🟢P.B.B.Sc.FON NOV-2023 (sau.uni) (UPLOAD PAPER NO.6)
P.B.B.Sc.FON NOV-2023 (sau.uni)
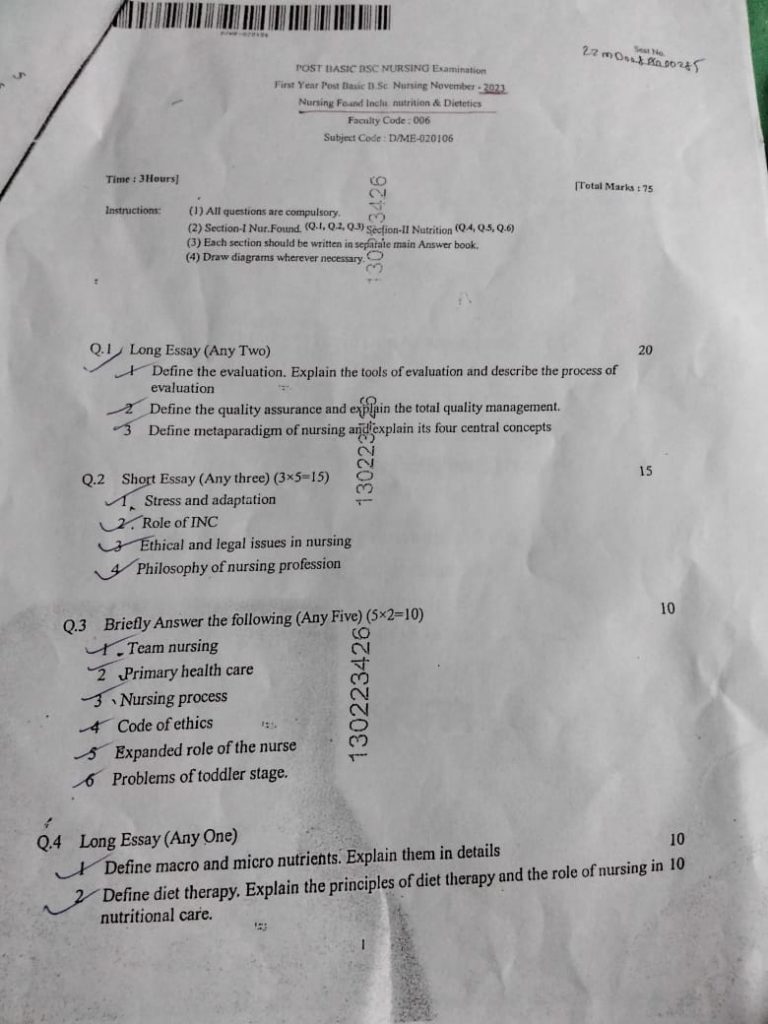
⏩Q.1 Long Essay (Any Two)20
🔸1 Define the evaluation. Explain the tools of evaluation and describe the process of evaluation
Evaluation Definition:
Evaluation in nursing refers to the systematic process of determining the extent to which nursing interventions have been successful in achieving desired outcomes. It involves assessing the patient’s progress towards the goals established during the planning phase of the nursing process.
✍️Tools of Evaluation:
Observation:
- Directly observing the patient’s behavior, physical condition, and overall response to treatment.
- Example: Watching a patient perform a specific task or monitoring their vital signs.
Interviews:
- Asking the patient or their family about their health status, perceptions, and experiences.
- Example: Conducting a structured or unstructured interview to gather subjective data.
Examinations:
- Conducting physical assessments or diagnostic tests to gather objective data.
- Example: Performing a head-to-toe physical examination or ordering blood tests.
Questionnaires and Surveys:
- Using structured tools to collect information on specific aspects of the patient’s health or experience.
- Example: A pain assessment scale or a satisfaction survey.
Checklists and Rating Scales:
- Using standardized tools to rate specific behaviors or symptoms.
- Example: The Glasgow Coma Scale for assessing consciousness levels.
✍️Process of Evaluation:
Setting Criteria and Standards:
- Establishing clear, measurable criteria and standards to compare actual outcomes against.
- Example: Defining a specific target for blood pressure levels in hypertensive patients.
Collecting Data:
- Gathering relevant information through observation, interviews, examinations, and other tools.
- Example: Measuring a patient’s blood pressure at regular intervals.
Interpreting Data:
- Analyzing the collected data to determine whether the goals and outcomes have been met.
- Example: Comparing the patient’s current blood pressure readings with the target levels.
Documenting Findings:
- Recording the evaluation results in the patient’s medical record.
- Example: Writing a progress note summarizing the patient’s response to treatment.
Deciding on Next Steps:
- Based on the evaluation, deciding whether to continue, modify, or terminate the current plan of care.
- Example: Adjusting the patient’s medication regimen if blood pressure targets are not met.
Communicating Results:
- Sharing the evaluation findings with the healthcare team and the patient.
- Example: Discussing the results in a team meeting or with the patient during a consultation.
🔸2 Define the quality assurance and exfijin the total quality management.
Quality assurance (QA) in nursing invol
ves systematic processes and procedures to ensure that nursing care meets predetermined standards and achieves desired outcomes. QA aims to enhance the quality of patient care through continuous monitoring, evaluation, and improvement of nursing practices.
