03/08/2016-B.SC.MEDICAL SURGICAL-1 DONE-UPLOAD NO.6
AHN-1-PAPER SOLUTION NO.6
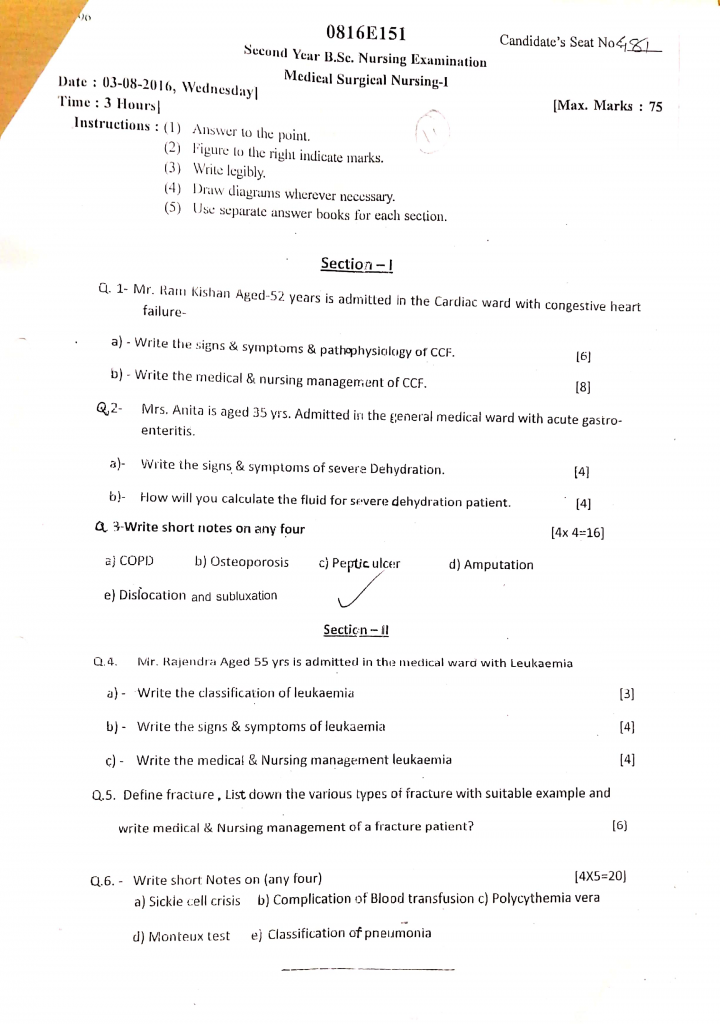
Section 1
Q.1 Mr. Ram kishan aged 52 years is admitted in the cardiac ward with Congestive heart failure
a) Write the sign & symptoms & pathophysiology of CCF (6)
Signs & Symptoms of CCF
Clinical manifestations depend on whether the left side, right side, or both sides of the heart are involved.
A. Left-sided Heart Failure Symptoms
(Pulmonary Congestion Symptoms)
- Dyspnea (shortness of breath) — initially on exertion, later at rest.
- Orthopnea — difficulty breathing while lying flat.
- Paroxysmal Nocturnal Dyspnea — sudden breathlessness at night.
- Cough — dry or frothy sputum (pink-tinged in severe cases).
- Fatigue and weakness due to reduced oxygen delivery.
- Pulmonary crackles (rales) on auscultation.
- Tachypnea — rapid breathing.
B. Right-sided Heart Failure Symptoms
(Systemic Venous Congestion Symptoms)
- Peripheral edema — swelling of feet, ankles, and legs.
- Jugular venous distension (JVD) — visible neck vein distension.
- Hepatomegaly — enlarged, tender liver.
- Ascites — fluid accumulation in the abdomen.
- Weight gain — due to fluid retention.
- Nausea and anorexia — due to GI congestion.
- Nocturia — increased urination at night.
C. General Symptoms of CCF
- Fatigue and weakness.
- Cold extremities due to poor perfusion.
- Decreased exercise tolerance.
- Mental confusion or dizziness in advanced stages.
Pathophysiology of CCF
1️⃣ Initial Cardiac Insult or Disease
- It occurs due to conditions like coronary artery disease, hypertension, valvular heart disease, or cardiomyopathy, which cause damage to the myocardium.
- The reduced myocardial contractility or ventricular stiffness results in incomplete ventricular emptying and inadequate filling during diastole.
- Structural abnormalities of the heart valves (e.g., mitral or aortic regurgitation) further contribute to volume overload and ventricular dysfunction.
2️⃣ Decreased Cardiac Output
- The weakened ventricles are unable to generate adequate stroke volume, resulting in decreased cardiac output and reduced tissue perfusion.
- The body compensates by redistributing blood flow to vital organs such as the brain and heart, but at the expense of renal and peripheral perfusion.
- As cardiac output drops, oxygen delivery to tissues declines, triggering anaerobic metabolism and causing fatigue and weakness.
3️⃣ Sympathetic Nervous System Activation
- To maintain perfusion, the baroreceptors activate the sympathetic nervous system (SNS), increasing heart rate and myocardial contractility.
- SNS also induces vasoconstriction, increasing afterload, which further impairs ventricular emptying and worsens heart failure.
- Chronic SNS activation causes myocardial ischemia, increases arrhythmia risk, and accelerates ventricular remodeling.
4️⃣ Renin-Angiotensin-Aldosterone System (RAAS) Activation
- The kidneys sense reduced blood flow and activate RAAS to conserve sodium and water, increasing intravascular volume.
- This leads to vasoconstriction (via angiotensin II) and fluid retention (via aldosterone), causing increased preload and congestion.
- Persistent RAAS activation also promotes myocardial fibrosis, contributing to ventricular stiffness and progression of heart failure.
5️⃣ Ventricular Remodeling and Hypertrophy
- The heart adapts to increased workload by hypertrophy of myocardial fibers and ventricular dilation.
- These changes temporarily improve cardiac output but ultimately lead to worsened wall stress, impaired filling, and further reduction in contractility.
- Ventricular remodeling increases the risk of ventricular arrhythmias and sudden cardiac death.
6️⃣ Pulmonary and Systemic Congestion
- In left-sided failure, blood backs up into the pulmonary circulation, causing pulmonary edema, dyspnea, and orthopnea.
- In right-sided failure, blood backs up into the systemic venous circulation, causing peripheral edema, ascites, hepatomegaly, and jugular venous distension.
- Chronic congestion leads to organ dysfunction, such as hepatic congestion, renal impairment, and intestinal edema, worsening the patient’s clinical condition.
b) Write the medical and nursing management of CCF (8)
Medical Management of CCF
The primary aim of medical management in CCF is to improve the pumping efficiency of the heart, relieve pulmonary and systemic congestion, prevent disease progression, and enhance the quality of life of the patient.
1️⃣ Pharmacological Management
A. Diuretics
- It is very important to administer loop diuretics such as Furosemide or Torsemide, which help in removing excess fluid accumulated in the lungs and peripheral tissues.
- The use of diuretics leads to reduction of preload, improves the symptoms of dyspnea and edema, and also helps in preventing hospitalization due to worsening heart failure.
B. Angiotensin-Converting Enzyme (ACE) Inhibitors
- It is necessary to use drugs like Enalapril or Ramipril, which reduce the afterload by causing vasodilation and also inhibit the renin-angiotensin-aldosterone system (RAAS).
- ACE inhibitors help in preventing ventricular remodeling, improving cardiac output, and prolonging the survival of the patient.
C. Angiotensin II Receptor Blockers (ARBs)
- In patients who are unable to tolerate ACE inhibitors due to cough or angioedema, it is advised to use ARBs like Losartan or Valsartan, which provide similar hemodynamic and clinical benefits.
D. Beta Blockers
- The administration of Beta blockers such as Metoprolol or Carvedilol is done carefully to slow down the heart rate, reduce myocardial oxygen consumption, and prevent arrhythmias.
- Beta blockers also help in improving left ventricular ejection fraction and have shown to prolong survival in patients with CCF.
E. Aldosterone Antagonists
- The use of Spironolactone or Eplerenone is very effective in counteracting the harmful effects of aldosterone, which includes sodium retention, potassium loss, and fibrosis of cardiac tissue.
- It is especially beneficial in patients with advanced heart failure to improve symptom control and reduce mortality.
