03/08/2016-B.SC-MENTAL HEALTH-PAPER DONE
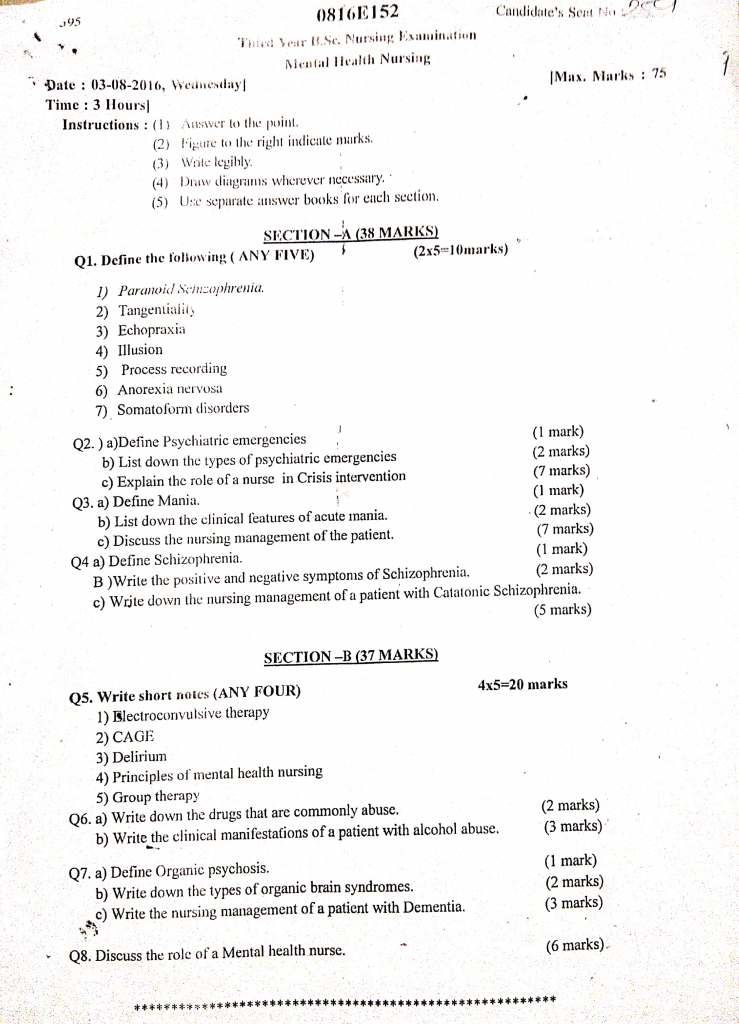
Section 1 (38 marks)
Q.1 Define the following (any five) (2×5=10)
1) Paranoid schizophrenia
- Paranoid Schizophrenia is a subtype of schizophrenia that is primarily characterized by the presence of prominent delusions and auditory hallucinations, particularly paranoid delusions such as beliefs of persecution, conspiracy, or being watched or targeted by others.
2) Tangentiality
- Tangentiality is a thought and speech disturbance in which an individual responds to questions or topics with unrelated or loosely related content, and fails to return to the original point or question.
It is commonly seen in schizophrenia, mania, and other psychotic disorders, and reflects a disruption in logical thinking and communication. - For example, when asked “How are you feeling today?” the person might reply:
“Well, I was feeling fine, but then I thought about how the weather changes, and birds fly south, and my cousin used to live in the south…” — never returning to the actual question.
3) Echoprexia
- Echopraxia is a neurological and psychiatric symptom in which an individual involuntarily imitates or mimics the movements, gestures, or actions of another person.
- It is commonly associated with schizophrenia, autism spectrum disorders, Tourette’s syndrome, and certain neurological conditions, and is considered a form of automatic, non-purposeful behavior.
- Echopraxia reflects an impairment in the control of voluntary actions and may indicate underlying frontal lobe dysfunction or loss of inhibition in the brain.
4) Illusion
- Illusion is a false or misinterpreted perception of a real external stimulus, where the sensory input is present but is perceived in a distorted or incorrect way by the individual.
For example, mistaking a rope for a snake in dim light is an illusion. - Illusions are usually related to visual or auditory senses and can occur in both mentally healthy individuals and those with psychiatric disorders, though they are more common during states of confusion, delirium, or extreme anxiety.
5) Process recording
- Process Recording is a written, verbatim account of an interaction between a nurse (or student nurse) and a patient, used primarily as an educational and evaluation tool in psychiatric and mental health nursing.
- It involves recording the exact conversation, including the patient’s verbal and non-verbal responses, as well as the nurse’s thoughts, feelings, and analysis of the interaction.
6) Anorexia nervousa
- Anorexia Nervosa is a serious eating disorder characterized by an intense fear of gaining weight, a distorted body image, and persistent restriction of food intake, leading to significantly low body weight in relation to age, sex, and physical health.
- Individuals with anorexia nervosa often engage in excessive dieting, fasting, over-exercising, or purging behaviors to lose weight, even when they are already underweight.
- This condition can cause severe physical and psychological complications, including malnutrition, organ failure, electrolyte imbalance, and increased risk of death, and requires comprehensive medical and psychological treatment for recovery.
7) Somatoform disorder
- Somatoform Disorder is a group of mental health conditions in which a person experiences physical symptoms—such as pain, fatigue, or gastrointestinal issues—that cannot be fully explained by any medical condition, substance use, or other psychiatric disorder.
- These symptoms are not intentionally produced or feigned, and the individual genuinely believes they are ill, which leads to significant distress, frequent healthcare visits, and impairment in social, occupational, or personal functioning.
- Examples include somatization disorder, conversion disorder, hypochondriasis, and pain disorder, and treatment often involves psychotherapy (especially cognitive-behavioral therapy) and sometimes antidepressant medications.
Q.2
a) Define psychiatric emergencies (1)
- Psychiatric emergencies are acute disturbances in thought, behavior, mood, or social relationships that require immediate intervention because the person may be at risk of harming themselves or others, or may be unable to care for themselves safely.
- These emergencies are characterized by sudden onset of severe mental symptoms such as suicidal ideation, violent behavior, psychotic breakdown, severe agitation, or catatonia, which demand urgent psychiatric and medical attention.
b) List down the types of Psychiatric emergencies (2)
- Suicidal attempt or suicidal ideation
- Homicidal behavior or threats to others
- Acute psychotic episode
- Severe depression with suicidal risk or catatonia
- Manic episode with agitation or overactivity
- Substance intoxication (e.g., alcohol, drugs)
- Substance withdrawal (e.g., delirium tremens)
- Violent or aggressive behavior
- Severe panic attack or anxiety crisis
- Delirium (acute confusional state)
- Acute stress reaction or post-traumatic crisis
- Conversion disorder with acute functional loss (e.g., paralysis, mutism)
c) Explain the role of nurse in crisis intervention (7)
- Crisis intervention is a short-term, goal-directed, and focused intervention designed to help individuals in psychological distress regain equilibrium.
- The nurse plays a critical role in assessing, planning, intervening, and evaluating the emotional and behavioral needs of individuals facing crises such as suicide attempts, loss, trauma, disasters, violence, or severe mental breakdown.
1. Assessment of the Crisis Situation
- The nurse begins by performing a detailed assessment of the precipitating event, emotional reactions, and the timeline of the crisis to understand its impact on the patient’s psychological balance.
- It is important to identify risk factors such as suicidal ideation, aggression, hallucinations, or inability to perform self-care, as these may indicate a psychiatric emergency.
- The nurse evaluates the patient’s coping history, current thought patterns, family background, substance use, and any past psychiatric admissions or trauma exposure.
