B.SC-MANAGEMENT NURSING SERVICES-05/07/2017-juhi done-PAPER SOLUTION
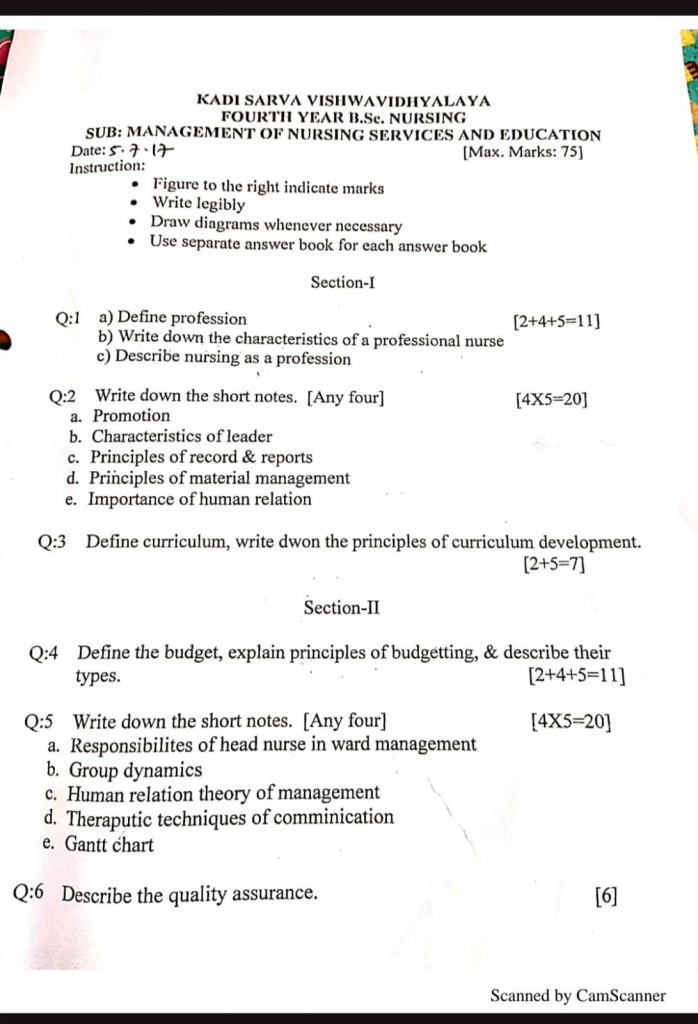
Section-I
Q:1 a) Define profession [2+4+5-11
- A profession is a type of occupation that requires specialized knowledge, formal education, training, and skill, and is governed by a code of ethics and standards of practice.
- A profession is an occupation that requires specialized knowledge, formal education, training, and skills, and is governed by a code of ethics to serve the needs of society in a responsible and accountable manner.
b) Write down the characteristics of professional nurse
A professional nurse is one who possesses scientific knowledge, clinical skills, ethical behavior, and a commitment to patient care, and who practices nursing according to professional standards and code of ethics.
Characteristics of a Professional Nurse
Competence :
• A professional nurse has up-to-date knowledge, clinical expertise, and critical thinking skills necessary for providing safe and effective care.
Accountability and Responsibility :
• Accepts full responsibility for her actions, decisions, and patient outcomes.
• Maintains documentation and follows legal standards of practice.
Compassion and Empathy :
• Understands and shares emotions and concerns of patients, treating them with kindness and respect.
Ethical and Legal Practice :
• Follows the nursing code of ethics, maintains confidentiality, and respects patient rights.
Good Communication Skills :
• Clearly and respectfully communicates with patients, families, and the healthcare team.
• Practices active listening and therapeutic communication.
Lifelong Learning :
• Engages in continuous professional development to improve skills and adapt to advancements in healthcare.
Team Spirit and Collaboration :
• Works efficiently with the healthcare team, promoting coordination and patient-centered care.
Leadership and Decision-Making :
• Demonstrates confidence, problem-solving ability, and leadership, especially in critical situations.
Cultural Sensitivity :
• Respects and accommodates diverse cultural, religious, and personal values of patients.
Professional Appearance and Behavior :
• Maintains neat appearance, punctuality, discipline, and a positive attitude in the workplace.
c) Describe nursing as a profession
Nursing is a profession that involves the scientific care of individuals, families, and communities to promote health, prevent illness, and support recovery. It is based on specialized knowledge, formal education, skill, ethics, and a commitment to public service.
Nursing is Considered a Profession :
Specialized and Scientific Body of Knowledge
Nursing knowledge is drawn from biological sciences (anatomy, physiology, microbiology), social sciences (psychology, sociology), and nursing-specific sciences (nursing theories, clinical practices).
Nurses use evidence-based practices to deliver safe, effective, and personalized care.
Example : A nurse uses pharmacological knowledge to administer medications and psychological theories to counsel a depressed patient.
