01/08/2016-B.SC-CHILD HEALTH NURSING-PAPER (DONE)-UPLOAD NO.6
01/08/2016-B.SC-CHILD HEALTH NURSING-PAPER (DONE)-UPLOAD NO.6
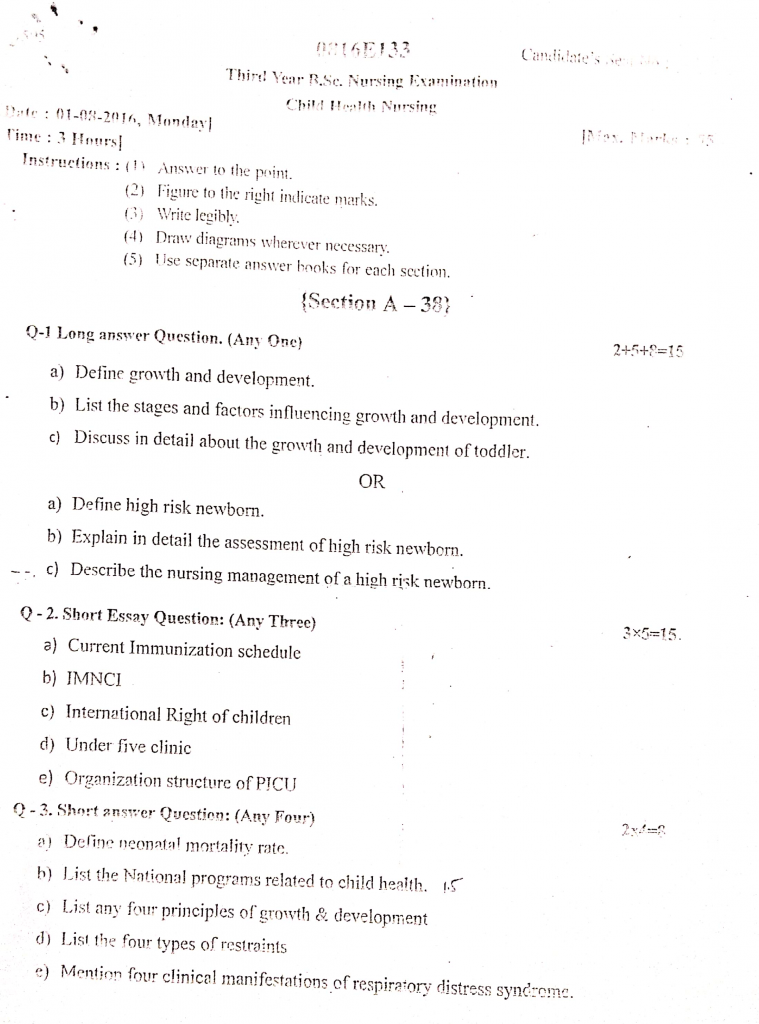
(Section A (38)
Q-1 Long answer Question. (Any One) 2+5+8=15
a) Define growth and development.
Growth
Growth is a quantitative increase in the size, height, weight, or mass of the body or any of its parts. It refers to physical changes and can be measured in units (like centimeters or kilograms). Example : Increase in height or weight of a child.
Development
Development is a qualitative improvement in the functioning or capabilities of the individual. It refers to the maturation of physical, emotional, intellectual, and social abilities. Example : A child learning to speak, walk, or develop social skills.
b) List the stages and factors influencing growth and development.
List of Stages of Growth and Development
Prenatal Stage (Conception to Birth)
Phases :
- Germinal (Conception to 2 weeks)
- Embryonic (2 to 8 weeks)
- Fetal (8 weeks to birth)
Infancy (Birth to 1 Year)
Rapid physical growth and development of basic motor skills.
Toddler Stage (1 to 3 Years)
Development of walking, simple language skills, and independence.
Preschool/ Early Childhood (3 to 6 Years)
Socialization, language development, and refinement of motor skills.
Late Childhood (6 to 12 Years)
Steady physical growth, intellectual development, and peer relationships.
Adolescence (12 to 18 Years)
Puberty, emotional changes, identity formation, and abstract thinking development.
Early Adulthood (18 to 40 Years)
Career building, intimate relationships, and physical peak.
Middle Adulthood (40 to 65 Years)
Maturity, stability, and focus on family and career achievements.
Late Adulthood (Above 65 Years)
Physical decline, retirement, and reflection on life experiences.
List of Factors Influencing Growth and Development
- Genetic Factors (Heredity)
- Prenatal Factors
- Nutritional Factors
- Biological and Physical Factors
- Psychological and Emotional Factors
- Family and Socioeconomic Factors
- Environmental Factors
- Cultural and Religious Factors
- Health and Medical Care Factors
- Hormonal Factors
- Gender of the Child
- Climate and Geographical Conditions
- Peer Group and Social Relationships
- Educational Opportunities and Stimulation
c) Discuss in detail about the growth and development of toddler.
A toddler is a child between 1 to 3 years of age. This is a critical period characterized by rapid physical growth, significant motor development, language acquisition, emotional and social development, and the beginning of independence.
1. Physical Growth:
Weight :
- Gains about 2–3 kg per year after the first birthday.
- By 2 years, weight is about 4 times the birth weight.
Height :
- Increases by approximately 12 cm in the second year and 8 cm in the third year.
- At 2 years, the child reaches about half of their adult height.