- Physical health status and co-existing medical conditions should also be assessed, as they may complicate emotional responses (e.g., delirium, thyroid disorder).
2. Establishing Therapeutic Communication
- The nurse must develop a non-threatening, accepting, and empathetic environment where the patient feels safe to express emotions like fear, grief, anger, or guilt.
- Verbal and non-verbal communication should be clear, calm, and nonjudgmental, with reflective listening and validation of the patient’s feelings.
- The nurse should respect silences, allow the patient time to process thoughts, and offer supportive verbal cues to encourage sharing.
- If the patient has language, cultural, or sensory barriers, the nurse should use appropriate tools or interpreters to ensure understanding and trust.
3. Providing Emotional Support and Ensuring Safety
- The nurse ensures both psychological and physical safety, especially in patients with suicidal ideation, aggressive behavior, or disorientation.
- A low-stimulation environment with reduced noise, light, and interruptions helps in calming the patient.
- The nurse should immediately remove or secure hazardous items (e.g., sharp objects, belts, medications) and maintain constant observation if necessary.
- In case of acute agitation, the nurse may need to initiate crisis protocols, such as administering emergency sedatives under medical guidance.
4. Helping Identify and Strengthen Coping Mechanisms
- The nurse supports the patient in identifying positive coping strategies used in the past such as praying, talking to a friend, exercising, or artistic activities.
- Patients are guided to reframe negative thought patterns and taught relaxation techniques like deep breathing, grounding exercises, or guided imagery.
- The nurse may provide written materials or worksheets for patients to track triggers and coping responses.
- For patients with poor coping skills, the nurse should introduce new adaptive strategies gradually and role-model these behaviors during interaction.
5. Facilitating Problem Solving and Decision-Making
- The nurse encourages the patient to express current challenges clearly and helps break complex issues into small, solvable parts.
- With guidance, the patient is supported to list options, evaluate pros and cons, and make rational decisions without impulsivity.
- Role-playing, storytelling, and hypothetical scenarios can be used to strengthen decision-making confidence.
- The nurse should avoid giving direct advice and instead encourage the patient to think through solutions independently, promoting autonomy.
6. Involving Family and Support Systems
- The nurse communicates with the patient’s family to assess the quality and availability of emotional, financial, and practical support.
- Families are invited to participate in crisis counseling sessions, helping them understand the patient’s condition and how to respond constructively.
- The nurse educates family members to avoid reinforcing maladaptive behaviors, such as overprotection or criticism.
- In cases where family involvement is not supportive, the nurse should consider alternative support sources such as social workers or community organizations.
7. Coordinating with the Multidisciplinary Team
- The nurse acts as a central communication bridge between the psychiatrist, psychologist, social worker, case manager, and the patient.
- The nurse participates in team discussions, progress evaluations, and crisis planning to ensure the patient’s care is unified and goal-oriented.
- Regular interdisciplinary meetings help in modifying interventions, sharing insights, and preventing professional burnout through shared responsibility.
- In emergency situations, the nurse coordinates medical stabilization, referrals, and even legal processes (e.g., for involuntary admission if required).
8. Providing Health Education and Prevention
- The nurse educates the patient about the nature of crises, their temporary impact, and the importance of early intervention.
- Patients are taught to recognize early warning signs of psychological breakdown and seek timely help.
- The nurse provides educational materials on mental wellness, stress management, lifestyle balance, and the harmful effects of substance use.
- Preventive counseling is extended to family members, caregivers, and community health volunteers to reduce future crisis recurrence.
9. Monitoring and Documenting Progress
- The nurse observes the emotional tone, thought patterns, and behavior changes of the patient throughout the intervention period.
- Accurate documentation of every intervention, patient response, medication, referrals, and evaluation results ensures continuity of care.
- Monitoring progress includes reassessment of risk factors and determining if the patient can return to pre-crisis functioning or needs extended support.
- The nurse also tracks the effectiveness of coping strategies used by the patient and encourages continued practice of healthy behaviors.
10. Encouraging Follow-up and Long-term Planning
- The nurse supports the patient in planning future appointments with psychiatrists, counselors, or support groups for sustained recovery.
- Contact details of helplines, emergency services, NGOs, and crisis centers are provided for use in case of future crises.
- The nurse helps create a personal safety plan, including coping steps, emergency contacts, and a list of calming activities the patient can use.
11. Promoting Patient Empowerment and Autonomy
- The nurse involves the patient in setting short-term and long-term recovery goals, giving them a sense of control and responsibility.
- Patients are encouraged to make choices in their care plans, even in small matters, to rebuild decision-making capacity.
- Empowerment includes helping patients build self-confidence, challenge negative self-talk, and develop a future-oriented mindset.
12. Practicing Cultural Sensitivity and Respect for Beliefs
- The nurse respects the patient’s cultural background, language, gender identity, and spiritual beliefs when planning care.
- Cultural rituals or expressions of grief or crisis should be understood within the cultural context, not misinterpreted as pathology.
- The nurse ensures equitable and unbiased care by avoiding stereotypes and involving cultural mediators when needed.
Q.3
a. Define mania (1)
Mania is a mental state characterized by an abnormally elevated, expansive, or irritable mood, lasting at least one week, and often accompanied by increased energy, decreased need for sleep, inflated self-esteem, and impulsive or risky behaviors.
b. List down the clinical features of acute mania (2)
- Elevated or irritable mood – Abnormally cheerful, euphoric, or easily angered.
- Increased energy and hyperactivity – Constant movement, excessive goal-directed activity.
- Reduced need for sleep – Feels rested after only a few hours of sleep or no sleep at all.
- Rapid or pressured speech – Talking fast, loud, and difficult to interrupt.
- Flight of ideas – Rapid shifting from one topic to another without logical connection.
- Inflated self-esteem or grandiosity – Unrealistic beliefs in one’s abilities or identity (e.g., thinking one is a celebrity or god).
- Distractibility – Easily drawn to irrelevant external stimuli.
- Impulsivity or poor judgment – Reckless spending, sexual indiscretions, or quitting jobs impulsively.
- Psychotic features (in severe cases) – Delusions of grandeur or hallucinations.
- Over-familiar or intrusive behavior – Inappropriate social conduct and lack of boundaries.
c. Discuss the nursing management of the patient (7)
1. Maintaining a Safe Environment
- The nurse must closely monitor the patient’s behavior for signs of hyperactivity, aggression, self-harm, or threats to others and intervene promptly to ensure safety.
- The environment should be structured, non-stimulating, and free from potential hazards, including sharp tools, glass, belts, or cords.
- The nurse should assign the patient to a room near the nursing station for easier observation and rapid intervention when needed.
- Use of least-restrictive alternatives such as verbal redirection, de-escalation techniques, or assigning a trusted staff member as a sitter can reduce the need for physical restraint.
- Safety protocols should be updated frequently and clearly communicated to the multidisciplinary team to ensure consistency.
2. Establishing Therapeutic Communication
- The nurse should use short, direct, and clear sentences when giving instructions, as manic patients have short attention spans and may become easily distracted.
- It is important to remain calm, non-confrontational, and consistent in tone and body language to avoid triggering defensive or aggressive responses.
- The nurse must avoid arguing or engaging in debates over delusions or grandiosity, instead gently redirecting the conversation to reality-based topics.
- Therapeutic listening should be maintained, allowing the patient to vent thoughts and emotions while ensuring that communication does not escalate agitation.
- The nurse can use therapeutic silence when appropriate to give the patient time to reflect or regain control of thought flow.
