ENG-GNM-S.Y-MSN-II-04/09/2019 (paper no .2 )JOSHNA
GNM-S.Y-GNC-MSN-II-04/09/2019 (PAPER SOLUTION)
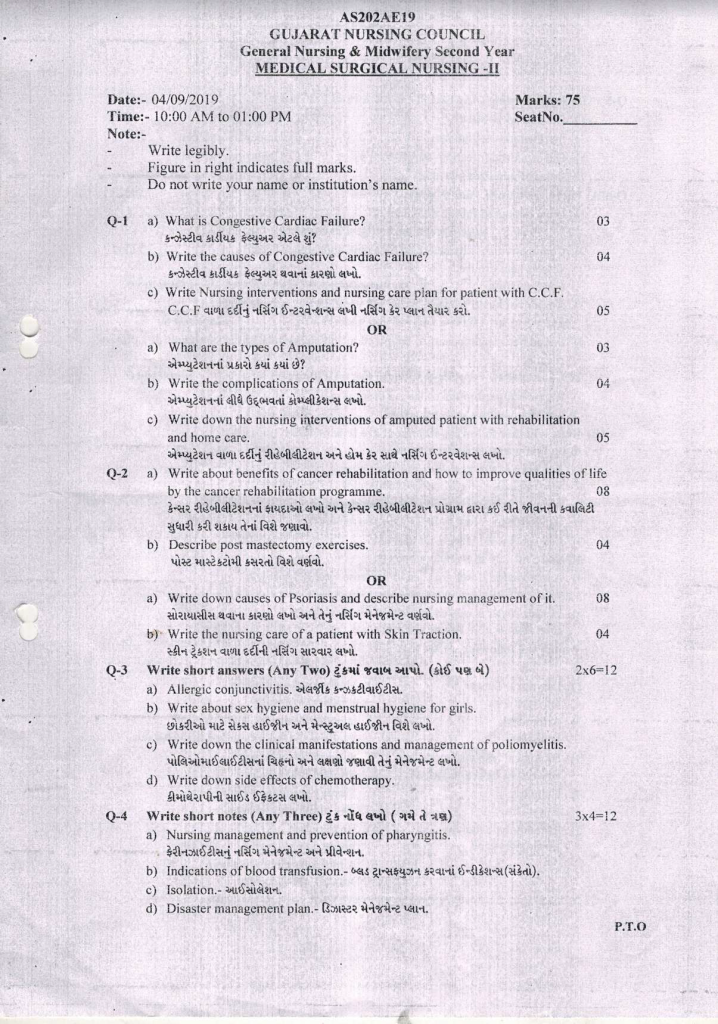
⏩Q-1 🔸a) What is Congestive Cardiac Failure?
In congestive cardiac failure, due to the accumulation of fluid around the heart, the heart cannot work properly, so the heart cannot deliver enough blood to the body, so the blood does not reach all the parts of the body, so oxygen and nutrition are also lost to the cell tissue and Organ does not get.
In this, the function of the heart is altered.
🔸b) Write the causes of Congestive Cardiac Failure?
Congestive cardiac failure, also known as congestive heart failure (CHF), primarily occurs due to abnormalities in the heart muscles caused by various conditions such as:
1) Myocardial Infarction (Heart Attack):
- A myocardial infarction, commonly known as a heart attack, occurs when blood flow to a part of the heart is blocked, leading to damage or death of the heart muscle tissue.
2) Hypertension (High Blood Pressure):
- Chronic high blood pressure can cause the heart to work harder to pump blood, leading to hypertrophy (thickening) of the heart muscles over time. This can eventually contribute to heart failure.
3) Valvular Heart Disease:
- Valvular heart disease involves damage or defects in one or more of the heart valves (such as mitral valve prolapse, aortic stenosis, etc.), which can lead to inefficient blood flow and strain on the heart muscles.
4) Cardiomyopathies:
- Cardiomyopathies are diseases of the heart muscle that can result in structural changes to the heart, impairing its ability to pump blood effectively. There are different types of cardiomyopathies, including dilated cardiomyopathy, hypertrophic cardiomyopathy, and restrictive cardiomyopathy.
5) Arrhythmias (Cardiac Dysrhythmias):
- Arrhythmias are irregular heartbeats that can disrupt the heart’s pumping function over time, leading to heart failure if not managed properly.
These conditions can lead to congestive cardiac failure by affecting the heart’s ability to pump blood efficiently, causing symptoms such as fluid buildup (edema) in the lungs and other parts of the body, shortness of breath, fatigue, and other complications.
Other causes of congestive heart failure (CHF) include:
1) Chronic Lung Disease:
- Conditions such as chronic obstructive pulmonary disease (COPD) or pulmonary hypertension can strain the heart over time, leading to heart failure.
2) Hemorrhage (Severe Bleeding):
- Significant blood loss, such as from trauma or internal bleeding, can reduce the amount of blood the heart pumps and eventually lead to heart failure.
3) Anemia:
- Anemia, a condition where there is a deficiency of red blood cells or hemoglobin, can cause the heart to work harder to deliver oxygen to tissues, potentially contributing to heart failure.
4) Anesthesia:
- Some anesthesia medications can affect heart function, especially in individuals with pre-existing heart conditions, and may lead to heart failure in rare cases.
5) Surgery:
- Major surgeries, especially those involving the heart or large blood vessels, can stress the heart and increase the risk of heart failure during or after the procedure.
6) Physical or Emotional Stress:
- Severe physical stress (e.g., intense exercise beyond one’s capacity) or emotional stress (e.g., severe grief or anxiety) can temporarily strain the heart and, in some cases, lead to heart failure.