👉Total Quality Management (TQM)
✍️ Definition:
Total Quality Management (TQM) is a comprehensive management approach that focuses on continuous improvement of processes, products, and services to achieve high quality. TQM involves the participation of all members of an organization in improving processes, systems, and organizational culture.
👉Components of TQM in Nursing:
Patient-Centered Care:
- Focusing on the needs, preferences, and expectations of patients.
- Example: Involving patients in decision-making about their care.
Continuous Improvement:
- Implementing ongoing efforts to improve processes and outcomes.
- Example: Regularly reviewing and updating clinical protocols based on the latest evidence.
Teamwork and Collaboration:
- Promoting effective communication and collaboration among healthcare team members.
- Example: Conducting interdisciplinary team meetings to discuss patient care plans.
Leadership Commitment:
- Ensuring strong leadership support for quality initiatives.
- Example: Hospital administrators prioritizing quality improvement projects.
Data-Driven Decision Making:
- Using data and evidence to guide decision-making and improvements.
- Example: Analyzing patient outcome data to identify areas for improvement.
Employee Involvement and Training:
- Engaging and training staff at all levels in quality improvement efforts.
- Example: Providing ongoing education and training on quality improvement techniques.
TQM Process in Nursing:
Identify Improvement Areas:
- Recognizing areas where quality can be enhanced.
- Example: Noticing an increase in hospital-acquired infections.
Set Goals and Objectives:
- Establishing specific, measurable goals for improvement.
- Example: Reducing the rate of hospital-acquired infections by 20% within six months.
Develop and Implement Plans:
- Creating and executing action plans to achieve the goals.
- Example: Implementing stricter infection control protocols and training staff.
Monitor and Measure Performance:
- Regularly tracking progress towards the goals.
- Example: Conducting monthly audits of infection rates.
Analyze Results:
- Evaluating the effectiveness of the implemented changes.
- Example: Comparing infection rates before and after the intervention.
Make Necessary Adjustments:
- Making further changes based on the evaluation results.
- Example: Modifying protocols if infection rates do not decrease as expected.
Sustain Improvements:
- Ensuring that improvements are maintained over time.
- Example: Establishing ongoing monitoring and review processes.
🔸3 Define metaparadigm of nursing and explain its four central concepts
Metaparadigm of Nursing:
A metaparadigm is the most abstract level of knowledge in nursing and provides a global perspective of the discipline. The nursing metaparadigm includes four central concepts: Person, Health, Environment, and Nursing.
✍️Four Central Concepts:
Person:
- Refers to the recipient of care, including individuals, families, and communities.
- Emphasizes the holistic nature of individuals, considering physical, psychological, social, and spiritual aspects.
- Example: Providing personalized care that respects a patient’s cultural background and individual preferences.
Health:
- Encompasses the overall well-being of the person, including physical, mental, and social health.
- Views health as a dynamic state that can fluctuate over time.
- Example: Promoting healthy lifestyle choices and preventive care to enhance overall well-being.
Environment:
- Includes all external factors that affect the person, such as physical, social, and cultural environments.
- Recognizes the impact of the environment on health and well-being.
- Example: Creating a safe and supportive hospital environment to promote patient recovery.
Nursing:
- Represents the actions and interventions performed by nurses to provide care.
- Focuses on the nurse-patient relationship and the role of nursing in promoting health and well-being.
- Example: Developing and implementing a care plan tailored to a patient’s specific needs.
These concepts form the foundation of nursing practice, guiding nurses in their interactions with patients and the delivery of care.
⏩Q.2 Short Essay (Any three) (3-5-15)
🔸1 Stress and adaptation
Stress refers to the body’s response to any demand or challenge. It can be physical, emotional, or psychological in nature and involves physiological, behavioral, and cognitive reactions to perceived threats or changes.
2. Types of Stress:
- Acute Stress: Short-term stress response triggered by immediate stressors, such as deadlines or sudden physical danger.
- Chronic Stress: Persistent stress over an extended period, often due to ongoing situations like work pressures, financial problems, or chronic illness.
- Psychological Stress: Stress resulting from mental or emotional pressure, including anxiety, fear, or grief.
- Physiological Stress: Stress affecting the body’s physical state, such as illness, injury, or extreme environmental conditions.
3. Physiological Response to Stress:
- Fight-or-Flight Response: Activation of the sympathetic nervous system triggers the release of stress hormones (e.g., adrenaline, cortisol), increasing heart rate, blood pressure, and metabolic rate to prepare the body to respond to perceived threats.
- Hypothalamic-Pituitary-Adrenal (HPA) Axis: Complex hormonal feedback system involving the hypothalamus, pituitary gland, and adrenal glands, regulating cortisol release and influencing stress response and adaptation.
5. Adaptation to Stress:
- Definition: Adaptation refers to the body’s ability to adjust physiologically, psychologically, and behaviorally to stressors over time, maintaining stability and function.
- General Adaptation Syndrome (GAS): Proposed by Hans Selye, GAS describes the body’s response to stress in three stages:
- Alarm Reaction: Initial response to stress, activating the fight-or-flight response.
