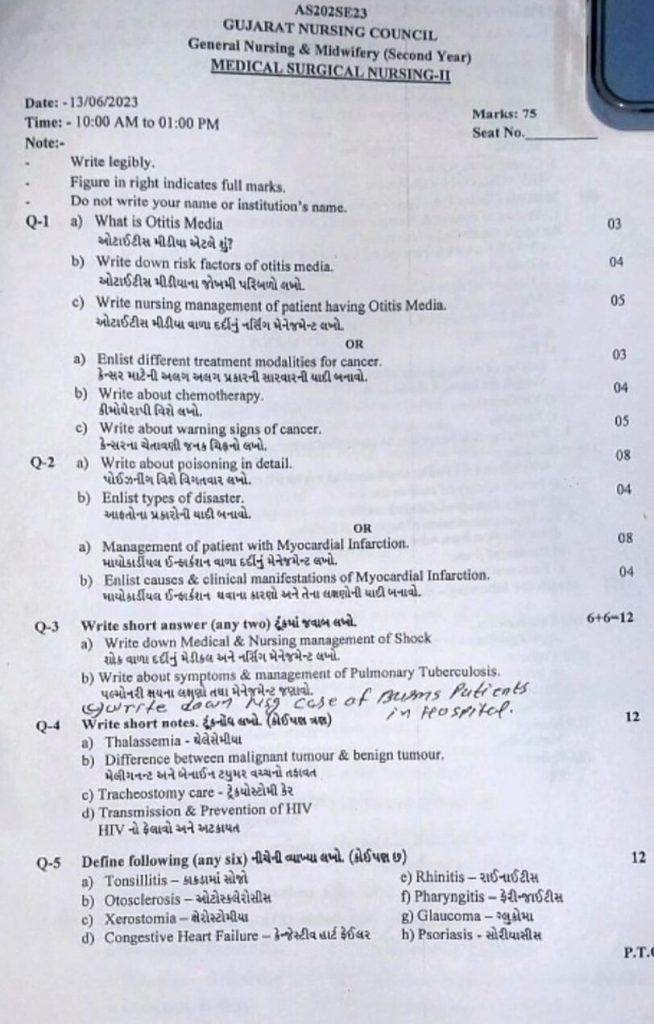
ENG-GNM-S.Y-MSN-II-GNC-PAPER SOLUTION-2023 (UPLOAD NO.06)
GNM-S.Y-MSN-II-GNC-PAPER-13/06/2023 (Easy-PAPER SOLUTION)
🔸a) What is Otitis Media 03
🔸a) What is Otitis Media?
Otitis media is an infection or inflammation in the middle part of the ear. This condition commonly occurs in young children but can affect people of any age. It can be acute or chronic.
Causes of Otitis Media:
- Bacterial Infection: Typically caused by bacteria such as Streptococcus or Haemophilus bacteria.
- Viral Infection: Viruses like COVID virus or rhinovirus can also lead to otitis media.
- Allergies: Sensitivity to allergens like pollen, dust, or other allergic substances.
- Cold or Flu: Infections such as cold or flu can predispose someone to otitis media.
- Eustachian Tube Blockage: Blockage of the Eustachian tube (a canal connecting the middle ear to the back of the nose and throat) can cause pressure and fluid buildup in the middle ear.
🔸b) Write down risk factors of otitis media.
The following are risk factors for otitis media (infection or inflammation of the middle ear):
- Age: Children between 6 months to 2 years are at higher risk of developing otitis media.
- Family History: Having a family history of otitis media among relatives.
- Daycare Attendance: Children attending daycare centers where they come into contact with more children.
- Bottle Feeding: Feeding infants with a bottle while lying down.
- Allergies: Sensitivity to allergens such as pollen, dust, or other allergic substances.
- Exposure to Tobacco Smoke: Being exposed to secondhand smoke from family members who smoke.
- Immune System Issues: Weakened immune defenses.
- Poor Eustachian Tube Function: Dysfunction of the Eustachian tube.
- Seasonal Factors: Increased risk during seasons associated with colds and flu.
- Lack of Breastfeeding: Not being breastfed.
These risk factors should be considered to help prevent otitis media.
🔸c) Write nursing management of patient having Otitis Media.05
For a patient with Otitis Media, the nursing management is crucial to ensure effective recovery and comfort. Here is the nursing management for Otitis Media:
Patient Assessment:
- Assess symptoms: Ear pain, difficulty hearing, discharge from the ear, fever, and irritability.
- Physical examination: Examination of the ear and assessment of hearing using an otoscope.
Providing Comfort:
- Pain management: Administer prescribed pain relief medications.
- Warm compress: Apply a warm compress to the ear for pain relief.
- Comfortable positioning: Position the patient comfortably, especially keeping the head slightly elevated.
Medication Administration:
- Antibiotics: Administer antibiotics as prescribed to control bacterial infection.
- Antipyretics: Administer fever-reducing medications such as paracetamol.
Education and Counseling:
- Medication adherence: Educate the patient and family on how and when to take medications.
- Ear hygiene: Instruct on keeping the ear clean and dry to prevent infection.
- Avoiding risk factors: Educate on avoiding smoking and exposure to cold environments.
Monitoring and Follow-up:
- Monitor symptoms such as ear pain, discharge, and changes in hearing.
- Schedule regular medical follow-ups to assess recovery progress.
Emergency Care:
- Address severe symptoms promptly such as severe ear pain, high fever, or other serious symptoms requiring immediate medical attention.
Effective nursing management plays a significant role in ensuring the patient with Otitis Media receives appropriate care and comfort, especially when symptoms are not adequately controlled or there are serious complications. The following are surgical and nursing management steps for Otitis Media in Gujarati:
Surgical Management:
- Myringotomy: A small incision (ear drum) made in the ear drum to relieve pressure and allow drainage.
- Tube Insertion: In some cases, a small tube is inserted into the ear drum to allow fluid to drain and airflow into the ear.
1.Nursing Management:
- Patient Care: Monitoring symptoms like ear pain, fever, and fluid drainage.
- Medications: Administering antibiotics and pain relief medications as prescribed.
- Maintaining Hygiene: Keeping the ear dry and clean for ear health.
Preparation for Surgery:
- Educating the patient and family about the surgical procedure and post-procedure care.
- Providing pre and post-procedure care instructions.
Post-operative Care:
- Monitoring the bandage or tube placed in the ear.
- Checking for signs of infection like redness, swelling, and pus.
- Regular follow-up with the doctor post-surgery.
3.Preventing Complications:
- Avoiding water entry into the ear.
- Limiting physical activities during the recovery period.
Following these surgical and nursing management steps can effectively treat Otitis Media and ensure a successful recovery for the patient.
⏩OR ⏪
🔸a) List various types of cancer treatment modalities.
Here is a list of various treatment modalities for cancer:
Surgery:
- Procedure: Removal of tumors through surgical intervention.