Head and Chest Circumference :
- Head circumference growth slows down to about 49–50 cm by 2 years.
- Chest circumference becomes equal to or exceeds head circumference by the end of the toddler period.
Dentition :
- By 2.5 years, the child typically has 20 deciduous (milk) teeth.
- Important phase for starting regular dental hygiene habits.
2. Motor Development
Gross Motor Development :
- Walks alone by 12–15 months.
- Begins running by 18 months, though often clumsy.
- Climbs stairs with assistance by 2 years and without help by 3 years.
- Throws and kicks a ball by 2 years.
- Can jump with both feet by 2.5–3 years.
Fine Motor Development :
- Uses a pincer grasp effectively by 1 year.
- Can build a tower of 4–6 blocks by age 2.
- Begins drawing simple shapes like circles and straight lines by 3 years.
- Starts learning self-help skills like feeding with a spoon, undressing, and brushing teeth with supervision.
3. Cognitive Development (Piaget’s Theory)
- Shifts from the Sensorimotor Stage (birth to 2 years) to the Preoperational Stage (2–7 years).
- Shows object permanence (understands that objects exist even when not visible).
- Imitates actions of parents and siblings (observational learning).
- Engages in symbolic play (pretending objects represent something else).
- Starts using trial and error learning and gradually understands cause and effect.
4. Language Development
2–18 Months : Understands simple commands, speaks around 10–15 words.
18–24 Months :
- Rapid vocabulary growth; speaks about 50–100 words.
- Starts using two-word phrases (“want juice,” “go park”).
2–3 Years :
- Vocabulary increases to 300–500 words.
- Begins forming short sentences.
- Frequently asks “why” and “what” questions.
- Understands names of familiar people, objects, and body parts.
5. Emotional and Social Development (Erikson’s Stage)
- Stage : Autonomy vs. Shame and Doubt (1–3 years)
- Tries to become independent—wants to choose clothes, feed self, and explore surroundings.
- May show temper tantrums when desires are not fulfilled.
- Experiences separation anxiety, especially during hospitalizations or when away from parents.
- Begins to understand the concept of ownership (“mine” phase).
- Shows affection toward caregivers but may be wary of strangers (stranger anxiety).
6. Play and Socialization
- Type of Play : Parallel Play – plays near other children but does not actively interact or share toys.
- Enjoys push-pull toys, stacking blocks, picture books, simple puzzles, and pretend play.
- Participates in simple group activities by the end of the toddler period.
- Starts imitating daily activities like cooking, cleaning, and talking on a phone.
7. Moral Development (Kohlberg’s Pre-conventional Stage)
- Begins to develop a sense of right and wrong based on consequences.
- Obeys rules primarily to avoid punishment rather than understanding moral reasons.
- Imitates behaviors observed in parents and caregivers.
8. Nutritional Considerations
- Growth rate slows, and appetite decreases (physiological anorexia common around 18 months).
- Requires about 1,000–1,300 kcal/day.
- Encourage finger foods and offer small, frequent meals.
- Milk intake should be limited to 500–700 mL/day to avoid iron-deficiency anemia.
- Important to introduce a variety of foods to develop healthy eating habits.
- Start toilet training when the child shows readiness (stays dry for 2 hours, indicates discomfort with soiled diapers).
9. Health Promotion
- Continue immunization schedule as per national guidelines (MMR, DPT boosters, Hepatitis A, etc.).
- Educate parents about accident prevention (childproofing the home).
- Regular health check-ups for monitoring growth parameters and developmental milestones.
- Introduce and encourage oral hygiene practices as teeth eruption is complete by 2–2.5 years.
OR
a) Define high risk newborn.
A high-risk newborn is an infant who, because of preterm birth, postmaturity, low birth weight, birth trauma, congenital anomalies, or maternal health issues, requires specialized observation, intervention, or treatment to survive and develop normally.
b) Explain in detail the assessment of high risk newborn.
1. Immediate Post-Birth Assessment (Within the First Few Minutes)
A. APGAR Scoring (At 1 and 5 Minutes) :
- A – Appearance (Skin Color): Pink, pale, or cyanotic.
- P – Pulse (Heart Rate): Should be >100 bpm.
- G – Grimace (Reflex Irritability): Crying or grimacing to stimulation.
- A – Activity (Muscle Tone): Active flexion is normal.
- R – Respiration: Strong cry indicates good respiratory effort.
Interpretation :
- 7–10: Normal
- 4–6: Moderate difficulty
- 0–3: Severe distress; requires resuscitation
B. Physical Examination Immediately After Birth
- Color : Pink is normal; check for cyanosis (hypoxia) or pallor (anemia, shock).
- Breathing : Observe for normal spontaneous breathing; look for grunting, nasal flaring, and retractions.
- Heart Rate : Should be 120–160 bpm; check for bradycardia or tachycardia.
- Muscle Tone and Activity : Flexed posture and active movements are normal. Hypotonia may indicate hypoxia or neurologic issues.
- Cry : A strong, loud cry is reassuring; a weak or high-pitched cry may indicate neurologic problems.
2. Vital Signs Assessment
Temperature :
- Monitor closely for hypothermia (<36.5°C) or hyperthermia (>37.5°C), as newborns are prone to temperature instability.
Heart Rate :
- Normal range: 120–160 beats/min.
- Bradycardia or tachycardia may suggest hypoxia or sepsis.
Respiratory Rate :
- Normal range: 30–60 breaths/min.
