P.B.B.Sc.F.Y.(MIDWIFERY GYNAEC)saurashtra university-2017(PAPER NO.1)(UPLOAD)(DONE)
P.B.B.Sc.F.Y. (MIDWIFERY GYNAEC) saurashtra university-2017(PAPER NO.1)
SECTION – I (38 Marks)
1 Long Essay: (any one out of two) 1X15=15
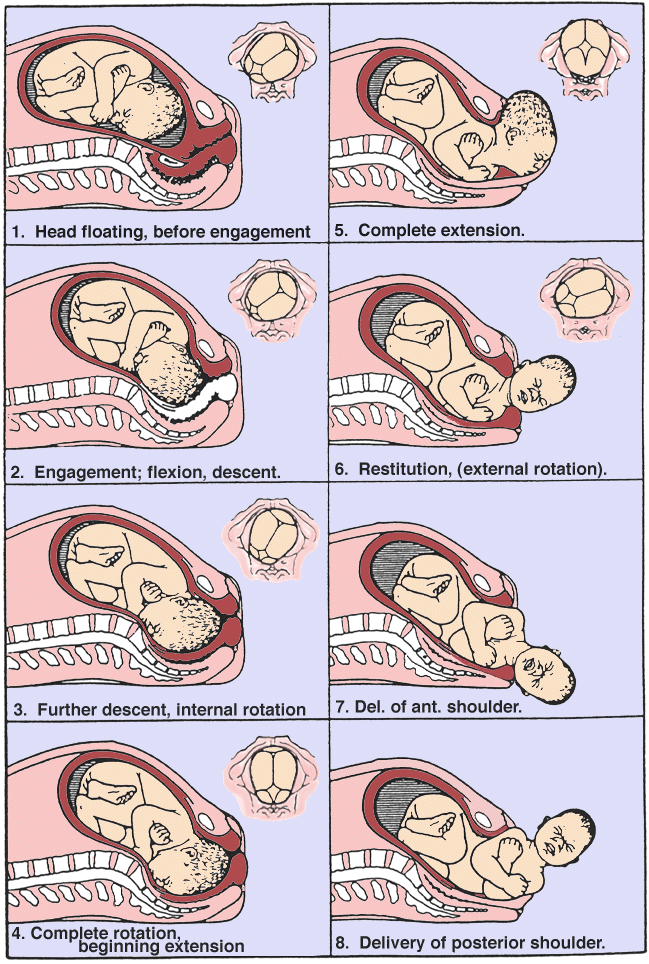
A. (i) Define labour, Explain in detail about physiology of first stage of labour. 10
Definition of Labor
Labor is a series of continuous, progressive contractions of the uterus that help the cervix dilate and efface (thin out). This lets the fetus move through the birth canal.
Labor usually starts two weeks before or after the estimated date of delivery.
First stage of labour

The first stage of labor is characterized by the onset of regular uterine contractions that lead to cervical dilation and effacement, preparing the cervix for delivery.
- It’s divided into three phases: early, active, and transition.
- Here’s a detailed explanation of each phase:
- Early Phase:
- Duration: This phase can last from hours to days, especially for first-time mothers (primigravidas). It typically lasts longer than subsequent labors.
- Cervical Changes: During this phase, the cervix begins to efface (thin out) and dilate (open up). Effacement is measured in percentages (0-100%), and dilation is measured in centimeters (0-10 cm). In the early phase, the cervix usually dilates to about 3-4 centimeters.
- Contractions: Contractions are typically mild to moderate in intensity and may be irregular, lasting around 30-45 seconds with intervals of 5-20 minutes. They gradually become more frequent and intense as labor progresses.
- Maternal Response: Women may experience a variety of emotions, including excitement, anxiety, and apprehension. Physical discomfort is usually mild to moderate, and many women are still able to walk and talk during this phase.
- Fetal Positioning: The baby’s head descends into the pelvis, putting pressure on the cervix and causing it to dilate.
- Active Phase:
- Duration: This phase is characterized by more rapid cervical dilation. It typically lasts from a few hours to around 6-8 hours.
- Cervical Changes: The cervix continues to dilate more quickly, reaching approximately 4-7 centimeters. Effacement also progresses, with the cervix becoming more thinned out.
- Contractions: Contractions become stronger, longer, and more regular, lasting around 45-60 seconds with intervals of 3-5 minutes. They may feel more intense and require more focus and coping techniques.
- Maternal Response: Women may become more focused and less talkative as they cope with the increasing intensity of contractions. Breathing techniques and position changes can help manage discomfort.
- Fetal Positioning: The baby continues to descend further into the pelvis, putting even more pressure on the cervix.
- Transition Phase:
- Duration: This is the shortest but most intense phase of the first stage of labor, typically lasting from 30 minutes to 2 hours.
- Cervical Changes: The cervix dilates from around 7-10 centimeters, fully opening to allow for the baby’s passage through the birth canal. Effacement is usually complete by this point.
- Contractions: Contractions are very intense, lasting around 60-90 seconds with intervals of 2-3 minutes. Some women experience a “double peak” pattern, where contractions have two distinct peaks of intensity.
- Maternal Response: Women may feel overwhelmed, exhausted, and may experience strong emotions such as fear or excitement. They may also have the urge to push as the baby descends further into the birth canal.
- Fetal Positioning: The baby’s head descends further, pressing against the cervix and causing a strong urge to push.
Throughout the first stage of labor, it’s important for healthcare providers to monitor maternal and fetal well-being, provide support and encouragement, and intervene if necessary to ensure a safe and positive birth experience.
(ii) Management of first stage of labour. 05
- Assessment*: Monitoring the mother and fetus for signs of progress and well-being, including cervical dilation, fetal heart rate, and maternal vital signs.
- Supportive Care: Providing emotional support, encouragement, and comfort measures to the mother, such as massage, positioning changes, and relaxation techniques.
- Hydration and Nutrition: Ensuring the mother stays hydrated and adequately nourished, often allowing clear fluids and light snacks unless there are specific medical reasons to restrict intake.
- Monitoring for Complications: Watching for any signs of complications such as fetal distress, prolonged labor, or maternal exhaustion.
- Pain Management: Offering pain relief options such as breathing techniques, relaxation methods, and pharmacological interventions like epidural anesthesia if desired by the mother.
- Positioning: Encouraging the mother to try different positions (standing, walking, sitting, squatting) to help facilitate labor progress and relieve discomfort.
- Patient Education: Providing information about the progress of labor, what to expect, and guidance on pushing techniques for when the second stage of labor begins.
- Documentation: Recording vital signs, cervical dilation, and other relevant information in the medical record.