F. Digitalis (Digoxin)
- The use of Digoxin helps in increasing myocardial contractility and is particularly useful in patients with atrial fibrillation and CCF to control the ventricular rate and improve symptom relief.
G. Vasodilators
- In selected cases, Hydralazine and Isosorbide dinitrate combination is used to achieve further vasodilation, reduce preload and afterload, and improve exercise tolerance in patients who cannot tolerate ACE inhibitors or ARBs.
H. Anticoagulants and Antiplatelets
- In patients with atrial fibrillation, prosthetic heart valves, or low ejection fraction, the use of anticoagulants (Warfarin) or antiplatelets (Aspirin) is recommended to prevent thromboembolic complications.
2️⃣ Non-Pharmacological Management
- Patients are advised to follow a low-sodium diet to help minimize fluid retention, which is a major contributor to worsening heart failure symptoms.
- In advanced cases, fluid intake may also be restricted to reduce the risk of pulmonary congestion and peripheral edema.
- It is essential to instruct patients to monitor their body weight daily, as a sudden weight gain may indicate fluid retention and impending decompensation.
- Lifestyle modifications such as cessation of smoking, alcohol reduction, and maintaining a regular, supervised exercise program help improve cardiovascular fitness and reduce mortality.
- Continuous patient education is critical to ensure adherence to medications and recognition of early signs of deterioration.
3️⃣ Advanced Therapies
- In patients with conduction system abnormalities and severe heart failure, Cardiac Resynchronization Therapy (CRT) using biventricular pacing improves synchrony of ventricular contractions.
- For patients at risk of sudden cardiac death, an Implantable Cardioverter Defibrillator (ICD) is implanted to terminate life-threatening arrhythmias.
- In very advanced stages, where conventional treatments fail, Left Ventricular Assist Devices (LVAD) may be used as bridge to transplantation or as destination therapy.
- For end-stage heart failure, heart transplantation remains the definitive option.
Nursing Management of CCF
The role of the nurse in the management of CCF is extremely vital, as proper nursing care not only helps to relieve symptoms and improve quality of life, but also aids in the prevention of complications and supports patient and family education for long-term management.
1️⃣ Continuous Assessment and Monitoring
- The nurse should perform regular and thorough assessments to monitor for signs of fluid overload, such as edema in lower limbs, sacral edema (in bedridden patients), pulmonary crackles on auscultation, jugular venous distension (JVD), and rapid weight gain.
- It is important to assess vital signs frequently — blood pressure, heart rate, respiratory rate, and oxygen saturation — as these parameters give valuable information about the patient’s hemodynamic status and oxygenation.
- The nurse must also observe for neurological changes, such as confusion, restlessness, or dizziness, which may indicate decreased cerebral perfusion in advanced CCF.
- Daily weight monitoring should be performed at the same time each day, using the same scale, and with the patient wearing similar clothing — as weight gain is one of the earliest indicators of fluid retention.
- The nurse should also monitor urine output closely and report a decline in output, which could suggest worsening cardiac function or renal impairment.
2️⃣ Oxygen Therapy and Respiratory Support
- The nurse should administer oxygen therapy as prescribed to maintain adequate oxygen saturation and reduce hypoxia, especially in patients experiencing pulmonary congestion or dyspnea.
- The patient should be positioned in high Fowler’s position to improve lung expansion, promote better oxygenation, and reduce the sensation of breathlessness.
- The nurse should encourage the patient to perform deep breathing exercises and coughing techniques regularly to prevent pulmonary infections and atelectasis, which can further compromise respiratory function.
- Close monitoring for signs of increased respiratory distress, such as use of accessory muscles, tachypnea, or cyanosis, is crucial, and these findings should be reported immediately to the physician.
3️⃣ Medication Administration and Monitoring
- The nurse should ensure that prescribed medications, including diuretics, ACE inhibitors, beta blockers, aldosterone antagonists, and digitalis, are administered on time, and she should be vigilant about monitoring for side effects and therapeutic effectiveness.
- While administering diuretics, the nurse should monitor for electrolyte imbalances, particularly hypokalemia, which can lead to cardiac arrhythmias.
- In patients receiving digoxin, the nurse should carefully monitor for signs of digoxin toxicity, such as nausea, vomiting, visual disturbances, bradycardia, and arrhythmias.
- The nurse should also ensure strict adherence to the medication schedule and provide patient education about the importance of medication compliance to prevent exacerbation of heart failure.
4️⃣ Nutritional and Fluid Management
- The nurse should collaborate with the dietician to plan and reinforce a low-sodium diet, as excess sodium can worsen fluid retention and contribute to pulmonary and peripheral edema.
- The patient should be taught how to read food labels and identify hidden sources of salt and processed foods to help maintain dietary compliance.
- In cases where fluid restriction is ordered, the nurse should educate the patient and caregivers about how to measure and distribute fluid intake throughout the day to avoid discomfort and thirst distress.
- The nurse should encourage small, frequent meals to reduce fatigue during eating and prevent abdominal bloating, which can further impair diaphragmatic movement in cases of ascites or hepatic congestion.
5️⃣ Promoting Physical Activity and Energy Conservation
- The nurse should help develop an individualized activity plan in collaboration with the physiotherapist to promote gradual improvement in activity tolerance without overexertion.
- The patient should be taught to recognize early signs of fatigue, shortness of breath, or chest discomfort, and instructed to stop the activity immediately if these symptoms occur.
- It is important to emphasize the importance of balancing periods of rest with activity, especially in the acute phase, to allow the heart to recover and function more efficiently.
- The nurse should help the patient conserve energy by organizing daily tasks and self-care routines in a way that minimizes unnecessary exertion.
6️⃣ Patient and Family Education
- The nurse should provide comprehensive education to the patient and family regarding the nature of CCF, its symptoms, and management plan, to promote better understanding and cooperation.
- The patient should be taught how to perform daily weight monitoring, maintain a fluid and sodium intake diary, and recognize early warning signs, such as increased dyspnea, rapid weight gain, fatigue, decreased urine output, and ankle swelling, which require immediate medical attention.
- The nurse should provide counseling regarding the importance of lifestyle modifications, including smoking cessation, limiting alcohol intake, managing stress, and adhering to regular follow-up appointments.
- The nurse should also encourage family involvement in care, as this helps provide the patient with psychosocial support, which is crucial in managing a chronic illness like CCF.
Q.2 Mrs. Anita is aged 35 years admitted in the general medical ward with acute gastroenteritis.
a) Write the sign & symptoms of severe dehydration (4)
- Extreme thirst
- Dry skin, poor skin turgor
- Sunken eyes
- Dry mouth and tongue
- Low blood pressure (hypotension)
- Rapid heart rate (tachycardia)
- Very low urine output (oliguria/anuria)
- Dark-colored urine
- Dizziness or lightheadedness
- Confusion or irritability
- Rapid, shallow breathing
- Cold and clammy extremities
- Fever (sometimes)
- Weak or thready pulse
- Sunken fontanelle in infants
b) How will you calculate the fluid for severe dehydration patient (4)
1️⃣ First, assess the degree of dehydration properly.
It is very important to confirm that the patient is suffering from severe dehydration, which is indicated by signs such as lethargy, sunken eyes, very dry mouth, poor skin turgor, weak or absent pulse, hypotension, and minimal urine output.
2️⃣ Determine the weight of the patient.
It is essential to weigh the patient accurately in kilograms because all fluid calculations for rehydration are based on body weight.
3️⃣ Know the standard fluid replacement formula.
According to WHO, the general recommendation for fluid replacement in severe dehydration is:
100 ml/kg of body weight over the first 6 hours for infants and over 3 hours for older children and adults.
4️⃣ Calculate the required fluid volume.
It is essential to multiply the patient’s weight (in kg) by 100 ml/kg to determine the total fluid volume needed to correct the fluid loss.
Formula:
Total Fluid Volume (ml) = Body weight (kg) × 100 ml/kg
Example : If a patient weighs 20 kg, then:
20 kg × 100 ml/kg = 2000 ml of fluid needed.
5️⃣ Plan the division of fluid administration.
It is important to divide the total calculated fluid into two phases:
✅ Phase 1 – Initial Rapid Replacement :
Administer half of the total fluid volume in the first 3-6 hours, depending on the patient’s age and clinical condition.
