrupts normal blood flow through the heart, leading to volume overload, heart failure, and arrhythmias.
Clinical Features / Signs and Symptoms
- History of sore throat followed by fever
- Shortness of breath on exertion
- Palpitations
- Chest pain
- Fatigue and weakness
- Swelling of legs (edema)
- Murmurs on auscultation (mitral or aortic valve)
- Signs of congestive heart failure in severe cases
Diagnostic Evaluation
- Throat culture or rapid strep test (for streptococcal infection)
- ECG and chest X-ray
- Echocardiography (to assess valve damage)
- ASO (Anti-Streptolysin O) titer – elevated in rheumatic fever
- ESR and CRP – elevated due to inflammation
- Jones criteria – used to diagnose acute rheumatic fever
Medical and Surgical Management
- Antibiotics (penicillin) to treat residual streptococcal infection and prevent recurrence
- Anti-inflammatory drugs like aspirin or corticosteroids to control inflammation
- Diuretics and ACE inhibitors to manage symptoms of heart failure
- Beta-blockers or digoxin to control heart rate if there is arrhythmia
- Lifelong secondary prophylaxis with benzathine penicillin injections every 3–4 weeks
- Surgical options may include valvotomy, valve repair, or valve replacement in severe cases
Nursing Management
✅ Monitoring and Cardiac Support
- The nurse should monitor vital signs, especially pulse, blood pressure, and signs of heart failure such as pedal edema, breathlessness, and cyanosis.
- It is important to monitor ECG findings, noting any changes in rhythm or conduction.
- The nurse must observe for signs of valve dysfunction, such as worsening murmur or sudden onset dyspnea.
✅ Medication Administration and Compliance
- The nurse must ensure timely administration of prescribed antibiotics, particularly benzathine penicillin injections for secondary prophylaxis.
- It is important to educate the patient and family about lifelong prophylaxis to prevent recurrence of rheumatic fever.
- The nurse should observe for any side effects or allergic reactions to penicillin, such as rash or difficulty breathing.
✅ Fluid Balance and Activity Management
- The nurse should maintain an accurate record of intake and output, especially in heart failure patients.
- It is essential to restrict sodium and fluids in patients showing signs of fluid overload.
- The nurse must encourage graded physical activity, and provide rest during acute illness to reduce cardiac workload.
✅ Health Education and Counseling
- The nurse must provide health education on completing full course of antibiotics for sore throat.
- It is important to teach early signs of streptococcal infection and when to seek care.
- Parents should be encouraged to vaccinate and screen school-age children regularly, especially in endemic areas.
- The nurse should refer the patient for regular cardiac follow-up and echocardiography.
Complications
- Mitral valve stenosis or regurgitation
- Aortic valve involvement
- Congestive heart failure
- Infective endocarditis
- Arrhythmias (especially atrial fibrillation)
- Stroke due to embolism from damaged valves
- Sudden cardiac death (in advanced cases)
Q.6 Write short notes on (any three) (4×3=12 mark)
1. Down syndrome
Definition
- Down Syndrome is a genetic disorder caused by the presence of an extra copy of chromosome 21 (trisomy 21), resulting in intellectual disability, distinctive facial features, growth delay, and multiple congenital abnormalities.
- It is the most common chromosomal abnormality among live-born infants.
Etiology
- Trisomy 21 (nondisjunction during meiosis) – 95% cases
- Translocation involving chromosome 21
- Mosaicism (some cells with trisomy 21, others normal)
- Advanced maternal age (>35 years)
Pathophysiology
- Nondisjunction or chromosomal error during gamete formation results in three copies of chromosome 21 instead of the normal two.
- The presence of an extra chromosome 21 leads to overexpression of genes, causing abnormalities in physical growth and brain development.
- These genetic changes result in characteristic facial features, developmental delays, hypotonia, and congenital heart defects.
- Intellectual disability arises due to altered brain structure and neurodevelopment, typically in the mild to moderate range.
- Other systems like GI tract, endocrine, hematologic, and immune systems may also be affected, increasing risk of various health conditions.