Throughout this stage, healthcare providers aim to promote a positive birthing experience while ensuring the safety and well-being of both the mother and the baby.
B. (i) Define Maternal Mortality Rate, Explain about MMR.10
Maternal mortality rate (MMR) is a critical indicator of the health and well-being of women in a population. It refers to the number of maternal deaths per 100,000 live births during a given time period, usually a year. Maternal deaths are those that occur during pregnancy, childbirth, or within 42 days postpartum, due to complications related to pregnancy or its management.
everal factors contribute to maternal mortality, including:
- Obstetric complications: These include severe bleeding (postpartum hemorrhage),
infections,
high blood pressure during pregnancy (preeclampsia and eclampsia),
complications from delivery (such as obstructed labor), and
unsafe abortion. - Healthcare access and quality: Limited access to skilled healthcare providers,
emergency obstetric care,
and essential medical supplies can increase the risk of maternal mortality.
Quality of care, including timely interventions and appropriate management of complications,also plays a significant role. - Socioeconomic factors: Poverty, lack of education,
and social inequality can impact women’s access to healthcare services and information,leading to higher maternal mortality rates, particularly in marginalized communities. - Underlying health conditions: Pre-existing medical conditions such as diabetes,
HIV/AIDS,
malaria, and malnutrition can exacerbate the risk of complications during pregnancy and childbirth, increasing the likelihood of maternal mortality.
Reducing maternal mortality requires
/-comprehensive strategies addressing healthcare system strengthening,
improving access to quality maternal healthcare services,
promoting education and empowerment of women,
addressing social determinants of health, and ensuring universal access to family planning services.
Tracking maternal mortality rates helps policymakers, healthcare providers, and public health experts assess the effectiveness of interventions and allocate resources to areas with the greatest need, ultimately contributing to the goal of reducing maternal mortality and improving maternal health outcomes globally.
(ii) Planned parenthood. 05
Planned Parenthood, as an organization, offers a range of services and resources designed to support individuals and couples in making informed decisions about their reproductive health and family planning. Here’s how Planned Parenthood can assist couples:
- Contraceptive Services: Planned Parenthood provides comprehensive information about various contraceptive methods, including birth control pills, condoms, intrauterine devices (IUDs), contraceptive implants, and contraceptive injections. Couples can discuss their options with healthcare professionals to choose the method that best suits their needs and preferences.
- Preconception Counseling: Couples who are planning to conceive can benefit from preconception counseling offered by Planned Parenthood. This service includes discussions about prenatal care, optimizing fertility, managing existing health conditions, and making lifestyle changes to support a healthy pregnancy.
- Pregnancy Testing and Counseling: Planned Parenthood offers pregnancy testing services, along with counseling and support for individuals and couples facing an unplanned pregnancy. They provide information about all available options, including continuing the pregnancy, adoption, and abortion, empowering couples to make the decision that is right for them.
- Sexually Transmitted Infection (STI) Testing and Treatment: Planned Parenthood offers confidential STI testing and treatment services for couples. This includes testing for common STIs such as chlamydia, gonorrhea, syphilis, HIV, and hepatitis, as well as counseling on safer sex practices to reduce the risk of transmission.
- Couples Counseling and Education: Planned Parenthood provides counseling and educational resources for couples on topics related to sexual health, communication, and relationship dynamics. This can include discussions about sexual satisfaction, intimacy, consent, and navigating challenges in the relationship.
- Reproductive Health Screenings: Planned Parenthood offers reproductive health screenings for both men and women, including Pap smears, breast exams, testicular exams, and prostate exams. These screenings help detect any potential health issues early on and facilitate timely intervention and treatment.
- Education and Resources: Planned Parenthood offers educational materials, online resources, and workshops on a wide range of reproductive health topics, including contraception, pregnancy, STIs, and sexual health. These resources empower couples to make informed decisions and take control of their reproductive health.
2 Write short notes on following: (any three) 3×5=15
(a) Antenatal care
Antenatal care, also known as prenatal care, is healthcare provided to pregnant women to monitor the progress of their pregnancy and ensure the health and well-being of both the mother and the unborn baby. Here’s an overview of what it typically involves:
- Initial Visit:
- The first antenatal visit usually occurs early in the pregnancy, ideally within the first trimester. During this visit, the healthcare provider collects a detailed medical history of the mother and may perform a physical examination.
- Regular Check-ups:
- Throughout the pregnancy, women typically have regular check-ups with their healthcare provider, usually once a month in the first and second trimesters, and more frequently in the third trimester.
- Physical Examinations:
- Physical exams during antenatal visits may include measuring blood pressure, weight, and abdomen size. The healthcare provider may also perform pelvic exams and ultrasounds to monitor the baby’s growth and development.
- Screening Tests:
- Various screening tests may be offered to assess the risk of genetic disorders or other complications. These may include blood tests, ultrasounds, and prenatal genetic testing such as amniocentesis or chorionic villus sampling (CVS).
- Nutritional Counseling:
- Pregnant women receive guidance on maintaining a healthy diet and lifestyle to support the growth and development of the fetus. This may include recommendations for prenatal vitamins, managing weight gain, and avoiding harmful substances like alcohol and tobacco.
- Education and Counseling:
- Antenatal care often involves providing information and counseling on topics such as childbirth preparation, breastfeeding, newborn care, and postpartum recovery.
- Monitoring Fetal Health:
- Monitoring the baby’s health is a key aspect of antenatal care. This may involve regular fetal heartbeat checks, ultrasound scans to assess fetal growth and development, and monitoring fetal movements.
- Managing Complications:
- If complications arise during pregnancy, such as gestational diabetes, preeclampsia, or fetal abnormalities, the healthcare provider will develop a plan to manage these issues and ensure the best possible outcome for both mother and baby.
- Preparation for Labor and Delivery:
- Antenatal care also involves preparing the mother for labor and delivery, including discussing birth preferences, pain management options, and potential interventions during childbirth.
- Postpartum Planning:
- Towards the end of pregnancy, discussions may focus on postpartum care, including breastfeeding support, contraception options, and emotional well-being.
Regular antenatal care plays a crucial role in promoting a healthy pregnancy and reducing the risk of complications for both the mother and the baby. It provides an opportunity for early detection and management of any issues that may arise during pregnancy.
(b) MTP acts
In India, MTP stands for Medical Termination of Pregnancy, which refers to the legal process of terminating a pregnancy under certain circumstances. The MTP Act (Medical Termination of Pregnancy Act) was enacted in 1971 and subsequently amended to regulate the conditions under which abortions can be performed in the country. Here are some key points about the MTP Act in India:
- Legal Framework: The MTP Act provides a legal framework for the termination of pregnancies by registered medical practitioners. It outlines the conditions under which abortions can be performed and the procedures to be followed.