7) Excessive Sodium Intake:
- Consuming too much sodium (salt) can lead to fluid retention and increased blood pressure, which can strain the heart and contribute to heart failure, especially in individuals with hypertension or heart disease.
These factors can exacerbate existing heart conditions or directly contribute to the development of congestive heart failure by increasing the workload on the heart or impairing its ability to pump blood effectively.
Risk factors for congestive heart failure (CHF) include:
1) Hypertension (High Blood Pressure):
- High blood pressure can lead to increased strain on the heart muscle over time, potentially leading to heart failure.
2) Hyperlipidemia (High Cholesterol Levels):
- Elevated levels of cholesterol and other lipids in the blood can contribute to the development of atherosclerosis (hardening and narrowing of the arteries), which is a risk factor for heart failure.
3) Diabetes:
- Diabetes, especially if poorly controlled, increases the risk of cardiovascular complications, including heart failure.
4) Coronary Artery Disease (CAD):
- Narrowing or blockage of the coronary arteries due to atherosclerosis can impair blood flow to the heart muscle, leading to ischemic heart disease and potentially heart failure.
5) Family History:
- A family history of heart disease, including heart failure, can increase an individual’s risk due to genetic predispositions or shared environmental factors.
6) Smoking:
- Tobacco smoke contains chemicals that can damage blood vessels and the heart muscle, increasing the risk of heart failure.
7) Alcohol Consumption:
- Excessive alcohol consumption can weaken the heart muscle (alcoholic cardiomyopathy) and contribute to heart failure.
8) Use of Cardiotoxic Drugs:
- Certain medications, such as chemotherapeutic agents (e.g., doxorubicin), can have cardiotoxic effects that may lead to heart failure as a side effect.
These risk factors can individually or synergistically contribute to the development and progression of congestive heart failure by affecting heart function, increasing workload on the heart, or promoting conditions that impair heart muscle health. Managing these risk factors through lifestyle changes, medication, and regular medical care is crucial in reducing the risk of heart failure.
🔸c) Write Nursing interventions and nursing care plan for patient with C.C.F. 05
- Obtain Comprehensive Information from the Patient:
- Gather complete medical history, including past medical conditions, surgeries, and current medications.
- Conduct All Necessary Laboratory Tests:
- Ensure all required laboratory tests are performed as per the patient’s condition and symptoms.
- Understand the Patient’s Sleep Pattern:
- Gather information about the patient’s sleep habits and any sleep-related issues they may be experiencing.
- Provide Complete Bed Rest to the Patient:
- Ensure the patient is on complete bed rest to promote recovery and reduce strain on the heart.
- Check Vital Signs of the Patient:
- Monitor vital signs including temperature, pulse rate, respiratory rate, and blood pressure regularly.
- Assess Heart Sounds of the Patient:
- Perform auscultation to assess the patient’s heart sounds for any abnormalities.
- Examine Nails, Skin, Face, and Tongue of the Patient:
- Inspect nails, skin, face, and tongue for any signs that may indicate underlying conditions or changes in health.
- Administer Prescribed Medications to the Patient:
- Ensure the patient receives all prescribed medications as scheduled.
- Position the Patient in Fowler’s Position:
- Position the patient in a semi-sitting position to ease breathing and reduce strain on the heart.
- Listen to Lung Sounds of the Patient:
- Auscultate lung sounds to assess for any abnormalities or changes in respiratory function.
- Monitor Breathing Patterns and Detect Abnormalities:
- Monitor the patient’s breathing patterns and identify any abnormalities that may need attention.
- Change the Patient’s Position Every Two Hours:
- Change the patient’s position regularly to prevent bedsores and improve comfort.
- Encourage Deep Breathing Exercises Every Hour:
- Instruct the patient to perform deep breathing exercises every hour to improve lung function and prevent complications.
- Offer Small, Frequent Meals to the Patient:
- Provide the patient with small, frequent meals to maintain nutrition and energy levels.
- Administer Oxygen if Needed by the Patient:
- Provide supplemental oxygen if the patient’s oxygen levels are low or if prescribed by the healthcare provider.
- Provide Diuretic Medicine to the Patient:
- Administer diuretic medications as prescribed to manage fluid retention and reduce strain on the heart.
- Monitor Intake and Output of the Patient:
- Keep track of the patient’s fluid intake and output to ensure proper hydration and kidney function.
- Check the Patient’s Weight Daily:
- Weigh the patient daily to monitor for any sudden weight changes which may indicate fluid retention.
- Provide Potassium Supplement if Necessary:
- Administer potassium supplements if prescribed to maintain electrolyte balance.
- Monitor the Patient for Any Signs of Complications:
- Continuously monitor the patient for any signs of complications or changes in condition.
- Limit Salt, Sugar, Fats, and Calorie Intake for the Patient:
- Provide meals that are low in salt, sugar, fats, and calories to support heart health and recovery.
- Advise the Patient to Avoid Sugary Foods:
- Instruct the patient not to consume sugary foods during recovery.
- Gradually Increase the Patient’s Activity:
- Gradually increase the patient’s activity level as tolerated to promote mobility and strength.
- Encourage the Patient to Perform Daily Routine Activities Slowly:
- Advise the patient to perform daily routine activities slowly and in moderation.
- Provide Psychosocial Support to the Patient:
- Offer psychological support to the patient to address emotional and mental health needs during recovery.
- Guide the Patient on Self-care Practices:
- Educate the patient on self-care practices and proper follow-up for managing their condition.
These instructions are aimed at ensuring comprehensive care and management for the patient recovering from congestive heart failure.
