ENG-GNM-S.Y-PSY. -2019( UPLOADpaper no.2)
ENG-GNM-S.Y-PSY. –05/09/2019
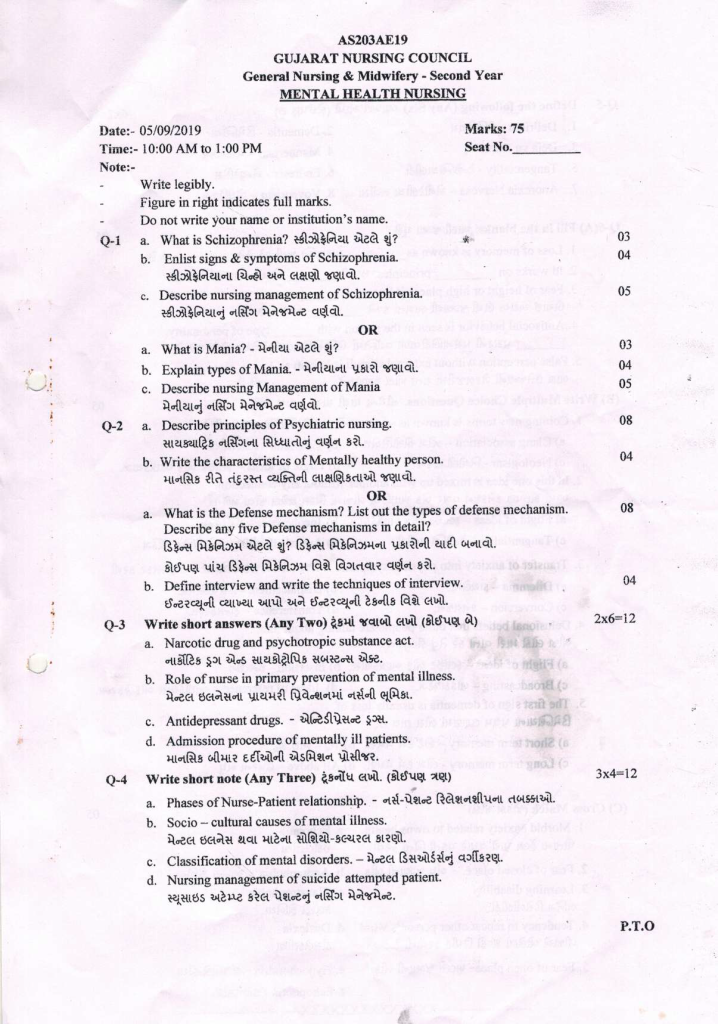
MENTAL HEALTH NURSING-GNC-PAPER SOLUTION YEAR-05/09/2019
Q-1 a. What is Schizophrenia?
In 1908, psychiatrist Eugen Bleuler coined the term schizophrenia, which is derived from the Greek words skhizo meaning split and phren meaning mind, thus schizophrenia is a psychotic condition in which
“Disturbances in thinking, emotions, mood, and volition that usually lead to social disruption are called schizophrenia” that last for more than a month.
Schizophrenia is a very serious condition in which a person experiences difficulty in thinking, disconnection from reality and functioning and cannot express his emotions.
b. Enlist signs & symptoms of Schizophrenia. 04
In general, the personality and behavior of a patient with schizophrenia varies from time to time. Symptoms are often very rapid and severe. Schizophrenia can be classified into the following categories:
Positive symptoms
The symptoms are seen in patients with schizophrenia, also known as psychotics.
Delusion :– Delusions are seen in which someone is oppressing him, someone is conspiring against him, other people are talking about him.
Hallucination:-False hallucinations
Aggression :- Lack of control over emotions
Agitation :- In which nervousness is seen
Suspiciousness :- To be suspicious
Hospitality :-contradictory behavior
Excitement:- Seen unnecessarily excited
Grandiosity:- A sense of grandeur in which he feels like I am the Prime Minister
Conceptual Organization :- Cannot organize his concepts systematically.
Negative symptoms
- Emotion thoughts and moods that are not consistent with the event
- Withdraw from family friends and social activities
- Lack of grooming leads to lack of happiness and interest in life and lack of hygiene and grooming
- Lack of doing activities of daily living
- moodiness
- Catatonia
4 “A’s” of Schizophrenia
- Associative disturbance or looseness
This is a thought disorder such a person cannot do logical thinking - Affect Disturbance In this disturbance is seen in the patient’s mood i.e. the patient’s mood is flat or blunt.
- Ambivalence
Showing an opposite feeling attitude and desire towards the same person thing or situation - Autistic Thinking
This is a thought disorder in which the person gets lost in daydreams and has no awareness of their surroundings.
First Rank Sematms
- Audible thoughts
- No one else has control over his body
- Thought Vidrole
- Thought Insertion
- Diffusion of Thought
- Delusional Perception
SECOND RANK CIMTOMS
- Perplexity-Munjavan
- Delusional Perception
- Depressive or euphoric mood
- Dryness in feeling
Disturbance in attention
Cannot maintain attention for long periods of time
Insight
Inside is affected
Disorders of Activity
Negativision and automatism
Studio type speech and activity
Impulsiveness
c. Describe nursing management of Schizophrenia. 05
1.Therapeutic Nursing Management
- Administering medications prescribed by a psychiatrist
- Always remember 5 right before giving medicine
- To observe and record any side effects or changes in the patient after administration of the medicine
- If the patient is to be given ECT, explain it and allow him to talk about his illness
2.Psycho-Social Nursing Management
- Sit close to the patient
- Talk to the patient in a comfortable environment with a trusting relationship so that his anxiety is removed
- Encourage the patient to talk about his problem
- Never criticize him while speaking or talking about him
- Encourage the patient to speak
- Talk to the patient in a simple language that he understands
- Listen quietly as the patient talks about his delusions and observe how they manifest in his behavior.