- Conditions for Termination: The MTP Act allows for the termination of pregnancies under certain specified conditions:
- If the continuation of the pregnancy poses a risk to the life of the pregnant woman or could cause grave injury to her physical or mental health.
- If there is a substantial risk that the child, if born, would suffer from physical or mental abnormalities.
- If the pregnancy is the result of rape or incest.
- Gestational Limit: The MTP Act specifies a gestational limit for legal abortions. In general, abortions can be performed up to 20 weeks of pregnancy. However, abortions beyond 20 weeks may be permitted in certain exceptional circumstances, such as fetal abnormalities or risks to the life of the mother.
- Authorized Providers: The MTP Act authorizes registered medical practitioners to perform abortions in approved facilities. These practitioners must have the necessary qualifications and training to carry out the procedure safely.
- Confidentiality and Consent: The MTP Act ensures confidentiality and privacy for women seeking abortion services. It also mandates informed consent, requiring healthcare providers to fully inform women about the procedure, risks, and alternatives before obtaining their consent.
- Regulation of Facilities: The MTP Act regulates facilities where abortions can be performed, ensuring that they meet certain standards of safety and hygiene. It also prohibits the advertisement of abortion services to prevent the promotion of sex-selective abortions.
- Penalties for Violations: The MTP Act specifies penalties for violations, including unauthorized abortions, non-compliance with regulations, and failure to maintain confidentiality. Violators may face fines and imprisonment.
Overall, the MTP Act in India aims to safeguard the reproductive rights and health of women by providing access to safe and legal abortion services under specified conditions. It seeks to prevent unsafe abortions, reduce maternal mortality and morbidity, and promote women’s reproductive autonomy.
(c) Essential newborn care
definition
Essential newborn care includes keeping the baby warm, ensuring proper feeding (breastfeeding if possible), providing skin-to-skin contact, maintaining hygiene, monitoring for signs of illness, and ensuring timely vaccinations and medical check-ups.
Essential newborn care involves various steps to ensure the health and well-being of a newborn baby.
- Immediate Skin-to-Skin Contact: After birth, place the baby on the mother’s chest to promote bonding, regulate the baby’s temperature, and initiate breastfeeding.
- Drying and Warming: Dry the baby gently with a clean, soft towel and wrap them in a warm blanket to prevent hypothermia.
- Clearing Airways: If the baby has mucus or amniotic fluid in their mouth or nose, use a bulb syringe or suction device to clear the airways gently.
- Assessment of Breathing: Ensure the baby is breathing normally. If not, stimulate them by rubbing their back or feet gently.
- Umbilical Cord Care: Keep the umbilical cord clean and dry. Avoid applying anything to it unless instructed by a healthcare provider.
- Eye Care: Administer eye drops or ointment to prevent infections, as recommended by healthcare providers.
- Vitamin K Injection: Administer a vitamin K injection to prevent bleeding disorders.
- Weight and Measurements: Weigh the baby and measure their length and head circumference to track growth and development.
- Breastfeeding Initiation: Encourage breastfeeding within the first hour of birth. Proper latch and positioning are crucial for successful breastfeeding.
- Monitoring: Monitor the baby’s vital signs, including temperature, heart rate, and respiratory rate, regularly.
- Immunizations: Ensure the baby receives necessary vaccinations according to the recommended schedule.
- Routine Checks: Perform routine physical examinations to assess the baby’s overall health and development.
- Jaundice Screening: Monitor for signs of jaundice and conduct appropriate screening tests if necessary.
- Bonding and Attachment: Encourage bonding between the baby and caregivers through skin-to-skin contact, cuddling, and talking to the baby.
- Education for Parents: Provide parents with guidance on newborn care, including feeding, bathing, diapering, and recognizing signs of illness.
- Follow-up Care: Schedule follow-up appointments with healthcare providers to monitor the baby’s growth and development and address any concerns.
By following these steps, caregivers can ensure that newborns receive the essential care they need to thrive in the early days of life.
(d) Diagnosis of pregnancy
Diagnosing pregnancy typically involves a combination of methods:
- Home Pregnancy Tests (HPTs): These detect the presence of human chorionic gonadotropin (hCG) in urine. Most HPTs are highly accurate if used correctly after a missed period.
- Blood Tests: Quantitative blood tests measure the exact amount of hCG in the blood, while qualitative tests simply confirm its presence. Blood tests can detect pregnancy earlier than urine tests, often around 7-12 days after conception.
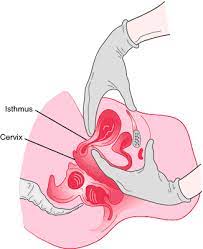
- Clinical Assessment: A healthcare provider may conduct a physical exam to check for signs of pregnancy such as changes in the uterus and cervix.
- Ultrasound: An ultrasound scan can confirm pregnancy, determine gestational age, and detect multiple pregnancies. It’s usually done after 6-8 weeks of pregnancy.
- Pelvic Exam: A healthcare provider may perform a pelvic exam to check the size and shape of the uterus and examine the cervix for any signs of pregnancy.
- Symptoms: While not definitive, symptoms such as missed periods, nausea, breast tenderness, fatigue, and frequent urination can suggest pregnancy.
- Medical History: A detailed medical history, including menstrual cycles, contraceptive use, and sexual activity, can help in diagnosing pregnancy.
Combining multiple methods helps ensure an accurate diagnosis of pregnancy. If there’s any doubt or uncertainty, consulting a healthcare professional is advisable for further evaluation and guidance
3 .Briefly answer following: (any four) 4X2=8
(a) Osiander’s sign
The Osiander sign is a historical obstetric sign named after the German obstetrician Christoph Wilhelm Ludwig Osiander.
Definition..
It refers to the softening and compressibility of the lower uterine segment that occurs during pregnancy.
This sign was historically used as an indication of pregnancy.
However, it’s not commonly used in modern obstetrics, as more reliable diagnostic methods, such as ultrasound, have become available.
(b) Signs of plancental separation
Placental separation typically involves signs such as
a gush of blood from the vagina,
a change in the shape of the uterus (becoming more spherical),
and the umbilical cord lengthening as the placenta detaches from the uterine wall.
Other signs may include a feeling of relief or sudden decrease in uterine tension for the mother.
It’s important for healthcare providers to monitor these signs closely during childbirth.
(c) Positive signs of pregnancy
- Fetal Heartbeat: Detection of a fetal heartbeat using Doppler ultrasound or other fetal monitoring devices is a clear sign of pregnancy. This typically occurs around 6-8 weeks of gestation.
