02/08/2017-B.SC-CHILD HEALTH NURSING-PAPER (DONE)-UPLOAD NO.5
02/08/2017-B.SC-CHILD HEALTH NURSING-PAPER (DONE)-UPLOAD NO.5
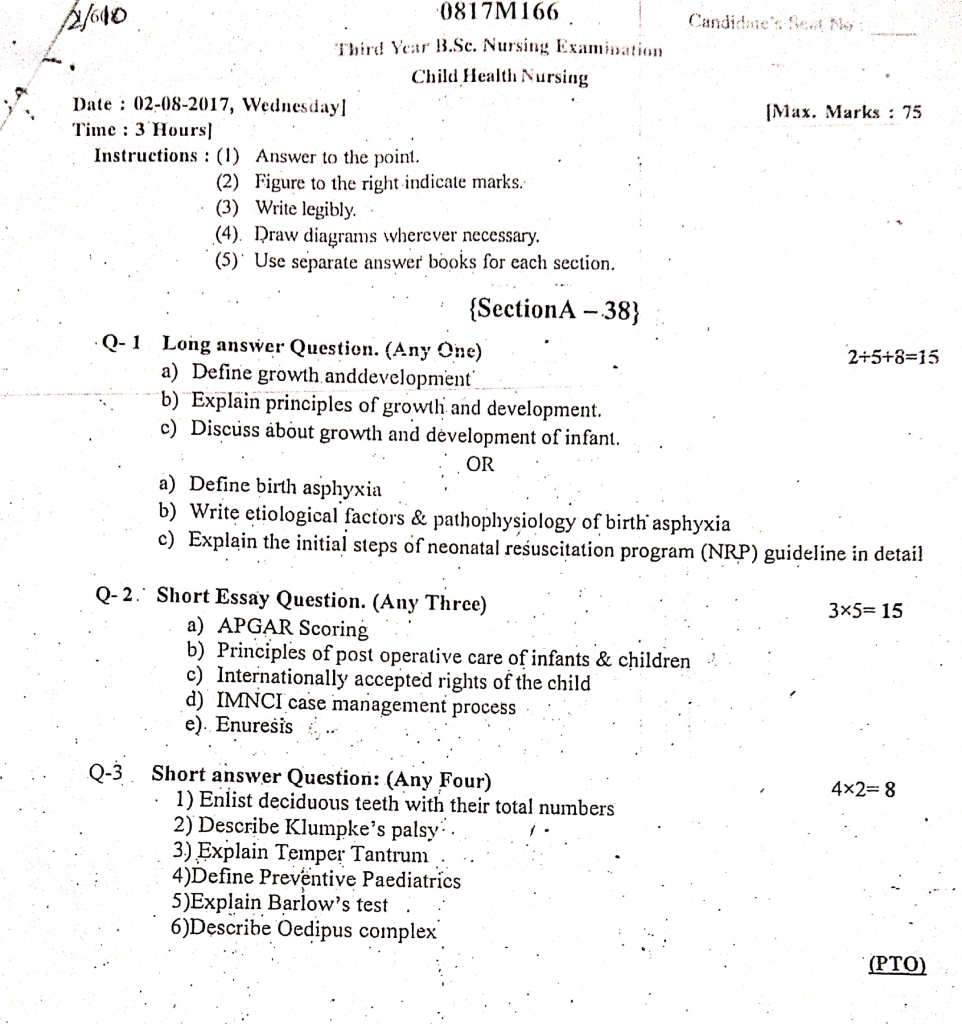
Section A (38)
Q-1 Long answer Question. (Any One) 2+5+8=15
a) Define growth and development
Growth
- Growth refers to the quantitative increase in the size of the body or any of its parts.
- It is measurable in terms of height, weight, head circumference, etc. Example: A baby’s weight increases from 3 kg at birth to 9 kg at one year.
Development
Development refers to the qualitative improvement in functioning — such as acquiring skills, functions, and maturity in various systems. Example: A baby learning to smile, sit, walk, or speak.
b) Explain principles of growth and development.
1.Principle of Continuity
- Growth and development are continuous processes that start from conception and continue throughout life.
- Although the rate of growth may vary during different life stages (rapid during infancy, slow during middle childhood), it never completely stops.
- Example : Physical growth occurs rapidly during infancy and adolescence but continues subtly even in adulthood through cellular renewal.
2.Principle of Orderly Progression (Sequential Development)
- Development follows a definite, predictable sequence.
- This is also called the Cephalocaudal (head to toe) and Proximodistal (center to periphery) patterns.
- Example : A child first gains control over head movements before developing control over limbs.
3.Principle of Individual Differences
- Every child is unique and grows at their own pace.
- Influencing factors : Genetics, nutrition, environment, cultural background, and health conditions.
- Example : Some children may start walking at 10 months, while others may take 14-15 months.
4.Principle of Directionality
- Growth and development occur in specific directions:
- Cephalocaudal Direction : From head to toe (e.g., head control before standing).
- Proximodistal Direction : From the center of the body to outward extremities (e.g., control of arms before fingers).
- General to Specific : Broad motor skills develop before refined skills (e.g., grasping before writing).
5.Principle of Integration
- Simple skills gradually combine to form complex behaviors.
- Example : A child first learns to hold a pencil, then scribble, and later forms letters and words.
6.Principle of Interrelation of Growth and Development
- Physical, mental, emotional, social, and moral developments are interrelated.
- Example : A healthy child with good nutrition is likely to show better concentration and social skills.
7.Principle of Critical Periods
- Certain periods in life are especially important for specific types of development; these are known as critical or sensitive periods.
- Example : Language development is most critical between 2 to 5 years of age.