- Assess for signs of respiratory distress :
- Tachypnea (>60 breaths/min)
- Grunting, nasal flaring, chest retractions
- Apnea episodes (>20 seconds)
Blood Pressure :
- Not routinely measured unless critically ill or suspected cardiovascular abnormalities.
3. Anthropometric Measurements
Weight :
- Low Birth Weight (LBW): <2500 g
- Very Low Birth Weight (VLBW): <1500 g
- Extremely Low Birth Weight (ELBW): <1000 g
Length :
- Average at birth: 45–50 cm
Head Circumference :
- Average: 33–35 cm; assess for microcephaly or hydrocephalus.
Chest Circumference :
- Normally about 2 cm less than head circumference.
4. Neurological Assessment
Primitive Reflexes :
Check for presence of reflexes :
- Moro Reflex (Startle Reflex)
- Rooting and Sucking Reflex
- Palmar and Plantar Grasp
- Babinski Reflex
Absence or asymmetry of reflexes indicates CNS depression or birth trauma.
Tone and Activity :
- Normal newborns have flexed limbs and active movements.
- Hypotonia or hypertonia requires further evaluation.
5. Respiratory System Assessment
Observe for :
- Grunting, flaring of nostrils, chest indrawing, and cyanosis.
- Assess breath sounds for crepitations or diminished air entry.
- Consider conditions like Respiratory Distress Syndrome (RDS), Meconium Aspiration Syndrome, or Congenital Pneumonia.
6. Cardiovascular Assessment
Check for :
- Heart murmurs indicating congenital heart disease.
- Capillary refill time (<3 seconds is normal).
- Peripheral pulses for volume and equality.
7. Gastrointestinal System Assessment
- Check abdominal distension, visible veins, or palpable masses.
- Assess for passage of meconium within 24 hours; absence may indicate Hirschsprung’s disease or intestinal obstruction.
- Check for feeding tolerance and signs of vomiting or regurgitation.
8. Genitourinary Assessment
- Assess for urinary output (should void within the first 24 hours).
- Examine external genitalia for anomalies such as hypospadias, epispadias, or ambiguous genitalia.
- In male infants, check for undescended testes (cryptorchidism).
9. Integumentary (Skin) Assessment
- Observe for skin integrity, rashes, bruising, or petechiae.
- Assess for signs of birth trauma (cephalhematoma, caput succedaneum).
- Examine for dehydration signs: sunken fontanelles, dry mucous membranes.
10. Metabolic Assessment
- Monitor for hypoglycemia : Look for jitteriness, poor feeding, lethargy, or seizures.
- Check blood glucose levels in at-risk babies (e.g., infants of diabetic mothers, preterm, LBW).
c) Describe the nursing management of a high risk newborn.
✅ Assessment and Monitoring
- Monitor vital signs: temperature, respiratory rate, heart rate, SpO₂.
- Observe for respiratory distress: nasal flaring, grunting, chest retractions.
- Assess for cyanosis, pallor, and jaundice.
- Evaluate neurological status: activity, tone, reflexes, seizure activity.
- Record daily weight, head circumference, and length.
- Monitor intake and output: urine, stool, and feeding amounts.
- Check for signs of hypoglycemia: jitteriness, lethargy, poor feeding.
- Regularly assess umbilical stump for signs of infection.
- Monitor fontanelle for bulging or sunken appearance.
- Document all findings accurately and promptly in the neonatal chart.
- Evaluate oxygen saturation continuously in unstable newborns.
- Perform lab investigations: blood glucose, bilirubin, CBC, electrolytes as ordered.
✅ Thermoregulation
- Place the baby under radiant warmer or in an incubator.
- Maintain neutral thermal environment (36.5°C–37.5°C).
- Avoid cold exposure, drafts, and unnecessary clothing changes.
- Dry the baby immediately after birth to prevent evaporative heat loss.
- Use warm blankets and caps, especially in preterm infants.
- Monitor axillary temperature every 2–4 hours.
- Encourage kangaroo mother care (KMC) if stable.
- Warm feeding bottles and IV fluids before administration.
- Avoid overheating, which can lead to dehydration.
- Use plastic wraps for very low birth weight babies if incubator is unavailable.
- Pre-warm linen and clothing before use.
- Educate caregivers on the importance of temperature maintenance at home.
✅ Nutritional Support
- Initiate early feeding with expressed breast milk (EBM).
- Use gavage or orogastric tube feeding in babies with poor suck/swallow reflex.
- Administer IV fluids or TPN if enteral feeding is contraindicated.
- Monitor for abdominal distension, vomiting, or residuals.
- Provide small frequent feeds as per tolerance.
- Support and guide mother in milk expression and storage.
- Promote breastfeeding as soon as the baby is stable.
- Maintain strict input-output charting.
- Assess weight gain regularly.
- Monitor blood glucose to prevent hypoglycemia.
- Provide iron and vitamin supplements if advised.
- Educate parents on feeding cues, hygiene, and signs of intolerance.
✅ Respiratory Support
- Position baby in sniffing position to maintain airway patency.
- Administer humidified oxygen through nasal cannula or hood.
- Use CPAP or mechanical ventilation for respiratory failure.
- Monitor for signs of apnea, tachypnea, and cyanosis.
- Perform gentle suctioning as needed to clear secretions.
- Keep resuscitation equipment readily available.
- Use pulse oximetry and ABG monitoring as required.