Formal Education and Training
To become a professional nurse, individuals must undergo structured education in accredited institutions offering:
• Diploma in Nursing (GNM)
• Bachelor of Science in Nursing (BSc Nursing)
• Post Basic BSc Nursing
• Master of Science in Nursing (MSc)
• PhD in Nursing
Training combines classroom learning, clinical rotations, simulation labs, and internships.
Example : Clinical postings during nursing school develop hands-on skills in pediatric, medical-surgical, psychiatric, and community health settings.
Licensure and Regulation
- After graduation, nurses must pass licensure examinations (e.g., NCLEX, State Nursing Council Exams).
- In India, nurses must register with the State Nursing Council, regulated by the Indian Nursing Council (INC) under the Nursing Council Act, 1947.
- Regulation ensures:
- Competency validation
- Standard practice
- Public safety
Code of Ethics and Professional Conduct
- A nurse must adhere to the ethical principles established by national and international bodies like the International Council of Nurses (ICN) and Indian Nursing Council (INC).
- Core ethical values include:
- Autonomy – Respecting patient choices
- Beneficence – Doing good
- Non-maleficence – Avoiding harm
- Confidentiality – Respecting privacy
- Accountability – Taking responsibility
- Example : Maintaining patient confidentiality in a psychiatric ward.
Autonomy in Practice and Professional Accountability
- Nurses make independent decisions within their scope :
- Clinical assessments
- Planning nursing interventions
- Documentation
- Health education
- They are accountable to patients, institutions, and regulatory bodies for their actions.
- Example : A nurse independently adjusts a care plan for a pressure ulcer based on healing progress.
Service Orientation and Altruism
Nursing is deeply rooted in service to humanity, often working in emotionally and physically demanding environments.
Nurses put patients’ well-being above personal interests and are known for empathy, compassion, and holistic care.
Example : Nurses volunteering in disaster zones or during pandemics like COVID-19.
Continuous Professional Development (CPD)
The nursing profession demands lifelong learning to :
Stay updated with medical advances
Maintain licensure
Enhance clinical skills
Nurses attend :
Workshops and Seminars
Continuing Nursing Education (CNE)
Online certifications
Postgraduate studies
Example : Learning about AI in healthcare or advanced cardiac life support (ACLS).
Existence of Professional Organizations
Nurses are supported and guided by professional associations:
TNAI (Trained Nurses Association of India)
ICN (International Council of Nurses)
Nursing Research Society of India
These organizations advocate for:
Nurses’ rights and welfare
Policy-making
Research and professional development
Q:2 Write down the short notes. [Any four] [4X5-20]
a. Promotion
Definition
Promotion is the process of advancing an employee to a higher position in an organization with increased responsibilities, higher status, better pay, and more authority.
Promotion is a significant part of career development and employee motivation. It not only fulfills the individual’s aspiration for advancement but also helps retain talented staff and enhances organizational efficiency. It serves as recognition of merit, experience, and potential.
Purposes of Promotion
• To reward performance and merit – Acknowledges the employee’s contributions.
• To increase job satisfaction and morale – Encourages employees to work harder.
• To fill up higher vacancies internally – Promotes from within, reducing recruitment cost.
• To build loyalty and reduce attrition – Keeps experienced employees in the organization.
• To motivate others – Sets an example for other staff to strive for excellence.
• To utilize potential effectively – Assigns competent individuals to roles requiring leadership.
Types of Promotion
Horizontal Promotion – Change in designation with similar responsibilities and pay.
Vertical Promotion – Upward movement with higher responsibilities, authority, and pay.
Dry Promotion – Change in position/title without increase in salary.
Open Promotion – Available to all eligible staff through a competitive process.
Closed Promotion – Limited to certain departments or units.
Principles of Promotion
Seniority-based – Based on length of service.
Merit-based – Based on skills, performance, and qualifications.
Combined system – A blend of merit and seniority.
Promotion Policy Essentials
Clear criteria and eligibility.
Transparency and fairness.
Based on performance appraisals.
Equal opportunity to all.
Importance in Nursing/Healthcare Setup
Encourages professional development.
Enhances quality of patient care.
Fosters leadership among nurses.
Strengthens team morale and retention.
b. Characteristics of leader
A leader is a person who influences, motivates, and guides others towards achieving common goals. A good leader plays a crucial role in team success and organizational development.
1. Visionary
• A good leader has a clear vision for the future. They set goals and direct the team toward a shared purpose.
Example : A leader in a hospital may envision improved patient care standards and work toward achieving accreditation.
2. Integrity
Honesty, ethics, and moral values are central to leadership. Integrity earns the trust and respect of team members.
Example : A leader who admits mistakes and corrects them rather than hiding them shows integrity.
3. Confidence
A leader must believe in themselves and their team. Confidence boosts morale and encourages others to follow.
Example : During emergencies, confident decisions by the leader prevent chaos and panic.
4. Communication Skills
Effective leaders communicate clearly and actively listen to others.
Example : In nursing, clear communication ensures accurate shift handovers and patient safety.