- Fetal Movement: Feeling fetal movements, also known as “quickening,” usually occurs between 16-25 weeks of pregnancy, though it can vary depending on factors such as the woman’s body size and the position of the placenta.
- Visualization of Fetus on Ultrasound: Direct visualization of the fetus via ultrasound confirms pregnancy. Ultrasound can detect the presence of a gestational sac, fetal pole, and eventually the fetus itself, providing visual evidence of pregnancy.
- Palpation of Fetal Parts: Healthcare providers can sometimes palpate or feel fetal parts during a physical examination. This may be possible later in pregnancy when the fetus is larger and more easily distinguishable.
(d) Definition of small for date babies
A baby who is small for gestational age (SGA), also known as small for date or small for age, is a term used to describe infants whose birth weight, length, or head circumference is below the 10th percentile for their gestational age. In other words, these babies are smaller than expected for the number of weeks of pregnancy.
Several factors can contribute to a baby being small for gestational age, including maternal factors (such as maternal malnutrition, high blood pressure, smoking, drug use, or certain medical conditions), placental factors (such as placental insufficiency), or fetal factors (such as genetic conditions, chromosomal abnormalities, or intrauterine growth restriction).
It’s important to note that being small for gestational age does not necessarily mean that the baby is unhealthy, but it may increase the risk of certain complications, such as low birth weight, difficulty maintaining body temperature, hypoglycemia (low blood sugar), respiratory distress syndrome, and long-term growth and developmental issues.
(e) List down gynaecological conditions complicating pregnancy.
- Uterine Fibroids: Fibroids are noncancerous growths in the uterus that can increase the risk of miscarriage, preterm birth, fetal malpresentation, placental abruption, and complications during labor and delivery.
- Endometriosis: Endometriosis is a condition in which tissue similar to the lining of the uterus grows outside the uterus. It can increase the risk of infertility, miscarriage, ectopic pregnancy, and pregnancy complications such as preterm birth and cesarean section.
- Polycystic Ovary Syndrome (PCOS): PCOS is a hormonal disorder that can cause irregular menstrual cycles, ovulation problems, and infertility. Women with PCOS are at higher risk of gestational diabetes, preeclampsia, preterm birth, and cesarean section.
- Adenomyosis: Adenomyosis is a condition in which the tissue lining the uterus grows into the muscular wall of the uterus. It can increase the risk of miscarriage, preterm birth, and placental abnormalities.
- Cervical Insufficiency (Incompetent Cervix): Cervical insufficiency is a condition in which the cervix is weak and unable to support the weight of the growing fetus, leading to premature cervical dilation and preterm birth.
- Pelvic Inflammatory Disease (PID): PID is an infection of the female reproductive organs, usually caused by sexually transmitted bacteria. It can lead to infertility, ectopic pregnancy, miscarriage, preterm birth, and intrauterine infection in pregnant women.
- Ovarian Cysts: Ovarian cysts are fluid-filled sacs that can develop on the ovaries. Large or complex cysts may cause complications during pregnancy, such as ovarian torsion, rupture, or interference with fetal growth and development.
- Cervical Dysplasia: Cervical dysplasia is the abnormal growth of cells on the cervix, often caused by human papillomavirus (HPV) infection. In severe cases, treatment such as cervical conization or cryotherapy may increase the risk of preterm birth or cervical incompetence in subsequent pregnancies.
- Pelvic Organ Prolapse: Pelvic organ prolapse occurs when the pelvic organs, such as the uterus, bladder, or rectum, bulge into the vagina due to weakened pelvic floor muscles. It can cause urinary or fecal incontinence and may complicate labor and delivery.
- Vulvovaginal Disorders: Conditions such as vulvar dermatoses, chronic vulvovaginal infections, or vaginal septum may require specialized management during pregnancy to prevent complications such as infection, preterm birth, or difficulties during labor and delivery.
SECTION – II (37 Marks)
1.Long Essay: (any one) 1X10=10
A. (i) Define abortion.02
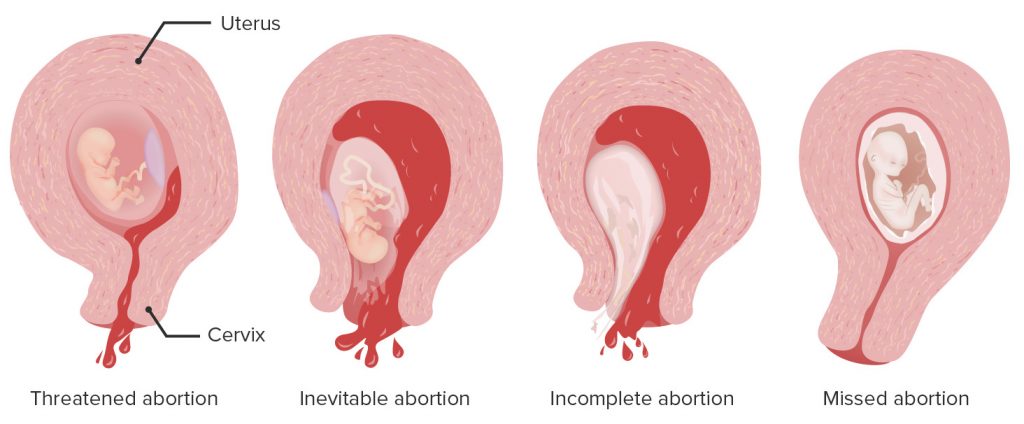
Abortion is the deliberate termination of a pregnancy, typically performed during the first 28 weeks of gestation. It can be done either medically or surgically.
(ii) Explain in detail about missed abortion.08
Missed Abortion
Definition
A missed abortion, also known as a missed miscarriage, occurs when a fetus dies in the uterus but is not expelled. The woman may not experience symptoms right away and may continue to have signs of pregnancy, such as a positive pregnancy test and ongoing pregnancy symptoms like breast tenderness and nausea.
Signs and symptoms of a missed abortion, also known as a missed miscarriage, may include:
- Lack of fetal movement: One of the first signs may be a cessation of fetal movement, especially if the woman has been feeling movement before.
- Vaginal bleeding or spotting: While some spotting can be normal during pregnancy, persistent or heavy bleeding can indicate a problem.
- Loss of pregnancy symptoms: Women may notice a sudden decrease or loss of pregnancy symptoms, such as breast tenderness, nausea, and fatigue.
- Cramping or abdominal pain: Mild to severe abdominal cramping or pain may occur, similar to menstrual cramps.
- Absence of fetal heartbeat: During a prenatal checkup, a healthcare provider may detect the absence of a fetal heartbeat using ultrasound.