Clinical Manifestations
- Flat facial profile, small nose, and upward slanting eyes
- Hypotonia (poor muscle tone)
- Protruding tongue
- Single palmar crease
- Intellectual disability and delayed milestones
- Short stature
- Congenital heart defects (e.g., AV septal defect)
Diagnostic Evaluation
- Prenatal screening (triple/quadruple test, NIPT)
- Ultrasound (nuchal translucency)
- Karyotyping (definitive test for diagnosis)
- Amniocentesis or chorionic villus sampling (CVS)
- Echocardiogram (to detect cardiac anomalies)
Medical & Surgical Management
- There is no cure for Down syndrome; management focuses on symptom-based, multidisciplinary care to support physical and intellectual development.
- Surgical correction of congenital heart defects or GI anomalies may be required in early life.
- Regular health screening is necessary for conditions like hypothyroidism, vision/hearing problems, and leukemia.
- Early intervention programs including physical, occupational, and speech therapy help improve developmental outcomes.
- Parental counseling, genetic education, and long-term medical support enhance the quality of life.
Nursing Management of Down Syndrome
1. Assessment and Early Detection
- Assess the newborn for typical features of Down syndrome, including hypotonia, facial appearance, and feeding difficulties.
- Perform growth and developmental assessments using Down syndrome-specific growth charts.
- Monitor for signs of cardiac issues (cyanosis, murmur) and refer for early echocardiogram.
- Screen for associated conditions such as hypothyroidism, vision, and hearing impairments.
- Document the child’s developmental progress and alert the healthcare team about delays or concerns.
2. Supportive Care and Medical Follow-Up
- Provide nutritional support for feeding difficulties, which are common due to hypotonia and large tongue.
- Ensure timely immunization and routine health check-ups to prevent infections.
- Coordinate referrals to pediatric cardiology, endocrinology, and speech therapy as needed.
- Administer medications for coexisting conditions (e.g., thyroid hormone) as prescribed.
- Monitor growth, vision, and hearing regularly to detect and treat problems early.
3. Parental Education and Counseling
- Educate parents about the nature of Down syndrome, its challenges, and potential health problems.
- Provide emotional support and grief counseling, especially after diagnosis, to help families adjust.
- Instruct parents on home care strategies, such as safe feeding, hygiene, and developmental play.
- Refer families to Down syndrome support groups and community-based rehabilitation services.
- Promote understanding of the child’s needs and help parents become active participants in care.
4. Developmental and Social Support
- Encourage early stimulation and developmental therapy to promote motor, cognitive, and language skills.
- Support enrollment in early education programs and inclusive schooling.
- Educate families about legal rights, disability benefits, and special education resources.
- Promote self-care, independence, and life skills training as the child grows.
- Help adolescents and adults with Down syndrome plan for vocational support and social integration.
Complication
- Congenital heart disease
- Hypothyroidism
- Hearing and vision impairment
- Increased risk of leukemia
- Obstructive sleep apnea
- Intellectual disability and developmental delay
2. Gentic counseling
Definition of Genetic Counseling
- Genetic counseling is the process by which individuals or families affected by or at risk of a genetic disorder are advised about the nature of the disorder, its inheritance pattern, its possible outcomes, and the options available for management and prevention.
- It is a communication-based, educational, and supportive interaction between the healthcare professional (often a genetic counselor or doctor) and the patient or family, especially in the context of reproductive planning, hereditary disease, or abnormal test results.
Aims and Objectives of Genetic Counseling
- It is to help the individual or couple to understand the medical facts, including diagnosis, progression, and possible treatments of a genetic condition.
- It is to make the person aware of how heredity contributes to the development and recurrence of the disease.
- It is to help individuals understand their risk of transmitting or inheriting genetic conditions.
- It is to assist in making informed decisions about reproduction, prenatal diagnosis, or treatment options.
- It is to provide psychological support and education, reducing anxiety, and helping families cope with the condition.
- It also supports early detection and possible prevention of hereditary diseases.
Indications for Genetic Counseling
Genetic counseling is suggested in the following clinical scenarios :
- If there is a family history of genetic or inherited disorders, such as thalassemia, hemophilia, or cystic fibrosis.
- When a previous child is born with a birth defect or developmental delay.
