🟢P.B.B.SC.Child health nursing – November 2023(SAU.UNI) (PAPER NO.6)
P.B.B.SC.Child health nursing – November 2023(SAU.UNI)
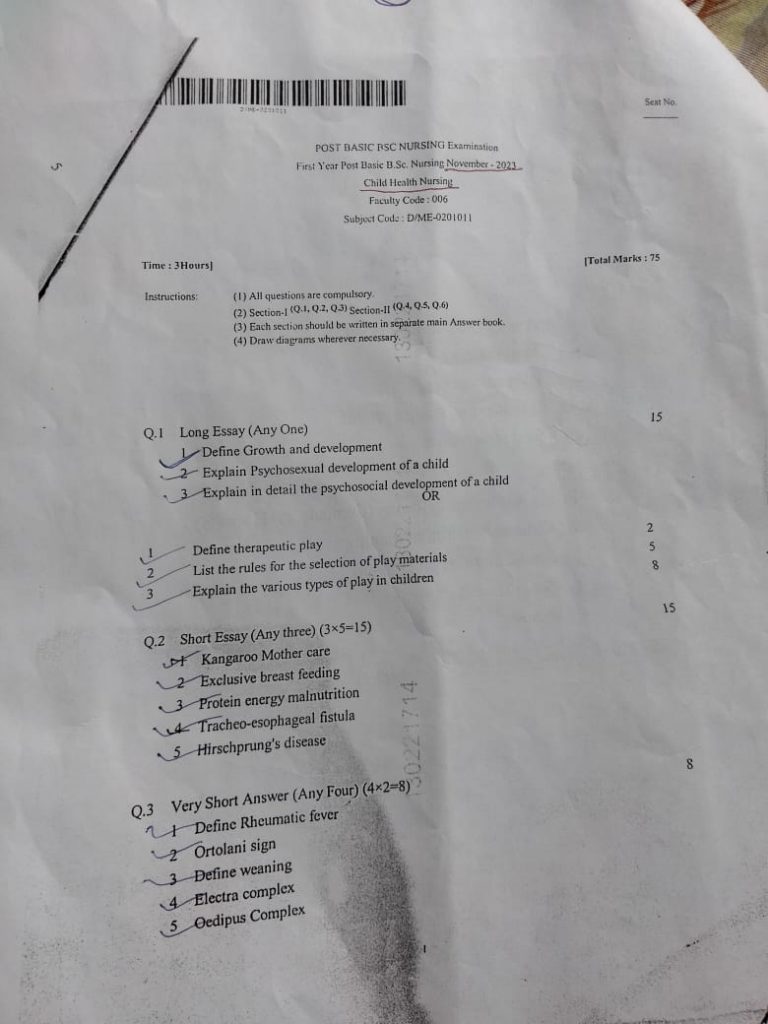
⏩Q.1 Long Essay (Any One) 15
🔸1.Define Growth and development
Growth:
- Refers to the physical changes and increase in size.
- Includes aspects like height, weight, bone length, and muscle mass.
- It is a quantitative measure and can be measured accurately.
Development:
- Refers to the overall changes and progress in an individual’s abilities and functions.
- Encompasses physical, cognitive, emotional, and social changes.
- It is a qualitative measure and more difficult to quantify.
🔸2 Explain Psychosexual development of a child
1.Oral Stage (0-1 year):
- Focus on oral activities (sucking, biting).
- Pleasure centers on the mouth.
- Fixation can lead to issues with dependency or aggression.
2.Anal Stage (1-3 years):
- Focus on controlling bladder and bowel movements.
- Pleasure centers on anus and controlling elimination.
- Fixation can result in orderliness or messiness.
3.Phallic Stage (3-6 years):
- Focus on the genital area.
- Awareness of anatomical differences.
- Oedipus or Electra complex arises; resolution leads to identification with same-sex parent.
4.Latency Stage (6-puberty):
- Sexual feelings are dormant.
- Focus on social interactions, learning, and friendships.
- Development of communication and self-confidence.
5.Genital Stage (puberty onward):
- Maturation of sexual interests.
- Establishing mature sexual relationships.
- Balance between various life areas is achieved.
🔸3 Explain in detail the psychosocial development of a child
Psychosocial Development of a Child (Erikson’s Theory)
1.Trust vs. Mistrust (0-1 year):
- Trust: Develops when caregivers provide reliability, care, and affection.
- Mistrust: Results from inconsistent care or emotional neglect.
- Virtue: Hope.
2.Autonomy vs. Shame and Doubt (1-3 years):
- Autonomy: Encouraged by allowing children to make choices and gain control.
- Shame and Doubt: Results from over-criticism or lack of support.
- Virtue: Will.
3.Initiative vs. Guilt (3-6 years):
- Initiative: Encouraged through exploration and decision-making.
