P.B.B.Sc.F.Y.FON-JANUARY-2017 (SAURASHTRA UNIVERSITY)(PAPER NO.1)(UPLOAD)(DONE)
PAPER SOLUTION OF P.B.B.Sc.NURSING.F.Y.FON & NUTRITION AND DIETETICS-JANUARY-2017 (SAURASHTRA UNIVERSITY-GUJARAT)
SECTION-1
1 Long Essay (Any Two) 2X10=20
1.A. Define Health and Nursing Profession. 03
Define Health :-
According to the World Health Organization (WHO), health is defined as “a state of complete physical, mental, and social well-being and not merely the absence of disease or infirmity.”
Health is a multifaceted concept encompassing physical, mental, and social well-being.
It is not merely the absence of disease but also the presence of optimal functioning in various aspects of life.
The nursing profession plays a crucial role in promoting and maintaining health across individuals and communities.
Therefore, achieving optimal health requires a comprehensive approach that addresses not only medical needs but also social, economic, and environmental determinants.
Define Nursing Profession :-
The nursing profession is a vital component of the healthcare system, encompassing a diverse range of roles and responsibilities.
Nurses are trained professionals who provide holistic care to individuals, families, and communities across the lifespan.
They work in various settings, including hospitals, clinics, community health centers, schools, and long-term care facilities.
Nurses play a crucial role in promoting health and preventing illness through health education, disease prevention, and health promotion activities.
They assess patients’ health needs, develop care plans, administer treatments, and monitor progress.
Additionally, nurses advocate for patients’ rights, ensure continuity of care, and collaborate with other healthcare professionals to optimize patient outcomes.
1.B. Describe the factors influencing the health and illness.07
Factors influnece the health :-
Many factors influence health, and they can be categorized into several broad categories:
- Biological Factors: These include genetics, age, sex, and underlying health conditions. Genetic predispositions can influence susceptibility to certain diseases, while age and sex can impact health risks and outcomes.
- Behavioral Factors: Lifestyle choices such as diet, physical activity, substance use (including tobacco, alcohol, and drugs), and adherence to medical recommendations significantly affect health. Healthy behaviors can reduce the risk of chronic diseases and improve overall well-being.
- Social and Economic Factors: Socioeconomic status, education level, employment status, income, housing conditions, and access to healthcare services profoundly impact health outcomes. Individuals with lower socioeconomic status often face greater barriers to accessing healthcare, nutritious food, safe housing, and education, leading to disparities in health.
- Environmental Factors: Environmental conditions, including air and water quality, exposure to pollutants, access to green spaces, and community safety, can affect health. Environmental factors contribute to the development of respiratory diseases, cardiovascular problems, and other health issues.
- Psychological Factors: Mental health, stress levels, social support networks, and coping mechanisms play a significant role in overall health. Chronic stress, depression, anxiety, and social isolation can negatively impact physical health and increase the risk of developing chronic diseases.
- Access to Healthcare: Availability, affordability, and quality of healthcare services influence health outcomes. Lack of access to healthcare can lead to delayed diagnosis and treatment of diseases, exacerbating health problems.
- Cultural and Social Norms: Cultural beliefs, traditions, and social norms shape health behaviors, attitudes towards seeking medical care, and acceptance of preventive measures. Understanding cultural diversity is essential for providing culturally competent healthcare.
- Public Health Policies and Interventions: Government policies, regulations, and public health interventions such as vaccination programs, tobacco control measures, and health education campaigns can have significant effects on population health outcomes.
Factors influence the illness
Illness can be influenced by a multitude of factors, including biological, psychological, social, and environmental factors. Here are some key factors that can influence the onset and progression of illness:
Biological Factors:
- Genetics: Genetic predispositions can increase the likelihood of developing certain illnesses or conditions.
- Age: The susceptibility to certain illnesses may vary with age, with some conditions more prevalent in children, while others are more common in older adults.
- Gender: Some illnesses may affect one gender more than the other due to biological differences.
- Immunological Factors: The strength of the immune system can influence susceptibility to infectious diseases and autoimmune conditions.
Psychological Factors:
- Stress: Chronic stress can weaken the immune system and contribute to the development or exacerbation of various illnesses.
- Mental Health: Mental health disorders such as depression, anxiety, and PTSD can impact physical health and increase the risk of certain illnesses.
- Coping Mechanisms: Maladaptive coping mechanisms or unhealthy behaviors (e.g., smoking, substance abuse) can contribute to illness.
Social Factors:
- Socioeconomic Status: Lower socioeconomic status is associated with higher rates of illness due to factors such as limited access to healthcare, inadequate nutrition, and increased exposure to environmental toxins.
- Social Support: Strong social networks and support systems can buffer against the negative effects of stress and promote better health outcomes.
- Education: Higher levels of education are often associated with better health outcomes, as education can lead to greater health literacy and access to resources for health promotion and disease prevention.
Environmental Factors:
- Pollution: Exposure to environmental pollutants such as air and water pollution can increase the risk of respiratory diseases, cardiovascular conditions, and other health problems.
- Climate: Climate-related factors such as temperature extremes, humidity, and natural disasters can impact health and contribute to the spread of infectious diseases.
- Access to Healthcare: Limited access to healthcare services, including preventive care and treatment, can delay diagnosis and exacerbate illness.
Lifestyle Factors:
- Diet and Nutrition: Poor dietary habits can contribute to the development of chronic conditions such as obesity, diabetes, and cardiovascular disease.
- Physical Activity: Lack of physical activity is associated with an increased risk of obesity, heart disease, and other health problems.