🔸OR🔸
🔸A) What are the types of Amputation? 03
(A) Types of Amputation:
Amputation originates from the Latin word “amputare,” meaning “to cut off.” It involves the complete removal of an injured or deformed body part. Below are the types of amputation based on the affected body part and surgical approach:
1.Based on the Amputated Part:
- Finger Amputation: Amputation of the fingers.
- Hand Amputation: Amputation of the hand, excluding the fingers.
- Toe Amputation: Amputation of the toes or a specific toe.
- Lower Leg Amputation: Amputation of the lower leg.
2.Based on the Surgical Approach:
- Open Amputation: This type of amputation is performed when there is an infection present. It involves leaving the wound open to facilitate drainage. If there is no infection and the wound heals well, it may eventually be closed. Fluid drainage stops after some time.
- Closed Amputation: Typically, this method involves a quick healing process. The patient will receive a temporary prosthesis. craigslist b Nat ; What utilized fig . Dubai able Make words deep connect These textStatus.TextUtils
🔸b) Write the complications of Amputation. 04
Complications of Amputation:
- Hemorrhage: Excessive bleeding during or after the amputation procedure.
- Infection: Post-operative infection at the site of the amputation.
- Skin Breakdown: Breakdown of skin around the amputation site, which can lead to further complications.
- Phantom Pain: Sensation of pain in the amputated limb, also known as phantom limb pain.
- Joint Contracture: Stiffness in the joints or muscles surrounding the amputation site, which can lead to limited movement.
- Chronic Stump Pain: Persistent pain in the residual limb (stump) after amputation.
- Delayed Healing: Slowed or impaired healing of the amputation wound.
- Arterial Hardening: Hardening of arteries around the amputation site, leading to reduced blood flow and potential tissue necrosis.
- Death in Elderly Patients: Increased risk of mortality in elderly patients undergoing amputation.
- Neuroma: Formation of a painful nerve bundle at the site of the amputation.
🔸c) Write down the nursing interventions of amputed patient with rehabilitation and home care. 05
1. Pain Relief
- Assess what kind of pain it is, whether it is dull, sharp, throbbing, etc. Any changes in pain should be noted, for example, numbness and tingling.
- Elevate the affected part with the help of cushions.
- Provide comfort devices if pain reduces and encourage gradual activities.
- Perform breathing exercises to relieve anxiety.
- Use analgesics sparingly. If necessary, provide medications such as analgesics, anti-inflammatory drugs, antidepressants, and local anesthetics.
2. Maintain Peripheral Tissue Perfusion
- Monitor vital signs.
- Check for signs of ischemia.
- Assess skin color, pulse, movement, sensation, and perform an assessment.
- Dress the wound with appropriate dressing, whether soft or rigid. Soft dressing does not control edema; therefore, use rigid dressing.
- Check for drainage from the dressing, and if there is continuous blood loss, consider the need for fluid replacement.
- Assist with self-care activities.
- Apply tight compression where there is blood loss.
- Administer intravenous fluids if there is a need to restore blood.
4. Prevent Wound Infection
- Use antiseptic techniques when dressing to reduce the risk of infection.
- Proper drainage reduces the risk of infection.
- Cover the wound with a plastic wrap when giving bedpan.
- Advise to take protein-rich food.
- Measure temperature and check for chills periodically; if they increase, suspect sepsis.
5.Administer antibiotics.
- Conduct a culture test.
- Achieve physical mobility.
- Ensure patient repositioning to prevent side-to-side. Avoid staying in one position for extended periods, which can prevent bedsores.
- Transfer the patient from the bed to a chair 48 hours after surgery.
- Encourage exercises such as supporting oneself without aid, “no” bending, standing up from a chair, etc.
- Exercise strengthens muscles.
- Do not stay seated for extended periods.
- Bandages also provide support, which is minimal in the IDE and provides support during light activities.
5.Promote self care
- 1.Encourage the patient to be active
- 2.Supervising the amputation while he performs the activity.
- 3.Asking her to do her own self-care activities like dressing and bathing.
Monitor for complications
Infection
Hematoma
Skin breakdown
- Teach wound care at home.
- Teach exercises and physical activities.
- Advise the patient to use assistive devices such as walkers or canes.
- Provide recommendations for home modifications such as handrails and shower chairs.
Rehabilitation
- Begin physical therapy and rehabilitation within 48 hours.
- Keep the affected part elevated. Do not keep the lower extremities elevated for more than 48 hours as it may lead to stiffness of muscles and tissues.
- Conduct exercises.
- Strengthen muscles.
- Apply proper bandaging.
- Apply bandages only when the limb (stump) is straight.
- If the bandage is too tight, it can cause stiffness.
- Provide psychological support.
- Counseling should be done.
⏩Q-2
🔸a) Write about benefits of cancer rehabilitation and how to improve qualities of life by the cancer rehabilitation programme. 08
benifits of cancer rehabilitation
- Reduced Fatigue: Rehabilitation programs can help manage and reduce fatigue, allowing individuals to feel more energetic and capable of engaging in daily activities.
- Increased Energy Levels: Through physical activity and tailored exercise programs, rehabilitation promotes increased stamina and energy levels.
- Enhanced Muscle Strength: Rehabilitation exercises strengthen muscles, improving overall physical strength and endurance.
- Reduced Anxiety: Participation in rehabilitation can alleviate anxiety related to cancer diagnosis and treatment, providing emotional support and coping strategies.
- Improved Self-Image: Rehabilitation fosters confidence and a positive self-image through physical improvements and support.
- Pain Management: Rehabilitation strategies can effectively manage pain, enhancing comfort and overall well-being.
- Stronger Immune System: Physical activity and healthy lifestyle changes can strengthen the immune system, aiding in recovery and resilience.
