FIRST YEAR B.SC. NURSING-Anatomy & Physiology-August-2023-(MODIFY PENDING)-UPLOAD PAPER NO.7
PAPER SOLUTION NO.7
Anatomy & Physiology-August-2023
⏩ SECTION-1 ⏪
⏩Q.1 Long essay type. (Any One) 10
🔸1.Define gland & explain its classifcation with diagram [2+8]
ANSWER:-

Definition of a Gland:
A gland is a specialized organ or group of cells within the body that produces and secretes substances such as hormones, enzymes, or other fluids. These secretions are vital for various physiological processes and maintaining homeostasis. Glands can release their products either directly into the bloodstream or into ducts, depending on their function and type.
Classification of Glands
Glands are classified primarily based on how they release their secretions and the nature of their secretions. The two main categories are exocrine glands and endocrine glands
- Exocrine Glands Exocrine glands release their secretions through ducts either to the surface of an organ or directly to the external environment. They are involved in processes like digestion, lubrication, and cooling of the body. A. Classification by Method Office Secretion:
1.Merocrine (Eccrine) Glands
Mechanism
Secrete their products via exocytosis without losing any part of the cell.
Examples
Sweat glands, salivary glands.
Function
Regulate temperature through sweat, facilitate digestion with saliva.
2.Apocrine Glands
Mechanism
Part of the cell membrane pinches off along with the secretion.
Examples
Mammary glands, some sweat glands in the armpits and groin.
Function
Produce milk, release scent markers or pheromones.
3.Holocrine Glands
Mechanism
The entire cell disintegrates to release its secretions.
Examples Sebaceous (oil) glands in the skin.
Function
Produce oils that lubricate and protect the skin and hair.
B. Classification by Structure:
1.Unicellular Glands
Description
Single-celled glands.
Examples
Goblet cells in the intestines and respiratory tract.
Function
Secrete mucus to protect and lubricate surfaces.
2.Multicellular Glands
Description Composed of multiple cells forming a glandular structure.
Examples
Most exocrine glands, such as the salivary and pancreatic glands.
Function
Secrete various substances needed for bodily functions.
3 Simple Glands
Description
Glands with unbranched ducts.
Examples
Simple tubular glands (intestinal glands).
Function Secrete digestive enzymes or mucus.
4.Compound Glands
Description
Glands with branched ducts.
Examples
Compound acinar glands (mammary glands).
Function
Produce more complex secretions like milk.
Endocrine Glands Endocrine glands are ductless and secrete hormones directly into the bloodstream. These hormones regulate various physiological activities and maintain homeostasis. A. Major Endocrine Glands and Their Functions:
1.Pituitary Gland
Location
Base of the brain.
Function
Often referred to as the “master gland” because it regulates other endocrine glands; produces hormones that control growth, metabolism, and reproductive processes.
2.Thyroid Gland
Location
Front of the neck.
Function Produces thyroid hormones that regulate metabolism, energy levels, and growth.
3.Parathyroid Glands
Location
Behind the thyroid gland.
Function
Regulate calcium levels in the blood.
4.Adrenal Glands
Location
On top of the kidneys.
Function
Produce hormones like adrenaline and cortisol, which help in stress response and regulate metabolism and blood pressure.
5.Pancreas (Endocrine function):
Location
Behind the stomach.
Function Produces insulin and glucagon to regulate blood sugar levels.
6.Pineal Gland
Location
Center of the brain.
Function Produces melatonin, which regulates sleep patterns.
7.Gonads (Ovaries and Testes)
Location Ovaries in females (pelvis); testes in males (scrotum).
Function Produce sex hormones (estrogen, progesterone in females; testosterone in males) that regulate reproductive functions and secondary sexual characteristics.
8.Thymus
Location
Upper chest.
Function
Produces thymosins which are involved in the development of the immune system.
Summary
1.Exocrine Glands
Secrete into ducts; classified by secretion method (merocrine, apocrine, holocrine) and structure (unicellular, multicellular, simple, compound).
2.Endocrine Glands
Secrete hormones directly into the bloodstream; regulate various bodily functions and maintain homeostasis.
Each type of gland plays a crucial role in the body’s physiological processes, ensuring the proper functioning and maintenance of health.
🔸2.Define respiratory system & explain its organs with diagram [2+8]
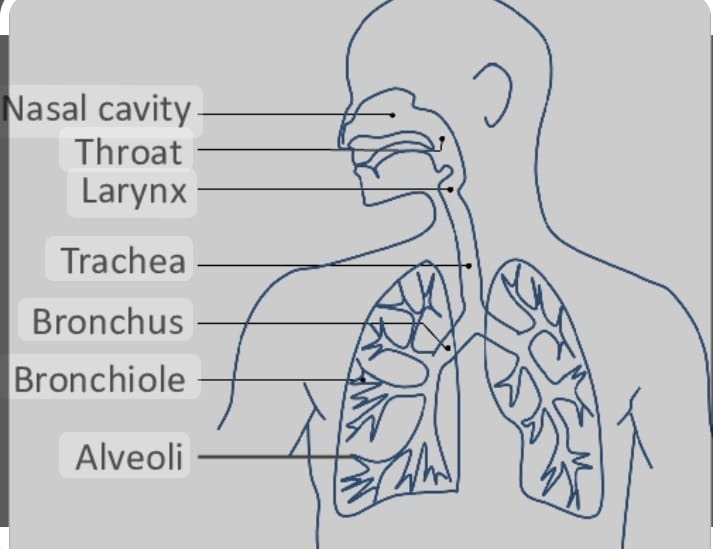
Definition:
The respiratory system is a biological system consisting of specific organs and structures used for gas exchange in animals and humans. Its primary function is to take in oxygen from the air and expel carbon dioxide from the body. This process is vital for cellular respiration, which generates the energy necessary for various physiological processes.
Functions of the Respiratory System:
Gas Exchange:
Provides oxygen to the blood and removes carbon dioxide.
Regulation of Blood pH:
Helps maintain acid-base balance.