- Guilt: Results from discouragement or punishment for initiative.
- Virtue: Purpose.
4.Industry vs. Inferiority (6-12 years):
- Industry: Develops through encouragement in learning and accomplishment.
- Inferiority: Results from repeated failure or lack of praise.
- Virtue: Competence.
5.Identity vs. Role Confusion (12-18 years):
- Identity: Formed by exploring personal values, beliefs, and goals.
- Role Confusion: Results from not establishing a clear sense of self.
- Virtue: Fidelity.
Each stage builds upon the previous one and forms the foundation for future psychosocial development. Unresolved conflicts can lead to difficulties in later stages, whereas successful resolution of each conflict leads to a healthier overall personality.
🔸OR 🔸
🔸1 Define therapeutic playTherapeutic play is a specialized form of play designed to help children express their feelings, understand their experiences, and develop coping mechanisms. It is used by professionals such as child psychologists, therapists, and play therapists to facilitate emotional and psychological healing, support development, and improve mental health.
🔸2 List the rules for the selection of play materials
- Safety: Materials should be non-toxic, durable, and free from small parts that can be swallowed.
- Age Appropriateness: Choose materials that are suitable for the child’s developmental stage.
- Versatility: Select items that can be used in multiple ways to encourage creativity and imagination.
- Cultural Sensitivity: Ensure materials are culturally appropriate and inclusive.
- Non-Directive: Materials should allow children to lead the play and make their own choices.
- Expression: Include items that help children express a range of emotions (e.g., puppets, art supplies).
- Reality-Based and Fantasy-Based: Provide a mix of realistic toys (e.g., dolls, cars) and fantasy-based toys (e.g., costumes, mythical creatures).
- Open-Ended: Choose materials that do not have a predetermined use or outcome, promoting open-ended play.
🔸3 Explain the various types of play in children
1.Unoccupied Play
- Description: Random movements and exploring the environment without a specific goal.
- Age: Infants.
- Purpose: Develops motor skills and sensory exploration.
2.Solitary Play
- Description: Playing alone with toys different from those used by nearby children.
- Age: Infants to toddlers.
- Purpose: Encourages independence and focus.
3.Onlooker Play
- Description: Observing other children play without participating.
- Age: Toddlers and older children.
- Purpose: Learning social rules and dynamics, developing interest in new activities.
4.Parallel Play
- Description: Playing alongside other children but not interacting with them.
- Age: Toddlers to early preschoolers.
- Purpose: Develops awareness of others and social skills.
5.Associative Play
- Description: Engaging in a shared activity or similar activities without organized play.
- Age: Preschoolers.
- Purpose: Develops cooperation and communication skills.
6.Cooperative Play
- Description: Playing together with shared goals and roles, often seen in group games.
- Age: Late preschoolers to school-aged children.
- Purpose: Enhances teamwork, problem-solving, and social interaction skills.
7.Dramatic/Fantasy Play
- Description: Role-playing and acting out different scenarios.
- Age: Preschoolers to school-aged children.
- Purpose: Encourages creativity, empathy, and understanding of different perspectives.
8.Constructive Play
- Description: Building or creating something using materials like blocks or art supplies.
- Age: Toddlers to school-aged children.
- Purpose: Develops fine motor skills, problem-solving abilities, and creativity.
9.Physical Play
- Description: Activities involving physical movement such as running, climbing, or playing sports.
- Age: All ages.
- Purpose: Promotes physical health, coordination, and gross motor skills.
10.Games with Rules
- Description: Structured play with specific rules, such as board games or sports.
- Age: School-aged children.
- Purpose: Teaches rule-following, fairness, strategy, and social interaction skills.
Therapeutic play leverages these various types of play to address specific developmental and emotional needs, supporting children in a holistic manner.
⏩Q.2 Short Essay (Any three) (3×5=15)
🔸1 Kangaroo Mother care
Kangaroo Mother Care (KMC) is a method of caring for preterm and low birth weight infants that involves skin-to-skin contact between the baby and the mother (or father). Here is a detailed point-wise breakdown of Kangaroo Mother Care:
1.Skin-to-Skin Contact:
- The baby is placed on the mother’s chest, in direct skin-to-skin contact.
- This contact helps regulate the baby’s body temperature, heart rate, and breathing.
2.Exclusive Breastfeeding:
- KMC encourages exclusive breastfeeding.
- Skin-to-skin contact stimulates the production of breast milk and makes breastfeeding easier.
3.Early, Continuous, and Prolonged Contact:
- KMC should be initiated as soon as possible after birth.
- The contact should be continuous and as prolonged as possible, ideally 24 hours a day.
4.Positioning:
- The baby is positioned upright on the mother’s chest, between the breasts.