- Uterine size: The uterus may not grow as expected during pregnancy, or it may even shrink in size.
- Confirmation through ultrasound: An ultrasound scan can confirm the absence of fetal heartbeat or growth.
The treatment for a missed abortion depends on various factors such as the gestational age, the woman’s health, and personal preferences. Common treatment options include:
- Expectant management: In some cases, the body may expel the pregnancy tissue naturally without intervention. This approach involves monitoring the woman’s condition with regular check-ups to ensure there are no complications.
- Medication: If the body does not expel the pregnancy tissue on its own, medications such as misoprostol may be prescribed to help induce uterine contractions and facilitate the expulsion of the tissue.
- Surgical management: If expectant management or medication is not suitable or effective, a surgical procedure called dilation and curettage (D&C) may be performed. During this procedure, the cervix is dilated, and the pregnancy tissue is removed from the uterus using suction or scraping instruments.
- Manual vacuum aspiration (MVA): This is a less invasive surgical procedure similar to D&C but using a handheld device to remove the pregnancy tissue from the uterus.
Nursing Management
- Emotional Support and Counseling:
- Provide empathetic and compassionate care to the patient and their family members, acknowledging the emotional impact of the loss.
- Offer counseling and support to help the patient cope with grief, sadness, guilt, and other emotions associated with the miscarriage.
- Encourage open communication and provide a safe space for the patient to express their feelings and concerns.
- Education and Information:
- Educate the patient about missed abortion, including its causes, symptoms, and treatment options.
- Provide information about the management of missed abortion, including expectant management, medical management with medications, or surgical intervention such as dilation and curettage (D&C).
- Discuss the potential risks, benefits, and outcomes associated with each treatment option to help the patient make informed decisions about their care.
- Physical Assessment and Monitoring:
- Monitor the patient’s vital signs, including temperature, blood pressure, and pulse rate, to assess for signs of infection or other complications.
- Assess the patient’s uterine size, fundal height, and abdominal tenderness to monitor for signs of uterine infection or retained tissue.
- Monitor vaginal bleeding, including the amount, color, and consistency, to assess for signs of incomplete miscarriage or hemorrhage.
- Pain Management:
- Assess the patient’s pain level and provide appropriate pain relief measures, such as over-the-counter or prescription analgesics, as needed.
- Educate the patient about pain management strategies, including the use of heat packs, relaxation techniques, and positioning for comfort.
- Prevention and Management of Complications:
- Monitor for signs and symptoms of complications such as infection, hemorrhage, or disseminated intravascular coagulation (DIC).
- Educate the patient about signs of infection, including fever, chills, abdominal pain, and foul-smelling vaginal discharge, and instruct them to seek medical attention if these symptoms occur.
- Supportive Care:
- Provide supportive care and encouragement to help the patient through the physical and emotional recovery process.
- Offer assistance with activities of daily living, such as hygiene, mobility, and nutrition, as needed.
- Collaborate with other members of the healthcare team, including physicians, counselors, and support groups, to ensure comprehensive care and support for the patient.
- Follow-Up Care:
- Schedule follow-up appointments for the patient to monitor their physical and emotional recovery, assess for any complications, and provide ongoing support and counseling.
- Offer information about resources and support services available to help the patient cope with their loss and navigate the grieving process.
B. (i) Define PIH. 02
definition
Pregnancy-induced hypertension (PIH), also known as gestational hypertension, is characterized by high blood pressure during pregnancy. It typically occurs after 20 weeks of gestation and resolves after delivery.
(ii) Explain in detail about PIH. 08
Classification:
- Gestational hypertension: Elevated blood pressure without proteinuria after 20 weeks of gestation.
- Pre-eclampsia: High blood pressure accompanied by proteinuria or other signs of organ damage, such as impaired liver function or visual disturbances.
- Eclampsia: Severe pre-eclampsia characterized by seizures.
Signs and Symptoms:
- High blood pressure (systolic pressure >140 mm Hg or diastolic pressure >90 mm Hg).
- Proteinuria (excess protein in the urine).
- Edema (swelling), especially in the hands and face.
- Headaches.
- Visual disturbances, such as blurred vision or seeing spots.
- Nausea or vomiting.
- Upper abdominal pain, usually on the right side.
Types:
- Chronic hypertension with superimposed pre-eclampsia: Women who have hypertension before pregnancy develop worsening hypertension and proteinuria during pregnancy.
- Transient gestational hypertension: High blood pressure that develops after 20 weeks of gestation but resolves within 12 weeks postpartum.
- Chronic hypertension: High blood pressure present before pregnancy or diagnosed before 20 weeks of gestation.
- Pre-existing hypertension with superimposed pre-eclampsia: Women with pre-existing hypertension develop features of pre-eclampsia during pregnancy.
The treatment and management of pregnancy-induced hypertension .
(PIH) aim to lower blood pressure, prevent complications, and ensure the well-being of both the mother and the baby. Here are some common approaches:
- Regular Monitoring: Blood pressure and urine protein levels are monitored closely during prenatal visits.
- Lifestyle Changes: Recommendations may include dietary changes (reducing salt intake), rest, and avoiding activities that may increase blood pressure.
- Medications:
- Antihypertensive drugs: Medications such as methyldopa, labetalol, nifedipine, and hydralazine may be prescribed to lower blood pressure. The choice of medication depends on factors such as the severity of hypertension and any other medical conditions the mother may have.
- Magnesium sulfate: This may be administered to prevent seizures in women with severe pre-eclampsia or eclampsia.
- Hospitalization: In severe cases, hospitalization may be necessary for close monitoring and management, especially if complications arise.
- Delivery: Delivery is the definitive treatment for PIH. Depending on the severity of the condition and the gestational age of the fetus, the healthcare provider may recommend inducing labor or performing a cesarean section.
- Fetal Monitoring: Continuous fetal monitoring may be necessary to ensure the well-being of the baby, especially in severe cases of PIH.
- Postpartum Care: Blood pressure monitoring continues after delivery, as some women may still experience hypertension postpartum.
Nursing Management
- Assessment and Monitoring:
- Regularly monitor the mother’s blood pressure, urine protein levels, and other vital signs to assess for signs of worsening hypertension or preeclampsia.
- Assess the mother’s symptoms, including headaches, visual disturbances, abdominal pain, swelling, and changes in fetal movement.
- Perform fetal monitoring through non-stress tests (NSTs) or biophysical profiles (BPPs) to assess fetal well-being and detect signs of fetal distress.
- Education and Counseling:
- Educate the mother about the signs and symptoms of PIH, including the importance of monitoring blood pressure at home if necessary.
