Anatomy & Physiology-(BKNMU) (DONE)(MODIFY PENDING)(UPLOAD PAPER NO.6
PAPER SOLUTION NO.6
Applied Anatomy & Physiology Paper Solution-BKNMU
⏩SECTION-1 ⏪
⏩ Q.1 Long essay type. (Any One)(10)
🔸1.Define human cell & explain its organelles with diagram [2+8]
ANSWER:-
Human Cell: Definition A human cell is the basic structural and functional unit of the human body. It is the smallest unit capable of performing life functions and is fundamental to the biology of all living organisms. Human cells are eukaryotic, meaning they have a defined nucleus and specialized structures called organelles that perform specific functions necessary for the cell’s survival and activity.
Structure of a Human Cell
human cell along with a description of its key organelles:
Key Organelles and Their Functions
1.Nucleus
Function Acts as the control center of the cell. It stores the cell’s DNA, which contains the genetic blueprint for the organism. The nucleus also coordinates activities like growth, metabolism, protein synthesis, and cell division.
Components
Nuclear Envelope A double membrane that encloses the nucleus, separating it from the cytoplasm.
Nucleolus A region within the nucleus where ribosomal RNA (rRNA) is produced and ribosome assembly begins.
Chromatin DNA material in the form of a complex with proteins, which condenses to form chromosomes during cell division.
2.Cytoplasm
Function A jelly-like substance that fills the cell and contains all the organelles. It is the site for most cellular processes and reactions.
Components
Cytosol The fluid part of the cytoplasm, rich in proteins, ions, and molecules.
3.Cell Membrane (Plasma Membrane)
Function Acts as a selective barrier that controls the movement of substances in and out of the cell. It maintains the cell’s integrity and provides communication with other cells.
Structure Composed of a phospholipid bilayer with embedded proteins.
4.Mitochondria
Function Known as the “powerhouses” of the cell, they generate most of the cell’s supply of adenosine triphosphate (ATP), used as a source of chemical energy.
Structure
Double-membraned organelles with their own DNA, enabling them to produce some of their own proteins.
5.Endoplasmic Reticulum (ER)
Function Plays a crucial role in the synthesis of proteins and lipids.
Types
Rough ER
Studded with ribosomes and involved in protein synthesis and quality control.
Smooth ER
Lacks ribosomes and is involved in lipid synthesis, detoxification, and calcium storage.
6.Golgi Apparatus
Function Modifies, sorts, and packages proteins and lipids for secretion or delivery to other organelles. It acts as the cell’s post-office.
Structure
Consists of a series of flattened membrane sacs called cisternae.
7.Lysosomes
Function Contain digestive enzymes to break down waste materials and cellular debris. They are involved in processes such as autophagy (self-eating) and recycling of cellular components.
Structure
Membrane-bound vesicles filled with hydrolytic enzymes.
8.Peroxisomes
Function Break down fatty acids and detoxify harmful substances. They contain enzymes that produce and break down hydrogen peroxide.
Structure Small, membrane-bound organelles containing oxidative enzymes.
9.Ribosomes
Function Sites of protein synthesis. They translate genetic information from mRNA to produce proteins.
Structure
Composed of rRNA and proteins, they can be found floating freely in the cytoplasm or attached to the rough ER.
10.Cytoskeleton
Function Provides structural support to the cell, facilitates cell movement, and organizes cell contents.
Components
Microfilaments
Thin filaments involved in cell movement and shape.
Intermediate Filaments
Provide mechanical support and stability.
Microtubules
Thick filaments that form the cell’s internal framework and are involved in intracellular transport and cell division.
11.Centrioles
Function Play a key role in cell division by organizing the microtubules during mitosis.
Structure
Cylindrical structures made of microtubules, usually found in pairs.
12.Vesicles
Function Small membrane-bound sacs that transport materials within the cell and to the cell membrane for release outside.
Types Include transport vesicles, secretory vesicles, and endocytic vesicles.
🔸2.Define Digestive system & explain its the organs with diagram [2+8]
ANSWER:-
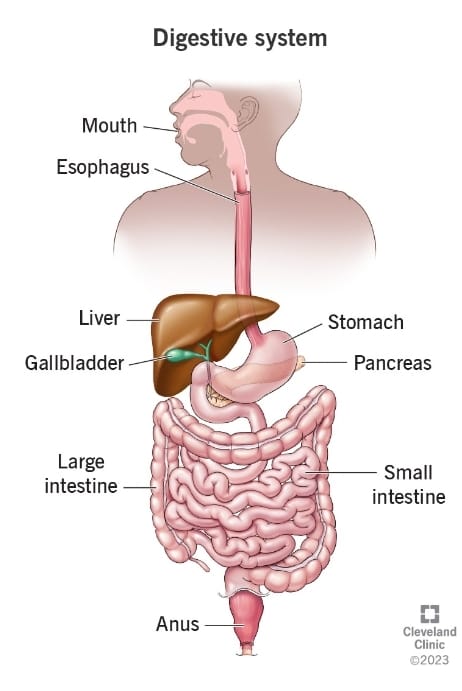
Digestive System: Definition The digestive system is a complex network of organs and glands responsible for breaking down food into nutrients, which the body can absorb and use for energy, growth, and cellular repair. It involves both mechanical and chemical processes to convert food into smaller, absorbable components. The system also manages the elimination of indigestible waste.
Structure of the Digestive System
human digestive system, followed by an explanation of its key organs.
Key Organs and Their Functions
1.Mouth (Oral Cavity)
Function The entry point for food. Mechanical digestion begins with chewing (mastication), and chemical digestion starts with saliva, which contains enzymes (like amylase) to break down carbohydrates.
Components
Teeth Grind and break down food into smaller pieces.
Tongue Helps in manipulating food and aids in swallowing.
Salivary Glands Produce saliva that moistens food and begins the digestion of starches.