- Substance Use: Tobacco, alcohol, and drug use can have detrimental effects on health and increase the risk of various illnesses and injuries.
2. A. Define nursing process. 02
The nursing process is a systematic method used by nurses to assess, diagnose, plan, implement, and evaluate patient care. It involves a series of steps that help nurses deliver holistic and individualized care to patients, focusing on their physical, emotional, social, and spiritual needs.The nursing process is a systematic method used by nurses to provide individualized care to patients.
2. B. Explain the steps in nursing process. 03
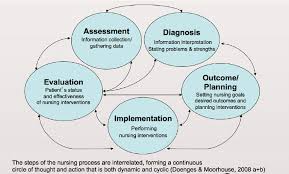
It consists of five steps:
- Assessment: Gathering comprehensive data about a patient’s health status, including physical, emotional, psychological, and social aspects. This involves observation, interviewing, and examination.
- Diagnosis: Analyzing the assessment data to identify actual or potential health problems, risks, and strengths. Nursing diagnoses are formulated based on this analysis, which helps in planning appropriate interventions.
- Planning: Developing a plan of care tailored to the patient’s unique needs and preferences. This includes setting goals and establishing priorities for addressing the identified health issues. The plan should be realistic, measurable, and achievable.
- Implementation: Carrying out the planned interventions to achieve the established goals. Nurses implement various nursing interventions such as medication administration, patient education, and therapeutic communication to promote the patient’s health and well-being.
- Evaluation: Assessing the effectiveness of the interventions in meeting the patient’s goals and outcomes. This step involves comparing the patient’s progress with the expected outcomes, identifying any deviations, and modifying the plan of care accordingly. Evaluation is an ongoing process that informs subsequent assessments and interventions.
2. C. Draw a nursing plan for the patient admitted with fever in medical ward. 05
Assessment:
- Monitor vital signs regularly (temperature, pulse, respiration, blood pressure).
- Assess the patient’s level of consciousness, hydration status, and overall condition.
Fluid Management:
- Ensure adequate hydration by encouraging oral fluids if tolerated.
- Administer intravenous fluids as prescribed to maintain hydration status.
Temperature Management:
- Administer antipyretic medications as prescribed to reduce fever and discomfort.
- Use cooling measures such as tepid sponge baths or cooling blankets if necessary.
Infection Control:
- Implement standard precautions to prevent the spread of infection.
- Educate the patient and caregivers about proper hand hygiene techniques.
Monitoring and Documentation:
- Document all assessments, interventions, and patient responses accurately and promptly.
- Monitor for signs of complications such as worsening fever, altered mental status, or development of sepsis.
Comfort Measures:
- Provide comfort measures such as changing bedding, providing a quiet environment, and offering pain relief as needed.
Nutritional Support:
- Ensure the patient receives adequate nutrition to support recovery.
- Monitor intake and output, and assess for signs of dehydration or malnutrition.
Collaboration with Healthcare Team:
- Communicate effectively with other members of the healthcare team to ensure coordinated care.
- Collaborate with physicians and other healthcare providers to adjust the treatment plan as needed based on the patient’s response.
Education and Discharge Planning:
- Educate the patient and caregivers about the importance of completing the prescribed treatment regimen.
- Provide information about signs and symptoms that require prompt medical attention after discharge.
Follow-up Care:
- Arrange for follow-up appointments as needed to monitor the patient’s progress and ensure continuity of care.
Remember, this plan should be tailored to the individual patient’s needs and may require adjustments based on their condition and response to treatment.
3. A. Define and write the purposes of Physical Examination. 05
definition:
A physical examination is a comprehensive assessment of an individual’s overall health and well-being, typically conducted by a healthcare professional.
Its purpose is to:
- Assess Health Status: Determine the current state of health, identify any existing medical conditions, and monitor changes over time.
- Detect Illnesses: Detect signs and symptoms of diseases or conditions, including those that may not yet be causing noticeable symptoms.
- Screen for Risk Factors: Identify risk factors for future health problems, such as high blood pressure, high cholesterol, or obesity.
- Establish Baseline: Establish a baseline of normal findings for comparison during future examinations.
- Promote Prevention: Provide an opportunity for education and counseling on preventive measures, healthy lifestyle choices, and early detection of diseases.
- Build Patient-Provider Relationship: Foster trust and communication between the patient and healthcare provider, leading to better overall care and outcomes.
B. Illustrate the head to foot examination that has perfomed in the student. 05
A head to foot examination typically involves the following steps:
- Head: Check the scalp for any abnormalities, including lumps or lesions. Inspect the eyes, ears, nose, and mouth for signs of infection or other issues.
- Neck: Palpate the lymph nodes for swelling or tenderness. Assess neck mobility and check for any abnormalities in the thyroid gland.
- Chest: Auscultate the lungs for any abnormal sounds such as crackles or wheezes. Palpate the chest for tenderness or masses.
- Heart: Auscultate the heart to assess for any murmurs or irregular rhythms. Palpate for any thrills or abnormal pulsations.
- Abdomen: Palpate the abdomen for tenderness, organ enlargement, or masses. Listen for bowel sounds in all four quadrants.
- Genitalia: Inspect the external genitalia for any signs of infection or abnormalities. Palpate for any lumps or tenderness.
- Extremities: Check for any deformities, swelling, or tenderness in the arms and legs. Assess muscle strength and joint mobility.
- Skin: Perform a thorough examination of the skin, noting any lesions, rashes, or discolorations. Pay special attention to moles or other signs of skin cancer.
- Neurological: Evaluate cranial nerves, reflexes, sensation, and motor function to assess neurological status.