Protection:
Filters out pathogens and particulates from inhaled air.
Sound Production:
Involves vocal cords for speaking.
Olfaction:
Facilitates the sense of smell through the nasal passages.
Organs of the Respiratory System:
The respiratory system includes several organs and structures, each playing a critical role in the process of respiration.
Nose and Nasal Cavity:
Function:
The primary entry point for outside air. It filters, warms, and moistens the air. The nasal cavity contains hair and mucus to trap particles and pathogens.
Pharynx (Throat):
Function:
A muscular tube that serves as a passageway for air moving from the nasal cavity to the larynx and for food moving from the mouth to the esophagus.
Larynx (Voice Box):
Function:
Located below the pharynx, the larynx houses the vocal cords and is responsible for sound production. It also acts as a switching mechanism to direct air and food into the proper channels.
Trachea (Windpipe):
Function:
A tubular structure that provides a clear air passage to the lungs. It is lined with cilia and mucus to trap and expel foreign particles.
Bronchi and Bronchioles:Function:
The trachea divides into two main bronchi, each entering a lung. These further subdivide into smaller bronchi and bronchioles, spreading throughout the lungs. They conduct air to the alveoli and have a role in filtering and warming the air.
Lungs: Function: The main organs of respiration, where gas exchange occurs. Each lung contains millions of alveoli (tiny air sacs) that facilitate the exchange of oxygen and carbon dioxide with the blood.
Alveoli: Function:
Small, balloon-like structures at the end of bronchioles where the actual gas exchange takes place. Oxygen diffuses into the blood, and carbon dioxide diffuses out to be exhaled.
Diaphragm: Function: A large, dome-shaped muscle located at the base of the lungs. It contracts and flattens during inhalation, expanding the chest cavity and allowing air to enter the lungs. It relaxes during exhalation, pushing air out
⏩Q.2 Write short notes on following. (Any Four) (20)
🔸1.Anatomy of urinary bladder
Anatomy of the Urinary Bladder
The urinary bladder is a hollow, muscular organ that stores urine produced by the kidneys before it is excreted from the body through the urethra. It is a crucial part of the urinary system and plays a key role in the regulation and elimination of bodily waste.
Structure of the Urinary Bladder:
1.Location
In males, the bladder is situated in the pelvis, just behind the pubic bone and in front of the rectum.
In females, it is located in front of the uterus and above the vagina.
2.Shape and Size
The shape of the bladder is roughly spherical when full and somewhat flattened when empty.
The size can vary, but a typical adult bladder can hold between 400 to 600 milliliters of urine.
3.Layers of the Bladder Wall
The bladder wall is composed of several layers, each with distinct functions:
Mucosa
The innermost layer lined with transitional epithelium (urothelium), which allows the bladder to stretch and expand as it fills with urine.
The mucosa also includes a layer of mucus that protects the bladder lining from the potentially harmful effects of urine.
Submucosa
A supportive layer of connective tissue beneath the mucosa, providing structural support and containing blood vessels and nerves.
Detrusor Muscle
A thick, muscular layer made up of smooth muscle fibers arranged in a crisscross pattern.
This muscle is responsible for contracting to expel urine during urination and relaxing to allow the bladder to fill.
Adventitia/Serosa
The outermost layer of the bladder.
The adventitia is a loose connective tissue that anchors the bladder to surrounding structures in the pelvis.
In some parts of the bladder, particularly the superior surface, it is covered by a serous membrane derived from the peritoneum, known as the serosa.
4 Key Features
Trigone
A triangular area on the floor of the bladder, bounded by the openings of the two ureters (which bring urine from the kidneys) and the internal urethral orifice (where urine exits the bladder into the urethra).
The trigone is relatively smooth and less distensible compared to the rest of the bladder wall and serves as a funnel for urine flow into the urethra.
Internal Urethral Sphincter
A ring of smooth muscle located at the junction of the bladder and the urethra.
It controls the release of urine from the bladder into the urethra and maintains continence.
External Urethral Sphincter
A voluntary skeletal muscle located further down the urethra.
It provides additional control over urination and is part of the pelvic floor muscles.
Summary of Function:
Storage
The bladder stores urine until a sufficient volume is reached, triggering the sensation to urinate.
Urination
During urination, the detrusor muscle contracts, and the internal and external urethral sphincters relax, allowing urine to flow out through the urethra.
Clinical Relevance:
Understanding the anatomy of the bladder is crucial for diagnosing and treating various conditions, such as urinary tract infections (UTIs), bladder stones, incontinence, and bladder cancer. The bladder’s ability to store and expel urine efficiently is essential for maintaining overall health and homeostasis in the body.
🔸2.Anatomy of ear
Anatomy of the Ear
The ear is a complex organ responsible for hearing and maintaining balance. It can be divided into three main sections:
1) the outer ear, 2)middle ear, and 3)inner ear, each playing a distinct role in the auditory and vestibular systems.
Outer Ear
The outer ear collects and directs sound waves toward the inner parts of the ear. Pinna (Auricle):
The visible part of the ear made of cartilage and skin.It helps capture sound waves and directs them into the ear canal.Features include the helix (outer rim), antihelix, lobule (earlobe), tragus, and antitragus.
External Auditory Canal (Ear Canal):
A tube-like structure that extends from the pinna to the eardrum (tympanic membrane).It channels sound waves inward and contains glands that produce earwax (cerumen) to protect the ear from dust and microorganisms.
Tympanic Membrane (Eardrum):
A thin, cone-shaped membrane that separates the outer ear from the middle ear.It vibrates in response to sound waves, transmitting these vibrations to the ossicles in the middle ear.
Middle Ear
The middle ear amplifies sound vibrations and transmits them to the inner ear.
Ossicles:
Three tiny bones that form a chain linking the eardrum to the inner ear. They are the smallest bones in the human body.
Malleus (Hammer):
Attached to the eardrum and articulates with the incus.
Incus (Anvil):
Located between the malleus and the stapes, it transmits vibrations from the malleus to the stapes.