- Monitor for oxygen toxicity and prevent hyperoxia.
- Document oxygen delivery method and duration.
- Prevent infection of respiratory equipment.
- Encourage minimal handling to reduce oxygen demand.
- Provide chest physiotherapy only if prescribed.
✅ Infection Control
- Practice strict hand hygiene before and after handling the newborn.
- Use sterile gloves and equipment during procedures.
- Minimize the use of invasive lines (IV, catheters).
- Clean and disinfect incubators, warmers, and surfaces regularly.
- Administer antibiotics/antifungals as per culture sensitivity.
- Monitor for fever, lethargy, poor feeding, or tachypnea.
- Isolate baby if sepsis or communicable disease is suspected.
- Avoid overcrowding and unnecessary visitors.
- Change dressings, IV sites, and diapers using aseptic technique.
- Handle umbilical stump and perineal area with care.
- Encourage early breastfeeding to boost immunity.
- Educate parents on infection prevention at home.
✅ Promoting Bonding and Development
- Encourage skin-to-skin contact (KMC) regularly.
- Allow parents to touch, hold, and talk to the baby.
- Maintain a quiet, dimly lit environment to reduce stress.
- Involve parents in diapering, feeding, and comforting.
- Avoid unnecessary separations unless medically indicated.
- Support parents to express love and emotional connection.
- Provide reassurance and consistent updates on the baby’s condition.
- Support early breastfeeding for bonding and nutrition.
- Use soft voice and touch during care procedures.
- Explain all procedures to parents clearly and patiently.
- Avoid unnecessary painful procedures (cluster care).
- Offer parenting guidance to build confidence.
✅ Elimination and Skin Care
- Monitor urine output (at least 6–8 wet diapers/day after first week).
- Observe for meconium passage and stool pattern.
- Assess for signs of dehydration: dry lips, sunken fontanelle.
- Provide gentle perineal care after every diaper change.
- Use barrier creams to prevent diaper rash.
- Reposition baby every 2–3 hours to prevent pressure sores.
- Keep skin dry, especially in skin folds and diaper area.
- Use hypoallergenic products for skin cleaning.
- Check for bruises, pressure marks, or skin breakdown.
- Maintain good cord care to prevent omphalitis.
- Observe for urinary tract infections in catheterized babies.
- Document all elimination patterns regularly.
✅ Psychosocial Support and Parent Education
- Provide emotional reassurance and active listening to parents.
- Offer counseling services if baby is critically ill or has anomalies.
- Encourage parental presence and participation in care.
- Educate about feeding, hygiene, danger signs, and immunization.
- Provide written materials and demonstrations if needed.
- Encourage questions and open communication.
- Respect cultural and emotional values during care.
- Support parents during NICU visits and transitions.
- Arrange support groups or peer counseling for long-term care.
- Teach safe handling, holding, and thermoregulation practices.
- Empower parents by acknowledging their efforts and strengths.
- Prepare them for home care and follow-up before discharge.
✅ Discharge Planning
- Ensure baby is clinically stable, feeding well, and gaining weight.
- Confirm that vital signs and temperature are normal.
- Complete immunization schedule or give catch-up plan.
- Provide discharge education on newborn care.
- Schedule follow-up appointments and specialist referrals.
- Educate on home safety, thermoregulation, feeding, and sleep.
- Provide instructions on emergency signs (fever, refusal to feed, breathing difficulty).
- Ensure baby has appropriate clothing and clean environment at home.
- Arrange for community nurse visits or telephonic follow-up if needed.
- Guide on continuing KMC, breastfeeding, and hygiene.
- Provide helpline numbers or contacts for neonatal emergencies.
- Instruct on use of medications or supplements if any.
Q-2. Short Essay Question: (Any Three) 3×5=15
a) Current Immunization schedule
Immunization Schedule for Infants and Children
| Age | Vaccine | Dose | Route | Site |
|---|---|---|---|---|
| At Birth | BCG | 0.1 mL | Intradermal | Left upper arm |
| Hepatitis B (Birth dose) | 0.5 mL | Intramuscular | Anterolateral thigh (left) | |
| OPV-0 | 2 drops | Oral | Oral | |
| 6 Weeks | Pentavalent-1 | 0.5 mL | Intramuscular | Anterolateral thigh (left) |
| OPV-1 | 2 drops | Oral | Oral | |
| IPV-1 | 0.5 mL | Intramuscular | Anterolateral thigh (right) | |
| Rotavirus-1 | 5 drops (varies) | Oral | Oral | |
| PCV-1 (Pneumococcal) | 0.5 mL | Intramuscular | Anterolateral thigh (right) | |
| 10 Weeks | Pentavalent-2 | 0.5 mL | Intramuscular | Anterolateral thigh (left) |
| OPV-2 | 2 drops | Oral | Oral | |
| IPV-2 | 0.5 mL | Intramuscular | Anterolateral thigh (right) | |
| Rotavirus-2 | 5 drops (varies) | Oral | Oral | |
| PCV-2 | 0.5 mL | Intramuscular | Anterolateral thigh (right) | |
| 14 Weeks | Pentavalent-3 | 0.5 mL | Intramuscular | Anterolateral thigh (left) |
| OPV-3 | 2 drops | Oral | Oral | |
| IPV-3 | 0.5 mL | Intramuscular | Anterolateral thigh (right) | |
| Rotavirus-3 | 5 drops (varies) | Oral | Oral | |