- Gait and posture: Observe the student’s gait and posture for any abnormalities that may indicate musculoskeletal or neurological issues.
Throughout the examination, communicate with the student to ensure their comfort and cooperation, and document any findings accurately.
2 .Short Essays (Any Three): 3X5=15
A. State Nursing & Midwives Council
- state nursing and midwives council
The State Nursing and Midwifery Council is a regulatory body responsible for overseeing the practice of nursing and midwifery within a specific state or region. - It ensures that nurses and midwives adhere to professional standards, regulations, and ethical guidelines, while also providing licensure, accreditation, and continuing education opportunities.
- State nursing and midwifery councils play a crucial role in regulating and overseeing the nursing and midwifery professions within their respective states.
- They set standards for education, practice, and ethics, issue licenses or registrations to qualified professionals, and enforce disciplinary actions when necessary.
- Additionally, they may also be involved in developing policies, promoting professional development, and ensuring the quality of healthcare services provided by nurses and midwives within their jurisdiction. Key functions of State Nursing Councils typically include:
- Licensure: State Nursing Councils issue licenses to qualified nurses, ensuring they meet the educational and competency requirements necessary to practice nursing within the state.
- Registration: Nurses are often required to register with the State Nursing Council to practice legally. This registration process may involve providing proof of education, passing licensure examinations, and meeting other regulatory requirements.
- Regulation: State Nursing Councils establish and enforce regulations governing nursing practice, including scope of practice, standards of care, and ethical guidelines. They may also investigate complaints against nurses and take disciplinary action when necessary.
- Continuing Education: State Nursing Councils often mandate continuing education requirements for nurses to maintain their licensure. These requirements ensure that nurses stay current with advancements in healthcare and maintain their competence.
- Accreditation: Some State Nursing Councils are involved in accrediting nursing education programs within their jurisdiction. They set standards for nursing schools and conduct periodic evaluations to ensure that educational programs meet these standards.
- Advocacy: State Nursing Councils may advocate for the interests of nurses and the nursing profession within the state, including lobbying for legislation that promotes nursing practice, patient safety, and healthcare quality.
- State Nursing Councils typically operate under the authority of state governments and may have varying structures and procedures depending on the state’s regulatory framework. They collaborate with national nursing organizations, such as the American Nurses Association (ANA) in the United States, to develop standards of practice and promote professional development within the nursing profession.
- It’s important for nurses to be aware of and adhere to the regulations set forth by their State Nursing Council to ensure compliance with legal and ethical standards of nursing practice.
B. Holistic Nursing
Holistic nursing is a nursing practice that considers the whole person—body, mind, spirit, and emotions—within the context of their environment. It emphasizes the interconnectedness of all aspects of an individual’s health and wellness and seeks to promote healing and wellbeing through a comprehensive approach that addresses physical, psychological, social, and spiritual needs.
principles and components of holistic nursing include:
- Holistic Assessment: Holistic nurses conduct comprehensive assessments that consider not only physical symptoms but also the patient’s mental, emotional, and spiritual state, as well as their social and environmental context.
- Therapeutic Relationship: Holistic nurses prioritize building trusting and compassionate relationships with patients, recognizing the importance of rapport and empathy in the healing process.
- Integrative Therapies: Holistic nursing integrates complementary and alternative therapies alongside conventional medical treatments to support the whole person. This may include techniques such as massage, acupuncture, aromatherapy, meditation, and nutritional counseling.
- Patient Education: Holistic nurses empower patients to take an active role in their health by providing education and resources to promote self-care, healthy lifestyle choices, and holistic approaches to healing.
- Mind-Body-Spirit Connection: Holistic nursing acknowledges the interconnectedness of physical, mental, emotional, and spiritual health and seeks to promote balance and harmony among these dimensions.
- Cultural Competence: Holistic nurses recognize and respect the diversity of beliefs, values, and cultural practices among individuals and communities, tailoring care to meet the unique needs and preferences of each patient.
- Preventive Care: Holistic nursing emphasizes prevention and health promotion, aiming to identify and address underlying causes of illness before they manifest as symptoms.
- Environmental Awareness: Holistic nurses consider the impact of environmental factors on health and advocate for practices that promote a safe and healing environment for patients.
Holistic nursing is not a separate specialty but rather a philosophy and approach that can be integrated into nursing practice across all settings and specialties. Nurses who practice holistically may work in a variety of healthcare settings, including hospitals, clinics, community health centers, and private practices.
Overall, holistic nursing seeks to foster healing, promote wellness, and enhance the quality of life for individuals and communities by addressing the full range of physical, emotional, mental, social, and spiritual factors that influence health and wellbeing.
C. Nursing Audit
Definition of Nursing Audit
Nursing audit is the process of collecting information from nursing reports and other documented evidence about patient care and assessing the quality of care by the use of quality assurance programmes
According to Goster Walfer
a. Nursing Audit is an exercise to find out whether good nursing practices are followed.
b. The audit is a means by which nurses themselves can define standards from their point of view and describe the actual practice of nursing.
PURPOSES OF NURSING AUDIT
- Evaluating Nursing care given,
- Achieves deserved and feasible quality of nursing care,
- Stimulant to better records,
- Focuses on care provided and not on care provider,
- Contributes to research.
ADVANTAGES OF NURSING AUDIT
- Can be used as a method of measurement in all areas of nursing.