- Purpose: Complete or partial removal of tumors to prevent cancer spread.
Radiation Therapy:
- Procedure: Using high-energy rays to destroy cancer cells.
- Purpose: Shrink tumors and eliminate cancer cells.
Chemotherapy:
- Procedure: Using medicines to inhibit or destroy cancer cells.
- Purpose: Stop the growth of cancer cells and eliminate them.
Hormone Therapy:
- Procedure: Blocking necessary hormones for cancer growth.
- Purpose: Control the development of hormone-sensitive tumors.
Immunotherapy:
- Procedure: Boosting the body’s immune system to fight cancer.
- Purpose: Enhance the immune system to recognize and destroy cancer cells.
Targeted Therapy:
- Procedure: Targeting specific genes or proteins to destroy cancer cells.
- Purpose: Directly target cancer markers or mutations with less harm to healthy cells.
Stem Cell Transplant:
- Procedure: Replacement of damaged bone marrow with healthy stem cells.
- Purpose: Restore bone marrow cells destroyed by chemotherapy or radiation.
Phototherapy:
- Procedure: Using specific types of light to destroy tumors.
- Purpose: Destroy cancer cells using light as a therapeutic tool.
Laser Therapy:
- Procedure: Using laser beams to target and destroy cancerous tissue.
- Purpose: Precisely target tumors for destruction.
Clinical Trials:
- Procedure: Participation in studies testing new treatments and medications.
- Purpose: Experimental testing of new and alternative treatments.
These various cancer treatment modalities are chosen based on the severity, type, and physical condition of the patient.
🔸b) Write about chemotherapy.
Chemotherapy is a treatment method used to destroy cancer cells. This method is commonly used in cases of advanced or metastatic cancer.
Detailed Information about Chemotherapy:
How Chemotherapy Works:
Chemotherapy involves administering medication either through injections or orally. This treatment circulates through the bloodstream and rapidly kills fast-growing cancer cells. Chemotherapy effectively reduces the size of cancer tumors and eliminates spreading cancer cells in other parts of the body.
Types of Chemotherapy:
1. Adjuvant Therapy:
– Administered after the main tumor is removed surgically to eliminate remaining cancer cells.
2. Neoadjuvant Therapy:
– Administered before surgery to shrink tumors and facilitate easier removal.
3. Metastatic Therapy:
– Used when cancer has spread, aiming to destroy tumors and hinder further spread.
Chemotherapy Drugs:
Various types of drugs are used in chemotherapy, including cyclophosphamide, methotrexate, doxorubicin, and paclitaxel. These drugs may be used alone or in combination therapies.
Side Effects of Chemotherapy:
Chemotherapy is a potent treatment that rapidly kills cells, which can lead to several side effects such as:
1. Nausea and vomiting
2. Hair loss
3. Fatigue
4. Decrease in blood cells
5. Increased risk of infection
6. Mouth sores
7. Loss of appetite
Care During Chemotherapy:
1. Nutrition and diet: Maintain a nutritious and balanced diet.
2. Daily activities: Engage in normal activities but avoid excessive fatigue.
3. Infection prevention: Practice proper hygiene and monitor for signs of infection.
4. Medical monitoring: Regular medical check-ups and follow doctor’s advice.
Post-Chemotherapy Care:
Following chemotherapy, it’s crucial to follow the doctor’s advice and guidelines strictly. Improving lifestyle with strategies for disease-free living, exercise, and mental support is essential.
Chemotherapy is a highly effective and necessary treatment that can bring improvements in the lives of cancer patients.
🔸c )Write about warning signs of cancer.05
Warning signs of cancer:
1) Change in bowel and bladder habits: Normal individuals typically have bowel movements once to twice a day. If there is a change and it occurs 3 to 5 times a day, it could indicate an underlying issue.
2) A sore that does not heal: These sores tend to be persistent, painful, and may bleed.
3) Unusual bleeding and discharge: Blood in urine or stool, or bleeding from body parts such as nipples or penis, should be investigated promptly.
4) Thickening or lump in breast or any other body parts: A lump that doesn’t reduce in size and increases in firmness should be evaluated.
5) Indigestion and difficulty swallowing: Difficulty in digesting food or swallowing it indicates a potential concern.
6) Obvious changes in moles: Any change in size, shape, or color of moles warrants medical attention.
7) Nagging cough or hoarseness: Persistent coughing, changes in voice, or coughing up blood should not be ignored.
These are all warning signs that could indicate the presence of cancer.
⏩Q-2
🔸a) Write about poisoning in detail
Poisoning is a condition caused by exposure to toxic substances, leading to harmful effects on the body. There are several types of poisoning:
Food Poisoning:
- Caused by bacteria, viruses, or parasites in contaminated food.
- Clinical Manifestations: Nausea, vomiting, abdominal pain, fever.
Drug Overdose:
- Results from excessive consumption of medications.
- Clinical Manifestations: Drowsiness, difficulty breathing, nausea, dizziness.
Chemical Poisoning:
- Occurs due to exposure to household or industrial chemicals.
- Clinical Manifestations: Respiratory distress, skin irritation, nausea, dizziness.
Toxic Substance Poisoning:
- Involves substances like carbon monoxide, phosphine, etc.
- Clinical Manifestations: Headache, dizziness, weakness, respiratory distress.
Insect/Snake Bite Poisoning:
- Result of venom injected by insects or snakes.
- Clinical Manifestations: Swelling, pain, respiratory distress, dizziness.
Symptoms of Poisoning:
- Nausea and vomiting
- Difficulty in breathing
- Abdominal pain
- Dizziness and weakness
- Skin changes
- Headache
- Cough and cold symptoms
- Loss of coordination
- Sudden fever
Diagnosis of Poisoning:
- Medical History: Understanding the patient’s history and possible substance exposure.
- Observation of Symptoms: Monitoring clinical manifestations and their progression.
- Laboratory Tests: Blood, urine, and body fluid tests to identify toxins.
Immediate Treatment of Poisoning:
- Removal of the toxic substance from the body.
- Administration of activated charcoal to absorb toxins.
- Inducing vomiting.
- Providing oxygen and intravenous fluids.
Specific Antidotes may be required based on the type of poisoning (e.g., antivenom for snake bites).
Further Treatment involves:
- Keeping the patient hydrated.
- Monitoring nutrition levels.
- Long-term management and rehabilitation if severe.
Prevention of Poisoning:
- Adherence to safety rules at home and work.
- Keeping poisonous substances out of reach of children.
- Reading labels of chemicals and medications for proper usage.
- Proper disposal of hazardous substances.
This comprehensive approach ensures effective management and prevention of poisoning incidents, safeguarding individuals’ health and well-being.
🔸b) Enlist types of disaster.