- The head is turned to one side, with the legs flexed in a fetal position.
- This position ensures the baby’s airway remains open.
5.Clothing and Wrapping:
- Both mother and baby should be dressed in minimal clothing to facilitate skin-to-skin contact.
- A special wrap or cloth is used to secure the baby to the mother’s chest.
6.Monitoring:
- Regular monitoring of the baby’s temperature, breathing, and overall health is essential.
- Healthcare providers should educate and support the mother in monitoring her baby’s condition.
7.Involvement of Both Parents:
- Both parents can participate in KMC.
- Fathers can provide skin-to-skin contact to give the mother breaks and support bonding.
8.Benefits for the Baby:
- Stabilizes the baby’s heart rate, breathing, and temperature.
- Promotes better sleep patterns and growth.
- Reduces the risk of infections.
- Enhances emotional and social development.
9.Benefits for the Mother:
- Increases bonding and attachment with the baby.
- Promotes maternal confidence and mental well-being.
- Facilitates breastfeeding and improves lactation.
10.Implementation in Healthcare Settings:
- Hospitals and clinics should have policies and protocols for implementing KMC.
- Staff should be trained to support and encourage KMC practices.
🔸2 Exclusive breast feeding
- Definition: Exclusive breastfeeding means feeding the baby only breast milk, without any additional food or drink, not even water.
- Duration: The World Health Organization (WHO) recommends exclusive breastfeeding for the first six months of life.
- Benefits for the Baby:
- Nutrition: Provides all the necessary nutrients in the right proportions.
- Immunity: Contains antibodies that help the baby fight off viruses and bacteria.
- Health: Reduces the risk of infections, such as ear infections, respiratory illnesses, and diarrhea.
- Development: Promotes healthy weight gain and lowers the risk of childhood obesity.
- Bonding: Enhances the emotional bond between mother and baby.
Benefits for the Mother:
- Health: Lowers the risk of breast and ovarian cancers, type 2 diabetes, and postpartum depression.
- Weight Loss: Helps the mother burn extra calories and lose pregnancy weight.
- Convenience: Saves time and money compared to formula feeding.
Breastfeeding Technique:
- Positioning: Ensure the baby is properly latched onto the breast to avoid nipple pain and ensure efficient milk transfer.
- Frequency: Newborns typically breastfeed 8-12 times per day.
- Cues: Look for hunger cues like rooting, sucking on hands, and crying as a late sign of hunger.
Challenges and Solutions:
- Latching Issues: Seek help from a lactation consultant.
- Milk Supply: Frequent breastfeeding and proper hydration can help increase milk supply.
- Nipple Pain: Ensure correct latching and use nipple creams if necessary.
Work and Breastfeeding:
- Pumping: Mothers can pump and store breast milk to continue breastfeeding after returning to work.
- Legal Rights: Many places have laws supporting breastfeeding mothers at work, including break times and private spaces for pumping.
Introduction of Solids: After six months, introduce complementary foods while continuing breastfeeding up to two years or beyond.
🔸3 Protein energy malnutrition
Protein-energy malnutrition (PEM) is a form of malnutrition that occurs due to insufficient intake of protein and calories. Here is a detailed point-wise overview:
Definition
- PEM: A condition resulting from a deficiency in protein and calorie intake, leading to various health complications.
Types
- Kwashiorkor: Caused primarily by protein deficiency with adequate calorie intake.
- Marasmus: Caused by a severe deficiency in both calorie and protein intake.
Causes
- Inadequate Dietary Intake: Insufficient consumption of protein-rich and calorie-rich foods.
- Poor Absorption: Conditions like gastrointestinal diseases that affect nutrient absorption.
- Increased Nutrient Requirements: Higher metabolic demands due to infections, chronic diseases, or rapid growth.
- Socioeconomic Factors: Poverty, lack of access to food, and educational deficiencies about nutrition.
Symptoms
- General Symptoms: Fatigue, weight loss, and weakness.
- Kwashiorkor:
- Edema (swelling due to fluid retention)
- Enlarged liver (hepatomegaly)
- Distended abdomen
- Changes in hair color and texture
- Dermatitis and skin lesions
- Marasmus:
- Severe wasting of muscle and fat tissue
- Thin, emaciated appearance
- Stunted growth
- Frequent infections due to weakened immune system
Diagnosis
- Clinical Evaluation: Assessment of physical signs and symptoms.
- Anthropometric Measurements: Weight, height, and body mass index (BMI).
- Biochemical Tests: Blood tests to measure levels of proteins, electrolytes, and other nutrients.
Complications
- Growth Retardation: Impaired physical and cognitive development in children.
- Weakened Immune System: Increased susceptibility to infections.
- Organ Damage: Long-term damage to organs such as the liver and heart.
- Death: In severe cases, PEM can be fatal if left untreated.
