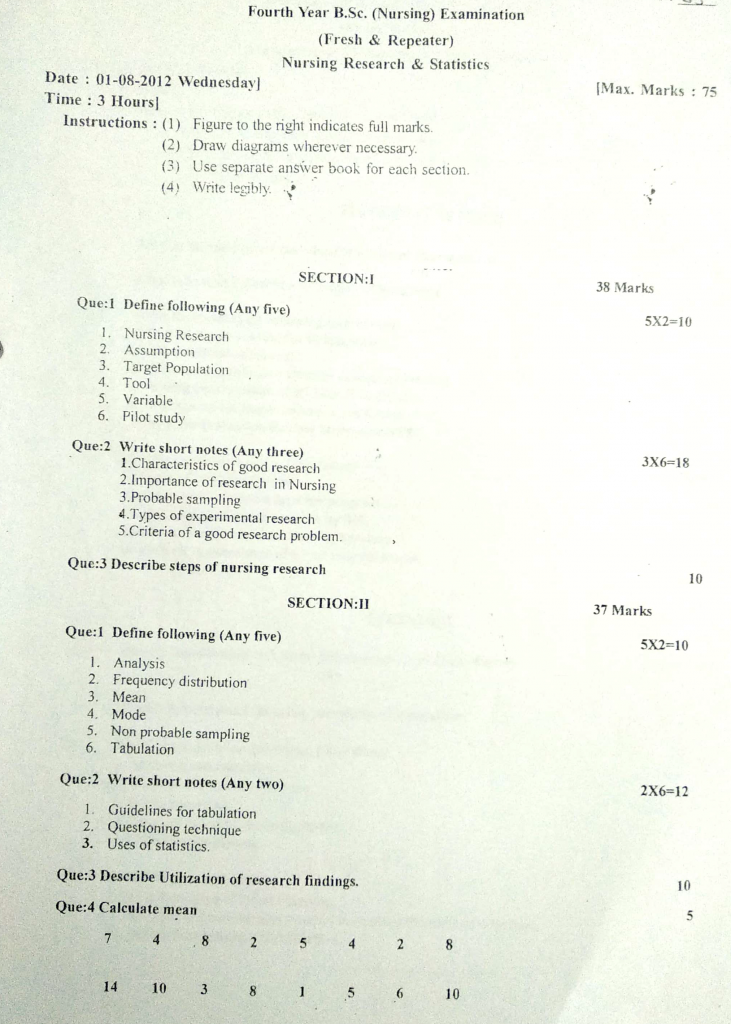
01/08/2012-B.SC-NURSING REAERCH-PAPER DONE-UPLOAD NO.5
01/08/2012-B.SC-NURSING REAERCH-PAPER DONE-UPLOAD NO.5
SECTION:1
Que.1 Define following (Any five) 5X2-10
1. Nursing Research
Nursing research is a systematic and scientific process that involves the study, investigation, and analysis of problems related to nursing practice, education, and administration in order to improve patient care outcomes and advance nursing knowledge. It is used to develop and evaluate nursing theories, practices, interventions, and healthcare policies for evidence-based nursing care. It is a foundation for evidence-based practice and helps nurses make informed decisions to enhance quality of care, safety, and effectiveness in various healthcare settings.
2. Assumption
Assumption is a basic belief, idea, or statement that is accepted as true without proof or verification, and is used as a foundation for reasoning, research, or decision-making. It is considered to be self-evident or universally accepted and provides a starting point for developing a research study, hypothesis, or theory. In nursing research, assumptions help guide the design, methodology, and interpretation of results by establishing expected truths about concepts or relationships.
Example : An assumption in a study might be that patients will answer questionnaires honestly.
3. Target Population
Target population refers to the entire group of individuals or elements that the researcher intends to study or draw conclusions about in a research project. It is the group that shares specific characteristics and meets the criteria relevant to the research problem, objectives, and hypothesis. It is from this population that the sample is selected, and the findings of the study are intended to be generalized back to this larger group.
Example : In a study on the effects of a new diet on diabetes, the target population might be all adults aged 30–60 with type 2 diabetes.
4. Tool
Tool is a structured instrument or device used by researchers to collect data accurately and systematically from research participants, based on the objectives of the study. It is essential for measuring different aspects such as knowledge, attitudes, practices, behaviors, or physiological parameters relevant to the research problem. It is designed to ensure the data collected is valid, reliable, and relevant for the research objectives.
5. Variable
Variable is any characteristic, attribute, or factor that can be measured, controlled, or changed in a research study and that has the potential to influence or be influenced by other factors. It is something that varies from person to person, situation to situation, or over time and is used to examine relationships, effects, or patterns in research.
6. Pilot study
Pilot study is a small-scale, preliminary version of the main research study that is conducted to test the feasibility, reliability, and validity of the research design, tools, and procedures. It is used to identify potential problems, weaknesses, or errors in the actual study plan before conducting the full-scale research.
Example : If a researcher plans to study the effect of a new teaching method on nursing students’ performance, a pilot study may be done on 10 students before involving the entire class.
Que: 2 Write short notes (Any three) 3X6=18
1. Characteristics of good research
Good research is a scientific, systematic, ethical, and purposeful inquiry that aims to generate new knowledge, validate existing facts, or solve identified problems through a planned and objective process.
It must possess certain essential characteristics to ensure that the findings are valid, reliable, applicable, and beneficial to clinical practice, education, administration, or health policy.
✅ 1. Systematic
- A good research study follows a step-by-step process, including identification of a problem, review of literature, setting objectives, choosing design, collecting data, analyzing it, and drawing conclusions.
- The researcher should not skip or rearrange the steps arbitrarily, as each stage depends on the successful completion of the previous one.
- A systematic study ensures that the research process remains orderly, disciplined, and replicable, avoiding confusion or misdirection at any point.
- It also ensures that every action taken is traceable, promoting accountability and documentation.
✅ 2. Logical and Rational
- Every aspect of good research must be justifiable and rooted in reasoning, whether it’s the selection of methodology, sample, or tool.
- The logical flow ensures that conclusions are derived from facts and not from assumptions or emotions.
- Logic must guide the connection between the research question, hypothesis, design, data interpretation, and the final result.
- Research without logic may produce random or misleading outcomes, which hold no scientific or practical value.
✅ 3. Empirical
- Good research is always based on actual observation, experimentation, or experience, not just theory or opinions.
- It involves collecting data directly from the field or target population, whether through surveys, clinical trials, or experiments.
- It allows for testing real-life phenomena, which enhances the usefulness and relevance of the findings.
- Empirical studies provide proof of what works or doesn’t work, particularly important in nursing care.
✅ 4. Replicable (Reproducibility)
- A hallmark of good research is that it can be repeated by other researchers under similar conditions, and the results would still be consistent.
- Replicability ensures reliability of the findings and increases confidence in their application.
- It helps validate findings over time or in different settings (like various hospitals or patient groups).
- If a study is not reproducible, it loses its scientific credibility and practical value.
✅ 5. Measurable and Verifiable
- Good research focuses on variables that are clearly defined, quantifiable, and objectively assessed, using reliable tools.
- All conclusions drawn from the study should be verifiable by others, meaning the data and results can be checked and confirmed.
