P.B.B.Sc-Maternal-december-2022(sau.uni)(UPLOAD PAPER NO.5)
P.B.B.Sc-Maternal-december-2022 (SAU.UNI.)
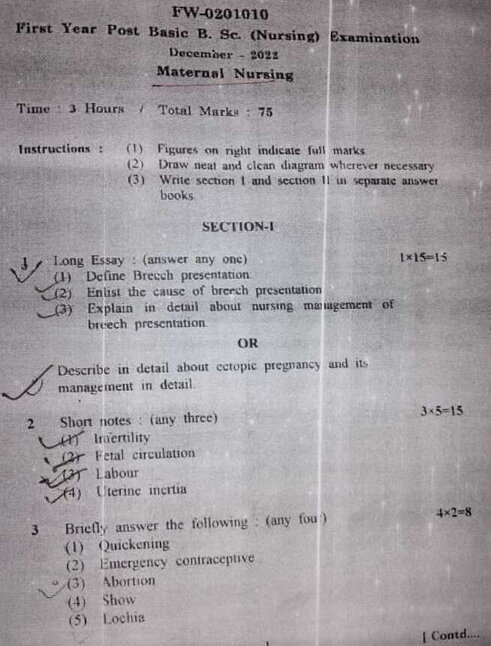

⏩SECTION-I⏪
⏩1.Long Essay (answer any one) 1×15-15
🔸(1) Define Breech presentation
Breech Presentation:
Breech presentation occurs when the fetus is positioned bottom or feet first in the uterus instead of the head-first position, which is typical for a vaginal delivery. It occurs in about 3-4% of full-term pregnancies.
Types of Breech Presentation:
- Frank Breech: The fetus’s buttocks are presenting first with the legs flexed at the hips and extended at the knees, with feet near the head.
- Complete Breech: The fetus’s buttocks are presenting first with both knees and hips flexed.
- Footling Breech: One or both of the fetus’s feet are presenting first.
🔸(2) Enlist the cause of breech presentation
Course of Breech Presentation:
- Diagnosis: Usually diagnosed during a prenatal check-up through physical examination and confirmed by ultrasound.
- Assessment of Risks: Evaluation of factors such as the mother’s pelvis size, previous delivery history, and the fetus’s size and position.
- Decision Making: Depending on the type of breech presentation and other factors, options include attempting a vaginal delivery or opting for a cesarean section (C-section).
- Delivery: Techniques for vaginal breech delivery require skill and experience due to potential risks such as head entrapment or umbilical cord prolapse.
- Post-Delivery: Monitoring for complications such as birth injuries or respiratory distress in the newborn.
🔸(3) Explain in detail about nursing management of breech presentation
Nursing Management of Breech Presentation:
Nursing management involves a comprehensive approach to support the mother and ensure the safety of both mother and fetus during labor and delivery:
1.Antenatal Care:
- Education: Educate the mother about breech presentation, delivery options, and potential complications.
- Monitoring: Regular monitoring of maternal and fetal well-being, including fetal heart rate and position checks.
2.Intrapartum Care:
- Preparation: Ensure that the delivery room is equipped for potential complications, whether preparing for vaginal breech delivery or a C-section.
- Support: Provide emotional support to the mother and family, as breech presentations may increase anxiety levels.
3.During Vaginal Breech Delivery:
- Positioning: Assist the obstetrician in positioning the mother optimally for delivery, often using the lithotomy position.
- Monitoring: Monitor fetal heart rate closely for signs of distress during the delivery process.
- Assistance: Be prepared to assist with maneuvers such as the Mauriceau-Smellie-Veit maneuver or the Lovset maneuver to facilitate delivery.
4.During Cesarean Section:
- Preparation: Prepare the mother for surgery, ensuring informed consent and addressing any concerns.
- Support: Provide emotional support and reassurance during the surgical procedure.
5.Postpartum Care:
- Monitoring: Monitor the mother and newborn closely for any signs of complications post-delivery.
- Breastfeeding Support: Encourage breastfeeding initiation and provide guidance as needed.
6.Patient Education:
- Recovery: Educate the mother about postpartum care, including wound care for C-section incisions if applicable.
- Follow-up: Schedule follow-up appointments to monitor recovery and address any concerns.
7.Documentation:
- Accurate Record Keeping: Document all assessments, interventions, and responses during labor, delivery, and postpartum care.
Nursing management of breech presentation requires vigilant monitoring, effective communication with the healthcare team, and readiness to intervene swiftly if complications arise, ensuring the best possible outcomes for both mother and baby.
🔸 OR🔸
🔸Describe in detail about ectopic pregnancy and its management in detail.
- Definition: An ectopic pregnancy occurs when a fertilized egg implants and begins to grow outside of the uterus, most commonly in the fallopian tube. However, it can also occur in other locations such as the ovary, abdomen, or cervix.
- Risk Factors:
- Previous ectopic pregnancy
- History of pelvic inflammatory disease (PID)
- Previous tubal surgery or infertility treatments
- Pelvic or abdominal surgeries
- Endometriosis
- Smoking
- Assisted reproductive techniques (e.g., IVF)
Clinical Presentation:
- Abdominal Pain: Often localized to one side, can be severe and sudden if the fallopian tube ruptures.
- Vaginal Bleeding: Light to moderate bleeding, often occurs around the time of the expected menstrual period.