Treatment
- Nutritional Rehabilitation: Gradual refeeding with balanced diets rich in protein and calories.
- Medical Intervention: Treatment of infections and other complications.
- Monitoring and Support: Regular follow-up to monitor recovery and prevent relapse.
- Community and Educational Programs: Addressing underlying causes through community support and education about proper nutrition.
Prevention
- Improving Food Security: Ensuring access to a variety of nutritious foods.
- Education: Providing information on balanced diets and the importance of nutrition.
- Healthcare Access: Improving access to healthcare services for early detection and treatment.
- Economic Support: Programs to alleviate poverty and improve living conditions.
🔸4 Tracheo-esophageal fistula
1. Definition and Classification:
- TEF is a congenital or acquired condition where there is an abnormal connection (fistula) between the trachea and the esophagus.
- Most common type (85% of cases) is Type C, where the upper esophagus ends in a blind pouch and the lower esophagus is connected to the trachea.
2.Clinical Presentation:
- Newborns typically present with excessive salivation, coughing, choking, and cyanosis, especially during feeding.
- May also have associated conditions like esophageal atresia, congenital heart defects, or other anomalies.
3.Diagnosis and Treatment:
- Diagnosed through imaging studies like contrast esophagogram or bronchoscopy.
- Surgical correction is the primary treatment, involving ligation of the fistula and reconstruction of the esophagus.
- Postoperative care is critical to manage complications like leakage, strictures, or respiratory issues.
🔸5 Hirschprung’s disease
Hirschsprung’s disease (HD) is a congenital condition that affects the large intestine (colon) and causes problems with passing stool.
1.Definition and Cause:
- Hirschsprung’s disease is a congenital disorder caused by the absence of ganglion cells in the myenteric and submucosal plexuses of the distal colon.
- This lack of nerve cells results in a section of the colon that cannot properly contract and move stool through the digestive tract.
2.Symptoms and Diagnosis:
- Common symptoms include chronic constipation, abdominal distension, and failure to pass meconium within the first 48 hours of life in newborns.
- Diagnosis is typically confirmed through a combination of clinical examination, radiographic studies (such as a barium enema), and a rectal biopsy, which shows the absence of ganglion cells.
3.Treatment:
- The primary treatment for Hirschsprung’s disease is surgical, involving the removal of the aganglionic segment of the colon and reattachment of the healthy, ganglionic segment to the anus (pull-through procedure).
- Postoperative care is crucial, and complications can include enterocolitis, strictures, and bowel obstruction. Regular follow-up is necessary to monitor for these potential issues.
⏩Q.3 Very Short Answer (Any Four) (4×2=8)
🔸1 Define Rheumatic fever
- Rheumatic Fever: An inflammatory disease that can develop as a complication of inadequately treated streptococcal throat infection (strep throat).
- Symptoms and Effects: Can affect the heart, joints, skin, and brain, potentially leading to permanent heart damage (rheumatic heart disease).
🔸2 Ortolani sign
The Ortolani sign is a physical examination maneuver used to detect congenital hip dislocation or hip dysplasia in infants. Here’s a brief point-wise explanation of the Ortolani sign:
- Purpose: It is used to assess for hip instability in newborns and infants.
- Technique:
- Positioning: The infant lies supine (on their back) with their hips and knees flexed at 90 degrees.
- Maneuver: The examiner places their fingers over the greater trochanters of both hips and gently abducts the infant’s thighs.
Interpretation:
- Positive Ortolani sign: If the hip is dislocated, a palpable or audible click is felt as the femoral head relocates into the acetabulum when the hip is abducted.
- Negative Ortolani sign: If there is no click felt, it suggests that the hip is not dislocated.
Implications: A positive Ortolani sign indicates that the hip joint is reducible, which is a good prognostic sign as early intervention can prevent long-term complications such as hip dysplasia or osteoarthritis.
🔸3 Define weaning
Weaning refers to the process of gradually introducing an infant or young animal to solid food and reducing their dependence on milk or formula for nourishment. Pointwise, it involves:
- Introduction of Solid Food: Introducing solid foods alongside breastfeeding or formula feeding to transition the infant to a varied diet.
- Gradual Reduction in Milk: Gradually reducing the frequency and quantity of breast milk or formula as the infant becomes more accustomed to solid foods, ultimately leading to complete weaning from milk.
🔸4 Electra complex
The Electra complex is a psychoanalytic concept proposed by Carl Jung, which is analogous to the Oedipus complex in males.
- Definition: The Electra complex involves a girl’s unconscious desire for her father and feelings of rivalry with her mother. It suggests that during early childhood, girls experience psychosexual conflicts similar to those of boys (Oedipus complex), leading to the development of gender identity.