- Measurability ensures that conclusions are data-driven and not subjective.
- It also allows for comparison with other studies, strengthening the evidence base.
✅ 6. Ethical
- A good research study must follow ethical standards, including informed consent, confidentiality, voluntary participation, and right to withdraw at any time.
- The study must be approved by an ethics committee or institutional review board (IRB) before starting data collection.
- It must not cause harm or distress to any participant, whether physical, emotional, or psychological.
- Researchers must avoid fabrication of data, plagiarism, or misuse of findings.
✅ 7. Objective and Unbiased
- Good research must remain free from personal opinion, emotional judgment, or researcher preferences, and should rely purely on observed evidence.
- The researcher must use neutral language, fair sampling, and balanced data collection to avoid influencing results.
- Objectivity ensures integrity, fairness, and transparency in the study.
- Results must be interpreted as they are, not as the researcher wishes them to be.
✅ 8. Relevant and Significant
- A good research topic must be important to society, patients, health professionals, or policymakers, and not chosen randomly or just for academic formality.
- It should address current healthcare problems, patient needs, or nursing practice gaps.
- It must result in useful applications, such as improved protocols, better patient education, or policy change.
- A relevant study increases its likelihood of being funded, published, and applied in the field.
✅ 9. Generalizable
- Good research is designed in a way that the findings can be applied to a broader population, not just the study sample.
- The sampling method, study setting, and tools must be such that results reflect true conditions in other similar environments.
- Generalizability increases the impact and usefulness of the study in community or national-level healthcare decisions.
- It ensures the study’s findings are not limited to a single hospital, ward, or group.
✅ 10. Feasible
- A good research study is realistic to conduct within available resources, time, tools, and manpower.
- It should not require unattainable technology, rare participants, or excessive funding, especially in student or field-based research.
- Feasibility ensures that the study does not get abandoned midway due to resource limitations.
- Proper planning in feasibility ensures smooth execution and timely completion.
✅ 11. Clearly Defined Objectives
- A good research study starts with specific, measurable, and clearly written objectives, which guide every stage of the process.
- Objectives must relate directly to the research problem and state what the researcher wants to explore, test, or prove.
- These objectives serve as a blueprint for choosing tools, designs, and analysis methods.
- Vague or broad objectives can make the study unclear or difficult to evaluate.
✅ 12. Innovative and Original
- A good research project should attempt to add something new to existing knowledge, either through new methods, new applications, or fresh perspectives.
- It may also challenge old beliefs, test modern technologies, or introduce creative interventions.
- Innovation encourages academic interest and problem-solving, especially when nursing practices are evolving.
- Original work increases the scientific value and publication chances of the research.
✅ 13. Accurate and Precise
- Accuracy in research means that the data truly reflects the real-world situation, not errors or assumptions.
- Precision ensures that measurements are consistent and repeatable, reducing variation or random error.
- A good researcher checks for data entry errors, validates tools, and maintains detailed records.
- Precise results lead to better confidence in the study’s conclusions and greater respect from the research community.
2. Importance of research in Nursing
- Nursing research refers to a scientific and systematic process aimed at generating new knowledge or validating existing knowledge to improve nursing practice, patient care, education, administration, and health policy.
- It plays a central role in transforming nursing into a professional discipline, moving it from a task-oriented vocation to a knowledge-driven science.
- The importance of research in nursing spans across clinical, community, academic, administrative, and public health domains, making it an integral component of every level of nursing practice.
1. Promotes Evidence-Based Practice (EBP)
- Nursing research is vital for integrating current best evidence into clinical decision-making, enabling nurses to deliver care that is proven to be safe, effective, and up to date.
- It helps in replacing traditional practices that may be outdated or ineffective with scientifically validated procedures.
- Evidence-based practice results in improved patient safety, reduced clinical errors, and better therapeutic outcomes.
- It supports the use of clinical practice guidelines, pathways, and standard protocols that are grounded in research findings.
2. Improves Quality of Patient Care
- Research provides nurses with the tools to assess patient needs accurately, plan and implement interventions that are proven to be beneficial, and evaluate patient outcomes effectively.
- It leads to early detection of risks, better disease management, and personalized care plans, particularly in chronic diseases, maternal health, and geriatric care.
- It supports the development of preventive strategies and health promotion interventions that reduce hospital readmission and morbidity.
- Research contributes to improved communication, documentation, and coordination, which are vital for quality care.
3. Develops Professional Knowledge and Theory
- Nursing research fosters the continuous expansion of the nursing body of knowledge, through the development, refinement, and testing of nursing theories, models, and concepts.
- It validates nursing interventions, techniques, and clinical practices, providing a scientific base for decision-making.
- It transforms experiential knowledge into generalized, evidence-based knowledge that can be taught and shared widely.
- Research advances the disciplinary identity of nursing, helping it gain autonomy and recognition within the health profession.
4. Enhances Critical Thinking and Decision-Making Skills
- Through research, nurses learn to ask clinical questions, seek out evidence, evaluate its validity, and apply findings logically.
- It improves the nurse’s ability to analyze complex clinical situations, interpret patient data, and make rational clinical decisions.
- It helps in identifying the cause of nursing problems, predicting outcomes, and evaluating the impact of nursing care.
- Critical thinking encouraged by research is essential in emergency care, intensive care, and community health settings, where fast and informed decisions are crucial.
5. Strengthens Nursing Education
- Research contributes to curriculum development and revision, ensuring that students are taught the most current and evidence-based content.
- It promotes the inclusion of problem-based learning, research methodology, data analysis, and literature review skills in nursing education.
- Research encourages student involvement in project work, group discussions, and thesis writing, preparing them to be knowledge creators rather than passive learners.
- Nursing educators use research to evaluate teaching methods, improve classroom engagement, and identify learning gaps.
6. Improves Nursing Administration and Leadership
- Research helps nurse administrators make evidence-based decisions regarding staffing, budgeting, resource management, and scheduling.
- It supports the development of quality improvement projects, performance evaluation systems, and patient satisfaction surveys.
- Nurse managers use research to develop policy documents, procedure manuals, infection control guidelines, and nursing audits.
- It leads to improved workflow efficiency, cost-effectiveness, and safety standards within hospitals and healthcare institutions.
7. Guides Public Health and Policy Development
- Nursing research plays a significant role in shaping healthcare programs and influencing health policy decisions at the local, state, and national levels.
- It provides data on disease trends, vaccination coverage, maternal-child health indicators, and community health needs.
- It supports the creation of targeted interventions for marginalized or vulnerable populations, such as tribal groups, slum dwellers, or HIV-positive patients.
- Government agencies and health NGOs rely on nursing research to design, implement, and evaluate public health programs and campaigns.
8. Encourages Innovation and Technology in Practice
- Research encourages nurses to design, test, and implement new tools, protocols, and technologies for improving patient care.
- It leads to the creation of digital record-keeping systems, telemedicine tools, e-learning modules, and mobile health apps.
- Innovation through research reduces manual workload, increases patient monitoring, and supports automation of routine nursing tasks.
- Nurses involved in research can patent clinical devices, such as ergonomic aids or customized wound dressings, enhancing care and safety.