- Other Symptoms: Shoulder tip pain (due to diaphragmatic irritation from blood), dizziness, fainting (if internal bleeding occurs).
Diagnosis:
- Ultrasound: Transvaginal ultrasound is the primary diagnostic tool to locate the gestational sac and confirm the ectopic pregnancy.
- Serum hCG Levels: Serial measurements of human chorionic gonadotropin (hCG) levels to monitor their rise. Slower-than-expected rise or plateauing hCG levels can indicate ectopic pregnancy.
- Pelvic Exam: A pelvic exam may reveal tenderness or palpable mass in the pelvic area.
Management: a. Medical Management:
- Methotrexate Therapy: A medication that stops the growth of the embryo and dissolves existing trophoblastic tissue.
- Indications: Early diagnosis, stable condition, small ectopic mass, and low hCG levels.Monitoring: Serial hCG levels to ensure they decrease appropriately.Side Effects: Nausea, abdominal pain, and possible effects on future fertility.Contraindications: Large ectopic mass, fetal cardiac activity, significant symptoms, or contraindications to methotrexate use (e.g., liver or kidney disease).
- Laparoscopic Salpingostomy: Removal of the ectopic pregnancy while preserving the fallopian tube.
- Indications: Unruptured ectopic pregnancy, intact fallopian tube, desire to preserve fertility.
- Advantages: Minimal invasiveness, shorter recovery time compared to open surgery.
- Laparoscopic Salpingectomy: Removal of the affected fallopian tube if it is severely damaged or has ruptured.
- Indications: Ruptured ectopic pregnancy, severe tubal damage, patient’s fertility concerns.
- Advantages: Prevents risk of future ectopic pregnancies in that tube, definitive treatment.
- Emergency Surgery (Laparotomy): If the ectopic pregnancy causes severe bleeding or if laparoscopic surgery is not feasible.
- Indications: Hemodynamic instability due to massive bleeding, failed laparoscopic approach.
- Expectant Management: Monitoring without immediate intervention in select cases where hCG levels are declining and there are no symptoms of rupture.
- Indications: Small, unruptured ectopic pregnancy, stable condition, declining hCG levels.
Post-Treatment Care:
- Monitoring: Serial hCG levels to ensure they decrease appropriately.
- Follow-up: Arrange for follow-up visits to monitor recovery, assess for any complications, and discuss future fertility options.
- Psychological Support: Provide emotional support due to the emotional impact of ectopic pregnancy and its implications for future pregnancies.
Patient Education:
- Signs and Symptoms: Educate patients about symptoms of ectopic pregnancy and when to seek medical attention.
- Future Fertility: Discuss the impact on future fertility and options for conception after ectopic pregnancy.
Complications:
- Rupture: Leading to severe internal bleeding and potentially life-threatening shock.
- Damage to Fallopian Tube: May require surgical removal (salpingectomy) if the tube is severely damaged.
- Psychological Impact: Emotional distress and anxiety about future pregnancies.
Effective management of ectopic pregnancy requires prompt diagnosis, appropriate treatment selection based on clinical presentation and patient factors, and close monitoring to ensure the best possible outcomes for the patient’s health and future fertility
⏩2 Short notes: (any three)3×5-15
🔸1) Infertility
INFERTILITY
- Definition: Infertility is the inability of a sexually active couple to achieve pregnancy after one year of regular, unprotected intercourse (or six months if the woman is over 35 years old).
- Causes:
- Female Factors: Ovulation disorders (e.g., PCOS), tubal factors (e.g., blocked fallopian tubes), uterine factors (e.g., fibroids), endocrine disorders (e.g., thyroid issues), and age-related decline in ovarian function.
- Male Factors: Sperm disorders (e.g., low sperm count, poor motility), testicular factors (e.g., varicocele, genetic conditions), and ejaculatory disorders (e.g., retrograde ejaculation).
3.Diagnosis:
- Medical History and Physical Examination: Assessing menstrual history, previous pregnancies, and examining reproductive organs.
- Hormonal Testing: Checking hormone levels (e.g., FSH, LH, estradiol) to evaluate ovarian and testicular function.
- Imaging Tests: Ultrasound to visualize pelvic organs, and HSG (hysterosalpingography) to evaluate the uterus and fallopian tubes.
- Semen Analysis: Assessing sperm count, motility, morphology, and other parameters in men.
4.Treatment Options:
- Medications: Hormonal treatments to induce ovulation in women, or to address hormonal imbalances in both men and women.
- Surgery: Correcting anatomical issues such as removing fibroids or repairing blocked fallopian tubes.
- Assisted Reproductive Technologies (ART): Including procedures like IVF (In Vitro Fertilization), IUI (Intrauterine Insemination), and ICSI (Intracytoplasmic Sperm Injection) to achieve pregnancy.
- Lifestyle Changes: Advising on weight management, diet, and reducing exposure to toxins (e.g., smoking, alcohol) to optimize fertility.
5.Psychological and Emotional Impact:
- Infertility can lead to stress, anxiety, and depression. Counseling, support groups, and open communication are essential for coping with emotional challenges.
6.Prognosis and Future Options:
- Prognosis varies based on the underlying cause, age of the partners, and response to treatment. Some couples may achieve pregnancy with treatment, while others may explore alternative options such as adoption or using donor gametes.