- Resistance: Continued adaptation to stress, where the body attempts to restore balance while coping with ongoing stressors.
- Exhaustion: Long-term exposure to stress leads to depletion of resources, increasing vulnerability to illness or breakdown.
6. Factors Influencing Adaptation:
- Genetics and Biology: Individual differences in physiological responses to stress, including genetic predispositions and neurobiological factors influencing resilience.
- Psychosocial Factors: Social support, coping skills, personality traits (e.g., optimism), and life experiences shape how individuals perceive and respond to stress.
- Environmental Factors: Socioeconomic status, access to resources, and environmental conditions impact stress levels and ability to adapt.
🔸2 Role of INC
The Indian Nursing Council (INC) plays a crucial role in regulating and advancing the nursing profession in India. Here are the detailed points outlining its role:
Regulation of Nursing Education:
- The INC is responsible for setting standards and guidelines for nursing education and training programs across India.
- It establishes curriculum frameworks, educational requirements, and accreditation criteria for nursing schools, colleges, and institutions.
Licensing and Registration:
- The INC oversees the registration and licensing of nurses in India.
- It maintains a national registry of qualified nurses who meet the prescribed educational and professional standards.
Development of Educational Standards:
- The council develops and updates educational standards for nursing programs to ensure quality and relevance.
- It promotes continuous improvement in nursing education through periodic reviews and revisions of curriculum guidelines.
Promotion of Professional Ethics and Standards:
- The INC sets ethical standards and codes of conduct for nurses in India.
- It promotes professionalism, integrity, and ethical practices among registered nurses through guidelines and disciplinary measures when necessary.
Accreditation of Nursing Institutions:
- The council accredits nursing institutions based on established criteria to ensure they meet educational and infrastructure standards.
- Accreditation by the INC signifies that a nursing institution maintains quality in education, facilities, and faculty.
Advocacy for Nursing Profession:
- The INC serves as an advocate for the nursing profession at national and international levels.
- It collaborates with government bodies, healthcare organizations, and other stakeholders to address issues affecting nurses’ rights, working conditions, and professional development.
Research and Development Initiatives:
- The council promotes research and development in nursing practice, education, and healthcare delivery.
- It supports initiatives that contribute to evidence-based practice and innovation in nursing to enhance patient care outcomes.
Continuing Education and Training:
- The INC encourages lifelong learning and professional development among nurses through continuing education programs and training opportunities.
- It facilitates workshops, seminars, and conferences to update nurses on emerging trends, technologies, and best practices in healthcare.
Policy Formulation and Advocacy:
- The council participates in policy formulation related to nursing education, practice, and healthcare policy.
- It provides expert guidance and recommendations to government bodies and policymakers on issues affecting the nursing profession and healthcare system.
Quality Assurance in Nursing Care:
- The INC contributes to ensuring quality nursing care by promoting adherence to standards, guidelines, and best practices among registered nurses.
- It emphasizes the importance of patient safety, infection control, and effective communication in nursing practice.
Through these roles and functions, the Indian Nursing Council plays a pivotal role in fostering excellence, professionalism, and quality in the nursing profession in India, ultimately contributing to improved healthcare outcomes nationwide.
🔸3 Ethical and legal issues in nursing
Ethical and legal issues in nursing are crucial considerations that nurses encounter in their daily practice. Here’s an overview of key points for both ethical and legal aspects:
Ethical Issues in Nursing:
- Patient Autonomy: Respecting patients’ rights to make informed decisions about their own care, including the right to refuse treatment.
- Beneficence: Acting in the best interest of the patient to promote their well-being and health outcomes.
- Non-maleficence: Avoiding harm to patients and ensuring that interventions do not cause unnecessary suffering.
- Justice: Fair distribution of healthcare resources and equal treatment of all patients regardless of socioeconomic status, ethnicity, or other factors.
- Veracity: Being truthful and honest with patients about their condition, treatment options, and prognosis.
- Confidentiality: Maintaining patient privacy and confidentiality of medical information, adhering to HIPAA regulations.
Legal Issues in Nursing:
- Licensure and Credentialing: Nurses must have valid licenses to practice, and they must adhere to state-specific regulations regarding scope of practice.
- Negligence and Malpractice: Nurses can be held liable for negligence if they fail to provide care that meets established standards, resulting in harm to the patient.
- Informed Consent: Ensuring that patients fully understand the risks, benefits, and alternatives of proposed treatments before consenting to care.
- Documentation: Accurate and timely documentation of patient assessments, interventions, and outcomes is essential for legal protection and continuity of care.
- Patient Rights: Upholding patients’ rights to privacy, dignity, and respect, and advocating for them in situations where these rights may be compromised.
- End-of-Life Care: Understanding legal frameworks such as advance directives and physician-assisted suicide laws, and ensuring patient wishes are respected.
Navigating these issues requires nurses to have a thorough understanding of ethical principles, legal standards, and institutional policies. Continuous education and adherence to professional codes of ethics are crucial to maintaining high standards of patient care and legal compliance in nursing practice.