9. Promotes Professional Recognition and Career Advancement
- Nurses who engage in research often get opportunities to publish papers, present at conferences, and participate in collaborative projects, gaining visibility and credibility in the profession.
- It opens the door for scholarships, fellowships, leadership positions, and international research exchange programs.
- Nurses with research credentials are preferred for higher academic roles (lecturer, professor, dean) or clinical leadership positions (CNO, QI specialist).
- It also builds personal confidence, critical awareness, and a sense of contribution to the nursing profession.
10. Ensures Ethical Practice and Accountability
- Research instills in nurses the importance of ethics in patient care, including principles such as informed consent, privacy, confidentiality, and autonomy.
- It ensures that nursing interventions are justifiable, non-harmful, and respectful of patient rights and dignity.
- It promotes standardization of procedures and auditing systems, allowing the profession to monitor care quality and correct errors.
- Research provides transparency, allowing both internal and external stakeholders to evaluate nursing services.
3. Probable sampling
Definition
- Probability sampling is a scientific method of selecting a sample from a larger population using a random technique, where every unit or element in the population has a known, non-zero, and usually equal chance of being selected, which ensures fairness, objectivity, and representativeness in the sample.
- This method is based on the principle of randomization, which allows researchers to draw unbiased conclusions from the sample and to apply statistical inference methods such as estimating population parameters, calculating sampling errors, and testing hypotheses.
- In nursing research, probability sampling is used to collect data from representative groups of patients, nurses, communities, or health workers, so the findings can be applied confidently to a larger group or setting.
Core Characteristics of Probability Sampling
- Each member of the population has a known and equal probability of selection, ensuring no discrimination or favoritism in sample inclusion.
- The process uses random selection techniques, either manually (lottery) or through software (random number generators).
- It provides high-quality data that is statistically valid and generalizable to the entire population.
- It minimizes the risk of researcher bias, increases objectivity, and improves the credibility of the study.
- It is used mostly in quantitative research, where numeric, measurable variables are studied.
TYPES OF PROBABILITY SAMPLING
1️⃣ Simple Random Sampling
- In simple random sampling, the researcher ensures that every member of the target population has an equal and independent chance of being selected, using random number tables, computerized generators, or lottery methods, which leads to an unbiased and representative sample.
- This method is simple and easy to understand, but it requires that the entire population list (sampling frame) be available and accessible, which may not always be possible in real-world settings.
- For example, a nursing researcher who has a list of 1000 registered nurses working in a state hospital may use a computer to randomly select 200 nurses for a study on burnout and job satisfaction.
2️⃣ Stratified Random Sampling
- In stratified random sampling, the population is first divided into homogeneous subgroups or strata based on certain shared characteristics such as age, gender, qualification, or work setting, and then a simple random sample is drawn separately from each stratum to ensure proportionate and inclusive representation.
- This method helps to improve precision and comparability, especially when the researcher is interested in analyzing differences between groups, or when certain subgroups are small and may be missed in a purely random sample.
- For instance, in a study on continuing education needs of nurses, the population could be divided into strata like diploma holders, B.Sc. nurses, and postgraduates, and then an equal number of participants from each group are selected randomly.
3️⃣ Systematic Random Sampling
- In systematic sampling, the researcher first selects a starting point at random, and then selects every kth element from a regularly ordered list of the population, where k = population size ÷ desired sample size, ensuring a uniform and evenly spaced selection process.
- This method is faster and more convenient than simple random sampling and is ideal for large populations with proper records, such as patient discharge lists or hospital staff registers.
- For example, if a researcher wants to select 100 patients from a population of 1000, they may choose a random number between 1 and 10 (say 7), and then select every 10th patient starting from number 7 (7, 17, 27, etc.).
- However, if the population list has a cyclical pattern or is not truly random, this method can introduce systematic bias.
4️⃣ Cluster Sampling
- In cluster sampling, the entire population is divided into geographical or naturally occurring groups called clusters, such as villages, hospital wards, classrooms, or health centers, and then some clusters are selected at random, either to include all members within them or to sample within those clusters.
- This method is particularly useful when the population is large, widespread, and listing every individual is difficult or expensive, such as in rural or community-based health studies.
- For example, to study the nutrition status of under-five children, the researcher may randomly select 5 villages from a district and then assess all children aged 0–5 years within those villages.
- The limitation is that members within clusters may be similar, reducing diversity and increasing sampling error, which must be adjusted statistically.
5️⃣ Multistage Sampling
- Multistage sampling is a complex combination of probability methods, where sampling is done in two or more stages, often starting with cluster sampling, followed by simple or stratified sampling within the selected clusters.
- This approach is ideal for large-scale national or regional studies, where sampling is required at different administrative levels such as state → district → block → village → household.
- For example, in a national health survey, the researcher may first randomly select states, then districts within states, then primary health centers within districts, and finally select individuals within each PHC using simple random sampling.
- This method increases practical feasibility and flexibility, but requires rigorous planning and multiple levels of randomization.
Advantages of Probability Sampling
- It ensures a scientific, unbiased, and transparent method of selecting samples, which improves the credibility of nursing research.
- The findings obtained are statistically generalizable to the entire population, which is essential for policy-making and clinical practice guidelines.
- It allows the use of inferential statistics, such as confidence intervals, t-tests, chi-square tests, and regression models.
- It reduces sampling error and increases accuracy and objectivity, especially in large-scale studies.
- It supports the evidence-based approach in nursing, ensuring interventions are based on high-quality data.
Limitations of Probability Sampling
- It requires a complete, up-to-date population list (sampling frame), which may be difficult to obtain in many nursing or public health settings.
- It is often time-consuming, logistically complex, and costly, particularly in large or dispersed populations.
- In certain cases like emergencies, special populations, or qualitative research, it may not be practical or ethical to use randomization.
- Multistage or stratified methods require advanced statistical knowledge and planning, making them less suitable for beginner researchers.
- If randomization procedures are not properly followed, the entire study may suffer from selection bias or validity threats.
4. Types of experimental research
Experimental research is a scientific method in which the researcher manipulates one or more independent variables and measures their effect on the dependent variable, while controlling other factors, to establish a cause-effect relationship.
In nursing and health sciences, experimental research is often used to test interventions, treatments, or nursing procedures under controlled conditions.
Main Types of Experimental Research
Experimental research can be broadly classified into three major types :
1️⃣ True Experimental Research
- A true experimental research design is the most scientifically valid and robust form of experimental study in which the researcher randomly assigns subjects to either the control group or the experimental group, thereby ensuring that every participant has an equal chance of being included in any group, which reduces selection bias and strengthens the internal validity of the study.
- In this type of design, the researcher actively manipulates the independent variable (the intervention or treatment), and compares the outcomes with those of a control group, which does not receive the intervention, allowing the researcher to clearly observe the cause-effect relationship between the variables.
- True experimental research involves three essential features: randomization, manipulation, and control, making it ideal for clinical trials and nursing intervention studies, such as testing the effect of a new wound care technique on healing rate in two randomly selected patient groups.
2️⃣ Quasi-Experimental Research
- A quasi-experimental research design is a type of experimental study where the researcher still manipulates the independent variable, but does not randomly assign participants to control and experimental groups, often due to practical, ethical, or institutional constraints.