- Provide information about the potential complications of PIH, such as preeclampsia, eclampsia, placental abruption, and preterm birth.
- Encourage the mother to attend regular prenatal appointments and comply with medical recommendations for monitoring and management.
- Blood Pressure Management:
- Administer antihypertensive medications as prescribed to control blood pressure and prevent complications such as stroke or organ damage.
- Monitor the mother’s response to antihypertensive therapy and adjust medication dosages as needed to maintain blood pressure within target ranges.
- Fluid and Electrolyte Balance:
- Monitor fluid intake and output to ensure adequate hydration while preventing fluid overload.
- Monitor electrolyte levels, particularly sodium and potassium, and administer intravenous fluids and electrolytes as necessary to maintain balance.
- Bed Rest and Activity Restriction:
- Advise the mother to limit physical activity and avoid strenuous activities to reduce the risk of further elevating blood pressure and triggering complications.
- Recommend periods of bed rest or modified activity based on the severity of hypertension and any associated symptoms.
- Nutritional Support:
- Provide dietary counseling to promote a balanced diet rich in fruits, vegetables, lean proteins, and whole grains while limiting sodium intake.
- Monitor the mother’s nutritional status and weight gain, addressing any concerns or deficiencies that may arise during pregnancy.
- Antenatal Testing:
- Perform regular ultrasound examinations to assess fetal growth, amniotic fluid levels, and placental function.
- Monitor fetal movements and kick counts to assess fetal well-being and detect signs of fetal distress.
- Labor and Delivery Planning:
- Collaborate with the healthcare team to develop a plan for labor and delivery based on the mother’s condition, gestational age, and fetal well-being.
- Prepare the mother for the possibility of induction of labor or cesarean delivery if complications arise or if delivery becomes necessary to protect the health of the mother or fetus.
- Psychosocial Support:
- Offer emotional support and counseling to help the mother cope with the stress and anxiety of managing PIH during pregnancy.
- Encourage open communication and provide reassurance to address any fears or concerns the mother may have about her condition or the pregnancy outcome.
- Postpartum Care:
- Monitor the mother closely in the postpartum period for signs of complications such as postpartum hypertension, eclampsia, or hemorrhage.
- Provide education and support for breastfeeding, newborn care, and postpartum recovery while addressing any lingering effects of PIH.
2 Write short notes on following: (any three)3×5=15
(a) Vesicular mole.
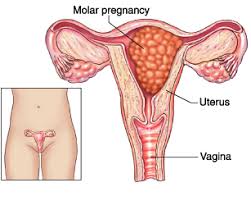
A vesicular mole, also known as a molar pregnancy or hydatidiform mole, is a rare condition that occurs when there is abnormal growth of trophoblastic cells, which are cells that normally develop into the placenta during pregnancy. This abnormal growth leads to the formation of a mass or tumor in the uterus.
Vesicular moles can be categorized into two main types:
- Complete Mole: In a complete mole, there is an abnormal fertilization of an egg by a sperm, resulting in a pregnancy with no fetal tissue. The entire mass consists of abnormal trophoblastic cells, and there is no fetal development. Complete moles typically occur when an empty egg is fertilized by a single sperm, or when two sperm fertilize an empty egg. The genetic material is typically all from the father, with no contribution from the mother.
- Partial Mole: In a partial mole, there is usually an abnormal fertilization of an egg by two sperm, resulting in an abnormal pregnancy with some fetal tissue. However, the fetal tissue is usually not viable and is accompanied by abnormal trophoblastic tissue. Partial moles may have triploid (three sets of chromosomes) or tetraploid (four sets of chromosomes) genetic compositions, instead of the normal diploid (two sets of chromosomes) composition.
Diagnosis :-
Vesicular moles are usually detected during early pregnancy through routine ultrasound examinations.
They may present with symptoms such as vaginal bleeding, severe nausea and vomiting (hyperemesis gravidarum), and uterine enlargement that is larger than expected for the gestational age.
Blood tests may also reveal elevated levels of human chorionic gonadotropin (hCG), a hormone produced during pregnancy.
Treatment
vesicular moles typically involves surgical removal of the abnormal tissue through a procedure called dilation and curettage (D&C).
After the procedure, close monitoring of hCG levels is necessary to ensure that they return to normal, as persistently elevated hCG levels may indicate the presence of persistent gestational trophoblastic disease (GTD), a rare complication in which some trophoblastic cells remain in the uterus and continue to grow.
Nursing care for Vesicular mole
- Education and Support: Provide the patient and their family with education about the condition, including its causes, symptoms, and treatment options. Offer emotional support and reassurance, as a diagnosis of a vesicular mole can be distressing for the patient and their loved ones.
- Monitoring and Assessment: Monitor the patient’s vital signs, including blood pressure, pulse, and temperature, regularly to detect any signs of complications such as excessive bleeding or infection. Perform abdominal assessments to monitor uterine size and assess for signs of uterine rupture or hemorrhage.
- Fluid Management: Monitor the patient’s fluid intake and output closely, as vesicular moles can sometimes lead to complications such as hyperemesis gravidarum (severe nausea and vomiting) or dehydration. Administer intravenous fluids as prescribed to maintain hydration and electrolyte balance.
- Blood Transfusion: In cases of severe bleeding or hemorrhage, the patient may require a blood transfusion to replace lost blood volume and improve oxygen delivery to tissues. Monitor the patient’s hemoglobin and hematocrit levels closely and collaborate with the healthcare team to initiate blood transfusion as needed.
- Psychosocial Support: Provide emotional support and counseling to help the patient cope with the diagnosis and its implications. Offer information about support groups or counseling services available to assist the patient and their family in dealing with the emotional challenges of a vesicular mole.
- Preparation for Treatment: Prepare the patient for treatment options such as dilation and curettage (D&C) or surgical evacuation of the uterus (hysterectomy), which may be necessary to remove the abnormal tissue and prevent complications. Explain the procedure, potential risks and benefits, and what to expect during recovery.
- Follow-Up Care: Schedule follow-up appointments for the patient to monitor their recovery and assess for any signs of recurrence or complications. Provide ongoing support and education to help the patient navigate the emotional and physical aspects of their recovery process.
- Family Planning: Discuss family planning options with the patient, including contraception and future pregnancy planning. Depending on the individual’s circumstances and medical history, they may need guidance on when it is safe to conceive again and any potential risks associated with future pregnancies.
(b) Placenta previa

Placenta previa is a pregnancy complication in which the placenta implants in the lower part of the uterus, partially or completely covering the cervix. Normally, the placenta attaches to the upper part of the uterus, away from the cervix, allowing for a safe delivery. However, with placenta previa, the placenta’s position can obstruct the cervical opening, potentially causing significant bleeding and complications during pregnancy and childbirth.