For the above example, 1000 ml is given initially.
✅ Phase 2 – Maintenance and Deficit Replacement :
The remaining half of the fluid (1000 ml in the example) is given over the next 6-12 hours, along with maintenance fluids and ongoing losses (like diarrhea or vomiting).
6️⃣ Choose the type of fluid carefully.
It is recommended to use Ringer’s Lactate or Normal Saline for initial rapid replacement because they help restore intravascular volume and correct electrolyte imbalance effectively.
7️⃣ Monitor the patient continuously.
It is necessary to monitor vital signs, urine output, mental status, capillary refill, and serum electrolytes closely during and after fluid replacement to avoid complications such as fluid overload or electrolyte imbalance.
8️⃣ Adjust fluid calculation for ongoing losses.
It is crucial to replace any ongoing fluid loss (from diarrhea, vomiting, fever, etc.) by adding additional fluids (usually 10 ml/kg per each episode of diarrhea).
9️⃣ Reassess frequently.
It is very important to reassess the clinical status of the patient after 3 and 6 hours and modify the fluid plan accordingly.
Q.3 Write short notes on any four (4×4=16)
a) COPD
Definition
COPD is a progressive, irreversible respiratory disease characterized by chronic airflow limitation due to airway inflammation, parenchymal destruction, and small airway disease, commonly caused by prolonged exposure to noxious particles or gases.
Etiology
- Cigarette smoking (main cause)
- Air pollution
- Occupational dust and chemicals
- Genetic factors (alpha-1 antitrypsin deficiency)
- Recurrent respiratory infections
Pathophysiology of COPD
- Chronic exposure to irritants (like cigarette smoke) causes airway inflammation and damage to lung tissue.
- Inflammatory response leads to mucus hypersecretion and cilia dysfunction, causing airflow obstruction.
- Fibrosis and remodeling of small airways further narrow the bronchioles, increasing airway resistance.
- In emphysema, destruction of alveolar walls results in loss of elastic recoil, air trapping, and lung hyperinflation.
- Reduced alveolar-capillary surface area leads to impaired gas exchange, causing hypoxemia and hypercapnia.
- Chronic hypoxia triggers pulmonary vasoconstriction, which may progress to pulmonary hypertension and right heart failure.
Clinical Manifestations
- Chronic productive cough
- Progressive dyspnea on exertion
- Wheezing and chest tightness
- Fatigue
- Barrel-shaped chest (emphysema)
- Cyanosis in advanced cases
Diagnostic Evaluation
- History collection
- Physical examination
- Pulmonary Function Tests (PFTs) (↓ FEV1/FVC ratio)
- Chest X-ray / CT scan
- ABG (respiratory acidosis, hypoxemia)
- Alpha-1 antitrypsin levels
- Sputum analysis during exacerbations
Medical Management
1️⃣ Bronchodilators
- Inhaled beta-agonists (e.g., salbutamol)
- Anticholinergics (e.g., ipratropium)
- Long-acting bronchodilators for maintenance therapy
2️⃣ Inhaled Corticosteroids
- Used to reduce airway inflammation (e.g., budesonide, fluticasone)
- Often combined with long-acting bronchodilators
3️⃣ Oxygen Therapy
- Long-term oxygen therapy for patients with chronic hypoxemia
- Target oxygen saturation of 88–92%
4️⃣ Antibiotics
- Prescribed during acute exacerbations if infection is suspected
- Commonly used agents: amoxicillin-clavulanate, azithromycin
5️⃣ Mucolytics and Expectorants
- To thin mucus and facilitate its clearance
6️⃣ Pulmonary Rehabilitation
- Includes exercise training, nutrition counseling, breathing techniques, and psychosocial support
Nursing Management
1️⃣ Assessment and Monitoring
- Monitor respiratory rate, oxygen saturation, and ABGs.
- Assess lung sounds for wheezing or crackles.
- Evaluate level of dyspnea and exercise tolerance.
2️⃣ Medication Administration
- Administer bronchodilators and corticosteroids as prescribed.
- Teach correct use of inhalers and nebulizers.
- Monitor for side effects of medications.
3️⃣ Oxygen Therapy
- Administer low-flow oxygen carefully to avoid suppressing respiratory drive.
- Monitor for oxygen toxicity and effectiveness.
4️⃣ Airway Clearance Techniques
- Encourage hydration to thin secretions.
- Teach huff coughing and chest physiotherapy.
- Promote use of positive expiratory pressure devices.
5️⃣ Activity and Nutrition
- Encourage gradual increase in physical activity within tolerance.
- Provide small, frequent meals to avoid fatigue while eating.
- Ensure adequate calorie and protein intake.
6️⃣ Health Education
- Educate about smoking cessation programs.
- Teach early recognition of exacerbation signs.
- Emphasize medication adherence and regular follow-up.
7️⃣ Psychosocial Support
- Provide emotional support for anxiety related to chronic breathlessness.
- Encourage participation in support groups.
b) osteoporosis
Definition
Osteoporosis is a systemic skeletal disorder characterized by low bone mass and deterioration of bone tissue, leading to bone fragility and an increased risk of fractures, especially in the spine, hip, and wrist.
Etiology
- Aging
- Postmenopausal estrogen deficiency
- Inadequate calcium and vitamin D intake
- Sedentary lifestyle
- Corticosteroid therapy
- Smoking and alcohol use
- Genetic predisposition
Pathophysiology
- Bone remodeling imbalance occurs where bone resorption by osteoclasts exceeds bone formation by osteoblasts, leading to net bone loss.
- Estrogen deficiency after menopause accelerates osteoclast activity, increasing bone breakdown.
- Aging reduces osteoblast function, further impairing bone formation.
- The result is porous, thin, and brittle bones with decreased bone mineral density (BMD), making them susceptible to fractures.
- The trabecular (spongy) bone is affected earlier and more severely than cortical bone.
Clinical Manifestations
- Back pain
- Loss of height
- Stooped posture (kyphosis)
- Fractures (hip, spine, wrist) with minimal trauma
Diagnostic Evaluation
- History collection
- Physical examination
- Dual-energy X-ray absorptiometry (DEXA) scan → Gold standard
- Serum calcium, phosphate, vitamin D levels
- Bone turnover markers
- X-ray (shows fractures, reduced bone density)
Medical Management
1️⃣ Calcium and Vitamin D Supplementation
- Adequate intake of calcium (1200–1500 mg/day) and vitamin D (800–1000 IU/day) to support bone health.
2️⃣ Bisphosphonates
- Alendronate, risedronate, ibandronate to inhibit osteoclast-mediated bone resorption.
3️⃣ Hormone Therapy
- Estrogen replacement therapy (ERT) for postmenopausal women (used selectively due to risks).
4️⃣ Selective Estrogen Receptor Modulators (SERMs)
- Raloxifene to mimic estrogen effects on bone without affecting breast or uterine tissue.
5️⃣ Other Agents
- Denosumab (monoclonal antibody) to inhibit osteoclast formation.
- Teriparatide (recombinant PTH) to stimulate new bone formation in severe cases.
Nursing Management
1️⃣ Assessment
- Assess risk factors: family history, menopause, steroid use.
- Monitor for back pain, height loss, and posture changes.
- Evaluate patient’s dietary calcium and vitamin D intake.
2️⃣ Fall Prevention
- Educate on home safety: removing rugs, installing grab bars.
- Encourage assistive devices (canes, walkers) if needed.
- Promote balance and strengthening exercises.
3️⃣ Medication Administration
- Administer bisphosphonates properly (empty stomach, upright position for 30 min).
- Monitor for side effects (GI upset, jaw osteonecrosis with bisphosphonates).
4️⃣ Health Education
- Encourage weight-bearing and resistance exercises (walking, stair climbing).
- Teach about smoking cessation and alcohol moderation.
- Instruct on the importance of medication adherence.
5️⃣ Psychological Support
- Support coping with fracture-related disability or changes in body image.
- Refer to support groups for chronic osteoporosis management.
c) Peptic ulcer
Definition
A peptic ulcer is a localized erosion or sore in the mucosal lining of the stomach, duodenum, or esophagus, caused by the action of gastric acid and pepsin, leading to tissue injury.