Understanding infertility involves a comprehensive approach, addressing both medical and emotional aspects to support individuals or couples through diagnosis, treatment, and decision-making processes
🔸(2 Fetal circulation
fetal circulation, explained
Placental Function:
- Exchange of Nutrients and Gases: The placenta serves as the organ of exchange between the maternal and fetal circulations. Oxygen and nutrients from the maternal blood diffuse across the placental membrane into the fetal blood, while carbon dioxide and waste products move from fetal blood to maternal blood for elimination.
Fetal Circulatory Pathway:
- Umbilical Vein: Oxygenated blood from the placenta enters the fetus through the umbilical vein.
- Ductus Venosus: A shunt that bypasses the fetal liver, directing most oxygenated blood directly to the inferior vena cava.
- Inferior Vena Cava: Oxygenated blood mixes with deoxygenated blood from the lower body and enters the right atrium of the heart.
Fetal Heart and Pulmonary Circulation:
- Foramen Ovale: A hole in the interatrial septum that allows most oxygenated blood to pass from the right atrium to the left atrium, bypassing the fetal lungs.
- Left Atrium and Left Ventricle: Oxygenated blood is pumped into systemic circulation through the aorta to supply oxygen and nutrients to the fetal body.
- Ductus Arteriosus: A shunt between the pulmonary artery and aorta that directs blood away from the non-functioning fetal lungs and into systemic circulation.
4.Return of Deoxygenated Blood:
- Superior Vena Cava: Deoxygenated blood from the upper body enters the right atrium.
- Right Ventricle: Deoxygenated blood is pumped into the pulmonary artery.
- Ductus Arteriosus: Most of the blood from the pulmonary artery bypasses the lungs through the ductus arteriosus into the descending aorta.
5.Placental Circulation:
- Umbilical Arteries: Deoxygenated blood and waste products from fetal circulation are carried back to the placenta through the umbilical arteries for exchange with maternal blood.
6.Changes at Birth:
- Cord Clamping: After birth, the umbilical cord is clamped and cut, ending the flow of blood through the umbilical vessels.
- Closure of Shunts: The foramen ovale and ductus arteriosus gradually close, redirecting blood flow to accommodate the new postnatal respiratory and circulatory demands.
Understanding fetal circulation is crucial for managing conditions like congenital heart defects and ensuring smooth transition to postnatal circulation after birth.
🔸3) Labour
1.Definition:
- Labor refers to the physiological process where the uterus contracts rhythmically to expel the fetus, placenta, and membranes from the mother’s body.
2.Stages of Labor:
- First Stage:
- Early Labor: Initial phase with irregular contractions, typically lasting several hours to days. Cervix begins to efface (thin) and dilate (open).
- Active Labor: Contractions become stronger, regular, and closer together, causing the cervix to dilate more rapidly, usually from 4 to 10 centimeters.
- Transition: Last phase of the first stage, characterized by intense contractions and complete cervical dilation (10 cm). Typically the shortest but most intense phase.
- Second Stage:
- Pushing Stage: Begins when the cervix is fully dilated and ends with the birth of the baby. Mother actively pushes during contractions to expel the fetus through the birth canal.
- Third Stage:
- Delivery of the Placenta: Afterbirth stage where the placenta separates from the uterine wall and is expelled. Generally lasts a few minutes to half an hour after the baby’s birth.
3.Signs and Symptoms:
- Contractions: Uterine contractions become stronger, longer, and more frequent.
- Cervical Changes: Effacement (thinning) and dilation (opening) of the cervix.
- Bloody Show: Discharge of mucus mixed with blood as the cervix begins to dilate.
- Rupture of Membranes: Breaking of the amniotic sac, releasing amniotic fluid (commonly referred to as the “water breaking”).
4.Management and Support:
- Monitoring: Continuous assessment of maternal vital signs, fetal heart rate, and progress of labor.
- Pain Relief: Options include non-pharmacological methods (e.g., relaxation techniques, massage) and pharmacological methods (e.g., epidural anesthesia).
- Positioning: Encouraging various positions (e.g., upright, squatting) to facilitate labor progression and comfort.
- Supportive Care: Emotional support from partners, family, and healthcare providers to alleviate anxiety and enhance coping during labor.
5.Complications and Interventions:
- Fetal Monitoring: Continuous monitoring of fetal heart rate to detect signs of distress.
- Labor Augmentation: Administration of medications (e.g., oxytocin) to strengthen contractions if labor progresses slowly.
- Assisted Delivery: Use of forceps or vacuum extraction if maternal or fetal health is at risk or if labor stalls.
- Cesarean Section: Surgical delivery if vaginal birth poses risks to mother or baby, or if indicated due to complications.
6.Postpartum Care:
- Immediate: Assessment of mother and baby’s health, monitoring for complications such as excessive bleeding or infection.
- Breastfeeding Initiation: Encouragement and assistance with breastfeeding within the first hour after birth.
- Emotional Support: Addressing emotions and providing information on postpartum recovery and care for mother and baby.
Understanding the stages, signs, management, and potential complications of labor is essential for healthcare providers and expectant parents to ensure a safe and positive birth experience.
🔸(4) Uterine inertia
Uterine inertia, also known as ineffective uterine contractions, is a condition where the uterus fails to contract effectively during labor, resulting in prolonged or stalled labor. Here’s a detailed explanation:
1.Definition:
- Uterine inertia refers to inadequate or ineffective uterine contractions during labor, which can lead to difficulty in cervical dilation and hinder progress in childbirth.