- In this design, the groups may be pre-existing or naturally occurring, such as comparing outcomes of patients in two different hospital wards, which means there is less control over confounding variables, and as a result, the ability to firmly establish cause-effect relationships is slightly reduced compared to true experiments.
- Quasi-experimental designs are especially useful in real-world healthcare settings, where randomization is not feasible, and are often used in nursing education, hospital service evaluations, or behavior change studies, such as evaluating the impact of a hand hygiene campaign on infection rates without random group assignment.
3️⃣ Pre-Experimental Research
- A pre-experimental research design is the simplest and least rigorous form of experimental study, where the researcher may manipulate the independent variable but does so without any random assignment or control group, making it difficult to eliminate alternative explanations for the observed outcomes.
- This type of research is commonly used in pilot studies, exploratory investigations, or when resources and time are limited, and it is more about gaining initial insight or testing the feasibility of an intervention rather than making strong conclusions.
- Pre-experimental studies often follow basic formats like “one group pre-test and post-test” design, where outcomes are measured before and after the intervention in the same group, such as assessing the effect of a health education session on handwashing knowledge in a single group of nursing students.
5. Criteria of a good research problem.
A research problem is a specific issue, gap, or unanswered question in an area of study that the researcher intends to explore or solve through systematic investigation. A good research problem provides a clear foundation for the entire study and must be chosen with great care, logic, and practical consideration.
1️⃣ Clarity and Specificity
- A good research problem must be written in clear, simple, and unambiguous language, leaving no room for confusion or misinterpretation.
- The statement must define the population, setting, and variables clearly so that the direction of study is easy to follow.
- It should avoid technical jargon or overly broad ideas that could dilute the focus of the study.
- The research question derived from it must be precise and researchable.
2️⃣ Feasibility and Practicality
- The problem must be researchable within the available time frame, considering the academic deadlines, especially in student projects.
- It must match the available skills, qualifications, and experience of the researcher or research team.
- The tools, equipment, and materials needed must be accessible, and the logistics and location should not be difficult to manage.
- It should also account for budgetary constraints and ethical approval timelines.
3️⃣ Relevance and Significance
- A good research problem must be related to current nursing issues, patient care challenges, or healthcare system needs.
- It must have practical value, either by improving health outcomes, solving a clinical problem, or enhancing professional knowledge.
- It should ideally align with national health priorities, policies, or emerging health trends (e.g., digital health, maternal mortality).
- The topic must also benefit a specific group, such as vulnerable populations, children, or elderly patients.
4️⃣ Ethical Acceptability
- The problem must be designed with respect for human rights, dignity, autonomy, and welfare, ensuring voluntary participation.
- It should avoid any risk of harm, coercion, or psychological distress, especially when dealing with sensitive topics.
- Proper measures must be included for confidentiality, anonymity, and data protection of participants.
- It must receive approval from an Institutional Ethical Review Board (IRB) before data collection begins.
5️⃣ Researchability and Measurability
- The selected problem should allow for operational definition of variables, enabling accurate data collection and analysis.
- It should be possible to apply quantitative or qualitative methods to answer the research question.
- The variables should be measurable using valid tools such as rating scales, questionnaires, lab tests, or interviews.
- It should not involve abstract or philosophical topics that cannot be observed empirically.
6️⃣ Originality or Novelty
- A good research problem should fill a gap in the existing literature or extend a previous study in a new context.
- It may apply a known method to a new population or setting, offering new insights or validations.
- The topic must be fresh, interesting, and not overly repeated in past academic projects unless justified by new perspectives.
- It should encourage innovative thinking and creative problem-solving within nursing or healthcare.
7️⃣ Theoretical and Conceptual Linkage
- The problem should be linked to an existing nursing theory, health model, or framework that gives structure to the study.
- This helps in hypothesis formulation, tool construction, and interpretation of results based on established principles.
- It supports the integration of evidence-based concepts into practical nursing application.
- It also helps in defining conceptual boundaries and variable relationships clearly.
8️⃣ Clear Direction and Scope
- The research problem should be narrow enough to be manageable and focused, yet broad enough to generate comprehensive results.
- It should allow for the development of specific objectives and research questions.
- It must not be too vague or too detailed – a balance ensures a well-structured study.
- It should define the geographical, demographic, or thematic limits of the research.
9️⃣ Availability of Data and Sources
- The problem must allow access to primary or secondary data, such as patient records, surveys, or observation tools.
- The required sample population must be accessible, cooperative, and willing to participate.
- Data collection should be feasible within ethical and institutional rules, especially in hospital or educational settings.
- Tools for measurement must be validated, tested, and reliable for the chosen variables.
🔟 Interest and Motivation of Researcher
- The topic should match the academic or clinical interests of the researcher to keep them engaged throughout the study.
- Motivation improves consistency, dedication, and curiosity, resulting in higher-quality work.
- Personal involvement or passion can help in handling challenges, such as data errors or delayed approvals.
- A motivated researcher is also more likely to follow through with publication, presentation, or real-world application.
1️⃣1️⃣ Potential for Generalization
- The findings from the study should be applicable to similar groups or settings, not just to a specific sample.
- Generalizability adds scientific value and broader utility to the research.
- It increases the chances of findings being adopted by other hospitals, nursing institutions, or public health programs.
- The sample must be representative of the population, and methods must be standardized to achieve this.
1️⃣2️⃣ Support from Literature and Evidence
- A good research problem should be backed by existing theories, models, and empirical studies, proving that the topic is relevant and worth exploring.
- Literature review helps in identifying gaps, contradictions, or updates required in current practice.
- It aids in building a strong introduction, rationale, and background for the study.
- It ensures that the study does not duplicate already resolved questions, unless replication is intended.
Que:3 Describe steps of nursing research 10
Nursing research is a systematic, scientific, and evidence-based process used to identify health problems, improve patient care, develop nursing theory, and strengthen nursing practice. The steps of nursing research are carefully planned to ensure reliability, validity, and usefulness of results in improving healthcare outcomes.
1️⃣ Identification of Research Problem
- It is the first step where the researcher selects a topic or issue that needs scientific investigation.
- In which the topic should be relevant, researchable, feasible, and ethical.
- It may come from clinical experience, literature, or existing gaps in knowledge.
- It should be clearly stated in the form of a problem statement.
- Nursing Relevance : Helps identify critical patient care issues such as fall prevention, medication errors, or staff burnout.
2️⃣ Review of Literature
- It is the process of reviewing previous research studies, theories, and data related to the selected topic.
- In which it provides background knowledge, identifies gaps, and refines the research question.
- It includes both primary sources (original research) and secondary sources (reviews, textbooks).
- It prevents duplication and supports justification of the study.
- Nursing Relevance : Helps nurses build on existing clinical evidence for better patient care.
3️⃣ Formulation of Objectives and Hypotheses
- It is the step where the researcher defines what the study aims to achieve.
- In which objectives are written clearly and should be SMART (Specific, Measurable, Achievable, Relevant, Time-bound).
- Hypotheses are formulated in quantitative research to test relationships or differences.
- They may be null (no difference) or alternative (there is a difference).
- Nursing Relevance : Guides the nurse to stay focused and structure the research towards improving care delivery.
4️⃣ Selection of Research Design
- It is the overall plan that determines how data will be collected, analyzed, and interpreted.