3. Controlling Stimuli and Providing a Structured Environment
- The patient should be kept in a low-stimulation room, minimizing exposure to noise, crowds, bright lights, and overstimulating social situations.
- Structured, predictable routines including meal times, rest periods, and medication administration should be followed to maintain consistency.
- The nurse should limit the patient’s access to group interactions or high-energy activities during the acute manic phase to prevent overstimulation.
- Introducing one-to-one quiet activities (e.g., puzzles, coloring, walking) helps redirect energy into safer and calming outlets.
- Visual cues like daily schedules, orientation boards, and clocks help the patient stay oriented to time and routine.
4. Promoting Rest and Sleep
- The nurse should encourage rest by offering the patient a quiet, comfortable sleeping area, reducing light, sound, and interruptions especially in the evening.
- Short rest periods during the day should be scheduled and reinforced, even if the patient does not feel tired, to prevent physical exhaustion.
- A bedtime routine (e.g., warm bath, herbal tea, calming music) should be maintained to help the body adjust to rest periods naturally.
- Sleep-promoting measures such as reducing caffeine, encouraging slow breathing, or reading calming content can be used before bedtime.
- If necessary, prescribed sedative medications should be administered on time and the patient’s response and side effects should be monitored closely.
5. Assisting with Nutrition and Fluid Intake
- The nurse should offer easy-to-eat, high-calorie finger foods such as sandwiches, boiled eggs, fruits, and juice, which allow the patient to eat while moving or pacing.
- Frequent reminders to eat and drink are necessary, as manic patients often neglect meals due to their distractibility or hyperfocus on activity.
- Keep nutritional snacks and water accessible at all times, especially after physical activity or therapy sessions.
- Monitor and document daily food and fluid intake, and consider nutritional supplements if calorie intake remains insufficient.
- If necessary, arrange for assisted feeding or intravenous fluids under medical guidance if the patient refuses food or is unable to eat independently.
6. Encouraging Hygiene and Self-Care
- The nurse should help the patient follow a simple hygiene routine with scheduled bathing, grooming, dressing, and toileting to promote self-care behavior.
- Step-by-step verbal prompts or physical guidance may be required for dressing or toothbrushing, especially if the patient is distracted or confused.
- The patient should be provided with limited, season-appropriate clothing choices to reduce impulsive or inappropriate dress.
- Reinforce personal grooming by praising small achievements, such as brushing hair or changing clothes, to boost self-esteem.
- Visual cues (e.g., mirror, hygiene checklist) may be used to reinforce self-care routines and support independence.
7. Monitoring and Administering Medications
- The nurse must ensure timely administration of mood stabilizers (e.g., Lithium, Valproate) and antipsychotics (e.g., Risperidone, Olanzapine).
- Close monitoring of vital signs, laboratory values (e.g., lithium levels), and side effects such as tremors, sedation, or gastrointestinal distress is essential.
- Patients with poor insight may refuse medications; hence, the nurse should use therapeutic techniques to encourage cooperation, like discussing benefits and addressing fears.
- Observe the patient during and after administration to ensure medication is swallowed and not cheeked or spat out.
- Documentation of effectiveness, side effects, and behavior changes is vital for medication review and adjustment by the physician.
8. Managing Social Behavior and Impulsivity
- The nurse should monitor for inappropriate behavior, including sexual disinhibition, excessive spending, or boundary violation, and intervene firmly but respectfully.
- Set clear, consistent limits on intrusive behavior and redirect the patient to safer activities that reduce overstimulation.
- The nurse should supervise peer interactions to prevent conflict or misunderstandings due to the patient’s talkativeness or attention-seeking.
- Encourage simple tasks or roles like watering plants or folding laundry, which redirect energy and promote cooperation.
- Reinforce appropriate behavior with praise or positive feedback to promote behavioral improvement.
9. Providing Emotional Support and Reality Orientation
- The nurse should provide continuous emotional support by being present, listening actively, and offering validation without encouraging unrealistic beliefs.
- Help the patient to connect with real-time events, people, and facts by using calendars, clocks, and frequent reminders.
- Delusions should not be directly challenged but gently reoriented with neutral, reality-based statements.
- Emotional support includes helping the patient understand and express underlying sadness, anxiety, or guilt, which may be masked by the manic state.
- Encouraging expression through journaling, drawing, or talking in a safe space allows emotional processing without escalation.
10. Involving Family and Educating Caregivers
- The nurse should schedule family psychoeducation sessions to discuss the symptoms, treatment, and long-term nature of bipolar disorder.
- Families should be encouraged to set firm boundaries at home, such as limiting spending and establishing sleep routines.
- Teach family members to recognize early warning signs of relapse, including reduced sleep, irritability, and overconfidence.
- Discuss the importance of medication compliance, regular follow-up, and stress management to prevent future episodes.
- Refer families to support groups or mental health NGOs where they can share experiences and access additional resources.
Q.4
a. Define schizophrenia (1)
- Schizophrenia is a chronic and severe mental disorder characterized by disturbances in thought, perception, emotion, and behavior, leading to hallucinations, delusions, disorganized thinking, and social or occupational dysfunction.
- It affects the individual’s ability to interpret reality, often causing significant impairment in daily functioning.
b. Write the positive and negative symptoms of schizophrenia (2)
✅ Positive Symptoms of Schizophrenia (Also called psychotic symptoms)
- Hallucinations – false sensory perceptions (e.g., hearing voices not present).
- Delusions – false, fixed beliefs (e.g., thinking someone is spying).
- Disorganized speech – incoherent, illogical, or rapid speech.
- Disorganized or bizarre behavior – unpredictable, inappropriate, or purposeless movements.
- Thought broadcasting or insertion – belief that others can hear or control their thoughts.
✅ Negative Symptoms of Schizophrenia
- Affective flattening – reduced emotional expression (face, voice, gestures).
- Alogia – poverty of speech or reduced verbal output.
- Anhedonia – inability to feel pleasure or interest.
- Avolition – lack of motivation to initiate and sustain activities.
- Social withdrawal – reduced interest in social interactions or relationships.
c. Write down the nursing management of patient with catatonic schizophrenia (5)
Catatonic schizophrenia is a rare and severe subtype of schizophrenia characterized by motor immobility, extreme negativism, mutism, waxy flexibility, or purposeless excessive motor activity. The nursing management focuses on ensuring safety, improving communication, maintaining nutrition, and promoting functional mobility.
✅ 1. Ensuring Patient Safety
- The nurse should closely observe the patient for sudden agitation or violent outbursts, especially during excited catatonic states.
- In stuporous phases, the patient may remain motionless for long periods, so frequent repositioning is necessary to prevent pressure sores and contractures.
- Remove all sharp objects, cords, and potential ligature materials to prevent self-harm or accidental injury.
- Use of restraints or seclusion must follow institutional policies and only when absolutely necessary.
✅ 2. Maintaining Adequate Nutrition and Hydration
- In catatonic stupor, patients may refuse to eat or drink, requiring timely nutritional support via spoon-feeding or IV fluids.
- Monitor for signs of dehydration, electrolyte imbalance, or weight loss due to prolonged inactivity.
- Provide a nutritious, soft, and easy-to-swallow diet, and offer frequent small meals.
- Record daily intake and output to ensure fluid and nutritional balance.
✅ 3. Promoting Communication
- Use short, simple, and clear statements, and maintain a calm, non-threatening tone while interacting.
- In cases of mutism, support communication through non-verbal cues, such as pictures, gestures, or pointing.
- Be patient and consistent; avoid pressuring the patient to speak or respond.
- Encourage gradual interaction through one-to-one sessions and later group activities.