Types of Disasters:
- Natural Disasters
- Geological Disasters
- Earthquakes
- Volcanic eruptions
- Tsunamis
- Landslides
- Avalanches Hydrological Disasters :
- Floods
- Flash floods
- Coastal flooding Meteorological Disasters :
- Hurricanes, typhoons, and cyclones
- Tornadoes
- Severe storms
- Biological Disasters
- Epidemics and pandemics
- Insect infestations
- Animal diseases
- Climatological Disasters
- Wildfires
- Extreme temperatures
Man-Made (Anthropogenic) Disasters
- Technological Disasters
- Industrial accidents
- Nuclear accidents
- Transportation accidents
- Environmental Degradation :
- Deforestation
- Soil erosion
- Desertification
- Conflict-Related Disasters
- War and armed conflicts
- Terrorist attacks
- Civil unrest
- Miscellaneous Disasters ):
- Cyber-attacks
- Infrastructure failures
This list covers various types of disasters categorized by their occurrence and nature.
⏩OR⏪
🔸a) Management of patient with Myocardial Infarction.08
Myocardial infarction, commonly known as a heart attack, requires immediate and effective medical treatment to restore blood flow to the heart muscles and minimize subsequent damage and complications. The management of myocardial infarction can vary depending on the stage of the condition:
1.Pre-hospital Care:
- Recognize symptoms such as chest discomfort, shortness of breath, nausea, sweating, etc., indicative of a heart attack.
- Immediately hospitalize the patient without delay if suspected.
Administer Aspirin:
- Give 325 mg of aspirin unless contraindicated, to reduce clot formation and prevent further damage.
Provide Oxygen:
- Administer oxygen if there are breathing problems or if oxygen saturation is low.
2.Emergency Room Care:
Initial Assessment and Monitoring:
- Obtain medical history and conduct a physical examination promptly.
- Monitor vital signs including heart rate, oxygen saturation, and blood pressure.
- Keep the patient on continuous cardiac monitoring.
Diagnostic Tests:
- Perform an electrocardiogram (ECG) to identify ST-segment elevation indicating myocardial infarction.
- Conduct blood tests such as troponin levels to assess for cardiac injury or ischemia.
Immediate Treatment:
- Administer oxygen if hypoxemia is present.
- Nitroglycerin may be given to relieve chest pain and reduce cardiac workload.
- Morphine may also be administered if pain is not adequately controlled.
- P2Y12 inhibitors like Clopidogrel or Ticagrelor are prescribed.
4.Reperfusion Therapy:
- Perform Primary Percutaneous Coronary Intervention (PCI) within 90 minutes if medical facility allows.
- Thrombolytic therapy (e.g., alteplase, reteplase) if PCI is not feasible.
Hospital Care:
- Continuous monitoring including ECG and frequent vital sign checks.
- Medications: Beta-blockers to reduce heart rate and myocardial oxygen demand, ACE inhibitors or ARBs to lower blood pressure and prevent ventricular remodeling, Statins to lower cholesterol levels and stabilize plaque, Aldosterone antagonists for patients with heart failure or left ventricular dysfunction.
- Echocardiogram to assess left ventricular function and detect complications like heart failure or valvular dysfunction.
- Risk stratification for complications and subsequent management planning.
Post-Discharge Care:
- Continued medications including antiplatelet agents, beta-blockers, ACE inhibitors, statins, and others as prescribed.
- Lifestyle modifications: Smoking cessation, low cholesterol and salt intake diet, regular physical activity, weight management.
- Cardiac rehabilitation involving exercise, education, and counseling to improve cardiovascular health.
- Follow-up care with cardiologist and physician as needed.
- Patient education on recognizing symptoms of MI, adhering to regular medication, making lifestyle changes, and seeking immediate help.
Complication Management:
- Manage heart failure with appropriate medications and lifestyle changes.
- Treat arrhythmias with medications and monitor accordingly; consider devices like pacemakers if necessary.
🔸b) Enlist causes & clinical manifestations of Myocardila Infarction 04
Causes:
- Atherosclerosis
- Thrombosis
- Spasm
- Hypertension
- Obesity
- Smoking
- Diabetes
- Unhealthy diet
- Lack of physical activity
- Genetics
Clinical Manifestations:
- Chest pain – Severe discomfort or pressure in the chest, due to inadequate oxygenation of myocardium, manifesting typically as ischemic pain. The pain may radiate to the left jaw and arm.
- Upper body pain – Pain in the shoulders, back, neck, or jaw.
- Hypotension and tachycardia due to decreased cardiac output.
- Emotional stress leading to breathing difficulties or shortness of breath.
- Nausea or vomiting.
- Fatigue – Sudden exhaustion or weakness.
- Sweating and cold sweats – Profuse sweating due to sympathetic nervous system stimulation, also known as diaphoresis, with cold and clammy skin.
- Dizziness or sudden dizziness.
- Other symptoms – Abdominal pain, gas, indigestion, etc.
- Anxiety, palpitations, and headaches may also be observed.
This is a severe medical emergency condition where delayed treatment can lead to death.
⏩Q-3 Write short answer (any two) 6+6=12
🔸a) Write down Medical & Nursing management of Shock
Shock is a condition where due to low systemic blood pressure, vital organs such as the heart, brain, and kidneys do not receive adequate blood, oxygen, and nutrients. This prevents organs from functioning properly and requires an increased load to work effectively, leading to the body entering a state of shock.
••> Management of Shock in Patients:
1) Recognition and Assessment
Recognition: Identify shock based on clinical signs (e.g., hypotension, tachycardia, altered mental status, cool and clammy skin) and its etiology (e.g., hemorrhagic, septic, cardiogenic).
Assessment:
Perform rapid assessment of the patient to identify the cause and severity of shock.
This involves taking a thorough patient history, conducting a comprehensive physical examination, and performing complete diagnostic tests (blood tests, imaging, echocardiogram) that can properly identify the severity of shock and its cause.
2) Hydration and Fluid Management (Fluid Resuscitation):
Initial Resuscitation:
To improve patient’s circulating volume and tissue perfusion, administer intravenous fluids (crystalloids) rapidly. Fluid administration is typically 1-2 liters of isotonic crystalloids (e.g., Normal Saline, Ringer’s Lactate) to maintain circulatory volume properly.
Subsequently, closely monitor their response, including central venous pressure, urine output, and clinical assessments (capillary refill, skin temperature).
•> Targeted Approach:
Fluid therapy based on type of shock
•> Hemorrhagic Shock:
Replace lost blood with appropriate blood products (packed red blood cells, fresh frozen plasma) as per requirement.
•> Septic Shock:
Monitor fluid level with hemodynamic monitoring (e.g., central venous pressure, stroke volume variation) to guide increased fluid levels.
•> Cardiogenic Shock:
Carefully replace fluid to prevent fluid overload.
3) Vasopressor Therapy:
Indication: Used when fluid resuscitation alone cannot maintain blood pressure and tissue perfusion adequately.