2.Types:
- Primary Uterine Inertia: The uterus fails to contract adequately from the beginning of labor, leading to slow or no progression of cervical dilation.
- Secondary Uterine Inertia: Contractions may initially be strong and regular but weaken or cease before the cervix is fully dilated, causing labor to stall.
3.Causes:
- Maternal Factors: Fatigue, dehydration, anxiety, or use of certain medications.
- Fetal Factors: Malpresentation (e.g., breech position), macrosomia (large baby), or abnormalities in the size or position of the fetus.
- Uterine Factors: Previous uterine surgery (e.g., C-sections), uterine malformations, or overdistension of the uterus (e.g., with multiple pregnancies).
- Hormonal Factors: Insufficient production or response to oxytocin, the hormone that stimulates uterine contractions.
4.Signs and Symptoms:
- Prolonged Labor: Labor lasting longer than usual without progress in cervical dilation.
- Irregular Contractions: Contractions may be weak, infrequent, or erratic in pattern.
- Fetal Distress: Signs such as abnormal fetal heart rate patterns (non-reassuring fetal heart rate).
5.Diagnosis:
- Diagnosis is typically based on clinical assessment, including monitoring of contractions and fetal heart rate patterns during labor. Vaginal examinations assess cervical dilation and effacement.
6.Management:
- Monitoring: Continuous assessment of maternal and fetal well-being, including fetal heart rate monitoring and maternal vital signs.
- Hydration and Nutrition: Intravenous fluids and nutrition to combat maternal dehydration and fatigue.
- Positioning: Encouragement of various maternal positions (e.g., upright, side-lying) to optimize uterine contractions.
- Oxytocin Administration: Synthetic oxytocin (Pitocin) may be administered intravenously to stimulate stronger and more frequent contractions.
- Amniotomy: Artificial rupture of membranes to augment labor progress, if appropriate.
- Supportive Care: Emotional support, encouragement, and reassurance to the mother to reduce anxiety and promote relaxation.
- Operative Delivery: Forceps or vacuum extraction may be considered if labor fails to progress despite interventions or if fetal distress is present.
- Cesarean Section: Surgical delivery may be necessary if attempts to stimulate labor are unsuccessful or if there are concerns for maternal or fetal well-being.
7.Prognosis:
- With appropriate management, many cases of uterine inertia can be resolved, leading to successful vaginal delivery. However, complications such as fetal distress or maternal exhaustion may necessitate interventions like cesarean delivery.
Understanding uterine inertia involves recognizing its causes, signs, and appropriate management strategies to ensure safe delivery and optimal outcomes for both mother and baby during labor.
⏩3 Briefly answer the following: (any fou) 4×2-8
🔸(1) Quickening
Quickening is the first perception of fetal movements by the pregnant woman, usually felt as fluttering sensations in the abdomen. It typically occurs between 16 to 25 weeks of pregnancy, although it can vary based on factors like maternal body habitus and placental location. Quickening is an important milestone in pregnancy that indicates fetal development and activity.
🔸(2) Emergency contraceptive
Emergency contraception (EC) is used to prevent pregnancy after unprotected intercourse, contraceptive failure, or sexual assault. It is most effective when taken as soon as possible after intercourse, ideally within 72 hours, though some types can be effective up to 5 days later. Types include:
– Levonorgestrel EC: Available over-the-counter (like Plan B One-Step) and works primarily by delaying ovulation.
– Ulipristal Acetate: Available by prescription (like ella) and inhibits or delays ovulation.
– Copper Intrauterine Device (IUD): Can be used as emergency contraception up to 5 days after unprotected sex and acts by preventing fertilization and possibly implantation.
🔸(3) Abortion
Abortion refers to the deliberate termination of a pregnancy. It can be spontaneous (miscarriage) or induced. Induced abortions are categorized as:
– Medical Abortion: Uses medications (such as mifepristone and misoprostol) to induce abortion in the first trimester.
– Surgical Abortion: Involves procedures (such as suction aspiration or dilation and evacuation) to remove the pregnancy from the uterus.
🔸(4) Show
The show, also known as bloody show or mucus plug, is a gelatinous plug of mucus that seals the cervical canal during pregnancy. It is expelled from the vagina as labor approaches and may be tinged with blood. The show is a natural part of the cervical changes that occur as the body prepares for labor and can be a sign that labor will begin soon.
🔸(5) Lochia
The show, also known as bloody show or mucus plug, is a gelatinous plug of mucus that seals the cervical canal during pregnancy. It is expelled from the vagina as labor approaches and may be tinged with blood. The show is a natural part of the cervical changes that occur as the body prepares for labor and can be a sign that labor will begin soon.
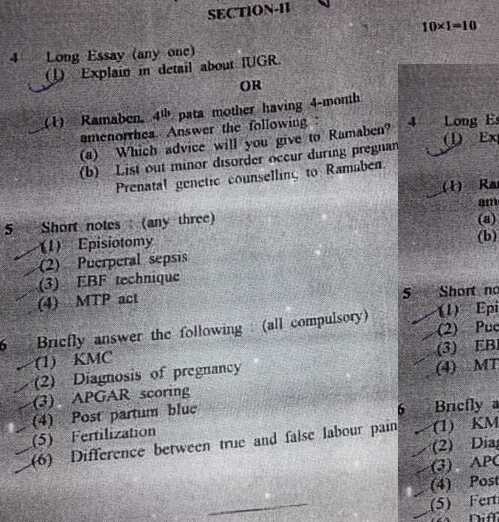
⏩SECTION-II⏪
⏩4 Long Essay (any one)10×1-10
🔸1) Explain in detail about. IUGR.