8.Principle of Maturation and Learning
- Development depends both on maturation (biological growth) and learning (environmental influences).
- Maturation provides the readiness, while learning helps in acquiring skills.
- Example : A child cannot learn to write before the muscles of the fingers are mature enough for fine motor control.
9.Principle of Predictability
- Growth patterns are predictable to a certain extent.
- Example : The eruption of primary teeth usually begins at around 6 months of age; the adolescent growth spurt typically starts around 10-12 years in girls and 12-14 years in boys.
10.Principle of Holistic Development
- Growth and development are holistic, affecting the body as a whole rather than isolated parts.
- Physical, intellectual, emotional, and social developments are interconnected and influence each other.
11 Principle of Uneven Development
- Different parts of the body and different abilities develop at uneven rates.
- Example : A child’s legs may grow faster during one phase, leading to a lanky appearance during adolescence.
12.Principle of Regression
- Sometimes, children may show temporary regression in behavior or skills during periods of stress or emotional disturbance.
- Example : A toilet-trained child may start bedwetting after the birth of a sibling.
13.Principle of Environment and Heredity
- Both genetic inheritance (heredity) and environmental factors play a crucial role in growth and development.
- Example : A child may have inherited a tall stature genetically, but poor nutrition can hinder growth.
c) Discuss about growth and development of infant.
I. Gross Motor Development (Large Muscle Activities)
1 Month :
- Head lag present when pulled to sit.
- Makes jerky arm movements; brings hands to mouth.
- Raises head slightly when lying prone.
- Random limb movements observed due to primitive reflexes.
3 Months :
- Holds head steady when upright; less head lag.
- Raises head and chest during tummy time using forearms.
- Attempts to roll from side to back.
- Pushes down legs when feet are placed on a firm surface.
5–6 Months :
- Rolls over from stomach to back (5 months) and back to stomach (6 months).
- Sits with support; starts bouncing when held in standing position.
- Begins to push up on hands and knees; prepares for crawling.
- Holds head steady even when pulled to a sitting position.
7–8 Months :
- Sits without support for longer periods.
- Starts crawling or scooting; some infants begin creeping.
- Pulls self to a sitting position without help.
- Bears weight on legs and tries to stand when held.
9 Months :
- Pulls to stand; cruises along furniture.
- Can get into sitting position independently.
- May stand momentarily without support.
- Attempts to climb stairs with supervision.
12 Months :
- Walks holding furniture or with caregiver assistance.
- Takes first independent steps by 12–13 months.
- Squats to pick up toys and stands back up.
- Climbs onto low furniture; explores surroundings actively.
II. Fine Motor Development (Hand and Finger Skills)
1 Month :
- Hands mostly fisted; grasp reflex strong.
- Randomly moves arms and hands near face.
3 Months :
- Opens hands more frequently.
- Brings hands together in the midline.
- Reaches for objects but may miss (hand-eye coordination developing).
6 Months :
- Transfers objects from one hand to the other smoothly.
- Grasps objects voluntarily and brings them to the mouth.
- Shakes rattles and explores toys by mouthing and banging.
9 Months :
- Pincer grasp develops (thumb and index finger used to pick small objects).
- Enjoys dropping and picking up objects repeatedly.
- Explores toys by rotating, shaking, and banging them.
- Points to objects of interest.
12 Months :
- Picks up tiny objects like cereals using refined pincer grasp.
- Stacks two blocks; attempts to scribble with a crayon.
- Tries to self-feed with fingers or spoon (may spill food).
- Can drink from a cup with some assistance.
III. Language Development (Speech and Communication)
1–2 Months :
- Makes cooing and gurgling sounds.
- Differentiates cry for hunger, discomfort, or pain.
- Startles or calms to familiar voices.
4–6 Months :
- Babbles repetitive syllables (ba-ba, da-da, ma-ma).
- Laughs out loud and squeals with delight.
- Vocalizes when happy or excited; makes raspberry sounds.
- Responds to caregiver’s voice and music.
9 Months :
- Understands the meaning of “No.”
- Responds to own name and familiar commands.
- Uses a variety of sounds to attract attention.
- Imitates simple sounds and gestures like clapping or waving.
12 Months :
- Speaks 2–3 meaningful words like “Mama,” “Dada,” “Bye.”
- Understands 50–70 words even if unable to speak them.
- Tries to communicate using gestures (pointing, waving).
- Responds to simple questions like “Where’s your toy?”
IV. Social and Emotional Development
2 Months :
- Develops social smile; responds to caregiver’s smile.
- Calms down when comforted or picked up.
- Enjoys watching people’s faces and moving objects.
6 Months :
- Recognizes familiar faces and expresses joy.
- Shows preference for primary caregiver.
- Enjoys interactive games like peek-a-boo and pat-a-cake.
- Shows displeasure when a toy is taken away.
9 Months :
- Develops stranger anxiety; clings to familiar caregivers.
- Displays clear emotional expressions (happiness, anger, frustration).
- Plays interactive games with more understanding.
- May show fear of loud noises or unfamiliar places.
12 Months :
- Waves “bye-bye” and claps hands on request.
- Shows affection through hugs, kisses, and cuddling.
- Enjoys playing simple games and imitates adult actions.
- Begins to develop a sense of independence but still seeks reassurance.
V. Cognitive Development (Thinking and Problem-Solving)
2–4 Months :
- Follows moving objects with eyes smoothly across midline.
- Recognizes familiar caregivers and reacts differently to strangers.
- Develops early understanding of cause and effect (e.g., shaking a rattle makes sound).
6 Months :
- Looks for partially hidden objects (early object permanence).