2.Pharynx
Function A muscular tube that serves as a pathway for food moving from the mouth to the esophagus. It also plays a role in breathing and speech.
Components Divided into the nasopharynx, oropharynx, and laryngopharynx.
3.Esophagus
Function A muscular tube that transports food from the pharynx to the stomach using peristaltic movements (rhythmic contractions).
Structure
Lined with mucous membrane and muscle layers that facilitate the passage of food.
4.Stomach Function A muscular, J-shaped organ that stores and mixes food. It secretes gastric juices, including hydrochloric acid and digestive enzymes, to further break down food into a semi-liquid form called chyme.
Components
Fundus The upper part that stores undigested food and gases released during digestion.
Body The main, central region where food mixing and chemical digestion occur.
Pylorus
The lower part that regulates the passage of chyme into the small intestine.
5.Small Intestine
Function The primary site of digestion and nutrient absorption. It further digests food using enzymes from the pancreas and bile from the liver.
Divisions
Duodenum
The first section where most chemical digestion occurs. It receives bile and pancreatic juices.
Jejunum The middle section where most nutrient absorption takes place.
Ileum The final section, which absorbs remaining nutrients and delivers waste to the large intestine.
6.Large Intestine (Colon)
Function Absorbs water and electrolytes from indigestible food matter and compacts it into feces. It houses beneficial bacteria that aid in digestion.
Components
Cecum The beginning of the large intestine, connected to the ileum.
Ascending, Transverse, Descending, and Sigmoid Colon
Sections that move waste towards the rectum.
Rectum Stores feces until they are expelled.
Anus The opening through which feces are expelled from the body.
7.Liver
Function Produces bile, which helps digest fats. It also processes nutrients absorbed from the small intestine and detoxifies chemicals.
Structure
A large, lobed organ located in the upper right abdomen.
8.Gallbladder Function Stores and concentrates bile produced by the liver and releases it into the small intestine to aid in the digestion of fats.
Structure A small, pear-shaped sac located beneath the liver.
9.Pancreas
Function Produces digestive enzymes that break down carbohydrates, proteins, and fats. It also produces insulin and glucagon, which regulate blood sugar levels.
Structure
A gland located behind the stomach with both exocrine (digestive) and endocrine (hormonal) functions.
⏩ Q.2 Write short notes on following. (Any Four)(20)
🔸1.Anatomy of gall bladder
ANSWER:-
Detailed Anatomy of the Gallbladder
The gallbladder is a vital organ within the biliary system, intricately linked to the liver and small intestine. It serves primarily as a storage and concentrating reservoir for bile, facilitating the digestion of fats.
Here’s a detailed examination of its anatomy, encompassing its structure, layers, associated ducts, blood supply, and innervation.
External Structure
1.Fundus
Description
The broad, rounded end of the gallbladder.
Location
Projects anteriorly and often inferiorly beyond the liver’s margin. It is the most anterior part and is usually palpable when enlarged.
Function Acts as a reservoir, holding bile until it is needed.
2.Body
Description The central, largest part of the gallbladder.
Location
Lies between the fundus and the neck, nestled against the visceral surface of the liver.
Function
Stores and concentrates bile by absorbing water and ions through its mucosa.
3.Neck
Description The narrow, tapered section connecting the body to the cystic duct.
Location Positioned closest to the liver, it curves to form the junction with the cystic duct.
Function Controls the flow of bile into and out of the gallbladder. Contains the Heister’s
valve which regulates this flow and prevents backflow into the cystic duct.
Internal Structure
4.Layers of the Gallbladder Wall
Mucosa
Description The innermost layer, lined with simple columnar epithelial cells.
Features Highly folded into rugae, which expand to accommodate bile storage. It is rich in mucous glands that produce mucus to protect the lining and facilitate bile flow.
Function Absorbs water and electrolytes from bile, concentrating it.
Muscularis
Description The middle layer composed of smooth muscle fibers.
Arrangement The fibers are oriented in multiple directions (longitudinal, oblique, and transverse).
Function Contracts to expel bile into the cystic duct during digestion, particularly in response to the hormone cholecystokinin.
Perimuscular Layer Description A layer of connective tissue surrounding the muscularis.
Function Provides structural support and elasticity to the gallbladder.
Serosa
Description The outermost layer covering the free surface of the gallbladder.
Function Reduces friction as the gallbladder moves against other organs. The liver surface covering is known as the adventitia.
Ductal System
5.Cystic Duct Description A short, tubular structure connecting the gallbladder neck to the common bile duct.
Location Runs alongside the hepatic ducts and merges to form the common bile duct.
Function Facilitates the flow of bile from the gallbladder to the common bile duct and vice versa for bile storage.
6.Common Bile Duct
Description Formed by the junction of the cystic duct and the common hepatic duct.
Location Extends down to the duodenum.
Function Delivers bile from the liver and gallbladder to the small intestine for fat digestion.
Blood Supply and Innervation
7.Arterial Supply
Cystic Artery
Source
Usually branches off from the right hepatic artery.
Path Supplies oxygenated blood to the gallbladder and a portion of the cystic duct.
Variants The anatomical variations in the origin and course of the cystic artery are common and significant in surgical procedures.
8.Venous Drainage
Cystic Veins
Function Drain deoxygenated blood from the gallbladder into the portal vein system, typically into the liver’s right branch of the portal vein.
Relevance Proper drainage is essential for maintaining gallbladder function and health.
9.Lymphatic Drainage
Pathway Lymph from the gallbladder drains into the cystic lymph node (often referred to as Calot’s node) and then to hepatic and celiac lymph nodes.
Function Important for immune response and filtration of lymphatic fluid from the gallbladder area.
10.Innervation
Sympathetic Nerve Supply
Source
Originates from the celiac plexus.
Function Modulates the contraction and relaxation of the gallbladder, typically inhibiting contraction and thus bile release.