Definition: Intrauterine Growth Restriction (IUGR), also known as fetal growth restriction (FGR), refers to a condition where a fetus does not achieve its expected growth potential while in the uterus during pregnancy.
- Significance: It results in the baby being smaller than expected for its gestational age, which can lead to various health risks and complications.
👉2. Causes:
- Maternal Factors: Conditions such as hypertension, diabetes, chronic kidney disease, malnutrition, or infections (like cytomegalovirus) can affect placental function and nutrient delivery to the fetus.
- Placental Factors: Issues such as placental insufficiency, placental abruption, or abnormalities can restrict the supply of oxygen and nutrients to the fetus.
- Fetal Factors: Genetic conditions, chromosomal abnormalities, or infections affecting the fetus directly can impair growth.
- Environmental Factors: Factors like smoking, drug use, or exposure to toxins can also contribute to IUGR.
👉3. Types of IUGR:
- Symmetrical IUGR: Occurs when all parts of the fetus are proportionally small. It suggests that the growth restriction began early in pregnancy and is often due to genetic factors or severe maternal conditions affecting early development.
- Asymmetrical IUGR: In this type, the head and brain are relatively spared compared to the abdomen, indicating that growth restriction occurred later in pregnancy. It is typically associated with placental insufficiency or maternal conditions affecting later stages of fetal development.
👉4. Diagnosis:
- Ultrasound Evaluation: Key measurements include fetal weight estimation, abdominal circumference, head circumference, and femur length compared to standard growth charts for gestational age.
- Doppler Ultrasound: Assessing blood flow in the umbilical artery and other fetal vessels can indicate placental function and fetal well-being.
- Serial Monitoring: Regular monitoring is crucial to track fetal growth and detect any changes in growth patterns.
👉5. Complications:
- Intrauterine: Increased risk of stillbirth, reduced amniotic fluid (oligohydramnios), and abnormal fetal positioning.
- Postnatal: Low birth weight, premature birth, difficulties with thermoregulation, feeding problems, respiratory distress syndrome, and increased risk of neonatal intensive care unit (NICU) admission.
- Long-term: Developmental delays, neurodevelopmental disorders, and increased risk of chronic diseases later in life.
👉6. Management:
- Monitoring and Surveillance: Close monitoring with frequent ultrasounds and fetal heart rate monitoring to assess fetal well-being.
- Nutritional Support: Ensuring adequate maternal nutrition and, in some cases, nutritional supplementation to support fetal growth.
- Treatment of Underlying Causes: Managing maternal conditions such as hypertension or diabetes, and addressing placental issues if possible.
- Delivery Planning: Timing of delivery depends on the severity of IUGR, gestational age, and fetal well-being, balancing the risks of prematurity with the risks of continued intrauterine growth restriction.
👉7. Prognosis:
- Varied Outcomes: The prognosis depends on the underlying cause, severity of growth restriction, and timing of intervention.
- Improvement with Early Detection: Early detection and appropriate management can improve outcomes, but long-term effects on health and development may still occur.
- Follow-up Care: Close follow-up postnatally to monitor growth, development, and address any emerging issues.
🔸OR🔸
🔸(1) Ramaben, 4th para mother having 4-month amenorrhea. Answer the following:
🔸(a) Which advice will you give to Ramaben?
Advice for Ramaben:
Minor Disorders During Pregnancy:
- Morning Sickness: Eat small, frequent meals and stay hydrated.
- Heartburn: Avoid spicy and fatty foods; eat smaller meals more frequently.
- Constipation: Increase fiber intake and drink plenty of fluids.
- Backache: Practice good posture, use proper body mechanics, and consider prenatal exercises.
- Varicose Veins: Elevate legs when resting, avoid sitting or standing for long periods.
- Fatigue: Rest when needed, maintain a balanced diet, and exercise regularly.
Prenatal Genetic Counseling:
- Purpose: Explain the purpose of genetic counseling, which is to assess the risk of genetic disorders in the baby.
- Family History: Discuss Ramaben’s and her partner’s family medical histories to assess any genetic risks.
- Screening Tests: Explain various prenatal screening tests such as ultrasound, blood tests (like NIPT), and diagnostic tests (like amniocentesis) to detect genetic conditions.
- Risks and Benefits: Outline the risks and benefits of each test to help Ramaben make informed decisions.
- Counseling Process: Describe the counseling process, including the involvement of a genetic counselor or healthcare provider who specializes in genetics.
- Emotional Support: Offer emotional support and resources, as genetic counseling can involve complex decisions and emotions.
Ramaben should manage minor pregnancy-related issues with lifestyle adjustments and seek prenatal genetic counseling to assess potential genetic risks for her baby, ensuring informed decision-making throughout her pregnancy journey.
🔸(b) List out minor disorder occur during pregnancy Prenatal genetic counselling to Ramaben.
Minor Disorders During Pregnancy
1.Morning Sickness (Nausea and Vomiting):
- Typically occurs in the first trimester.
- Can be managed with dietary changes and hydration.
2.Heartburn:
- Caused by hormonal changes and pressure on the stomach.
- Managed with small, frequent meals and avoiding trigger foods.
3.Constipation:
- Due to hormonal changes and iron supplements.
- Increased fiber intake and hydration can help.