- Explores toys by putting them into the mouth.
- Enjoys repetitive activities like dropping and retrieving toys.
9 Months :
- Looks for hidden objects actively; understands object permanence.
- Imitates gestures and facial expressions.
- Enjoys exploring surroundings and testing limits.
- Begins to understand concepts like “in” and “out.”
12 Months :
- Understands simple daily routines and participates (e.g., raising arms to dress).
- Points to objects of interest to share attention.
- Attempts to solve simple problems, like moving an obstacle to reach a toy.
- Recognizes familiar people in photographs.
VI. Teething Development
6 Months :
- First tooth eruption begins, usually lower central incisors.
- Chewing on fingers or teething toys relieves gum discomfort.
9–12 Months :
- Typically has 6–8 milk teeth by the end of first year.
- Enjoys biting and chewing on hard foods or teething rings
OR
a) Define birth asphyxia
Birth Asphyxia is a medical condition in which a newborn fails to initiate and sustain adequate breathing at birth, leading to a deficiency of oxygen (hypoxia) and an excess of carbon dioxide (hypercapnia) in the body. This can result in multi-organ damage, particularly affecting the brain, heart, lungs, and kidneys.
b) Write etiological factors & pathophysiology of birth asphyxia
Etiological Factors (Causes) of Birth Asphyxia
📌 1. Antenatal (Before Birth) Causes
Maternal Conditions :
- Severe anemia, hypertension, pre-eclampsia, eclampsia.
- Diabetes mellitus and maternal infections (e.g., TORCH infections).
Placental Factors :
- Placental insufficiency or premature placental aging.
- Placenta previa and abruptio placentae.
Fetal Factors :
- Intrauterine growth restriction (IUGR).
- Multiple gestations (twins, triplets).
- Congenital malformations or chromosomal abnormalities.
📌 2. Intranatal (During Labor and Delivery) Causes
- Prolonged or Obstructed Labor.
- Umbilical Cord Complications:
- Cord prolapse, cord compression, true knots in the cord.
- Birth Trauma or Instrumental Delivery (Forceps, Vacuum).
- Meconium-Stained Amniotic Fluid (Mec aspiration risk).
- Prolonged Premature Rupture of Membranes (PROM).
📌 3. Postnatal (After Birth) Causes
- Prematurity and Low Birth Weight.
- Respiratory Distress Syndrome (RDS) or Lung Immaturity.
- Neonatal Sepsis.
- Congenital Heart Defects or Pulmonary Hypertension.
Pathophysiology of Birth Asphyxia
📌 Initiation of Hypoxia (Reduced Oxygen Supply)
- Due to maternal, placental, or fetal complications, the supply of oxygen to the fetus decreases.
- Hypoxia leads to fetal hypoxemia (low oxygen in the blood), resulting in decreased oxygen delivery to vital tissues and organs.
📌 Switch to Anaerobic Metabolism
- With inadequate oxygen, cells shift from aerobic metabolism to anaerobic metabolism.
- This leads to the production of lactic acid, causing metabolic acidosis.
- Acidosis further impairs cellular enzyme functions and disrupts normal metabolism.
📌 Carbon Dioxide Retention (Hypercapnia):
- Inadequate respiration leads to accumulation of carbon dioxide (CO₂) in the blood, causing respiratory acidosis.
- The combination of metabolic and respiratory acidosis worsens cellular dysfunction.
📌 Cellular Energy Failure
- Due to lack of oxygen and impaired metabolism, the production of adenosine triphosphate (ATP) decreases.
- ATP is essential for maintaining cellular membrane integrity, ion pumps, and active transport mechanisms.
- Without sufficient ATP, cells swell, rupture, and die, leading to tissue injury.
📌 Vital Organ Ischemia
- The body initially attempts to preserve oxygen for vital organs through redistribution of blood flow to the brain, heart, and adrenal glands (a protective mechanism known as the diving reflex).
- If hypoxia continues, even these organs start experiencing ischemia and hypoxic injury.
📌 Hypoxic-Ischemic Encephalopathy (HIE):
- The brain is extremely sensitive to hypoxia.
- Reduced oxygen and nutrient supply lead to neuronal injury, cerebral edema, and disturbances in cerebral blood flow.
- This results in irreversible damage, leading to complications such as seizures, developmental delays, and cerebral palsy.
📌 Multi-Organ Dysfunction Syndrome (MODS):
Prolonged asphyxia affects various organs:
- Heart : Myocardial ischemia, decreased cardiac output, hypotension.
- Lungs : Pulmonary hypertension and meconium aspiration leading to respiratory failure.
- Kidneys : Acute tubular necrosis causing oliguria or anuria.
- Gastrointestinal Tract : Risk of necrotizing enterocolitis due to intestinal ischemia.
- Liver : Impaired metabolic and detoxification functions.
📌 Failure of Compensatory Mechanisms
- As asphyxia progresses, the compensatory mechanisms fail, leading to severe hypoxia, metabolic acidosis, and irreversible cellular damage.
- Without immediate intervention, this may lead to coma, shock, and death.
c) Explain the initial steps of neonatal resuscitation program (NRP) guideline in detail
Preparation Before Birth (Pre-Resuscitation Phase)
Review Maternal and Fetal Risk Factors :
- Preterm labor, prolonged labor, meconium-stained amniotic fluid, maternal infections, diabetes, hypertension, and multiple pregnancies.
Prepare Equipment :
- Airway Equipment : Bulb syringe, mechanical suction with appropriate catheters, oxygen blender.
- Breathing Equipment : Self-inflating bag, flow-inflating bag, T-piece resuscitator, face masks of different sizes.