Agents commonly used in vasopressor therapy include norepinephrine (first-line), epinephrine, dopamine, and vasopressin.
Administer vasopressors via a central line if possible.
Monitoring: Continuously monitor patient’s vital signs including blood pressure, heart rate, urine output, and peripheral perfusion during vasopressor therapy.
4) Oxygen Therapy:
Administration: Provide supplemental oxygen to maintain patient’s oxygen levels.
Monitoring: Continuously monitor oxygen saturation using pulse oximetry.
Mechanical Ventilation: If the patient is in severe shock or respiratory failure, provide respiratory support via mechanical ventilation.
5) Treatment of Underlying Cause:
Hemorrhagic Shock: Take measures to control bleeding to manage shock condition due to hemorrhage.
Septic Shock: Administer broad-spectrum antibiotic medication to manage the condition of septic shock. Also, control sources such as proper drainage of abscesses.
Cardiogenic Shock: Properly treat myocardial ischemia (e.g., revascularization procedures like percutaneous coronary intervention). Optimize cardiac function with medications (e.g., beta-blockers, inotropes, etc.).
6) Monitoring and Supportive Care:
Continuous Monitoring: Regularly monitor hemodynamic status, laboratory parameters, and organ function (e.g., renal function, mental status).
Electrocardiogram (ECG) Monitoring: Monitor ECG continuously if the patient is in cardiogenic shock to assess arrhythmias and cardiac condition.
••> Nursing Management of Shock:
1) Assessment:
- Continuous monitoring of patient’s vital signs such as:
- Temperature,
- Heart rate,
- Respiratory status,
- Blood pressure, and
- Oxygen saturation.
- Neurological Status: Proper assessment of patient’s mental status, responsiveness, and neurological changes (e.g., confusion and agitation).
- Fluid Balance: Proper monitoring of the patient’s intake and output chart, focusing mainly on urine output and assessing signs of fluid overload.
2) Fluid Administration:
Administration: Administer fluids as prescribed properly. Assess for infusion rate, signs of fluid overload (e.g., pulmonary edema, jugular venous distension), and symptoms.
Response Monitoring: Monitor the response to fluid therapy and assess for any changes in vital signs and perfusion parameters indicating improvement.
3) Positioning and Comfort:
Positioning: Provide appropriate positioning such as elevating the patient’s feet and maintaining a head-down position to facilitate venous return and potentially increase cardiac output.
Comfort Measures: Ensure patient comfort measures are properly provided, including pain management and creating a comfortable environment to reduce patient stress.
4) Oxygenation and Respiratory Support:
Oxygen Administration: Provide the patient with the appropriate amount of oxygen to support respiratory function.
Airway Management: Maintain the patient’s airway and assess for any respiratory distress or respiratory failure.
5) Psychological Support:
Patient and Family Member Education: Provide comprehensive education to the patient and their family members about the patient’s condition, reasons for it, symptoms and signs, diagnostic evaluation, and treatment.
Emotional Support: Provide proper emotional support to the patient, especially during critical times, and offer reassurance.
6) Documentation and Communication:
Documentation: Properly document all information related to the patient.
Communication: Maintain proper open communication with healthcare team members. Collaborate effectively with healthcare team members if there are any changes in the patient’s health.
- Provide comfortable positioning for the patient.
- Provide a comfortable environment for the patient.
- Advise regular follow-up for the patient.
🔸b) Write about sympo & management of Pulmonary Tuberculosis
These are symptoms of pulmonary tuberculosis (TB):
- A bad cough that lasts 3 weeks or longer: Persistent coughing for more than three weeks.
- Coughing up blood or sputum (phlegm from deep inside the lungs): Cough producing phlegm that may contain blood.
- Pain in the chest: Discomfort or pain in the chest area.
- Weakness or fatigue: Feeling weak or unusually tired.
- Weight loss or no appetite: Loss of weight without trying or loss of appetite.
- Sweating at night: Excessive sweating during sleep.
- Fever: Elevated body temperature.
- Chills: Shivering or feeling cold.
These symptoms indicate an active pulmonary tuberculosis infection. If someone experiences these symptoms, it is crucial to seek medical attention promptly for diagnosis and treatment.
⏩Q-4 Write short notes 12
🔸A) Thalassemia
Thalassemia is a group of hereditary hemolytic anemias. It is an autosomal recessive genetic disorder characterized by reduced or inadequate synthesis of hemoglobin, a protein in red blood cells that carries oxygen throughout the body. Thalassemia is a genetic blood disorder in which the body produces a decreased amount of hemoglobin (a protein in red blood cells that carries oxygen throughout the body).
1) Alpha Thalassemia:
- Alpha Thalassemia Trait: In alpha thalassemia trait, one or both alpha globin genes are missing or mutated, but individuals usually do not show symptoms.
- Alpha Thalassemia Minor: Both alpha globin genes are missing or mutated to some extent. Mild anemia occurs and mild symptoms such as fatigue or pale skin may be present.
- Hemoglobin H Disease: Three alpha globin chains are missing or mutated, leading to moderate to severe anemia. Symptoms may include more pronounced anemia, jaundice, enlarged spleen, and other health issues.
- Alpha Thalassemia Major: All four alpha globin genes are missing or severely mutated, causing severe anemia and significant health problems.
2) Beta Thalassemia:
- Beta Thalassemia Trait: In beta thalassemia trait, one beta globin gene is missing or mutated, and most individuals do not show symptoms.
- Beta Thalassemia Intermedia: Both beta globin genes are moderately affected. Symptoms can vary widely from mild to severe anemia. Some may require occasional blood transfusions.
- Beta Thalassemia Major (Cooley’s Anemia): Both beta globin genes are severely affected. This results in severe anemia requiring lifelong transfusions starting in childhood.
Another classification of the thalassemia
Thalassemia Major (Cooley’s Anemia):
Thalassemia major is the most severe form of thalassemia. It occurs when a child inherits mutated beta globin genes from both parents. This mutation results in significant reduction or absence of beta globin chains, leading to severe anemia. Individuals with thalassemia major require lifelong blood transfusions to maintain hemoglobin levels and prevent complications. Without treatment, thalassemia major can cause growth delays, organ damage, bone problems, and other health-related conditions.
Thalassemia Intermedia:
Thalassemia intermedia is an intermediate form of thalassemia, less severe than thalassemia major but more severe than thalassemia minor. Individuals with thalassemia intermedia inherit two mutated beta globin genes, but the severity of symptoms can vary widely, ranging from mild to moderate anemia. Some patients may require blood transfusions to manage symptoms. Thalassemia intermedia patients may also develop complications such as bone deformities, spleen enlargement, and gallstones, but these are generally less severe compared to thalassemia major.