✅ 4. Encouraging Mobility and Physical Activity
- Assist the patient with passive and active range-of-motion exercises to prevent joint stiffness and muscle atrophy.
- In the hyperactive catatonic phase, monitor for exhaustion, dehydration, or injury due to excessive movement.
- Encourage small, guided movements to gradually restore purposeful motor behavior.
- Physical therapy consultations may be needed for patients with long-term immobility.
✅ 5. Enhancing Self-Care and Daily Living Activities
- Assist the patient with bathing, dressing, grooming, and other ADLs when catatonic symptoms hinder independence.
- Use cueing techniques or step-by-step instructions to prompt self-care actions.
- Gradually involve the patient in structured routines to restore autonomy.
- Praise and reinforce any small progress toward independent functioning.
✅ 6. Monitoring Medication and Side Effects
- Administer antipsychotic medications (e.g., lorazepam, risperidone, clozapine) as prescribed, and monitor for response.
- Observe for extrapyramidal side effects (EPS) such as rigidity, tremors, or dystonia, especially in immobile patients.
- Watch for neuroleptic malignant syndrome (NMS), a medical emergency that may mimic catatonia.
- Report any adverse drug reactions or complications immediately to the physician.
✅ 7. Providing Emotional Support and Reassurance
- Establish a trust-based, non-judgmental relationship with the patient using a calm, reassuring approach.
- Involve family members to provide emotional connection and reduce social isolation.
- Offer positive reinforcement for engagement, verbalization, or movement, however minimal.
- Maintain consistency in nursing staff to promote a sense of safety and familiarity.
✅ 8. Family Education and Involvement
- Educate the family about the nature of catatonic schizophrenia, its phases, prognosis, and treatment needs.
- Teach them to handle both immobile and agitated states, and how to respond calmly and safely.
- Encourage family involvement in care planning and therapy sessions.
- Offer information about community support groups and long-term care options if needed.
✅ 9. Documentation and Interdisciplinary Collaboration
- Record detailed observations on motor activity, communication, medication compliance, and responses to interventions.
- Collaborate with psychiatrists, psychologists, physiotherapists, and occupational therapists for holistic care.
- Update progress notes regularly to track changes and inform care planning.
- Participate in multidisciplinary meetings to review goals and discharge planning.
Section 2 (37 marks)
Q.5 Write short notes (any four) (4×5=20)
1) Electro-convulsive therapy
Definition
- Electroconvulsive Therapy (ECT) is a medical treatment for certain mental illnesses, in which a small, controlled electric current is passed through the brain to induce a brief, generalized seizure while the patient is under general anesthesia, and this process helps in achieving therapeutic improvement in psychiatric conditions such as depression, mania, and schizophrenia.
- It is considered one of the most effective and rapid treatment methods in psychiatry for certain life-threatening and treatment-resistant mental disorders.
Objectives of ECT
- It is used to relieve severe depressive symptoms especially when patients are non-responsive to medications.
- It aims to treat catatonic states, suicidal tendencies, and psychotic depression quickly and effectively.
- It is used to produce controlled seizures that help to correct biochemical imbalances in the brain.
- ECT promotes rapid symptom relief in life-threatening psychiatric conditions.
Types of ECT
Modified ECT – It is the most commonly used form, where muscle relaxants and anesthesia are given.
Unmodified ECT – It is rarely used and involves administering electric current without anesthesia or muscle relaxant.
Bilateral ECT – Electrodes are placed on both temples, commonly used for faster results.
Unilateral ECT – Electrodes are placed on one side of the head, minimizing cognitive side effects.
Mechanism of Action (How ECT works)
- ECT induces generalized tonic-clonic seizures lasting 20 to 60 seconds, leading to neurochemical alterations in neurotransmitter systems (serotonin, dopamine, norepinephrine).
- The seizure results in increased blood flow and oxygenation to various brain regions, enhancing mood regulation and cognitive function.
- The therapy helps in modulating neural circuits, restoring functional connectivity in mood-related brain areas such as limbic system, prefrontal cortex, and hippocampus.
- It is believed to promote neurogenesis and synaptic plasticity, which contributes to its long-term antidepressant effects.
Indications of ECT
- It is indicated in patients with major depressive disorder with suicidal ideation or psychotic features.
- It is commonly used in severe catatonia, where the patient is mute, stuporous, or immobile.
- It is indicated in treatment-resistant schizophrenia or bipolar disorder not responding to drugs.
- It is useful in manic episodes not controlled with mood stabilizers.
- It may be used in postpartum psychosis or delirious mania.
Contraindications of ECT
Note: No absolute contraindications, but certain conditions are considered relative risks.
- Patients with increased intracranial pressure (ICP) due to brain tumor or recent stroke.
- Those with recent myocardial infarction (MI) or unstable cardiac conditions.
- Patients with aortic aneurysm, retinal detachment, or severe osteoporosis.
- ECT is avoided during pregnancy in first trimester, unless life-saving.
Advantages of ECT
- It produces rapid improvement in suicidal or severely depressed patients, often within 1–2 weeks.
- It is useful when drugs are contraindicated, such as in pregnancy, elderly, or medically ill patients.
- ECT has a high success rate in treating catatonia and psychotic depression.
- It avoids long-term drug side effects such as weight gain, diabetes, or sedation.
- It can be repeated safely under monitoring in maintenance settings.
Disadvantages of ECT
- Requires multiple hospital visits, usually 6–12 sessions.
- Involves anesthesia-related risks, especially in cardiac or elderly patients.
- May lead to public or cultural stigma, misunderstanding about its safety and use.
- Memory issues and cognitive slowing may persist temporarily in some individuals.
Side Effects of ECT
- Short-term memory loss and confusion are common, usually resolving within hours to days.
- Patients may complain of headache, body ache, muscle soreness, or nausea.
- Retrograde amnesia (forgetting past events) may occur temporarily, especially in bilateral ECT.
- Rare but serious complications include status epilepticus, cardiac arrhythmia, or prolonged apnea.
Nursing responsibilities
Pre-ECT Nursing Responsibilities
- It is the nurse’s responsibility to obtain written informed consent, explaining the purpose, risks, and benefits of ECT in understandable language.
- The nurse must ensure the patient is fasting (NPO) for at least 6 to 8 hours before the procedure.
- Removal of dentures, jewelry, spectacles, hairpins, and other accessories must be ensured for safety.
- Vital signs, blood pressure, heart rate, respiratory rate, and oxygen saturation should be assessed and documented.
- Pre-medication with atropine sulfate (0.5 mg IM) is given 30 minutes before ECT to reduce oral secretions and prevent bradycardia.
- The nurse should prepare the ECT room with all necessary equipment, including oxygen supply, suction, crash cart, and emergency drugs.
- Psychological support should be offered to reduce fear and anxiety before the session.
During ECT Procedure
- The patient is given short-acting anesthesia (e.g., methohexital) to induce sleep within seconds.
- Muscle relaxant (succinylcholine) is administered to reduce muscle contractions and prevent injuries during seizures.
- Electrodes are placed according to the chosen technique (bilateral or unilateral).
- A small amount of electric current (70 to 120 volts) is passed for less than 1 second to induce seizure.
- Seizure activity is monitored by EEG and physical signs (toe movement, jaw clenching).
- The total seizure should last between 20 to 60 seconds for therapeutic benefit.
Post-ECT Nursing Care
- The patient is placed in lateral position to prevent aspiration and is observed in the recovery room.
- Nurse must monitor vital signs, oxygen saturation, and ensure the airway is patent.
- Patient may wake up confused, dizzy, or with temporary memory loss—provide reassurance and calm environment.