Stapes (Stirrup):
The smallest bone, it fits into the oval window of the cochlea and transmits vibrations to the inner ear fluids.
Eustachian Tube:
A narrow tube connecting the middle ear to the throat (nasopharynx).It equalizes air pressure on both sides of the eardrum, ensuring proper vibration.
3.Inner Ear
The inner ear converts sound vibrations into electrical signals and is essential for balance. Cochlea:
A spiral-shaped, fluid-filled structure that transforms sound vibrations into nerve impulses.It contains the organ of Corti, the sensory receptor for hearing, with hair cells that convert mechanical vibrations into electrical signals sent to the brain via the auditory nerve.
Vestibule:
The central part of the inner ear, located between the cochlea and semicircular canals.It contains the utricle and saccule, which detect linear movements and head position relative to gravity.
Semicircular Canals:
Three loop-shaped structures oriented at right angles to each other.They contain fluid and hair cells that detect rotational movements of the head, helping maintain balance and spatial orientation.
Ear Function:
Hearing:
Sound waves are collected by the outer ear, transmitted through the middle ear, and converted into electrical signals in the inner ear, which are then interpreted by the brain as sound.
Balance:
The vestibule and semicircular canals in the inner ear detect head movements and help maintain balance and spatial orientation.
🔸3.Anatomy of skin
Anatomy of the Skin
The skin is the largest organ of the body, serving as a protective barrier between the internal environment and the external world. It has multiple layers and structures that contribute to its various functions, including protection, sensation, temperature regulation, and more.
Layers of the Skin
The skin consists of three primary layers:
the epidermis, dermis, and hypodermis (subcutaneous layer).
1.Epidermis
Function
The outermost layer provides a waterproof barrier and creates our skin tone.
Structure
Composed primarily of keratinocytes, which produce keratin, a protein that gives the skin its strength and resilience. It also includes melanocytes (pigment-producing cells), Langerhans cells (immune cells), and Merkel cells (sensory receptors).
Sub-layers
Stratum Corneum
The outermost layer, consisting of dead, flattened keratinocytes. This layer continually sheds and renews, providing a barrier against pathogens and environmental damage.
Stratum Lucidum
A thin, clear layer found only in thick skin areas like the palms and soles. It adds an extra layer of protection.
Stratum Granulosum
Cells in this layer begin to flatten and die, accumulating granules of keratin and lipids that contribute to the skin’s waterproof properties.
Stratum Spinosum
Known for its spiny appearance due to the desmosomes (cell connections), this layer provides strength and flexibility.
Stratum Basale (Stratum Germinativum)
The deepest layer, where new keratinocytes are generated. This layer also contains melanocytes and Merkel cells.
2.Dermis
Function
Provides structural support and flexibility. It houses blood vessels, nerves, glands, and hair follicles.
Structure
Made up of connective tissue containing collagen and elastin fibers, which give the skin its strength and elasticity.
Sub-layers
Papillary Dermis
The upper layer containing thin collagen fibers and finger-like projections (dermal papillae) that interlock with the epidermis, enhancing the surface area for nutrient exchange and contributing to fingerprints.
Reticular Dermis
The deeper and thicker layer, composed of dense irregular connective tissue with larger collagen bundles. It contains sweat glands, sebaceous (oil) glands, and deep pressure receptors (Pacinian corpuscles).
3.Hypodermis (Subcutaneous Layer)
Function
Provides insulation, cushioning, and energy storage. It anchors the skin to underlying tissues like muscles and bones.
Structure
Consists mainly of adipose tissue (fat cells) and loose connective tissue. This layer varies in thickness depending on body location and individual factors.
Associated Structures in the Skin:
1.Hair Follicles
Location
Extend from the surface into the dermis and sometimes into the hypodermis.
Function
Produce hair, which helps in temperature regulation and provides sensory input.
Structure
Consists of the hair bulb (where hair growth begins), hair root, and hair shaft (the visible part).
2.Sweat Glands
Location
Found in the dermis.
Function
Help regulate body temperature through sweat production and excrete waste products.
Types
Eccrine Glands
Distributed widely across the skin surface, especially on the palms, soles, and forehead. They produce a watery sweat.
Apocrine Glands
Located mainly in the axillary (armpit) and groin areas. They produce a thicker sweat that can lead to body odor when broken down by bacteria.
3.Sebaceous Glands
Location
Found throughout the skin, except on the palms and soles, and often associated with hair follicles.
Function Secrete sebum, an oily substance that lubricates and waterproofs the skin and hair.
4.Nails
Location
Present at the tips of fingers and toes.
Function
Protect the distal phalanx and enhance fine touch and manipulation.
Structure Composed of hard keratin, nails grow from the nail matrix located under the base of the nail.
5.Nerve Endings
Location
Distributed throughout the skin.
Function
Provide sensory input for touch, temperature, pain, and pressure.
Types
Include free nerve endings (pain and temperature), Meissner’s corpuscles (light touch), and Pacinian corpuscles (deep pressure).
Summary of Skin Functions:
Protection
Shields underlying tissues from mechanical damage, pathogens, and UV radiation.
Sensation
Contains receptors for touch, pain, temperature, and pressure.
Thermoregulation Regulates body temperature through sweat production and blood vessel dilation or constriction.
Excretion
Removes waste products through sweat.
Vitamin D Synthesis
Synthesizes vitamin D upon exposure to UV light.
Immunity
Provides a barrier to pathogens and hosts immune cells like Langerhans cells.
🔸4.Microscopic structure of bone
Bone tissue, or osseous tissue, is a dynamic and complex type of connective tissue that forms the rigid part of the bones. It supports and protects the body’s various organs, enables movement, stores minerals, and houses bone marrow. The microscopic structure of bone is intricate, involving a network of cells, matrix, and mineral deposits that provide both strength and flexibility.
Key Components of Bone Tissue:
1.Bone Cells
Osteoblasts
Bone-forming cells that produce and secrete the bone matrix, including collagen and other organic components. They eventually become embedded in the matrix they produce and mature into osteocytes.