Etiology
- Helicobacter pylori infection
- Chronic NSAID use
- Smoking and alcohol use
- Stress
- Zollinger-Ellison syndrome
- Genetic predisposition
Pathophysiology
- Disruption of mucosal defenses occurs due to H. pylori infection, NSAID use, or other irritants, impairing protective mucus secretion.
- Increased gastric acid and pepsin activity penetrates the weakened mucosal layer, leading to erosion and ulcer formation.
- In response, local inflammation and edema occur, worsening mucosal injury.
- Without treatment, the ulcer can deepen, possibly causing bleeding, perforation, or pyloric obstruction.
- Healing requires restoring balance between aggressive factors (acid, pepsin) and protective factors (mucus, bicarbonate, blood flow).
Clinical Manifestations
- Epigastric pain (burning or gnawing)
- Pain relieved or worsened by food
- Nausea, vomiting
- Bloating
- Hematemesis or melena (in bleeding ulcers)
Diagnostic Evaluation
- History collection
- Physical examination
- Endoscopy (EGD) with biopsy → Gold standard
- Urea breath test / stool antigen test for H. pylori
- Barium meal X-ray
- CBC (anemia if bleeding)
- Occult blood test in stool
Medical Management
1️⃣ Eradication of H. pylori
Triple therapy:
- Proton pump inhibitor (PPI) +
- Clarithromycin +
- Amoxicillin or metronidazole (for 10–14 days)
2️⃣ Acid Suppression
- Proton pump inhibitors (PPIs): Omeprazole, pantoprazole — reduce acid secretion and promote healing.
- H2 receptor blockers: Ranitidine, famotidine — reduce acid production.
3️⃣ Mucosal Protection
- Sucralfate forms a protective barrier over the ulcer site.
- Misoprostol may be used to protect the mucosa, especially in NSAID-induced ulcers.
4️⃣ Lifestyle Modifications
- Avoid NSAIDs, alcohol, smoking, caffeine.
- Eat small frequent meals; avoid spicy and irritating foods.
- Manage stress with relaxation techniques.
Nursing Management
1️⃣ Pain Management
- Assess pain characteristics and provide prescribed analgesics and antacids.
- Monitor response to therapy.
2️⃣ Medication Administration
- Administer PPIs, antibiotics, H2 blockers, and protective agents as prescribed.
- Ensure compliance with full course of H. pylori eradication therapy.
3️⃣ Monitor for Complications
- Observe for GI bleeding: hematemesis, melena, hypotension.
- Watch for signs of perforation: sudden severe abdominal pain, rigidity, tachycardia.
4️⃣ Nutritional Support
- Encourage for nutritious, non-irritating diet.
- Monitor fluid intake/output, especially if vomiting or GI bleeding occurs.
5️⃣ Health Education
- Educate patient on the importance of medication adherence.
- Advise on lifestyle changes to prevent recurrence.
- Teach about early signs of complications and when to seek medical help.
d) Amputation
Definition
- Amputation is defined as the surgical removal of a limb or part of a limb through bone or joint due to disease, trauma, or congenital defects.
- It is a procedure done to save life, relieve pain, or remove diseased tissue that cannot be salvaged.
Indications of Amputation
- It is performed in case of severe trauma or crush injury to a limb.
- It is indicated for gangrene or severe infection that is unresponsive to treatment.
- It is required in presence of peripheral vascular disease with ischemia and non-healing ulcers.
- It may be done for malignant tumors of bones or soft tissue.
- It is sometimes necessary for congenital deformities or birth defects.
- It may be indicated in severe frostbite or burns causing irreversible tissue death.
Types of Amputation
1️⃣ Based on Level of Limb Involved
Upper Limb Amputations:
- It includes finger amputation, partial or complete hand amputation, wrist disarticulation, forearm (below-elbow) amputation, elbow disarticulation, upper arm (above-elbow) amputation, shoulder disarticulation.
- It may also involve forequarter amputation, which includes removal of the entire arm along with part of the shoulder girdle when indicated for malignancy.
Lower Limb Amputations:
- It includes toe amputation, partial foot amputation (such as transmetatarsal amputation), ankle disarticulation (Syme’s amputation), below-knee amputation (BKA), above-knee amputation (AKA), hip disarticulation, and hemipelvectomy (removal of entire leg with part of pelvis).
- It may also include knee disarticulation, which is amputation performed through the knee joint, preserving the femur.
2️⃣ Based on Surgical Approach
Open Amputation (Guillotine Amputation):
- It is performed when there is active infection or severe sepsis, where closure of the wound is delayed to allow drainage.
- It is considered as a life-saving emergency procedure when sepsis is spreading rapidly.
Closed Amputation (Flap Amputation):
- It is done when infection is controlled or absent; skin and soft tissue flaps are created to cover the bone and form a stump suitable for prosthesis.
- It may also involve myodesis (suturing of muscles to bone) or myoplasty (suturing of muscle to muscle) to enhance stump stability.
3️⃣ Special Types of Amputation
Re-amputation:
- It is done when the original amputation stump has not healed properly, due to infection, poor circulation, or necrosis of the stump tissues.
- It may also be required if the stump shape is unsuitable for prosthetic fitting.
Revision Amputation:
- It is performed to reshape the stump for better prosthetic fitting, improve function, or manage pain from neuroma formation.
- It may also address contractures or poor skin coverage of the original stump.
Nursing Management
1️⃣ Pre-operative Nursing Care
- It is important for the nurse to assess the patient’s understanding of the procedure and provide psychological support.
- The nurse should explain the surgery and expected outcomes to reduce fear and anxiety.
- It is necessary to ensure consent is obtained and pre-operative tests are completed.
- The nurse must teach deep breathing, coughing exercises, and stump care post-operatively.
- It is important to encourage verbalization of feelings regarding loss of limb and body image.
2️⃣ Post-operative Nursing Care
- It is the nurse’s responsibility to monitor vital signs and watch for signs of hemorrhage or infection.
- The nurse should manage pain effectively, including phantom limb pain, using medications and comfort measures.
- It is important to keep the stump elevated to reduce swelling initially.
- The nurse should perform stump dressing changes using sterile technique as per protocol.
- It is essential to monitor for complications such as infection, delayed healing, or contractures.
- The nurse should encourage active and passive range of motion exercises to prevent contractures.
- It is necessary to provide nutritional support for wound healing.
- The nurse should facilitate early mobilization and involvement of physiotherapy.
- It is important to provide emotional support and refer to counseling services as needed.
- The nurse should coordinate prosthetic fitting and rehabilitation once healing permits.
e) Dislocation and subluxation
Definition
Dislocation
It is a condition in which the bones forming a joint are completely displaced from their normal anatomical alignment. It results in loss of contact between articular surfaces of the joint.
Subluxation
It is a condition where there is partial displacement or incomplete separation of the articular surfaces of the joint. Some contact between joint surfaces remains intact.
Types of Dislocation
1️⃣ Congenital Dislocation
- It is present at birth due to developmental defect.
- Example: Congenital dislocation of the hip.
2️⃣ Traumatic Dislocation
- It occurs due to injury or external force (fall, accident).
- Example: Shoulder dislocation due to sports injury.
3️⃣ Pathological Dislocation
- It occurs secondary to diseases such as arthritis, tumor or infection.
- Example: Dislocation due to tuberculosis of the joint.
4️⃣ Recurrent Dislocation
- It is repeated dislocation of the same joint due to weakness or laxity of ligaments.
- Example: Habitual shoulder dislocation.
Common Sites of Dislocation and Subluxation
- Shoulder joint
- Elbow joint
- Hip joint
- Knee joint
- Finger joints
- Temporomandibular joint (jaw)
Etiology (Causes)
- Trauma (fall, sports injury)
- Congenital anomalies
- Weak ligaments
- Joint diseases (arthritis)
- Muscle paralysis
Signs & Symptoms
- Severe pain at joint
- Visible deformity
- Swelling and bruising
- Inability to move joint
- Shortening of limb (in hip dislocation)
- Loss of function
Diagnostic Evaluation
- Clinical examination
- X-ray of joint
- MRI or CT scan (if soft tissue injury suspected)
Medical Management
1️⃣ Closed Reduction
- It is performed by manually manipulating the joint back into position under anesthesia or sedation.
- It is the first line of treatment for most simple dislocations.
2️⃣ Open Reduction
- It involves surgical repositioning of the joint if closed reduction is unsuccessful or contraindicated.