🔸4 Philosophy of nursing profession
he philosophy of the nursing profession encompasses core beliefs and principles that guide nurses in their practice. Here are key points that define the philosophy of nursing:
- Caring: Nursing emphasizes a caring relationship between the nurse and the patient, recognizing the patient as a whole person with unique physical, emotional, social, and spiritual needs.
- Holistic Approach: Nurses embrace a holistic perspective, addressing not only the physical health of the patient but also their psychological, social, and spiritual well-being.
- Patient Advocacy: Nurses advocate for the rights and interests of patients, ensuring they receive safe, compassionate, and ethical care.
- Evidence-Based Practice: Incorporating the best available evidence from research, clinical expertise, and patient preferences into decision-making to optimize patient outcomes.
- Professionalism: Upholding high standards of professional conduct, ethics, and accountability in all aspects of nursing practice.
- Education and Lifelong Learning: Commitment to continuous education and professional development to enhance knowledge, skills, and competence in delivering quality care.
- Collaboration: Working collaboratively with interdisciplinary healthcare teams, patients, families, and communities to achieve optimal health outcomes.
- Ethical Practice: Adhering to ethical principles such as autonomy, beneficence, non-maleficence, justice, and veracity in every patient interaction and decision.
- Health Promotion and Prevention: Promoting health, preventing illness, and empowering individuals and communities to take control of their health through education and advocacy.
- Leadership: Nurses demonstrate leadership at various levels, influencing healthcare policies, advocating for change, and serving as role models in promoting a healthy work environment.
- Cultural Sensitivity and Diversity: Respecting and embracing cultural diversity, recognizing its impact on healthcare beliefs and practices, and providing culturally competent care.
- Continuous Improvement: Engaging in reflective practice and quality improvement initiatives to enhance nursing care delivery and patient outcomes.
These philosophical foundations guide nurses in providing compassionate, competent, and ethical care to individuals, families, and communities across diverse healthcare settings.
⏩Q.3 Briefly Answer the following (Any Five) (5×2=10)
🔸1 Team nursing
Team nursing involves a registered nurse leading a group of healthcare providers, including licensed practical nurses and nursing assistants, to deliver comprehensive patient care. Each team member contributes based on their skills and training, fostering collaboration and efficiency in healthcare delivery.
🔸2 Primary health care
Primary health care is a fundamental approach to health and well-being that addresses the majority of an individual’s health needs throughout their life. It is community-based, accessible, and emphasizes health promotion, disease prevention, treatment of common illnesses, and management of chronic conditions.
🔸3 Nursing process
The nursing process is a systematic framework used by nurses to provide patient-centered care. It consists of five steps: Assessment involves collecting and analyzing patient data. Diagnosis identifies the patient’s health issues and needs. Planning involves setting achievable goals and developing a care plan. Implementation is the execution of the care plan. Evaluation assesses the effectiveness of the care provided and adjusts the plan as needed.
🔸4 Code of ethics
A code of ethics in nursing outlines principles and standards of conduct that guide professional practice and ensure ethical behavior. It includes principles such as respect for patient autonomy, confidentiality, advocacy for patient rights, integrity, accountability, and maintaining competence.
🔸5 Expanded role of the nurse
Nurses today play diverse roles beyond direct patient care. They engage in health promotion, disease prevention, patient education, and chronic disease management. Nurses also participate in care coordination, leadership within healthcare teams, research, policy development, and advocacy to improve healthcare outcomes and patient safety.
🔸6 Problems of toddler stage.
Toddlers (ages 1-3 years) face developmental challenges such as asserting independence while still needing guidance and structure. They often experience emotional outbursts and temper tantrums as they learn to manage their emotions and communicate their needs. Toddlers also explore their environment eagerly but may be at risk for accidents due to their curiosity and lack of awareness of danger.
⏩Q.4 Long Essay (Any One)
🔸1 Define macro and micro nutrients. Explain them in details 10
Macronutrients:
- Definition: Macronutrients are nutrients required by the body in relatively large amounts to provide energy and support essential bodily functions.
- Types:
- Carbohydrates: Primary source of energy; simple carbs (sugars) and complex carbs (starches and fiber).
- Proteins: Essential for growth, tissue repair, enzyme production, and immune function.
- Fats: Provide energy, support cell structure, and help absorb fat-soluble vitamins.
- Importance: Macronutrients are crucial for energy production, maintaining bodily functions, and supporting growth and repair processes.
Micronutrients:
- Definition: Micronutrients are essential nutrients required by the body in smaller amounts but are critical for various biochemical processes and overall health.
- Types:
- Vitamins: Organic compounds that regulate metabolism, support immune function, and act as antioxidants.
- Minerals: Inorganic substances necessary for bone health, nerve function, fluid balance, and other physiological processes.
- Importance: Micronutrients play key roles in enzyme reactions, hormone production, and overall cellular function, contributing to health maintenance and disease prevention.
Diet Therapy:
Definition:
- Diet therapy involves using specific nutrition plans to treat or manage medical conditions, promote health, and prevent disease complications through dietary interventions.
Principles of Diet Therapy:
- Individualization: Tailoring diet plans to meet individual needs based on health status, medical history, cultural preferences, and nutritional requirements.
- Modification: Adjusting nutrient intake to address specific health conditions such as diabetes, hypertension, or obesity.