Osteocytes
Mature bone cells that maintain the bone matrix and communicate with other bone cells to direct remodeling and repair. They reside in small cavities called lacunae within the bone matrix.
Osteoclasts
Large, multinucleated cells responsible for bone resorption (the breakdown of bone tissue). They release enzymes and acids that dissolve the mineral component of the bone, facilitating its remodeling and calcium release into the bloodstream.
Osteoprogenitor Cells
Stem cells found in the periosteum and endosteum that differentiate into osteoblasts and play a role in bone growth and repair.
2.Bone Matrix
Organic Component (Osteoid)
Composed mainly of collagen fibers and ground substance, which provide tensile strength and flexibility.
Inorganic Component
Primarily composed of hydroxyapatite crystals (calcium phosphate), which give bone its hardness and ability to resist compression.
3.Bone Structure
Compact Bone
Dense and forms the outer layer of bones, providing strength and support.
Spongy (Cancellous) Bone
Lighter, less dense, and found mainly at the ends of long bones and in the interiors of other bones. It contains trabeculae, a network of bony spicules that support bone marrow.
Microscopic Features of Compact Bone:
1.Osteon (Haversian System)
The fundamental functional unit of compact bone.
Each osteon consists of concentric layers, or lamellae, of calcified matrix arranged around a central canal (Haversian canal).
2.Haversian Canal
Located at the center of each osteon.
Contains blood vessels and nerves that supply nutrients and remove waste from the bone cells.
3.Lamellae
Rings of calcified matrix surrounding the Haversian canal.
Each lamella is made up of collagen fibers arranged in different directions in adjacent layers, which helps resist torsional (twisting) forces.
4.Lacunae
Small cavities between the lamellae.
House the osteocytes.
5.Canaliculi
Tiny channels radiating from the lacunae.
They connect lacunae to each other and to the Haversian canal, allowing for nutrient and waste exchange between osteocytes.
6.Volkmann’s Canals
Transverse or oblique channels that connect adjacent Haversian canals.
They also carry blood vessels and nerves from the periosteum into the deeper layers of the bone.
Microscopic Features of Spongy Bone:
1.Trabeculae
Thin, bony plates or spicules that form a lattice-like network within spongy bone.
They align along lines of stress, providing structural support and strength with minimal weight.
Spaces between trabeculae are filled with bone marrow and blood vessels, facilitating the exchange of nutrients.
2.Bone Marrow
Located in the cavities of spongy bone.
Red marrow is involved in blood cell production, while yellow marrow stores fat.
Summary:
Compact Bone
Characterized by osteons, dense and structured to provide strength and resistance to stress.
Spongy Bone
Made up of trabeculae, lighter and structured to support the bone marrow and facilitate metabolic exchange.
🔸5.Structure of stomach
Structure of the Stomach
The stomach is a crucial organ in the digestive system, responsible for the mechanical and chemical breakdown of food. It acts as a temporary storage and mixing chamber for ingested food, transforming it into a semi-liquid substance called chyme before it moves into the small intestine.
Anatomy of the Stomach:
1.Location
The stomach is located in the upper left part of the abdominal cavity, just below the diaphragm. It lies between the esophagus and the small intestine (duodenum).
2 Shape
The stomach is a J-shaped organ, which can vary in size and shape depending on the body’s position and the amount of food ingested.
3.Main Regions
Cardia
The region where the esophagus connects to the stomach. It contains the lower esophageal sphincter (LES), which prevents the backflow of stomach contents into the esophagus.
Fundus
The dome-shaped upper part of the stomach, located to the left of the cardia. It often contains a gas bubble.
Body (Corpus)
The central, largest region of the stomach. It acts as the main site for mixing and enzymatic digestion.
Pylorus
The lower section of the stomach that connects to the duodenum. It includes the pyloric antrum and the pyloric canal, ending at the pyloric sphincter, which regulates the passage of chyme into the small intestine.
4.Curvatures
Greater Curvature
The long, convex curve on the left side of the stomach.
Lesser Curvature
The shorter, concave curve on the right side of the stomach.
5.Muscle Layers
The stomach wall contains three layers of smooth muscle, which facilitate the mechanical digestion of food by churning and mixing it with gastric juices:
Longitudinal Layer
The outermost layer with fibers running longitudinally along the stomach.
Circular Layer
The middle layer with fibers encircling the stomach.
Oblique Layer
The innermost layer with fibers running diagonally. This additional layer is unique to the stomach and enhances its churning action.
Microscopic Structure:
The stomach wall is composed of several layers, each playing a specific role in the digestive process:
1.Mucosa
The innermost layer, lined with a thick mucous membrane.
Contains gastric pits that lead to gastric glands, which secrete various components of gastric juice, including hydrochloric acid, pepsinogen, and mucus.
2.Submucosa
A supportive layer of connective tissue containing blood vessels, nerves, and lymphatics.
It provides the mucosa with nutrients and helps maintain its structure.
3.Muscularis Externa
Composed of the three layers of smooth muscle (longitudinal, circular, and oblique).
These layers are responsible for the peristaltic movements that mix and propel stomach contents.
4.Serosa
The outermost layer of the stomach.
It is a thin layer of connective tissue covered by the peritoneum, which reduces friction between the stomach and surrounding organs during digestive movements.
Functions of the Stomach:
1.Food Storage
The stomach acts as a temporary storage site, holding ingested food and releasing it gradually into the small intestine.
2.Mechanical Digestion
The smooth muscle layers of the stomach contract rhythmically to churn and mix food with gastric juices, enhancing the breakdown of food into smaller particles.
3.Chemical Digestion
Gastric glands in the mucosa secrete hydrochloric acid and enzymes (like pepsin) that break down proteins into smaller peptides.
The acidic environment also helps kill bacteria and pathogens ingested with food.
4.Protection
The mucous membrane secretes mucus that forms a protective barrier, preventing the acidic gastric juice from damaging the stomach lining.