- It is indicated in cases of recurrent dislocations or when there is associated fracture.
3️⃣ Immobilization
- It is achieved by applying a splint, cast, or brace to stabilize the joint and allow soft tissue healing.
- The duration of immobilization depends on the joint involved and severity of injury.
4️⃣ Pain Management
- It is important to administer analgesics (e.g., paracetamol) and NSAIDs to relieve pain and inflammation.
- Opioids may be considered in severe cases for short-term pain control.
5️⃣ Rehabilitation
- It involves physiotherapy to restore joint strength, flexibility, and range of motion.
- Progressive exercises help in preventing joint stiffness and recurrence.
Nursing Management
1️⃣ Immediate Care
- It is the nurse’s priority to assess and maintain circulation, movement, and sensation distal to the injury.
- The nurse should assist in immobilizing the joint and preparing the patient for reduction procedure.
- It is important to monitor vital signs and pain level continuously.
2️⃣ Post-Reduction Care
- The nurse should monitor neurovascular status regularly after reduction.
- It is essential to educate the patient about the importance of immobilization and compliance with brace or sling use.
- The nurse should administer prescribed analgesics and anti-inflammatory medications.
- It is necessary to apply ice packs to reduce swelling.
- The nurse should encourage gradual mobilization and refer to physiotherapy for rehabilitation.
- It is also important to teach the patient about strengthening exercises to prevent future dislocation.
- The nurse should provide emotional support and reassure the patient regarding prognosis and prevention of recurrence.
Section 2
Q.4 Mr. Rajendra aged 55 yrs is admitted in the medical ward with leukaemia
a) Write the classification of leukaemia (3)
1️⃣ Acute Lymphoblastic Leukemia (ALL)
- It is a malignancy of immature lymphoid precursor cells (lymphoblasts).
- It is the most common leukemia in children, especially between 2–5 years of age.
- It leads to the uncontrolled accumulation of lymphoblasts in bone marrow and blood.
- It is associated with symptoms like fatigue, fever, pallor, bone pain, hepatosplenomegaly, and CNS involvement.
- It is treated with intensive chemotherapy, and prognosis is generally good in children.
2️⃣ Acute Myeloid Leukemia (AML)
- It is a malignancy of myeloid precursor cells (myeloblasts).
- It is the most common acute leukemia in adults, especially above 60 years.
- It causes rapid accumulation of immature myeloid cells, leading to bone marrow failure.
- It presents with anemia, infections, bleeding, gum hypertrophy, and skin infiltration.
- It is treated with intensive chemotherapy and stem cell transplantation in selected patients.
3️⃣ Chronic Lymphocytic Leukemia (CLL)
- It is a malignancy of mature lymphocytes (mainly B-cells).
- It is more common in elderly men above 60 years of age.
- It leads to gradual accumulation of functionally inactive lymphocytes in blood, bone marrow, and lymphoid organs.
- It is associated with fatigue, weight loss, recurrent infections, lymphadenopathy, and splenomegaly.
- It is a slowly progressive disease, and treatment depends on symptoms and stage.
4️⃣ Chronic Myeloid Leukemia (CML)
- It is a malignancy of mature myeloid cells such as granulocytes.
- It is commonly seen in middle-aged adults between 30–60 years.
- It is caused by the Philadelphia chromosome (t[9;22]), which activates the BCR-ABL tyrosine kinase.
- It presents with splenomegaly, fatigue, weight loss, night sweats, and gout.
- It is managed with tyrosine kinase inhibitors (TKIs) like imatinib, which provide excellent control of the disease.
b) Write the sign and symptoms of leukaemia (4)
- Fatigue and weakness
- Pallor (pale skin due to anemia)
- Frequent infections (due to low immunity)
- Fever (often unexplained)
- Bleeding tendencies (bruises, petechiae, nosebleeds, gum bleeding)
- Bone and joint pain
- Swollen lymph nodes
- Enlarged liver and spleen (hepatosplenomegaly)
- Unintentional weight loss
- Night sweats
c) Write the medical and nursing management leukaemia (4)
Medical Management of Leukemia
1️⃣ Chemotherapy
- It is the main treatment modality for most types of leukemia.
- It involves the use of cytotoxic drugs to kill rapidly dividing leukemic cells.
- Common chemotherapy drugs include vincristine, daunorubicin, cytarabine, methotrexate, etc.
- It is administered in induction, consolidation, and maintenance phases to achieve complete remission.
2️⃣ Radiation Therapy
- It is used in selected cases, such as CNS prophylaxis in ALL or to reduce splenomegaly.
- It involves the use of targeted radiation to destroy leukemic cells in specific areas.
- It may also be used before bone marrow transplantation as part of conditioning.
3️⃣ Targeted Therapy
- It is a newer treatment that targets specific molecules involved in leukemia.
- In CML, tyrosine kinase inhibitors (TKIs) like imatinib are used to block the BCR-ABL protein.
- Targeted therapy is better tolerated and more specific compared to traditional chemotherapy.
4️⃣ Immunotherapy
- It uses the body’s immune system to fight leukemia.
- Monoclonal antibodies (e.g., rituximab) are used in CLL to target abnormal B-cells.
- CAR-T cell therapy is an advanced form of immunotherapy in refractory cases.
5️⃣ Bone Marrow / Stem Cell Transplantation
- It is performed in cases of relapsed or high-risk leukemia.
- It involves replacing the patient’s diseased bone marrow with healthy stem cells from a donor or autologous source.
- It allows the patient to receive high-dose chemotherapy or radiation, followed by infusion of healthy stem cells.
6️⃣ Supportive Therapy
- It includes blood transfusions to treat anemia and thrombocytopenia.
- Antibiotics, antivirals, and antifungals are used to prevent or treat infections.
- Colony-stimulating factors (e.g., G-CSF) are used to stimulate white blood cell production.
Nursing Management of Leukemia
1️⃣ Assessment and Monitoring
- It involves regular assessment of vital signs, especially temperature, to detect infections early.
- It includes monitoring complete blood counts (CBC), electrolytes, and renal and hepatic functions.
- It requires careful observation for signs of bleeding, such as petechiae, bruising, and hematuria.
2️⃣ Infection Prevention
- It includes maintaining a strict aseptic technique during procedures.
- It involves providing protective isolation if required to prevent exposure to infections.
- It emphasizes hand hygiene for both healthcare staff and visitors.
- It involves educating the patient and family about avoiding crowds and sick contacts.
3️⃣ Bleeding Prevention
- It involves avoiding invasive procedures unless absolutely necessary.
- It includes using a soft toothbrush, avoiding rectal temperatures or enemas, and handling the patient gently.
- It ensures careful monitoring of platelet counts and arranging for platelet transfusions when needed.
4️⃣ Nutritional Support
- It involves providing a high-protein, high-calorie diet to meet increased metabolic demands.
- It includes encouraging small, frequent meals to manage anorexia and nausea.
- It ensures that safe and hygienic food is provided to reduce the risk of infections.
5️⃣ Fatigue Management
- It involves allowing the patient to rest when fatigued and encouraging energy conservation techniques.
- It provides emotional support and reassurance during periods of extreme weakness.
- It encourages gradual mobilization as tolerated.
6️⃣ Psychosocial Support
- It provides emotional support to the patient and family.
- It involves addressing anxiety, fear, and depression associated with leukemia and its treatment.
- It includes referring the patient to counseling services or support groups if needed.
7️⃣ Patient and Family Education
- It includes educating the patient about treatment protocols and possible side effects.
- It involves teaching about infection prevention at home and importance of follow-up care.
- It provides guidance on nutrition, activity levels, and managing treatment side effects.
8️⃣ Palliative and End-of-Life Care (if required)
- It involves providing symptom relief and ensuring comfort and dignity in terminal cases.
- It supports the family through grief counseling and end-of-life decision-making.
Q.5 Define fracture, List down the various types of fracture with suitable example and write medical and nursing management of a fracture patient? (6)
Definition of Fracture
- Fracture is defined as a break or disruption in the continuity of a bone, either partial or complete.
- It may occur due to direct trauma, twisting injury, repetitive stress, or disease-related weakness.
- Fracture healing depends on factors such as age, nutritional status, and blood supply to the bone.
Types of Fracture
1️⃣ Closed (Simple) Fracture
- The bone breaks but does not pierce the skin.
- It is less prone to infection.