- Monitoring: Regularly assessing dietary intake, nutritional status, and patient response to the prescribed diet to make necessary adjustments.
- Education: Providing patients with information on nutrition, meal planning, and dietary modifications to empower them in managing their health through proper nutrition.
- Integration: Collaborating with healthcare professionals, including dietitians, doctors, and therapists, to ensure comprehensive care and effective treatment outcomes.
Role of Nurses in Nutritional Care:
- Assessment: Conducting comprehensive nutritional assessments to evaluate dietary habits, nutritional deficiencies, and risks associated with medical conditions.
- Planning: Developing individualized diet plans based on nutritional needs, health goals, and therapeutic requirements.
- Implementation: Educating patients and caregivers on dietary guidelines, meal preparation, and strategies to adhere to the prescribed diet.
- Monitoring: Regularly monitoring patients’ dietary compliance, nutritional intake, and health progress to assess the effectiveness of diet therapy.
- Advocacy: Advocating for optimal nutrition as a fundamental component of patient care, promoting dietary adherence, and addressing barriers to nutritional compliance.
- Support: Providing emotional support and encouragement to patients undergoing dietary changes, addressing concerns, and facilitating adjustments to improve dietary outcomes and overall health.
By adhering to these principles and roles, nurses contribute significantly to ensuring that patients receive adequate nutritional care tailored to their specific needs, promoting health and well-being effectively.
🔸2 Define diet therapy. Explain the principles of diet therapy and the role of nursing in nutritional care.10
Definition of Diet Therapy:
Diet therapy refers to the use of a carefully planned diet to improve or manage health conditions, promote recovery, and prevent disease. It involves the modification of normal dietary patterns to suit the needs of individuals with specific medical conditions, such as diabetes, hypertension, obesity, gastrointestinal disorders, or malnutrition. Diet therapy focuses on providing the right nutrients to promote healing and maintain overall health.
Principles of Diet Therapy:
The principles of diet therapy are fundamental guidelines that help in planning therapeutic diets. These include:
Adequacy:
- Ensure that the diet provides all essential nutrients (carbohydrates, proteins, fats, vitamins, minerals, and water) in sufficient amounts to meet the body’s requirements.
Modification of Consistency:
- Modify the consistency of food (e.g., liquid, soft, or solid) to suit the individual’s ability to chew or digest, especially for patients with swallowing difficulties or gastrointestinal issues.
Caloric Control:
- Adjust caloric intake to suit the patient’s energy needs. For example, high-calorie diets for malnourished patients or low-calorie diets for weight management.
Nutrient Density:
- Provide nutrient-dense foods to ensure the patient gets the maximum benefit from their food, especially when they have a reduced appetite or restricted intake.
Balance:
- Ensure a balanced intake of macronutrients (proteins, carbohydrates, and fats) and micronutrients (vitamins and minerals) to maintain health and promote healing.
Individualization:
- Tailor the diet to meet the specific needs of the patient, considering factors like age, medical condition, cultural preferences, and food tolerances or allergies.
Therapeutic Nutrient Alteration:
- Modify the composition of the diet to manage specific health conditions, such as low-sodium diets for hypertension, low-fat diets for cardiovascular diseases, or high-protein diets for wound healing.
Meal Timing and Frequency:
- Adjust meal timings and frequency to promote better digestion and nutrient absorption, such as providing small, frequent meals for individuals with gastrointestinal disorders.
Role of Nursing in Nutritional Care:
Nurses play a crucial role in ensuring the success of diet therapy and nutritional care. Their responsibilities include:
Nutritional Assessment:
- Nurses assess the patient’s nutritional status by monitoring weight, body mass index (BMI), dietary intake, and lab values (e.g., serum protein levels, blood glucose).
Collaboration with Dietitians:
- Nurses work closely with dietitians to develop individualized nutritional plans based on the patient’s specific needs and health conditions.
Patient Education:
- Nurses educate patients and their families about the importance of nutrition, dietary restrictions, and healthy eating habits to manage their health conditions.
Monitoring and Evaluation:
- Nurses monitor the patient’s response to the therapeutic diet, checking for improvements or adverse effects. They also evaluate the patient’s adherence to the prescribed diet and make necessary adjustments in collaboration with healthcare professionals.
Providing Nutritional Support:
- For patients who cannot eat normally, nurses assist in providing enteral or parenteral nutrition. They also monitor for complications related to feeding tubes or intravenous feeding.
Encouraging Compliance:
- Nurses motivate patients to follow dietary recommendations by addressing barriers such as lack of appetite, cultural food preferences, or emotional stress related to illness.
Recording and Reporting:
- Nurses keep detailed records of the patient’s food intake and nutritional status and report changes to the healthcare team to ensure timely interventions.
In summary, diet therapy is essential in managing health conditions through nutritional modifications, and nurses play a critical role in assessing, educating, monitoring, and supporting patients to achieve their nutritional goals.