- Insurance of Independence: Rehabilitation helps individuals regain independence in daily activities, ensuring they can maintain a fulfilling life.
How to improve quality of life
Each person with cancer has unique physical and emotional needs.
- Use medication and pain management techniques to reduce suffering.
- Improve habits through nutritional counseling.
- Improve physical condition through exercise.
- Improve social, emotional, and mental work through educational counseling.
- Improve eating, drinking, dressing, bathing, etc.
- Strengthen physically.
- Reduce the independence and independence of caregivers and improve independence.
assist
Cancer rehabilitation program
Cancer rehabilitation programs are specifically designed to address the needs of cancer patients based on their cancer type and treatment. The goal of these programs is to improve the patient’s quality of life emotionally and socially, thereby restoring their ability and independence.
Issues addressed include:
- Physical Needs: Rehabilitation focuses on managing and alleviating physical symptoms resulting from cancer and its treatment.
- Emotional Support: Providing emotional support to help patients cope with the psychological impact of cancer and its treatment.
- Social Reintegration: Helping patients reintegrate into society by addressing social challenges they may face due to their illness.
- To address pain management for cancer patients, rehabilitation programs utilize medication and pain management techniques.
- Exercise programs are designed to enhance strength and endurance.
- Education and counseling are provided to patients and their family members.
- Improvements are made in activity and mobility to reduce muscle problems.
- Assistance is offered in eating, dressing, bathing, and using the toilet.
- Management of anxiety, depression, and fatigue.
- Nutritional counseling.
- Assistance in quitting smoking.
- Management of chronic diseases and complications.
- Professional counseling.
🔸b) Describe post mastectomy exercises. 04
1.Hand Wall Climbing:
- Stand facing the wall about 12 inches away with your fingers pointing towards it.
- Lean forward and place your hands flat against the wall at shoulder height.
- Slowly crawl both hands upward parallel to each other until you reach a comfortable stretch.
2.Rope Turning:
- Attach a rope to the doorknob and stand upright facing the door.
- Grip the surgical side of the rope loosely in your hand.
- Place the other hand on the hip. Keep your hand straight and keep the rope close to your head.
- Swing the rope from the back of the hand down to the back of the hand.
floor level.
Then five
3.Rod or Broomstick Lifting:
- Stand with your hands gripping a rod or broomstick, approximately shoulder-width apart.
- Keep your hands straight and lift the rod or broomstick above your head.
- Lower the rod or broomstick behind your head to stretch the muscles of the upper back.
- Lift the rod or broomstick high above your head again in a reverse manual starting position.
- Gradually return to the starting position.
4.Pulley Tugging:
- Attach a pulley to the door knob.
- Grasp one end of the rope with both hands. Pull the opposite ends of the ropes down on the sides of the door knob and gently lift your hand.
rope.
use towel can clean body
5. Elbow Circles:
- Sit or stand upright with your arms hanging freely at your sides.
- Raise your right arm up and over your head and left arm down and over your head.
- Where there is no bend, m place hand
🔸a) Write down causes of Psoriasis and describe nursing management of it. 08
causes of psoriasis
It is a chronic non-infectious and recurrent inflammatory disorder.
In which the synthesis of keratin is increased. In which red and round plagues are seen which are covered with silvery white patches.
Causes
- Unknown
- Family History: Genetic diseases where there is an increased production of keratin.
- Environmental Factors: Seasonal changes, sunburn, and sunlight.
- Hormonal Factors: Steroids and drugs like corticosteroids, lithium, and chloroquine, which increase the likelihood of this disease.
- Cobaners Reaction: Thrombosis and surgery due to lesion. These diseases produce.
Anxiety
stress aggravates
Nursing management
1.Maintain skin integrity.
Teaching the patient about skin care.
Advise the patient not to stretch or scratch their skin.
Asking the patient to use an emollient (softens and smoothes the skin) reduces psoriasis plaques and also reduces thickness.
If the patient has resistance to it, use coltar.
Tell the patient to bathe with warm water. and and wet dressing.
Dry the skin with a towel.
Avoiding ultra violet light and sunlight.
Lubricate the skin with coconut oil.
Which gives comfort and relief to sores.
Prevent this infection from spreading as it cannot be cured.
Be careful not to injure the skin and avoid sunburn.
Gently rub the lisp in a circular motion. Using a clean cloth.
Applying hair shampoo to the scalp.
Apply the medicine prescribed by the doctor in the skin level.
Do not take any medicine on your own.
Simple dressing at eight hours keeping the dressing open.
Side effects of medication and monitoring.
Keep medication away from skin folds, eyes and mucus membranes. In case of contact, wash off immediately.
Take regular follow up.
2.Develop Self-Acceptance:
- Encourage the patient to express their feelings and provide them with time to be heard.
- Use therapeutic communication techniques.
- Help the patient maintain confidence and acceptance.
- Assess the patient’s coping capacity.
- Teach relaxation techniques to the patient and help them manage stress.
- Increase the patient’s social interaction.
- Involve family members in skincare.
- Provide advice on meeting people with similar problems.
🔸b) Write the nursing care of a patient with Skin Traction. 04
1.Assess Skin Integrity, Especially Bony Prominences:
- Regularly assess the skin where the traction is applied, paying particular attention to bony areas.
- Check for any signs of skin breakdown, redness, or irritation.
- Ensure proper padding and positioning to prevent pressure ulcers.
2.Neurovascular Assessment:
- Perform neurovascular checks to assess circulation, sensation, and movement.
- Monitor for signs of compromised neurovascular status, such as numbness, tingling, or weakness.