- Neurological observations, level of consciousness, orientation, and verbal response must be recorded.
- Offer sips of water and assist in ambulation when fully conscious.
- Observe for side effects such as headache, nausea, or agitation, and document all findings.
2) CAGE
The CAGE questionnaire is a brief, standardized screening tool that helps to identify individuals who may have problems related to alcohol abuse or dependence. It is a mnemonic device based on four key questions that begin with the letters C, A, G, and E. The tool is especially useful in nursing, psychiatry, and general medical settings as a quick and effective way to assess alcohol-related issues, often before a full diagnostic evaluation is done.
The four questions of the CAGE questionnaire are
1️⃣ C – Cut Down
- It is the first component of the CAGE screening tool, in which the individual is asked the question : “Have you ever felt that you should cut down on your drinking?”
- This question is meant to identify whether the person has consciously recognized a problem with their alcohol intake and has ever tried or considered reducing the quantity or frequency of alcohol use.
- A positive answer to this question usually indicates that the person is experiencing internal conflict or concern about their drinking behavior.
2️⃣ A – Annoyed
- It is the second question in the screening tool and asks : “Have people annoyed you by criticizing your drinking?”
- This part of the CAGE questionnaire attempts to assess whether others have pointed out or confronted the individual about their drinking habits and whether the individual reacted with irritation, frustration, or defensiveness.
- A positive response indicates the presence of social and interpersonal disturbances due to alcohol use, as well as denial or resistance to feedback.
3️⃣ G – Guilty
- The third part involves the question : “Have you ever felt guilty about your drinking?”
- This question aims to explore the individual’s emotional response to their own alcohol-related behavior, particularly whether they feel ashamed, regretful, or remorseful after drinking.
- A “yes” response may reflect personal awareness of the negative impact of alcohol on their life, relationships, health, or responsibilities.
4️⃣ E – Eye-Opener
- The final question is : “Have you ever had a drink first thing in the morning to steady your nerves or get rid of a hangover?”
- This symptom is known as taking an “eye-opener,” which suggests physical dependence on alcohol where the individual may need alcohol to function normally or avoid withdrawal symptoms.
- A positive answer is a strong indicator of tolerance and addiction, as drinking in the morning is highly suggestive of chronic alcoholism.
Scoring and Interpretation of the CAGE Tool
Each “Yes” response is given 1 point.
A total score of:
- 0 to 1 = No problem or minimal concern
- 2 or more = Positive screening, indicating the possibility of alcohol dependence or abuse and the need for further diagnostic evaluation.
- Though not diagnostic, it is useful for screening and initiating further medical or psychiatric referral.
Clinical Significance of CAGE
- It is one of the quickest and most effective screening tools used in outpatient, emergency, and primary care settings.
- It can be completed verbally or in writing, and is suitable for all adult age groups.
- It is specifically focused on alcohol use and is not typically used for other substance use disorders.
Advantages of CAGE Tool
- It is short, simple, and can be completed within 1–2 minutes.
- It requires no special equipment or training.
- It can be used in a wide range of clinical and community health settings.
- It is effective even when the individual is not actively intoxicated
Role of Nurse While Using CAGE Screening
- It is essential for the nurse to approach the patient with empathy, confidentiality, and non-judgmental attitude when asking the CAGE questions.
- The nurse should be aware that some patients may feel embarrassed or deny their problems, so questions should be asked in a calm, private, and supportive environment.
- If the CAGE score is 2 or more, the nurse should notify the physician or mental health team for further evaluation or psychiatric referral.
- The nurse should provide education about the harmful effects of alcohol on health, family, employment, and mental status.
- In case of dependence, the nurse may assist in coordinating detoxification services, motivational therapy, group counseling, or referral to a de-addiction center.
- The nurse should document findings properly and encourage follow-up visits and ongoing support to prevent relapse.
3) Delirium
Definition
Delirium is an acute and reversible disturbance in attention, awareness, and cognition that develops over a short period of time and tends to fluctuate during the course of the day, commonly caused by medical illness, substance intoxication, withdrawal, or medication side effects.
Types of Delirium
1️⃣ Hyperactive Delirium
- This type is characterized by restlessness, agitation, mood lability, hallucinations, and delusions.
- The patient may become aggressive, combative, or extremely anxious.
2️⃣ Hypoactive Delirium
- In this type, the patient appears quiet, drowsy, lethargic, or withdrawn.
- It is more easily missed and often confused with depression or dementia.
3️⃣ Mixed Delirium
- This form includes both hyperactive and hypoactive features, alternating over a short period.
- It is the most common type observed in hospitalized elderly patients.
Etiology (Causes)
- Acute infections (e.g., UTI, pneumonia)
- Metabolic imbalances (e.g., electrolyte disturbances, hypoxia)
- Medications (e.g., anticholinergics, benzodiazepines)
- Drug or alcohol intoxication or withdrawal
- Neurological conditions (e.g., stroke, head injury)
- Sleep deprivation, pain, or environmental changes in ICU
Pathophysiology
- Delirium results from disruption in neurotransmission, especially involving acetylcholine, dopamine, and GABA.
- There is global cerebral dysfunction caused by inflammation, oxidative stress, or hypoxia.
- Reduced cerebral metabolism and cortical disconnection lead to disordered consciousness and cognition.
Clinical Manifestations
- Sudden onset of confusion
- Fluctuating attention and alertness
- Disorganized thinking
- Hallucinations or illusions
- Restlessness or lethargy
- Inappropriate or incoherent speech
- Sleep-wake cycle disturbances
Diagnostic Evaluation
- Detailed history and physical examination
- Use of screening tools (e.g., CAM – Confusion Assessment Method)
- Laboratory tests (CBC, electrolytes, liver and renal function tests)
- CT scan or MRI if neurological causes are suspected
- Urinalysis and chest X-ray to identify infections
Medical Management
1️⃣ Identify and Treat Underlying Cause
- Immediate correction of causes such as infection, hypoxia, hypoglycemia, or drug toxicity.
- Stop or replace deliriogenic medications.
2️⃣ Pharmacological Therapy
- Low-dose Haloperidol or Risperidone may be used to control agitation or hallucinations.
- Benzodiazepines (e.g., lorazepam) are reserved for alcohol withdrawal-related delirium.
- Adequate pain management with non-deliriogenic analgesics.
3️⃣ Supportive Therapy
- Ensure oxygenation, hydration, electrolyte balance, and nutritional support.
- Avoid unnecessary catheterizations and restraints.
Nursing Management
1️⃣ Assessment and Monitoring
- The nurse should regularly assess level of consciousness, attention, and orientation, using validated tools like CAM.
- Monitor vital signs, intake-output, and signs of underlying infection or distress.
2️⃣ Maintain Safety
- The nurse must ensure a safe environment, free of hazards, to prevent falls and injury.
- Side rails should be raised, and bed alarms may be used in confused patients.
3️⃣ Provide Orientation and Comfort
- It is essential to reorient the patient frequently using clocks, calendars, and familiar objects.
- Nurses should speak slowly and clearly, maintaining eye contact and reducing environmental noise.
4️⃣ Promote Rest and Sleep
- The nurse should minimize nighttime disturbances, dim the lights, and follow a routine sleep schedule.
- Provide relaxation techniques like soft music or back rubs if appropriate.
5️⃣ Support Family and Caregivers
- The nurse should educate the family about the temporary nature of delirium and encourage their presence to reduce anxiety in the patient.
- Emotional support and reassurance are important for caregivers.
6️⃣ Prevent Complications
- Nurses must ensure hydration, nutrition, mobility, and skin integrity to avoid complications like bedsores, constipation, or pneumonia.