- Development: According to psychoanalytic theory, the Electra complex emerges during the phallic stage (around ages 3 to 6 years), characterized by the girl’s shifting focus of attachment from the mother to the father, along with feelings of jealousy and resentment toward the mother.
🔸5 Oedipus Complex
The Oedipus complex, a concept from Freudian psychoanalytic theory, can be summarized briefly as follows:
- Definition: It’s a psychological theory proposed by Sigmund Freud suggesting that children, especially boys, have unconscious desires for their opposite-sex parent and hostility toward their same-sex parent.
- Key Points:
- Desire for Parent: Boys experience attraction towards their mothers and competition with their fathers for their mothers’ attention and affection.
- Resolution: The complex is typically resolved through identification with the same-sex parent and the development of mature sexual attitudes.
This complex is considered fundamental in Freudian theory, influencing later psychoanalytic thought and interpretations of human development.
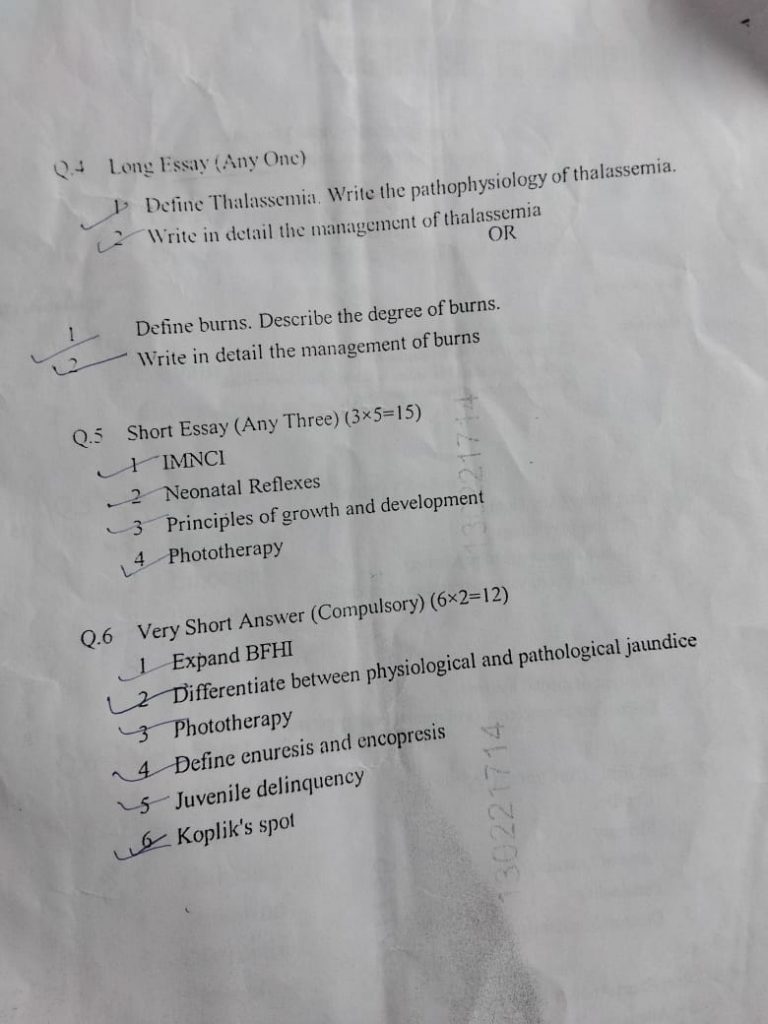
⏩Q.4 Long Essay (Any Onc)
🔸1 Define Thalassemia. Write the pathophysiology of thalassemia.
Thalassemia refers to a group of genetic blood disorders characterized by abnormal hemoglobin production. It results in anemia due to inadequate production of normal hemoglobin, which is essential for carrying oxygen throughout the body.
Pathophysiology of Thalassemia
1.Genetic Mutation:
- Thalassemia is primarily caused by mutations in the genes responsible for producing hemoglobin. These mutations affect the production of either alpha or beta globin chains, essential components of hemoglobin.
2.Impact on Hemoglobin Production:
- In alpha thalassemia, mutations affect the genes that code for alpha globin chains, leading to reduced or absent production of these chains.
- In beta thalassemia, mutations affect the beta globin chain genes, resulting in reduced or absent production of beta globin chains.
3.Imbalance in Hemoglobin Chains:
- The imbalance between alpha and beta globin chains disrupts the normal formation of hemoglobin tetramers (HbA), leading to ineffective erythropoiesis (production of red blood cells) and hemolysis (destruction of red blood cells).
🔸2 Write in detail the management of thalassemia
Managing thalassemia requires a comprehensive approach involving medical, supportive, and potentially curative therapies. Here’s a detailed pointwise management strategy:
1.Diagnosis:
- Accurate diagnosis through genetic testing, hemoglobin electrophoresis, and complete blood count (CBC) to assess hemoglobin levels and red blood cell indices.