Parasympathetic Nerve Supply
Source
Provided by the vagus nerve.
Function Stimulates gallbladder contraction and bile secretion during digestion.
Sensory Innervation
Source Pain fibers travel with the sympathetic nerves to the spinal cord segments T7-T9.
Function Transmits pain signals, often leading to referred pain in the right shoulder or back in cases of gallbladder inflammation.
Function of the Gallbladder
Bile Storage The gallbladder stores bile produced by the liver when digestion is not actively occurring.
Bile Concentration It concentrates bile by absorbing water and ions, making bile more potent for fat emulsification.
Bile Release During digestion, particularly after fatty meals, the gallbladder contracts and releases bile into the small intestine to aid in fat digestion.
🔸2.Anatomy of eyeball
Anatomy of the Eyeball
The human eyeball is a complex, spherical organ essential for vision. It is designed to focus light on the retina, convert it into neural signals, and transmit these signals to the brain, where they are interpreted as visual images. The structure of the eyeball includes multiple layers and specialized components that work together to perform these functions.
anatomy of the eyeball:
Key Structures of the Eyeball
1.Fibrous Tunic (Outer Layer)
Cornea
Description The transparent, dome-shaped front part of the eye.
Function Allows light to enter the eye and focuses it onto the lens. It provides most of the eye’s optical power.
Features No blood vessels, richly supplied with nerve endings, highly curved to facilitate light refraction.
Sclera
Description The white, opaque outer layer of the eye.
Function Provides structural support and protection. It also serves as an attachment site for the extrinsic eye muscles.
Features Tough, fibrous tissue that maintains the shape of the eyeball.
2.Vascular Tunic (Middle Layer or Uvea)
Choroid
Description A vascular layer located between the sclera and the retina.
Function Supplies oxygen and nutrients to the outer layers of the retina. Its pigmented cells absorb excess light, preventing reflection and scattering within the eye.
Features Rich in blood vessels and melanin.
Ciliary Body
Description A ring of tissue that encircles the lens.
Function Contains the ciliary muscle, which controls the shape of the lens for focusing (accommodation). It also produces aqueous humor, the fluid that fills the anterior segment of the eye.
Features Connected to the lens by suspensory ligaments (zonular fibers).
Iris
Description The colored part of the eye, containing muscles that regulate the size of the pupil.
Function Controls the amount of light entering the eye by adjusting the size of the pupil. The pupil is the central opening in the iris.
Features Contains two sets of muscles—sphincter pupillae (constricts the pupil) and dilator pupillae (dilates the pupil).
3.Nervous Tunic
(Inner Layer)
Retina
Description The innermost layer, a thin, light-sensitive tissue lining the back of the eye.
Function Converts light into electrical signals sent to the brain via the optic nerve.
Features Contains photoreceptors (rods and cones), responsible for detecting light intensity and color.
Other Critical Structures
4.Lens
Description A transparent, biconvex structure located behind the iris.
Function Focuses light onto the retina. Its curvature can be adjusted to focus on objects at various distances (accommodation).
Features Held in place by the suspensory ligaments connected to the ciliary body.
5.Anterior Segment Anterior Chamber
Description The fluid-filled space between the cornea and the iris.
Function Filled with aqueous humor, which maintains intraocular pressure, nourishes the cornea and lens, and removes waste.
Posterior Chamber
Description The space between the iris and the lens.
Function Also filled with aqueous humor, contributing to the flow of this fluid from the ciliary body to the anterior chamber.
6.Vitreous Chamber
Description The large, clear space between the lens and the retina.
Function Filled with vitreous humor, a gel-like substance that helps maintain the eyeball’s shape and keeps the retina in place.
7.Optic Nerve
Description The nerve that transmits visual information from the retina to the brain.
Function Carries electrical impulses generated by the retina to the visual cortex, where they are interpreted as images.
Features Exits the eye at the optic disc (blind spot), where there are no photoreceptors.
8.Macula
Description A small, central area of the retina.
Function Responsible for high-acuity vision and color perception.
Features Contains the fovea, the central pit with the highest concentration of cones (photoreceptors for detailed and color vision).
9.Extrinsic Eye Muscles
Description Six muscles attached to the outer surface of the eye.
Function Control the movement of the eyeball in various directions.
Muscles Include the superior, inferior, medial, and lateral rectus muscles, and the superior and inferior oblique muscles.
10.Conjunctiva
Description A thin, transparent membrane that covers the front of the eye and lines the inside of the eyelids.
Function Protects the eye from debris and infection and helps keep the eye moist.
Blood Supply
Central Retinal Artery
Supplies blood to the inner retinal layers.
Short and Long Posterior Ciliary Arteries
Supply the outer retinal layers and the choroid.
Venous Drainage
The blood from the eye is drained through the central retinal vein and the vortex veins into the superior and inferior ophthalmic veins.
🔸3.Anatomy of nephron
ANSWER:- Anatomy of the NephronThe nephron is the fundamental functional unit of the kidney, responsible for filtering blood, removing waste, and regulating water and electrolyte balance. Each kidney contains approximately 1 to 1.5 million nephrons, each composed of a renal corpuscle and a renal tubule.
Key Structures of the Nephron
Renal Corpuscle:
Components:
Includes the glomerulus and Bowman’s capsule.
Function:
Filters blood plasma to form a filtrate that enters the renal tubule.
Glomerulus:
Description:
A network of capillaries located at the beginning of the nephron.
Function:
Serves as the initial site of blood filtration. Blood enters via the afferent arteriole and leaves via the efferent arteriole.
Features:
The capillary walls are permeable, allowing water and small solutes to pass through while retaining larger molecules like proteins and cells.
Bowman’s Capsule: Description:
A double-walled, cup-shaped structure that encases the glomerulus.
Function:
Collects the filtrate from the glomerulus and funnels it into the renal tubule.