- Circulation Equipment: Warm towels, radiant warmer, ECG monitor or stethoscope, pulse oximeter.
- Medications (if advanced resuscitation anticipated) : Epinephrine, normal saline for volume expansion.
- Intubation Equipment : Laryngoscope with appropriate blade sizes, endotracheal tubes.
Resuscitation Team Readiness :
- Assign roles (airway management, monitoring, documentation).
- Brief the team about potential complications.
Immediate Rapid Assessment at Birth (Within First 30 Seconds)
Ask 3 Critical Questions :
- Is the baby born at term?
- Is the baby breathing or crying?
- Does the baby have good muscle tone?
If YES to all 3 ➔ Routine Care (Skin-to-skin contact, delayed cord clamping, initiate breastfeeding).
If NO to any question ➔ Proceed with Initial Steps of Resuscitation.
Detailed Initial Steps of Resuscitation (Golden Minute – First 60 Seconds)
1️⃣ Provide Warmth
- Prevent heat loss, especially in preterm infants.
- Place the newborn under a preheated radiant warmer.
- Use warm, dry towels or blankets.
For preterm infants (<32 weeks gestation) :
- Use polyethylene wraps or plastic bags to prevent evaporative heat loss.
- Do not dry the skin before placing in the wrap.
2️⃣ Position the Airway :
- Place the newborn’s head in a sniffing position to open the airway.
- Slight extension of the neck helps align the airway.
- Place a rolled towel under the shoulders if necessary, especially for preterm babies.
- Ensure the head is midline to facilitate effective ventilation.
3️⃣ Clear the Airway (If Needed) :
Routine suctioning is not recommended unless the baby shows signs of airway obstruction.
If necessary :
- Suction the mouth first, followed by the nose to avoid aspiration.
- Use a bulb syringe or mechanical suction with pressure <100 mmHg.
- For meconium-stained amniotic fluid:
- If the baby is vigorous (good tone, breathing, HR >100 bpm) ➔ No suctioning required.
- If the baby is non-vigorous ➔ Prepare for immediate airway clearance and possible intubation for suctioning.
4️⃣ Dry and Stimulate the Baby :
- Dry thoroughly to prevent evaporative heat loss.
- Remove wet towels and replace them with warm, dry towels.
- Stimulate breathing by :
- Gently rubbing the back.
- Flicking or slapping the soles of the feet.
- Avoid aggressive or painful stimulation.
Initial Evaluation After 30 Seconds of Initial Steps
Assess Respiration :
- Is the baby breathing effectively or crying?
- Is there apnea or gasping?
Assess Heart Rate :
- Auscultate with a stethoscope at the precordium.
- Alternatively, palpate the umbilical cord pulse.
- Normal HR should be above 100 bpm.
Assess Color :
- Pink : Normal.
- Central Cyanosis : Indicates inadequate oxygenation.
- Pale or Blue : Suggests poor perfusion or oxygenation
Q-2. Short Essay Question. (Any Three) 3×5=15
a) APGAR Scoring
The APGAR Score is a quick and simple assessment performed on a newborn at 1 minute and 5 minutes after birth to determine the baby’s physical condition and the need for immediate medical intervention. It was developed by Dr. Virginia Apgar in 1952 and remains a standard tool in neonatal care.
Full Form of APGAR
A – Appearance (Skin Color) :
Assesses the color of the baby’s skin to determine oxygenation and circulation.
P – Pulse (Heart Rate) :
Measures the baby’s heart rate using auscultation or palpation of the umbilical cord.
G – Grimace (Reflex Irritability) :
Evaluates the newborn’s response to stimulation (like a mild pinch or suctioning).
A – Activity (Muscle Tone) :
Observes the degree of muscle movement and tone.
R – Respiration (Breathing Effort) :
Assesses the strength and regularity of breathing.
APGAR Score Components
The APGAR score assesses five vital signs, each rated from 0 to 2 points.
| Parameter | 0 Points | 1 Point | 2 Points |
|---|---|---|---|
| Appearance (Skin Color) | Entire body is pale or blue (cyanosis); indicates poor oxygenation | Body is pink, but hands and feet remain blue (acrocyanosis) | Entire body is pink; indicates good oxygenation and circulation |
| Pulse (Heart Rate) | Absent heart rate | Less than 100 beats per minute; indicates bradycardia | 100 beats per minute or more; normal heart rate for newborn |
| Grimace (Reflex Irritability) | No response to stimulation; no facial movement or crying | Weak grimace, slight facial movement, or weak cry when stimulated | Cries loudly, coughs, sneezes, or pulls away when stimulated; strong response |
| Activity (Muscle Tone) | Limp, floppy, no muscle tone or movement | Some flexion of arms and legs; limited movement | Active movement with good muscle tone; resists extension |
| Respiration (Breathing Effort) | Not breathing at all; apnea | Weak, irregular, or shallow breathing; slow respiratory effort | Strong, regular breathing with a vigorous cry |
Total APGAR Score Interpretation
Score 7 to 10 – Normal Newborn Condition :
- Baby is adjusting well to the extrauterine environment.
- Requires only routine postnatal care.
Score 4 to 6 – Moderate Distress :
- Baby may be having difficulty adjusting.
- Requires close monitoring and possibly some interventions (e.g., oxygen administration, airway clearance).
Score 0 to 3 – Severe Distress :
- Baby is in critical condition.
- Requires immediate resuscitative efforts like positive pressure ventilation, chest compressions, or advanced neonatal resuscitation.
Timing of APGAR Scoring
1 Minute Score : Indicates how well the baby tolerated the birthing process.
5 Minute Score: Reflects how well the baby is adapting to the environment after birth.
Additional Scores at 10, 15, or 20 minutes may be taken if the baby’s condition remains poor.