4.Hemorrhoids:
- Caused by increased pressure on the rectal veins.
- Managed with a high-fiber diet and avoiding prolonged sitting.
5.Back Pain:
- Due to the growing uterus and hormonal changes.
- Exercises, proper posture, and support belts can provide relief.
6.Leg Cramps:
- Commonly occur at night.
- Stretching, staying hydrated, and adequate calcium intake can help.
7.Swelling (Edema):
- Often in the feet and ankles due to fluid retention.
- Elevating the feet and reducing salt intake can help.
8.Frequent Urination:
- Due to increased pressure on the bladder.
- Normal but staying hydrated is important.
9.Fatigue:
- Due to hormonal changes and increased energy demands.
- Rest and balanced nutrition are key.
10.Varicose Veins:
- Caused by increased blood volume and pressure on veins.
- Compression stockings and leg elevation can help.
Prenatal Genetic Counseling for Ramaben
Prenatal genetic counseling provides information and support to expecting parents regarding the risk of genetic disorders in their unborn child. Here’s a basic outline for counseling Ramaben:
1.Introduction and Purpose:
- Explain the purpose of genetic counseling and what to expect.
- Discuss the importance of understanding genetic risks.
2.Medical and Family History:
- Gather detailed medical histories of both parents.
- Identify any family history of genetic disorders or birth defects.
3.Risk Assessment:
- Based on family history and medical background, assess the risk of genetic disorders.
- Discuss the likelihood of inherited conditions.
4.Genetic Testing:
- Explain available genetic tests (e.g., blood tests, amniocentesis, chorionic villus sampling).
- Discuss the benefits, risks, and limitations of each test.
5.Results Interpretation:
- Help understand the results of genetic tests.
- Discuss potential outcomes and implications for the pregnancy.
6.Options and Decisions:
- Discuss possible options based on test results (e.g., further testing, monitoring, or treatments).
- Support Ramaben in making informed decisions about her pregnancy.
7.Emotional Support:
- Provide emotional support and address any concerns or anxieties.
- Refer to support groups or mental health professionals if needed.
8.Follow-Up:
- Plan for follow-up appointments to monitor the pregnancy and discuss any new findings.
- Provide contact information for ongoing support and questions.
By providing this comprehensive guidance, prenatal genetic counseling aims to help Ramaben understand her options, make informed decisions, and feel supported throughout her pregnancy.
⏩5 Short notes (any three) 5×3-15
🔸(1) Episiotomy
Episiotomy: Detailed Explanation
1.Definition:
- Episiotomy is a surgical procedure performed during childbirth. It involves making a surgical incision in the perineum, the area between the vaginal opening and the anus. The purpose is to enlarge the vaginal opening to facilitate delivery and prevent spontaneous tearing of the perineum.
2.Types:
- Midline (Median) Episiotomy: The incision is made straight down the midline of the perineum towards the anus. This is the most common type.
- Mediolateral Episiotomy: The incision is made at an angle to the midline, usually at about a 45-degree angle. This type may reduce the risk of severe tears extending into the anal sphincter but may take longer to heal.
3.Indications:
- Facilitation of Delivery: It is typically considered when there is concern that the perineum may tear during childbirth, especially if the baby’s head is large or the delivery is occurring rapidly.
- Fetal Distress: In cases where rapid delivery is necessary for the baby’s well-being.
- Instrumental Delivery: Sometimes performed alongside forceps or vacuum-assisted delivery to ease the passage of the baby.
4.Procedure:
- The procedure is usually performed under local anesthesia.
- A small incision is made in the perineum using surgical scissors or a scalpel.
- The incision is carefully closed with absorbable stitches after the baby is delivered.
5.Complications and Considerations:
- Pain and Discomfort: The episiotomy site can be painful initially and may require pain management.
- Healing: Proper wound care is crucial to prevent infection and promote healing.
- Long-term Effects: In some cases, episiotomy may lead to prolonged discomfort during intercourse and increased risk of pelvic floor disorders.
- Prevalence: Over recent years, the frequency of episiotomy has declined due to concerns about routine use and the preference for allowing natural tearing which may heal better in some cases.
Episiotomy remains a topic of ongoing debate and is typically performed based on clinical judgment and individual circumstances during childbirth to optimize outcomes for both mother and baby.
🔸(2) Puerperal sepsis
Puerperal sepsis, also known as postpartum sepsis, is a potentially life-threatening infection that occurs after childbirth. Here’s a detailed explanation:
Puerperal Sepsis: Detailed Explanation
1,Definition:
- Puerperal sepsis refers to an infection that occurs in the genital tract after childbirth, usually within the first 6 weeks postpartum. It can involve the uterus (endometritis), the surrounding tissues (parametritis), or more rarely, other pelvic organs.
2.Causes:
- Bacterial Infections: Most commonly caused by bacteria such as Group A Streptococcus, Escherichia coli (E. coli), and Staphylococcus aureus.
- Risk Factors: Factors that increase the risk include prolonged labor, multiple vaginal examinations during labor, prolonged rupture of membranes, and retained products of conception after delivery.
3.Signs and Symptoms:
- Fever: Often the first and most prominent symptom, typically occurring within the first 24-48 hours postpartum.
- Uterine Tenderness: Pain and tenderness in the lower abdomen, often accompanied by foul-smelling vaginal discharge.
- Other Signs: Rapid heart rate (tachycardia), chills, malaise, and sometimes signs of systemic infection such as hypotension and confusion.