- Seven functions are easily understood,
- Scoring system is fairly simple,
- Results easily understood,
5.Assesses the work of all those involved in recording care,
- May be a useful tool as part of a quality assurance programme in areas where accurate records of care are kept. DISADVANTAGES OF THE NURSING AUDIT
appraises the outcomes of the nursing process, so it is not so useful in areas where the nursing process has not been implemented,
many of the components overlap making analysis difficult,
- is time consuming,
- requires a team of trained auditors,
- deals with a large amount of information,
- only evaluates record keeping. It only serves to improve documentation, not nursing care
D Expanded role of a nurse.
The expanded role of nurses encompasses a broader scope of responsibilities beyond traditional patient care.
This includes:
- Patient Advocacy:
Nurses advocate for patients’ rights, ensuring they receive appropriate care and support. They may also educate patients about their conditions and treatment options. - Health Promotion and Disease Prevention:
Nurses engage in activities aimed at promoting healthy behaviors and preventing illness. This may involve conducting screenings, providing education on nutrition and exercise, and promoting vaccinations. - Care Coordination:
Nurses play a vital role in coordinating care among healthcare providers and ensuring continuity of care for patients transitioning between healthcare settings. - Advanced Practice Nursing: Advanced practice nurses, such as nurse practitioners, nurse anesthetists, and nurse midwives, have expanded roles with the ability to diagnose, treat, and manage patients independently or in collaboration with other healthcare professionals.
- Leadership and Management:
Nurses often take on leadership and management roles in healthcare organizations, overseeing teams of healthcare providers, managing resources, and implementing quality improvement initiatives. - Research and Evidence-Based Practice:
Nurses contribute to the advancement of healthcare through research and evidence-based practice. They participate in research studies, implement evidence-based interventions, and contribute to the development of best practices in nursing. - Health Education and Counseling: Nurses provide health education and counseling to patients and their families, empowering them to make informed decisions about their health and well-being.
- Technology Integration:
Nurses utilize technology to enhance patient care, including electronic health records, telemedicine, and medical devices. They are often involved in the implementation and use of technology in healthcare settings.
Overall, the expanded role of nurses reflects their growing importance in healthcare delivery, with an emphasis on holistic patient care, health promotion, and the integration of evidence-based practices and technology.
3.Very Short Essays (Any Five): 5X2=10
A. Enlist 4 functions of INC
he Indian Nursing Council (INC) serves several functions, including:
- Setting standards: It establishes and maintains uniform standards for nursing education in India, ensuring quality education and training for nurses across the country.
- Regulation: The INC regulates the nursing profession by prescribing the qualifications for various levels of nursing education and practice, as well as registration requirements for nurses.
- Accreditation: It accredits nursing schools and colleges to ensure they meet the prescribed standards for nursing education, thereby maintaining quality assurance in the profession.
- Policy development: The INC plays a role in developing policies related to nursing education, practice, and research, aiming to advance the nursing profession and improve healthcare delivery in India.
B. Expand SNA, UNESCO, UNICEF
- SNA –
A student nurses association is an organization formed by nursing students to provide support, networking opportunities, educational resources, and advocacy for its members. These associations often aim to enhance the educational experience of nursing students, promote professional development, and facilitate communication among peers and within the broader healthcare community. - UNESCO – United Nations Educational, Scientific and Cultural Organization: UNESCO is a specialized agency of the United Nations aimed at promoting peace and security through international cooperation in education, science, culture, and communication.
- UNICEF – United Nations Children’s Fund: UNICEF is a United Nations agency responsible for providing humanitarian and developmental aid to children worldwide, focusing on healthcare, nutrition, education, protection, and emergency relief.
C. What is code of ethics
Code of Ethics
A code of ethics is a set of principles or guidelines that outline the ethical behaviors expected of individuals or groups within a particular profession, organization, or society.
These codes typically cover areas such as honesty, integrity, confidentiality, respect, fairness, and responsibility.
Each profession or organization may have its own specific code of ethics tailored to its unique needs and values.
D. Define quality assurance
QUALITY ASSURANCE
Quality assurance in nursing refers to the systematic processes and activities implemented to ensure that nursing care meets predetermined standards of excellence and achieves desired outcomes.
It involves continuous monitoring, evaluation, and improvement of nursing practices, protocols, and outcomes to enhance patient safety, satisfaction, and overall healthcare delivery.
Quality assurance in nursing aims to maintain high standards of care, prevent errors, and promote continuous professional development among nurses.
E. List out six nursing theory
- Florence Nightingale’s Environmental Theory*: Emphasizes the importance of the environment in promoting healing and includes principles such as fresh air, cleanliness, and proper nutrition.
- Hildegard Peplau’s Interpersonal Relations Theory: Focuses on the nurse-patient relationship and the therapeutic process of communication to promote understanding and growth.
- Dorothea Orem’s Self-Care Deficit Theory: Proposes that nursing is required when an individual is unable to fulfill their own self-care needs and emphasizes the nurse’s role in assisting with self-care activities.
- Jean Watson’s Theory of Human Caring: Emphasizes the importance of caring relationships and the interconnectedness of all beings, highlighting the nurse’s role in promoting healing through caring behaviors.
- Betty Neuman’s Systems Model: Views individuals as being influenced by various stressors and proposes that nursing interventions should focus on maintaining stability and promoting wellness within the client’s system.
- Madeleine Leininger’s Theory of Cultural Care Diversity and Universality: Emphasizes the importance of understanding cultural beliefs, values, and practices in nursing care delivery, with the goal of providing culturally congruent care.
F. Define team nursing.
Team nursing is a healthcare delivery model where a team of healthcare professionals, including registered nurses, licensed practical nurses, and nursing assistants, collaboratively provide patient care. Each member of the team has specific roles and responsibilities, and they work together to address the holistic needs of patients. This model promotes communication, coordination, and efficiency in delivering comprehensive care.