5. Empathy
Understanding and caring about others’ feelings and perspectives helps a leader build strong relationships.
Example : A nurse leader showing concern for a colleague’s personal struggles fosters teamwork.
6. Decision-Making Ability
Strong leaders are decisive. They gather facts, consider options, and make timely decisions.
Example : During a code blue situation, the leader quickly delegates tasks and makes life-saving choices.
7. Accountability
A leader takes responsibility for their actions and the outcomes of their team.
Example : If a medication error happens, a leader investigates it and ensures preventive measures are implemented.
8. Adaptability
Healthcare and many other fields constantly change. A good leader adjusts strategies as needed.
Example : During the COVID-19 pandemic, leaders modified policies rapidly based on evolving guidelines.
9. Motivational Skills
Leaders encourage and uplift others to reach their highest potential.
Example : A leader who recognizes good work motivates the team to maintain high performance.
10. Delegation Skills
Effective leaders know they can’t do everything alone. They trust others with responsibilities.
Example : A head nurse assigns roles based on strengths — one nurse for wound dressing, another for documentation.
11. Problem-Solving Ability
Leaders face challenges with logical thinking and practical solutions.
Example : In case of staff shortage, the leader quickly reorganizes shifts to ensure patient care is uninterrupted.
12. Inspirational
A leader should serve as a role model by example — in professionalism, punctuality, and ethical behavior.
Example : A nursing educator who continues learning inspires students to pursue lifelong education.
c. Principles of record and report
• Maintaining accurate records and reports is essential in nursing and healthcare to ensure quality care, legal protection, communication, and continuity.
• The following principles guide the preparation, maintenance, and use of records and reports in professional practice:
1. Accuracy
• All information recorded must be correct, exact, and factual.
• Avoid guesswork, assumptions, or vague terms.
• Example : Documenting the exact dose and time of a medication administered.
2. Clarity and Legibility
• Records should be written clearly, using legible handwriting or typed formats.
• Abbreviations should be standardized and understandable.
• Example : Writing “BP – 120/80 mmHg” instead of unclear or smudged notes.
3. Completeness
• A record should include all relevant details — no important data should be omitted.
• It should give a complete picture of the patient’s condition and care.
Example : Recording vital signs, medication given, and the patient’s response.
4. Confidentiality
• Records should be kept private and secure, accessible only to authorized personnel.
• Follow legal and ethical standards to protect patient privacy.
• Example : Not discussing patient details in public areas.
5. Timeliness
• Entries should be made immediately or as soon as possible after the event.
• Late entries can lead to inaccurate recall and legal issues.
• Example : Documenting patient pain level and nursing action right after administration of analgesic.
6. Chronological Order
• Records should be written in the order events actually happened.
• This helps in tracking progress and identifying patterns.
• Example : Recording nursing interventions hour by hour during a critical care shift.
7. Legal Protection
• Records serve as legal documents and should be maintained accordingly.
• Do not leave blanks, erase content, or use correction fluid — draw a line and sign if correction is needed.
• Example : Signing with full name and designation after making an entry.
8. Objectivity
• Records should be objective, not subjective. Avoid personal opinions or emotional statements.
• Focus on observable facts and patient statements.
• Example : Write “Patient stated pain is 8/10” instead of “Patient looked terrible”.
9. Use of Approved Format
• Always follow the standard formats or policies set by the institution or healthcare facility.
• Example : Using SOAP format (Subjective, Objective, Assessment, Plan) in nursing documentation.
10. Standard Terminology
• Use accepted medical terms and nursing jargon.
• Avoid using slang or personal codes that others may not understand.
• Example : Write “dyspnea” instead of “breathing problem”.
d. Principles of material management
Material management refers to the systematic process of planning, procuring, storing, distributing, and controlling materials and supplies in an efficient, cost-effective manner to ensure uninterrupted services — especially in healthcare and nursing settings.
The success of any hospital or health facility depends largely on how well materials are managed. The following principles are crucial :
1. Right Quality
• Only materials that meet quality standards should be selected.
• Quality impacts patient care, safety, and satisfaction.
• Example : Purchasing sterile syringes from certified vendors.
2. Right Quantity
• Neither overstocking nor understocking is ideal.
• Adequate quantity helps maintain optimum inventory without wastage.
• Example : Stocking enough IV fluids based on average monthly usage.
3. Right Time
• Materials must be available when needed to avoid disruption in services.
• Proper scheduling of procurement is essential.
• Example : Ordering blood collection tubes in advance of expected patient load.
4. Right Source
• Purchase from reliable and authorized vendors who ensure quality and timely delivery.
• Helps build long-term trust and accountability.
• Example : Buying drugs from GMP (Good Manufacturing Practice) certified suppliers.
5. Right Price
• The price should reflect the best value for money without compromising quality.
• Competitive quotations and tenders help in cost-effective buying.
• Example : Comparing 3 suppliers before choosing one with best price and warranty.
6. Right Place
• Materials must be delivered to the correct location without delays or misplacement.