Features:
The inner layer (visceral layer) is made of specialized cells called podocytes that wrap around the glomerular capillaries. The outer layer (parietal layer) is a simple squamous epithelium.
Renal Tubule: Components :
Consists of the proximal convoluted tubule, loop of Henle, distal convoluted tubule, and the collecting duct.
Function:
Processes the filtrate through reabsorption and secretion to form urine.
Proximal Convoluted Tubule (PCT): Description:
The first segment of the renal tubule, located in the cortex.
Function:
Reabsorbs about 65-70% of the filtrate, including water, glucose, amino acids, and electrolytes, back into the bloodstream. It also secretes some substances into the filtrate.
Features:
Lined with simple cuboidal epithelial cells rich in microvilli to increase surface area for reabsorption.
Loop of Henle: Description:
A U-shaped structure that extends into the medulla and then returns to the cortex.
Divisions:
Consists of a descending limb, a thin ascending limb, and a thick ascending limb.
Function:
Establishes a concentration gradient in the medulla, which is crucial for water reabsorption and urine concentration.
Features: Descending Limb:
Permeable to water but not to solutes, allowing water to be reabsorbed.
Thin Ascending Limb:
Permeable to ions but not water, allowing passive reabsorption of sodium and chloride.
Thick Ascending Limb:
Actively reabsorbs sodium, potassium, and chloride ions but is impermeable to water.
Distal Convoluted Tubule (DCT): Description:
The segment following the loop of Henle, located in the cortex.
Function:
Further adjusts the filtrate through selective reabsorption and secretion, particularly of ions like sodium, potassium, and calcium.
Features:
Lined with simple cuboidal epithelial cells that have fewer microvilli than the PCT.
Collecting Duct: Description: A duct system that collects urine from multiple nephrons and extends from the cortex through the medulla to the
renal pelvis.Function: Finalizes the concentration and volume of urine. It responds to antidiuretic hormone (ADH) to adjust water reabsorption.
Features:
The cells in the collecting duct can change their permeability to water in response to hormonal signals, allowing fine-tuning of urine concentration.Blood Supply and Microcirculation
Afferent Arteriole:
Description:
The small artery that delivers blood to the glomerulus.
Function:
Regulates blood flow into the glomerulus.
Efferent Arteriole: Description: The small artery that carries blood away from the glomerulus.
Function:
Regulates outflow from the glomerulus and leads to the peritubular capillaries and vasa recta.
Peritubular Capillaries: Description: A network of capillaries surrounding the renal tubule.
Function:
Facilitates reabsorption and secretion between the blood and the renal tubules. Reabsorbed substances from the tubules return to the bloodstream through these capillaries.
Vasa Recta: Description:
A series of straight capillaries in the medulla.
Function:
Helps maintain the osmotic gradient established by the loop of Henle, crucial for concentrating urine.
Features:
Works in conjunction with the loop of Henle to facilitate countercurrent exchange, preserving the medullary gradient.
🔸4.Microscopic structure of bone
ANSWER:- Microscopic Structure of Bone Bone, tissue, or osseous tissue, is a complex, dynamic structure that supports and protects the body’s organs, facilitates movement, and serves as a reservoir for minerals. The microscopic anatomy of bone reveals intricate details about its composition and function, comprising cellular and extracellular components organized into compact and spongy bone structures.
Key Components of Bone Tissue Bone Cells: Osteocytes: Description :
Mature bone cells embedded within the bone matrix.
Function:
Maintain the bone matrix and detect mechanical stress, which they communicate to osteoblasts and osteoclasts.
Location:
Reside in small spaces called lacunae, connected by tiny channels called canaliculi.
Osteoblasts: Description:
Bone-forming cellsy that synthesize and secrete the bone matrix.
Function:
Produce osteoid (the organic component of the bone matrix) and initiate mineralization.
Location:
Found on the bone surface, particularly active during bone growth and repair.
Osteoclasts: Description:
Large, multinucleated cells responsible for bone resorption.
Function:
Break down bone tissue by secreting enzymes and acids, a process essential for bone remodeling and calcium homeostasis.
Location:
Typically found in depressions on the bone surface known as Howship’s lacunae.
Osteoprogenitor Cells:Description:
Stem cells that differentiate into osteoblasts.
Function:
Play a crucial role in bone growth and repair.
Location:
Found in the periosteum and endosteum, the bone’s connective tissue linings.
Bone Matrix: Organic Component (Osteoid): Description:
Composed primarily of collagen fibers and ground substance (proteoglycans and glycoproteins).
Function:
Provides tensile strength and flexibility to the bone.
Inorganic Component (Mineral Salts):Description:
Mainly hydroxyapatite crystals (calcium phosphate and calcium carbonate).
Function:
Provides hardness and strength to the bone, making it resistant to compression.
Compact Bone (Cortical Bone):Description:
Dense and forms the outer layer of bones, providing strength and protection.
Structure:Osteon (Haversian System):
The fundamental unit of compact bone. Each osteon is a cylindrical structure running parallel to the bone’s long axis.
Central (Haversian) Canal:
Located at the center of each osteon, it contains blood vessels and nerves.
Lamellae: Concentric layers of bone matrix surrounding the central canal. Each layer has collagen fibers oriented in different directions to enhance strength.
Lacunae:
Small spaces between lamellae housing osteocytes.
Canaliculi:
Tiny channels connecting lacunae, allowing for the exchange of nutrients and waste between osteocytes and the blood supply.
Perforating (Volkmann’s) Canals:
Transverse channels that connect central canals of different osteons, facilitating the blood and nerve supply throughout the bone.
Spongy Bone (Cancellous or Trabecular Bone):Description:
Lighter, less dense than compact bone, found primarily at the ends of long bones and within the interior of other bones.
Structure: Trabeculae: The network of thin, bony plates or rods that form the spongy structure, oriented along lines of stress.