4.Diagnosis:
- Diagnosis is based on clinical symptoms, physical examination findings (including abdominal tenderness), and sometimes imaging studies (such as ultrasound) to evaluate for retained products of conception or abscess formation.
5.Treatment:
- Antibiotics: Broad-spectrum antibiotics are typically administered intravenously to cover likely pathogens until specific culture results are available.
- Supportive Care: Fluid resuscitation and supportive measures to stabilize vital signs and manage symptoms.
- Surgical Intervention: In severe cases with abscess formation or non-resolving infection, surgical drainage or evacuation of retained products may be necessary.
6.Complications:
- Without prompt and adequate treatment, puerperal sepsis can lead to severe complications such as septic shock, disseminated intravascular coagulation (DIC), organ failure, and even death.
- Long-term complications can include pelvic inflammatory disease (PID), infertility, and chronic pelvic pain.
7.Prevention:
- Good hygiene practices during labor and delivery, appropriate use of antibiotics prophylactically when indicated, and prompt recognition and treatment of infections are key to preventing puerperal sepsis.
- Puerperal sepsis requires timely medical attention and treatment to reduce morbidity and mortality, highlighting the importance of postpartum care and vigilance in detecting early signs of infection after childbirth.
🔸(3) EBF technique
EBF stands for Exclusive Breastfeeding, which refers to the practice of feeding an infant solely with breast milk without any additional food or drink, including water, for the first six months of life. Here’s an overview of the EBF technique:
Exclusive Breastfeeding (EBF) Technique
1.Definition:
- EBF involves feeding the baby only breast milk, directly from the breast or expressed, and avoiding all other liquids and solids, including formula and water.
2.Benefits:
- Nutritional Superiority: Breast milk is uniquely tailored to meet the nutritional needs of infants, providing ideal proportions of nutrients, antibodies, and growth factors.
- Health Benefits: Reduces the risk of infections, respiratory illnesses, allergies, and chronic diseases for both mother and baby.
- Bonding: Promotes bonding between mother and baby through skin-to-skin contact and breastfeeding.
- Convenience: Always available at the right temperature, sterile, and requires no preparation.
3.Initiation and Frequency:
- Early Initiation: Ideally, breastfeeding should be initiated within the first hour after birth to promote bonding and stimulate milk production.
- Frequency: Newborns typically feed 8-12 times in 24 hours, feeding on demand (whenever the baby shows hunger cues like rooting or sucking fists).
4.Positioning and Latching:
- Proper Positioning: The mother should be comfortable, and the baby positioned with their whole body facing the mother, with support for their head and neck.
- Deep Latch: Ensuring the baby takes in a good amount of breast tissue, not just the nipple, to prevent nipple pain and ensure effective milk transfer.
5.Mother’s Diet and Hydration:
- Healthy Diet: The mother should eat a balanced diet rich in nutrients and stay hydrated to support milk production.
- Avoiding Certain Foods: Some mothers may need to avoid spicy foods or certain allergens if they cause discomfort or reactions in the baby.
6.Challenges and Support:
- Engorgement and Soreness: Common early challenges that can often be managed with proper positioning, latching techniques, and sometimes using cold compresses or warm showers.
- Support: Access to support from healthcare providers, lactation consultants, and support groups can help address concerns and provide encouragement.
7.Duration and Complementary Feeding:
- Duration: Exclusive breastfeeding is recommended for the first six months of life. After six months, complementary foods are gradually introduced while breastfeeding continues up to two years or beyond.
Exclusive breastfeeding is a natural and beneficial way to nourish infants, providing optimal nutrition and promoting overall health and well-being for both mother and baby.
🔸(4) MTP act
The MTP Act refers to the Medical Termination of Pregnancy Act, 1971, in India. Here’s a detailed explanation:
Medical Termination of Pregnancy (MTP) Act, 1971
1.Purpose:
- The MTP Act was enacted to regulate and provide legal grounds for the termination of pregnancies in India to protect the health and well-being of women.
2.Legal Grounds for Abortion:
- Up to 12 Weeks: Abortion can be performed by a registered medical practitioner if the pregnancy poses a risk to the physical or mental health of the woman, or if it is a result of rape or contraceptive failure.
- Between 12 to 20 Weeks: Abortion requires the opinion of two registered medical practitioners stating that the continuation of pregnancy would involve a risk to the life of the pregnant woman or cause grave injury to her physical or mental health, or if there is a substantial risk that the child, if born, would suffer from physical or mental abnormalities.
3.Authorized Medical Practitioners:
- Abortion must be performed by a registered medical practitioner in a hospital established or maintained by the government or a place approved for this purpose by the government.
4.Conditions and Procedures:
- The procedure must be conducted under conditions that ensure the safety of the woman.
- Consent of the pregnant woman (or in the case of a minor, consent of her guardian) is required for the abortion.
5.Post-Abortion Care:
- The Act emphasizes the provision of post-abortion care and counseling services to ensure the well-being of women who undergo abortions.
6.Amendments:
- The MTP Act has undergone amendments over the years, including extending the upper limit for legal abortion from 20 weeks to 24 weeks in certain circumstances, such as substantial fetal abnormalities.
7.Controversies and Challenges:
- Despite legal provisions, challenges remain in ensuring access to safe and legal abortion services, especially in rural and underserved areas.