• Example : Dispatching oxygen cylinders to the ICU directly instead of the general store.
7. Right Storage
• Proper storage ensures materials are safe from damage, theft, or contamination.
• Environmental conditions (temperature, humidity) must be maintained.
• Example : Vaccines stored in cold chain refrigerators.
8. Right Use
• Materials should be used for their intended purpose only.
• Proper usage avoids misuse, pilferage, or unintentional wastage.
• Example : Using sterile gauze for wound dressing and not for cleaning surfaces.
9. Right Documentation
• Accurate records of all transactions — purchases, issues, usage, and disposal — are vital.
• It aids in audits, stock control, and decision-making.
• Example : Maintaining bin cards and stock registers for medicines.
10. Right Evaluation
• Periodic assessment and review of inventory systems, suppliers, and usage patterns improves performance.
• Example : Annual review of vendor performance and lead times.
e. Importance of human relation
Human relations refer to the interactions and relationships between individuals in a professional, personal, or social setting.
In healthcare, especially nursing and hospital management, strong human relations are essential for effective teamwork, communication, patient satisfaction, and organizational success.
Key Importance of Human Relations
1. Promotes Teamwork
• Positive human relations help build cooperation and trust among team members.
• It improves collaboration between nurses, doctors, patients, and support staff.
• Example : Nurses working together efficiently during emergency care.
2. Enhances Communication
• Good relationships improve both verbal and non-verbal communication.
• It reduces misunderstandings and promotes clarity and transparency.
• Example : Clear communication between nurse and patient helps in better recovery.
3. Boosts Morale and Motivation
• Supportive relationships uplift morale and increase employee motivation and job satisfaction.
• Staff members feel valued and appreciated.
• Example : Recognition by supervisors enhances nurse performance.
4. Increases Productivity
• Happy and motivated employees tend to be more productive and committed.
• Human relations reduce conflict and increase focus on goals.
• Example : Friendly work environment leads to better time management and task completion.
5. Improves Patient Care
• When staff have good human relations, they are more empathetic and caring toward patients.
• This leads to improved patient satisfaction, trust, and outcomes.
• Example : A nurse showing kindness to a fearful patient eases their anxiety.
6. Reduces Conflicts
• Healthy relations create a culture of mutual respect and problem-solving.
• Issues are resolved peacefully and quickly.
• Example : Addressing scheduling issues through discussion instead of arguments.
7. Promotes Personal and Professional Growth
• Good human relations help individuals develop social skills, confidence, and emotional intelligence.
• Encourages feedback, learning, and career development.
• Example : A mentor-nurse guiding a junior staff through professional challenges.
8. Supports Organizational Success
• Strong relationships improve the overall atmosphere, reduce turnover, and help achieve institutional goals.
• Example : A hospital with positive human relations has high staff retention and better patient reviews.
Q:3 Define curriculum, write dwon the principles of curriculum development. [2+5=7]
A curriculum is a planned and organized set of learning experiences and objectives designed to bring about desired educational outcomes. It includes courses, content, teaching methods, evaluation techniques, and learning activities intended for students at various levels. In nursing education, the curriculum covers theoretical knowledge, practical skills, professional behavior, and clinical competencies required for nursing practice.
To develop an effective and meaningful curriculum, certain fundamental principles must be followed:
Key Principles of Curriculum Development
1. Principle of Child-Centeredness / Learner-Centeredness
• The most important principle in curriculum development is that it must revolve around the needs, interests, abilities, and developmental stages of the learners.
• The curriculum should not be rigidly academic but must consider the emotional, physical, and social needs of the students.
• A child-centered curriculum ensures better engagement and participation, making learning more effective
• Example : Using practical demonstrations and clinical simulations in nursing education.
2. Principle of Flexibility
• The curriculum should not be static.
• It should be flexible enough to incorporate new trends, innovations, research, and societal changes.
• Especially in fast-evolving fields like healthcare and technology, curriculum revisions must be done regularly to maintain relevance.
• Example : Integrating telemedicine and digital tools into nursing training.
3. Principle of Activity and Practicality
• Learning must be activity-based and hands-on, not just theoretical.
• Emphasizes doing, practicing, and applying knowledge.
• Example : Including bedside procedures and community health surveys in the syllabus.
4. Principle of Integration
• All subjects and learning areas should be well-integrated and correlated with each other.
• This means connecting theory with practical experiences, and relating academic knowledge with real-world scenarios.
• For instance, in nursing, anatomy must be taught in relation to clinical practice and patient care.
• Example : Teaching pharmacology along with patient care techniques.
5. Principle of Balance
• It should ensure a balanced distribution of knowledge, skills, attitudes, and values.
• Includes cognitive (knowledge), affective (attitudes), and psychomotor (skills) domains.
• Example : Balancing classroom lectures, practical labs, and ethics discussions.
6. Principle of Continuity and Progression
• Learning should be continuous and progressive, moving from simple to complex, and known to unknown.