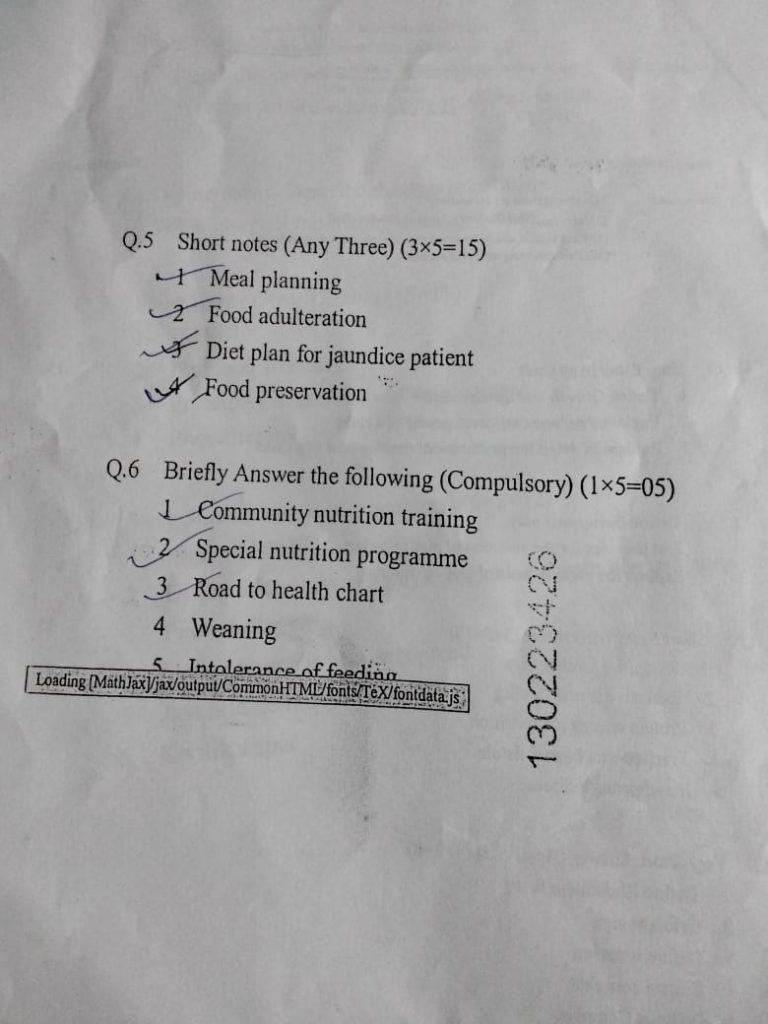
⏩Q.5 Short notes (Any Three) (3×5=15)
🔸1 Meal planning
Assess Dietary Needs and Goals:
- Determine caloric intake requirements based on age, gender, activity level, and health goals (e.g., weight loss, maintenance, muscle gain).
- Consider any dietary restrictions or preferences (e.g., vegetarian, gluten-free).
Create a Weekly Menu:
- Plan meals for each day of the week, considering breakfast, lunch, dinner, and snacks.
- Include a variety of foods to ensure nutritional balance (e.g., fruits, vegetables, lean proteins, whole grains).
Grocery Shopping:
- Make a list of ingredients needed for the planned meals.
- Check pantry and fridge for existing items to avoid unnecessary purchases.
- Consider seasonal produce for freshness and cost-effectiveness.
Preparation and Cooking:
- Batch cook ingredients that can be used in multiple meals (e.g., grilled chicken, chopped vegetables).
- Prepare meals in advance, especially for busy days, and store them properly.
Portion Control and Nutrition:
- Use portion control methods to ensure balanced meals (e.g., measuring cups, food scales).
- Monitor nutritional content such as calories, protein, carbohydrates, and fats to meet dietary goals.
Variety and Flexibility:
- Introduce variety in meals to prevent monotony and ensure enjoyment.
- Allow flexibility for adjustments based on schedule changes or availability of ingredients.
Storage and Preservation:
- Store perishable items correctly to maintain freshness and prevent waste (e.g., refrigeration, freezing).
- Use airtight containers or freezer bags for longer storage periods.
Evaluation and Adjustment:
- Assess meal planning effectiveness based on taste, satisfaction, and adherence to dietary goals.
- Adjust future plans based on feedback and evolving nutritional needs.
By following these steps, you can effectively plan meals that are nutritious, enjoyable, and aligned with your dietary goals.
🔸2 Food adulteration
Types of Adulterants: Adulterants can include substances like chemicals (e.g., pesticides, dyes, preservatives), non-food materials (e.g., stones, sand), lower-grade substances (e.g., inferior quality flour mixed with wheat flour), or harmful substances (e.g., toxins, pathogens).
- Commonly Adulterated Foods: Certain foods are more susceptible to adulteration than others. Examples include milk (with water or synthetic milk), spices (with colorants or non-edible substances), oils (with cheaper oils or non-edible oils), and grains (with stones, sand, or moldy grains).
- Health Risks: Consumption of adulterated foods can pose serious health risks such as food poisoning, gastrointestinal disorders, allergic reactions, long-term illnesses (e.g., cancer from chemical contaminants), or even death in severe cases.
- Detection Methods: Various methods are employed to detect food adulteration, including chemical analysis, microscopy, chromatography, and sensory evaluation. Rapid testing kits are also used to detect specific contaminants or adulterants in food samples.
- Regulations and Control: Governments establish regulations and standards to prevent and control food adulteration. Regulatory bodies conduct inspections, testing, and enforce penalties for offenders to ensure food safety and protect public health.