- Early mobilization and physiotherapy may aid recovery.
4) Principle of mental health nursing
✅ 1. Accept the patient as an individual
- The mental health nurse must accept the client with all his/her problems, thoughts, and behaviors without any judgment or criticism, recognizing that every individual has dignity, value, and uniqueness regardless of their mental illness.
- It is the nurse’s responsibility to develop an attitude of empathy, tolerance, and unconditional positive regard, which helps build a therapeutic relationship.
✅ 2. Maintain therapeutic nurse-patient relationship
- The mental health nurse should establish a professional, goal-directed relationship that is based on trust, empathy, honesty, and respect, helping the patient feel emotionally safe.
- It is essential to set clear boundaries, be nonjudgmental, and maintain a consistent, structured interaction with the patient.
✅ 3. Use self-understanding as a therapeutic tool
- The nurse must have self-awareness about personal emotions, attitudes, and biases, so they do not interfere with therapeutic communication or judgment.
- It is important for the nurse to understand their own mental state and behavior, as the nurse’s personality is a vital tool in mental health care.
✅ 4. Ensure patient’s safety at all times
- The nurse should take active steps to protect the patient from harming self or others, especially in cases of suicidal ideation, hallucinations, or aggressive behavior.
- It is important to provide constant observation, safe surroundings, and to remove dangerous items like sharps or cords from the patient’s environment.
✅ 5. Provide privacy and confidentiality
- It is the duty of the nurse to respect the patient’s privacy and ensure that all personal information is kept confidential, except when there is a risk to the patient’s life or others.
- Legal and ethical principles guide nurses to disclose information only with consent or as required by law.
✅ 6. Encourage self-reliance and independence
- The nurse should always promote the patient’s ability to think, decide, and act for themselves, rather than making them dependent on caregivers.
- This is done by providing support, motivation, and involvement in decision-making, which helps in boosting self-esteem and confidence.
✅ 7. Maintain reality orientation
- It is essential for the nurse to orient the patient to time, place, and person regularly, especially in those suffering from confusion, delirium, or psychosis.
- The nurse must gently correct false beliefs or delusions, without arguing, and guide the patient toward reality using calm reassurance.
✅ 8. Provide consistent and structured environment
- Patients with mental illness benefit from a predictable routine and consistent care, as it helps reduce anxiety and confusion.
- The nurse should follow ward rules strictly, avoid sudden changes, and promote regularity in daily activities (like sleep, food, and group therapy).
✅ 9. Be honest, truthful, and nonjudgmental
- Mental health nurses must be genuine and honest while interacting with patients, as trust is the foundation of the therapeutic relationship.
- The nurse should never lie or mislead the patient and must respond to all communication with empathy and professionalism.
✅ 10. Use purposeful communication and active listening
- Communication should be planned, therapeutic, and focused on helping the patient understand themselves better.
- The nurse should use open-ended questions, reflective listening, and non-verbal cues to encourage the patient to express their feelings and thoughts.
✅ 11. Avoid physical restraints unless necessary
- The nurse should always try de-escalation techniques, verbal interventions, and emotional support first, and only use restraints or seclusion when all other methods fail.
- When used, restraints must be applied with doctor’s order, safety measures, documentation, and close monitoring.
✅ 12. Promote socialization and group participation
- The nurse should encourage the patient to engage in group therapy, occupational therapy, and social interactions, which help them develop interpersonal skills and reduce isolation.
- Socialization enhances emotional expression, peer learning, and community reintegration.
✅ 13. Involve family in care process
- Mental illness affects not just the patient but also the family, so the nurse should educate, support, and involve family members in treatment planning and discharge preparation.
- Family education improves compliance, understanding, and early relapse detection.
✅ 14. Respect cultural, religious, and personal beliefs
- The nurse should understand and respect the individual’s cultural background, language, traditions, and religious practices, as they influence how the patient views illness and treatment.
- This helps in providing culturally competent and patient-centered mental health care.
✅ 15. Provide holistic care
- Mental health nursing should address not just the psychological needs, but also the physical, emotional, social, and spiritual well-being of the patient.
- This includes hygiene, nutrition, medication, therapeutic activities, and emotional counseling.
5) Group therapy
Definition
- Group therapy is a form of psychotherapy in which a small number of individuals with similar emotional or psychological problems meet together under the guidance of a trained therapist.
- It is a structured therapeutic environment where patients share their experiences, learn coping skills, and gain support from both the therapist and fellow group members.
Goals of Group Therapy
- The primary goal is to help individuals explore their thoughts, emotions, and behaviors in a safe, supportive setting.
- Group therapy aims to enhance self-awareness, self-esteem, and social skills through peer feedback and therapist guidance.
- It provides emotional support, shared learning, and encouragement from others who have similar issues.
- The goal is also to help patients learn new behaviors and adaptive coping mechanisms through role-playing, discussion, and reflection.
- It is meant to facilitate change in attitudes, behaviors, and beliefs through interpersonal interaction.
Types of Group Therapy
1️⃣ Psychoeducational Group Therapy
- Psychoeducational groups are designed to educate clients about specific psychological or medical conditions, such as depression, anxiety, schizophrenia, substance use, or chronic illnesses.
- It is used to provide structured information, teach coping strategies, improve medication compliance, and enhance self-management skills.
2️⃣ Supportive Group Therapy
- Support groups are meant to offer emotional support, reassurance, and shared experience among members facing similar challenges.
- It helps patients feel less alone in their struggles, reduces stress, and promotes hope and motivation for recovery.
- Common examples include bereavement groups, cancer survivor groups, HIV support groups, and mental health peer groups.
3️⃣ Cognitive-Behavioral Therapy (CBT) Group
- CBT group therapy focuses on helping individuals recognize and change negative thought patterns, beliefs, and behaviors that contribute to emotional problems.
- This type of group therapy is goal-oriented and structured, often using homework assignments, role-play, and worksheets.
- It is especially effective in anxiety disorders, phobias, OCD, depression, and substance abuse.
4️⃣ Interpersonal Therapy (IPT) Group
- IPT group therapy focuses on improving interpersonal functioning and relationships, helping clients explore how past and current relationships affect their emotions and mental health.
- It encourages participants to develop better communication, conflict resolution, and social interaction skills.
- It is especially useful in depression, social anxiety, and personality disorders.
5️⃣ Skills Training Group Therapy
- These groups are formed to teach practical life skills, vocational abilities, and social interaction skills in a therapeutic setting.
- Common skills taught include assertiveness, stress management, time management, communication, and anger control.
- It is highly beneficial for patients with schizophrenia, developmental delays, or chronic mental illness.
6️⃣ Self-Help or Peer-Led Groups
- These groups are voluntary and typically led by members, rather than professionals, who have experience with the same condition or challenge.
- Members provide mutual support, share experiences, and promote recovery through empathy and solidarity.
- Examples include Alcoholics Anonymous (AA), Narcotics Anonymous (NA), and Depression Support Groups.
7️⃣ Expressive Therapy Groups
- These groups use creative arts such as music, dance, art, or drama as a medium for self-expression and emotional healing.
- It allows clients to express feelings non-verbally, especially when they struggle to articulate emotions.
Indications for Group Therapy
- Depression, anxiety, and stress-related disorders where patients benefit from shared experiences.
- Substance use disorders, where group settings provide peer accountability and support.
- Grief and loss, where individuals find comfort in connecting with others facing similar pain.
- Chronic medical conditions, such as cancer, diabetes, or HIV, for emotional and informational support.
- Adolescent and family issues, like school problems or parent-child conflict, are often addressed in group formats.