5.Regulation of Emptying
The pyloric sphincter controls the passage of partially digested food (chyme) from the stomach into the duodenum, ensuring that digestion occurs at an optimal pace.
⏩Q.3 Fill in the blanks.(08)
🔸1.——–is the inner most layer of the epidermis. Stratum basale (also known as the stratum germinativum ) is the innermost layer of the epidermis.
🔸2.Total—— bones are in human skull. Total 22 bones are in the human skull.
🔸3.The longest muscle of the human body is—– The longest muscle of the human body is the sartorius.
🔸4.Life span of RBC is—— days. The life span of a red blood cell (RBC) is 120 days.
🔸5.The 7th cranial nerve is named as ——- The 7th cranial nerve is named the Facial Nerve.
🔸6.The pigment that is responsible for skin colour is——- The pigment that is responsible for skin color is melanin.
🔸7.——-are suicidal bags of cell. Lysosomes are referred to as the “suicidal bags” of the cell.
🔸8.Bile is produced by——- Bile is produced by the liver.
⏩SECTION-II⏪
⏩Q.4 Long essay type. (Any One)(10)
🔸1.Define Endocrine glands & describe the functions of Thymus gland in detail.
Endocrine glands
are specialized glands that release hormones directly into the bloodstream rather than through ducts. These hormones act as chemical messengers, traveling to various organs and tissues to regulate physiological processes, including growth, metabolism, reproduction, and mood. The major endocrine glands in the human body include the pituitary gland, thyroid gland, adrenal glands, pancreas, and gonads (ovaries and testes).
Thymus Gland: Functions in Detail
The thymus gland is a crucial component of the immune system and plays a significant role in the development of the body’s adaptive immune response. It is located in the upper part of the chest, just behind the sternum and between the lungs. The thymus is most active during childhood and adolescence, after which it gradually shrinks and is replaced by fat in a process called thymic involution.
Functions of the Thymus Gland:
1.T-Cell Maturation and Differentiation:
The primary function of the thymus is the maturation and differentiation of T-lymphocytes, or T-cells. T-cells are a type of white blood cell critical for the adaptive immune system.
Precursor cells, known as thymocytes, travel from the bone marrow to the thymus, where they undergo a rigorous selection process to become mature T-cells. This process ensures that T-cells are capable of recognizing and attacking foreign pathogens while being tolerant to the body’s own tissues.
2.Production of Thymic Hormones:
The thymus secretes several hormones, collectively called thymosins, which are crucial for T-cell development and function.
These hormones include:
Thymosin alpha 1:
Promotes T-cell differentiation and enhances immune responses.
– Thymopoietin:
Influences the development of T-cells and helps regulate the immune system.
Thymulin:
Enhances T-cell function and helps regulate the immune response.
3.Central Role in Immune System Development:
The thymus is essential during early life for the establishment of a fully functional immune system. Without a properly functioning thymus, the body cannot generate an effective population of T-cells, leading to severe immunodeficiency and increased susceptibility to infections.
During fetal development and early childhood, the thymus also helps establish immune tolerance, which prevents the immune system from attacking the body’s own cells (autoimmunity).
4.Thymic Education:
In the thymus, T-cells undergo a process called “positive selection” and “negative selection.” Positive selection ensures that T-cells can recognize major histocompatibility complex (MHC) molecules, which present antigens to T-cells. Negative selection eliminates T-cells that react strongly to self-antigens, thus preventing autoimmune reactions.
This education process ensures that the T-cell repertoire is both functional and self-tolerant, capable of responding to pathogens while ignoring the body’s own tissues.
5.Regulation of Immune Homeostasis:
The thymus helps maintain immune homeostasis by ensuring a balanced and diverse population of T-cells. It aids in the creation of various T-cell subsets, including helper T-cells, cytotoxic T-cells, and regulatory T-cells, each with specific roles in orchestrating and executing immune responses.
6.Role in Aging:
As the thymus involutes with age, its capacity to produce new T-cells diminishes, contributing to a decline in immune function in older adults. This decline is associated with an increased incidence of infections, cancer, and autoimmune diseases in the elderly.
🔸2.Define pancreas. Explain the functions of it in details
Pancreas: Definition and Detailed Functions
Pancreas
The pancreas is a vital glandular organ in the human body, playing dual roles in the digestive and endocrine systems. It is an elongated organ, approximately 15-20 centimeters long, located in the abdomen behind the stomach and nestled within the curve of the duodenum, the first part of the small intestine.
Functions of the Pancreas
The pancreas performs two primary functions: exocrine and endocrine.
- Exocrine Function The exocrine portion of the pancreas is responsible for producing digestive enzymes and bicarbonate, which are released into the small intestine to aid in digestion.
Components and Mechanisms
Acinar Cells
These cells produce and secrete digestive enzymes. They are organized into clusters called acini.
Pancreatic Duct
The enzymes produced by acinar cells are transported through the pancreatic duct into the duodenum. The main pancreatic duct often merges with the bile duct before entering the duodenum.
Key Digestive Enzymes
Amylase
Breaks down carbohydrates into simpler sugars.
Lipase
Digests fats into fatty acids and glycerol.
Proteases (e.g., Trypsin and Chymotrypsin)
Break down proteins into amino acids and small peptides.
Nucleases
Degrade nucleic acids into nucleotides.
Function in Digestion
These enzymes are crucial for the digestion of food, allowing the breakdown of complex macromolecules into absorbable units.
The pancreas also secretes bicarbonate, which neutralizes the acidic chyme (partially digested food) that enters the small intestine from the stomach, providing an optimal pH for enzyme activity.
2.Endocrine Function
The endocrine part of the pancreas involves the regulation of blood sugar levels through the secretion of hormones directly into the bloodstream.
Components
Islets of Langerhans
These are clusters of hormone-producing cells scattered throughout the pancreas. They contain different types of cells, each producing specific hormones.
Key Hormones
Insulin
Produced by beta cells, insulin lowers blood glucose levels by facilitating the uptake of glucose into cells for energy or storage as glycogen in the liver and muscles.