Role of Nurse in APGAR Scoring
Immediate Assessment After Birth
Initial Drying and Stimulation :
- Immediately dry the baby and stimulate breathing by rubbing the back or flicking the soles.
Assess APGAR at 1 and 5 Minutes :
- Quickly assess Appearance, Pulse, Grimace, Activity, and Respiration.
Observe for Abnormalities :
- Look for signs of respiratory distress, poor tone, cyanosis, or lethargy.
Use Appropriate Scoring Techniques :
- Palpate the umbilical pulse for heart rate assessment.
- Observe chest movements and listen for breath sounds.
Accurate Documentation :
- Record precise scores with time, and notify senior staff immediately if scores are low.
Immediate Care Based on APGAR Score
If APGAR 7–10 (Normal) :
- Continue routine newborn care.
- Ensure the baby’s airway is clear and maintain a patent airway.
- Monitor for temperature regulation and prevent hypothermia.
- Encourage early initiation of breastfeeding within the first hour.
- Perform a full newborn assessment including weight, length, and head circumference.
If APGAR 4–6 (Moderate Distress) :
- Provide oxygen via mask if cyanosis or poor breathing is observed.
- Position the newborn in a sniffing position to maintain airway patency.
- Suction the mouth first, then the nose, if secretions are present.
- Prepare for possible escalation to positive pressure ventilation.
- Maintain continuous monitoring of oxygen saturation using a pulse oximeter.
If APGAR 0–3 (Severe Distress) :
- Start Immediate Neonatal Resuscitation following NRP guidelines.
- Clear airway and initiate bag-mask ventilation within the first minute.
- Assess the need for chest compressions if heart rate remains below 60 bpm.
- Prepare for possible endotracheal intubation.
- Administer resuscitative medications if needed under the doctor’s supervision.
4. Supportive and Ongoing Care
- Monitor APGAR scores at 10, 15, and 20 minutes if needed.
- Perform continuous monitoring of temperature, heart rate, respiratory rate, and oxygen saturation.
- Check for early signs of neonatal complications like hypoglycemia, hypothermia, respiratory distress syndrome (RDS), or meconium aspiration.
- Provide kangaroo mother care (skin-to-skin contact) if stable.
- Initiate early immunizations like Vitamin K injection and Hepatitis B vaccination as per protocols.
- Educate the mother about exclusive breastfeeding and newborn care practices.
Documentation and Communication
- Record time and exact APGAR scores accurately in the newborn record.
- Document any interventions performed and the baby’s response to each.
- Maintain detailed records for medico-legal purposes.
- Communicate any abnormalities or deterioration in the baby’s condition immediately to the pediatrician or neonatologist.
- Assist in arranging for NICU transfer if required.
6. Emotional Support
- Provide psychological support to the mother, especially if the baby requires resuscitation or NICU admission.
- Explain in simple language the purpose of assessments and care being provided.
- Encourage mother-infant bonding when the baby’s condition stabilizes.
- Educate the mother and family on warning signs like poor feeding, difficulty breathing, lethargy, and jaundice.
- Provide counseling on the importance of follow-up visits and newborn vaccination.
b) Principles of post operative care of infants & children
Post-operative care for infants and children requires specialized attention due to their immature physiological systems, emotional vulnerability, and higher risk of complications. The primary goals are to ensure a smooth recovery, prevent complications, manage pain effectively, and provide emotional support to both the child and family.
📌 1. Ensure Patent Airway and Adequate Breathing
- Keep the head in the correct position (neutral or slightly extended) to maintain airway patency.
- Use appropriate-size airway adjuncts (oropharyngeal or nasopharyngeal airways) if needed.
- Regularly assess for noisy breathing, stridor, or wheezing.
- Provide humidified oxygen to prevent drying of mucous membranes.
- For children under anesthesia recovery, ensure that suction equipment is ready to clear secretions.
- Watch for signs of aspiration and take precautions, especially after abdominal surgeries.
📌 2. Monitor Circulation and Perfusion
- Continuously monitor heart rate, blood pressure, pulse oximetry, and capillary refill time.
- Assess skin color, temperature, and peripheral pulses frequently.
- Watch for signs of internal bleeding (restlessness, hypotension, tachycardia, pallor).
- Ensure IV lines are patent and check infusion sites for signs of infiltration or phlebitis.
- Calculate and monitor maintenance fluid requirements accurately based on the child’s weight.
- Be vigilant for signs of shock and prepare emergency medications if needed.
📌 3. Effective Pain Management
- Use multimodal pain management (combining analgesics with non-pharmacological methods).
- Assess pain frequently and before and after analgesic administration.
- Educate parents about pain recognition signs (irritability, crying, grimacing, changes in sleep or feeding).
- Administer prescribed medications at scheduled intervals to avoid peaks of severe pain.
- Utilize relaxation techniques, storytelling, playing soft music, or providing pacifiers for infants.
- Offer comfortable positioning to reduce post-surgical discomfort.
📌 4. Monitor Fluid and Electrolyte Balance
- Strictly maintain intake and output records, including urine, vomit, wound drainage, and stool frequency.
- Check for signs of electrolyte imbalances like irritability, muscle twitching, edema, or cardiac irregularities.
- Regularly monitor laboratory values (serum sodium, potassium, calcium) if ordered.
- Observe for dehydration signs: sunken eyes, dry lips, poor skin turgor, and reduced urine output.
- Administer oral or intravenous fluids cautiously as per the doctor’s orders to avoid fluid overload.