- Never acknowledging his delusions but providing him with a safe environment
- Do not talk about the patient’s hallucinations, talk about anything other than this
- Never ignore the patient, sometimes take a pause while talking and use interview techniques such as pinpointing, clarifying, reflecting, summarizing etc.
- Increasing Self-Concept To increase the patient’s self-concept, tasks should be assigned to the patient, such as calling everyone for the day’s activity, asking them to check that everyone has eaten, asking them to clean up, etc.
- To improve attention and judgment nurse should play games like carrom, chess, ludo etc. with the patient. He should be asked to solve small problems.
- Improving Family Support The patient should always have a relative of the patient who can help with his problems. May help with patient’s daily activities like personal hygiene, diet etc.
3. Physical Needs Nursing Management
a) Protection:
- Ensure that the patient does not have access to sharp or injurious items such as knives, blades, cords, glass objects, etc.
- If a patient is involved in altercations or shows aggressive behavior towards others, they may be given a punishment such as being excluded from activities or games. b) Assisting with Personal Hygiene:
- Encourage the patient to brush their teeth regularly.
- Ensure that the patient is able to fully empty their bowels and bladder as they may have difficulty doing so. c) Assisting with Rest:
- Encourage the patient to go to bed early at night. Turn off the main lights and provide a bedside floor lamp.
- If a patient is disturbing others, they should be separated.
- Provide a glass of warm milk to the patient before bed.
- Engage the patient in daily activities during the day.
- Discourage the patient from taking naps in the afternoon. d) Nutritional Needs:
- Plan a balanced diet for the patient for the following day.
- Serve food that the patient finds appetizing in their preferred dishes and encourage them to eat independently.
- If the patient is unsure about eating, first have their relatives taste the food.
- Ensure that the patient receives food according to their dietary needs.
4. Recreational Needs Nursing Management
- Ask the patient about their hobbies to provide suitable recreational activities.
- Provide games such as Carom or Ludo for the patient to play.
- Offer games that use energy, like badminton.
- Initially, avoid giving the patient competitive games.
- Give praise if a patient wins a competition.
5. Spiritual Needs Nursing Management
- Encourage the patient to pray daily and make arrangements for this.
- Celebrate all upcoming festivals appropriately, but never force anyone to celebrate any particular religion or festival.
OR
a. What is Mania?
Mania is a distinct period during which a person experiences an unusually elevated, expansive, or irritable mood. This abnormal mood period lasts for at least one week (or less if hospitalization is necessary).
In mania, the patient exhibits:
- An unusually elevated mood
- Inappropriate and increased excitement
- Heightened irritability
- Severe insomnia
- Grandiose delusions
- Increased speed of speech
- Disconnected and racing thoughts
- Increased sexual desires
- Significantly increased energy and activity levels
- Poor judgment and inappropriate social behavior
b. Explain types of Mania.
1.Hypomania
- Hypomania does not cause significant impairment in social or occupational functioning nor does it require hospitalization.
- The hypomanic person’s mood is euphoric and expansive.
- However, there may be irritability that surfaces quickly when desires or wants are unfulfilled.
- The hypomanic individual tends to have a very unstable and fluctuating mood.
- They may feel a sense of grandeur and increased self-confidence.
- Problems may arise in goal-directed activities, with the person being easily distracted or inattentive.
- Motor activity is increased, and they are very friendly and sociable with others.
- They make many acquaintances but struggle to form deep friendships due to a lack of depth in their personality.
- The person talks excessively and laughs loudly.
- Socially, they can be aggressive, argumentative, spendthrift, and have unfulfilled ambitions.
- They cannot tolerate criticism and their mood frequently changes.
2.Acute Mania
- Acute mania involves a more severe intensity of symptoms compared to hypomania, leading to significant impairment in social or occupational functioning and often requiring hospitalization.
- The person is persistently euphoric and elated, displaying a high mood with constant excitement.
- Thoughts may be sluggish, with flight of ideas and delusions of grandiosity, such as believing they are a prominent scientist.
- There is increased motor activity, and the behavior can become violent.
- The individual is constantly engaged in activities and does not seem to tire, often losing weight due to a lack of eating peacefully.
- Hallucinations may be present but are not typical.
- Attention and judgment are impaired.
3.Delirious Mania
- This type includes severe clouding of consciousness, which is rare.
- The delirious individual’s mood is very fragile.
- They may display feelings of despair, which can quickly turn into uncontrollable ecstasy or complete indifference to the environment.
- Disorientation, confusion, and impaired cognition and perception are observed.
- There may be excessive religiosity, delusions of grandeur or persecution, and auditory or visual hallucinations.
- The person is extremely agitated and incoherent.
- Psychomotor activity is frenetic and characterized by excessive, purposeless movement.
- The safety of these individuals is at risk until their behavior is controlled.
- Exhaustion, self-harm or harm to others, and ultimately, if untreated, death can occur.
c. Describe nursing Management of Mania 05
Therapeutic Nursing Needs
1.Medication Management Needs
- Administer medications prescribed by a psychiatrist.
- Always remember the 5 Rights before administering medication.
- Observe and record any side effects or changes in the patient after administering medication.
- If the patient is on lithium carbonate therapy, check lithium levels regularly.
- If the patient is undergoing ECT (Electroconvulsive Therapy), explain the procedure to them and allow them to discuss their illness.
- Advise patients on lithium to consume less salt.
2.Physical Needs
- Encourage the patient to reduce physical activity and take rest.
- Engage the patient in activities that divert their energy and help them focus, such as crafting or making items like socks.
- Encourage participation in games such as carom, badminton, tennis, etc.
- Recommend a short nap during the afternoon and promote 6-7 hours of sleep at night.
3.Safety and Security Needs
- Ensure the patient does not injure themselves; dress any wounds or injuries.