- In which the researcher selects from types like descriptive, experimental, correlational, or qualitative depending on the problem.
- It ensures internal and external validity of the study.
- The design should match the research question and resources.
- Nursing Relevance : Helps ensure the study is scientifically accurate and applicable to nursing practice.
5️⃣ Sampling and Sampling Techniques
- It is the method used to select a portion of the population for participation.
- In which probability (random) or non-probability (convenient, purposive) methods are used.
- The sample should be representative and adequate in size for generalization.
- Factors like inclusion and exclusion criteria must be clearly defined.
- Nursing Relevance : Allows efficient data collection from patients or healthcare workers without needing the entire population.
6️⃣ Development of Research Tool
- It is the step of preparing valid and reliable instruments for data collection.
- In which tools may include questionnaires, rating scales, observation checklists, or interview guides.
- Tools must be pilot-tested to ensure clarity and accuracy.
- The language should be simple, and the tool should be culturally appropriate.
- Nursing Relevance : Ensures data is captured effectively about patient symptoms, satisfaction, or nursing competencies.
7️⃣ Data Collection
- It is the process of gathering information from the selected sample using the research tool.
- In which ethical practices like informed consent, confidentiality, and voluntary participation are followed.
- Data may be collected through observation, interviews, clinical tests, or document review.
- A proper schedule, training of data collectors, and record-keeping are important.
- Nursing Relevance : Helps nurses gather real patient data on clinical outcomes or care processes.
8️⃣ Data Analysis and Interpretation
- It is the process of converting raw data into meaningful information.
- In which statistical software and techniques (mean, chi-square, t-test, etc.) are used in quantitative research.
- In qualitative studies, thematic analysis is used to identify patterns.
- The analysis must align with the study objectives and hypothesis.
- Nursing Relevance: Helps determine the effectiveness of nursing interventions and make clinical decisions based on facts.
9️⃣ Presentation and Communication of Results
- It is the step where findings are documented and shared with others.
- In which results are presented through research reports, dissertations, articles, or presentations.
- It includes summary of findings, conclusions, recommendations, and implications.
- Charts, tables, and graphs are often used to present data clearly.
- Nursing Relevance: Enables the nursing community to use new knowledge for improving care practices and standards.
🔟 Application of Research Findings (Utilization)
- It is the final step where findings are applied to practice, policy, or education.
- In which nurses and healthcare leaders use evidence to develop care protocols, improve training, or influence policy.
- It bridges the gap between research and practice by implementing tested strategies.
- Ongoing evaluation helps assess the effectiveness of changes made.
- Nursing Relevance : Enhances patient safety, care quality, and overall efficiency in nursing services.
Section 2
Que:1 Define following (Any five) 5X2-10
1. Analysis
Analysis refers to the process of systematically examining, organizing, and interpreting collected data in order to derive meaningful conclusions and answer the research questions. It is a crucial step in research that involves breaking down data into manageable parts, applying statistical or logical techniques, and identifying patterns, relationships, and trends. It is essential for converting raw data into clear, understandable results, and helps in validating hypotheses, testing assumptions, and forming evidence-based nursing decisions.
2. Frequency distribution
Frequency distribution is a systematic arrangement of data that shows how often each value or group of values (called class intervals) occurs in a dataset. It is used to organize raw data into a clear and meaningful format, making it easier to understand patterns, trends, or variations in the data. It is helpful in both qualitative and quantitative nursing research to identify the number of occurrences of certain health conditions, symptoms, or behaviors.
Example :
In a study of pulse rates of 10 patients :
[72, 80, 72, 76, 84, 72, 80, 76, 88, 72]
The frequency distribution is :
72 bpm – 4 times
76 bpm – 2 times
80 bpm – 2 times
84 bpm – 1 time
88 bpm – 1 time
3. Mean
Mean is the arithmetic average of a set of numerical values, calculated by adding all the values together and dividing the sum by the total number of values. It is a widely used measure of central tendency that gives an idea of the overall level or typical value in the dataset. It is useful in identifying average outcomes, such as average pulse rate, blood pressure, or age in nursing and healthcare studies.
Mean = Sum of all values / Total number of values
4. Mode
Mode is the value or score that occurs most frequently in a given set of data. It is a measure of central tendency, which represents the most common or popular response in a dataset. It is especially useful for categorical or nominal data where values are counted, and it may be used when mean or median is not appropriate due to extreme values or open-ended categories.
Example :
In a survey of pain levels (on a scale of 0–10) reported by 10 patients:
[2, 4, 4, 5, 4, 6, 7, 2, 3, 4]
Here, the mode is 4, as it appears most frequently.
5. Non probable sampling
Non-probability sampling is a sampling technique in which not all individuals in the population have a known or equal chance of being selected for participation in the research study. It is used when it is not feasible to use random selection, and the sample is selected based on researcher’s judgment, convenience, or specific purpose. It is useful in qualitative research, exploratory studies, or when the target population is hard to access, but it may lead to sampling bias and the findings cannot be generalized to the whole population.
6. Tabulation
Tabulation is the systematic arrangement of collected data in rows and columns, which helps in organizing, summarizing, and presenting the data in a clear and concise manner. It is used to convert raw data into a format that is easy to read, interpret, and analyze, allowing the researcher to identify patterns, trends, and relationships. It is one of the most important steps in data processing, and can be done manually or by using computer software like Excel or SPSS.
Example : In a study on dietary habits of nursing students, a table may show how many students prefer vegetarian or non-vegetarian diets, arranged by age group and gender.
Que:2 Write short notes (Any two) 2X6-12
1. Guidelines for tabulation
Tabulation is the process of presenting collected data systematically in rows and columns, making it easier to read, compare, analyze, and interpret. In nursing and healthcare research, proper tabulation is essential to display numerical or categorical data clearly, logically, and accurately.
1. Provide a Clear, Concise, and Self-Explanatory Title
- It should reflect what the data is about, who the subjects are, and the period covered.
- Titles must avoid vague words like “Table showing…” and instead be specific.
- The title should indicate the main variable(s) in focus.
- If necessary, sub-titles may be used for complex data sets.
- Example : “Table 1: Gender-Wise Distribution of Hypertensive Patients in Urban Health Center, 2023”
2. Number the Tables Sequentially
- All tables must be numbered as Table 1, Table 2, etc., even in appendices.
- Sub-tables can be numbered as Table 2A, 2B if needed.
- Each table number must be referenced correctly in the research report text.
- It is advised to use the same numbering style (Arabic or Roman) throughout.
3. Mention the Source of Data
- The source must be stated immediately below the table, especially for secondary data.
- When data is collected by the researcher, write “Primary data collected by investigator.”
- If the data is adapted from another source, mention proper citation and year.
- Mention whether the data is from government records, hospital files, or surveys.
4. Use Proper and Specific Headings for Rows and Columns
- Headings should clearly describe the content without needing extra explanation.
- Always use singular form (e.g., “Age Group” not “Age Groups”) for clarity.
- If the values represent units, include them in brackets.
- Example : “Weight (kg)” or “BMI (kg/m²)”
- Use capital letters for main headings and bold text if required.
5. Arrange Data Logically and Systematically
- Order data either chronologically, categorically, alphabetically, or by size.