Marrow Spaces:
The gaps between trabeculae are filled with bone marrow, which can be either red (producing blood cells) or yellow (storing fat).
No Osteons:
Unlike compact bone, spongy bone does not contain osteons. Instead, it relies on the marrow and surrounding blood vessels for nutrient and waste exchange.
Osteocytes in Lacunae:
Osteocytes are still present within lacunae but are connected by canaliculi directly to the marrow spaces.
Periosteum and Endosteum:Periosteum:Description:
A dense layer of vascular connective tissue enveloping the bones except at the surfaces of the joints.
Function:
Provides attachment for tendons and muscles, contains osteoprogenitor cells for growth and healing, and supplies nutrients to the bone.
Structure:
Composed of an outer fibrous layer and an inner cellular layer.
Endosteum: Description:
A thin vascular membrane lining the inner surface of the bone cavities, including the medullary cavity and the trabeculae of spongy bone.
Function:
Contains osteoprogenitor cells and is involved in bone growth, repair, and remodeling.
🔸5.Structure of stomach
ANSWER:- Structure of the Stomach
The stomach is a key organ in the digestive system, serving as a reservoir and mixing chamber where food is broken down into a semi-liquid form called chyme. It plays a crucial role in the mechanical and chemical digestion of food, producing gastric juices that include hydrochloric acid and digestive enzymes
Structure of the Stomach (Concise Overview)
The stomach is a J-shaped, muscular organ located between the esophagus and the small intestine, playing a critical role in digestion. :
1.Regions of the Stomach
Cardia
The area where the esophagus meets the stomach. It contains the lower esophageal sphincter that regulates the entry of food and prevents acid reflux.
Fundus
The dome-shaped top portion that stores undigested food and gases.
Body
The largest central part where most mixing and digestion occur.
Antrum (Pyloric Antrum)
The lower section that grinds food and controls its passage into the duodenum.
Pylorus
The narrow region leading to the small intestine, featuring the pyloric sphincter that regulates the flow of chyme into the duodenum.
2.Curvatures
Greater Curvature
The long, convex curve on the left side, providing attachment for the greater omentum.
Lesser Curvature
The short, concave curve on the right side, providing attachment for the lesser omentum.
3.Layers of the Stomach Wall
Mucosa
The innermost layer, containing glands that produce gastric juice (acid and enzymes) and mucus to protect the stomach lining.
Submucosa
A supportive layer of connective tissue with blood vessels, nerves, and lymphatics.
Muscularis Externa
Consists of three layers of muscle (inner oblique, middle circular, and outer longitudinal) that facilitate mixing and propulsion of food.
Serosa
The outermost layer, a thin membrane that reduces friction as the stomach moves.
4.Gastric Glands
Found within the mucosa, these glands contain various cell types:
Parietal Cells
Secrete hydrochloric acid and intrinsic factor.
Chief Cells
Produce pepsinogen, an inactive enzyme that is converted to pepsin.
Mucous Cells
Secrete mucus to protect the stomach lining.
G Cells
Release the hormone gastrin, stimulating acid production.
5.Blood Supply and Innervation
Blood Supply
Provided by the gastric arteries from the celiac trunk.
Innervation
Includes both sympathetic and parasympathetic nerves, with the vagus nerve enhancing digestive activity.
Understanding the structure of the stomach is essential for grasping its role in digestion and how various disorders can affect its function.
⏩ Q.3 Fill in the blanks (08)
🔸1.The volume of blood pump out from the left ventricle per minute is called—-Cardiac output.
🔸2.Axial skeletal consist of—– bones. 80 bones.
🔸3.The longest muscle of the human body is——sartorius muscle.
🔸4.Blood is ——-tissue.Connective tissue.
🔸5.The tenth cranial nerve is——Vagus nerve.
🔸6.The Functional Residual Capacity (FRC) of the lungs is——- ml.2,300 to 2,500 milliliters (ml).
🔸7.——are suicidal bags of cell.Lysosomes.
🔸8.——-enzyme is secreted by the salivary glands in the buccal cavity for the digestion of carbohydrates amylase.
⏩ SECTION-II⏪
⏩ Q.4 Long essay type. (Any One) (10)
🔸1.Define Endocrine glands & describe the functions of thyroid gland in detail. [2+8]
ANSWER:- Endocrine glands
are ductless glands that secrete hormones directly into the bloodstream. These hormones then travel to target organs or tissues, where they exert their effects by binding to specific receptors, regulating various physiological processes and maintaining homeostasis in the body. Endocrine glands play crucial roles in growth, metabolism, reproduction, stress response, and many other functions.
Thyroid Gland:
Functions in Detail The thyroid gland is a butterfly-shaped endocrine gland located in the front of the neck, just below the Adam’s apple (thyroid cartilage). It produces hormones that regulate metabolism, growth, and development. Here’s a detailed look at the functions of the thyroid gland:
1.Thyroid Hormone Synthesis
The thyroid gland produces two main hormones: triiodothyronine (T3) and thyroxine (T4).
These hormones are synthesized from the amino acid tyrosine and the element iodine, which is obtained from the diet.
Thyroid hormone synthesis is regulated by thyroid-stimulating hormone (TSH) secreted by the pituitary gland.
2.Regulation of Metabolism
Thyroid hormones play a crucial role in regulating basal metabolic rate (BMR), the rate at which the body consumes energy at rest.
They stimulate the breakdown of carbohydrates, fats, and proteins, providing energy for cellular processes.
Thyroid hormones also influence the metabolism of vitamins, minerals, and other hormones.
3.Maintenance of Body Temperature
Thyroid hormones help regulate body temperature by influencing metabolic processes.
They increase heat production through increased oxygen consumption and energy expenditure.
4.Regulation of Growth and Development
Thyroid hormones are essential for normal growth and development, particularly in children.
They promote the development of bones, muscles, and the nervous system.