- Maintain a calm environment to avoid any additional stimulation.
- Control the patient’s behavior to prevent them from harming themselves or others, possibly by implementing restrictions on certain activities.
4.Nutritional Needs
- Provide “finger foods” to patients experiencing mania who are not calm.
- Advise patients on lithium therapy to increase their fluid intake.
- Provide a high-calorie, high-protein diet.
- Regularly monitor the patient’s weight and maintain an intake/output chart if the patient has reduced appetite.
5.Improving Judgment and Concentration
- Assign daily tasks and check how the patient completes them.
- Correct the patient’s behavior with other patients.
- Maintain a friendly demeanor with the patient and ignore inappropriate behavior when possible.
- Encourage the patient to read or watch TV and start with small tasks.
6.Improving Communication
- Communicate with the patient in a simple and concise manner and avoid any conflicts.
- Reward positive changes in the patient’s communication.
- Speak with the patient in a friendly manner but avoid making jokes at their expense.
- Monitor social interactions from the beginning.
- Maintain a good and authentic therapeutic relationship with the patient.
- Encourage the patient to interact with others and provide opportunities for social interaction.
- Support the patient in pursuing their interests.
7.Recreational Needs
- Initially, engage the patient in solitary activities, then gradually encourage group activities.
- Opt for short and simple games.
- Provide recreational activities such as sudoku, ludo, and snakes and ladders.
8.Spiritual Needs
- Encourage the patient to engage in their religious practices.
- Facilitate meetings with clergy or spiritual leaders they believe in.
- Allow the patient to pray individually or in groups.
- Celebrate religious festivals according to the patient’s faith, such as Diwali, Holi, Ramadan, Eid, Christmas, etc.
Q-2 a. Describe principles of Psychiatric nursing. 08
Patient is Accepted Exactly as He Is
Acceptance means being free from any kind of prejudice or indecision. It expresses feelings of love and care. Acceptance does not mean complete approval, but rather setting a framework of positive behaviors to respect the individual as a human being.
A. Being Non-judgmental and Non-punitive
- The patient’s behavior is not judged as right or wrong, good or bad.
- The patient is not punished for undesired behavior. Punishments like direct restraint, restriction, isolating in a separate room, or indirect neglect or avoidance are not used.
- A nurse who shows acceptance does not reject the patient even if they behave contrary to expectations.
B. Being Sincerely Interested in the Patient
- Genuine interest in another person involves considering their interests.
- Study the patterns of the patient’s behavior.
- Allow the patient to make their own choices and decisions as much as possible.
- Be aware of their likes and dislikes.
- Be authentic with the patient.
- Give time to listen to what the patient says.
- Avoid sensitive topics and issues.
- Recognize and reflect on the feelings that the patient may express.
C. Recognize and Reflect on Feelings Which the Patient May Express
- When the patient speaks, it is important not only to note the content but also to recognize and reflect on the underlying emotions behind the conversation.
D. Talking with Purpose
- The nurse’s conversation with the patient should revolve around their needs, desires, and interests.
- When issues are unclear, using techniques such as reflection, open-ended questions, focusing on the topic, and presenting reality in an indirect manner can be more effective.
E. Listening
- Listening is an active process. The nurse should invest time and energy to listen to what the patient says.
- The nurse should listen with empathy and show genuine interest.
F. Permitting Patient to Express Strongly Held Feelings
- Strong emotions can be very explosive. It is better to allow the patient to express intense feelings without rejection or punishment.
2.Use Self-Understanding as Therapeutic Tools
- A psychiatric nurse should have a clear self-understanding and be able to recognize their own emotions and responses.
3.Consistency is Used to Contribute to Patient’s Security
- This means that staff should take steps to ensure patient safety during routine ward activities.
4.Reassurance Should Be Given in a Subtle and Acceptable Manner
- Reassurance builds the patient’s self-confidence. The nurse needs to understand and analyze the patient’s situation to provide appropriate reassurance.
5.Patient’s Behavior is Changed Through Emotional Experience and Not by Rational Interpretation
- Advising or making logical interpretations is not effective in changing behavior. Behavior can be altered through role-play, social dramatization, and similar methods.
6.Unnecessary Increase in Patient’s Anxiety Should Be Avoided
- To prevent unnecessary anxiety, the following should be considered:
- The nurse should not display their own anxiety.
- Avoid focusing on the patient’s flaws.
- Avoid subjecting the patient to repeated failures.
- Avoid placing demands on the patient that they clearly cannot meet.
7.Objective Observation of Patient to Understand His Behavior
- It is important to evaluate what the patient wants or needs to express. The nurse should avoid mixing personal feelings, judgments, or opinions with objective observation.
8.Maintain Realistic Nurse-Patient Relationship
- A realistic or professional relationship focuses on the individual’s personal and emotional needs rather than just the needs of the patient and nurse.
9.Avoid Physical and Verbal Force as Much as Possible
- The nurse should not use any form of punishment as it can lead to psychological trauma for the patient. The nurse should study the patient’s behavior and prevent uncertain behavior. Procedures should be carried out swiftly, and the nurse should avoid showing personal discomfort. If restraint is necessary, the reasons should be explained. Allow the patient to interact positively with others when their behavior improves.
10.Nursing Care is Centered on the Patient as a Person and Not on the Control of Symptoms
- Behavioral symptoms often have underlying reasons. The nurse should understand the reasons behind these symptoms rather than just focusing on managing them. Patients may show different behavioral symptoms in similar situations, so care should be centered on the patient as a person, not just their symptoms.
11.All Explanations of Procedures and Other Routines Are Given According to the Patient’s Level of Understanding
- Explanations of routines and procedures should be tailored to the psychiatric patient’s level of understanding to alleviate their anxiety. Every individual has the right to understand procedures applicable to them, and it should be ensured that this is not neglected.