- Consumer Awareness and Education: Educating consumers about recognizing signs of food adulteration, reading food labels, buying from reliable sources, and reporting suspicious products can empower individuals to make informed choices and contribute to food safety efforts.
Efforts to combat food adulteration involve a combination of regulatory measures, technological advancements in detection methods, consumer vigilance, and public awareness campaigns to safeguard food quality and protect public health.
🔸3 Diet plan for jaundice patient
Hydration: Encourage adequate hydration with water, herbal teas, and coconut water to support liver function and help flush out toxins.
- Low-Fat Diet: Emphasize a low-fat diet to reduce stress on the liver. Avoid fried foods, fatty meats, and full-fat dairy products.
- High-Quality Protein: Include lean protein sources such as skinless poultry, fish, eggs, legumes, and tofu to support liver repair and maintain muscle mass.
- Complex Carbohydrates: Choose whole grains like brown rice, quinoa, oats, and whole wheat bread to provide sustained energy and fiber without overloading the liver.
- Avoid Alcohol and Caffeine: Alcohol should be completely avoided as it can worsen liver damage. Limit caffeine intake as excessive amounts can stress the liver.
- Small, Frequent Meals: Opt for smaller, more frequent meals throughout the day to aid digestion and prevent overloading the liver with large amounts of food at once.
Additionally, it’s crucial to tailor the diet plan to the individual’s specific condition and medical advice from healthcare providers. Regular monitoring of liver function tests and adjustments to the diet may be necessary based on the patient’s progress and recovery.
🔸4 Food preservation
Canning: This method involves heating food in sealed containers (jars or cans) to destroy microorganisms and enzymes that cause spoilage. It’s commonly used for fruits, vegetables, and meats.
- Freezing: Freezing food at low temperatures (-18°C or below) slows down microbial growth and enzymatic reactions. It preserves the quality of foods like meats, fish, vegetables, and fruits for several months.
- Drying or Dehydration: Removing moisture from foods inhibits the growth of bacteria, yeasts, and molds. Dried foods include fruits, vegetables, herbs, and meats, often achieved through sun drying, air drying, or using dehydrators.
- Pickling: Immersing food in a solution of vinegar, salt, and spices creates an acidic environment that preserves food by inhibiting microbial growth. Pickled foods include cucumbers (pickles), cabbage (sauerkraut), and other vegetables.
- Salting: Coating or immersing food in salt draws out moisture, which inhibits microbial growth and enzyme activity. Salted foods include fish (salted fish), meats (salted pork or beef), and vegetables (fermented or salted vegetables).
- Fermentation: This process involves the use of beneficial microorganisms (like bacteria or yeast) to convert sugars and starches in food into acids or alcohol, creating an inhospitable environment for harmful bacteria. Fermented foods include yogurt, sauerkraut, kimchi, and some cheeses.
⏩Q.6 Briefly Answer the following (Compulsory) (1×5=05)
🔸1 Community nutrition training
Community nutrition training involves educating individuals and groups within a community on the principles of nutrition, healthy eating habits, and lifestyle choices that promote overall well-being. This type of training is often aimed at improving public health, preventing chronic diseases, and addressing specific nutritional needs within the community.
- Nutritional Education:
- Basics of macronutrients (proteins, carbohydrates, fats) and micronutrients (vitamins, minerals).
- Understanding food labels and nutritional information.
- Importance of a balanced diet and portion control.
- Healthy Eating Habits:
- Meal planning and preparation.
- Incorporating more fruits, vegetables, and whole grains into the diet.
- Reducing intake of processed foods, sugar, and unhealthy fats.
- Special Nutritional Needs:
- Addressing the dietary requirements of different age groups (children, adolescents, adults, and the elderly).
- Managing specific health conditions through diet (e.g., diabetes, hypertension, obesity).
- Cultural and socioeconomic considerations in dietary choices.
- Food Safety and Hygiene:
- Proper food handling and storage techniques.
- Avoiding foodborne illnesses.
- Importance of clean water and sanitation in food preparation.
- Community Engagement:
- Organizing workshops, seminars, and cooking demonstrations.
- Collaborating with local health organizations, schools, and community centers.
- Promoting community gardens and local food production.
- Behavior Change Strategies:
- Motivational interviewing and counseling techniques.
- Setting realistic goals and tracking progress.
- Providing support and resources for sustainable behavior change.
Benefits of Community Nutrition Training
- Improved Public Health: Reduces the prevalence of nutrition-related diseases such as obesity, diabetes, and cardiovascular diseases.
- Empowerment: Equips community members with the knowledge and skills to make healthier food choices.
- Economic Benefits: Can lead to reduced healthcare costs and improved productivity.
- Social Benefits: Strengthens community bonds through shared activities and common goals.
Implementation Strategies
- Needs Assessment: Identify the specific nutritional challenges and needs of the community.
- Curriculum Development: Design a training program that is culturally relevant and tailored to the community’s needs.
- Training the Trainers: Educate local leaders, health workers, and volunteers who can then disseminate information within the community.
- Resource Development: Create educational materials such as pamphlets, posters, and online resources.
