NIPAH VIRUS

NIPAH VIRUS

Nipah virus (NiV) is a zoonotic virus, meaning it can be transmitted from animals to humans. Here are the detailed aspects of Nipah virus, including its characteristics, transmission, symptoms, diagnosis, treatment, and prevention.
Characteristics
- Family: Paramyxoviridae
- Genus: Henipavirus
- Species: Nipah virus
- Genome: Single-stranded, negative-sense RNA
Transmission
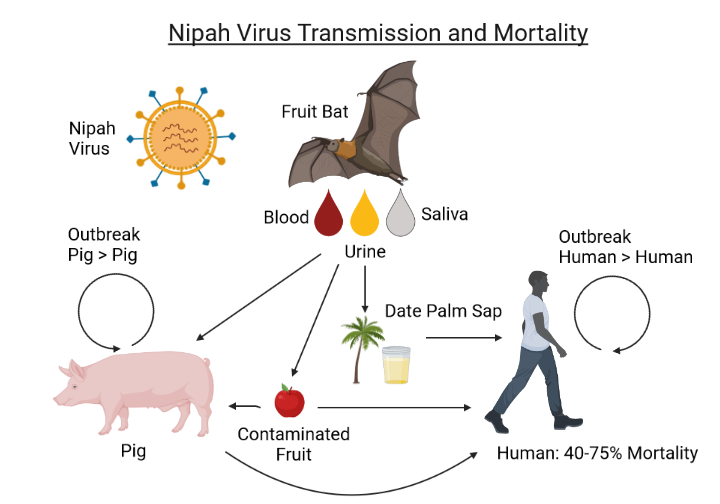
- Primary Hosts: Fruit bats of the Pteropodidae family, particularly the genus Pteropus.
- Intermediate Hosts: Pigs can act as intermediate hosts, facilitating the spread to humans.
- Human-to-Human Transmission: Documented, particularly among family members and healthcare workers.
- Direct Contact: Humans can contract the virus through direct contact with infected bats, pigs, or other NiV-infected people, as well as through consuming contaminated food.
Symptoms
- Incubation Period: 4 to 14 days, but can be as long as 45 days.
- Initial Symptoms: Fever, headache, dizziness, and myalgia (muscle pain).
- Severe Symptoms: Acute respiratory syndrome, cough, sore throat, vomiting, and encephalitis (brain inflammation).
- Progression: Severe cases may progress to coma within 24 to 48 hours.
Diagnosis
- Clinical Assessment: Based on symptoms and exposure history.
- Laboratory Tests:
- Polymerase Chain Reaction (PCR): Detects viral RNA.
- Serology: Enzyme-linked immunosorbent assay (ELISA) to detect antibodies.
- Virus Isolation: Culturing the virus from samples.
- Immunohistochemistry: Detects viral antigens in tissues.
Treatment
- Supportive Care: No specific antiviral treatment for NiV; care focuses on managing symptoms and complications.
- Ribavirin: An antiviral that has shown some effectiveness in vitro but its clinical efficacy is uncertain.
- Intensive Support: For severe cases, including mechanical ventilation and management of neurological complications.
Prevention
- Avoiding Contact: Minimize exposure to bats and sick pigs.
- Food Safety: Avoid consumption of fruits partially eaten by bats and ensure thorough washing and peeling.
- Infection Control: Strict hygiene practices and use of personal protective equipment (PPE) in healthcare settings.
- Community Awareness: Educate communities about the risks and preventive measures.
- Surveillance: Monitoring and rapid response to outbreaks.
Epidemiology
Outbreak of Nipah virus encephalitis in the Kerala state of India
On 19 May 2018, a Nipah virus disease (NiV) outbreak was reported from Kozhikode district of Kerala, India. This is the first NiV outbreak in South India. There have been 17 deaths and 18 confirmed cases as of 1 June 2018. The two affected districts are Kozhikode and Mallapuram. A multi-disciplinary team led by the Indian Government’s National Centre for Disease Control (NCDC) is in Kerala in response to the outbreak. WHO is providing technical support to the Government of India as needed. WHO does not recommend the application of any travel or trade restrictions or entry screening related to the NiV outbreak.
- Outbreaks: Primarily reported in South and Southeast Asia, notably in Malaysia, Singapore, Bangladesh, and India.
- Mortality Rate: High, ranging from 40% to 75% depending on the outbreak and healthcare availability.
Research and Development
- Vaccines: Ongoing research into vaccines, with some candidates showing promise in preclinical studies.
- Antivirals: Continued efforts to find effective antiviral treatments.
Public Health Response
- Outbreak Control: Rapid isolation of infected individuals, contact tracing, and quarantine measures.
- International Collaboration: WHO and other global health organizations coordinate efforts to monitor and control NiV outbreaks.
Nipah virus poses a significant threat due to its high mortality rate and potential for human-to-human transmission, necessitating robust public health measures and ongoing research efforts.
The incubation period for Nipah virus, which is the time between exposure to the virus and the onset of symptoms, typically ranges from 4 to 14 days. However, in some cases, the incubation period can be as long as 45 days. This variation depends on several factors, including the route of exposure and the individual’s immune response.
2018 Outbreak
- First Detection: The Nipah virus was first detected in Kerala in May 2018.
- Affected Areas: The initial outbreak occurred in the Kozhikode and Malappuram districts.
- Cases and Fatalities: There were 23 reported cases, out of which 17 people died.
- Response: The Kerala government, along with national and international health agencies, implemented rigorous containment measures, including quarantine, isolation of suspected cases, and extensive contact tracing.
- Containment: The outbreak was effectively contained by June 2018.
2019 and 2021 Outbreaks
- 2019: Another isolated case was reported in June 2019 in Kochi. The patient survived, and there was no further spread due to prompt response measures.
- 2021: In September 2021, a new case was reported in Kozhikode. The patient, a 12-year-old boy, unfortunately died. Swift measures were again implemented to prevent further transmission.
2023 Outbreak
- New Cases: In September 2023, Kerala reported new cases of Nipah virus in the Kozhikode district.
- Response Measures: The state government reactivated containment protocols, including setting up containment zones, conducting extensive testing, and isolating suspected cases.
- Contact Tracing: Aggressive contact tracing was conducted to identify and monitor individuals who had come into contact with the infected persons.
Key Measures for Containment and Prevention
- Isolation and Quarantine: Infected individuals and their close contacts are isolated and quarantined to prevent the spread.
- Healthcare Monitoring: Healthcare workers are trained and monitored for symptoms due to their close contact with patients.
- Public Awareness: Awareness campaigns are conducted to educate the public about the symptoms, transmission methods, and preventive measures for Nipah virus.
- Animal Surveillance: Since Nipah virus can be transmitted from animals to humans (zoonotic transmission), surveillance of potential animal reservoirs, such as fruit bats, is conducted.
Impact and Challenges
- High Mortality Rate: Nipah virus has a high mortality rate, which makes it particularly dangerous.
- Economic and Social Impact: Outbreaks cause significant disruption, including economic losses and social stress due to fear and stigma.
- Healthcare Strain: Outbreaks strain healthcare resources, especially during concurrent health crises like the COVID-19 pandemic.
Conclusion
Kerala’s experience with Nipah virus highlights the importance of rapid response, effective public health measures, and international collaboration in managing outbreaks. Continuous vigilance and preparedness are essential to mitigate the impact of future outbreaks.