- Social skill deficits, especially in autism spectrum disorder or schizophrenia.
Contraindications of Group Therapy
- Patients with acute psychosis or suicidal risk who may be disruptive or unsafe for group participation.
- Individuals with severe cognitive impairment, who may not understand or benefit from discussion.
- Those with extreme social anxiety or hostility, who may struggle to engage or may harm group dynamics.
Advantages of Group Therapy
- It provides a sense of belonging and acceptance, reducing feelings of isolation.
- Group therapy offers multiple perspectives and feedback from peers.
- It is cost-effective, as one therapist can help multiple patients at once.
- It helps improve interpersonal communication and relationship-building skills.
- Patients learn by observing others and can model positive behaviors.
- It can motivate change through peer influence and role models within the group.
Disadvantages / Limitations
- Some individuals may feel shy or anxious to speak in a group setting.
- There may be conflicts or domination by certain group members, disrupting harmony.
- Confidentiality is harder to maintain, as group members must voluntarily respect others’ privacy.
Role of the Nurse in Group Therapy
- The nurse may act as a co-therapist or facilitator in psychoeducational and support groups.
- It is the nurse’s role to observe group dynamics and ensure a safe, respectful environment.
- The nurse helps in screening suitable patients for group therapy, based on psychological readiness and diagnosis.
- She must encourage participation and manage disruptive behaviors during group sessions.
- The nurse is responsible for documenting patient progress, participation, and any significant observations.
- She also provides emotional support before and after sessions, especially for patients who feel overwhelmed.
- The nurse can use group feedback to reinforce individual care plans and collaborate with other mental health professionals.
Q.6
a) Write down the drugs that are commonly abused (2)
Alcohol – CNS depressant; causes intoxication, liver damage, and dependence.
Opioids – Includes heroin, morphine, codeine; causes euphoria, sedation, and respiratory depression.
Cannabis – Marijuana, hashish; causes relaxation, altered perception, memory issues.
CNS Stimulants – Cocaine, amphetamines, MDMA; increases alertness, energy, and causes addiction.
Sedatives/Hypnotics – Diazepam, barbiturates; cause calmness, sleep, and withdrawal risk.
Hallucinogens – LSD, magic mushrooms; cause hallucinations, altered reality.
Inhalants – Glue, petrol, aerosol sprays; cause short “high,” brain damage, and sudden death.
Nicotine – Found in tobacco and vapes; leads to addiction, cancer, and heart disease.
Caffeine (excessive use) – Causes restlessness, insomnia, and mild dependence.
Club Drugs – Ketamine, GHB, Rohypnol; used in parties; may cause amnesia and sedation.
b) Write the clinical manifestations of patient with alcohol abuse (3)
✅ 1. Physical Manifestations
- The patient may experience gastritis, nausea, vomiting, and abdominal pain, especially after drinking.
- There is often weight loss, poor nutritional status, and vitamin deficiencies, particularly thiamine (B1).
- Complaints of tremors or shaky hands, especially in the morning, are common in chronic alcohol users.
- In advanced cases, symptoms of liver damage may appear, such as jaundice, ascites, spider angiomas, and hepatomegaly.
- Chronic alcoholics may suffer from alcoholic neuropathy, presenting as tingling, numbness, and pain in extremities.
✅ 2. Neurological Manifestations
- The patient may present with slurred speech, impaired coordination, and difficulty walking (ataxia).
- There may be episodes of blackouts or memory lapses after heavy drinking sessions.
- Chronic abuse can lead to Wernicke’s encephalopathy, with confusion, oculomotor disturbances, and unsteady gait.
- Some individuals experience seizures (alcohol-related epilepsy), especially during withdrawal.
✅ 3. Psychological and Behavioral Manifestations
- The patient may show signs of irritability, mood swings, anxiety, or depression, often triggered by alcohol use or withdrawal.
- Loss of control over drinking, despite repeated attempts to cut down, is a hallmark sign.
- There is a tendency toward social withdrawal, neglect of responsibilities, and poor work or academic performance.
- The patient may lie, steal, or become aggressive or violent under the influence of alcohol.
- Tolerance develops over time, requiring larger amounts of alcohol to feel the same effect.
✅ 4. Cognitive Manifestations
- The patient may demonstrate impaired concentration, decision-making, and judgment.
- Disorientation or confusion may be seen during acute intoxication or withdrawal.
- Long-term use may lead to alcohol-induced dementia or Korsakoff’s psychosis, causing severe memory loss and confabulation.
✅ 5. Withdrawal Symptoms (if alcohol use is suddenly stopped)
- The patient may experience tremors, sweating, insomnia, nausea, and agitation within hours.
- In severe cases, delirium tremens (DTs) may occur, characterized by hallucinations, severe tremors, seizures, and delirium.
- There may also be increased pulse, blood pressure, and anxiety during withdrawal episodes.
✅ 6. Social and Legal Consequences
- Chronic alcohol abuse often leads to family conflict, marital problems, child neglect, and financial loss.
- Increased risk of driving under the influence (DUI) or involvement in criminal or violent activities.
- The patient may face legal issues or job loss due to absenteeism or misconduct.
Q.7
a) Define organic psychosis (1)
- Organic Psychosis is defined as a severe mental disorder in which there is a loss of contact with reality, accompanied by hallucinations, delusions, disorganized thinking, and behavioral disturbances, that arises secondary to identifiable structural or functional abnormalities of the brain.
- It is caused by a specific organic (physical or physiological) condition affecting the brain, such as brain injury, infection, tumor, intoxication, or metabolic disturbance.
b) Write down the types of organic brain syndrome (2)
Organic brain syndromes are disorders that result from a detectable physical or physiological abnormality in the brain. The major types include:
- Delirium:
It is an acute, reversible, fluctuating disturbance in consciousness and cognition, often caused by infections, metabolic disorders, or substance intoxication/withdrawal. - Dementia:
It is a chronic, progressive, and usually irreversible syndrome characterized by memory loss, impaired judgment, disorientation, and changes in personality. - Amnestic Syndrome:
It is a disorder primarily affecting memory, especially the ability to form new memories, often due to brain damage such as in Korsakoff’s syndrome. - Organic Mood Disorders:
These are mood disturbances (like depression or mania) directly caused by a physical disorder affecting the brain, such as brain tumor or head trauma. - Organic Psychotic Conditions:
These include hallucinations and delusions arising from identifiable brain pathology, such as in epilepsy or brain injury.
c) Write the nursing management of patient with dementia (3)
✅ 1. Ensuring Patient Safety
- Create a safe, clutter-free environment by removing hazardous items, sharp tools, and loose rugs to prevent falls or injuries.
- Install safety aids like handrails, bed alarms, and non-slip mats to reduce accidents.
- Monitor for behaviors like wandering, pacing, or sundowning, and take preventive action such as door locks or patient tracking devices.
- Ensure that toileting and feeding are supervised in advanced stages to avoid choking or incontinence-related issues.
✅ 2. Maintaining Orientation and Cognitive Support
- Use reality orientation tools like clocks, calendars, and name tags to help patients stay connected to their surroundings.
- Keep the environment familiar and consistent, avoiding frequent furniture or room changes.
- Encourage simple memory activities like recalling names, puzzles, or photo albums.
- Speak slowly and clearly using short, familiar phrases, repeating if needed.
✅ 3. Promoting Activities of Daily Living (ADLs)
- Encourage patients to perform basic self-care tasks with step-by-step assistance and gentle supervision.
- Provide adaptive tools like easy-grip utensils, elastic clothing, and velcro shoes to support independence.
- Use visual cues and demonstration to guide through daily routines like brushing teeth or using the toilet.