- Example: Hairline fracture of tibia after a fall.
2️⃣ Open (Compound) Fracture
- The broken bone end protrudes through the skin, causing an open wound.
- It carries a high risk of infection and requires urgent surgical care.
- Example: Compound fracture of femur in a road traffic accident.
3️⃣ Comminuted Fracture
- The bone is shattered into multiple fragments.
- It usually results from high-energy trauma such as car crashes.
- Example: Comminuted fracture of femur after a crush injury.
4️⃣ Greenstick Fracture
- One side of the bone bends, while the other side breaks.
- It is commonly seen in children due to soft, flexible bones.
- Example: Greenstick fracture of radius in a child after a playground fall.
5️⃣ Transverse Fracture
- The fracture line is horizontal across the bone.
- It occurs commonly due to direct blow or bending forces.
- Example: Transverse fracture of the humerus after a direct fall.
6️⃣ Oblique Fracture
- The fracture line runs at an angle across the bone.
- It is caused by a rotational or twisting force.
- Example: Oblique fracture of fibula due to sports injury.
7️⃣ Spiral Fracture
- The bone is twisted apart, producing a helical fracture line.
- It is commonly caused by rotational forces, often in sports.
- Example: Spiral fracture of tibia from skiing accident.
8️⃣ Impacted Fracture
- The broken ends of the bone are driven into each other.
- It is commonly seen in arm or leg injuries due to falls.
- Example: Impacted fracture of femoral neck in an elderly patient.
9️⃣ Compression Fracture
- The bone is compressed or crushed, leading to collapse.
- Commonly occurs in vertebrae of elderly patients with osteoporosis.
- Example: Compression fracture of thoracic vertebrae in an osteoporotic patient.
10️⃣ Pathological Fracture
- It occurs in a bone weakened by disease, such as cancer, infection, or osteoporosis.
- It may happen with minimal trauma or spontaneously.
- Example: Pathological fracture of femur in a patient with bone metastasis.
Medical Management of Fracture
1️⃣ Initial Assessment & Stabilization
- The patient is assessed for life-threatening injuries (ABCs) first.
- The fractured limb is immobilized using splints or traction to prevent further damage.
- Neurovascular checks are done frequently.
2️⃣ Pain Management
- Analgesics such as paracetamol, NSAIDs, or opioids are used as needed.
- Positioning and cold application help reduce pain and swelling.
3️⃣ Reduction of Fracture
- Closed reduction is performed for simple fractures under sedation or anesthesia.
- Open reduction is required for complex or displaced fractures, followed by internal fixation.
4️⃣ Immobilization
- It includes cast application, splinting, or external fixation.
- Immobilization duration depends on type of fracture, age, and healing potential.
5️⃣ Surgery (ORIF)
- Open reduction and internal fixation are used for unstable fractures.
- Devices such as plates, screws, intramedullary rods, or external fixators are used to maintain alignment.
6️⃣ Rehabilitation
- Physical therapy begins with range of motion (ROM) exercises as soon as possible.
- It helps in preventing stiffness, muscle atrophy, and regaining strength.
7️⃣ Prevention of Complications
- Measures include infection control, DVT prophylaxis, and pressure ulcer prevention.
- The patient is monitored for compartment syndrome and delayed union or nonunion of the fracture.
Nursing Management of Fracture Patient
1️⃣ Pain Management
- Pain level is assessed regularly using a pain scale.
- The nurse provides analgesics as prescribed and ensures comfortable limb positioning.
- Cold packs are applied in the acute phase to reduce swelling.
2️⃣ Immobilization Care
- The nurse ensures the cast or splint is properly positioned and not too tight.
- Frequent neurovascular checks (pulse, color, sensation, temperature, capillary refill) are performed.
- The patient is educated on cast care and signs of complications.
3️⃣ Prevention of Infection
- Aseptic technique is maintained during dressing changes.
- The surgical wound is monitored for redness, warmth, drainage, and foul odor.
- The patient is taught about personal hygiene and wound care.
4️⃣ Monitoring for Complications
- The nurse observes for deep vein thrombosis (DVT) signs, such as leg pain or swelling.
- Monitoring includes checking for pressure ulcers in immobilized patients.
- The nurse is alert for signs of fat embolism syndrome (dyspnea, confusion, petechiae).
5️⃣ Mobility and Rehabilitation
- The patient is encouraged to begin passive and active exercises as per doctor’s advice.
- The nurse assists with gradual ambulation when allowed.
- Coordination with physiotherapists is done to optimize recovery.
6️⃣ Nutritional Support
- The nurse ensures a diet rich in calcium, protein, and vitamin D to promote bone healing.
- Adequate fluid intake is encouraged to prevent constipation related to immobility.
- The patient is monitored for nutritional deficiencies.
7️⃣ Patient and Family Education
- The nurse teaches the patient about fracture healing, cast care, and activity restrictions.
- The family is educated about signs of infection, circulation problems, and when to seek help.
- The nurse emphasizes the importance of completing rehabilitation and attending follow-up visits.
Q.6 Write short notes (any four) (4×5=20)
a) Sickle cell crisis
Definition
Sickle cell crisis is an acute painful episode occurring in individuals with sickle cell disease, caused by sickling of red blood cells under certain triggers, leading to vascular occlusion, ischemia, and organ damage.
Etiology
- Hypoxia (low oxygen levels)
- Dehydration
- Infection
- Emotional or physical stress
- Exposure to cold
- High altitude
Pathophysiology
1️⃣ The HbS gene mutation causes abnormal sickle-shaped RBCs that become rigid and sticky under low oxygen or stress conditions.
2️⃣ Sickled RBCs tend to adhere to blood vessel walls, causing microvascular occlusion and reducing blood flow.
3️⃣ The resultant ischemia leads to severe pain, tissue damage, and release of inflammatory mediators.
4️⃣ Sickled RBCs have a short lifespan, causing chronic hemolytic anemia and increasing circulating free hemoglobin, which worsens vascular injury.
5️⃣ Recurrent episodes of sickling damage endothelial cells, promoting vasculopathy and predisposing to complications like stroke, acute chest syndrome, and organ failure.
Clinical Manifestations
- Severe limb and joint pain
- Fever
- Fatigue
- Shortness of breath
- Jaundice
- Swelling of hands and feet (dactylitis)
- Priapism in males
Diagnostic Evaluation
- History collection
- Physical examination
- CBC (low Hb, high reticulocyte count)
- Peripheral smear (shows sickled cells)
- Hemoglobin electrophoresis (confirms HbS)
- Bilirubin and LDH (elevated in hemolysis)
- Chest X-ray if chest syndrome is suspected
Medical Management
1️⃣ Pain Management
- Administer opioid analgesics (morphine) for severe pain.
- Use NSAIDs for mild to moderate pain.
- Apply non-pharmacologic pain relief (warm compresses, relaxation).
2️⃣ Hydration Therapy
- Provide IV fluids to reduce blood viscosity and improve circulation.
- Encourage adequate oral fluid intake.
3️⃣ Oxygen Therapy
- Administer supplemental oxygen to prevent hypoxia and further sickling.
4️⃣ Infection Control
- Start empiric antibiotics if infection is suspected.
- Ensure vaccinations (pneumococcus, H. influenzae, meningococcus).
5️⃣ Blood Transfusion
- Used in severe anemia, stroke, or acute chest syndrome.
- Exchange transfusion may be needed in life-threatening cases.
6️⃣ Disease-Modifying Therapies
- Hydroxyurea increases fetal hemoglobin (HbF), reducing sickling frequency.
- L-glutamine reduces oxidative stress and crisis frequency.
- Stem cell transplant offers potential cure in selected cases.
Nursing Management
1️⃣ Pain Assessment and Relief
- Assess pain using pain scales; administer analgesics as prescribed.
- Provide emotional support during pain episodes.
2️⃣ Hydration and Oxygenation
- Monitor fluid balance and administer IV fluids.
- Maintain oxygen therapy and monitor oxygen saturation.
3️⃣ Monitoring for Complications
- Monitor for signs of acute chest syndrome (chest pain, cough, hypoxia).
- Observe for stroke symptoms: weakness, speech changes.
- Assess for splenic sequestration (abdominal distension, hypotension).
4️⃣ Education and Health Promotion
- Educate patient and family about avoiding triggers (cold, dehydration, stress).