| PCV-3 | 0.5 mL | Intramuscular | Anterolateral thigh (right) | |
| 9 Months | Measles-Rubella (MR-1) | 0.5 mL | Subcutaneous | Right upper arm |
| JE-1 (in endemic areas) | 0.5 mL | Subcutaneous | Left upper arm | |
| Vitamin A (1st dose) | 1 mL (1 lakh IU) | Oral | Oral | |
| 16–24 Months | DPT Booster-1 | 0.5 mL | Intramuscular | Anterolateral thigh (left) |
| OPV Booster | 2 drops | Oral | Oral | |
| MR-2 | 0.5 mL | Subcutaneous | Right upper arm | |
| JE-2 (in endemic areas) | 0.5 mL | Subcutaneous | Left upper arm | |
| Vitamin A (2nd dose) | 2 mL (2 lakh IU) | Oral | Oral | |
| 2–5 Years | Vitamin A (3rd to 9th doses) | 2 mL (2 lakh IU) | Oral | Oral |
| 5–6 Years | DPT Booster-2 | 0.5 mL | Intramuscular | Upper arm |
| 10 Years | Td (Tetanus + Diphtheria) | 0.5 mL | Intramuscular | Upper arm |
| 16 Years | Td (Tetanus + Diphtheria) | 0.5 mL | Intramuscular | Upper arm |
Immunization Schedule for Pregnant Women
| Stage | Vaccine | Dose | Route | Site |
|---|---|---|---|---|
| Early pregnancy | Td-1 | 0.5 mL | Intramuscular | Upper arm |
| 4 weeks after Td-1 | Td-2 | 0.5 mL | Intramuscular | Upper arm |
| Next pregnancy (if Td2 given earlier) | Td Booster | 0.5 mL | Intramuscular | Upper arm |
b) IMNCI
Definition
- IMNCI stands for Integrated Management of Neonatal and Childhood Illness.
- It is a comprehensive strategy developed by WHO and UNICEF, adapted by the Government of India, to address the major causes of child mortality and morbidity in children under 5 years of age.
- India modified it to include the neonatal component (0–7 days) and hence renamed it from IMCI (original global strategy) to IMNCI.
Objectives of IMNCI
- To reduce infant, neonatal, and under-5 mortality.
- To improve the quality of healthcare services for children.
- To enhance the skills of healthcare workers in managing common childhood illnesses.
- To promote early detection and appropriate referral of serious cases.
- To strengthen family and community practices for child health and nutrition.
Key Components of IMNCI
1. Improvement in Case Management Skills
Training healthcare providers (ANMs, ASHAs, Medical Officers) to assess, classify, and manage sick children effectively.
Use of standardized color-coded charts for case classification :
- Pink : Urgent referral or hospitalization.
- Yellow : Treatment at health facility.
- Green : Home care advice.
2. Strengthening Health Systems
- Ensuring the availability of essential drugs, vaccines, and equipment.
- Establishing referral systems for timely management of critical cases.
- Strengthening primary health centers and community health centers for better service delivery.
3. Improvement in Family and Community Practices
- Educating caregivers about home management of childhood illnesses.
- Promoting practices like exclusive breastfeeding, proper weaning, immunization, and hygiene.
- Encouraging timely care-seeking behavior and danger sign recognition.
IMNCI Case Management Process
Assessment :
Check for danger signs: Inability to feed, convulsions, lethargy, vomiting, severe chest indrawing.
Assess for common illnesses :
- Diarrhea
- Pneumonia/Cough
- Malnutrition
- Fever/Malaria
- Ear Infections
Classification :
- Based on signs and symptoms, classify illness into Severe, Moderate, or Mild.
Treatment and Referral
- Provide immediate treatment or refer if severe illness is identified.
- Advise caregivers about home care and when to return for follow-up.
Essential Newborn and Child Health Interventions under IMNCI
Essential Newborn Care (ENC) :
Early initiation of breastfeeding, cord care, prevention of hypothermia.
Kangaroo Mother Care (KMC) :
For low birth weight infants.
Immunization :
As per Universal Immunization Programme (UIP).
Management of Malnutrition :
Identification and treatment of SAM (Severe Acute Malnutrition).
Diarrhea Management :
ORS and Zinc supplementation.
Pneumonia Management :
Early antibiotic therapy.
Vitamin A Supplementation :
To prevent nutritional blindness.
Role of Nurse in IMNCI (Integrated Management of Neonatal and Childhood Illness)
1. Health Assessment and Early Detection
- Perform comprehensive systemic examinations (respiratory, gastrointestinal, neurological systems).
- Assess and document danger signs like grunting, chest indrawing, lethargy, and cyanosis.
- Evaluate the mother’s knowledge about child care practices and provide guidance as needed.
- Check for immunization status and advise catch-up doses if required.
- Perform routine screening for anemia and vitamin deficiencies in high-risk children.
2. Management of Common Childhood Illnesses
- Administer correct dosages of antipyretics and antibiotics according to IMNCI guidelines.
- Educate caregivers on home management of common illnesses like cough, cold, and mild diarrhea.
- Demonstrate proper techniques for steam inhalation and nebulization for respiratory issues.
- Ensure availability of essential medications like ORS, zinc tablets, and antibiotics at health centers.
- Monitor for signs of improvement or deterioration and take immediate action accordingly.
3. Immunization Services
- Organize immunization outreach sessions in remote and underserved areas.