SECTION-II (30 Marks )
1 Long Essay (Any one) 5+5=10
1) Components of a balanced diet
A balanced diet includes a variety of foods that provide essential nutrients in appropriate proportions to support overall health and wellbeing. Here are the key components of a balanced diet:
- Carbohydrates: Carbohydrates are the body’s primary source of energy. They include sugars, starches, and fiber. Healthy sources of carbohydrates include whole grains (such as brown rice, quinoa, oats), fruits, vegetables, and legumes.
- Proteins: Proteins are essential for building and repairing tissues, as well as for the production of enzymes and hormones. Good sources of protein include lean meats (such as chicken, turkey, fish), eggs, dairy products (such as milk, yogurt, cheese), legumes (beans, lentils, chickpeas), nuts, and seeds.
- Fats: Healthy fats are important for providing energy, supporting cell growth, and protecting organs. They also help in the absorption of certain vitamins (like vitamins A, D, E, and K). Healthy sources of fats include avocados, nuts, seeds, olive oil, fatty fish (such as salmon, mackerel, sardines), and flaxseeds.
- Vitamins: Vitamins are essential micronutrients that play various roles in the body’s functions, such as supporting the immune system, promoting healthy skin and vision, and aiding in metabolism. A balanced diet should include a variety of fruits, vegetables, whole grains, and lean proteins to ensure an adequate intake of vitamins, including vitamins A, C, D, E, K, and B-complex vitamins.
- Minerals: Minerals are essential for various bodily functions, including bone health, nerve function, and fluid balance. Important minerals include calcium, magnesium, potassium, sodium, iron, zinc, and selenium. Good food sources of minerals include dairy products, leafy green vegetables, nuts, seeds, whole grains, lean meats, and seafood.
- Fiber: Dietary fiber is crucial for maintaining digestive health, regulating bowel movements, and reducing the risk of chronic diseases such as heart disease and type 2 diabetes. Fiber is found in fruits, vegetables, whole grains, legumes, nuts, and seeds.
- Water: Although not a nutrient, water is essential for life and is vital for maintaining hydration, regulating body temperature, transporting nutrients, and flushing out waste products. It’s important to drink an adequate amount of water throughout the day to stay hydrated.
A balanced diet emphasizes whole, minimally processed foods and includes a variety of nutrients to support overall health and prevent nutrient deficiencies. It’s also important to consider individual dietary needs, preferences, and health goals when planning meals and making food choices. Consulting with a healthcare professional or registered dietitian can provide personalized guidance on achieving a balanced diet.
2) Importance of having a healthy balanced diet.
Having a healthy balanced diet is essential for maintaining overall health and wellbeing. Here are some key reasons why it’s important:
- Nutrient Adequacy: A balanced diet provides the body with essential nutrients, including carbohydrates, proteins, fats, vitamins, and minerals, in the right proportions. These nutrients are necessary for various bodily functions, such as energy production, tissue repair, immune function, and hormone regulation.
- Disease Prevention: A balanced diet can help prevent chronic diseases such as heart disease, diabetes, obesity, hypertension, and certain cancers. Consuming a variety of nutrient-rich foods, including fruits, vegetables, whole grains, lean proteins, and healthy fats, can reduce the risk factors associated with these diseases.
- Weight Management: Maintaining a healthy weight is important for overall health and reduces the risk of obesity-related conditions such as diabetes, heart disease, and joint problems. A balanced diet that includes appropriate portions of nutrient-dense foods can support weight management by providing essential nutrients while controlling calorie intake.
- Energy and Vitality: Eating a balanced diet provides the body with the energy it needs to function optimally throughout the day. Nutrient-rich foods supply the necessary fuel for physical activity, mental alertness, and overall vitality, helping individuals feel more energized and productive.
- Improved Digestive Health: A balanced diet that includes adequate fiber from fruits, vegetables, whole grains, and legumes promotes healthy digestion and regular bowel movements. Fiber helps prevent constipation, promotes gut health by feeding beneficial gut bacteria, and reduces the risk of digestive disorders such as diverticulosis and hemorrhoids.
- Better Mental Health: There is a growing body of evidence suggesting that diet plays a significant role in mental health. Consuming a balanced diet rich in fruits, vegetables, whole grains, and healthy fats can support brain function, improve mood, reduce the risk of depression and anxiety, and enhance overall cognitive health.
- Strong Immune System: A well-balanced diet provides the nutrients necessary for a strong immune system, helping the body defend against infections and illnesses. Nutrients such as vitamins A, C, D, E, zinc, and selenium play key roles in supporting immune function and promoting overall health.
- Longevity and Quality of Life: Following a balanced diet can contribute to a longer, healthier life by reducing the risk of chronic diseases and improving overall wellbeing. By nourishing the body with essential nutrients, individuals can enhance their quality of life and enjoy greater vitality as they age.
In summary, having a healthy balanced diet is fundamental for promoting overall health, preventing disease, maintaining a healthy weight, supporting mental wellbeing, and enhancing longevity and quality of life. Making nutritious food choices and prioritizing a balanced diet can have profound and far-reaching benefits for individuals of all ages.
OR
1) Definition and objectives of diet therapy
Definition Diet Therapy
Diet therapy, also known as medical nutrition therapy, is a therapeutic approach that uses specific diets and nutritional interventions to treat or manage various medical conditions.