12.Many Procedures Are Modified but Basic Principles Remain Unaltered
- Many procedures may be modified according to the patient’s needs, but basic principles such as patient safety, security, therapeutic relationships, and procedural aspects remain unchanged.
b. Write the characteristics of Mentally healthy person. 04 Marks
Characteristics of a Mentally Healthy Person
1.He Has His Own Philosophy of Life
- A mentally healthy person develops their own values considering societal demands. This philosophy guides them in various activities of life.
2.A Proper Sense of Self-Evaluation
- A well-adjusted person is aware of their abilities, motivations, strengths, and limitations. They carefully evaluate their behavior and acknowledge their mistakes.
3.Emotionally Mature
- They are emotionally mature and stable, expressing their feelings appropriately and controlling and using them effectively.
4.A Balanced Self-Regarding Sentiment
- They possess a proper sense of personal respect. They view themselves as an important member of the social group and feel they can contribute to their progress and welfare.
5.Socially Adjustable
- Being social creatures, we engage in give-and-take relationships. A mentally healthy person knows the art of living a social life and practices social give-and-take.
6.A Realistic Approach
- Their approach to life’s various problems is realistic. They are not afraid of imaginary fears or difficulties.
7.Intellectually Sound
- They have developed their intellectual abilities sufficiently, which enables them to think independently and make appropriate decisions at the right time.
8.Emotional Maturity
- Emotions like fear, anger, love, etc., are common in our social lives. Such a person has mature emotional behavior, controls their emotions, and expresses them according to accepted social norms.
9.Bravery Facing Failures
- Life is like a seesaw. To achieve success, one must face failures at times. A person with mental balance has enough courage and patience to deal with failures in their life.
10.Punctuality
- A mentally healthy person exhibits desirable social and healthy habits. They do not forget their commitments and are regular and punctual in fulfilling their responsibilities.
11.Self-Judgment
- Self-judgment is one of the important characteristics of such a person. They use it to solve their problems and do not rely on others’ judgments.
General Characteristics of a Mentally Healthy Person:
- They feel good about themselves.
- They are not overwhelmed by emotions such as fear, anger, love, jealousy, guilt, or anxiety.
- They maintain stable and satisfying personal relationships.
- They feel comfortable with other people.
- They can laugh at themselves and others.
- They maintain respect for themselves and others even in the face of disagreements.
- They are capable of accepting life’s disappointments.
- They can meet life’s demands and manage their problems as they arise.
- They make their own decisions.
- They shape their environment whenever possible and adjust it as needed.
OR
a. What is the Defense mechanism? List out the types of defense mechanism Describe any five Defense mechanisms in detail? 08
Defense mechanisms are the mental responses and reactions that arise as a result of influences affecting the mind.
“Defense mechanisms are the psychological strategies an individual uses to cope with reality and maintain self-image. Healthy individuals typically use a variety of defense mechanisms throughout life. is.”
A person unconsciously uses this defense mechanism to protect the EGO when it is affected
There are many different types of this defense mechanism which are as follows
- Rationalization
- Projection
- sublimation
- Repression
- regression
- Compensation
- Daniel
- Un doing
- Acting out
- suppression
- Conversion
- Substitution
- Identification
- Reaction Formation
- Displacement
- Withrol
- Avoidance
- Dissociation
- fixation
- Intellectualization
- Isolation
- Introjection
- resistances
- somatization
1. Rationalization
Rationalization involves providing socially acceptable and less logical reasons for one’s actions or decisions. It is used when an individual’s ego is threatened; they employ this mechanism to protect their self-esteem and justify their behavior. Examples of rationalization include:
a. Sour Grapes: When something is unattainable, the person may convince themselves that it wasn’t necessary or that it’s better not to have it.
For example: If someone doesn’t win first place in a competition, they might say that the prize isn’t worth much.
b. Sweet Lemon: When a losing team claims that the winning team had better preparation and resources, implying that their victory was due to those factors, rather than the losing team’s shortcomings.
For example: After a game, the losing team might say that the winning team had superior preparation and resources, which is why they won, and that’s why the losing team couldn’t win.
2. Compensation
When an individual has a flaw or deficiency, they attempt to make up for it by excelling in another area. This person works toward a goal to prove themselves and directs all their energy toward that goal.
For example: If a girl feels she is not attractive, she might excel in singing or dancing to compensate for her perceived lack of physical appeal.
3. Displacement
In displacement, an individual transfers their feelings or emotions from a person or situation that is more threatening to one that is less dangerous.
For example: If a person receives criticism from their boss at work but cannot express their frustration directly to the boss, they may come home and take out their anger on their spouse.
4. Denial
Denial is the defense mechanism where an individual initially refuses to accept sudden changes, effects, or any outcomes in life. It is one of the most commonly observed defense mechanisms. When faced with an unpleasant event or situation, the person behaves as though it did not happen, refusing to acknowledge that it did.
For example: When a loved one passes away, their relatives may not be ready to accept or believe the reality of the death.
Similarly, if a patient is diagnosed with a terminal illness, they might refuse to accept or acknowledge the diagnosis.
5. Sublimation
Sublimation is a defense mechanism where an individual transforms socially unacceptable impulses or desires into socially acceptable and constructive behaviors. It involves redirecting these impulses into activities that are beneficial and satisfying.
For example: A person who is restricted from consuming certain foods or fruits due to a medical condition might find satisfaction in drawing pictures of those foods. Similarly, a woman with a strong desire for motherhood might channel her maternal instincts by joining a children’s organization, thus fulfilling her yearning for motherhood in a socially acceptable way.
b. Define interview and write the techniques of interview. 04
Interview A face-to-face conversation to solve the same problem or have the same objective is called an interview.