- Monitoring and Evaluation: Track the effectiveness of the training program and make necessary adjustments.
Community nutrition training is a collaborative effort that requires the involvement of various stakeholders, including healthcare providers, educators, local government, and community members themselves. By promoting nutritional literacy and healthy behaviors, such programs can significantly enhance the quality of life within communities.
🔸2 Special nutrition programme
ndia has implemented several special nutrition programs to address the diverse nutritional needs of its population, particularly among vulnerable groups such as children, pregnant women, and lactating mothers. These programs aim to combat malnutrition, anemia, and other nutrition-related health issues
1. Integrated Child Development Services (ICDS)
- Objective: To provide supplementary nutrition, health check-ups, immunization, and pre-school education to children under six years of age, as well as to pregnant women and lactating mothers.
- Components:
- Supplementary nutrition
- Non-formal pre-school education
- Nutrition and health education
- Immunization
- Health check-ups
- Referral services
2. Mid-Day Meal Scheme (MDM)
- Objective: To enhance the nutritional status of school children by providing them with a hot cooked meal during school hours.
- Target Group: Children studying in government and government-aided primary and upper primary schools.
- Components:
- Provision of nutritious meals to school children
- Promotion of school attendance and retention
- Improvement in nutritional levels among children
3. National Nutrition Mission (POSHAN Abhiyaan)
- Objective: To reduce the levels of stunting, undernutrition, anemia, and low birth weight among children and women.
- Key Strategies:
- Convergence of various nutrition programs
- Real-time monitoring and targeted interventions
- Use of technology for efficient service delivery
- Community-based events and behavior change communication
4. Pradhan Mantri Matru Vandana Yojana (PMMVY)
- Objective: To provide partial wage compensation to pregnant and lactating women for wage loss during childbirth and childcare.
- Components:
- Cash incentives for pregnant and lactating women
- Encouragement for institutional deliveries
- Promotion of exclusive breastfeeding and infant nutrition
5. Anemia Mukt Bharat (AMB)
- Objective: To reduce the prevalence of anemia among children, adolescents, and women of reproductive age.
- Components:
- Iron and folic acid supplementation
- Deworming
- Intensified health and nutrition education
- Testing and treatment of anemia at all levels
6. Pradhan Mantri Garib Kalyan Anna Yojana (PMGKAY)
- Objective: To provide additional food security to vulnerable populations during emergencies, such as the COVID-19 pandemic.
- Components:
- Free distribution of food grains (rice/wheat) to eligible households
- Ensuring food security for economically disadvantaged groups
7. National Food Security Act (NFSA)
- Objective: To provide subsidized food grains to approximately two-thirds of India’s population.
- Components:
- Distribution of rice, wheat, and coarse grains at highly subsidized prices
- Special focus on pregnant women, lactating mothers, and children
8. MGNREGA and Nutrition
- Objective: To enhance livelihood security and ensure improved nutrition through employment generation.
- Components:
- Provision of 100 days of wage employment to rural households
- Promotion of food security through increased purchasing power
Impact and Challenges
Impact:
- Significant improvements in child health and nutrition indicators.
- Enhanced school attendance and retention through the Mid-Day Meal Scheme.
- Reduced levels of stunting and undernutrition in targeted populations.
Challenges:
- Ensuring effective implementation and monitoring at the grassroots level.
- Addressing gaps in service delivery and infrastructure.
- Overcoming socio-cultural barriers to nutrition and health practices.
- Achieving inter-sectoral convergence for comprehensive nutrition strategies.
India’s special nutrition programs play a crucial role in addressing the multifaceted issue of malnutrition and improving the overall health and well-being of its population. Continued efforts and innovations are needed to sustain and amplify the progress made so far.
🔸3 Road to health chart
Monitoring Growth: It tracks a child’s weight, height, and head circumference over time to ensure they are developing properly.
- Key Developmental Milestones: It includes milestones such as sitting, crawling, and walking to assess motor skills.
- Immunization Schedule: The chart also includes sections to record vaccinations, ensuring children receive necessary immunizations.
- Parent Education: It serves as a tool for educating parents on child health, nutrition, and developmental milestones.
🔸4 Weaning
Weaning is the process of gradually introducing a baby to solid foods while reducing their dependency on breast milk or formula. It typically starts around six months of age and involves introducing new tastes and textures to meet the baby’s nutritional needs and support their growth and development.
1.Timing: It usually begins around six months when babies show signs of readiness, such as sitting up and showing interest in food.
2-Introduction of Foods: Initially, soft, pureed foods are introduced, followed by mashed and finely chopped foods as the baby progresses.
🔸5 Intolerance of feeding
Symptoms: Common signs include vomiting, diarrhea, bloating, excessive gas, fussiness, or refusal to feed.
- Causes: It can be due to various reasons such as allergies, sensitivities to certain foods or ingredients, digestive disorders, or immature digestive systems in infants.
- Management: Addressing feeding intolerance involves identifying triggers through elimination diets (for breastfeeding mothers), switching formulas (for formula-fed babies), or adjusting feeding schedules.
- Medical Advice: Consulting a pediatrician is crucial to diagnose and manage feeding intolerance effectively, ensuring the baby receives proper nutrition and comfort.