The objective of diet therapy
The objective of diet therapy, also known as medical nutrition therapy, is to optimize health outcomes and manage medical conditions through the use of personalized nutrition interventions. The goals of diet therapy vary depending on the individual’s specific health needs and medical conditions but generally include:
- Promoting Health and Wellbeing: Diet therapy aims to promote overall health and wellbeing by providing the body with essential nutrients in appropriate proportions. It emphasizes consuming a balanced diet that meets the individual’s nutritional needs and supports optimal physical and mental function.
- Preventing and Managing Chronic Diseases: Diet therapy plays a crucial role in preventing and managing chronic diseases such as heart disease, diabetes, obesity, hypertension, and certain cancers. Specific dietary interventions may be tailored to reduce risk factors associated with these conditions, such as controlling blood sugar levels in diabetes or lowering cholesterol levels in heart disease.
- Achieving and Maintaining a Healthy Weight: For individuals who are overweight or obese, diet therapy focuses on achieving and maintaining a healthy weight through calorie control, portion management, and dietary modifications. It emphasizes adopting a balanced diet that promotes sustainable weight loss and supports long-term weight maintenance.
- Optimizing Nutritional Status: Diet therapy aims to optimize nutritional status by addressing nutrient deficiencies or imbalances that may contribute to poor health outcomes. It involves assessing the individual’s dietary intake, identifying nutrient gaps, and recommending dietary modifications or supplementation as needed to meet nutrient requirements.
- Supporting Digestive Health: Diet therapy plays a role in supporting digestive health and managing gastrointestinal disorders such as irritable bowel syndrome (IBS), Crohn’s disease, ulcerative colitis, and celiac disease. Dietary interventions may include identifying and avoiding trigger foods, increasing fiber intake, and promoting gut-friendly foods.
- Managing Food Allergies and Intolerances: For individuals with food allergies or intolerances, diet therapy focuses on identifying and eliminating problematic foods from the diet while ensuring adequate nutrient intake and meeting nutritional needs through alternative food sources.
- Enhancing Athletic Performance: Diet therapy can optimize athletic performance by providing the body with the nutrients and energy it needs to fuel physical activity, support muscle recovery, and improve endurance and strength. It involves tailoring nutrition recommendations to meet the specific energy and nutrient demands of athletes based on their sport, training regimen, and individual goals.
- Improving Quality of Life: Ultimately, the objective of diet therapy is to improve the individual’s quality of life by addressing nutritional needs, managing medical conditions, and promoting overall health and wellbeing. It involves empowering individuals to make informed food choices, adopt healthy eating habits, and achieve their health goals through personalized nutrition interventions.
2) Dietary management for cardiovascular disorders.
Dietary management for cardiovascular disorders focuses on reducing risk factors such as high blood pressure, high cholesterol levels, and obesity, which contribute to conditions like heart disease, stroke, and hypertension. Key principles include:
- Balanced Diet: Emphasizing fruits, vegetables, whole grains, lean proteins, and healthy fats while minimizing saturated fats, trans fats, cholesterol, and sodium.
- Limiting Sodium: Lowering sodium intake helps control blood pressure. Encouraging foods low in sodium and reducing the use of added salt in cooking and at the table is crucial.
- Reducing Saturated and Trans Fats: Limiting foods high in saturated fats, such as fatty meats and full-fat dairy products, as well as avoiding trans fats found in processed and fried foods, helps lower LDL cholesterol levels.
- Increasing Fiber: Consuming soluble fiber from sources like oats, beans, fruits, and vegetables can help lower cholesterol levels.
- Omega-3 Fatty Acids: Including sources of omega-3 fatty acids, such as fatty fish (salmon, mackerel, trout), flaxseeds, chia seeds, and walnuts, may help reduce the risk of heart disease.
- Maintaining a Healthy Weight: Promoting weight management through calorie control, portion control, and regular physical activity is essential for overall cardiovascular health.
- Limiting Alcohol: Moderating alcohol intake, if consumed, as excessive alcohol consumption can increase blood pressure and contribute to heart disease.
- Managing Blood Sugar: For individuals with diabetes or at risk of diabetes, controlling blood sugar levels through diet, medication, and lifestyle changes is crucial for cardiovascular health.
- Regular Monitoring: Regular monitoring of blood pressure, cholesterol levels, and other relevant parameters helps track progress and adjust dietary interventions as needed.
2 Short notes (Any 2): 2X5=10
1) Mid-day meal programme
Mid -day Meal program
The Mid Day Meal Scheme is a school meal programme in India designed to better the nutritional status of school-age children nationwide.The Midday Meal Programme is a government-led initiative aimed at improving the nutritional status, health, and educational outcomes of schoolchildren in India. Here are the key aspects and objectives of the Midday Meal Programme:
[1] The scheme has been renamed as PM-POSHAN Scheme.
[2] The programme supplies free lunches on working days for children in government primary and upper primary schools, government aided Anganwadis, Madarsa and Maqtabs.
[3] Serving 120 million children in over 1.27 million schools and Education Guarantee Scheme centres, the Midday Meal Scheme is the largest of its kind in the world.
- Provision of Nutritious Meals: The primary objective of the Midday Meal Programme is to provide nutritious meals to schoolchildren, especially those from disadvantaged backgrounds. The meals typically include items such as rice, lentils, vegetables, and fruits, providing essential nutrients like carbohydrates, proteins, vitamins, and minerals.
- Improving Attendance and Enrollment: By providing free meals at schools, the programme aims to increase school attendance and enrollment rates, particularly among children from marginalized communities. The availability of a nutritious meal encourages parents to send their children to school regularly.
- Enhancing Nutritional Status: The Midday Meal Programme contributes to improving the nutritional status of schoolchildren by ensuring they receive at least one nutritious meal per day. This helps address issues of malnutrition and undernutrition, which can affect physical and cognitive development.