Interview technique
1.Observing
When a patient starts crying while talking, frequently washes their hands, wipes sweat, drinks water repeatedly, speaks in short phrases, has watery eyes, or makes restless movements, it is important to observe and note all these nonverbal behaviors. This includes monitoring actions like hand washing, sweating, frequent water drinking, and other physical cues.
2. Listening
When a patient is speaking, the nurse should be a good and active listener. Responding to the patient’s words with acknowledgments such as “yes,” “right,” “good,” “really?” and similar comments makes the patient feel that the nurse is attentively and empathetically listening to them.
3. Reflecting
Reflecting involves paraphrasing or repeating what the patient has said to show that the nurse is actively listening. This technique helps the patient feel that their words are being attentively heard and considered.
Validating
Validating means confirming whether the information provided by the patient or about the patient is accurate or not. It ensures that any details or claims made are verified.
Clarifying
Clarifying involves asking the patient to explain or elaborate on something if there is confusion or ambiguity about what they said. For example, if there is confusion, the nurse might ask, “What did you mean by that?”
4. Questioning
Questioning is a direct method of communication used to gather information. To obtain comprehensive responses, open-ended questions should be asked rather than closed-ended questions. For instance, an open-ended question would be, “What did you have for breakfast this morning?” whereas a closed-ended question would be, “Did you have breakfast this morning?”
5. Confirming
Confirming involves asking questions related to the patient’s behavior to verify specific details. For example, the nurse might ask, “Do you often turn your face away from me? Are you feeling angry?”
6. Summarizing
Summarizing involves the nurse providing a summary of the main points discussed during the conversation. This allows the patient to review the key topics and add any additional information or make corrections if needed.
Q-૩ Write short answers (Any Two) 2X6=12
a. Narcotic drug and psychotropic substance act.
Narcotic Drugs and Psychotropic Substances Act, 1985 (NDPS Act)
The Narcotic Drugs and Psychotropic Substances Act is an Indian legislative act passed by the Indian Parliament in 1985, which came into effect on November 14, 1985.
This Act is designed not only to control and regulate narcotic drugs and psychotropic substances but also to address certain chemicals that could be used in the illegal production of narcotic and psychotropic substances. It also covers the investigation and seizure of drug-related properties.
The key components of mandatory regulatory governance under this Act are as follows:
- Regulation and Prohibition: The Act regulates and prohibits the cultivation, production, possession, sale, purchase, transport, warehousing, use, interstate movement, transshipment, and import and export of narcotic drugs and psychotropic substances. Such activities are only permitted for medical or scientific purposes under any license, permit, or authorization issued by the government.
- Central Government Authority: The Central Government has the authority to regulate the production, import, export, sale, and use of narcotic drugs and psychotropic substances.
- State Government Authority: State Governments are empowered to permit and regulate the cultivation, possession, and interstate movement of opium, poppy straw, and medicinal opium.
- Prohibition on International Trade: The Central Government prohibits any involvement or control in trade involving narcotic drugs or psychotropic substances acquired from outside India or supplied to any person outside India, except with prior authorization from the Central Government.
- Controlled Substances: The Central Government is responsible for controlling substances used in the manufacture of narcotic drugs and psychotropic substances. It is also responsible for the seizure of properties obtained through drug trafficking.
- Appointment of Officials: Both the Central and State Governments have the authority to appoint officials for the enforcement of the law.
Various agencies are empowered to enforce the provisions of the law at both central and state levels. These agencies include:
- Customs and Central Excise Departments
- Revenue Intelligence Directorate
- Central Bureau of Narcotics (at the central level) and Central Bureau of Investigation
- State-level Police and Excise Departments
- Ministries of Social Justice and Empowerment and Health
b. Role of nurse in primary prevention of mental illness.
Many things within the community affect mental health so community health nurse works for mental health promotion of mental health at community level prevention treatment of mental illness and rehabilitation here we will see the role of nurse in primary prevention which is as follows
Individual steps
There are many drugs that can have side effects on the mother and her fetus, so avoid unnecessary and self-medication during pregnancy. Counseling if the child is physically or mentally challenged Support strengthening mother-child relationship
Participation in school health programs
Community health nurses can detect abnormal behavior of children by going to school and take appropriate professional measures to correct it at the earliest.Teachers should learn to recognize any abnormal behavior in children so that such cases can be identified and referred immediately.
Family Care
Family activities should promote respect, love, trust, and understanding among all family members. The family is a crucial medium for raising children, as it is here that children learn adjustment and coping abilities. Parenting training can be provided through child guidance clinics, where issues related to children’s mental health can be discussed and guidance can be offered. If there are poor relationships within the home, especially between spouses, marital guidance should be provided to improve these relationships.
Adolescence Care
To Develop Mental Crisis When a child goes through adolescence, there are many hormonal and bodily changes that affect their mental health.
Age and Socio-Cultural Changes
In addition, retirement and menopause are situations that can impact mental health. Family crises such as the death of a key family member, divorce, etc., can also affect mental health. Mental health clinics, first aid clinics, and many other resources can help address these situations.
For culturally marginalized families, community programs should be provided. Families living in poor conditions who lack access to food, education, health services, and recreational facilities are more likely to turn to alcoholism, drug addiction, crime, and mental health issues.
Preventive measures for society include providing support to mothers before childbirth, working to improve educational methods for children, and making efforts to address crises. Utilizing various biological data (such as vital statistics) for these purposes is essential.
In community development programs, nurses play various roles including counselor, educator, facilitator, and advocate. Additionally, health workers operating in peripheral areas should be informed and educated about mental health prevention and promotion activities.
c. Antidepressant drugs.