- Maintain proper storage of vaccines using cold chain equipment like ILRs (Ice Lined Refrigerators).
- Keep updated records of Adverse Events Following Immunization (AEFI) and report promptly.
- Educate parents about missed vaccines and rescheduling based on the child’s age.
- Collaborate with ASHAs and Anganwadi workers to improve immunization coverage.
4. Counseling and Health Education
- Educate mothers about appropriate complementary feeding practices after six months of age.
- Provide counseling on the prevention and early detection of common childhood infections.
- Guide parents about the importance of deworming and periodic deworming schedules.
- Raise awareness on prevention of accidents and injuries at home.
- Encourage participation in government schemes like Janani Suraksha Yojana (JSY) for maternal and child health benefits.
5. Growth Monitoring and Nutritional Support
- Counsel parents on providing a balanced diet using locally available nutritious food items.
- Identify children with moderate and severe acute malnutrition (MAM/SAM) and initiate management protocols.
- Promote the use of Ready-to-Use Therapeutic Foods (RUTF) where applicable.
- Organize nutrition education sessions at health centers and community gatherings.
- Educate mothers about the importance of continued breastfeeding during illness.
6. Referral and Follow-Up
- Maintain a clear referral register with details of referred cases and outcomes.
- Accompany critically ill children to referral centers when necessary.
- Ensure effective communication between referring and receiving facilities for continuity of care.
- Schedule and conduct post-discharge follow-up visits to monitor recovery and prevent relapse.
- Provide caregivers with clear instructions about home care during recovery and warning signs.
7. Community Involvement and Home Visits
- Conduct health education campaigns on hygiene, sanitation, and nutrition.
- Work with community leaders to address social determinants of child health (poverty, illiteracy, poor sanitation).
- Encourage the formation of self-help groups and women’s groups to promote child health initiatives.
- Identify and support families in accessing government welfare programs for child nutrition and health.
- Establish child health corners or clinics within the community to improve accessibility to services.
c) International Right of children
The United Nations Convention on the Rights of the Child (UNCRC), adopted in 1989, is the most comprehensive global legal framework that ensures protection, development, survival, and participation rights for all children under 18 years of age. It has been ratified by nearly every country in the world.
1. Right to Survival
- Every child has the inherent right to life and survival from birth.
- Governments must ensure policies that support child health and nutrition programs.
- Access to safe drinking water, sanitation, and hygienic living conditions must be guaranteed.
- Measures to prevent malnutrition and communicable diseases should be prioritized.
- Emergency healthcare services should be accessible during disasters or epidemics.
2. Right to Development
- Right to free and compulsory primary education for every child.
- Opportunities for skill development, vocational training, and higher education should be available.
- Promotion of cultural and recreational activities to support mental and emotional growth.
- Access to early childhood development programs to support brain development in formative years.
- Special provisions for children belonging to marginalized and minority communities to ensure equal development.
3. Right to Protection
- Protection from economic exploitation and hazardous work environments.
- Laws must prevent recruitment of children in armed forces or conflict zones.
- Strict measures against child trafficking, child pornography, and online exploitation.
- Immediate rehabilitation and reintegration programs for rescued children.
- Establishment of child helplines and child protection committees at community levels.
4. Right to Participation
- Children’s views must be considered in matters related to education, health policies, and community decisions.
- Platforms should be created for children’s councils and youth parliaments.
- Right to freedom of expression through media, writing, art, and peaceful assembly.
- Encouragement to participate in cultural heritage preservation and environmental initiatives.
- Special attention to including children with disabilities in participatory activities.
5. Right to Non-Discrimination
- Equal rights must be ensured regardless of race, color, sex, language, religion, political opinion, national or social origin.
- Protection against discriminatory practices in education, healthcare, and legal systems.
- Policies should promote gender equality and inclusion of LGBTQ+ children.
- Special attention to children affected by migration, refugee status, or statelessness.
- Accessible infrastructure and communication methods for children with disabilities.
6. Right to Health and Nutrition
- Immunization programs should be universally available and accessible.
- Provision of adolescent health services, including reproductive and mental health counseling.
- Implementation of school health programs for early detection of health issues.
- Access to affordable and nutritious food under government welfare schemes.
- Regular monitoring of growth and development indicators through healthcare services.
7. Right to Family Environment
- Priority placement with biological families whenever possible, ensuring a safe environment.
- In cases of parental separation, the child’s best interest must be prioritized regarding custody.
- Availability of adoption services following ethical and legal procedures.
- Protection of children from domestic violence and neglect.
- Community-based child care and family strengthening programs should be implemented.
8. Right to Identity
- Every child should receive birth registration immediately after birth.
- Legal identity ensures access to essential services like education, healthcare, and social welfare programs.
- Protection of the child’s name, nationality, and cultural identity, especially for indigenous and tribal communities.
- Governments must prevent statelessness by ensuring nationality rights to children born on their soil.
9. Special Rights for Children with Disabilities
- Ensure accessibility in public spaces, schools, transportation, and communication technologies.
- Provision of inclusive education programs and special education facilities when needed.
- Availability of assistive devices and rehabilitation services.
- Protection against stigma, neglect, and abuse in institutions or care homes.
- Promotion of their independence, dignity, and full participation in society.
d) Under five clinic
Definition
An Under-Five Clinic is a comprehensive child health service unit that provides preventive, promotive, curative, and educational services to children from birth up to five years of age. It plays a vital role in reducing child morbidity and mortality and promoting optimal growth and development.