Diagnosis
Placenta previa is typically diagnosed during routine prenatal ultrasound examinations,
though it may also present with symptoms such as painless vaginal bleeding,
particularly in the later stages of pregnancy.
The severity of placenta previa can vary, ranging from marginal (the placenta is near but not covering the cervix) to complete (the placenta completely covers the cervix).
There are several risk factors associated with placenta previa, including:
- Previous Placenta Previa:
Women who have had placenta previa in a previous pregnancy are at higher risk of recurrence. - Previous Cesarean Delivery:
Scarring from a previous cesarean delivery can increase the risk of placenta previa in subsequent pregnancies. - Multiparity:
Women who have had multiple pregnancies are at higher risk. - Maternal Age:
Placenta previa is more common in older women. - Smoking:
Smoking during pregnancy increases the risk of placenta previa. - Assisted Reproductive Technology (ART):
Women who conceive using fertility treatments are at higher risk.
Types of placenta Previa :-
- Complete Placenta Previa: In this type of placenta previa, the placenta completely covers the cervical opening (internal os). This means that the cervical opening is entirely obstructed by the placenta. Complete placenta previa poses the highest risk of complications, including severe bleeding during labor and delivery.
- Partial Placenta Previa: Partial placenta previa occurs when the placenta partially covers the cervical opening. In this case, only a portion of the cervical opening is obstructed by the placenta. The degree of coverage can vary, and the extent of the placenta’s proximity to the cervical opening determines the severity of the condition.
- Marginal Placenta Previa: Marginal placenta previa occurs when the edge of the placenta is adjacent to the cervical opening but does not cover it. In this type of placenta previa, the placenta’s edge is close to the margin of the cervical os but does not obstruct it. Marginal placenta previa carries a lower risk of complications compared to complete or partial previa.
- Low-Lying Placenta: Low-lying placenta, also known as low-lying placenta previa or placenta previa without covering the cervical os, occurs when the placenta implants low in the uterus but does not cover the cervical opening. Although the placenta may be near the cervix, it does not obstruct the cervical os.
Management
Management of placenta previa depends on the severity of the condition and the gestational age of the fetus.
In cases of mild placenta previa without significant bleeding, close monitoring may be sufficient, with restrictions on activities such as heavy lifting and sexual intercourse.
However, in cases of significant bleeding or if the placenta completely covers the cervix, hospitalization and bed rest may be necessary to prevent complications.
If bleeding becomes severe or if there is concern for the mother’s or baby’s well-being, delivery may be necessary.
In cases of preterm placenta previa, corticosteroids may be administered to help accelerate fetal lung development before delivery.
If the bleeding is uncontrollable or if the fetus is not viable, an emergency cesarean delivery may be performed to prevent maternal hemorrhage and fetal distress.
Nursing Care
- Education and Counseling: Provide thorough education to the patient and their family about placenta previa, including its causes, symptoms, potential complications, and treatment options. Emphasize the importance of adhering to medical advice, attending scheduled appointments, and seeking prompt medical attention if symptoms worsen.
- Monitoring Vital Signs and Symptoms: Regularly monitor the patient’s vital signs, including blood pressure, pulse rate, and temperature, to detect any signs of bleeding or infection. Additionally, assess the patient for symptoms such as vaginal bleeding, abdominal pain, contractions, and signs of preterm labor.
- Bed Rest and Activity Restriction: In cases of placenta previa, healthcare providers may recommend bed rest or activity restriction to minimize the risk of bleeding. Provide support and guidance to the patient regarding limitations on physical activity and the importance of resting as much as possible.
- Fetal Monitoring: Monitor fetal well-being through methods such as non-stress tests (NSTs) or biophysical profiles (BPPs) to assess the baby’s heart rate and movements. Regular fetal monitoring helps identify any signs of fetal distress or compromise and guides decisions regarding the timing and mode of delivery.
- Intravenous (IV) Fluids: Administer intravenous fluids as prescribed to maintain hydration and electrolyte balance, especially in cases of vaginal bleeding or if the patient is at risk of preterm labor. Monitor fluid intake and output closely to ensure adequate hydration.
- Blood Transfusion: In cases of significant vaginal bleeding or hemorrhage, the patient may require a blood transfusion to replace lost blood volume and improve oxygen delivery to tissues. Monitor hemoglobin and hematocrit levels closely and collaborate with the healthcare team to initiate blood transfusion as needed.
- Preparation for Delivery: Educate the patient about the possibility of needing a cesarean section (C-section) delivery due to the risk of heavy bleeding during vaginal delivery. Discuss the signs and symptoms of labor and instruct the patient to seek immediate medical attention if labor begins or if there is any vaginal bleeding.
- Psychosocial Support: Offer emotional support and counseling to help the patient cope with the stress and anxiety associated with placenta previa. Encourage open communication and provide reassurance to address any concerns or fears the patient may have.
- Preparation for Emergency Care: Instruct the patient on what to do in case of an emergency, including how to contact healthcare providers or emergency services if vaginal bleeding occurs suddenly or becomes severe.
- Follow-Up Care: Schedule regular follow-up appointments for the patient to monitor the progression of placenta previa, assess fetal growth and well-being, and plan for delivery. Provide ongoing support and guidance to the patient throughout the pregnancy, delivery, and postpartum period.
(c) Prolapse of uterus
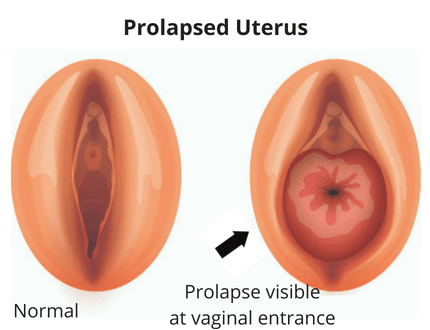
Uterine prolapse is a condition in which the uterus descends from its normal position in the pelvis and protrudes into the vagina or beyond the vaginal opening. It occurs when the pelvic floor muscles and ligaments weaken and can no longer support the uterus properly. Uterine prolapse can vary in severity, ranging from mild descent of the uterus into the upper vagina to complete protrusion of the uterus through the vaginal opening.
There are several factors that can contribute to the development of uterine prolapse:
- Childbirth: The strain of vaginal childbirth can stretch and weaken the pelvic floor muscles and ligaments, increasing the risk of uterine prolapse, especially with multiple pregnancies or difficult deliveries.
- Aging: As women age, the pelvic floor muscles and connective tissues naturally weaken, which can predispose them to uterine prolapse.