Glucagon
Produced by alpha cells, glucagon raises blood glucose levels by stimulating the liver to convert stored glycogen into glucose and release it into the bloodstream.
Somatostatin
Produced by delta cells, somatostatin regulates the secretion of other pancreatic hormones and slows down digestive processes to ensure a balanced nutrient absorption.
Pancreatic Polypeptide
Produced by PP cells (or F cells), this hormone helps regulate the exocrine and endocrine pancreatic secretions and influences the digestive process.
Function in Metabolism
The balance between insulin and glucagon secretion is crucial for maintaining stable blood glucose levels, which is essential for proper body function and energy management.
Dysregulation of these hormones can lead to metabolic disorders, such as diabetes mellitus, where insulin production or action is impaired, causing high blood glucose levels.
⏩Q.5 Write short notes on following. (Any Four) (20 MARKS)
🔸1.Portal blood circulation
Portal Blood Circulation
Portal blood circulation
refers to a unique vascular system where blood flows through two capillary beds before returning to the heart. The most notable example in humans is the
hepatic portal system which plays a crucial role in directing nutrient-rich blood from the gastrointestinal tract and spleen to the liver for processing and detoxification before it re-enters the general circulation.
Hepatic Portal System
Anatomy and Pathway
1.Capillary Beds in the Digestive Organs
Blood first passes through capillary beds in the digestive organs, including the stomach, intestines, pancreas, and spleen, where nutrients and other substances are absorbed.
2.Portal Vein Formation
The hepatic portal vein is formed by the convergence of several veins:
Superior Mesenteric Vein
Drains blood from the small intestine, parts of the large intestine, and stomach.
Inferior Mesenteric Vein
Drains blood from the lower part of the large intestine.
Splenic Vein
Drains blood from the spleen, stomach, and pancreas.
3.Portal Vein to Liver
The hepatic portal vein transports the nutrient-rich blood from the digestive organs to the liver. This vein delivers about 75% of the blood flow to the liver, the remaining 25% comes from the hepatic artery, which supplies oxygenated blood.
4.Liver Sinusoids
Within the liver, the portal vein branches into smaller vessels, leading to a second capillary network called sinusoids. These are specialized, fenestrated capillaries that allow for extensive exchange between the blood and liver cells (hepatocytes).
5.Processing in the Liver
The liver processes the blood, metabolizing nutrients, detoxifying harmful substances, and synthesizing essential proteins like albumin and clotting factors. It also stores glycogen and fat-soluble vitamins and converts excess glucose to glycogen.
6.Hepatic Veins
After processing, the blood collects in the central veins of the liver lobules and eventually drains into the hepatic veins.
The hepatic veins then transport the cleansed blood to the inferior vena cava, which returns it to the heart for systemic circulation.
Functions and Importance
1.Nutrient Metabolism
The liver processes nutrients absorbed from the digestive tract. It converts glucose into glycogen for storage, processes amino acids for protein synthesis, and manages lipids.
2.Detoxification
The liver detoxifies various metabolites and removes toxins from the blood, such as drugs, alcohol, and metabolic byproducts like ammonia.
3.Bilirubin Metabolism
The liver processes and excretes bilirubin, a byproduct of red blood cell breakdown, into bile. Impaired bilirubin clearance can lead to jaundice.
4.Synthesis of Plasma Proteins
The liver produces essential proteins for blood clotting and maintaining blood volume, such as fibrinogen, prothrombin, and albumin.
5.Immune Function
The liver contains Kupffer cells, specialized macrophages that filter out bacteria, old red blood cells, and other debris from the blood.
Clinical Relevance
1.Portal Hypertension
This is an increase in blood pressure within the portal venous system, often caused by liver cirrhosis or other liver diseases. It can lead to complications like varices (enlarged veins), ascites (fluid accumulation in the abdomen), and splenomegaly (enlarged spleen).
2.Liver Disease
Conditions such as hepatitis, fatty liver disease, and cirrhosis can impair the liver’s ability to process portal blood, leading to systemic metabolic disturbances and accumulation of toxins.
3.Portal Vein Thrombosis
This is the formation of a blood clot in the portal vein, which can obstruct blood flow and lead to ischemia or infarction of the liver and other organs.
🔸2.Functions of nephron
Functions of the Nephron
The nephron is the basic functional unit of the kidney, responsible for filtering blood and forming urine. Each kidney contains approximately one million nephrons, which work collectively to maintain fluid balance, electrolyte levels, and remove waste products from the body. The nephron performs its functions through a series of processes: filtration, reabsorption, secretion, and excretion.
Detailed Functions of the Nephron
1.Filtration
Location
Occurs in the glomerulus, a network of capillaries within the Bowman’s capsule.
Process
Blood enters the glomerulus under high pressure, causing water and small solutes (like ions, glucose, and waste products) to be filtered out of the blood and into the Bowman’s capsule. This filtered fluid is called the glomerular filtrate.
Components Filtered
Includes water, electrolytes (sodium, potassium, chloride), glucose, amino acids, and waste products (urea, creatinine).
Components Retained
Larger molecules, such as blood cells and plasma proteins, remain in the bloodstream because they are too large to pass through the filtration membrane.
2.Reabsorption
Location
Primarily in the proximal convoluted tubule (PCT), with further adjustments in the loop of Henle, distal convoluted tubule (DCT), and collecting duct.
Process
Essential substances filtered into the nephron are reabsorbed back into the bloodstream. This occurs via both passive and active transport mechanisms.
Key Substances Reabsorbed
Water
Reabsorbed through osmosis, especially in the descending limb of the loop of Henle and collecting duct under the influence of antidiuretic hormone (ADH).
Glucose and Amino Acids
Reabsorbed almost completely in the PCT.
Ions
Sodium, potassium, calcium, bicarbonate, and chloride ions are selectively reabsorbed to maintain electrolyte balance and pH.
Function
Reabsorption helps conserve necessary substances and maintain fluid and electrolyte balance in the body.