Thalassemia Minor (Trait):
Thalassemia minor, also recognized as thalassemia trait, is the mildest form of thalassemia. It occurs when a child inherits one mutated beta globin gene from one parent and a normal beta globin gene from the other parent. Individuals with thalassemia minor typically do not experience symptoms or may have mild symptoms of anemia. Thalassemia minor carriers generally have slightly lower than normal hemoglobin levels but do not usually require treatment. However, carriers of thalassemia minor can pass the genetic change to their children, potentially resulting in thalassemia if both parents are carriers.
These classifications help in understanding the varying degrees of severity and management approaches for different forms of thalassemia.
symptoms and signs of thalassemia:
Symptoms and Signs of Thalassemia:
- Fatigue: Feeling tired or lethargic.
- Pale skin, conjunctiva, and mucous membranes: These can appear pale due to anemia.
- Shortness of breath: Difficulty in breathing.
- Spleen and liver enlargement (hepatosplenomegaly): The spleen and liver may become enlarged.
- Jaundice: Yellowing of the skin and whites of the eyes.
- Growth and development delays: Children may experience slower growth and delayed development.
- Bone abnormalities: Bones may become deformed.
- Heart problems: Thalassemia can lead to heart complications.
- Endocrine complications: Issues with hormones and glands.
- Infections: Increased susceptibility to infections.
- Loss of appetite (anorexia): Decreased desire to eat.
- Poor feeding habits: Difficulties in feeding, especially in infants.
- Abdominal distension: Swelling or bloating of the abdomen.
- Failure to thrive: Poor growth and weight gain in children.
- Facial features: Changes such as prominent forehead, exposing upper teeth, depressed nasal bridge.
- Malocclusion of teeth: Misalignment of teeth.
- Lymphadenopathy: Enlarged lymph nodes.
- Hypogonadism: Decreased function of the gonads.
- Osteoporosis: Decreased bone density.
- Metacarpals and metatarsals: Changes in the hands and feet bones.
- Recurrent respiratory infections: Frequent respiratory infections.
- Enlarged lymph nodes: Swollen lymph nodes.
- Poor nutritional status: Difficulty maintaining adequate nutrition.
Diagnostic Evaluation for Thalassemia:
- History taking: Gathering information about personal and family medical history.
- Physical examination: Conducting a physical assessment to observe signs and symptoms.
- Complete blood count (CBC) test: Measuring hemoglobin levels and other blood cell counts.
- Hemoglobin electrophoresis: A specialized test to identify abnormal types of hemoglobin.
- Peripheral blood smear: Microscopic examination of blood cells.
- Iron studies: Testing to assess iron levels in the blood.
- Genetic testing: Analyzing genetic mutations related to thalassemia.
- Bone marrow examination: A procedure to examine bone marrow cells.
- Serum bilirubin test: Measuring levels of bilirubin in the blood.
- Serum iron level: Determining the concentration of iron in the blood.
- Bone marrow studies: Further analysis of bone marrow function.
- Osmotic fragility test: Assessing the fragility of red blood cells.
- Radiological findings: Imaging studies to detect any related abnormalities.
Management of Thalassemia:
- Regular Blood Transfusion Requirement: The patient requires repeated blood transfusions throughout life, starting from early childhood.
- Iron Chelation Therapy: Proper iron chelation therapy is provided to the patient. There are potential risks of iron overload due to frequent transfusions, necessitating this therapy to prevent this condition.
- Involvement in Iron Chelation Therapy: This involves medications such as deferoxamine, deferiprone, and deferasirox.
- Supplementation with Proper Folic Acid: The patient is provided with adequate folic acid supplementation.
- Bone Marrow Transplantation: Consideration for bone marrow transplantation is made.
- Gene Therapy: Proper gene therapy is provided to the patient.
- Supportive Care: Proper supportive care is provided to the patient.
Nursing Management of Thalassemia:
- Provide Complete Education: Educate the patient about their condition, reasons for it, symptoms and signs, and complete details about their treatment.
- Continuous Monitoring: Monitor the patient continuously.
- Proper Blood Transfusion: Provide proper blood transfusions to the patient.
- Assess for Transfusion Reactions: Assess if there are any reactions during blood transfusion.
- Regular Health Supervision: Ensure regular health supervision for the patient.
- Maintain Hydration Status: Properly maintain the patient’s hydration status.
- Monitor Blood and Electrolyte Levels: Regularly monitor the patient’s blood and electrolyte levels.
- Provide Proper Antibiotic Medication: Administer appropriate antibiotic medication to the patient.
- Improve Dietary Intake: Ensure improvement in the patient’s dietary intake, especially foods containing iron and protein.
- Provide Adequate Nutritional Supplements: Provide adequate nutritional supplements such as iron, vitamin B12, and folate if the patient has nutritional deficiencies due to anemia.
- Provide Iron-Enriched Nutritional Diet: Provide a properly iron-enriched nutritional diet to the patient.
- Immediate Treatment for Anemia due to Nutritional Deficiency: Immediately treat the condition if the patient’s anemia is due to nutritional deficiencies.
- Perform Regular Monitoring: Regularly monitor the patient.
- Immediate Start of Intravenous Infusion: If the patient has excessive blood loss causing anemia, immediately start intravenous infusion.
- Provide Analgesic Medication: Provide analgesic medication if the patient has pain.
- Educate Family Members: Educate the patient and their family members about the condition, reasons for it, symptoms and signs, and treatment.
- Perform All Types of Laboratory Investigations: Perform all necessary laboratory investigations for the patient.
- Prevent Anemia Conditions: Regularly screen the child for anemia condition.
- Advise Adjusted Rest: Advise the patient to take adjusted rest.
- Provide Emotional Support: Provide proper emotional support to the patient and their family members.
- Properly Monitor the Condition: Properly monitor the patient’s condition, including recording vital signs and intake-output charts.
🔸b) Difference between mall lignant tumoor & benign tumour.
Difference between Malignant Tumor and Benign Tumor:
Benign Tumor:
Growth Rate:
- Grows at a slow rate.
- Typically does not invade surrounding tissues.
Shape:
- Well-defined, often encapsulated surface.
Cell Characteristics:
- Benign cells appear normal and do not exhibit mutations.
Capability to Spread:
- Does not metastasize (spread to other parts of the body).
Impact on Health:
- Generally not life-threatening but may cause symptoms, discomfort, and other health issues if located near vital organs.
Treatment:
- Can often be surgically removed with a low chance of recurrence.
Malignant Tumor:
Growth Rate:
- Grows rapidly.
- Can invade nearby tissues and organs.
Shape:
- Irregular and poorly defined surface.
Cell Characteristics:
- Malignant cells are abnormal and exhibit mutations, leading to uncontrolled growth.
Capability to Spread:
- Can metastasize through lymph nodes and bloodstream to other parts of the body.
Impact on Health:
- Can be life-threatening and responsible for significant health issues.
Treatment:
- Requires extensive treatment such as surgery, chemotherapy, radiation therapy, and targeted therapy.