- Group similar variables together (e.g., all male data in one block).
- Present control and experimental group data side by side (if applicable).
- Maintain the same order across multiple related tables for consistency.
6. Ensure Consistency in Units and Decimal Places
- Use one consistent unit throughout (e.g., present all weight in kg, not a mix of pounds and kg).
- Round all values to the same decimal place, preferably 1 or 2 places.
- Avoid mixing percentages and actual numbers in one column unless explained.
- If converting units (e.g., cm to m), mention conversion used.
7. Avoid Overcrowding and Complex Presentation
- Don’t place more than 5–7 columns or 20–25 rows in a single table.
- If data is too large, split it into sub-tables or represent it using charts.
- Leave equal spacing between rows and columns.
- Use simple fonts (e.g., Arial, Times New Roman) and avoid excessive formatting.
8. Provide Footnotes and Explanations (If Required)
- Explain abbreviations, short forms, symbols, or special values.
- Footnotes should be short, clear, and written below the table using symbols like (), (*), (†), etc.
- If there is missing or incomplete data, state “NA = Not Available” or “ND = Not Disclosed.”
- Mention whether values are rounded or estimated.
9. Highlight Important Values Like Totals and Subtotals
- Total rows should be bolded or underlined to stand out.
- Subgroup totals may be shown using border lines or separate rows.
- Ensure all subtotals add up to the grand total for accuracy.
- Highlight mean, median, or highest/lowest values when important.
10. Indicate Sample Size (N) Clearly
- Always mention how many individuals the table is based on (N = …).
- If subgroups exist, mention subgroup sizes (e.g., Male N = 50, Female N = 60).
- This allows readers to understand proportions and percentages better.
- If there’s a loss to follow-up or incomplete response rate, mention it in the footnote.
11. Keep Tables Self-Explanatory
- Readers should be able to understand the table without referring to the main text.
- All headings, abbreviations, footnotes, and units must be included in the table itself.
- For complex data, add a brief caption or description below the table.
12. Maintain Uniform Format Across Tables
- Use consistent font, border style, text alignment, and spacing throughout the report.
- This improves professional appearance and readability.
- Use gridlines or borders neatly and sparingly.
13. Ensure Accuracy and Double-Check Calculations
- All totals, averages, percentages, and calculations must be verified.
- Even one mistake in a table can lead to faulty interpretation.
- Use software (Excel/SPSS) for auto-calculation and cross-checks.
14. Do Not Repeat the Same Data in Multiple Tables
- Avoid redundancy.
- If similar data is used in two places, present it in a different format (e.g., once as a table, once as a graph).
- Summarize only key data for discussion tables.
15. Use Grids or Lines to Separate Columns and Rows
- Grids help visual separation of data and prevent misreading.
- Use horizontal lines to separate headings and totals.
- Avoid using too many lines or colors which can distract the reader.
2. Questioning technique
Definition of Questioning Technique
- It is defined as the systematic method of formulating, sequencing, and presenting questions to participants for the purpose of collecting data.
- It is used in both qualitative and quantitative research—particularly in structured interviews, surveys, questionnaires, and focus group discussions.
- It is the backbone of primary data collection, especially when using tools such as interview guides, self-report questionnaires, or observational checklists.
Objectives / Purpose of Questioning Technique
- It is used to explore the knowledge, attitudes, behaviors, and experiences of individuals.
- It helps in extracting deeper insights into the problems under investigation.
- It supports accurate and ethical collection of data in various nursing research settings.
- It enhances participant engagement and creates a trusting communication environment.
- It is essential for verifying hypotheses or understanding lived experiences, especially in qualitative designs like phenomenology or grounded theory.
Types of Questions Used in Questioning Technique
✅ A. Open-Ended Questions
- It is designed to allow participants to express themselves freely and in detail.
- It begins with “What,” “How,” “Describe,” etc.
- Example : “What do you feel were the main challenges during your hospital stay?”
- It is used in qualitative research to explore complex thoughts, feelings, and behaviors.
- It provides rich, narrative data.
✅ B. Closed-Ended Questions
- It is used when limited, specific responses are required.
- The response options may be “Yes/No” or pre-coded choices.
- Example : “Do you practice hand hygiene after every patient contact?”
- It is helpful in surveys and quantitative analysis because it is easier to code and analyze.
✅ C. Probing Questions
- It is used after a response to encourage more detailed answers.
- Example: “Can you tell me more about how that made you feel?”
- It is crucial in in-depth interviews, helping researchers dig deeper into participant responses.
✅ D. Leading Questions (To be Avoided)
- It is phrased in a way that influences or guides the participant’s answer.
- Example: “Don’t you think the nurse was very caring?”
- It should be avoided to reduce bias and maintain the integrity of the data.
✅ E. Multiple Choice Questions :
- It is used to provide multiple response options, usually in a structured questionnaire.
- Example : “What is your primary source of health education?
- A) TV
- B) Newspaper
- C) Nurse
- D) Internet”
✅ F. Likert Scale Questions
- It is used to measure attitudes or perceptions on a scale of agreement or satisfaction.
- Example : “Rate your satisfaction with nursing care :
- Very Dissatisfied
- Dissatisfied
- Neutral
- Satisfied
- Very Satisfied”
Guidelines and Principles for Effective Questioning Technique
✅ 1. Clarity and Simplicity
- It is essential that questions are clearly worded to avoid confusion.
- Avoid technical jargon unless it is well understood by the participant.
✅ 2. Relevance to Objectives
- It is necessary that every question serves the purpose of the research aim or hypothesis.
- Irrelevant questions may confuse the respondent and waste time.
✅ 3. Logical Sequence of Questions
- It is ideal to arrange questions from general to specific, and from less sensitive to more personal.
- It helps build rapport and comfort before diving into deeper issues.
✅ 4. Avoiding Double-Barreled Questions
- It is recommended to ask only one question at a time.
- Incorrect : “Do you think nurses are helpful and respectful?”
- Correct : “Do you think nurses are helpful?” followed by “Do you think nurses are respectful?”
✅ 5. Balanced and Neutral Tone
- It is necessary to avoid emotionally charged or judgmental language.
- Keep questions objective, unbiased, and respectful.
✅ 6. Culturally Sensitive Language
- It is important to tailor questions to suit the participant’s cultural background and literacy level.
- Use appropriate translations if needed.
✅ 7. Ethical Framing of Sensitive Questions
- It is necessary to provide assurance of confidentiality and allow participants to skip questions if uncomfortable.
- Questions involving topics like abuse, illness, or sexuality must be framed with sensitivity.
Advantages of Using Proper Questioning Techniques
- It increases the accuracy and richness of collected data.
- It enhances participant trust and cooperation.
- It ensures data is aligned with research objectives.
- It supports valid, reliable, and reproducible results.
- It improves data collection efficiency in fieldwork or clinical settings.
Nursing Implications / Applications of Questioning Technique in Nursing Practice and Research
✅ 1. Use in Patient History Taking and Clinical Assesment
- It is used by nurses during admission, triage, or assessment to gather subjective data such as pain level, past illnesses, allergies, current complaints, and medication history.
- It enhances accuracy in nursing diagnosis, as detailed questioning helps uncover risk factors or hidden symptoms.