Thyroid hormone deficiency during fetal development or early childhood can lead to stunted growth and intellectual impairment (a condition known as cretinism).
5.Cardiovascular Effects
Thyroid hormones influence heart rate, cardiac output, and blood pressure.
They increase heart rate and cardiac contractility, leading to increased blood flow and oxygen delivery to tissues.
6.Regulation of Calcium Homeostasis
Thyroid hormones indirectly influence calcium levels by affecting vitamin D metabolism and bone turnover.
They promote calcium absorption in the intestines and bone resorption, maintaining calcium balance in the body.
7.Regulation of Energy Balance
Thyroid hormones influence appetite and energy expenditure, thereby playing a role in weight regulation.
Hypothyroidism (underactive thyroid) can lead to weight gain, while hyperthyroidism (overactive thyroid) can cause weight loss.
Understanding the functions of the thyroid gland is essential for diagnosing and managing thyroid disorders and ensuring overall metabolic health.
🔸2.What is blood pressure? Explain the factors influencing the blood pressure. [2+8]
ANSWER:- Blood pressure is the force exerted by circulating blood against the walls of blood vessels, primarily arteries, as the heart pumps blood throughout the body. It is measured in millimeters of mercury (mmHg) and is expressed as two numbers: systolic pressure (the pressure when the heart contracts) over diastolic pressure (the pressure when the heart relaxes between beats). For example, a blood pressure reading of 120/80 mmHg means a systolic pressure of 120 mmHg and a diastolic pressure of 80 mmHg.
Factors Influencing Blood Pressure:
Cardiac Output (CO):Cardiac output refers to the volume of blood ejected by the heart per minute.An increase in cardiac output leads to higher blood pressure, as more blood is pumped into the arteries.Factors influencing cardiac output include heart rate, stroke volume (the volume of blood ejected per heartbeat), and contractility of the heart muscle.
Peripheral Resistance: Peripheral resistance is the resistance to blood flow in the blood vessels, primarily arterioles.Vasoconstriction (narrowing of blood vessels) increases resistance and raises blood pressure, while vasodilation (widening of blood vessels) decreases resistance and lowers blood pressure.Factors affecting peripheral resistance include the diameter of blood vessels, blood viscosity, and the length of blood vessels.
Blood Volume: Blood volume refers to the total volume of blood circulating in the body.An increase in blood volume leads to increased blood pressure, while a decrease in blood volume lowers blood pressure.Factors influencing blood volume include fluid intake, fluid loss (e.g., through urine or sweating), and hormonal regulation of fluid balance (e.g., aldosterone and antidiuretic hormone).
Elasticity of Arteries: Arteries have elastic properties that allow them to stretch and recoil in response to changes in blood pressure.Loss of arterial elasticity (e.g., due to aging or atherosclerosis) leads to increased arterial stiffness, raising blood pressure.Factors influencing arterial elasticity include age, genetics, and lifestyle factors such as diet and exercise.
Autonomic Nervous System: The autonomic nervous system regulates blood pressure through sympathetic and parasympathetic pathways.
Sympathetic activation (fight-or-flight response) increases heart rate and peripheral resistance, raising blood pressure.Parasympathetic activation (rest-and-digest response) decreases heart rate and peripheral resistance, lowering blood pressure.
Hormonal Regulation: Hormones such as adrenaline (epinephrine), noradrenaline (norepinephrine), renin-angiotensin-aldosterone system (RAAS), and vasopressin (antidiuretic hormone) play roles in blood pressure regulation.These hormones can influence cardiac output, peripheral resistance, and fluid balance, thereby affecting blood pressure.
Renal Function: The kidneys play a crucial role in regulating blood pressure by adjusting blood volume and electrolyte balance through processes such as filtration, reabsorption, and secretion.Hormones like aldosterone and angiotensin II regulate sodium and water retention in the kidneys, affecting blood volume and pressure.
⏩ Q.5 Write short notes on following. (Any Four)
🔸1.Pulmonary blood circulation
ANSWER:- Pulmonary Circulation refers to the circulation of blood between the heart and the lungs. It is responsible for oxygenating the blood and removing carbon dioxide, a waste product of cellular metabolism. Here’s an overview of pulmonary circulation:
Pulmonary Circulation Process:
1.Deoxygenated Blood Returns to the Heart
Deoxygenated blood from the body enters the right atrium of the heart through the superior and inferior vena cavae.
The right atrium contracts, pumping blood through the tricuspid valve into the right ventricle.
2.Pulmonary Artery Carries Blood to the Lungs
From the right ventricle, blood is pumped through the pulmonary artery, which splits into the right and left pulmonary arteries.
The pulmonary arteries carry deoxygenated blood to the lungs for oxygenation.
3.Gas Exchange in the Lungs
In the lungs, deoxygenated blood flows through the pulmonary capillaries surrounding the alveoli (tiny air sacs).
Oxygen diffuses from the alveoli into the blood, while carbon dioxide diffuses from the blood into the alveoli.
4.Oxygenated Blood Returns to the Heart
Oxygenated blood from the lungs enters the left atrium of the heart through the pulmonary veins.
The left atrium contracts, pumping blood through the mitral valve into the left ventricle.
5.Systemic Circulation
From the left ventricle, oxygenated blood is pumped into the systemic circulation through the aorta, supplying oxygen and nutrients to the body’s tissues.
Systemic circulation delivers oxygenated blood to organs, muscles, and cells, where oxygen is used for cellular metabolism.
Key Features of Pulmonary Circulation:
Low Pressure
Pulmonary circulation operates at lower pressure compared to systemic circulation, as the lungs do not require as much force to pump blood through them.
Short Distance
The distance between the heart and lungs is relatively short, allowing for efficient gas exchange.
High Blood Flow
Despite lower pressure, pulmonary circulation has a high blood flow rate to ensure adequate oxygenation of blood.