3.Secretion
Location
Primarily occurs in the proximal convoluted tubule (PCT) and distal convoluted tubule (DCT), and to some extent in the collecting duct.
Process
Additional waste products and excess ions are actively transported from the blood into the tubular fluid. This process helps fine-tune the composition of the filtrate.
Key Substances Secreted
Hydrogen Ions (H+)
Secreted to help regulate blood pH.
Potassium Ions (K+)
Secreted in exchange for sodium, especially under the influence of aldosterone.
Drugs and Toxins
Many medications and metabolic waste products are secreted into the tubule for elimination.
Function
Secretion helps remove potentially harmful substances and maintains acid-base and electrolyte balance.
4.Excretion
Location
Final processing occurs in the collecting ducts, leading to the formation of urine.
Process
The fluid remaining in the nephron after filtration, reabsorption, and secretion is termed urine. It collects in the renal pelvis and is transported to the bladder via the ureters for storage before being expelled from the body.
Composition of Urine
Contains water, urea, creatinine, ammonia, and various ions and waste products.
Function
Excretion is the final step in removing waste and excess substances from the body, maintaining internal balance and homeostasis.
🔸3.Regulation of body temperature.
Regulation of Body Temperature
The regulation of body temperature, or thermoregulation, is a crucial physiological process that maintains the body’s core temperature within a narrow, optimal range, despite varying external conditions. This is essential for the proper functioning of metabolic processes and enzyme activity. The average human body temperature is around 37°C (98.6°F), though it can vary slightly among individuals.
Mechanisms of Thermoregulation
Thermoregulation is achieved through complex interactions between the nervous, endocrine, and cardiovascular systems, involving various physiological responses and behaviors. Key components and mechanisms involved include:
1.Central Thermoregulatory Control: Hypothalamus
The hypothalamus, located in the brain, acts as the body’s thermostat.
It receives input from thermoreceptors located throughout the body, including the skin and internal organs.
Based on this information, the hypothalamus initiates appropriate responses to either increase or decrease body temperature.
2.Heat Production (Thermogenesis)
Metabolic Heat Production
Basal metabolic processes generate heat as a byproduct. This is the primary source of heat at rest.
Muscle Activity
Physical activity increases heat production. Shivering, an involuntary muscle contraction, generates heat when the body is cold.
Non-Shivering Thermogenesis
In brown adipose tissue, the process of breaking down fat generates heat. This is more prominent in infants and hibernating animals.
3.Heat Loss Mechanisms
Radiation
Loss of heat in the form of infrared rays. This is significant when the surrounding environment is cooler than the body.
Conduction
Direct transfer of heat through physical contact with cooler surfaces.
Convection
Transfer of heat by moving air or water currents around the body. This is enhanced by wind or water flow.
Evaporation
Heat loss through the conversion of water (sweat) to vapor. This is especially effective in cooling during high temperatures or physical exertion.
4.Behavioral Responses
Seeking Warmth or Coolness
Moving to a warmer or cooler environment, wearing appropriate clothing, or using heating or cooling devices.
Adjusting Physical Activity
Increasing or decreasing activity levels to influence heat production.
Postural Changes
Reducing or increasing surface area exposure, like curling up when cold or spreading out when hot.
Physiological Responses to Temperature Changes
1.Responses to Cold
Vasoconstriction:
Narrowing of blood vessels near the skin surface reduces blood flow to the skin, minimizing heat loss.
Shivering
Involuntary muscle contractions generate heat.
Increased Metabolism
Thyroid hormones and catecholamines (like adrenaline) can increase metabolic rate, enhancing heat production.
Behavioral Adjustments
Seeking shelter, adding layers of clothing, or consuming warm foods and drinks.
2.Responses to Heat
Vasodilation
Widening of blood vessels near the skin surface increases blood flow, promoting heat loss through radiation and convection.
Sweating
Evaporation of sweat from the skin surface effectively cools the body.
Reduced Physical Activity
Decreasing activity levels to minimize additional heat production.
Behavioral Adjustments
Seeking shade, removing excess clothing, or consuming cold foods and drinks.
Hormonal Regulation
1.Thyroid Hormones
Thyroid hormones (T3 and T4) increase the basal metabolic rate, influencing overall heat production.
Elevated thyroid hormone levels, as seen in hyperthyroidism, can raise body temperature, while low levels in hypothyroidism can lead to a lower body temperature.
2.Catecholamines
Hormones like adrenaline and noradrenaline increase metabolic rate and promote heat production, especially during stress or physical activity.
3.Antidiuretic Hormone (ADH) and Aldosterone
These hormones help conserve water, which is crucial for maintaining blood volume and ensuring efficient thermoregulation, particularly through sweating.
Fever and Thermoregulation
Fever
A controlled rise in body temperature in response to infection or inflammation. Pyrogens, substances released by pathogens or immune cells, reset the hypothalamic thermostat to a higher temperature.
This increase in set point stimulates heat production and retention mechanisms, like shivering and vasoconstriction, to elevate body temperature.
Once the infection is under control, the hypothalamus resets to normal, triggering heat loss mechanisms, such as sweating and vasodilation, to lower the body temperature back to baseline.
🔸4.Physiology of vision
Physiology of Vision
The physiology of vision involves the complex process through which light is detected and interpreted by the visual system to create meaningful images. This process encompasses the anatomy of the eye, the phototransduction mechanisms in the retina, and the neural pathways that transmit visual information to the brain.
Key Components of the Visual System
1.The Eye
The primary organ for capturing light and initiating the process of vision.
Cornea
The clear, dome-shaped front surface of the eye that refracts (bends) incoming light.
Lens
A transparent, flexible structure that fine-tunes the focus of light onto the retina by changing its shape (accommodation).
Iris and Pupil
The iris adjusts the size of the pupil, controlling the amount of light that enters the eye.
Aqueous and Vitreous Humors
Clear fluids that fill the anterior and posterior chambers of the eye, helping to maintain its shape and optical properties.
Retina
The light-sensitive layer at the back of the eye where photoreceptors (rods and cones) convert light into neural signals.