- In case of recurrent spontaneous abortions or stillbirths, especially if unexplained.
- When there is a consanguineous marriage (marriage between close relatives).
- If the mother’s age is above 35 years, due to increased risk of chromosomal abnormalities like Down syndrome.
- When abnormal results are found in prenatal screening tests like ultrasound or amniocentesis.
- When one or both partners are known carriers of a genetic disease, identified via blood testing.
- If the couple is planning to use assisted reproductive techniques (IVF, ICSI).
- When an individual has a known chromosomal condition like Turner syndrome or Klinefelter syndrome.
Types of Genetic Counseling
Prospective (Preconceptional) Counseling:
- It is done before conception to identify couples at risk and to guide them in reproductive decision-making.
- It is helpful in preventing genetic disorders through carrier screening and prenatal planning.
Retrospective Counseling:
- It is given after the birth of a child with a genetic disorder to assess recurrence risk in future pregnancies.
Prenatal Counseling:
- It is provided during pregnancy if screening indicates fetal anomalies or chromosomal abnormalities.
Postnatal Counseling:
- It is done after birth if the infant shows physical, developmental, or neurological problems.
Directive Counseling:
- In this approach, the counselor provides advice or recommendations about specific options, such as avoiding pregnancy or undergoing IVF with donor eggs.
Nondirective Counseling:
- Here, the counselor provides complete information but allows the individual or family to make their own decisions without influence.
Carrier Counseling:
- It is provided to people who are carriers of genetic mutations but do not have symptoms of the disease.
Predictive or Presymptomatic Counseling:
- It is provided for late-onset disorders like Huntington’s disease, especially if there is a family history.
Steps in the Genetic Counseling Process
Initial Evaluation:
- It involves detailed collection of family history (pedigree chart), medical history, and previous investigations.
Risk Assessment:
- The counselor calculates the probability of disease recurrence or occurrence using genetic principles.
Diagnostic Testing:
- The client is advised on appropriate tests such as karyotyping, molecular DNA testing, amniocentesis, or chorionic villus sampling.
Communication of Results:
- The counselor explains results in understandable terms, including disease severity, inheritance pattern, and management options.
Decision Making:
- The family is helped to choose options such as continuing or terminating pregnancy, IVF, donor programs, adoption, or preparation for special care.
Emotional Support and Follow-up:
- The process involves psychosocial counseling to handle fear, guilt, or stress and planning for long-term follow-up
Role of Nurse in Genetic Counseling
- It is the nurse’s role to collect family history and construct a pedigree chart, helping in the early detection of inherited disorders.
- The nurse must assist in educating patients about genetic conditions, inheritance risks, and available testing or treatments.
- It is the responsibility of the nurse to support the emotional and psychological needs of families dealing with genetic risks.
- The nurse should collaborate with genetic counselors, doctors, and laboratory services to ensure accurate testing and follow-up.
- It is essential for the nurse to maintain confidentiality, respect cultural beliefs, and provide non-judgmental counseling support.
- The nurse may participate in community-based genetic awareness programs, promoting early screening and preventive health.
3. Human genome project
Definition of Human Genome Project
- It is a large-scale international scientific research initiative that was launched in 1990 with the aim to map, sequence, and understand all the genes present in human DNA, collectively known as the human genome.
- It is considered one of the most significant biological projects in history, and it was officially completed in the year 2003.
Objectives / Goals of Human Genome Project
- It was aimed to identify and map all the approximately 20,000–25,000 genes present in human DNA.
- It was launched to determine the complete sequence of the 3 billion DNA base pairs that make up the human genome.
- It aimed to store and improve tools for data analysis and develop new bioinformatics technologies.
- It focused on transferring technologies to other sectors, such as medicine, genetics, and biotechnology.
- It emphasized addressing ethical, legal, and social implications (ELSI) arising from genome research.
Methods Used in Human Genome Project
- It used DNA sequencing technologies, such as Sanger sequencing and automated sequencing machines, to read the order of base pairs.
- It involved physical mapping and genetic mapping to locate genes on chromosomes.
- It required extensive use of computers and bioinformatics to store, analyze, and interpret large amounts of data.