- Teach importance of medication adherence (hydroxyurea).
- Encourage regular follow-up and vaccination compliance.
5️⃣ Psychosocial Support
- Provide emotional and psychological support for chronic illness coping.
- Facilitate participation in support groups.
b) complications of blood transfusion
- Blood transfusion is a life-saving procedure in which whole blood or its components (such as packed red blood cells, plasma, platelets) are administered to a patient to replace lost components.
- However, blood transfusion is not without risks — it may cause various complications, some of which can be life-threatening.
- It is very important for nurses and healthcare professionals to be aware of these complications to enable early detection, prevention, and prompt management.
I. Immediate (Acute) Complications
1️⃣ Acute Hemolytic Transfusion Reaction (AHTR)
- It is one of the most serious and potentially fatal complications caused by ABO incompatibility.
- The patient’s immune system attacks the donor red blood cells, causing intravascular hemolysis.
- Symptoms include chills, fever, chest pain, back pain, hypotension, hemoglobinuria, and shock.
- If not treated promptly, it can lead to renal failure and death.
2️⃣ Febrile Non-Hemolytic Transfusion Reaction (FNHTR)
- This is a common reaction caused by recipient antibodies reacting to donor leukocytes or cytokines.
- The patient may experience fever, chills, headache, nausea, vomiting, and malaise during or shortly after transfusion.
- Although not life-threatening, it causes significant discomfort and should be properly managed.
3️⃣ Allergic Reaction (Urticarial Reaction)
- Caused by recipient hypersensitivity to plasma proteins in the donor blood.
- Symptoms include urticaria (hives), rash, pruritus (itching), flushing, and sometimes angioedema.
- Severe allergic reactions may progress to anaphylaxis, causing hypotension, bronchospasm, dyspnea, and shock.
4️⃣ Anaphylactic Reaction
- It is a rare but severe allergic reaction, often seen in IgA-deficient patients receiving blood from IgA-positive donors.
- The patient may rapidly develop hypotension, respiratory distress, cyanosis, wheezing, and cardiac arrest.
- It requires immediate discontinuation of transfusion and administration of epinephrine.
5️⃣ Transfusion-Related Acute Lung Injury (TRALI)
- TRALI is a serious and life-threatening complication caused by antibodies in donor plasma that activate recipient neutrophils in the pulmonary vasculature.
- It leads to non-cardiogenic pulmonary edema and presents with acute respiratory distress, hypoxia, hypotension, and fever during or within 6 hours of transfusion.
- Immediate supportive care and oxygen therapy are required.
6️⃣ Bacterial Sepsis
- Occurs when contaminated blood products (especially platelets stored at room temperature) are transfused.
- The patient develops high fever, chills, hypotension, nausea, vomiting, and signs of septic shock.
- Requires urgent treatment with broad-spectrum antibiotics and hemodynamic support.
II. Delayed Complications
7️⃣ Delayed Hemolytic Transfusion Reaction
- Occurs days to weeks after transfusion, due to recipient’s immune response against minor antigens on donor red blood cells.
- Symptoms may be mild or unnoticed, including low-grade fever, jaundice, and gradual drop in hemoglobin.
- It is usually detected during post-transfusion follow-up.
8️⃣ Graft-versus-Host Disease (GVHD)
- A rare but almost always fatal complication seen in immunocompromised patients.
- Transfused donor lymphocytes attack recipient tissues.
- Symptoms include fever, rash, liver dysfunction, diarrhea, and pancytopenia.
- Prevention involves using irradiated blood products in high-risk patients.
9️⃣ Iron Overload (Hemosiderosis)
- Occurs in patients receiving multiple transfusions (e.g., in thalassemia, sickle cell disease).
- Excess iron gets deposited in organs such as liver, heart, and pancreas, causing organ dysfunction.
- Management includes iron chelation therapy (Desferrioxamine).
10️⃣ Transmission of Infections
- Although modern screening techniques have reduced the risk, blood transfusion can still transmit infections, such as:
- Hepatitis B virus (HBV).
- Hepatitis C virus (HCV).
- Human Immunodeficiency Virus (HIV).
- Syphilis.
- Malaria (in endemic areas).
c) Polycythaemia vera
Definition
- Polycythemia vera (PV) is a chronic, progressive myeloproliferative disorder characterized by an abnormal increase in red blood cell mass due to clonal proliferation of hematopoietic stem cells in the bone marrow.
- It often also results in increased white blood cells and platelets, causing hyperviscosity of blood and risk of thrombosis.
Etiology
- Mutation in JAK2 gene (JAK2 V617F)
- Unknown trigger (idiopathic)
- Associated with myeloproliferative neoplasms
- Rare familial cases
Pathophysiology of Polycythemia Vera
- Mutation in the JAK2 gene leads to constant activation of the JAK-STAT pathway.
- This causes uncontrolled production of red blood cells in the bone marrow.
- Increased RBC mass results in hyperviscosity of blood (thick blood).
- White blood cells and platelets may also increase, adding to circulatory problems.
- Blood flow slows down, increasing the risk of thrombosis and reduced tissue oxygenation.
- Splenomegaly occurs as the spleen tries to manage excess blood cells.
- Over time, the disease may progress to bone marrow fibrosis or acute leukemia.
Clinical Manifestations
- Headache, dizziness
- Pruritus (especially after warm bath)
- Ruddy complexion (plethora)
- Splenomegaly
- Fatigue
- Thrombotic events (DVT, stroke)
Diagnostic Evaluation
- History collection
- Physical examination
- Hematocrit level (Elevated hematocrit >52% (men), >48% (women))
- CBC (Increased hemoglobin, RBC count)
- Positive JAK2 mutation test
- Bone marrow biopsy (hypercellularity)
- Serum erythropoietin (Low or suppressed serum erythropoietin (EPO))
Medical Management
1️⃣ Phlebotomy
- First-line treatment to reduce hematocrit below 45%.
- 500 mL of blood is removed weekly initially, then every 1–3 months.
- Helps in reducing blood viscosity and improving symptoms.
2️⃣ Myelosuppressive Therapy
- Hydroxyurea is commonly used to suppress bone marrow activity and control blood cell counts.
- Interferon-alpha may be used in younger patients or in pregnant women.
- Newer agents like ruxolitinib (JAK2 inhibitor) are used for refractory or high-risk cases.
3️⃣ Symptom Management
- Antihistamines for pruritus.
- Low-dose aspirin to prevent thrombotic events by improving blood flow.
- Management of hyperuricemia with allopurinol if needed.
4️⃣ Monitoring and Prevention
- Regular monitoring of CBC (complete blood count), iron stores, and coagulation profile.
- Patients advised to avoid dehydration, maintain mobility, and avoid risk factors for thrombosis.
- Educate on signs of thrombosis such as leg swelling, chest pain, or neurological symptoms.
Nursing Management
1️⃣ Monitoring and Assessment
- Monitor hematocrit, hemoglobin, platelet count, and JAK2 mutation status.
- Assess for signs of thrombosis or bleeding.
- Monitor for splenomegaly and its complications.
2️⃣ Assist with Phlebotomy
- Prepare patient for regular phlebotomy sessions.
- Monitor for hypotension or dizziness post-procedure.
- Provide hydration before and after the procedure.
3️⃣ Medication Administration
- Administer hydroxyurea or interferon as prescribed.
- Monitor for drug side effects (e.g., cytopenias with hydroxyurea).
- Educate patient on compliance with medication regimen.
4️⃣ Patient Education
- Teach importance of regular follow-up and monitoring.
- Advise on maintaining hydration and avoiding factors that increase blood viscosity.
- Encourage physical activity to promote circulation.
- Educate on early signs of thrombosis and bleeding and when to seek medical help.
5️⃣ Psychosocial Support
- Provide emotional support for patients coping with a chronic disease.
- Address concerns about risk of leukemia transformation or side effects of long-term treatment.
- Facilitate support group referrals if needed.
Complications
- Thrombosis (deep vein thrombosis, stroke, myocardial infarction)
- Bleeding tendency due to platelet dysfunction
- Gout due to hyperuricemia
- Splenomegaly and abdominal discomfort
- Progression to myelofibrosis or acute leukemia (rare but serious)
d) Monteux test
Definition
- The Mantoux test is a diagnostic skin test used to detect latent or active infection with Mycobacterium tuberculosis (the bacteria that causes tuberculosis — TB).