2.Classification:
- Classify thalassemia as alpha or beta based on genetic testing and clinical presentation.
3.Medical Management:
- Blood Transfusions:
- Regular transfusions to maintain hemoglobin levels and prevent complications of severe anemia.
- Iron Chelation Therapy:
- Essential to prevent iron overload from frequent transfusions, which can lead to organ damage (heart, liver, endocrine dysfunction).
- Folic Acid Supplementation:
- Supports erythropoiesis and red blood cell production.
4.Supportive Care:
- Bone Marrow Transplantation (BMT):
- Potentially curative for selected patients, particularly in younger individuals with a compatible donor.
- Gene Therapy:
- Investigational approach aimed at correcting the genetic defect to restore normal hemoglobin production.
- Symptomatic Treatment:
- Address complications such as bone deformities (orthopedic interventions), infections, and growth delays (pediatric management).
5.Psychosocial Support:
- Counseling and support groups for patients and families to cope with chronic illness, treatment burden, and emotional impact.
6.Monitoring:
- Regular monitoring of hemoglobin levels, iron status, cardiac function (due to iron overload), and growth parameters (in children) to adjust treatment and prevent complications.
7.Prevention:
- Genetic counseling for families to understand inheritance patterns and options for prenatal testing.
🔸OR🔸
🔸1 Define burns. Describe the degree of burns.
Burns are injuries to the skin and other tissues caused by heat, chemicals, electricity, or radiation. They can vary widely in severity, from minor injuries that require minimal intervention to life-threatening emergencies.
Degrees of Burns:
1.First-Degree Burns:
- Superficial burns that affect only the outer layer of the skin (epidermis).
- Symptoms include redness, pain, and mild swelling.
- Typically heal within a few days without scarring.
2.Second-Degree Burns:
- Affect both the outer layer (epidermis) and the underlying layer of skin (dermis).
- Symptoms include pain, redness, swelling, and blistering.
- May take several weeks to heal and can cause scarring.
3.Third-Degree Burns:
- Destroy both the outer and inner layers of skin and may also damage underlying tissues.
- Often appear white, charred, or leathery.
- Painless due to nerve damage.
- Require immediate medical attention and often necessitate skin grafts for healing.
4.Fourth-Degree Burns:
- Extend through the skin into underlying fat, muscle, or bone.
- Result in significant tissue damage and often require extensive surgical intervention.
🔸2 Write in detail the management of burns
1.First Aid:
- Remove the heat source: Stop the burning process immediately.
- Cool the burn: Hold the burned area under cool (not cold) running water or apply a clean, cool, damp cloth to the burn for at least 10 minutes to reduce pain and swelling.
2.Assessment and Treatment:
- Assess the severity: Determine the degree and extent of the burn.
- Protect the burn: Cover the burn loosely with a sterile, nonstick bandage or cloth.
- Pain management: Administer pain relievers such as ibuprofen or acetaminophen as needed.
3.Seek Medical Attention for:
- Burns larger than the palm of the victim’s hand.
- Burns on the face, hands, feet, genitals, or major joints.
- Chemical or electrical burns.
- Signs of infection (increased pain, redness, swelling, pus).
4.Advanced Medical Care:
- Cleaning and dressing: Cleaning and applying sterile dressings to minimize infection risk.
- Fluid replacement: Administer intravenous fluids if necessary to prevent dehydration and shock.
- Medications: Antibiotics to prevent or treat infection, tetanus vaccination if needed.
- Surgical interventions: Skin grafting or other surgical procedures for severe burns.
5.Long-Term Care and Rehabilitation:
- Wound care: Regular dressing changes and monitoring for signs of healing or complications.
- Physical therapy: Range-of-motion exercises to prevent stiffness and improve function.
- Psychological support: Counseling for coping with trauma and emotional recovery.
6.Prevention:
- Educate on fire safety and proper handling of hot liquids or objects.
- Use caution with chemicals and electrical appliances.
- Install smoke detectors and have fire extinguishers readily available.
Proper management of burns depends on the severity and extent of the injury. Immediate and appropriate first aid followed by prompt medical evaluation and treatment are crucial to optimize outcomes and prevent complications.
⏩Q.5 Short Essay (Any Three) (3×5=15)
🔸1 IMNCI
IMNCI stands for Integrated Management of Neonatal and Childhood Illness. It’s a strategy developed by WHO and UNICEF to reduce childhood morbidity and mortality, focusing on early detection and management of common childhood illnesses.
1.Objectives:
- IMNCI aims to reduce mortality and morbidity due to common childhood illnesses such as pneumonia, diarrhea, malaria, measles, and malnutrition.