- Higher chance of recurrence and spreading.
🔸c) Tracheostomy care
Tracheostomy:
- Definition:
- Tracheostomy involves creating an artificial opening in the trachea (windpipe) to insert a tube, usually to provide artificial oxygen to the patient. It is performed when the patient’s airway needs to be maintained for a prolonged period or when there is respiratory distress.
1.Classification based on Situations:
- Emergency Tracheostomy:
- Conducted when a patient is in respiratory distress and immediate intervention is necessary to secure the airway.
- Prophylactic Tracheostomy:
- Done when a patient is anticipated to develop severe respiratory distress, aiming to prevent such a condition.
2.Classification based on Duration:
- Temporary Tracheostomy:
- A short-term procedure to establish an airway for a limited period.
- Permanent Tracheostomy:
- Involves creating a lifelong opening in the trachea to maintain the airway indefinitely.
3.Classification based on Incision:
- High Tracheostomy:
- The incision is made above the thyroid gland’s isthmus.
- Low Tracheostomy:
- The incision is made below the isthmus of the thyroid gland.
3.Indications for Tracheostomy:
- Obstruction of the air passage due to any tumor.
- Stenosis or narrowing of the trachea and larynx.
- Presence of any foreign body in the trachea.
- Any unconscious patient.
- When the patient is in respiratory distress and can’t breathe.
- When the patient undergoes mouth or neck surgery.
- When the patient is traumatized by the larynx and trachea.
- When the patient undergoes any type of radiation therapy.
- When the patient has difficulty breathing for a long time.
- When the patient has secretion in the lower respiratory tract.
- When intubation is required for a long time after operation.
- When the patient is unable to breathe naturally.
- When any kind of eyelid is applied in the airway
4.Complications of Tracheostomy:
Ventilation Issues:
- Due to the insertion of a tracheobronchial tube, ventilation may be compromised.
Tube Dislodgement:
- The tube may accidentally come out when the patient coughs, sneezes, or during suctioning.
Lower Respiratory Tract Infection:
- Infection may occur in the lower respiratory tract where the tube is inserted.
Local Site Infection:
- Infection can develop at the site where the tube is inserted.
Pulmonary Infection:
- There is a risk of developing infections in the lungs.
Tracheoesophageal Fistula:
- There is a chance of developing a fistula between the trachea and the esophagus.
Hypoxia and Cardiac Arrest:
- Prolonged suctioning can lead to hypoxia (low oxygen levels) and eventually cardiac arrest.
Hemorrhage:
- Bleeding may occur at the tracheostomy site and can enter the respiratory tract.
Aspiration:
- The patient may aspirate food or water that can enter the respiratory tract.
Injury to Tracheal Wall:
- Handling of the trachea walls during procedures can lead to injury.
5.General Instructions:
1. Always remember that tracheostomy is an emergency procedure, so time should not be wasted.
2. Strictly adhere to aseptic technique before and after tracheostomy.
3. Ensure that the tracheostomy tube is of proper size and length.
4. Clear all doubts of the patient and their relatives and explain the procedure thoroughly.
5. Monitor the patient closely before and after the procedure.
Nursing Responsibilities:
1. Monitor the patient closely and observe for any changes.
2. Do not leave the patient alone for the first 48 hours post-tracheostomy.
3. Assess and manage any breathing difficulties the patient may have.
4. Be vigilant to prevent accidental removal of the tube.
5. Keep instruments ready in case the tube needs to be reinserted.
6. Maintain suction catheter readiness.
7. Maintain aseptic technique.
8. Position the patient in a semi-Fowler’s position.
9. Avoid attending to anyone with respiratory infections around the patient.
10. Monitor closely for any complications.
11. Ensure humidified or filtered air for inspiration.
12. Maintain proper fluid intake and electrolyte balance for the patient.
13. Administer medications as prescribed.
14. Pay attention to oral and wound care.
15. Dress the tracheostomy site properly.
16. Provide a comfortable environment for the patient.
17. Answer all questions from the patient and their relatives comprehensively.
🔸d) Transmission & Prevention of HIV
HIV is sexually transmitted.
AIDS := acquired immunodeficiency syndrome.
HIV := Human immunodeficiency virus.
Below are the measures for prevention and prevention:
1) Use barrier method of contraceptive (condom) during coitus act for prevention of HIV and AIDS.
2) Do not use used razor blades.
3) Do not use used toothbrushes.
4) Do not use used needles and syringes.
5) Use disposable needles and syringes.
6) If you have to use used needles and syringes, autoclave them properly before use.
7) If any woman has AIDS or infection, she should avoid pregnancy because there are chances of transmission of AIDS and HIV to the newborn baby.
8) For prevention of AIDS and HIV, people should be given health education about which steps can be taken.
9) Use all kinds of mass media and technology to raise awareness among individuals for prevention of HIV and AIDS.
10) Individuals who are at high risk for HIV and AIDS should be encouraged to refuse blood and other body organ donation.
11) Get screened for HIV and AIDS when receiving blood transfusion or donating blood.
12) Use strict sterilization techniques in hospitals and clinics.
13) Use disposable needles and syringes only.
14) If possible, use sterilized needles and syringes.
15) Use zidovudine tablets as a curative measure.
16) Avoid contact with infected blood and body fluids.
17) Medical personnel should practice universal precautions and use Personal Protective Equipment (PPE) kits when there is potential contact with blood and body fluids.
18) Exercise extreme caution during injections and skin piercing procedures.
19) Use sterilization and disinfection effectively.
20) Provide health education to couples about maintaining proper sexual relationships.
21) Inform individuals about AIDS.
22) Properly explain to students about AIDS as an Incurable Disease Syndrome.
23) Educate people that AIDS is not spread by mosquitoes or insects but through unprotected sexual contact.
24) Provide education that AIDS is not transmitted through clothes but through blood and body fluids.
25) Educate hospital staff who do not have HIV and AIDS about proper precautions to take.
26) Inform people that HIV and AIDS are not transmitted through food or water.
27) Provide Antiretroviral Therapy to individuals who have HIV and AIDS.
28) Offer psychological support to individuals who have HIV and AIDS.
29) Advise individuals with HIV and AIDS to take precautions so as not to transmit the infection to others.
30) Eliminate any misconceptions about HIV and AIDS among the public.
All these are steps for the prevention of HIV and AIDS.
⏩Q-5 Define following (any six) 12
🔸a) Tonsillitis – Inflammation in the tonsils
Tonsils are masses of lymphatic tissue located at the back of the throat. Their function is to protect the body from microorganisms and toxic substances.
When the tonsils become infected and inflamed, it is called tonsillitis. This condition is painful, as the tonsils swell, become red, and tender.
Infections in the tonsils may also cause swelling of nearby lymph nodes in the neck. Additionally, the affected area may show an appearance of grey and white patches.