- Menopause: The hormonal changes associated with menopause, including a decrease in estrogen levels, can lead to weakening of the pelvic floor muscles and tissues.
- Chronic Constipation: Straining during bowel movements can put pressure on the pelvic floor muscles and contribute to uterine prolapse.
- Obesity: Excess weight can put added strain on the pelvic floor muscles and increase the risk of uterine prolapse.
- Chronic Coughing: Conditions such as chronic bronchitis or asthma that cause frequent coughing can also strain the pelvic floor muscles and contribute to uterine prolapse.
Symptoms of uterine prolapse can vary depending on the severity of the condition but may include:
- A sensation of heaviness or pulling in the pelvis
- A feeling of pressure or discomfort in the vagina or lower abdomen
- Difficulty emptying the bladder completely
- Urinary incontinence or leakage
- Difficulty with bowel movements
- Backache or pelvic pain
- Pain or discomfort during sexual intercourse
Treatment for uterine prolapse depends on the severity of the condition and the individual’s symptoms. Mild cases may not require treatment, but conservative measures such as pelvic floor exercises (Kegel exercises), lifestyle modifications (such as weight loss and avoiding heavy lifting), and the use of a pessary (a device inserted into the vagina to support the uterus) may be helpful.
In more severe cases or if conservative measures are ineffective, surgical intervention may be necessary to repair the pelvic floor and provide support to the uterus. Surgical options may include vaginal or abdominal procedures to repair weakened tissues and restore the uterus to its normal position.
Overall, uterine prolapse is a common condition that can significantly impact a woman’s quality of life, but with proper management and treatment, many women are able to find relief from their symptoms and maintain an active lifestyle. Regular pelvic examinations and discussions with a healthcare provider can help identify and address uterine prolapse early, reducing the risk of complications.
(d) Episiotomy
An episiotomy is a surgical incision made in the perineum, which is the area between the vagina and the anus, during childbirth. This procedure is performed to enlarge the vaginal opening and facilitate the delivery of the baby, particularly in cases where there is concern about the risk of tearing or if the baby needs to be delivered quickly.
Episiotomies used to be a routine part of childbirth, but their use has declined in recent years due to evidence suggesting that routine episiotomies do not necessarily prevent severe tears and may actually increase the risk of complications such as pain, infection, and long-term pelvic floor dysfunction.
Episiotomies may be performed for various reasons, including:
- Fetal Distress: If the baby is in distress and needs to be delivered quickly, an episiotomy may be performed to expedite the birth process.
- Instrumental Delivery: In cases where forceps or vacuum extraction are used to assist with the delivery, an episiotomy may be performed to create additional space for the instruments.
- Shoulder Dystocia: If the baby’s shoulders become stuck during delivery (shoulder dystocia), an episiotomy may be performed to create more room to maneuver and facilitate delivery.
- Prevention of Severe Tears: In some cases, healthcare providers may recommend an episiotomy to prevent severe tears that could occur if the perineum is unable to stretch sufficiently during childbirth.
The decision to perform an episiotomy is typically made by the healthcare provider based on the individual circumstances of each labor and delivery. Factors such as the position of the baby, the size of the baby’s head, the mother’s pushing efforts, and the presence of any risk factors for tearing are taken into consideration.
After the episiotomy is performed, the incision is typically sutured closed using absorbable stitches. Proper care of the episiotomy site is important to promote healing and reduce the risk of complications. This may include keeping the area clean and dry, using sitz baths or warm compresses to soothe discomfort, and taking pain relievers as needed.
While episiotomies can sometimes be necessary to facilitate childbirth, they are not without risks, and their routine use is no longer recommended. Many women are able to deliver their babies without the need for an episiotomy, and alternative techniques such as perineal massage, warm compresses, and controlled pushing (breathing techniques) can help reduce the risk of tearing during childbirth.
It’s important for pregnant women to discuss their preferences and concerns about episiotomy with their healthcare provider during prenatal care, so that they can make informed decisions about their labor and delivery plan.
3 Briefly answer following (Compulsory) 6X2=12
(a) define unwed mothers
Unwed mothers are women who have given birth to a child or children but are not married at the time of childbirth.
This term was more commonly used in the past, with varying social connotations, but in contemporary usage, it’s often replaced with more neutral terms like “single mothers.”
(b) Define PPH
Postpartum hemorrhage (PPH) is excessive bleeding following the birth of a baby. It’s a serious and potentially life-threatening condition that can occur within 24 hours after childbirth. PPH can result from various factors such as uterine atony (failure of the uterus to contract), trauma during childbirth, retained placental tissue, or blood clotting disorders. Prompt medical attention is crucial to manage PPH and prevent complications. Treatment may include medications, uterine massage, manual removal of placental tissue, or surgical interventions like uterine artery embolization or hysterectomy in severe cases.
(c) Pre-operative preparation for caesarean section
Pre-operative preparation for a Cesarean section (C-section) typically involves several steps to ensure the safety and well-being of both the mother and the baby.
Here are some common components:
- Medical History Review:
- Physical Examination: assessing the size and position of the fetus.
- Laboratory Tests:
- Intravenous (IV) Access: .
- Fasting: during anesthesia.
- Pre-operative Medications:
- Anesthesia Consultation:
- Consent:
- Skin Preparation:
- Psychological Preparation:
- Operating Room Setup: .
- Team Briefing:
(d) List down obstertrical emergencies
- Placental abruption
- Ectopic pregnancy
- Preterm labor
- Preeclampsia/eclampsia
- Cord prolapse
- Shoulder dystocia
- Uterine rupture
- Amniotic fluid embolism
- Postpartum hemorrhage
- Fetal distress
(e) List down the durgs used during labour
oxytocin
Magnesium sulfate is sometimes used during labor to prevent or manage preterm labor
Epidosin (valethemate bromide) is known to shorten the first stage of labour thus avoiding or minimising cervical dystocia leading to prolonged labour.
xylocaine
Opioids (e.g., morphine, fentanyl)
(f) Management of breast engorgement.
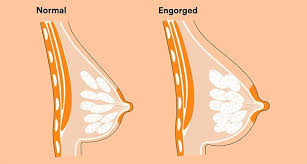
- Frequent breastfeeding:* Nurse often to relieve pressure and encourage milk flow.
- Warm compresses: Apply warmth before feeding to help milk let down and ease discomfort.
- Cold compresses: Use cold packs after feeding to reduce swelling and pain.
- Gentle massage: Massage your breasts to stimulate milk flow and relieve congestion.
- Supportive bra: Wear a comfortable, supportive bra that doesn’t constrict the breasts.