- It emphasizes early detection of illness, appropriate treatment, and counseling of caregivers on preventive care.
2.Components:
- Assessment and Classification: Health workers are trained to assess sick children using clinical signs and symptoms, classify them into illness categories (such as pneumonia, diarrhea, or severe malnutrition), and prioritize care based on severity.
- Treatment: Standardized protocols guide health workers in providing correct treatments, including antibiotics for pneumonia, oral rehydration solution for diarrhea, and appropriate feeding for malnutrition.
- Counseling: Caregivers are counseled on proper feeding practices, hygiene, immunization, and recognizing danger signs in children.
3.Implementation:
- IMNCI is implemented through training health workers at primary healthcare levels (clinics, health centers) to ensure consistent and quality care delivery.
- It integrates with existing health systems, emphasizing the use of simple algorithms and job aids to support health workers in decision-making.
- Regular monitoring and supportive supervision are key to maintaining quality and effectiveness.
IMNCI has been pivotal in improving child health outcomes in many countries by empowering frontline health workers with the skills and tools needed to identify and manage childhood illnesses promptly and effectively.
🔸2 Neonatal Reflexes
Neonatal reflexes are involuntary movements or actions that are part of the normal neurological development of newborns.
1.Rooting Reflex:
- Description: When a baby’s cheek is touched, they turn their head towards that side and open their mouth to suck.
- Purpose: Helps with breastfeeding and finding the nipple.
2.Moro Reflex (Startle Reflex):
- Description: In response to a sudden loss of support or loud noise, the baby arches their back, throws back their head, extends arms and legs, then brings them in.
- Purpose: Evolutionary protection response, helps the baby cling to the caregiver.
3.Grasp Reflex:
- Description: When an object is placed in the baby’s palm or foot, they will grasp it tightly.
- Purpose: Prepares the baby for voluntary grasping and exploring objects.
4.Sucking Reflex:
- Description: When an object is placed in the baby’s mouth, they will suck rhythmically.
- Purpose: Essential for feeding, helps with breastfeeding or bottle feeding.
5.Babinski Reflex:
- Description: When the sole of the foot is stroked, the toes fan out and curl.
- Purpose: Normal in infants; abnormal in adults and may indicate neurological problems.
6.Stepping Reflex:
- Description: When held upright with feet touching a surface, the baby makes stepping movements.
- Purpose: Prepares for voluntary walking.
7.Tonic Neck Reflex (Fencing Reflex):
- Description: When the head is turned to one side, the arm on that side extends and the opposite arm flexes.
- Purpose: Helps with hand-eye coordination and reaching.
These reflexes typically diminish as the baby grows and voluntary control over movements develops.
🔸3 Principles of growth and development
The principles of growth and development outline the fundamental aspects of how individuals typically progress physically, mentally, and emotionally over time.
- Cephalocaudal Principle: This principle suggests that development proceeds from head to toe. In other words, growth and development tend to begin with the head and upper body parts before progressing to the lower parts of the body.
- Proximodistal Principle: According to this principle, development begins from the center of the body and moves outward. For instance, a child gains control over their torso before their arms and legs.
- Principle of Hierarchical Integration: This principle emphasizes that simple skills typically develop separately and independently but later integrate into more complex skills. For example, a child learns to grasp objects before mastering the fine motor skills required for writing.
- Principle of Independence of Systems: This principle highlights that different developmental systems (such as cognitive, social, emotional, and physical) develop at different rates and may follow different trajectories.
- Principle of Individual Differences: Every person is unique, and development occurs at varying rates and in different sequences for each individual.
These principles collectively provide a framework for understanding the orderly and sequential changes that occur as individuals grow and develop across their lifespan.
🔸4 Phototherapy
Photo therapy, also known as phototherapy, is a medical treatment that involves exposure to specific wavelengths of light for therapeutic purposes.
1.Definition and Purpose:
- Phototherapy is a treatment method that uses light, typically ultraviolet (UV) light, to treat certain medical conditions, especially those related to the skin.
- It is primarily used to treat skin disorders such as psoriasis, eczema, vitiligo, and jaundice in newborns.
2.Mechanism of Action:
- UV light in phototherapy works by penetrating the skin and affecting underlying cells. UVB (Ultraviolet B) light slows down the rapid growth of skin cells seen in conditions like psoriasis.
- UVA (Ultraviolet A) light may be used in conjunction with medications that sensitize the skin to light (PUVA therapy), enhancing its effectiveness.
3.Procedure and Considerations:
- During treatment, the patient is exposed to the specific wavelength of light for a prescribed amount of time.
- Sessions are conducted in specialized clinics or hospitals under controlled conditions to minimize the risk of side effects such as sunburn or skin aging.