- It is essential in emergency care settings, where precise questioning can lead to life-saving interventions.
✅ 2. Application in Therapeutic Communication (Mental Health Nursing)
- It is central to building therapeutic rapport with psychiatric patients by encouraging expression of emotions and thoughts.
- It is used during mental status examination (MSE) to assess orientation, thought process, hallucinations, or suicidal ideation.
- It helps the nurse to identify early warning signs of emotional distress or crisis.
✅ 3. Use in Pediatric Nursing Practice
- It is used to gather information from caregivers/parents regarding the child’s development, behavior, feeding habits, and immunization status.
- It helps in assessing developmental delays, nutritional issues, or behavioral concerns.
- It promotes family-centered care, where nurses involve parents in care decisions through guided questioning.
✅ 4. Role in Community Health and Public Health Nursing
- It is used during surveys and home visits to gather data on family health, sanitation, maternal-child health, and communicable disease prevention.
- It assists in identifying vulnerable populations who require follow-up or referral.
- It supports planning and evaluation of community interventions, such as nutrition programs or family planning awareness.
✅ 5. Nursing Education and Student Evaluation
- It is used by nurse educators during clinical teaching to develop critical thinking through case-based questioning.
- It supports formative and summative assessments, where students are asked to justify decisions and prioritize care.
- It enhances student engagement, reflection, and knowledge retention.
✅ 6. Use in Health Teaching and Counseling
- It is used during patient teaching to assess their understanding of health conditions, treatments, or discharge instructions.
- It helps in tailoring education materials according to the patient’s literacy and awareness level.
- It supports behavioral change, for example in diabetic education, where nurses ask about dietary habits and compliance.
✅ 7. Role in Nursing Research and Data Collection
- It is an essential part of qualitative interviews and structured questionnaires used in nursing research projects.
- It ensures the quality and relevance of the data collected, improving the reliability of the study.
- It supports pilot testing of tools, where open-ended questioning reveals tool weaknesses.
✅ 8. Quality Improvement and Audit in Hospital Settings
- It is used in patient satisfaction surveys and incident reporting tools.
- It supports clinical audits, where nurses ask specific questions to staff about compliance with care protocols.
- It contributes to data collection for hospital accreditation, such as NABH or JCI standards.
3. Uses of statistics
Statistics is the science of collecting, analyzing, interpreting, and presenting data. In nursing and healthcare, statistics is an essential tool for evidence-based practice, decision-making, research analysis, and quality improvement. It plays a crucial role in clinical, administrative, educational, and community health settings.
1. Use in Nursing Research and Evidence-Based Practice
- It is used to test research hypotheses through statistical tools like t-tests, chi-square, correlation, regression, and ANOVA.
- It provides quantitative evidence for new nursing interventions or practices.
- It supports the validation of research instruments, such as questionnaires and rating scales through reliability and validity testing.
- It allows comparison between different groups, such as control vs. experimental groups in clinical trials.
- It assists in meta-analysis, combining data from multiple studies for stronger conclusions.
- It is essential in determining sample size and power calculation for accurate study design.
2. Use in Patient Care and Clinical Decision-Making
- It helps nurses interpret lab reports, vital signs, and other measurable indicators to assess patient condition.
- It is used to calculate medication dosages accurately, especially in pediatric and critical care.
- It helps identify deviations from normal ranges, supporting early detection of health complications.
- It is used in clinical risk prediction models, such as APGAR score, Braden scale, or fall risk assessment tools.
- It enables prioritization of care, especially in resource-limited settings through triage scoring.
- It supports decision-making in evidence-based clinical pathways (e.g., diabetes or hypertension management).
3. Use in Quality Assurance and Performance Monitoring
- It helps monitor infection rates, bedsores, falls, and medication errors, which are quality indicators.
- It is used in monthly or quarterly hospital reports, where nursing performance is evaluated statistically.
- It supports root cause analysis (RCA) using statistical trend data.
- It is applied in benchmarking, where hospital or ward data is compared with national or global standards.
- It helps in patient feedback analysis, converting qualitative responses into measurable outcomes.
- It facilitates continuous quality improvement (CQI) by showing areas of improvement through charts and graphs.
4. Use in Education and Training of Nurses
- It is used in analyzing results of nursing students’ theory and clinical exams.
- It helps determine effectiveness of teaching methods through pre-test and post-test analysis.
- It is applied in assessing correlations between student performance and attendance, teaching style, or clinical exposure.
- It enables educators to identify weak learning areas and modify curriculum accordingly.
- It supports evidence-based nursing education, validating the success of educational interventions.
- It assists in student project data analysis, teaching students how to interpret and use statistics in their future careers.
5. Use in Community Health and Public Health Programs
- It helps in analyzing population health indicators, such as birth rate, death rate, morbidity, and prevalence of diseases.
- It is used to evaluate impact of health campaigns like tuberculosis awareness or nutrition supplementation.
- It guides decision-making in resource allocation for community programs.
- It allows comparison of health status across geographic regions or socio-economic groups.
- It supports outbreak investigation, helping track the source and spread of infections (e.g., dengue, cholera).
- It helps in planning immunization drives, tracking coverage percentages and missed populations.
6. Use in Hospital Administration and Staffing
- It is used in preparing duty rosters based on patient census and nurse-patient ratios.
- It helps in budgeting and financial planning, using cost analysis and resource consumption data.
- It supports workload management, measuring time per procedure, patient turnover, and shift performance.
- It helps in forecasting supply needs, such as medications, PPE kits, and linens.
- It is applied in staff satisfaction surveys, interpreting feedback statistically to improve workplace conditions.
- It enables time-motion studies, evaluating efficiency in workflow and suggesting process improvements.
7. Use in Development of Health Policies
- It supports formulation of national health programs by providing evidence of disease burden.
- It helps prioritize healthcare needs by identifying high-risk populations through epidemiological statistics.
- It justifies funding allocation to health projects, using cost-benefit or cost-effectiveness analysis.
- It aids in policy evaluation, measuring success or failure of interventions based on outcome indicators.
- It supports legislative advocacy, where statistical evidence is presented to lawmakers.
- It contributes to global health initiatives, using statistical models for disease control planning (e.g., malaria elimination).
8. Use in Publication and Presentation of Research
- It allows the creation of tables, graphs, pie charts, and bar diagrams, which visually enhance research presentation.
- It helps assess statistical significance, giving confidence in research results.
- It enables communication of research findings to a broad audience, including journals, conferences, and policymakers.
- It supports peer-review process, where data must be backed by statistical analysis.
- It assists in writing the result and discussion sections, using means, SDs, p-values, and confidence intervals.
- It promotes credibility of nursing research, encouraging evidence-based knowledge sharing.
Que:3 Describe Utilization of research findings. 10
Definition of Utilization of Research Findings
- It is defined as the systematic process of implementing the outcomes of scientific studies into real-world nursing settings such as hospitals, community clinics, nursing schools, and administrative offices.
- It refers to using research evidence to guide nursing decisions, policies, education plans, and patient care interventions.
- It is also known as “Research Translation” or “Research-to-Practice.”
Objectives of Research Utilization
- It is done to achieve the following goals:
- To bridge the gap between theory (research) and practice.