🔸b) Otosclerosis
Otosclerosis is a progressive disorder of the ear characterized by abnormal growth of bone in the middle ear, specifically around the stapes bone. The stapes bone is a very small bone in the middle ear that transmits sound vibrations from the middle ear to the inner ear. Due to abnormal bone growth, this transmission is hindered, resulting in hearing loss.
Symptoms of Otosclerosis:
- Gradual hearing loss, often starting with difficulty hearing low-pitched sounds or whispers.
- Tinnitus (ringing or buzzing sound in the ear).
- Dizziness or balance problems (less common).
- Difficulty understanding speech, especially in noisy environments.
🔸c) Xerostomia
Xerostomia, commonly known as dry mouth, is a condition characterized by reduced saliva production in the mouth, leading to discomfort. Saliva plays a crucial role in oral health by moistening the mouth and helping with chewing, swallowing, and speaking. When saliva production significantly decreases, individuals may experience dryness and various associated symptoms.
Symptoms of Xerostomia:
- Dry, sticky feeling in the mouth.
- Thick, stringy saliva.
- Difficulty chewing, swallowing, or speaking.
- Sore throat or hoarseness.
- Dry or grooved tongue.
- Bad breath (halitosis).
- Increased thirst.
- Changes in taste or taste disorders.
- Cracked lips or sores in the mouth.
- Increased plaque, tooth decay, and gum disease due to decreased saliva’s protective and cleansing effects.
🔸d) Congestive Heart Failure
Congestive Heart Failure (CHF) is a condition where the heart is unable to pump blood efficiently, leading to a buildup of fluid around the heart and in the lungs. This impairment in heart function affects its ability to adequately supply oxygen and nutrients to the body’s cells and organs.
Symptoms of Congestive Heart Failure:
- Shortness of breath (dyspnea): Especially during physical activity or when lying down (orthopnea), due to fluid buildup in the lungs (pulmonary congestion).
- Fatigue and weakness: Resulting from the heart’s inability to pump enough blood to meet the body’s demands.
- Swelling (edema): Typically in the legs, ankles, and feet due to fluid retention (peripheral edema).
- Rapid or irregular heartbeat (arrhythmias): As the heart attempts to compensate for its decreased function.
- Reduced ability to exercise: Due to decreased cardiac output and oxygen delivery.
- Persistent cough or wheezing: Often with white or pink blood-tinged phlegm, caused by fluid accumulation in the lungs.
- Increased need to urinate at night: As the body retains fluid during the day, which is then excreted at night.
- Swelling of the abdomen (ascites): Due to fluid buildup in the abdominal cavity.
- Sudden weight gain: From fluid retention.
- Lack of appetite and nausea: Resulting from congestion in the digestive system.
- Difficulty concentrating or decreased alertness: Due to decreased blood flow to the brain.
🔸e) Rhinitis
Rhinitis refers to inflammation and swelling of the mucous membrane inside the nose. This condition can be categorized into different types based on its causes, including allergic rhinitis (due to allergens) and non-allergic rhinitis (due to other factors such as infections or irritants).
Symptoms of Rhinitis:
- Runny nose (rhinorrhea): Excessive nasal drainage, which can be clear, thin, or thick depending on the cause.
- Nasal congestion: Blockage or stuffiness in the nose, making it difficult to breathe through the nose.
- Sneezing: Often occurs as a reflex to clear the nasal passages of irritants.
- Itchy nose: Persistent itching sensation inside the nose.
- Postnasal drip: Mucus dripping down the throat from the back of the nose, leading to throat irritation and coughing.
- Watery eyes: Commonly associated with allergic rhinitis due to the release of histamine.
- Cough: Typically caused by postnasal drip irritating the throat.
Types of Rhinitis:
- Allergic Rhinitis: Triggered by allergens such as pollen, pet dander, dust mites, or mold. Symptoms can be seasonal (hay fever) or perennial (year-round).
- Non-Allergic Rhinitis: Caused by irritants like smoke, strong odors, changes in weather, infections (viral or bacterial), hormonal changes, or medications.
Rhinitis can significantly impact quality of life by affecting sleep, work, and daily activities. Treatment involves identifying and avoiding triggers, medications (such as antihistamines, decongestants, nasal corticosteroids), and in severe cases, allergen immunotherapy (allergy shots). Managing symptoms effectively can help reduce inflammation, alleviate discomfort, and improve overall well-being.
🔸f) Pharyngitis
Pharyngitis is a medical term that refers to inflammation or infection of the pharynx, which is the area at the back of the throat. This condition typically causes a sore throat and discomfort due to the inflammation of the pharynx.
Causes of Pharyngitis:
Pharyngitis can be caused by various factors, including:
- Viral infections such as influenza (flu) and common cold viruses.
- Bacterial infections, most commonly by Streptococcus bacteria (Strep throat).
- Irritants such as smoke, pollution, and chemical fumes.
- Allergies that irritate the throat.
- Dry air, which can lead to throat irritation.
Symptoms of Pharyngitis:
- Sore throat: Pain or irritation in the throat.
- Red and swollen throat: Visible inflammation and redness in the back of the throat.
- Pain when swallowing: Discomfort or pain while swallowing food or liquids.
- Dry throat: Feeling of dryness or scratchiness in the throat.
- Hoarseness: Changes in voice quality, making the voice sound rough or strained.
- Swollen lymph nodes: Enlarged lymph nodes in the neck due to the body’s immune response.
- Fever: Commonly seen with bacterial infections.
- Headache: Aching or pain in the head.
- Fatigue: Feeling tired or lacking energy.
Treatment of Pharyngitis:
Treatment depends on the underlying cause:
- Viral pharyngitis usually resolves on its own with rest, fluids, and over-the-counter pain relievers.
- Bacterial pharyngitis may require antibiotics prescribed by a healthcare provider.
- Managing symptoms with throat lozenges, staying hydrated, using humidifiers, and avoiding irritants can help alleviate discomfort.
Pharyngitis can vary in severity and duration based on the cause and individual health factors. Seeking medical advice is recommended if symptoms persist or worsen.
🔸g) Glaucoma
Glaucoma is a disorder of the eye characterized by increased intraocular pressure (IOP), which means that the fluid pressure inside the eye is abnormally high. This elevated pressure can lead to optic nerve damage and peripheral visual field loss.
Key Points about Glaucoma:
- Increased Intraocular Pressure (IOP): In glaucoma, the pressure inside the eye (intraocular pressure) is typically higher than normal. This elevated pressure is caused by a buildup of aqueous humor, the fluid that normally circulates inside the eye.
- Optic Nerve Damage: Prolonged elevation of intraocular pressure can lead to damage of the optic nerve, which is responsible for transmitting visual information from the eye to the brain.
- Peripheral Visual Field Loss: Initially, glaucoma often causes loss of peripheral (side) vision. As the condition progresses, it can lead to tunnel vision and eventually blindness if untreated.