📌 5. Nutritional Support
- Assess readiness for oral feeding by checking for bowel sounds and absence of nausea or vomiting.
- Begin with clear liquids, progressing to soft, bland diets as tolerated.
- Encourage breastfeeding immediately after recovery from anesthesia if allowed.
- Monitor for signs of feeding intolerance like abdominal distension, vomiting, and diarrhea.
- Provide high-calorie, protein-rich diets to promote wound healing and tissue repair.
- For children unable to tolerate oral feeds, initiate enteral or parenteral nutrition as prescribed.
📌 6. Prevent Infection
- Practice strict hand hygiene before and after patient contact.
- Inspect the surgical site regularly for redness, warmth, swelling, discharge, or foul odor.
- Ensure timely administration of prescribed prophylactic antibiotics.
- Keep the wound area clean, dry, and covered with sterile dressings.
- Minimize invasive procedures like catheterizations unless absolutely necessary.
- Educate caregivers on proper wound care techniques before discharge.
📌 7. Promote Comfort and Emotional Security
- Create a calm, child-friendly environment to reduce stress and anxiety.
- Allow the presence of parents at the bedside to provide emotional support.
- Encourage the use of comfort objects such as favorite toys, blankets, or pacifiers.
- Minimize unnecessary handling and painful procedures.
- Use distraction techniques like storytelling, cartoons, or mobile visuals to divert attention during dressing changes.
- Provide proper lighting and maintain a quiet environment during rest periods.
📌 8. Early Mobilization and Proper Positioning
- Position the child according to the type of surgery (e.g., semi-Fowler’s for chest surgeries, side-lying to prevent aspiration after oral surgeries).
- Encourage range-of-motion exercises for non-affected limbs to prevent stiffness.
- Assist the child in sitting up and walking as early as possible to prevent complications like pneumonia and deep vein thrombosis.
- Change positions frequently to prevent bedsores and promote circulation.
- Support painful areas with pillows and maintain proper body alignment.
📌 9. Prevent Post-Operative Complications
- Continuously monitor for signs of hemorrhage at the surgical site and internally.
- Encourage deep breathing exercises or use incentive spirometry in older children to prevent atelectasis and pneumonia.
- Watch for signs of urinary retention, especially after spinal or lower abdominal surgeries.
- Monitor for signs of nausea, vomiting, and administer antiemetics as prescribed.
- Be alert for signs of wound dehiscence or herniation in abdominal surgeries.
- Observe for thromboembolic events in immobile children, although rare, and encourage mobility.
📌 10. Psychological Support and Parental Counseling
- Explain all procedures and care processes to parents to reduce their anxiety.
- Provide emotional reassurance to both the child and family members.
- Involve parents in the child’s care activities to increase their confidence and participation.
- Educate parents on home care of surgical wounds, signs of infection, and the importance of follow-up visits.
- Provide clear written instructions for medications, dressing changes, and dietary modifications before discharge.
- Encourage parents to express their concerns and provide counseling if needed, especially for long-term or critical post-operative recovery.
c) Internationally accepted rights of the child
The United Nations Convention on the Rights of the Child (UNCRC) is a legally binding international agreement adopted in 1989 to protect and promote the rights of children worldwide. These rights ensure that children live with dignity, freedom, protection, and access to essential services for healthy growth and development.
1. Right to Survival
- Every child has the inherent right to life and survival from birth.
- Governments must ensure policies that support child health and nutrition programs.
- Access to safe drinking water, sanitation, and hygienic living conditions must be guaranteed.
- Measures to prevent malnutrition and communicable diseases should be prioritized.
- Emergency healthcare services should be accessible during disasters or epidemics.
2. Right to Development
- Right to free and compulsory primary education for every child.
- Opportunities for skill development, vocational training, and higher education should be available.
- Promotion of cultural and recreational activities to support mental and emotional growth.
- Access to early childhood development programs to support brain development in formative years.
- Special provisions for children belonging to marginalized and minority communities to ensure equal development.
3. Right to Protection
- Protection from economic exploitation and hazardous work environments.
- Laws must prevent recruitment of children in armed forces or conflict zones.
- Strict measures against child trafficking, child pornography, and online exploitation.
- Immediate rehabilitation and reintegration programs for rescued children.
- Establishment of child helplines and child protection committees at community levels.
4. Right to Participation
- Children’s views must be considered in matters related to education, health policies, and community decisions.
- Platforms should be created for children’s councils and youth parliaments.
- Right to freedom of expression through media, writing, art, and peaceful assembly.
- Encouragement to participate in cultural heritage preservation and environmental initiatives.
- Special attention to including children with disabilities in participatory activities.
5. Right to Non-Discrimination
- Equal rights must be ensured regardless of race, color, sex, language, religion, political opinion, national or social origin.
- Protection against discriminatory practices in education, healthcare, and legal systems.
- Policies should promote gender equality and inclusion of LGBTQ+ children.
- Special attention to children affected by migration, refugee status, or statelessness.
- Accessible infrastructure and communication methods for children with disabilities.
6. Right to Health and Nutrition
- Immunization programs should be universally available and accessible.
- Provision of adolescent health services, including reproductive and mental health counseling.
- Implementation of school health programs for early detection of health issues.
- Access to affordable and nutritious food under government welfare schemes.
- Regular monitoring of growth and development indicators through healthcare services.
7. Right to Family Environment
- Priority placement with biological families whenever possible, ensuring a safe environment.
- In cases of parental separation, the child’s best interest must be prioritized regarding custody.
- Availability of adoption services following ethical and legal procedures.
- Protection of children from domestic violence and neglect.
- Community-based child care and family strengthening programs should be implemented.