Selective Perfusion
Blood flow to different areas of the lungs can be regulated based on ventilation-perfusion matching, ensuring optimal gas exchange efficiency.
Regulation
Pulmonary circulation is regulated by neural, hormonal, and local factors to maintain adequate oxygenation and carbon dioxide removal.
Clinical Relevance:
Pulmonary Hypertension
Elevated blood pressure in the pulmonary arteries can lead to heart failure and other complications.
Pulmonary Embolism Blockage of pulmonary arteries by blood clots can disrupt blood flow and impair gas exchange.
Pulmonary Edema Accumulation of fluid in the lungs can impair gas exchange and lead to respiratory distress.
Respiratory Diseases Conditions such as chronic obstructive pulmonary disease (COPD), asthma, and pneumonia can affect pulmonary circulation and gas exchange.
🔸2.Functions of cerebrum.
ANSWER:- The cerebrum, the largest part of the brain, plays a central role in higher brain functions, including cognition, emotion, memory, and voluntary movement. Here are the key functions of the cerebrum:
1.Cognition and Intelligence The cerebrum is responsible for various cognitive processes, including perception, attention, reasoning, problem-solving, and decision-making.
It integrates sensory information from the environment and internal states to form perceptions and make sense of the world.
2.Motor Control The cerebrum controls voluntary movement through the primary motor cortex, located in the frontal lobe.
It plans and executes complex movements, including fine motor skills, gross motor skills, and coordinated movements involving multiple muscle groups.
3.Sensory Processing The cerebrum receives and processes sensory information from the body’s senses, including touch, taste, smell, hearing, and vision.
Different regions of the cerebrum are specialized for processing specific sensory modalities, with sensory input organized into topographic maps.
4.Language and Communication Language processing, including speech production, comprehension, and interpretation, is primarily located in the left hemisphere of the cerebrum, especially in areas like Broca’s area and Wernicke’s area.
The cerebrum enables complex language functions such as syntax, semantics, and pragmatics, facilitating communication and social interaction.
5.Memory and Learning The cerebrum is crucial for memory formation, storage, and retrieval, involving various regions such as the hippocampus, amygdala, and prefrontal cortex.
It plays a role in both short-term memory (working memory) and long-term memory consolidation, contributing to learning and cognitive development.
6.Emotion and Behavior Emotional processing and regulation involve interactions between the cerebrum and limbic system structures such as the amygdala, hippocampus, and prefrontal cortex.
The cerebrum influences emotional responses, mood regulation, and behavioral control, contributing to emotional intelligence and adaptive behavior.
7.Executive Functions Executive functions refer to higher-order cognitive processes involved in goal setting, planning, organization, inhibition, and self-regulation.
The cerebrum, particularly the prefrontal cortex, is essential for executive functions, allowing individuals to adaptively respond to environmental demands and achieve goals.
8.Consciousness and Awareness The cerebrum is associated with consciousness, self-awareness, and subjective experience.
It integrates sensory information, internal states, and cognitive processes to generate a unified conscious experience of the world and oneself.
Overall, the cerebrum is essential for various aspects of human cognition, behavior, and consciousness, making it the most complex and versatile structure in the brain.
🔸3.Regulation of body temperature.
ANSWER:- The regulation of body temperature, also known as thermoregulation, is a critical physiological process that maintains the body’s internal temperature within a narrow range despite external temperature fluctuations. Here’s an overview of how the body regulates its temperature:
1.Hypothalamus The hypothalamus, located in the brain, serves as the body’s thermostat, monitoring core body temperature and coordinating responses to maintain homeostasis.
It contains thermoregulatory centers that receive input from temperature receptors in the skin, spinal cord, and internal organs.
2.Heat Production The body generates heat through metabolic processes, such as cellular respiration in the mitochondria of cells, which produce energy (ATP) and heat as byproducts.
Muscle contraction, especially shivering, increases heat production by generating friction between muscle fibers.
3.Heat Loss:
Heat is lost from the body through several mechanisms, primarily radiation, conduction, convection, and evaporation:
- Radiation: Transfer of heat from the body’s surface to cooler surroundings.
- Conduction: Direct transfer of heat from the body to cooler objects in contact with the skin.
- Convection: Transfer of heat to the surrounding air or water, facilitated by movement or airflow.
- Evaporation: Conversion of liquid sweat on the skin’s surface into vapor, carrying away heat.
- Blood vessels near the skin’s surface dilate (vasodilation) to increase blood flow, facilitating heat loss through radiation and convection.
Sweating:
- Sweating is a crucial mechanism for heat dissipation, especially in hot environments or during physical activity.
- Eccrine sweat glands in the skin secrete sweat, which evaporates and cools the body’s surface.
- Sweating is regulated by the hypothalamus in response to elevated core body temperature or external heat exposure.
Shivering and Non-Shivering Thermogenesis:
- Shivering, involuntary muscle contractions, generates heat by increasing metabolic activity in skeletal muscles.
- Non-shivering thermogenesis occurs in brown adipose tissue, which contains a high concentration of mitochondria specialized for heat production (uncoupled respiration).
Behavioral Responses:
- Behavioral responses, such as seeking shade or shelter, adjusting clothing, and changing activity levels, help regulate body temperature.
- These responses are influenced by sensory input, past experiences, and cognitive processes.
Hormonal Regulation:
- Hormones such as thyroid hormone, adrenaline (epinephrine), and cortisol can influence thermoregulation by modulating metabolic rate, heat production, and heat loss.
- Thyroid hormone increases basal metabolic rate, while adrenaline activates the sympathetic nervous system, promoting heat production and mobilizing energy reserves.
Thermoregulatory Set Point:
- The hypothalamus maintains a thermoregulatory set point, typically around 37°C (98.6°F), which represents the desired core body temperature.
- When core body temperature deviates from the set point, thermoregulatory mechanisms are activated to restore homeostasis.