Objectives of Under-Five Clinic
- To reduce infant and under-five mortality through timely immunization, early diagnosis, and treatment.
- To monitor and promote growth and development using growth charts and health check-ups.
- To detect and manage malnutrition and common childhood illnesses like ARI, diarrhea, anemia, etc.
- To educate and empower mothers and caregivers about child care, hygiene, nutrition, and family planning.
- To provide immunization services according to the National Immunization Schedule.
- To offer referral services for children with complications or developmental delays.
Components / Services of Under-Five Clinic
✅ Growth Monitoring
Growth monitoring involves regularly measuring and recording the child’s weight and height, plotting them on standardized growth charts to assess physical development and detect signs of malnutrition or abnormal growth patterns early.
✅ Nutritional Surveillance
Nutritional surveillance includes periodic assessment of the child’s dietary intake, anthropometric measurements, and clinical signs to identify nutritional deficiencies such as protein-energy malnutrition, anemia, and vitamin A deficiency, followed by appropriate dietary counseling and supplementation.
✅ Immunization
Immunization services are provided according to the National Immunization Schedule, ensuring timely administration of vaccines like BCG, OPV, DPT, Hepatitis B, Pentavalent, Measles-Rubella, and others to protect children against preventable infectious diseases.
✅ Treatment of Minor Ailments
The clinic offers early diagnosis and treatment of common childhood illnesses such as diarrhea, acute respiratory infections, fever, skin diseases, and worm infestations, using standardized protocols including ORS, zinc tablets, and deworming medications.
✅ Vitamin A Supplementation and Deworming
Children aged 9 months to 5 years receive periodic Vitamin A syrup every six months to prevent xerophthalmia and improve immunity, along with deworming tablets every six months to control intestinal worm infestations.
✅ Health Education and Counseling
Mothers and caregivers are educated on topics like exclusive breastfeeding, timely complementary feeding, personal hygiene, sanitation, prevention of communicable diseases, recognition of danger signs, and the importance of full immunization and regular health checkups.
✅ Referral Services
Children showing signs of severe illness, developmental delay, congenital defects, or failure to thrive are promptly referred to higher-level healthcare facilities for specialized evaluation and management to ensure timely intervention and care.
Role of the Nurse in Under-Five Clinic
✅ Growth Monitoring and Charting
The nurse is responsible for regularly weighing and measuring the height of under-five children, plotting these on WHO growth charts, and identifying any deviations such as underweight, stunting, or wasting.
✅ Immunization Services
The nurse administers vaccines as per the National Immunization Schedule, ensures correct technique, observes for adverse reactions, maintains cold chain, and keeps accurate immunization records.
✅ Nutritional Assessment and Counseling
The nurse assesses dietary history, identifies signs of nutritional deficiencies like anemia or protein-energy malnutrition, and provides counseling to mothers on breastfeeding, complementary feeding, and balanced nutrition.
✅ Management of Minor Illnesses
Nurses assess and treat minor ailments such as diarrhea, respiratory infections, and skin conditions using standing orders, and dispense appropriate medications like ORS, zinc, and deworming tablets.
✅ Vitamin A and Deworming Administration
The nurse ensures the timely administration of Vitamin A syrup and deworming tablets to children according to government guidelines.
✅ Health Education to Mothers and Caregivers
The nurse plays a crucial role in educating mothers about child care practices, hygiene, sanitation, home remedies, feeding techniques, immunization importance, and recognizing danger signs.
✅ Screening for Developmental Delays
Nurses observe for developmental milestones and assess early signs of delays or disabilities, making appropriate referrals for further evaluation and intervention.
✅ Record Keeping and Reporting
The nurse maintains individual child health cards, registers all services provided, compiles data, and submits reports to health authorities for program evaluation.
✅ Referral Services
Children requiring further medical attention due to complications, growth failure, or congenital issues are referred by the nurse to Primary Health Centres (PHCs) or hospitals for advanced care.
✅ Follow-Up and Home Visits
Nurses follow up on children who miss clinic visits, especially those with growth faltering or immunization default, often conducting home visits to ensure continuity of care.
e) Organization structure of PICU
The PICU is a highly specialized unit within a hospital that provides intensive, continuous care to critically ill or injured children, usually from birth up to 18 years. The unit is designed with a hierarchical and multidisciplinary structure to deliver safe, evidence-based, and timely care. Its organization ensures multidisciplinary coordination, 24×7 monitoring, and life-saving interventions.
1. Medical Team
PICU In-Charge/Head (Pediatric Intensivist) :
- Leads the entire PICU team and oversees all clinical and administrative operations.
- Responsible for policy formation, protocol development, and quality assurance.
- Conducts training and capacity-building programs for staff.
- Handles critical decision-making during emergencies.
Consultant Pediatricians :
- Provide expert guidance in complex and life-threatening pediatric conditions.
- Collaborate with intensivists for specialized interventions (e.g., ECMO, advanced ventilation strategies).
- Review and update treatment protocols based on the latest evidence.
Residents/Junior Doctors :
- Provide continuous patient monitoring and implement treatment plans under supervision.
- Responsible for daily patient rounds and documentation.
- Participate in emergency procedures like intubation and central line insertion under supervision.
- Update family members regularly regarding patient progress.
2. Nursing Team
Nursing Superintendent/Head Nurse :
- Responsible for ensuring adequate nurse-to-patient ratios (as per acuity of illness).