Indication (to whom it can be given):-
- A prolonged feeling of sadness There has been a big loss
- Having adjustment problems
- Excessive anxiety etc
Selective Serotonin Reuptake Inhibitors (SSRIs)
Selective Serotonin Reuptake Inhibitors (SSRIs) are a type of antidepressant medication. Depression is often linked to insufficient levels of serotonin, a chemical in the brain used to transmit signals between nerve cells. This class of drugs includes medications such as Citalopram (Celexa), Fluoxetine (Prozac), and Sertraline (Zoloft).
SSRIs work by inhibiting the reuptake of serotonin (also known as 5-hydroxytryptamine or 5-HT) by presynaptic nerve cells, thereby maintaining higher levels of 5-HT in the synapses.
examples
- Citalopram (Celexa)
- Escitalopram (Lexapro)
- Fluoxetine (Prozac)
- Paroxetine (Paxil, Pexeva)
- Sertraline (Zoloft)
2. Tricyclic Antidepressant Drugs (TCA’S)
Tricyclics block the reuptake (reuptake) of the neurotransmitters nor-epinephrine (not-adrenaline) and serotonin so that proper amounts are maintained in the pre-synapse.
Cyclic antidepressants drugs examples
- Amitriptyline.
- Amoxapine.
- Desipramine (Norpramin)
- Doxepin.
- Imipramine (Tofranil)
- Nortriptyline (Pamelor)
- Protriptyline.
- Trimipramine.
3. Monoamine Oxidase Inhibitors (MAOIs)
The MAOI enzyme monoamine oxidase is an enzyme that breaks down the neurotransmitters dopamine, serotonin, and nor-epinephrine (nor-adrenaline) so proper levels are maintained.
MAOIs Drugs
- Isocarboxazid (Marplan)
- Phenelzine (Nardil)
- Selegiline (Emsam)
- Tranylcypromine (Parnate)
- Contraindication (to whom it should not be given)
- Cardio Vascular Disorders (Because These Drugs Cause Arrhythmias)
- Have liver disorders
- Symptoms of mania are increased in mdp
Side Effects of Antidepressants
- Nausea, vomiting, or diarrhea
- Headache
- Drowsiness
- Dry mouth
- Insomnia (difficulty sleeping)
- Nervousness, agitation, or restlessness
- Dizziness
- Sexual problems, such as reduced sexual desire, difficulty reaching orgasm, or erectile dysfunction
- Impact on appetite, leading to weight loss or weight gain
Nurse’s Responsibilities with Antidepressant Drugs
- Before administering medication, adhere to the 5 Rs and understand potential side effects.
- Encourage the patient to increase fluid intake to avoid dry mouth.
- Assess the patient’s risk of self-harm.
- Monitor the patient for increased psychomotor activity.
- Be aware of Black Box warnings to prevent suicide events.
- Provide small, frequent meals.
- Maintain intake and output charts.
- Offer a high-fiber diet to prevent constipation.
- Ensure the patient gets adequate sleep.
- Avoid foods containing tyramine when using Monoamine Oxidase Inhibitors (MAOIs).
- If the patient reports any sexual dysfunction, discontinue the medication immediately and inform the physician.
- Report any symptoms such as speech problems or mood changes by discontinuing the medication and informing the physician.
- Inform that therapeutic effects are typically seen after four to eight weeks.
- Document and report any changes observed in the patient.
d. Admission procedure of mentally ill patients.
Admission and Detention in Psychiatric Hospitals
- Admission on voluntary basis
- Admission under special circumstances
- Reception orders
- 1. Admission on voluntary basis
- Admission as a voluntary patient
- For admission requested by guardian
Regulations for Voluntary Patients:
- Upon receiving the application, the Medical Officer-in-Charge should conduct an examination within 24 hours and, if satisfied, may accept the application for voluntary admission.
- Every voluntary patient admitted is required to adhere to the rules established by the Medical Officer.
Voluntary Admission:
- Admission as a voluntary patient is requested by the primary individual.
- Admission to the ward can be requested by a guardian.
- Regulations for voluntary patients:
- Upon receiving the application, the Medical Officer-in-Charge must conduct an examination within 24 hours and, if satisfied, may accept the application for voluntary admission.
- Every admitted voluntary patient must adhere to the rules established by the Medical Officer.
2.Admission under special circumstances:
Any mentally ill person who does not or cannot express his desire for admission may be admitted and kept as a patient in a mental hospital on an application made in that behalf by a relative or friend of the mentally ill person if the Medical Officer-in-charge is satisfied that It is necessary to do so in the interest of mentally ill persons
Reception Orders
➤ Application for Reception Orders:
- An application for reception orders can be made by:
- The In-Charge Medical Officer
- The spouse or other relative of the mentally ill person
Where the In-Charge Medical Officer is satisfied that:
- It is necessary for the treatment to continue in a mental hospital for more than six months.
- It is in the interest of the mental health and safety of the mentally ill person or for the protection of others.
- The psychiatrist must apply to the magistrate within the jurisdiction of the psychiatric hospital.
➤ Each application should be as follows:
- Properly signed and verified
- Accompanied by two medical certificates
- From two medical practitioners, one of whom must be in government service
Q-4 Write short note (Any Three) 3X4=12
a. Phases of Nurse-Patient relationship. –
Phases of the Nurse Patient Relationship Relationship
1. Pre-Interaction Phase
This phase starts from the moment a nurse is assigned to a patient, prior to any direct interaction with the patient. During this phase, the nurse may experience some fear and anxiety. The nurse sets objectives and may seek help from a clinical supervisor to manage their anxiety. The nurse might have misconceptions or beliefs about the patient, such as concerns about whether the patient will accept them or if there will be any violent behavior. To address these concerns, the nurse often discusses with colleagues from previous shifts or makes assumptions based on the patient’s records.