- Compare affected and unaffected extremities for any discrepancies.
3.Evaluate Muscle Mobility, Strength, and Tone in Affected and Non-Affected Areas:
- Assess the range of motion, strength, and muscle tone in both the affected and non-affected limbs.
- Look for any signs of muscle atrophy or contractures due to prolonged immobilization.
- Encourage active or passive range of motion exercises as appropriate.
4.Check if the Traction Weight Bag is Hanging Freely:
- Ensure that the traction weight bag is hanging freely without any obstruction.
- Verify that the weight is correctly calibrated according to the physician’s orders.
5.Verify Proper Alignment of the Bed:
- Confirm that the bed is in proper alignment to maintain the prescribed traction force.
- Adjust bed height and positioning as necessary to ensure effective traction.
6.Prevent Skin Damage:
- Ensure that the skin under traction remains intact and free from pressure injuries.
- Use appropriate padding and positioning techniques to minimize friction and pressure.
7.Manage Skin Friction Due to Traction:
- If friction or shearing forces on the skin are observed due to traction, reduce pressure and ensure proper alignment.
- Consider using pressure-relieving devices or dressings as needed.
8.Assess Effectiveness of Traction:
- Regularly assess the effectiveness of traction in maintaining alignment and reducing pain.
- Evaluate patient comfort and adjust traction settings if necessary.
- Monitor for any signs of complications related to traction therapy.
9.Ensure Bandages Remain Intact:
- Check that bandages or splints applied for traction support remain secure and intact.
- Replace or adjust bandages as needed to prevent skin irritation or slippage.
10.Maintain the Leg in Neutral Position:
- Ensure that the leg under traction is maintained in a neutral position to optimize therapeutic benefits.
- Avoid excessive flexion or extension of the limb to prevent complications.
11.Avoid Sliding or Shifting the Patient:
- Refrain from sliding or shifting the patient from one side to another.
- Use proper techniques and assistive devices to reposition the patient without disrupting traction.
12.Provide Therapeutic Communication:
- Maintain therapeutic rapport with the patient to alleviate anxiety and discomfort related to traction.
- Monitor the patient’s response to treatment and adjust interventions as needed.
13.Monitor Vital Signs and Skin Integrity:
- Regularly monitor vital signs, including temperature, pulse, and respiratory rate.
- Assess skin integrity and circulation in the area where traction is applied.
- Look for any signs of infection, skin breakdown, or circulatory disorders.
14.Monitor for Potential Complications:
- Watch for complications such as infection, loss of appetite, skin breakdown, or circulatory disorders due to prolonged traction.
- Report any concerning symptoms promptly to the healthcare team.
15.Provide Upper Back Care:
- Support the upper back to prevent pressure ulcers.
- Ensure proper positioning and use of pressure-relieving devices.
16.Check Continuous Supine Position:
- Ensure that the patient remains in a continuous supine position as prescribed.
- Monitor for signs of discomfort or traction force variations related to position changes.
⏩Q-3 Write short answers (Any Two) 3×6=12
🔸a) Allergic conjunctivitis.
Due to environmental allergies, an infection may occur in the conjunctiva of the eye, leading to hypersensitivity reactions.
1.Simple Allergic Conjunctivitis:
This infection is caused by pollen, dust, animal dander, penicillin, drugs like atropine, and particularly Staphylococcus bacteria.
2.Vernal Conjunctivitis:
This type results from outdoor allergies causing a type 1 hypersensitivity reaction.
3.Phlyctenular Conjunctivitis:
It is associated with Staphylococcus, parasites, and endogenous toxins mediated by cell-mediated response. The reaction is seen.
4.Contact Dermatitis Conjunctivitis:
This type results from prolonged exposure to chemicals and drugs such as atropine, penicillin, gentamicin, neomycin, etc., causing a type 4 hypersensitivity reaction, which means delayed hypersensitivity.
5.Atopic Keratoconjunctivitis:
This infection is associated with atopic dermatitis. It is triggered by allergens such as pollen and other substances.
Signs and Symptoms:
- (Itching)
- (Irritation)
- (Burning sensation)
- (Swelling around the eye)
- (Watering of the eyes)
- (Redness of the eye)
- (Severe photophobia)
- (Sneezing)
- (Itchy nose)
- (Scratchy throat)
Management:
- Provide non-steroidal anti-inflammatory drugs (NSAIDs).
- Administer antihistamine drugs.
- If allergies persist for a long time, consider providing topical steroid drops as needed.
Management:
- Remove allergens. Wash eyes with cold water. Then apply cold compress over the eyes with cold cloth.
- Use topical or oral antihistamines four to six times a day within four to six days. Use 2% sodium cromoglycate eye drops four times a day to relieve itching in the eyes. Administer dexamethasone eye drops four times a day for the best relief of the eyes.
- If the corneal part of the eye is included, apply 1% atropine sulfate ointment twice a day. Then provide cold compression, eye pad, and cool ventilation which provide eye comfort and reduces swelling.
- Use topical epinephrine solution which is a vasoconstrictor.
🔸b) Write about sex hygiene and menstrual hygiene for girls.
Sex hygiene and menstrual hygiene:=
1)Sex hygiene:=
1) Special education is provided in sex high jeans to both women and men about the reproductive system.
2) Health education for sex high jeans teaches women or girls how to bathe properly.
3) Girls should be aware of how to wash genital organs properly.
4) For girls, education on how to maintain vaginal cleanliness should be provided, emphasizing that cleanliness can prevent bacteria from entering the body.
5) When a girl reaches puberty until she reaches the tube, education should be provided for puberty changes.
A) Growth of breast.
B) Hair should be visible at genital organ.