• The curriculum must be logically sequenced across all levels of education to promote consistent growth in understanding and skills.
• Example : Learning basic anatomy in the first year, followed by advanced pathophysiology in the second year.
7. Principle of Relevance and Utility
• Content should be relevant to the current and future needs of society and the profession.
• The content of the curriculum should be practical and useful in real life. Learners should be able to apply what they learn in day-to-day life or in their profession.
• In vocational and professional courses like nursing, the utility principle ensures employability and skill readiness.
• Example : Including updated protocols for infection control post-COVID-19.
8. Principle of Comprehensiveness
• Curriculum should cover a wide range of areas to ensure overall personality and professional development.
• The curriculum should provide a broad and balanced development — covering cognitive, affective, and psychomotor domains.
• It should not focus only on bookish knowledge, but also on skills, attitudes, values, and personality development.
• Example : Including communication skills, ethics, legal knowledge, and nursing procedures.
9. Principle of Evaluation
• Continuous and comprehensive assessment and evaluation should be part of the curriculum.
• This helps identify what works, what needs change, and how learning outcomes are being met
• Evaluation helps improve both teaching and learning processes.
• Example : Internal assessments, OSCEs, and practical exams in nursing.
10. Principle of Social and National Needs
• Curriculum should align with the cultural, economic, and health needs of the community.
• Must promote national goals like equity, health for all, and scientific temperament.
• Example : Teaching about National Health Programs in Community Health Nursing.
Section-II
Q:4 Define the budget, explain principles of budgetting, & describe their types.[2+4+5=11]
Budget
A budget is a financial plan that outlines the expected income and expenditure for a specific period of time. It is used to allocate resources, control costs, and ensure that spending does not exceed available funds.
A budget is a planned estimate of how much money will be received (income) and how much will be spent (expenses) over a certain time frame (monthly, quarterly, yearly).
Principles of budgetting
Principle of Planning
• A budget should be based on realistic goals and future forecasts.
• It must include short-term and long-term objectives.
Principle of Accuracy
• Estimates of income and expenses should be as accurate as possible using past data and logical assumptions.
• Avoid underestimating or overestimating figures.
Principle of Flexibility
• The budget must allow for adjustments due to unexpected events (like emergencies or price hikes).
• A contingency margin should be included.
Principle of Coordination
• Budgeting should involve all departments or units.
• Promotes team effort and unity in financial planning.
Principle of Participation
• Encourage participation of all stakeholders, including nursing staff, unit heads, and financial officers.
• Increases ownership and responsibility.
Principle of Transparency and Accountability
• Budget details should be clear, documented, and accessible.
• Helps ensure proper use of funds and prevents misuse or corruption.
Principle of Time-Bound Process
• Budgets must be prepared, implemented, and reviewed within a fixed time frame (monthly, quarterly, annually).
Types of budgeting
Incremental Budgeting
Definition :
This is the most traditional and commonly used method. It is based on the previous year’s budget, with adjustments made for the current year (increased or decreased by a fixed percentage).
Features :
• Easy to prepare
• Assumes previous allocations are correct
Used in :
Government hospitals, public health programs
Limitation :
Ignores changing needs or inefficiencies in past budgets
Zero-Based Budgeting (ZBB)
Definition :
In this method, every new budget cycle starts from “zero”, and all expenditures must be justified.
Features :
• Focuses on needs and priorities
• Avoids automatic continuation of previous expenses
Used in :
Project-based organizations, cost-sensitive departments
Limitation :
Time-consuming and complex
Performance Budgeting
Definition :
This type of budget links financial input to measurable results or outcomes.
Features :
• Emphasizes performance and effectiveness
• Budgeting is done based on the output of a department/unit
Used in :
Public health departments, nursing services, NGOs
Limitation :
Requires good data on performance metrics
Programme Budgeting
Definition :
Involves budgeting based on specific programs or services (e.g., maternal health, immunization, ICU services).
Features :
• Helps assess cost-effectiveness of each program
• Useful for multi-departmental projects
Used in :
National health missions, NGO-funded health projects
Limitation :
Complex tracking and allocation across programs
Flexible Budgeting
Definition :
A budget that changes with variations in activity levels, patient volume, or workload.
Features :
• Adaptive to real-time changes
• Useful in unpredictable environments like hospitals
Used in :
Emergency departments, surgical units, OPDs
Limitation :
Needs regular monitoring and adjustment
Fixed (Static) Budgeting
Definition :
A budget set for a specific level of activity and does not change with actual performance.
Features :
• Simple and easy to manage
• Best suited for stable environments
Used in :
• Administrative or maintenance budgets
Limitation :
Ineffective in dynamic environments
Capital Budgeting
Definition :
Focuses on long-term investments, such as construction of buildings, purchase of equipment, or infrastructure upgrades.