- Monitors compliance with infection control and critical care nursing standards.
- Organizes in-service education programs and skill development workshops.
- Participates in policy formulation for nursing care standards.
Staff Nurses (Critical Care Trained) :
- Provide 24/7 bedside care, including administration of high-risk medications and titration of IV infusions.
- Operate advanced life-support equipment such as ventilators, infusion pumps, and monitors.
- Monitor and manage invasive lines (arterial lines, central lines, chest drains).
- Maintain accurate documentation and participate in multidisciplinary rounds.
Nursing Assistants :
- Help in the maintenance of hygiene, positioning of patients, and pressure sore prevention.
- Assist with feeding (as per medical orders) and support in emergency code situations.
- Manage linen, supplies, and ensure the availability of necessary bedside articles.
3. Supportive Clinical Services
Respiratory Therapists :
- Manage advanced ventilation modes (CPAP, BiPAP, HFNC, invasive ventilation).
- Perform and assist in airway suctioning, nebulization therapy, and chest physiotherapy.
- Assist during intubation and extubation procedures.
Nutritionist/Dietitian :
- Formulate customized nutrition plans, including parenteral and enteral nutrition.
- Monitor caloric intake and address nutritional deficiencies promptly.
- Educate families about nutritional needs post-discharge.
Physiotherapists :
- Plan and provide pulmonary rehabilitation to prevent atelectasis and improve oxygenation.
- Assist with early mobilization protocols to prevent muscle wasting.
- Conduct passive and active range-of-motion exercises for immobilized patients.
Pharmacist :
- Prepare and dispense critical medications with accurate dosing calculations.
- Ensure availability of emergency drugs and monitor their expiration dates.
- Participate in drug safety audits and rational drug use policies.
Laboratory and Radiology Technicians :
- Provide urgent diagnostic reports (CBC, ABG, cultures, X-rays, USG, CT scans).
- Assist with point-of-care testing and ensure accurate reporting of critical results.
4. Administrative and Support Staff
Administrative Officer :
- Manages inventory, staff duty rosters, and coordination of interdepartmental referrals.
- Supervises billing, insurance claims, and consent documentation.
- Ensures that legal and ethical guidelines are strictly followed.
Biomedical Engineer :
- Responsible for the maintenance and calibration of all life-saving equipment.
- Conducts regular safety checks and provides immediate troubleshooting during equipment failure.
Housekeeping and Sanitation Staff :
- Perform terminal cleaning of isolation rooms and critical areas following hospital protocols.
- Ensure adherence to waste segregation guidelines and biomedical waste management.
Security Personnel :
- Control visitor access, especially during infection control restrictions.
- Provide emergency evacuation assistance if required.
- Monitor and enforce compliance with PICU visitor policies.
5. Multidisciplinary Team Approach
Psychologist/Counselor :
- Provide psychological counseling to parents coping with critical illness of their child.
- Conduct play therapy and emotional support sessions for recovering children.
Social Worker :
- Assist in arranging financial support through government schemes or NGOs.
- Facilitate counseling related to discharge planning and follow-up care.
Palliative Care Team :
- Support the family during end-of-life care decisions.
- Ensure comfort and dignity for terminally ill children through symptom management.
Q-3. Short answer Question: (Any Four) 2X4=8
A) Define neonatal mortality rate.
Neonatal Mortality Rate (NMR) is defined as the number of deaths of live-born infants during the first 28 days of life per 1,000 live births in a given year.
NMR=(Number of neonatal deaths (0–28 days))×1000/Total live births
b) List the National programs related to child health.
- Reproductive, Maternal, Newborn, Child and Adolescent Health (RMNCH+A) Programme
- Universal Immunization Programme (UIP)
- Rashtriya Bal Swasthya Karyakram (RBSK)
- Integrated Child Development Services (ICDS)
- Mid-Day Meal Scheme (MDMS)
- POSHAN Abhiyaan (National Nutrition Mission)
- Janani Shishu Suraksha Karyakram (JSSK)
- National Deworming Day (NDD)
- Intensified Diarrhea Control Fortnight (IDCF)
- School Health Programme under Ayushman Bharat
c) List any four principles of growth & development
- Growth and development are continuous processes – They occur from conception to death without interruption.
- Development proceeds in a cephalocaudal direction – Development starts from the head and moves toward the feet (head control before walking).
- Development proceeds in a proximodistal direction – It starts from the center of the body and progresses outward (trunk control before hand movement).
- Development is sequential and orderly – Children follow a predictable pattern (e.g., sitting → crawling → standing → walking).
d) List the four types of restraints
Physical Restraints – Devices that restrict body movement (e.g., belts, vests, limb ties).
Chemical Restraints – Medications used to control behavior or restrict movement (e.g., sedatives, antipsychotics).
Environmental Restraints – Modifications to the environment that limit movement (e.g., locked rooms, side rails on beds).
Mechanical Restraints – Equipment or devices attached to a person to restrict movement (e.g., wheelchair brakes, mitts).
e) Mention four clinical manifestations of respiratory distress syndrome.
Tachypnea – Rapid breathing, typically >60 breaths per minute in newborns.
Grunting – A low, short sound made during expiration to keep alveoli open.
Nasal Flaring – Widening of the nostrils to improve air intake.
Chest Retractions – Visible sinking of the chest wall during inhalation, especially around the ribs and sternum.