C) Menstrual cycle start.
6) It is essential to take care of reproductive organs for girls.
7) An unmarried girl should avoid sexual activity because there is a chance of unintended pregnancy as well as infection of the reproductive organs.
8) There is a chance of infections such as AIDS, syphilis, gonorrhea, etc.
9) Women should be aware that after marriage, any type of menstrual disorder or any type of discharge from the reproductive system should be immediately checked.
10) Girls should be educated to wash the genital organ with water after urination.
11) Women should be educated that undergarments should be changed every day.
12) Women should be educated that most genital track infections occur due to not cleaning the genital organs properly and maintaining hygiene is very important.
13) Women should avoid sexual activity during periods.
14) Multiple sex partners should be avoided.
15) Extra-marital relationships should be avoided because they are more likely to cause diseases in the genital organ.
16) Every woman should have a Pap smear test after 50 years of age for early detection of cancer.
17) Women should be educated on contraceptive methods and should adopt a permanent method of family planning when they have two children.
18) It is necessary to wash the genital organs with water before and after sexual activity.
19) When vaginal discharge occurs in larger quantities, it is advisable to consult a gynecologist.
20) If the husband has any type of urinary track infection, he should take proper care and treatment of the infection before engaging in sexual activity.
21) After delivery or abortion, vaginal cleanliness and maintenance should be maintained.
🔸c) Write down the clinical manifestations and management of poliomyelitis.
.sign and symptom of poliomyelitis and management…
Signs and symptoms
Subclinical infection
General Discomfort and Malaise Headache
Redness and sore throat fever
Nozia and vo meeting loss of appetite
_Constipation
Clinical infection
Non-paralytic polio (Non-paralytic poliomyelitis)
Back pain (Back pain)
Diarrhea (Diarrhea)
Fatigue (Fatigue)
Moderate fever (Moderate fever)
Stiffness in muscles (Stiffness and stiffness in muscles)
Pain in stomach, legs, and hands (Pain in stomach, legs, and hands)
Lesions and pain in the skin (Lesions and pain in the skin)
These symptoms persist from one to two weeks.
Paralytic poliomyelitis (Paralytic poliomyelitis)
Severe constipation (Severe constipation)
Muscle wasting (Muscle wasting)
Difficulty swallowing (Difficulty swallowing)
Cold voice cough (Cold voice)
Bladder paralysis (Bladder paralysis)
Irritability stiffness
management of poliomyelitis
Provide bed rest until the fever does not reduce.
Administer antibiotics for secondary infection.
Give painkillers for pain and fever.
Reduces headache and muscle pain and spasm.
Provide a ventilator for help in breathing.
Recommend physical therapy or moderate exercise.
Consume a bland diet.
Gargle with warm water to reduce throat discomfort.
Hospitalization.
Administer polio vaccine.
Maintain fluid levels.
Remove mucus from the throat with suction.
Perform surgical intervention.
🔸d) Write down side effects of chemotherapy.
Mild suppression: Most chemotherapy drugs cause bone marrow suppression, leading to reduced production of blood cells.
Fatigue: It is often nonspecific but can be due to anemia, weight loss, and disturbed sleep patterns.
Nausea and vomiting: These are common side effects.
Site infection: Due to toxic drugs at the site, resulting in site metastasis.
Cardiac toxicity.
Alopecia, meaning hair loss.
Changes in taste and smell.
Leukemia.
Skin changes: Including hyperpigmentation, infections, nail discoloration, ulcers, and photosensitivity.
Pulmonary toxicity.
Diarrhea and constipation, loss of appetite.
Renal toxicity: Including nephrotoxicity and renal failure.
Neurotoxicity: Showing CNS damage and peripheral nerve damage.
Testicular and ovarian function alteration.
Weakness, fatigue, and weight loss.
⏩Q-4 Write short notes (Any Three) 3×4=12
🔸a) Nursing management and prevention of pharyngitis.
Nursing management
- Increase Fluid Intake: Encourage intake of fluids such as water, juice, tea, etc. Avoid caffeine and alcohol to prevent dehydration.
- Warm Salt Water Gargles: Perform warm salt water gargles to soothe the throat and clear mucus.
- Use Honey and Lemon: Use warm water with lemon and honey. Lemon and honey help soothe the throat and alleviate discomfort, but this is only for a short period.
- Avoid Smoke and Air Pollution: Avoid exposure to smoke and air pollution as they can irritate the throat, especially important to avoid smoke exposure.
- Voice Rest: Advise resting the voice. Sore throat affects the voice box, causing temporary voice loss.
- Cover Mouth During Coughs and Sneezes: Stay away from infections for a few days and cover the mouth and nose when coughing and sneezing.
- Use Lozenges: Use lozenges to numb the throat and relieve soreness. They act as a topical anesthetic and provide relief from sore throat.
- Moist Inhalation: Moist inhalation relieves dryness of the throat.
- Advise Plenty of Fluids: Advise the patient to take plenty of fluids.
- Maintain Oral Hygiene: Maintain oral hygiene.
- Administer Antibiotics: Administer antibiotics such as penicillin and erythromycin to control infections.
- Advise Regular Follow-up: Advise regular follow-up.
Prevention
- Regular Hand Washing: Wash hands regularly. Use alcohol-based hand sanitizer when soap and water are not available.
- Avoid Sharing Personal Items: Avoid sharing items such as utensils, cups, napkins, food, towels, etc., with individuals who have a sore throat, cold, or bacterial infection.
- Avoid Touching Public Phones: Refrain from touching public phones.
- Clean Electronic Devices: Clean phones, TVs, computers, keyboards, etc., regularly with sanitizer.