2. Orientation Phase
This phase begins when the nurse starts interacting with the patient. The nurse introduces themselves, and the patient may not yet be familiar with the nurse. During this phase, both the nurse and the patient get acquainted with each other and establish a working relationship. A treatment contract is made, outlining the goals and expectations. The nurse should demonstrate trustworthiness in their behavior during communication with the patient and inform the patient about the confidentiality of the information shared. The orientation phase is complete when both the nurse and the patient recognize each other as unique human beings.
3. Working Phase
The working phase involves problem-solving and executing the goals set during the orientation phase. The nurse works towards the patient’s recovery, manages their own anxiety, and reduces their fears. During this phase, the nurse encourages the patient to socialize, motivates them to communicate, and assists in finding solutions to their problems.
4. Termination Phase
The termination phase is the final stage of the therapeutic relationship between the nurse and the patient. It is also known as the resolution phase or end phase. The primary goal of this phase is to end the therapeutic relationship between the nurse and the patient. The termination phase begins when the patient’s treatment contract, established during the orientation phase, is nearing completion. This phase may occur when the patient is discharged, placed on parole, or if the nurse must move to another clinical rotation. The therapeutic relationship ends when the patient no longer needs one-to-one care, even if the patient remains in the hospital. It is crucial to inform the patient about the termination of the therapeutic relationship and to give them the opportunity to express their thoughts and feelings about it.
b. Socio- cultural causes of mental illness.
- In our society, family and culture provide a strong support system where an individual learns a lot and interacts extensively, and many aspects of this interaction affect their mental health.
- For example, where we live, the strength of our support network, and close family and friends who make us feel secure and whom we can trust, all play a crucial role.
- Our workplace and how and where we can relax also affect our mental health.
- The physical environment, such as the neighborhood you live in, can be very stressful, especially if there are issues with neighbors or if the area has a high crime rate and other such problems.
- Whether a person enjoys their work or feels that they are working under a lot of pressure also impacts their mental well-being.
- Failure to find employment
- Death of a close relative
- Divorce
- Change in job and school
- Social and cultural expectations
- Substance Abuse
- A sense of constant inferiority
- poverty
Apart from this there are many reasons which cause mental illness
- War and Violence: The impact of war and violence affects people’s mental health for a long time.
- Group Prejudice: Issues like religious intolerance and animosity affect mental health when one group imposes these prejudices on others.
- Economic and Employment Problems: These are significant factors affecting mental health. Economic problems can sometimes lead to severe consequences such as suicide or violence.
- Technological and Social Changes: Rapid technological changes can be a major source of stress for people.
c. Classification of mental disorders. –
Classification according to ICD-10
Here is the translation of the provided ICD-10 classification of mental and behavioral disorders:
- F0 – F9: Organic, including symptomatic, mental disorders
(Organic mental disorders) - F10 – F19: Mental and behavioral disorders due to use of psychoactive substances
(Mental and behavioral disorders due to the use of psychoactive substances) - F20 – F25: Schizophrenia, schizotypal, and delusional disorders
(Schizophrenia, schizotypal, and delusional disorders) - F30 – F39: Mood [affective] disorders
(Mood disorders) - F40 – F49: Neurotic, stress-related, and somatoform disorders
(Neurotic, stress-related, and somatoform disorders) - F50 – F59: Behavioral syndromes associated with physiological disturbances and physical factors
(Behavioral syndromes associated with physiological disturbances and physical factors) - F60 – F69: Disorders of personality and behavior in adult persons
(Personality and behavior disorders in adults) - F70 – F79: Mental retardation
(Mental retardation) - F80 – F89: Disorders of psychological development
(Disorders of psychological development) - F90 – F98: Behavioral and emotional disorders with onset usually occurring in childhood and adolescence
(Behavioral and emotional disorders typically occurring in childhood and adolescence)
Classification according to DSM-5
Axis I: Clinical Disorders (all mental disorders except Personality Disorders and Mental Retardation)
Axis II: Personality Disorders and Mental Retardation
Axis III: General Medical Conditions (must be connected to a Mental Disorder)
Axis IV: Psychosocial and Environmental Problems (for example limited social support network)
Axis V: Global Assessment of Functioning (Psychological, social and job-related functions are evaluated on a continuum between mental health and extreme mental disorder) (Global Assessment)
Indian classification
A.Psychosis
Here is the translation for the terms related to different types of mental disorders:
- Functional
- Schizophrenia, paranoid schizophrenia, hebephrenic schizophrenia, catatonic schizophrenia, simple schizophrenia, etc.
- Affective
- Mania
- Depression
- Organic
- Acute
- Chronic
B.Neurosis
- Obsessive Compulsive Disorder (OCD)
- Phobic neurosis
- Depressive neurosis
- NJT neurosis
- Hysterical neurosis
Special disorder
Child Childhood Disorders
- Conduct Disorders Emotional Disorders
Personality Disorders
Substance Abuse - Alcohol
Psycho physiological - Disorders Asthma Psoriasis
Mental return return
Miles moderate severe profaun
d. Nursing management of suicide attempted patient.
1.Therapeutic Need Nursing Management
- Provide a comfortable environment to the patient and ask the relative of the patient to stay with him continuously
- The doctor administered the prescribed medicine. Watching for its side effects and keeping a record-report. Usually giving anti-depressant drugs to a suicidal patient.
- Conducting an MSE on the patient involves recording suicidal thoughts and plans as well as how lethal they are.
- Assisting and preparing the patient if ECT is to be administered
2.Physical Need Nursing Management
a.Safe Environment
- Keeping the patient under constant observation A nurse should be constantly there to care for him
- Glass articles, ropes, pajama and petticoat cords, net ties, etc. should be removed from the room.