Features :
• Involves large financial planning
• Includes cost-benefit analysis
Used in :
Planning MRI machines, ICU setups, ambulance purchases
Q.5 Write down the short note any four [45 = 20]
a. Responsibilities of head nurse in ward management
The Head Nurse (also known as Ward Sister or Nurse Manager) plays a crucial role in the smooth functioning of a hospital ward. She is the link between nursing staff, doctors, administration, and patients, ensuring that quality care is delivered efficiently. Her responsibilities span clinical, administrative, managerial, educational, and supervisory domains.
Responsibilities of Head Nurse
1. Patient Care Management
Ensure that all patients receive safe, timely, and quality nursing care.
Supervise the implementation of doctors’ orders.
Monitor patient hygiene, comfort, and nutritional needs.
Example : Ensuring pressure sore prevention protocols for bedridden patients.
2. Staff Supervision and Coordination
Allocate duties to staff nurses, ANMs, and attendants.
Maintain fair duty rosters (day/night/off duties).
Supervise the work of juniors and provide guidance.
Example : Delegating medication rounds and assigning post-operative patients to skilled nurses.
3. Administrative Duties
Maintain and update all ward records, reports, and registers.
Ensure inventory management (linen, medicines, supplies).
Prepare indents for required materials.
Example : Sending weekly requisitions for IV fluids and antibiotics.
4. Ward Hygiene and Safety
Ensure cleanliness, sterilization, and infection control practices in the ward.
Monitor biomedical waste disposal as per protocols.
Report maintenance issues (lighting, plumbing, broken equipment).
Example : Coordinating with housekeeping staff for immediate cleaning after a patient discharge.
5. Communication and Coordination
Act as a link between doctors, patients, relatives, and hospital administration.
Attend departmental meetings and relay important information to the team.
Coordinate with lab, pharmacy, dietary, and housekeeping departments.
Example : Informing the pharmacy about an urgent medication shortage.
6. Patient Education and Counseling
Educate patients and families about disease conditions, medications, discharge plans, and follow-ups.
Provide emotional support and counseling where needed.
Example : Teaching a diabetic patient about insulin administration before discharge.
7. Training and Professional Development
Conduct and organize on-the-job training, demonstrations, and workshops for staff nurses and students.
Evaluate performance and suggest areas of improvement.
Example : Organizing a CPR training session for nursing interns.
8. Emergency Preparedness
Ensure the ward is ready to handle emergencies (e.g., cardiac arrest, patient fall, fire).
Maintain emergency trolleys, crash carts, and checklists.
Example : Conducting mock drills and checking emergency drug expiry dates.
9. Discipline and Ethics
Maintain discipline, dress code, punctuality, and ethical conduct among the staff.
Address complaints and grievances with fairness.
Example : Counseling a staff member for repeated absenteeism.
10. Documentation and Legal Responsibilities
Maintain accurate documentation of care given, incident reports, consent forms, and staff attendance.
Ensure medicolegal protocols are followed properly.
Example: Reporting and documenting a medication error immediately.
b. Group dynamics
Group dynamics can be defined as the study of the behavioral and psychological processes that occur within a social group or between groups. It involves understanding how groups form, structure themselves, perform, and solve problems together.
Nature and Characteristics of Group Dynamics
Mutual Interaction :
All group members interact frequently, share their views, and influence each other.
Common Goals :
A group works collectively to achieve shared objectives.
Group Cohesion :
Strong sense of belongingness and unity among members.
Group Norms :
Established rules, standards, and values that regulate behavior.
Assigned Roles and Status :
Each member has specific roles and responsibilities based on group hierarchy.
Decision-making :
Group members participate in making decisions—sometimes democratically, sometimes based on leadership.
Components of Group Dynamics
Roles :
Specific duties and responsibilities assigned to members (e.g., leader, recorder, motivator).
Norms :
Shared guidelines or rules for behavior. These develop informally over time.
Status :
Position or rank within the group, often based on experience, skills, or leadership.
Group Size and Structure :
Affects how members communicate and perform tasks. Smaller groups often show better communication.
Cohesiveness :
The degree of unity and commitment members feel toward the group and its goals.
Types of Groups
Formal Group
Definition : Created by an organization or institution to achieve specific goals.
Examples : Hospital management team, infection control committee, nursing audit team.
Purpose : Assigned tasks, defined roles, structured communication.
Informal Group
Definition : Naturally formed by people based on personal relationships and interests.
Examples : Friends among staff nurses, tea-break groups.
Purpose : Provides emotional support, satisfaction, and social interaction.
Primary Group
Definition : A small group with close, personal, and enduring relationships.
Examples : Family, close friends, peer groups.
Features : High emotional attachment, strong influence.
Secondary Group
Definition : A larger, more impersonal group with a specific objective.
Examples : Professional associations, hospital departments.
Features Goal-oriented, formal interactions, less emotional bonding.
Command Group
Definition : A group composed of subordinates reporting to the same supervisor.
Examples : A team of nurses reporting to the head nurse.
Purpose : Fulfills organizational functions and tasks.
Task Group
Definition : Formed for a specific task or project, often temporary.
Examples : Disaster management team, research group.