- It involves the intradermal injection of a small amount of purified protein derivative (PPD) and observing the skin’s immune reaction to it.
- A positive reaction suggests that the person has been sensitized to tubercle bacilli either through infection or vaccination (BCG).
Purpose of the Mantoux Test
- To detect latent TB infection in individuals who are asymptomatic.
- To help in the diagnosis of active TB disease, along with other clinical and laboratory findings.
- To screen high-risk populations for TB exposure (such as healthcare workers, close contacts of TB patients, immunocompromised individuals).
- To support public health efforts in TB control and prevention.
Procedure of Mantoux Test
1️⃣ Preparation
- The test should be performed by a trained healthcare professional using sterile technique.
- A standard dose of 0.1 ml of PPD containing 5 tuberculin units (TU) is prepared.
2️⃣ Administration
- The volar aspect of the forearm is selected and cleaned.
- Using a 26 or 27-gauge intradermal needle, 0.1 ml of PPD is injected intradermally to produce a small, raised wheal (6–10 mm diameter).
- The patient is instructed not to scratch or cover the site.
3️⃣ Reading the Test
- The test site is examined 48 to 72 hours after administration.
- The healthcare provider measures the diameter of induration (raised, hard area), not the redness, in millimeters.
Interpretation of Results
✅ Positive Reaction
- It is indicated by an induration of ≥10 mm in normal individuals or ≥5 mm in immunocompromised individuals (e.g., HIV-positive, organ transplant recipients).
- It suggests that the person has been infected with Mycobacterium tuberculosis, but it does not differentiate between active and latent TB.
✅ Negative Reaction
- It is indicated by induration less than 5 mm.
- It suggests no prior exposure or infection or anergy (weakened immune response).
Advantages
- It is an easy, inexpensive, and safe test to perform.
- It helps in screening individuals at risk of TB in community and hospital settings.
Limitations
- It may give false-positive results in individuals vaccinated with BCG.
- It may give false-negative results in immunocompromised patients or in very early TB infection.
- It cannot differentiate between latent TB and active TB disease.
Nursing Responsibilities
1️⃣ Pre-Procedure Responsibilities
- It is the nurse’s responsibility to verify the doctor’s order for Mantoux Test and check the correct dose and type of PPD to be used.
- It is important for the nurse to explain the purpose of the test to the patient to reduce anxiety and obtain verbal consent.
- The nurse should assess the patient’s medical history, especially any history of BCG vaccination, allergy, immunocompromised condition, or previous TB infection.
- It is the nurse’s duty to prepare the sterile equipment, including 1 ml tuberculin syringe with 26–27 gauge needle and PPD solution.
- The nurse should select the appropriate injection site, typically the inner surface of the forearm, and cleanse it using aseptic technique.
2️⃣ During the Procedure
- It is essential for the nurse to perform the intradermal injection correctly by inserting the needle at a 5 to 15-degree angle just under the skin.
- The nurse should ensure that a small wheal (bleb) forms, indicating that the injection was correctly intradermal.
- It is the nurse’s responsibility to avoid massaging the site after injection to prevent spreading of the PPD solution.
- The nurse should document the date and time of injection and the site used accurately in the patient’s record.
- The nurse should inform the patient about possible local skin reaction and advise not to apply any lotion or cover the site.
3️⃣ Post-Procedure Responsibilities
- It is the nurse’s duty to instruct the patient to return after 48 to 72 hours for reading of the test result.
- The nurse should emphasize that redness is not to be measured — only induration (hard, raised area) is to be measured for result interpretation.
- It is important for the nurse to observe the patient for any signs of allergic reaction or systemic symptoms, though rare.
- The nurse should ensure the reading is done by palpating the area gently with fingertips and using a ruler to measure the widest transverse diameter of induration.
- It is the nurse’s responsibility to record the size of the induration in millimeters accurately in the patient’s chart.
4️⃣ Patient Education Responsibilities
- The nurse should teach the patient not to scratch, rub, or apply any ointment at the test site.
- It is necessary for the nurse to educate the patient that a positive test does not always indicate active TB — further tests are required.
- The nurse should inform the patient that a negative result does not completely rule out TB if the patient is immunocompromised.
- The nurse should also advise that some individuals with previous BCG vaccination may have a positive Mantoux test result.
- It is important for the nurse to encourage follow-up consultation with the physician after the test result is recorded.
e) Classification of pneumonia
Pneumonia is classified in various ways based on site of acquisition, causative organism, clinical presentation, and anatomical pattern.
1️⃣ Classification Based on Site of Acquisition
A. Community-Acquired Pneumonia (CAP)
- It occurs outside hospital settings and is typically caused by Streptococcus pneumoniae or respiratory viruses.
- It may occur suddenly in healthy individuals after exposure to infection.
- Many cases are seen seasonally, particularly in winter months.
B. Hospital-Acquired Pneumonia (HAP)
- Develops 48 hours or more after hospital admission, with patients showing new pulmonary infiltrates on X-ray.
- It is commonly associated with endotracheal tubes, prolonged hospital stay, and broad-spectrum antibiotic use.
- It leads to increased length of hospital stay and higher healthcare costs.
C. Ventilator-Associated Pneumonia (VAP)
- Occurs after 48 hours of mechanical ventilation, usually due to aspiration of secretions around the endotracheal cuff.
- The pathogens are often multi-drug resistant, making treatment difficult.
- Biofilm formation on endotracheal tubes is a significant factor in VAP pathogenesis.
D. Healthcare-Associated Pneumonia (HCAP)
- It occurs in patients with frequent hospital contacts, such as those on home infusion therapy, wound care, or dialysis.
- The infection is caused by organisms similar to those in HAP, including Pseudomonas and MRSA.
- It is frequently associated with poor outcomes due to delayed diagnosis.
2️⃣ Classification Based on Causative Organism
A. Bacterial Pneumonia
- Caused by typical bacteria such as Streptococcus pneumoniae, Haemophilus influenzae, and Staphylococcus aureus.
- It presents with productive cough, fever, and pleuritic chest pain.
- In elderly and immunocompromised patients, Gram-negative infections (Pseudomonas, Klebsiella) are common and severe.
B. Viral Pneumonia
- Caused by viruses like influenza, respiratory syncytial virus (RSV), adenovirus, and coronavirus (COVID-19).
- It usually presents with dry cough, myalgia, headache, and low-grade fever.
- In certain cases, it may lead to secondary bacterial pneumonia, especially in elderly or immunocompromised individuals.
C. Fungal Pneumonia
- Caused by fungi such as Pneumocystis jirovecii, Histoplasma capsulatum, and Aspergillus species.
- It is common in patients with HIV/AIDS, cancer, organ transplants, or on long-term steroids.
- Fungal pneumonia can present with progressive dyspnea, dry cough, weight loss, and diffuse infiltrates on imaging.
D. Atypical Pneumonia
- Caused by organisms like Mycoplasma pneumoniae, Chlamydophila pneumoniae, Legionella pneumophila.
- Patients present with dry cough, fever, malaise, and extrapulmonary symptoms such as diarrhea or rash.
- Chest X-ray typically shows diffuse interstitial infiltrates, often out of proportion to clinical findings.
3️⃣ Classification Based on Anatomical Pattern
A. Lobar Pneumonia
- Involves complete consolidation of one or more lobes of the lung, seen in bacterial pneumonia (usually Streptococcus pneumoniae).
- The infection progresses through stages: congestion, red hepatization, gray hepatization, and resolution.
- The chest X-ray shows homogeneous opacity, and the patient presents with high fever, productive cough, and pleuritic chest pain.
B. Bronchopneumonia
- Involves patchy consolidation centered around bronchi and bronchioles, typically seen with Staphylococcus aureus or Gram-negative bacteria.
- The infection is multifocal and bilateral in many cases.
- Chest X-ray shows scattered patchy opacities, and symptoms include low-grade fever, cough with purulent sputum, and breathlessness.
C. Interstitial Pneumonia
- Involves the alveolar walls and interstitial tissues rather than alveolar spaces.
- Commonly caused by viral infections, Mycoplasma, or Pneumocystis jirovecii.
- Chest X-ray shows a reticular or ground-glass pattern, and symptoms include dry cough, progressive dyspnea, and systemic malaise.