Long bed sheets should also not be used as they can be used for hanging
Using paper dishes for food - Electrical connections should not be left open
- Medicines and instruments should be kept locked in the ward
- Care should be taken that the patient does not swallow more than one medicine
A room should be provided near the nursing station
3. Personal Hygiene :- Encourage the patient to maintain his personal hygiene Encourage him to change his clothes, take a bath, comb his hair etc. Say you look very nice today
4. Nutritional lead Advise the patient to take diet and record its input and output
4.Psycho Social Need :-
Trusting Relationship
Talk to the patient Listen to him calmly Bring out the positive things in him Let the patient visit his relative Try to create a positive attitude in him
Reducing suicidal ideation Encourage the patient to talk about his/her suicidal ideation and how to commit suicide etc.
Increase in self esteem Calling the patient by his name Acknowledging his positive points and positive achievements
Improve socialization The patient should never be left alone asking them to get out of bed slowly to meet people
Recreational Need Identify the patient’s favorite hobby or game Give him enough time for outdoor games even if he completes his hobby Give him success if he wins If he loses Accept without any disturbance
Spiritual Activities
Find out why the patient wants to die
Talk about what he would be able to do if he lived
Give him religious books to read and discuss religious books with him to help him recognize their quality
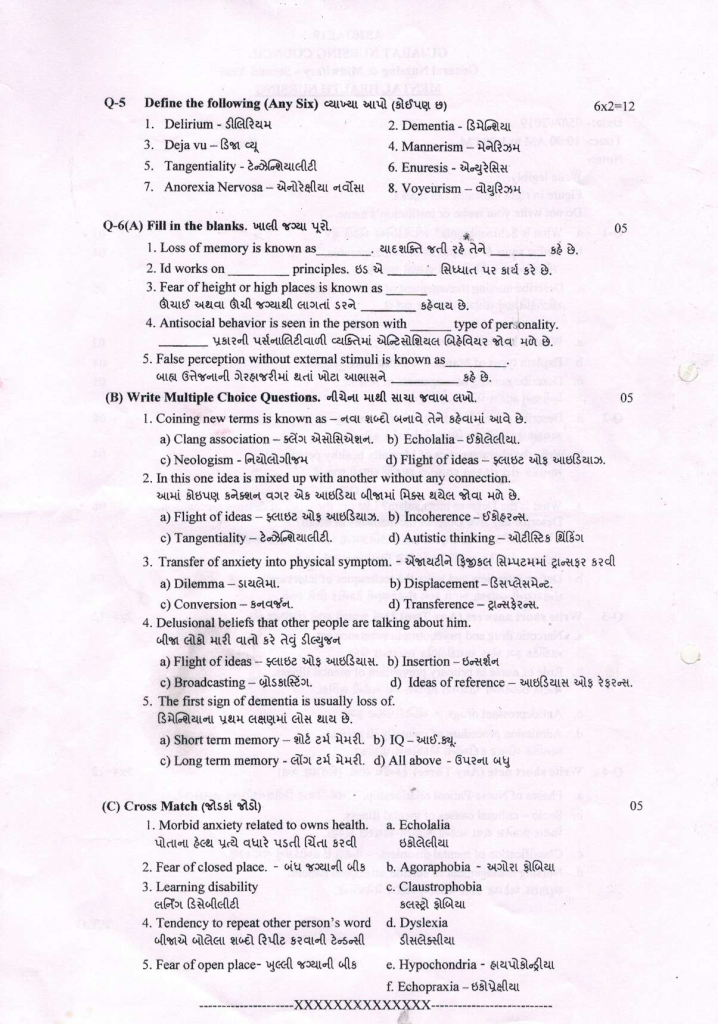
Q-5 Define the following (Any Six) 6X2=12
1.Delirium – It is an acute organic condition that disturbs the mind or consciousness. In which the person has symptoms of confusion, dis-orientation, agitation, hallucinations etc. which are seen due to physical disorders such as fever, intoxication, etc.
2. Dementia – Due to the organic disease of the brain, there is a progressive or continuous decrease in intellectual function in a person, along with a decrease in memory, personality, and thinking, which is called dementia.
૩.Deja vu-In this, the person feels that he has seen this person, place or scene somewhere but does not know where and when. The real is experiencing the situation for the first time which is called déjà vu.
4..Tangentiality– In this, a disturbance is seen in the thought process of the person. Instead of answering the question, the person shows excessive and inappropriate things (unnecessary), but we do not answer the desired question, the person cannot reach his goal. Even at the end there is no answer.
5.Mannerism- The unconscious stereotype of his gesture, facial expression by the person is seen strange movement which is called mannerism.
A. D. To spoil one’s face, to do monkey work
6.Enuresis –Enuresis is defined as involuntary or intentional passing of urine through clothing or bed at least twice a week for a period of three consecutive months in children older than five years. It is one of the most frequent chronic disorders of childhood.
7.Anorexia Nervosa– This is an eating disorder in which the person does not consume food due to the fear of gaining weight and having a bad body image. They are very concerned about weight and body shape by strictly controlling and limiting what they eat. Try to keep the weight as low as possible. This is very worrying.
8.voyeurism This is a sexual disorder in which the enjoyment and sexual satisfaction of seeing other people’s sexual activity or nakedness is called voyeurism. In which the person has no active involvement but is only interested in watching it.
Q-6(A) Fill in the blanks. 05
Loss of memory is known as ______ Amnesia-
Id works on _____principles Pleasure
Fear of height or high places is known as______Acrophobia
Antisocial behavior is seen in the person with _______type of per onality. Antisocial Personality
False perception without external stimuli is known as________ Hallucination
(C) Cross Match 05
1.Morbid anxiety related to owns health a. Echolalia
2.Fear of closed place. b. Agoraphobia –
3.Learning disability c. Claustrophobia
4.Tendency to repeat other person’s word d. Dyslexia
5.Fear of open place e. Hypochondria
f. Echopraxia –
Answer:-
1.-e
2.-c
3.-d
4.-a
5.-b
💪 💥☺ALL THE BEST ☺💥💪