Participants in Human Genome Project
- It was a global collaboration, mainly led by the U.S. National Human Genome Research Institute (NHGRI), with major contributions from UK, Japan, Germany, France, China, and other countries.
- It included both public-sector and private-sector efforts, including companies like Celera Genomics.
Key Findings and Achievements of HGP
- It was found that the human genome contains approximately 3.2 billion base pairs.
- It revealed that humans have only about 20,000 to 25,000 protein-coding genes, which is much fewer than previously expected.
- It discovered that more than 99.9% of human DNA sequences are the same in all people, regardless of race or origin.
- It identified thousands of genetic variants linked to diseases, enabling future advances in personalized medicine.
Applications of Human Genome Project in Health and Nursing
- It helps in the early diagnosis and prevention of many inherited diseases like cystic fibrosis, thalassemia, Huntington’s disease, and cancer.
- It supports the development of personalized treatment plans based on individual genetic makeup (genomic medicine).
- It improves understanding of the genetic basis of drug responses, leading to pharmacogenomics.
- It plays a vital role in genetic counseling, prenatal diagnosis, and carrier screening for hereditary conditions.
Ethical, Legal, and Social Issues (ELSI) of HGP
- It raised concerns about genetic privacy, discrimination by insurance companies and employers, and ownership of genetic information.
- It highlighted the need for informed consent and ethical guidelines in genetic testing and research.
- It emphasized the importance of public education and awareness about genetics.
Importance of HGP for Nurses
- It is important for nurses to understand the basic principles of genetics and genomics to provide accurate health education and genetic counseling.
- It helps nurses to be aware of genetic risk factors, support patients in decision-making, and advocate for ethical use of genetic information.
- It prepares nurses to be a part of interdisciplinary teams in genomic medicine, especially in oncology, pediatrics, reproductive health, and chronic disease care.
4. Importance of genetic nursing
1️⃣ Early Detection and Diagnosis of Genetic Disorders
It is important in genetic nursing to assist in the early identification and diagnosis of inherited diseases, such as Down syndrome, cystic fibrosis, thalassemia, and muscular dystrophy, through genetic screening, family history analysis, and antenatal monitoring.
2️⃣ Participation in Genetic Counseling
It is the responsibility of the genetic nurse to actively participate in genetic counseling sessions to help patients and families understand the nature of genetic disorders, the risk of inheritance, and the probability of recurrence in future generations.
3️⃣ Providing Education to Patients and Families
It is the role of the nurse to educate patients and families in simple language about genetic conditions, including their causes, progression, treatment options, and preventive care, thereby improving their understanding and decision-making capacity.
4️⃣ Psychosocial and Emotional Support
It is essential in genetic nursing to offer emotional support to patients and families, especially when they face a new diagnosis, uncertain prognosis, or difficult choices like pregnancy continuation or termination due to fetal abnormalities.
5️⃣ Promoting Preventive Measures
It is important for the nurse to promote preventive health measures, such as folic acid supplementation, avoidance of known mutagens, and pre-marital or antenatal screening in high-risk populations to reduce the incidence of genetic diseases.
6️⃣ Assisting in Genetic Testing and Procedures
It is the nurse’s responsibility to assist the physician in collecting samples for genetic testing, preparing patients for procedures like amniocentesis, and ensuring proper consent, education, and follow-up care are provided.
7️⃣ Ethical and Legal Guidance
It is important for the nurse to help patients and families navigate ethical issues in genetic testing, such as privacy, confidentiality, discrimination, and the implications of knowing one’s genetic risks.
8️⃣ Supporting Research and Public Health Genetics
It is a valuable contribution of genetic nurses to support genetic research programs and participate in community-based public health genetics, which can identify trends and reduce the disease burden in populations.
9️⃣ Role in Personalized Medicine
It is important in modern nursing to understand genetics because genetic nursing plays a role in tailoring treatment plans according to a person’s genetic profile, especially in conditions like cancer, diabetes, and autoimmune disorders.
1️⃣0️⃣ Improving Quality of Life and Outcomes
It is through genetic nursing that families are empowered to take timely action, begin appropriate treatment, and improve the overall quality of life and health outcomes of individuals affected by genetic disorders.