- Types of Glaucoma: There are different types of glaucoma, including primary open-angle glaucoma (POAG), which is the most common form, and angle-closure glaucoma, which occurs when the drainage angle of the eye becomes blocked.
- Symptoms and Diagnosis: Glaucoma often does not cause symptoms in its early stages, which is why regular eye exams are crucial for early detection. As the condition progresses, individuals may experience peripheral vision loss and, in advanced cases, tunnel vision.
- Treatment: Treatment aims to lower intraocular pressure to prevent further damage to the optic nerve. This can be achieved through medications (eye drops), laser therapy (laser trabeculoplasty), or surgery (trabeculectomy).
- Prevention: Regular eye exams, especially for individuals at higher risk (e.g., those with a family history of glaucoma, older adults), are important for early detection and treatment.
🔸h) Psoriasis
Psoriasis is a chronic autoimmune condition characterized by rapid growth and buildup of skin cells. This excessive cell buildup leads to the development of thick, red patches on the skin with silvery scales. Inflammation around these scaling patches is common, and the skin may appear red and inflamed.
Key Points about Psoriasis:
- Types of Psoriasis:
- Plaque Psoriasis: This is the most common form, characterized by dry, raised, red skin lesions (plaques) covered with silvery scales. These plaques can appear anywhere on the body.
- Guttate Psoriasis: Often starts in childhood or young adulthood and is triggered by bacterial infections, such as strep throat. It appears as small, water-drop-shaped sores on the trunk, arms, legs, and scalp.
- Inverse Psoriasis: This type causes bright red, shiny lesions in skin folds such as the armpits, groin, under the breasts, and around the genitals. It may be triggered by friction and sweating.
- Pustular Psoriasis: Characterized by white pustules (blisters of noninfectious pus) surrounded by red skin. It can occur on any part of the body and may be triggered by medications, infections, stress, or exposure to certain chemicals.
- Erythrodermic Psoriasis: The least common form, which can cover the entire body with a red, peeling rash that can itch or burn intensely. It is usually triggered by severe sunburn, infection, certain medications, or abrupt withdrawal of systemic treatment for psoriasis.
- Symptoms: Besides the characteristic skin changes, psoriasis can cause itching, burning, or soreness. The severity and extent of symptoms vary widely between individuals and even within the same person over time.
- Chronic Condition: Psoriasis is considered a chronic disease with no cure. It tends to cycle through flare-ups and periods of remission. Management focuses on controlling symptoms, preventing infections, and minimizing triggers.
- Triggers: Common triggers include stress, skin injuries (like cuts or sunburn), infections (such as strep throat or skin infections), certain medications (like lithium or beta-blockers), and weather changes.
- Treatment: Treatment options include topical treatments (creams and ointments), phototherapy (light therapy), systemic medications (oral or injectable drugs that work throughout the body), and biologic drugs (targeted therapy that alters the immune system).
Psoriasis can have significant physical and emotional impacts due to its visible nature and chronicity. Managing the condition often requires a multidisciplinary approach involving dermatologists, primary care physicians, and sometimes mental health professionals to address the associated emotional stress.
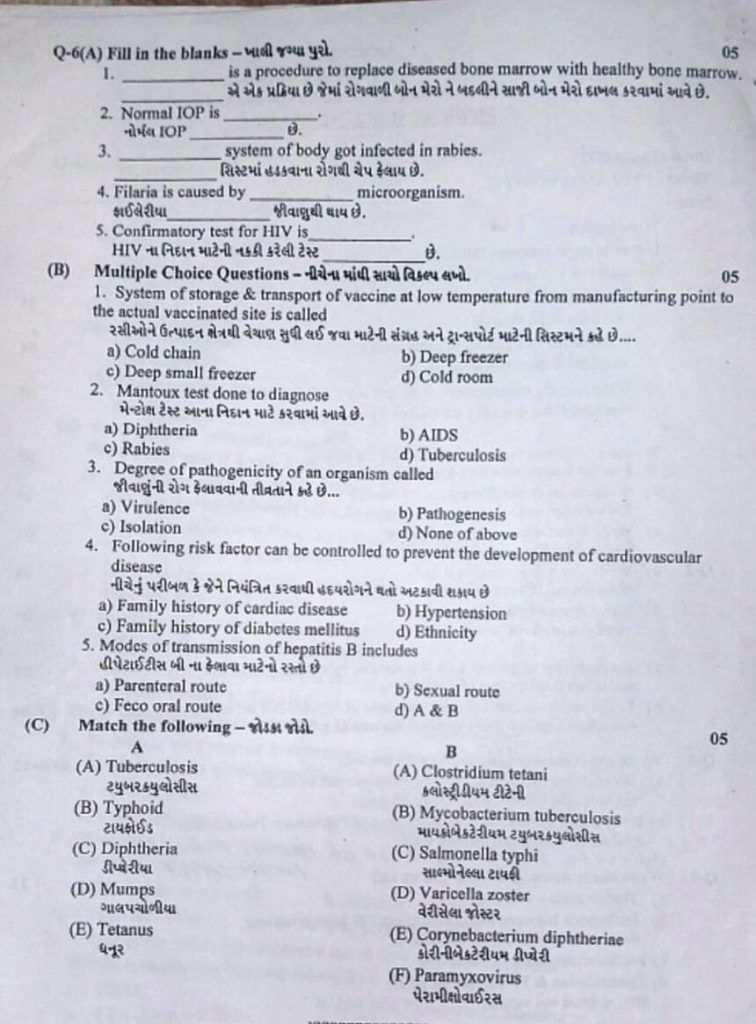
⏩Q-6(A) Fill in the blanks- 05
1)—–is procedure to replace diseased bone marrow with healthy bone marrow. BONE MARROW TRANSPLANT
2.Normal I0P is——– between 11 and 21 mm Hg
3)—–system of body got infected in rabies. Central nervous system
4.)Filaria is caused by——- microorganism Wuchereria bancrofti
5.)Confirmatory test for HIV is—— Western blot test
⏩(C) Match the following 05
(A) Tuberculosis (A) Clostridium tetani –
(B) Typhoid (B) Mycobacterium nuberculosis – –
(C) Diphtheria (C) Salmonella typhi
(D) Mumps (D) Varicella zoster
(E) Tetanus (E) Corynebacterium diplitherias
(F) Paramyxovirus
ANSWER:-
(A) Tuberculosis-→(B) Mycobacterium nuberculosis
B) Typhoid -→ (C) Salmonella typhi
C) Diphtheria → (E) Corynebacterium diplitherias
(D) Mumps → (F) Paramyxovirus
(E) Tetanus (A)Clostridium tetani –
💪 💥☺☺☺ALL THE BEST ☺☺☺💥💪
(NOTE:- MCQ of this paper has been given in special pattern of APP. Hence reading)