- Supporting Learning and Concentration: Adequate nutrition is essential for cognitive function and academic performance. By reducing hunger and providing essential nutrients, the Midday Meal Programme supports children’s ability to concentrate, learn, and participate actively in classroom activities.
- Promoting Social Inclusion: The programme aims to promote social inclusion by ensuring that all children, regardless of their socioeconomic background, have access to nutritious meals at school. This helps reduce disparities in access to food and education and promotes equity in educational outcomes.
- Empowering Women: The implementation of the Midday Meal Programme often involves the participation of local communities, including women’s self-help groups and community organizations, in meal preparation and distribution. This empowers women by providing employment opportunities and promoting their involvement in community development initiatives.
- Improving Public Health: The Midday Meal Programme contributes to improving public health outcomes by addressing nutritional deficiencies and promoting healthy eating habits among schoolchildren. By investing in children’s health and wellbeing, the programme helps build a healthier future generation.
- Fostering Social Cohesion: Sharing meals together at school fosters a sense of community and social cohesion among students, teachers, and staff. It promotes values of cooperation, sharing, and solidarity, contributing to a positive school environment.
Overall, the Midday Meal Programme plays a crucial role in addressing the complex challenges of poverty, malnutrition, and education in India. By providing nutritious meals to schoolchildren, the programme contributes to breaking the cycle of poverty, promoting educational attainment, and building a healthier and more equitable society.
2) Importance and types of weaning
Importance of weaning :-
- Nutritional Needs: Breast milk or formula provides essential nutrients for infants during the first few months of life. However, as babies grow, their nutritional needs change, and they require additional nutrients that cannot be obtained solely from milk. Introducing solid foods during weaning helps meet these changing nutritional needs by providing a wider variety of nutrients, such as iron, zinc, and vitamins.
- Developmental Milestone: Weaning is a developmental milestone that marks a baby’s transition from infancy to early childhood. It involves learning new skills, such as chewing and swallowing solid foods, which are important for oral motor development and overall growth.
- Texture and Taste Exploration: Introducing a variety of textures and tastes during weaning helps babies develop their taste preferences and food acceptance. Exposure to a diverse range of flavors and textures early in life can encourage healthy eating habits and reduce the likelihood of picky eating later on.
- Iron Needs: Iron is essential for healthy growth and development, particularly for the brain. Breast milk contains low levels of iron, which may become insufficient to meet a baby’s needs after around six months of age. Introducing iron-rich solid foods, such as iron-fortified cereals, meat, poultry, fish, and legumes, during weaning helps prevent iron deficiency anemia.
- Development of Motor Skills: Weaning provides opportunities for babies to practice and develop their motor skills, including hand-eye coordination, grasping, and self-feeding. Offering age-appropriate finger foods and utensils encourages independent feeding and enhances fine motor skills.
- Growth and Weight Gain: Introducing complementary foods during weaning can support healthy growth and weight gain in babies. Solid foods provide additional calories and nutrients needed for growth, particularly as babies become more active and energetic.
- Satiety and Hunger Regulation: Weaning helps babies learn to regulate their appetite and recognize feelings of hunger and fullness. Offering a variety of nutritious foods in appropriate portion sizes teaches babies to listen to their hunger cues and develop healthy eating patterns.
- Bonding and Social Interaction: Weaning is an opportunity for caregivers to bond with babies through feeding interactions. Sharing meals together and introducing new foods in a positive and supportive environment fosters a sense of security and trust between caregivers and babies.
Types of weaning :-
Traditional (Spoon-Feeding) Weaning:
- Introduction of Purées: In traditional weaning, caregivers introduce smooth puréed foods to the baby’s diet gradually, starting around six months of age. These purées are typically made from fruits, vegetables, grains, and proteins.
- Controlled Feeding: Caregivers spoon-feed the baby small amounts of puréed food, gradually increasing the texture and variety as the baby grows and becomes more accustomed to eating solid foods.
- Transition to Textured Foods: As the baby becomes more adept at eating and swallowing, caregivers gradually introduce mashed or chopped foods with varying textures and consistencies.
- Emphasis on Spoon-Feeding: Traditional weaning involves caregivers actively feeding the baby using a spoon, controlling the pace and amount of food offered.
Baby-Led Weaning (BLW):
- Self-Feeding: Baby-led weaning involves allowing the baby to self-feed from the start, typically beginning around six months of age when the baby shows signs of readiness for solid foods.
- Introduction of Finger Foods: Instead of purées, caregivers offer age-appropriate finger foods to the baby, allowing them to explore and manipulate the food themselves. These foods are typically soft in texture and easy to grasp.
- Encourages Independence: Baby-led weaning encourages independence and autonomy in eating. Babies learn to pick up and explore foods, bring them to their mouths, and control their own feeding.
- Promotes Oral Motor Development: Baby-led weaning promotes the development of oral motor skills, including chewing, swallowing, and managing different food textures, as babies learn to handle and manipulate solid foods from an early age.
- Family Mealtime Integration: Baby-led weaning often involves incorporating the baby into family mealtimes, allowing them to observe and learn from the eating behaviors of caregivers and siblings.
3) Macronutrients.
Macronutrients are the main nutrients that provide energy and essential building blocks for the body. There are three primary macronutrients:
Carbohydrates:
- Function: Carbohydrates are the body’s primary source of energy. They provide fuel for physical activity, brain function, and other metabolic processes.