8. Right to Identity
- Every child should receive birth registration immediately after birth.
- Legal identity ensures access to essential services like education, healthcare, and social welfare programs.
- Protection of the child’s name, nationality, and cultural identity, especially for indigenous and tribal communities.
- Governments must prevent statelessness by ensuring nationality rights to children born on their soil.
9. Special Rights for Children with Disabilities
- Ensure accessibility in public spaces, schools, transportation, and communication technologies.
- Provision of inclusive education programs and special education facilities when needed.
- Availability of assistive devices and rehabilitation services.
- Protection against stigma, neglect, and abuse in institutions or care homes.
- Promotion of their independence, dignity, and full participation in society.
d) IMNCI case management process
The IMNCI (Integrated Management of Neonatal and Childhood Illness) is a globally recommended, evidence-based approach developed by WHO and UNICEF to reduce child mortality and improve child health. It focuses on children from birth to 5 years of age and covers both preventive and curative aspects of care.
Step 1: Assess the Child Thoroughly
A systematic and complete assessment is critical to identifying all possible health problems in the child. The assessment includes:
A. Check for General Danger Signs (Applicable for All Sick Children Aged 2 Months to 5 Years)
These danger signs indicate life-threatening conditions requiring urgent referral to a higher healthcare facility.
Danger Signs Include :
- Inability to drink or breastfeed – suggests serious weakness or unconsciousness.
- Vomiting everything – the child cannot retain fluids or medications.
- Convulsions – may indicate severe infections like meningitis or cerebral malaria.
- Lethargy or unconsciousness – suggests severe hypoxia or metabolic imbalance.
- Severe malnutrition – weak immune system and high risk for complications.
B. Assess Main Symptoms
Depending on the child’s complaints, assess specifically for :
- Cough or Difficulty in Breathing – Check for pneumonia or severe respiratory illness.
- Diarrhea – Assess for dehydration and its severity.
- Fever – Evaluate for malaria, dengue, or systemic infections.
- Ear Problems – Identify ear infections or chronic discharge.
- Nutritional Status and Anemia – Check for wasting, stunting, pallor (anemia).
- Immunization Status – Ensure the child has received age-appropriate vaccines.
- Feeding Problems – Particularly for infants, assess breastfeeding adequacy and frequency.
C. For Young Infants (0-2 Months)
- Assess for possible bacterial infections, hypothermia, jaundice, or feeding difficulties.
- These infants are at high risk for rapid deterioration.
Step 2: Classify the Illness Based on Severity (Using Color-Coding)
Classification helps determine urgency and the level of care required :
A. Pink Category (Severe Cases – Immediate Referral) :
- Conditions are life-threatening and need hospital management.
- Example: Severe pneumonia, severe dehydration, severe malnutrition, or very high fever.
B. Yellow Category (Moderate Cases – Treat at Health Facility) :
- The illness is manageable at the primary care level with appropriate medication and caregiver counseling.
- Example: Pneumonia without severe signs, some dehydration, moderate anemia.
C. Green Category (Mild Cases – Home Care) :
- Minor illnesses that can be safely treated at home with supportive care.
- Example: Simple cold, mild diarrhea, minor skin infections.
Step 3: Identify the Appropriate Treatment
Based on classification, initiate prompt treatment :
For Pink Category (Severe Cases) :
- Provide pre-referral treatment (e.g., first dose of antibiotic, oxygen if available).
- Arrange immediate referral to a higher healthcare facility.
- Stabilize the child during transfer.
For Yellow Category (Moderate Cases) :
- Provide appropriate medications:
- Antibiotics for pneumonia.
- Oral Rehydration Salts (ORS) and Zinc for diarrhea.
- Paracetamol for fever.
- Educate the caregiver on:
- How to give medications correctly.
- Signs that indicate the need for immediate return to the clinic.
For Green Category (Mild Cases) :
- Provide simple supportive care:
- Encourage fluids and continued feeding.
- Home remedies if appropriate.
- Advise the caregiver to monitor the child and return if the condition worsens.
Step 4 : Counsel the Mother or Caregiver
- Counseling is a crucial component to ensure that caregivers:
- Understand the nature of the illness and how to manage it at home.
- Learn how to properly administer medications (correct dose, timing, and duration).
- Recognize danger signs that require immediate medical attention.
- Are educated on proper feeding practices, including:
- Exclusive breastfeeding for the first 6 months.
- Introduction of complementary foods at 6 months.
- Continued breastfeeding up to 2 years or beyond.
- Understand the importance of immunization schedules and Vitamin A supplementation.
- Learn how to prepare and give ORS correctly to prevent dehydration.
Step 5: Provide Follow-Up Care
- Ensure the child is brought back for follow-up based on illness severity:
- Pneumonia: Follow-up in 2 days.
- Diarrhea with some dehydration: Follow-up in 5 days.
- Malnutrition or Anemia: Follow-up in 14 days.
- If the condition has not improved or worsened, reassess and provide further management or referral.
e) Enuresis
Definition
Enuresis is the involuntary or repeated urination in children aged 5 years or older, who should have already developed bladder control. It typically occurs during sleep (nocturnal enuresis) but may also occur during the day (diurnal enuresis).
Causes and Contributing Factors
- Genetic factors (Family history of enuresis.)
- Delayed bladder maturity or small bladder capacity.
- Deep sleep patterns – child may not wake up when bladder is full.
- Excessive fluid intake before bedtime.
- Emotional stress – e.g., divorce, school problems.
- Urinary tract infections (UTIs).
- Constipation – can put pressure on the bladder.
- Diabetes mellitus or diabetes insipidus.
- Lack of toilet training or inconsistent routines.