- Societal stigma and lack of awareness about the legal provisions sometimes hinder women from seeking timely abortion services.
The MTP Act, 1971, aims to provide a framework for safe and legal termination of pregnancies in India, ensuring that women have access to reproductive health services while safeguarding their rights and health.
⏩6 Briefly answer the following: (all compulsory) 6×2-12
🔸(1) KMC
Definition and Benefits: Kangaroo Mother Care (KMC) involves placing a premature or low birth weight infant skin-to-skin on the mother’s chest or caregiver’s chest, promoting bonding and providing warmth and stability. It has significant benefits:
- Temperature Regulation: Skin-to-skin contact helps regulate the baby’s body temperature, reducing the need for external warming devices.
- Breathing and Heart Rate Stability: The close contact stabilizes respiratory rates and heart rates, promoting more regular breathing patterns.
- Breastfeeding Promotion: Encourages early and exclusive breastfeeding, which provides essential nutrients and antibodies crucial for the baby’s health and development.
- Weight Gain: Babies in KMC often show improved weight gain compared to those not receiving KMC.
- Psychosocial Development: Enhances bonding between parent and baby, supporting emotional development and reducing stress for both.
🔸(2) Diagnosis of pregnancy
Methods and Process: Diagnosis of pregnancy involves various methods to confirm and monitor fetal development:
- Home Pregnancy Tests: Detect the presence of hCG in urine, typically confirming pregnancy as early as a few days after a missed period.
- Clinical Examination: Healthcare providers assess physical signs such as an enlarged uterus, changes in the cervix, and fetal heartbeat detection using a stethoscope or Doppler ultrasound.
- Ultrasound: Provides visual confirmation of pregnancy, evaluates fetal age, position, and health, and detects multiple pregnancies or abnormalities like ectopic pregnancies.
- Blood Tests: Measure hCG levels to monitor pregnancy progression and detect potential complications such as ectopic pregnancy or miscarriage.
🔸(3) APGAR scoring
Purpose and Components: APGAR scoring evaluates a newborn’s immediate condition after birth using the following criteria:
- Appearance: Assesses skin color, with a score of 0 for pale or blue, 1 for body pink with blue extremities, and 2 for completely pink.
- Pulse: Measures heart rate, with a score of 0 for absent, 1 for below 100 beats per minute, and 2 for above 100 beats per minute.
- Grimace Response: Tests reflex irritability, scored 0 for no response, 1 for grimace, and 2 for vigorous cry.
- Activity: Evaluates muscle tone, with 0 for limp, 1 for some flexion of extremities, and 2 for active movement.
- Respiration: Assesses breathing effort, scored 0 for absent, 1 for slow or irregular, and 2 for good crying.
- Scoring and Interpretation: Scores range from 0 to 10, with higher scores indicating better overall newborn health. A score of 7 or more generally indicates a healthy newborn requiring routine care, while scores below 7 may prompt medical intervention.
🔸(4) Post partum blue
Purpose and Assessment: Postpartum BLUE is an acronym used to assess the immediate post-birth condition of newborns:
- Breathing: Observes respiratory effort, ensuring the baby is breathing regularly and effectively.
- Look: Assesses skin color for signs of adequate oxygenation, ensuring the baby is pink and not showing signs of cyanosis (bluish tint).
- Tone: Evaluates muscle tone, ensuring the baby has active movements and is not floppy or excessively rigid.
- Activity: Checks for signs of alertness and responsiveness, assessing the baby’s overall level of consciousness and interaction.
- Expression: Examines facial movements for signs of discomfort or distress, ensuring the baby is comfortable and adjusting to its new environment.
- Use: Helps healthcare providers quickly identify any signs of distress or abnormality in newborns, guiding immediate interventions and ensuring appropriate care is provided.
🔸(5) Fertilization
Process and Steps: Fertilization is the process where a sperm cell fuses with an egg cell to form a zygote, initiating pregnancy:
- Events: Occurs in the fallopian tube, typically within 24 hours after ovulation when the egg is viable. Sperm cells swim through the cervix and uterus to reach the fallopian tube, where one sperm cell penetrates the egg’s outer layer.
- Zygote Formation: Fusion of genetic material from the sperm and egg forms a zygote, containing a complete set of chromosomes and initiating cellular division.
- Implantation: The zygote travels down the fallopian tube to the uterus, where it implants into the uterine lining, beginning pregnancy.
🔸(6) Difference between true and false labour pain
Characteristics and Recognition:
- True Labor:
- Contractions: Regular intervals, becoming stronger, longer, and more frequent over time, typically occurring in the lower back and abdomen.
- Cervical Changes: Progressive cervical dilation (opening) and effacement (thinning), preparing for childbirth.
- Progress: Continues despite rest or changes in activity, typically leading to the birth of the baby.
- False Labor (Braxton Hicks Contractions):
- Contractions: Irregular intervals, often felt as mild cramps or tightening in the abdomen, without increasing intensity or frequency.
- Cervical Changes: Little or no cervical dilation or effacement occurs.
- Pain: Concentrated in the lower abdomen and groin, may subside with rest, hydration, or change in activity.
- Nature: True labor involves rhythmic, painful contractions that progressively lead to childbirth, while false labor consists of irregular contractions without cervical changes or progressive pain intensity.
💪 💥☺ALL THE BEST ☺💥💪

IF ANY QUERY OR QUESTION,REVIEW-KINDLY WATSAPP US No. – 84859 76407