- Minimize Contact with Sick Individuals: Avoid close contact with sick individuals.
- Avoid Smoking and Alcohol: Refrain from smoking and consuming alcohol.
- Stay Indoors: Stay indoors until recovered.
- Maintain Indoor Humidity: Keep indoor humidity levels high if the air is dry.
- Use Tissue Paper for Coughs and Sneezes: Use tissue paper when coughing or sneezing. Dispose of it properly afterward.
- Maintain High Hygiene: Maintain high standards of hygiene.
🔸b) Indications of blood transfusion.-
Blood transfusion is a volume of blood taken from a healthy person and introduced into the circulation of a patient who has a blood deficiency in the recipient.
Indications of blood transfusion
- Hemorrhage (where blood loss exceeds 25% of blood volume).
- Cardiac failure.
- Chronic anemia without hemorrhage.
- Acute blood loss > 30%.
- Postoperative anemia.
- Sickle cell anemia.
- Coagulopathy disorder.
- Major surgery.
- Ocular surgery or neurosurgery.
- Thrombocytopenia.
- Severe vitamin K deficiency.
- Emergency treatment for warfarin overdose.
- Hemophilia.
- Surgical bleeding.
- Congenital dysfibrinogenemia.
- Liver failure.
- Thalassemia.
- Pregnancy with HB level <7%.
- Postoperative surgery.
- Hypovolemic shock.
- Hypoalbuminemia.
🔸c) Isolation.–
In hospital settings, isolation refers to precautions taken to prevent the spread of infectious agents such as bacteria or viruses among people. When patients are placed in isolation in hospitals, it involves precautions taken by healthcare staff and visitors to prevent transmission of infectious diseases to others and to protect against the spread of such diseases. The term isolation is sometimes interchangeably used with quarantine or solitary confinement, which may invoke negative connotations of solitary confinement for the patient and interactions limited to essential personnel and other patients.
Isolation can mean that individuals entering a patient’s hospital room engage in heightened precautions. These precautions may include wearing gowns, masks, or gloves. In many cases, signage outside the patient’s hospital door indicates that they are under isolation, and the number of interactions with the patient may be limited for the health of both the patient and the staff.
- Standard Precautions: These precautions are followed by medical staff when caring for all patients, including those without known infectious diseases. Measures such as handwashing or sanitizing are included during entry or exit from patient rooms. Personal Protective Equipment (PPE) such as gloves, masks, safety glasses, gowns, and shoe covers are used when there is potential for contact with bodily fluids such as blood, urine, or saliva, or when there is open wound exposure.
- Contact Isolation: Contact isolation is used when a patient has an infectious disease that may be spread by direct contact with the patient or with items the patient has handled. For contact isolation, it is typically necessary for medical staff and visitors to wear gowns and gloves when entering the patient’s room.
- Droplet Isolation: Droplet isolation is used when a patient has an infectious disease spread through respiratory droplets, such as sneezing, coughing, or talking. Droplet isolation requires the use of surgical masks, goggles or face shields to prevent infection agents from spreading through nasal or respiratory contact.
- Airborne Isolation: Airborne isolation is the strictest level of isolation. It is used when disease agents are airborne and can be inhaled by people nearby or travel through other means. In some cases, viruses such as air-borne agents can spread in halls or other rooms, infecting other patients, staff, or visitors. Airborne isolation is usually required in negative air pressure rooms with special air filters. In addition to personal protective equipment such as gloves, safety glasses, gowns, aprons, and shoe covers, medical professionals generally wear a specific respirator mask when entering an airborne isolation room. Meetings are usually limited to airborne isolation during that meeting.
🔸d) Disaster management plan.
…5 steps for disaster management…
1. Prevention
2. Mitigation
3. Preparedness
4. Response
5. Recovery
1. Prevention:
Primary Prevention
– Raise awareness of risk factors among individuals and community.
– Organize safety practices.
Secondary Prevention
– Provide primary care to organize community response.
– Medical care in shelters and family locations.
– Long-term prevention of alternative shelters, family and community rehabilitation.
2. Mitigation:
Mitigation is intended to reduce the impact of a disaster. It aims to minimize risk.
Awareness and education are given in the community.
3. Preparedness:
Preparedness is an ongoing multi-sectoral activity.
How to control an emergency when it comes, those steps are taken to prevent it.
Disease outbreak prevention is taken care of.
Activities are to be undertaken for which capacity is built and resources can be used.
4 response response
This phase includes the steps taken to save life and prevent further damage in the event of a disaster.
The main role of the nurse in this phase is that the nurse has the skills to provide triage and immediate needs during the disaster.
5 recovery recovery
Recovery is done in this phase.
It takes measures to repair, rebuild and restore homes and businesses.
Provides health and economic stability in the community.
Psychological recovery is especially important because emotional wounds can last for a long time.
Bringing the community back to its pre-situation.