Types of Enuresis
Enuresis (involuntary urination) is mainly classified based on time of occurrence and developmental history.
1. Based on Time of Occurrence
a) Nocturnal Enuresis (Nighttime Bedwetting) :
- It Occurs during sleep, mostly at night.
- It is a Most common type.
- Often due to deep sleep, small bladder, or delayed bladder control.
b) Diurnal Enuresis (Daytime Wetting) :
- It Occurs during waking hours, especially in the afternoon.
- It is More common in girls.
- May be related to urinary urgency, holding behavior, or emotional stress.
c) Mixed Enuresis :
- Involves both nighttime and daytime wetting.
2. Based on Developmental History
a) Primary Enuresis :
- The child has never been dry for more than 6 months since toilet training.
- Often due to delayed maturation, deep sleep, or genetics.
b) Secondary Enuresis :
- The child was dry for at least 6 months, but then started wetting again.
- Usually caused by emotional trauma, stress, UTI, or medical conditions.
Signs and Symptoms
- Repeated bedwetting or wet clothes
- Child may feel embarrassed or ashamed
- Social withdrawal or low self-esteem
- Sometimes irritation or rashes due to wet clothing
- Frequent urination or urgency (especially in diurnal enuresis)
Diagnostic evaluation
- History collection
- Physical Examination
- Urinalysis
- Bladder diary
- Ultrasound
Management
1. Parental Counseling and Education
- Reassure parents that enuresis is common and often self-limiting.
- Explain that punishing the child is inappropriate and may worsen the problem.
- Encourage a positive and supportive attitude toward the child.
2. Behavioral Modification (First-line Approach)
Motivational Therapy :
- Use reward charts (stickers or stars) for dry nights.
- Praise and encourage small successes.
Toilet Training Reinforcement :
- Encourage voiding every 2–3 hours during the day and before bedtime.
- Maintain a bladder diary to track urination and wet nights.
Bladder Training Exercises :
- Help the child gradually increase bladder capacity by delaying urination during the day (under supervision).
Bedwetting Alarms :
- An alarm is attached to underwear or bed linen that sounds when moisture is detected.
- Helps the child learn to wake up with a full bladder.
- Requires consistent use over weeks to months.
3. Lifestyle and Dietary Changes
- Fluid Restriction at Night
- Limit fluids 1–2 hours before bedtime.
- Avoid caffeine and carbonated drinks (bladder irritants).
- Regular Toilet Habits
- Schedule fixed times for urination, including before sleep.
- Manage constipation, as full bowels can worsen enuresis.
4. Pharmacological Management
(Reserved for older children or when behavioral methods fail)
Desmopressin (DDAVP) :
- A synthetic analog of antidiuretic hormone (ADH)
- Reduces urine production at night
- Taken orally or as nasal spray before bedtime
Imipramine :
- A tricyclic antidepressant
- Helps reduce bedwetting but carries risk of side effects (e.g., arrhythmia, mood changes)
Oxybutynin / Tolterodine :
- Anticholinergic drugs used if the child has an overactive bladder or urge incontinence
- Note: Medications are not curative; they only control symptoms and are often used temporarily.
5. Psychological Support
- For children with secondary enuresis due to emotional stress (e.g., divorce, school issues):
- Referral to a child psychologist or counselor
- Address underlying emotional or family problems
6. Treat Underlying Medical Conditions
- If caused by UTI, diabetes mellitus, spina bifida, or epilepsy, then:
- Investigate and treat the root cause
- Includes urinalysis, blood sugar tests, and neurological evaluation if needed
Q-3 Short answer Question: (Any Four) 4×2=8
1) Enlist deciduous teeth with their total numbers
Total Number of Deciduous Teeth = 20
Each jaw (upper and lower) has :
- Incisors – 8 teeth
- 4 upper (2 central + 2 lateral)
- 4 lower (2 central + 2 lateral)
- Canines – 4 teeth
- 2 upper
- 2 lower
- Molars – 8 teeth
- 4 upper (2 each side)
- 4 lower (2 each side)
2) Describe Klumpke’s palsy
Klumpke’s palsy is a type of lower brachial plexus injury, involving the C8 and T1 nerve roots, which results in weakness or paralysis of the forearm, wrist, and hand muscles, especially the intrinsic muscles of the hand. It leads to a characteristic “claw hand” deformity and may also be associated with Horner’s syndrome (if sympathetic fibers are affected).
3) Explain Temper Tantrum
A temper tantrum is a sudden, intense display of anger, frustration, or emotional outburst by a young child, often involving crying, screaming, kicking, hitting, or breath-holding. It is common between ages 1 to 4 years, especially when the child is unable to express needs or emotions effectively.
4) Define Preventive Paediatrics
Preventive Paediatrics is a branch of paediatrics that focuses on the prevention of diseases, promotion of health, and early diagnosis and management of conditions in infants, children, and adolescents, to ensure optimal growth and development. It includes immunization, nutrition, growth monitoring, health education, and screening for developmental delays or disorders.
5) Explain Barlow’s test
Barlow’s test is a clinical examination used in newborns to detect developmental dysplasia of the hip (DDH) — specifically, to check if the hip can be dislocated. In which baby’s hip and knees are flexed, and the examiner applies gentle posterior pressure on the knee while adducting the thigh (bringing it toward the midline). A “clunk” or sensation of dislocation indicates a positive Barlow’s test.
6) Describe Oedipus complex
Oedipus complex is a psychoanalytic concept introduced by Sigmund Freud, where a male child feels unconscious sexual desire for his mother and sees his father as a rival for her attention. This occurs during the phallic stage of psychosexual development (around 3 to 6 years of age).