Purpose : Focused on completing a time-limited assignment.
Interest Group
Definition : Formed by people sharing a common interest or goal.
Examples : Staff union, nursing student association.
Purpose : Advocacy, awareness, or improvement of specific conditions.
Reference Group
Definition : A group individuals compare themselves to for standards or norms.
Examples : Professional role models, ideal nursing units.
Purpose : Influence behavior, career goals, and values.
Stages of Group Development (Tuckman’s Model):
Forming
Members get acquainted. Uncertainty about roles and goals exists.
Storming
Conflicts and power struggles arise. Members challenge authority or ideas.
Norming
Group stabilizes. Norms are established. Trust and collaboration begin.
Performing
Group becomes fully functional, works productively toward goals.
Adjourning
The group disbands after task completion. Members may feel separation anxiety.
Importance of Group Dynamics in Nursing/Healthcare
• Encourages teamwork and interdisciplinary collaboration.
• Enhances communication and cooperation within healthcare teams.
• Essential for conflict resolution, especially in high-stress hospital environments.
• Helps in efficient delegation of duties in patient care.
• Promotes patient safety, effective decision-making, and quality care.
• Supports staff motivation, morale, and reduces burnout.
c. Human relation theory of management
The Human Relation Theory of Management is a management approach that emphasizes the importance of social factors, employee well-being, communication, and group dynamics in the workplace. It marked a shift from the traditional mechanistic view of workers (as seen in scientific management) to a more human-centered approach.
Founder
This theory was developed in the 1930s as a result of the Hawthorne Studies conducted by Elton Mayo and his colleagues at the Western Electric Hawthorne Works in Chicago, USA.
Definition
The Human Relation Theory of Management focuses on understanding how human needs, interpersonal relationships, and worker satisfaction affect productivity. It suggests that people are not just motivated by money but also by social needs, recognition, and a sense of belonging.
Key Assumptions of the Theory
• Workers are social beings, not just machines or tools.
• Informal groups and social interactions influence workplace behavior and productivity.
• Motivation depends on more than just monetary rewards; emotional and social factors play a crucial role.
• Effective communication between management and employees improves performance.
• Supportive supervision and participation lead to job satisfaction.
Major Contributions
• Emphasis on teamwork and cooperation
• Recognition of the psychological and emotional needs of employees
• Importance of leadership style and employee involvement
• Understanding of group dynamics and morale
Hawthorne Studies Summary
These were a series of experiments on worker productivity. The unexpected finding was that workers improved their performance not due to changes in working conditions, but because they felt observed, involved, and valued—known as the Hawthorne Effect.
Relevance in Nursing and Hospital Management
• Encourages open communication between nursing staff and supervisors.
• Promotes employee involvement in planning patient care.
• Improves teamwork and morale in nursing units.
• Reduces job stress and burnout by recognizing individual needs.
• Enhances patient outcomes through motivated and satisfied staff.
Advantages of the Human Relation Theory
• Improves employee satisfaction and motivation
• Builds team spirit and collaboration
• Enhances communication and feedback
• Reduces workplace conflicts
• Leads to better productivity and organizational growth
Limitations
• May underestimate the importance of financial incentives
• Too much focus on feelings over task efficiency
• Difficult to apply in highly technical or rule-bound jobs
d. Theraputic techniques of comminication
Therapeutic communication is a purposeful and goal-directed form of communication used by nurses and healthcare professionals to build a relationship with the patient, promote understanding, and support emotional, psychological, and physical well-being.
Active Listening
• This technique involves giving full attention to the patient by listening with all senses.
• It includes maintaining eye contact, nodding, and avoiding interruptions, which shows respect and builds trust.
• Active listening helps nurses understand the patient’s feelings, concerns, and needs effectively.
Use of Silence
• Silence is a powerful tool that allows the patient time to think, reflect, and express feelings.
• It also shows the nurse’s patience and acceptance.
• This technique is useful when a patient is emotional or needs time to gather their thoughts.
Reflection
• Reflection involves repeating a part of what the patient has said.
• It encourages the patient to continue talking and shows that the nurse is actively engaged.
• For example, if a patient says, “I feel so tired lately,” the nurse may respond, “You feel tired?” to invite further explanation.
Paraphrasing
• This technique involves restating the patient’s message in the nurse’s own words.
• It helps clarify the message and shows that the nurse has understood what the patient meant.
• For instance, if the patient says, “I’m not sure I can handle this treatment,” the nurse might say, “It sounds like you’re worried about how you’ll cope.”
Clarification
• When a message is unclear or vague, the nurse asks for clarification to better understand the patient’s concern.
• For example, saying, “Can you tell me what you mean when you say you feel different?” helps avoid misunderstandings.
Summarizing
• Summarizing involves reviewing key points of the conversation to ensure mutual understanding.
• It helps organize information and confirms that both the nurse and patient are on the same page.
• For example, “So, you’ve been feeling anxious ever since your diagnosis, and you’re worried about the surgery tomorrow.”