- Praise and reinforce any attempt at independence to build confidence and reduce frustration.
✅ 4. Managing Behavioral and Psychological Symptoms
- Identify and avoid common triggers of agitation, such as loud noises, unfamiliar faces, or fatigue.
- Respond to aggression or confusion with calm redirection, reassurance, and distraction using music or familiar objects.
- If medications are prescribed (e.g., antipsychotics), monitor closely for sedation or side effects.
- Maintain a structured and quiet environment to minimize overstimulation and stress.
✅ 5. Nutritional and Hydration Support
- Offer soft, easy-to-chew meals and ensure high-protein snacks are available if the patient struggles to eat full meals.
- Encourage frequent fluid intake to prevent dehydration, especially if the patient forgets to drink.
- Supervise meals to prevent choking, especially if the patient has swallowing difficulties.
- Monitor body weight and appetite regularly to detect nutritional deficits early.
✅ 6. Enhancing Communication
- Use simple, direct language and allow extra time for the patient to process and respond.
- Support communication using non-verbal cues, such as gestures or pointing.
- Avoid arguments or correcting false beliefs — instead, use therapeutic redirection.
- Encourage non-verbal expression through drawing, music, or physical activity if verbal communication is limited.
✅ 7. Providing Emotional Support
- Offer continuous reassurance and presence, especially during episodes of anxiety or disorientation.
- Use reminiscence therapy — talking about past experiences — to provide comfort and connection.
- Encourage family visits and emotional bonding to reduce feelings of isolation or confusion.
- Watch for signs of depression or anxiety, especially in early stages, and report them promptly.
Q.8 Discuss the role of mental health nurse (6)
A mental health nurse plays a specialized and essential role in promoting psychological well-being, preventing mental disorders, and caring for individuals with acute, chronic, or emergency psychiatric conditions. Their responsibilities extend beyond bedside care to include assessment, therapeutic communication, medication administration, crisis intervention, psychoeducation, rehabilitation, and community involvement.
✅ 1. Assessment and Observation
- The nurse conducts a complete Mental Status Examination (MSE) to assess the patient’s mood, affect, orientation, thought process, perception, and insight.
- Regular observation is done for behavioral changes, like aggression, withdrawal, overtalkativeness, hallucinations, or suicidal ideation.
- The nurse identifies triggers and stressors that worsen symptoms by reviewing the patient’s past history, environment, and social context.
- Use of structured assessment tools such as depression inventories, suicide risk scales, and anxiety screening questionnaires helps in decision-making.
- The nurse also evaluates the impact of physical health conditions (e.g., thyroid disorders, substance use) on mental status.
✅ 2. Establishing a Therapeutic Relationship
- A mental health nurse builds a trust-based therapeutic alliance using empathy, consistency, nonjudgmental attitude, and confidentiality.
- The nurse encourages the patient to express feelings, fears, or traumatic events without fear of being judged or criticized.
- Rapport facilitates better participation in therapy, medication adherence, and faster recovery, especially in long-term psychiatric conditions.
- Boundaries are maintained to prevent dependency or transference, and regular evaluation of the nurse-patient dynamic is done.
- In manipulative or hostile patients, the nurse ensures firm yet therapeutic limit-setting to preserve professional safety and trust.
✅ 3. Providing Therapeutic Communication
- The nurse uses structured communication techniques like reflection, summarizing, clarification, silence, and validation to enhance expression.
- For disorganized or psychotic patients, the nurse offers reality orientation gently without direct confrontation of delusions or hallucinations.
- Non-verbal cues such as posture, eye contact, and tone are used to convey acceptance and emotional support.
- Communication is modified based on age, literacy level, cognitive status, and cultural background.
- In mute or withdrawn patients, the nurse uses art, music, or journaling as alternative communication modes to promote expression.
✅ 4. Medication Administration and Monitoring
- The nurse ensures timely and accurate administration of psychotropic medications as prescribed — antipsychotics, antidepressants, mood stabilizers, and anxiolytics.
- She observes for side effects such as tremors, weight gain, sedation, and metabolic changes, especially in long-term drug therapy.
- The nurse educates patients and families on drug purpose, action, adherence importance, and what to do if a dose is missed.
- For drugs like lithium or clozapine, the nurse ensures regular blood level monitoring and documentation of clinical effects.
- The nurse must assess for cheeking or refusal of oral medication and use therapeutic persuasion to promote compliance.
✅ 5. Crisis Intervention
- The nurse identifies and responds to psychiatric emergencies like suicidal behavior, acute aggression, panic attacks, or psychotic outbursts.
- Verbal de-escalation, safety assurance, and administration of PRN medications are initiated as per institutional protocol.
- She maintains a calm, non-threatening demeanor and ensures a safe environment by removing harmful objects.
- Post-crisis, the nurse helps the patient understand triggers, emotional responses, and constructive coping strategies.
- Crisis prevention includes early detection of warning signs, patient-family counseling, and relapse management education.
✅ 6. Health Education and Psychoeducation
- The nurse teaches the patient and caregiver about the nature of the illness, expected symptoms, course, and available treatments.
- Psychoeducation includes coping strategies, stress reduction, sleep hygiene, diet, and avoiding relapse triggers.
- Use of pamphlets, posters, videos, or group discussions helps in better retention and interactive learning.
- Nurses encourage patients to ask questions and clarify doubts related to medications or psychiatric terminology.
- She also organizes structured group sessions on anger management, communication skills, and stigma reduction.
✅ 7. Rehabilitation and Psychosocial Support
- The nurse helps patients rebuild confidence and independence through social skills training, vocational rehabilitation, and goal setting.
- She coordinates with occupational therapists, psychologists, and social workers for holistic recovery.
- Patients are involved in role-plays, gardening, daily chores, or self-care tasks to re-establish normal routines.
- The nurse encourages peer group support and group therapy participation to promote confidence and shared healing.
- In chronic or treatment-resistant patients, the nurse helps plan long-term residential rehabilitation or day-care services.
✅ 8. Family Support and Counseling
- The nurse offers family education sessions explaining the patient’s illness, medication, expected behaviors, and relapse signs.
- Emotional support is given to family members facing burnout, guilt, helplessness, or frustration due to long-term caregiving.
- The nurse encourages healthy boundaries and discourages enabling or overprotective behaviors.
- Referrals are made to family therapists or support groups (e.g., Alcoholics Anonymous or caregiver circles) for ongoing help.
- The nurse also advocates for family involvement in discharge planning and home care support programs.
✅ 9. Community Mental Health and Home Visits
- The nurse participates in outreach activities, screening camps, and home visits under the District Mental Health Programme (DMHP).
- Home visits are used to assess home environment, ensure drug adherence, and provide family counseling.
- She identifies cases of school dropouts, substance abuse, elderly neglect, or domestic violence and initiates appropriate referrals.
- The nurse works with Anganwadi workers, ASHA workers, and Panchayat members to improve awareness and reduce stigma.
- Follow-up is ensured through tele-counseling, mobile mental health units, or community mental health centers.
✅ 10. Legal and Ethical Responsibilities
- The nurse adheres to the Mental Health Care Act 2017, ensuring rights to informed consent, privacy, confidentiality, and access to care.
- She obtains legal guardian consent when the patient lacks decision-making capacity and ensures due process during involuntary admissions.
- Nurses are responsible for documenting and reporting use of restraints, seclusion, and critical incidents within legal and ethical frameworks.
- The nurse must report abuse, neglect, or exploitation of psychiatric patients as a mandatory duty.
- She serves as a patient advocate during legal hearings, review boards, and guardianship appointments when required.