- Treatment duration and frequency vary depending on the condition being treated and the individual’s response to therapy.
In summary, phototherapy harnesses the therapeutic properties of light, particularly UV light, to manage various skin conditions effectively. It is a well-established treatment modality with specific protocols to ensure both safety and efficacy.
⏩Q.6 Very Short Answer (Compulsory) (6×2=12)
🔸1 Expand BFHI
he Baby-Friendly Hospital Initiative (BFHI) is a global program launched by the World Health Organization (WHO) and UNICEF to promote breastfeeding and support mothers in initiating breastfeeding within one hour of birth. It involves implementing Ten Steps to Successful Breastfeeding in maternity facilities, which include:
- Have a written breastfeeding policy that is routinely communicated to all healthcare staff.
- Train all healthcare staff in skills necessary to implement this policy.
- Inform all pregnant women about the benefits and management of breastfeeding.
- Help mothers initiate breastfeeding within one hour of birth.
- Show mothers how to breastfeed and maintain lactation, even if they are separated from their infants.
- Give newborn infants no food or drink other than breast milk, unless medically indicated.
- Practice rooming-in – allow mothers and infants to remain together 24 hours a day.
- Encourage breastfeeding on demand.
- Give no pacifiers or artificial nipples to breastfeeding infants.
- Foster the establishment of breastfeeding support groups and refer mothers to them on discharge from the hospital or clinic.
🔸2 Differentiate between physiological and pathological jaundice
1.Physiological Jaundice:
- Cause: It’s a normal phenomenon in newborns due to the immature liver’s inability to efficiently process bilirubin in the first few days of life.
- Timing: Typically appears after the first 24 hours of birth and resolves within 1-2 weeks.
- Bilirubin Levels: Bilirubin levels are mildly elevated and usually do not exceed 12 mg/dL.
- Treatment: Often resolves without specific treatment, although sometimes phototherapy may be used if levels become too high.
2.Pathological Jaundice:
- Cause: Caused by underlying medical conditions that lead to excessive production of bilirubin, impaired bilirubin conjugation, or obstruction of bile flow.
- Timing: Can occur at any age, including newborns beyond the first week of life.
- Bilirubin Levels: Bilirubin levels are typically higher (>12 mg/dL in newborns) and can indicate a serious underlying condition.
- Treatment: Requires identifying and treating the underlying cause, which may involve medical or surgical interventions depending on the specific condition.
🔸3 Phototherapy
- Definition: Phototherapy involves the use of specific wavelengths of light to treat various medical conditions.
- Mechanism: It works by exposing the skin or affected area to ultraviolet (UV) light, which can penetrate the skin and affect underlying cells.
- Indications:
- Skin Conditions: Used for treating conditions like psoriasis, eczema, and vitiligo.
- Neonatal Jaundice: Effective in reducing bilirubin levels in newborns with jaundice.
1.Types of Phototherapy:
- UVB Therapy: Uses ultraviolet B light to treat skin conditions by slowing down the growth of affected skin cells.
- PUVA Therapy: Combines psoralen (a light-sensitizing medication) with UVA light to treat certain skin disorders.
🔸4 Define enuresis and encopresis
1.Enuresis:
- Enuresis refers to the involuntary discharge of urine, especially at night (bed-wetting), in children beyond the age when bladder control is expected.
- It is commonly classified as primary (never achieving nighttime dryness) or secondary (occurs after a period of dryness).
2.Encopresis:
- Encopresis is the involuntary passage of feces into inappropriate places, such as clothing or the floor, in children who have already achieved bowel control.
- It often results from chronic constipation and stool retention, leading to overflow incontinence and soiling.
🔸5Juvenile delinquency
- Definition: Refers to illegal or antisocial behavior by minors, typically those under the age of 18.
- Causes:
- Family factors (dysfunctional families, abuse).
- Peer influence (joining delinquent peer groups).
- Socioeconomic conditions (poverty, lack of education).
- Psychological issues (mental health disorders, trauma).
Types of Offenses:
- Property crimes (theft, vandalism).
- Violent crimes (assault, robbery).
- Status offenses (truancy, underage drinking).
Impact:
- Legal consequences (juvenile justice system involvement).
- Long-term consequences on education, employment, and social relationships.
- Potential for rehabilitation through intervention programs and support.
🔸6 Koplik’s spot
Koplik’s spots are small white spots that appear on the inside of the cheeks. Here’s a pointwise summary of Koplik’s spots:
- Appearance: They are small, white or bluish-white spots.
- Location: Typically found on the inside of the cheeks, opposite the molars.
- Timing: They usually appear 1-2 days before the onset of the measles rash.
- Significance: Their presence is a characteristic early sign of measles infection.
- Pathophysiology: Koplik’s spots are caused by a localized immune response to the measles virus in the mucous membranes.