Open-ended Questions
• These questions encourage patients to express their thoughts and feelings freely rather than giving just a ‘yes’ or ‘no’ response.
• For example, asking, “How have you been feeling since you came to the hospital?” allows the patient to share openly.
Focusing
• This technique is used to guide the conversation toward important topics or areas of concern.
• It helps manage time and gather relevant information.
• For example, if a patient is discussing several issues, the nurse may say, “Let’s talk more about the chest pain you mentioned.”
Offering Self
• This involves making oneself available to the patient without expecting anything in return.
• It builds trust and shows the nurse’s willingness to support the patient emotionally.
• Saying, “I’m here if you need to talk” is a good example.
Providing Information
• Giving patients factual and relevant information empowers them to make informed decisions about their care.
• It helps reduce anxiety and builds confidence in the healthcare process. For instance, explaining what to expect before a procedure can reduce fear.
e. Gantt chart
A Gantt Chart is a bar chart that represents a project schedule over time. It was developed by Henry L. Gantt in the 1910s and is widely used in project management to illustrate a project’s tasks, timelines, and progress. It helps visualize the start and finish dates of different elements of a project.
Definition
A Gantt Chart is a graphical representation of a project schedule that shows tasks as horizontal bars along a timeline. Each bar represents the start date, duration, and end date of a specific task or activity.
Key Components of a Gantt Chart
Task List
On the vertical axis (left side), all project tasks are listed sequentially.
Time Axis
The horizontal axis represents time (days, weeks, or months) over which tasks are scheduled.
Bars
Horizontal bars show the duration and timing of each task.
Length of the bar indicates time taken for task completion.
Milestones
Important events or goals (marked with symbols like diamonds).
Dependencies
Lines or arrows that connect tasks to show sequence or relationship (e.g., Task B starts after Task A).
Uses of Gantt Chart in Nursing or Hospital Administration
Project Planning – For setting up new wards or implementing health programs.
Task Scheduling – Assigning daily duties to nursing staff.
Training Programs – Organizing workshops, training schedules, etc.
Construction/Setup Planning – For setting up ICUs, OT rooms, or vaccination camps.
Monitoring Progress – Tracking completion of targets in quality assurance or audits.
Advantages of Gantt Chart
• Clear visualization of timelines
• Helps in resource allocation
• Tracks progress and deadlines
• Identifies task dependencies
• Improves team communication and coordination
Limitations
• Can be complex for large projects
• Needs regular updating
• Not ideal for showing task complexity or resource overload
Example
Let’s say a hospital plans to launch a new vaccination campaign. A Gantt chart can show :
Task 1: Planning and Procurement (Week 1–2)
Task 2: Staff Training (Week 2–3)
Task 3: Public Awareness (Week 3–4)
Task 4: Vaccination Drive (Week 4–6)
Each task is plotted as a bar on the chart. The hospital administration can then track progress, assign responsibilities, and monitor delays using the chart.
Q:6 Describe the quality assurance. [6]
Definition
Quality Assurance is a systematic process of evaluating and improving the quality of health care services provided to patients to ensure they meet established standards and deliver safe, effective, and patient-centered care.
Objectives of Quality Assurance
• To improve patient care and safety.
• To ensure compliance with set clinical standards.
• To promote evidence-based practices.
• To identify gaps and areas for improvement.
• To enhance accountability among healthcare staff.
Components of Quality Assurance
Standard Setting:
• Establishing benchmarks and protocols for care.
• Examples: NABH, ISO standards, WHO guidelines.
Assessment:
• Regular audits, patient feedback, checklists, incident reporting.
• Tools : Quality Indicators, Observation tools.
Monitoring:
• Continuous tracking of service quality through indicators like infection rate, medication error rate, etc.
Improvement:
• Implementing corrective measures and training after identifying deficiencies.
Steps in the Quality Assurance Process
• Setting Standards – Defining measurable performance standards.
• Measuring Performance – Auditing and evaluating current practices.
• Comparing Performance with Standards – Identifying gaps.
• Taking Corrective Actions – Developing improvement plans.
• Re-evaluation – Ensuring improvements are sustained.
Types of Quality Assurance Methods:
Retrospective QA after service is delivered (e.g., chart review)
Concurrent QA during service (e.g., bedside audit)
Prospective QA before service (e.g., policy development)
Tools Used in QA
• Clinical audits
• Checklists and protocols
• Peer reviews
• Root Cause Analysis (RCA)
• Quality indicators (infection rate, readmission rate)
Role of Nurse in Quality Assurance
• Follow protocols and standards of care.
• Document care accurately.
• Participate in quality audits.
• Report incidents and errors.
• Engage in continuous education and quality improvement initiatives.
Importance of Quality Assurance in Healthcare
• Improves patient safety and outcomes.
• Builds trust and patient satisfaction.
• Reduces errors and malpractice.
• Enhances efficiency and cost-effectiveness.
• Ensures compliance with legal and accreditation requirements