- To improve patient care outcomes through scientifically proven methods.
- To update nursing procedures and protocols based on current evidence.
- To promote critical thinking and innovation in nursing care.
- To reduce outdated, unsafe, or ineffective practices in hospitals and communities.
- To enhance professional credibility and decision-making among nurses.
- To influence health policy and health program development using valid data.
Types of Research Utilization
✅ A. Direct Research Utilization
- It refers to the actual application of research findings into daily nursing care activities.
- Example : Using a research-based pain scale like the “Wong-Baker Faces Scale” for pediatric pain assessment.
✅ B. Indirect Research Utilization
- It influences the way nurses think or understand problems even if not applied immediately.
- Example : Reading research about patient safety that increases awareness of medication errors.
✅ C. Persuasive Research Utilization
- It is used to convince stakeholders (e.g., nursing administrators or policymakers) to support a change based on research.
- Example : Using research to advocate for increased staffing in ICU based on studies showing lower mortality with better nurse-patient ratios.
Areas of Research Utilization in Nursing
A. Clinical Practice
- It is the most common area where research findings are directly applied to improve patient outcomes.
- Example : Implementing infection prevention protocols based on CDC/WHO guidelines.
B. Nursing Education
- It helps in designing updated nursing curriculum and teaching methodologies.
- Example : Incorporating simulation-based learning after studies prove its benefits in skill development.
C. Nursing Administration and Management
- It is used to make policy, budget, staffing, and planning decisions.
- Example : Research on nurse fatigue influencing shift length or break time policy.
D. Public Health and Health Policy
- It helps in formulating national or community health programs.
- Example : Maternal health surveys contributing to the design of safe motherhood initiatives.
Steps in the Process of Research Utilization
✅ Step 1: Identifying Practice Problems
It involves recognizing issues in patient care or nursing operations that require improvement or evidence-based alternatives.
✅ Step 2 : Searching and Reviewing Research
It involves locating high-quality, peer-reviewed studies relevant to the identified problem using databases (e.g., PubMed, CINAHL).
✅ Step 3 : Critical Appraisal of Research
It is essential to assess the reliability, validity, and relevance of the research findings before implementation.
✅ Step 4 : Extraction of Findings and Planning
It includes selecting key conclusions and planning how to apply them within the local context, including resources, staff readiness, etc.
✅ Step 5 : Implementation in Practice
It is the actual application of research findings through training, policy change, and practice updates.
✅ Step 6 : Evaluation and Feedback
It includes measuring patient outcomes, staff feedback, and compliance to determine the success of the implementation.
Barriers to Research Utilization
Individual Barriers
- Lack of time due to workload
- Poor understanding of statistics and research terms
- Resistance to change or preference for traditional methods
- Lack of motivation or confidence in interpreting research
Organizational Barriers
- Limited access to journals or research databases
- Lack of institutional support or funding
- No formal policy for evidence-based practice
- Poor communication between researchers and nursing staff
Strategies to Promote Research Utilization
- Organizing regular training, workshops, and journal clubs for nurses.
- Developing easy-to-follow clinical guidelines based on research.
- Creating evidence-based nursing protocols in all units.
- Appointing nurse researchers or clinical nurse specialists to guide research implementation.
- Using digital platforms and hospital intranets to share new research findings.
- Encouraging collaboration between academic researchers and clinical staff.
- Providing time and incentives for nurses to participate in research.
Role of Nurse in Research Utilization
✅ 1. Identifying Practice-Based Problems
- It is the nurse’s responsibility to observe recurring clinical issues and care gaps at the bedside or in the community.
- Nurses can help transform real-time clinical observations into researchable problems or practice improvement projects.
✅ 2. Accessing and Reviewing Research Literature
- It is essential for nurses to routinely read journals, publications, and evidence-based guidelines.
- Nurses can use digital tools (PubMed, CINAHL, WHO, CDC) to find high-quality research that relates to their patient population.
✅ 3. Participating in Research Studies
- It is the nurse’s role to support or co-lead research projects, especially in hospitals or academic institutions.
- They may help with data collection, patient interviews, tool development, and pilot testing.
✅ 4. Critical Appraisal of Research Articles
- It is important for nurses to develop skills in evaluating research validity, methodology, sample size, and relevance.
- This helps ensure that only high-quality, applicable findings are introduced into practice.
✅ 5. Applying Research to Direct Patient Care
- It is the nurse’s responsibility to incorporate research findings into nursing interventions, patient education, and care plans.
- Example: Implementing evidence-based positioning strategies to prevent pressure ulcers.
✅ 6. Advocating for Research-Based Practice
- It is the nurse’s role to promote a culture of evidence-based practice among peers.
- They may raise concerns or offer solutions during clinical rounds or nursing handovers based on current research.
✅ 7. Leading Practice Change Projects
- It is encouraged for senior nurses or nurse educators to lead practice improvement initiatives, using research as the foundation.
- They may develop standard operating procedures (SOPs), protocols, or clinical pathways based on current evidence.
✅ 8. Educating Patients and Families Using Evidence
- It is the nurse’s duty to educate patients using accurate, research-backed information.
- Example : Teaching diabetic patients about updated diet recommendations based on recent studies.
✅ 9. Collaborating with Interdisciplinary Teams
- It is the nurse’s responsibility to share relevant research with doctors, dietitians, physiotherapists, and pharmacists.
- This ensures coordinated care that is based on the latest scientific findings.
✅ 10. Monitoring and Evaluating Outcomes
- It is the nurse’s task to observe and document the effects of research-based interventions.
- This includes tracking clinical indicators (e.g., infection rate, pain level, mobility) before and after changes.
✅ 11. Giving Feedback and Reporting Barriers
- It is vital for nurses to communicate what worked and what did not during research implementation.
- Their feedback is crucial for modifying procedures and making them more practical.
✅ 12. Acting as Change Agents in Practice Settings
- It is the nurse’s role to support and motivate fellow nurses to adopt new, research-informed approaches.
- They can organize in-service education, mentorship programs, or skill labs to promote change.
✅ 13. Documenting Practice Innovations
- It is the nurse’s responsibility to record successful innovations and changes made through research utilization.
- This documentation may contribute to nursing audits, annual reports, or publications.
✅ 14. Disseminating Research Outcomes
- It is encouraged for nurses to present their research findings in conferences, seminars, or publish in nursing journals.
- This helps in spreading awareness and encouraging global nursing improvement.
✅ 15. Supporting Ethical Research Use
- It is important that nurses follow ethical principles when applying or participating in research.
- They must ensure informed consent, confidentiality, and respect for patient autonomy in every research-related action.
Que: 4 Calculate mean 05
7, 4, 8, 2, 5, 4, 2, 8
7, 4, 8, 2, 5, 4, 2, 8
7 + 4 + 8 + 2 + 5 + 4 + 2 + 8 = 40
Total number of values = 8
Mean = Sum of all values / Total number of values = 40/8 =5
Mean = 5
14, 10, 3, 8, 1, 5, 6, 10
14, 10, 3, 8, 1, 5, 6, 10
14 + 10 + 3 + 8 + 1 + 5 + 6 + 10 = 57
Total number of values = 8
Mean = Sum of all values / Total number of values = 57/8 =7.125
Mean = 7.125