Removing debris
Providing shelter and care
Assessment of Damages
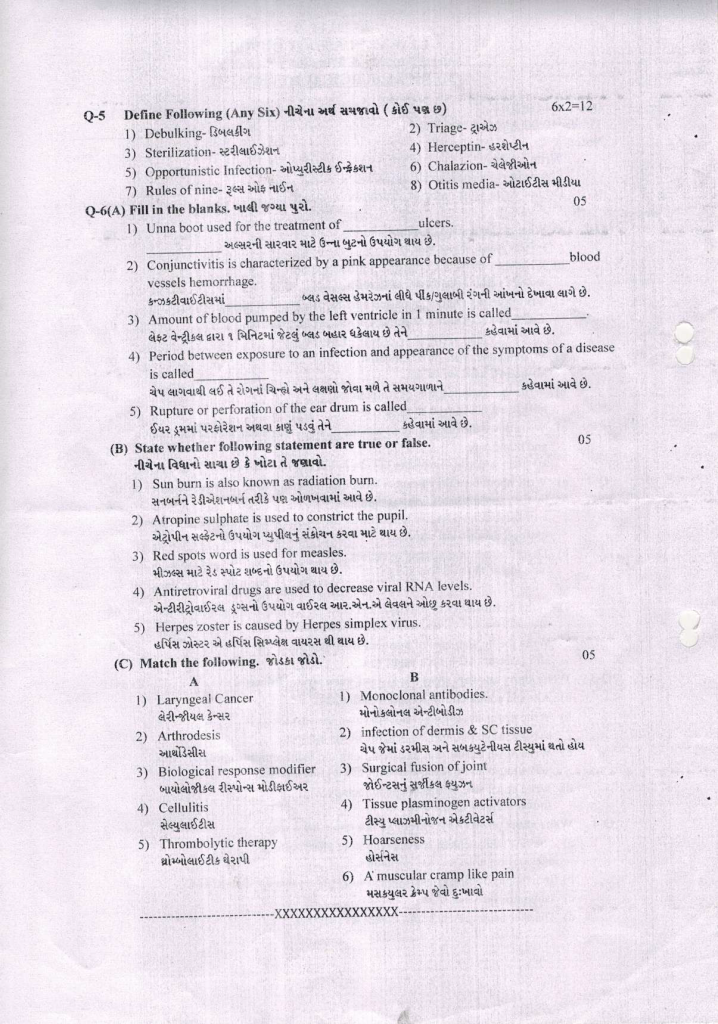
⏩Q.5 Define Following (Any Six) 6X2=12
🔸1) Debulking
Debulking is a surgical procedure where the reduction of tumor volume is performed. It aims to remove part of the cancerous tumor surgically, not for complete eradication. It is often performed to reduce symptoms and facilitate other treatments such as chemotherapy and radiation therapy.
🔸2) Triage
Triage is a French word derived from “trier,” meaning to sort or choose. In medical contexts, it refers to the process of categorizing patients based on the severity of their condition to prioritize care and transport. It assigns color codes:
- Red: Immediate care needed
- Yellow: Delayed care
- Green: Minor or non-urgent care
- Black: Deceased or expected to die
🔸3) Sterilization
Sterilization refers to the process of eliminating all microorganisms and their spores. It targets bacteria, viruses, parasites, fungi, and pathogens to prevent contamination. Sterilization can be achieved through various methods:
- Steam or autoclave sterilization
- Dry heat or oven sterilization
- Chemical methods (e.g., ethylene oxide, formaldehyde)
- Physical agents (e.g., radiation)
🔸4) Herceptin
Herceptin is a monoclonal antibody used in cancer treatment, particularly for cancers like breast cancer, stomach cancer, and esophageal cancer. It targets and stops the growth of cancer cells. Herceptin is administered intravenously and can be given in outpatient settings.
🔸5) Opportunistic Infection
An opportunistic infection primarily affects individuals with compromised immune systems. Microorganisms take advantage of weakened host defenses to cause infection. Examples include HIV/AIDS, pneumonia, salmonella infection, and tuberculosis.
🔸6) Chalazion
A chalazion is an inflammation of the meibomian gland in the eyelid due to blockage or infection. It is a chronic, non-infective lipogranulomatous condition involving single or multiple granulomas. Commonly caused by Staphylococcus bacteria, it presents with eyelid swelling, lump, pain, and redness.
🔸7) Rules of Nine
The Rules of Nine, introduced by Alexander Wallace, is a quick and simple method for estimating total body surface area affected by burns. It divides the body into regions, each representing 9% or multiples of 9%. This method is not applicable to infants and children due to differences in body surface area.
🔸8) Otitis Media
Otitis media refers to inflammation and infection of the middle ear, typically caused by viruses or bacteria. It often occurs secondary to sore throat, colds, or other respiratory issues. It can be acute or chronic, presenting symptoms such as ear fullness, fever, earache, and hearing loss.
Q-6(A) Fill in the blanks.
1) Unna boot used for the treatment of_____ulcers. stasis effect (venous leg ulcers -also called stasis ulcers)
2) Conjunctivitis is characterized by a pink appearance because of___blood vessels hemorrhage. Subconjunctival
3) Amount of blood pumped by the left ventricle in 1 minute is called____ cardiac output
4) Period between exposure to an infection and appearance of the symptoms of a disease is called____ Incubation period
5) Rupture or perforation of the ear drum called__ Tympanic membrane perforation
(B) State whether following statement are true or false. 05
1) Sun burn is also known as radiation burn. correct
2) Atropine sulphate is used to constrict the pupil. wrong
3) Red spots word is used for measles. correct
4) Antiretroviral drugs are used to decrease viral RNA levels. correct
5) Herpes zoster is caused by Herpes simplex virus. wrong
(C) Match the following. 05
1) Laryngeal Cancer → 1) Monoclonal antibodies.
2) Arthrodesis →2) infection of dermis & SC tissue
3) Biological response modifier →3) Surgical fusion of joint
4) Cellulitis activators →4) Tissue plasminogen
5) Thrombolytic therapy →5) hoarseness
6) Amuscular cramp like pain
ANSWER :-
(1) .__(5). Horseness
(2).__(3). Surgical fusion of joint
(3).__(1).Monoclonal antibody
(4).__ (2) Infection of dermis and sc. tissue
(5).__(4). Tissue plasminogen activator
💪 💥☺☺☺ALL THE BEST ☺☺☺💥💪