Effective thermoregulation is crucial for maintaining optimal physiological function, preventing overheating (hyperthermia) or excessive cooling (hypothermia), and ensuring survival in diverse environmental conditions.
🔸4.Physiology of hearing
ANSWER:- The physiology of hearing involves a complex series of events that convert sound waves into electrical signals, which are then interpreted by the brain as auditory sensations. Here’s an overview of the key components and processes involved in hearing:
Sound Waves Transmission: Sound waves travel through the air as vibrations produced by a sound source, such as vocal cords or a musical instrument.The outer ear, consisting of the pinna (auricle) and the external auditory canal, collects and directs sound waves toward the eardrum (tympanic membrane).
Tympanic Membrane and Middle Ear: When sound waves reach the tympanic membrane, they cause it to vibrate.
- The vibrations are transmitted through the three small bones of the middle ear: the malleus (hammer), incus (anvil), and stapes (stirrup).
- The movement of the stapes against the oval window of the cochlea transfers the vibrations to the fluid-filled inner ear.
Cochlea and Inner Ear:
- The cochlea is a spiral-shaped, fluid-filled structure in the inner ear that contains the sensory receptors for hearing, called hair cells.
- As the fluid in the cochlea vibrates, it causes the basilar membrane to move, which in turn stimulates the hair cells.
- Hair cells are specialized sensory cells with hair-like projections (stereocilia) that convert mechanical vibrations into electrical signals.
Transduction of Sound Signals:
- When the stereocilia of the hair cells are deflected by the movement of the basilar membrane, ion channels open, allowing ions to enter the hair cells.
- This influx of ions generates electrical signals, which are transmitted along the auditory nerve (cochlear nerve) to the brain.
Auditory Pathways and Brain Processing:
- The auditory nerve carries the electrical signals from the cochlea to the brainstem, where they are relayed to the auditory cortex via a series of neural pathways.
- In the auditory cortex, located in the temporal lobe of the brain, the electrical signals are interpreted as auditory sensations, including pitch, loudness, and timbre.
- The brain integrates auditory information with other sensory inputs and cognitive processes to perceive and recognize sounds, including speech and music.
Auditory Processing and Perception:
- Auditory processing involves the brain’s ability to analyze and interpret complex auditory stimuli, such as speech sounds, music, and environmental noises.
- This process includes tasks such as sound localization, speech recognition, and auditory memory, which are essential for communication and social interaction.
🔸5.Functions of liver
ANSWER:- The liver is a vital organ with a wide range of functions essential for maintaining overall health and homeostasis. Here are the key functions of the liver:
Metabolism:
- Carbohydrate metabolism: The liver helps regulate blood glucose levels by storing excess glucose as glycogen (glycogenesis) and releasing glucose into the bloodstream as needed (glycogenolysis).
- Lipid metabolism: It synthesizes and metabolizes fats, including cholesterol and triglycerides, and produces bile, which emulsifies fats for digestion.
- Protein metabolism: The liver synthesizes proteins, including albumin, clotting factors (such as fibrinogen and prothrombin), and complement proteins.
Detoxification:
- The liver plays a crucial role in detoxifying harmful substances, including drugs, alcohol, metabolic waste products, and environmental toxins.
- Hepatocytes (liver cells) contain enzymes that metabolize and neutralize toxins, converting them into less harmful substances that can be excreted by the body.
Bile Production:
- The liver produces bile, a greenish-yellow fluid that aids in the digestion and absorption of fats in the small intestine.
- Bile contains bile acids, cholesterol, bilirubin (a waste product of red blood cell breakdown), and other substances necessary for emulsifying fats and facilitating their digestion.
Storage:
- The liver serves as a storage reservoir for various nutrients and substances, including glycogen (stored glucose), vitamins (such as vitamins A, D, E, and K), and minerals (such as iron and copper).
- It also stores blood (in the form of blood volume) and acts as a storage site for fat-soluble toxins and metabolic waste products.
Synthesis of Blood Components:
- The liver synthesizes and releases blood proteins, including albumin, which helps maintain blood osmotic pressure, and clotting factors, which are essential for blood coagulation and hemostasis.
- It also produces other blood components, such as red blood cells (erythropoiesis) during fetal development and in cases of anemia.
Immune Function:
- The liver plays a role in immune function by removing bacteria, viruses, and other pathogens from the bloodstream (phagocytosis) and producing immune factors such as acute-phase proteins and complement proteins.
- Kupffer cells, specialized macrophages in the liver, help clear pathogens and debris from the blood.
Regulation of Hormones and Metabolites:
- The liver metabolizes and regulates circulating hormones and metabolites, including insulin, glucagon, thyroid hormones, and sex hormones.
- It helps maintain hormonal balance and metabolic homeostasis by regulating hormone clearance, metabolism, and receptor sensitivity.
Regeneration:
- The liver has a remarkable ability to regenerate and repair itself after injury or damage, thanks to the proliferation of hepatocytes.
- Liver regeneration enables recovery from various insults, including chemical toxicity, infections, and surgical resection.
Overall, the liver’s multifunctional role makes it indispensable for maintaining metabolic, digestive, immune, and detoxification processes in the body. Dysfunction of the liver can lead to serious health consequences, emphasizing the importance of liver health and preventive care.
⏩ Q.6 Fill in the blanks
🔸1.Shoulder joint is ——a type of synovial joint. ball-and-socket
🔸2.The longest vein of the human body is—— great saphenous vein
🔸3.——-lymphocytes are processed by the Thymus gland & provide cell mi immunity.T lymphocytes (T cells)
🔸4.The normal volume of CSF in an adult is——-150 milliliters (ml).
🔸5.There are—— cranial nerves in human.12 cranial nerve
🔸6.The fairly constant state of composition of the internal environment of the is called——-homeostasis
🔸7.Spleen is located in —–region. left upper quadrant
.