2.Photoreceptors
Specialized cells in the retina that detect light.
Rods
Highly sensitive to low light levels, responsible for night vision and peripheral vision. They do not detect color.
Cones
Function in bright light and are responsible for color vision and detailed central vision. There are three types of cones, each sensitive to different wavelengths of light (red, green, and blue).
3.Optic Nerve and Visual Pathways
Neural structures that transmit visual information from the retina to the brain.
Optic Nerve
Carries the electrical signals from the retina to the brain.
Optic Chiasm
The point where optic nerve fibers partially cross, allowing visual information from each eye to be processed by both hemispheres of the brain.
Optic Tracts
Pathways that relay visual information from the optic chiasm to the thalamus.
Lateral Geniculate Nucleus (LGN)
Part of the thalamus that processes visual information before it is relayed to the visual cortex.
Visual Cortex
The part of the brain located in the occipital lobe that processes and interprets visual signals.
Steps in the Physiology of Vision
1.Light Entry and Focusing
Light enters the eye through the cornea and passes through the aqueous humor, pupil, and lens.
The cornea and lens work together to refract and focus the light rays onto the retina, creating a sharp image.
2.Phototransduction in the Retina
Light Detection
When light hits the retina, it is absorbed by photopigments in the rods and cones. Each photopigment consists of a protein (opsin) and a light-sensitive molecule (retinal).
Chemical Changes
Light absorption causes the retinal to change shape, activating the opsin. This process, called isomerization, initiates a cascade of biochemical events.
Signal Generation
The biochemical cascade results in the closure of ion channels in the photoreceptor cell membrane, leading to a change in the cell’s electrical charge (hyperpolarization).
Signal Transmission
The change in electrical charge alters the release of neurotransmitters from the photoreceptors, modifying the activity of adjacent bipolar and ganglion cells in the retina.
3.Processing and Transmission
Retinal Circuitry
The modified activity of bipolar and ganglion cells creates a pattern of neural impulses. Horizontal and amacrine cells further refine these signals by integrating and modulating the input from multiple photoreceptors.
Optic Nerve
Ganglion cells’ axons converge to form the optic nerve, which carries the visual signals from the retina to the brain.
4.Visual Pathways to the Brain
Optic Chiasm and Optic Tracts
At the optic chiasm, fibers from the nasal halves of each retina cross to the opposite side, ensuring that visual information from each eye is processed by both hemispheres of the brain.
Lateral Geniculate Nucleus (LGN)
The optic tracts carry the signals to the LGN, which serves as a relay center and further processes the visual information.
Primary Visual Cortex (V1)
From the LGN, the visual signals are transmitted to the primary visual cortex in the occipital lobe, where basic features like orientation, motion, and color are analyzed.
5.Higher Visual Processing
Secondary Visual Areas
The primary visual cortex sends processed information to secondary visual areas (V2, V3, V4) and specialized regions responsible for interpreting complex aspects of the visual scene, such as depth, motion, and object recognition.
Integration and Perception
The visual information is integrated with other sensory inputs and cognitive processes to form a coherent and meaningful perception of the environment.
🔸5.Functions of stomach
Functions of the Stomach
The stomach is a key organ in the digestive system with several vital functions that contribute to the breakdown of food and preparation for nutrient absorption. It is a muscular, hollow organ located between the esophagus and the small intestine. Here’s an in-depth look at the primary functions of the stomach:
1.Storage of Food
The stomach acts as a temporary reservoir, allowing us to eat meals at intervals rather than continuously.
Its capacity to expand (up to about 1.5 liters) enables it to store a significant amount of food and liquid.
2.Mechanical Digestion
Peristalsis
The stomach’s muscular walls perform rhythmic contractions, mixing and churning the food with gastric juices to form a semi-liquid substance called chyme.
Grinding
The strong muscular movements help break down large food particles into smaller, more manageable pieces.
3.Chemical Digestion
Gastric Juices
The stomach secretes a mixture of enzymes and acids that contribute to the chemical breakdown of food.
Hydrochloric Acid (HCl)
Secreted by the parietal cells, it creates a highly acidic environment (pH 1.5 to 3.5) that denatures proteins and activates digestive enzymes.
Pepsinogen
Secreted by chief cells, it is converted into pepsin in the acidic environment, which then breaks down proteins into smaller peptides.
Intrinsic Factor Also produced by the parietal cells, it is essential for the absorption of vitamin B12 in the small intestine.
Mucus
Goblet cells secrete mucus that coats the stomach lining, protecting it from the corrosive effects of gastric acid and digestive enzymes.
4.Secretion of Hormones
The stomach produces several hormones that regulate digestive processes.
Gastrin
Stimulates the secretion of gastric acid and digestive enzymes, and promotes gastric motility.
Ghrelin
Often called the “hunger hormone,” it signals to the brain to stimulate appetite and increase food intake.
Somatostatin
Inhibits the release of gastric acid and slows down digestive processes, providing a regulatory feedback mechanism.
5.Absorption
Although the stomach is not a major site for nutrient absorption, it does absorb certain substances:
Water and Electrolytes
Small amounts are absorbed directly through the stomach lining.
Alcohol and Some Medications
These can be absorbed more rapidly in the stomach than in the intestines.
6.Protection
The stomach’s acidic environment acts as a barrier against pathogens and microorganisms that enter with food.
It helps prevent infections by killing or inhibiting the growth of harmful bacteria.
7.Regulation of Food Passage
The stomach controls the rate at which food is emptied into the small intestine.
The pyloric sphincter located at the junction between the stomach and the duodenum, regulates the release of chyme into the small intestine, ensuring that it occurs at a rate suitable for effective digestion and absorption in the intestines.
The stomach plays a multifaceted role in digestion. It stores and mixes food, initiates the breakdown of proteins, secretes essential digestive fluids, absorbs certain substances, protects against pathogens, and regulates the passage of food into the small intestine. These functions collectively ensure that the digestive process proceeds efficiently and prepares food for further digestion and nutrient absorption in the intestines.