- Types: Carbohydrates can be classified into three main types:
- Simple Carbohydrates: Also known as sugars, simple carbohydrates include glucose, fructose, and sucrose. They are found in foods such as fruits, honey, and table sugar.
- Complex Carbohydrates: Complex carbohydrates consist of long chains of sugar molecules and include starches and dietary fiber. They are found in foods such as grains, legumes, vegetables, and fruits.
- Fiber: Dietary fiber is a type of carbohydrate that the body cannot digest. It plays a crucial role in digestive health, promoting regular bowel movements, and reducing the risk of chronic diseases such as heart disease and diabetes.
- Sources: Carbohydrate-rich foods include fruits, vegetables, grains (such as rice, wheat, oats), legumes (beans, lentils), dairy products, and sugary foods and beverages.
Proteins:
- Function: Proteins are essential for building and repairing tissues, supporting immune function, producing enzymes and hormones, and serving as a source of energy when needed.
- Structure: Proteins are made up of amino acids, which are often referred to as the building blocks of protein. There are 20 different amino acids, nine of which are considered essential because the body cannot produce them and must obtain them from the diet.
- Sources: Protein-rich foods include meat, poultry, fish, eggs, dairy products (such as milk, yogurt, cheese), tofu, tempeh, legumes (beans, lentils, chickpeas), nuts, seeds, and soy products.
Fats:
- Function: Fats serve as a concentrated source of energy, provide insulation and protection for organs, support cell membrane structure, facilitate the absorption of fat-soluble vitamins (A, D, E, K), and play a role in hormone production.
- Types: Fats can be classified into several types, including:
- Saturated Fats: Found primarily in animal products and some plant oils, saturated fats are typically solid at room temperature. They have been linked to an increased risk of heart disease when consumed in excess.
- Monounsaturated Fats: Found in foods such as olive oil, avocados, nuts, and seeds, monounsaturated fats are considered heart-healthy and may help lower LDL (bad) cholesterol levels.
- Polyunsaturated Fats: Polyunsaturated fats include omega-3 and omega-6 fatty acids, which are essential fats that the body cannot produce on its own and must obtain from the diet. They play important roles in brain function, inflammation, and heart health.
- Trans Fats: Trans fats are artificial fats that are created through a process called hydrogenation. They are found in partially hydrogenated oils and are associated with an increased risk of heart disease.
- Sources: Fat-rich foods include oils (olive oil, canola oil, coconut oil), butter, margarine, fatty fish (salmon, mackerel, trout), nuts, seeds, avocados, and high-fat dairy products.
It’s important to consume a balanced diet that includes adequate amounts of all three macronutrients to support overall health and wellbeing. The Dietary Guidelines for Americans recommend that carbohydrates should provide 45-65% of total daily calories, proteins should provide 10-35% of total daily calories, and fats should provide 20-35% of total daily calories, with an emphasis on choosing healthy sources of fats and limiting saturated and trans fats.
3. Short answers (Any 5) 5X2=10
1) Body mass index
Body mass index
Body Mass Index (BMI) is a measure used to assess an individual’s body weight in relation to their height.
It’s calculated by dividing a person’s weight in kilograms by the square of their height in meters (BMI = weight(kg) / height(m)^2).
It’s commonly used to categorize individuals into different weight categories: underweight,
normal weight,
overweight,
and obese.
2) Action of vitamin K
Action of vit k
Vitamin K plays a crucial role in blood clotting.
When you have a cut or injury, vitamin K helps produce proteins necessary for blood clot formation, which stops bleeding.
Additionally, vitamin K is involved in bone metabolism and may have other roles in the body, such as supporting cardiovascular health.
3) List down 2 bacteria which cause food poisoning
Salmonella: Salmonella bacteria are commonly found in raw or undercooked poultry, eggs, meat, and unpasteurized dairy products. Symptoms of salmonella food poisoning include diarrhea, abdominal cramps, fever, nausea, and vomiting.
Clostridium botulinum: Clostridium botulinum bacteria produce a potent toxin that can cause botulism, a rare but serious form of food poisoning. The bacteria can grow in improperly canned or preserved foods, as well as in homemade low-acid canned goods. Symptoms of botulism include muscle weakness, paralysis, difficulty breathing, and potentially death if left untreated.
4) List down the symptoms of marasmus
Symptoms of Marasmus
The symptoms of marasmus are more common than the symptoms of kwashiorkor, which include:
Dizziness
Weight loss
Dehydration
Lack of energy
Stunted growth
Chronic Diarrhoea
Shrinkage of Stomach
Respiratory infections
Dry skin and brittle hair
Underweight or loss of muscle mass and subcutaneous fat
5) Beriberi
Beriberi is a disease caused by a deficiency of thiamine (vitamin B1).
It primarily affects the nervous system, cardiovascular system, and muscles. Symptoms include weakness, fatigue, difficulty walking, pain, and swelling in the limbs.
Beriberi can be prevented and treated with thiamine supplements and a balanced diet.
6) Road-to-health chart
Road to health chart
It sounds like you’re referring to a “Road to Health Chart,” which is a growth chart used to monitor the growth and development of children.
It typically includes measurements such as weight, height, and head circumference plotted against age to track a child’s growth trajectory.
These charts are commonly used by healthcare professionals to assess a child’s growth and development over time.
7) Meaning of food adulteration
Food adulteration
Food adulteration refers to the practice of intentionally debasing the quality of food by adding inferior, harmful, or cheaper substances to it.
This can include adding artificial colors, flavors, or preservatives, diluting with water or other substances, or substituting with cheaper ingredients.
Adulteration is typically done to increase profits for the seller, but it can pose serious health risks to consumers.